Chalcones as Anti-Glioblastoma Stem Cell Agent Alone or as Nanoparticle Formulation Using Carbon Dots as Nanocarrier
Abstract
:1. Introduction
2. Materials and Methods
2.1. Chemistry
2.2. Cell Culture
2.3. In Vitro Drug Testing
2.4. Sphere Forming Assay
2.5. Western Blot Analysis
2.6. Synthesis of C-Dots-Trans-Chalcone Derivatives
2.7. Characterization of C-Dots-Trans-Chalcone Derivatives
2.8. Statistical Analysis
3. Results
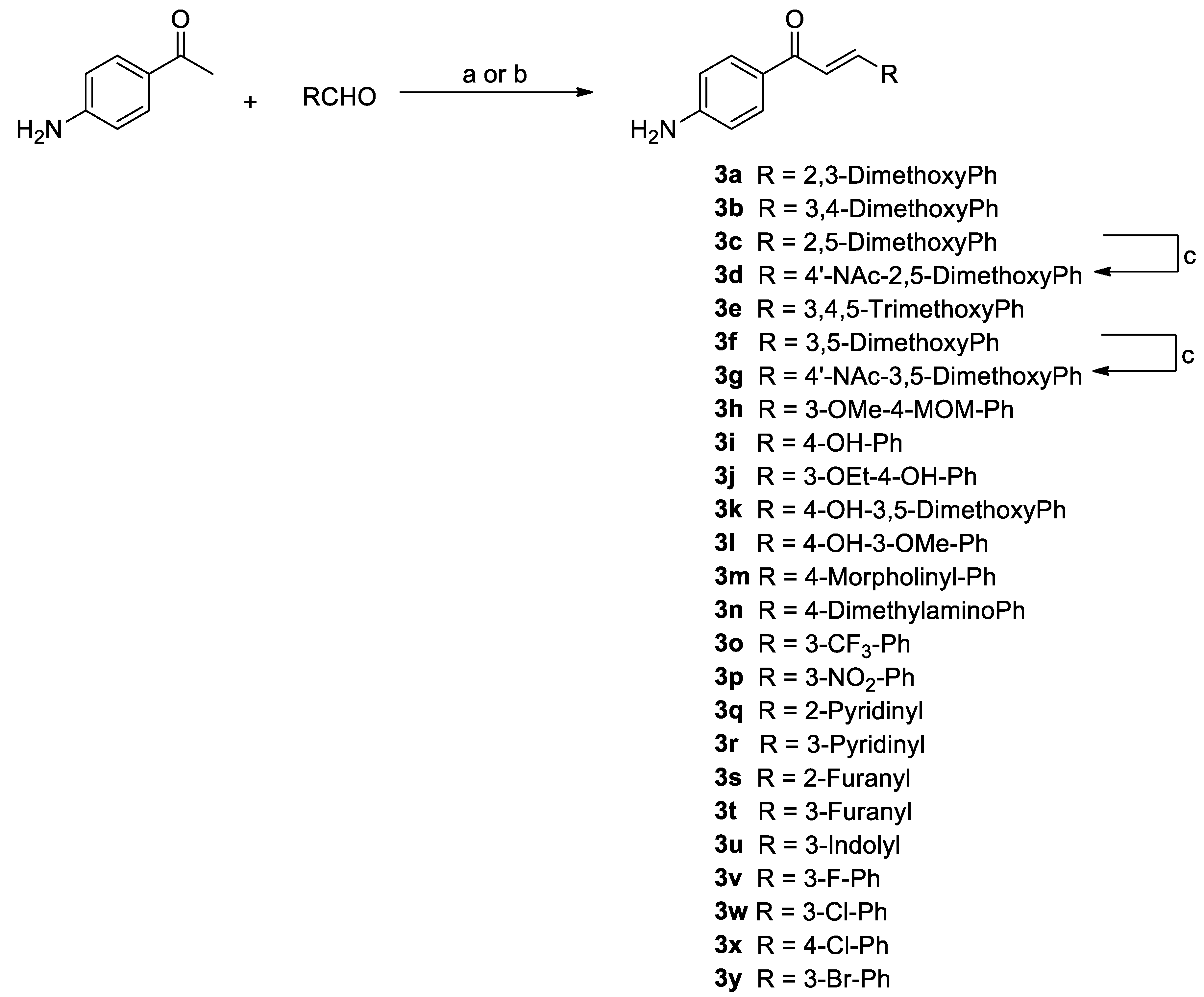
3.1. Synthesis of Chalcone Analogues
3.2. 4′-Aminoacetophenone Series
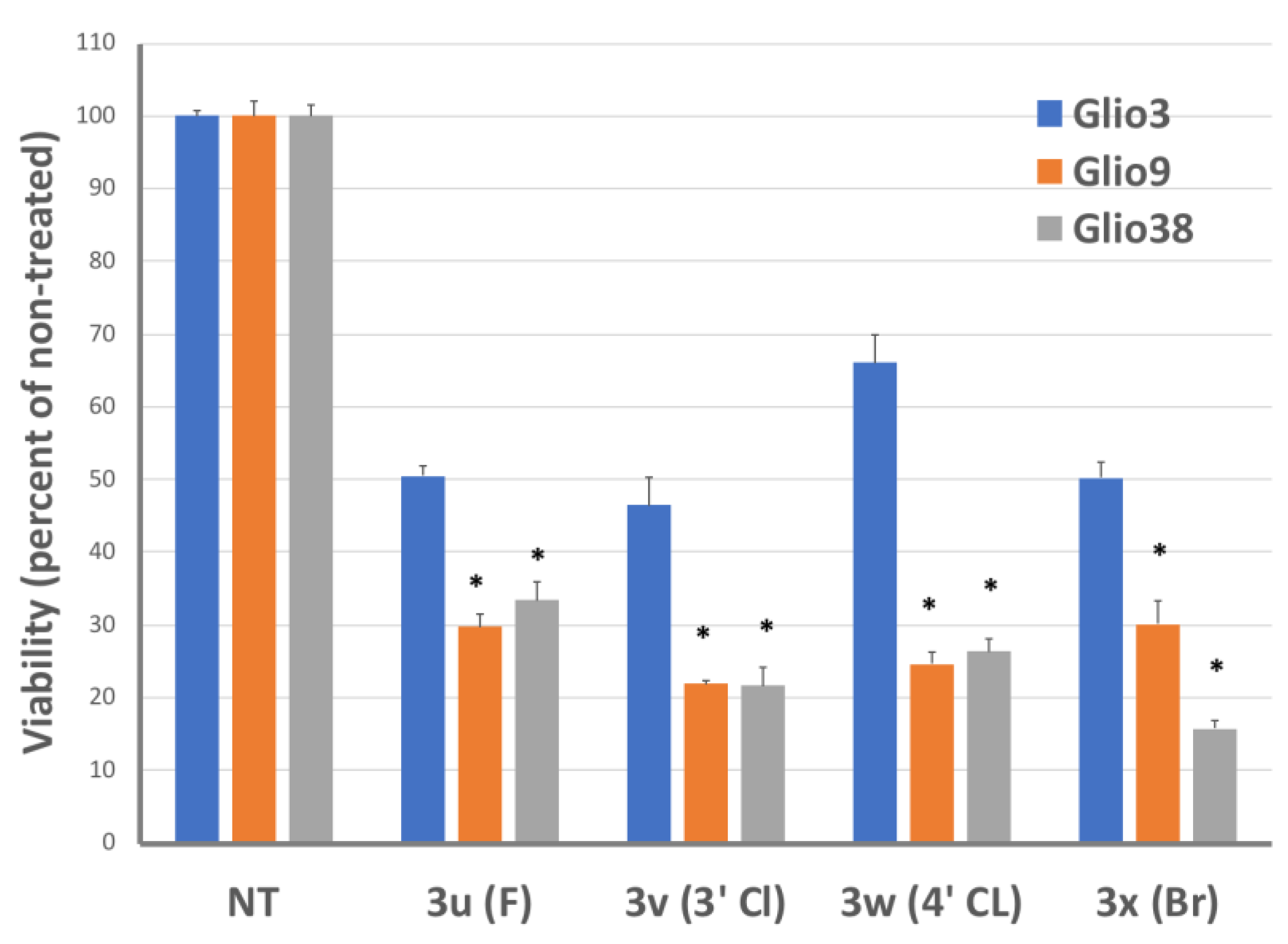
3.2.1. Halogens
3.2.2. Heteroaryl Chalcones
3.2.3. Nitro Chalcone
3.2.4. Novel Chalcones
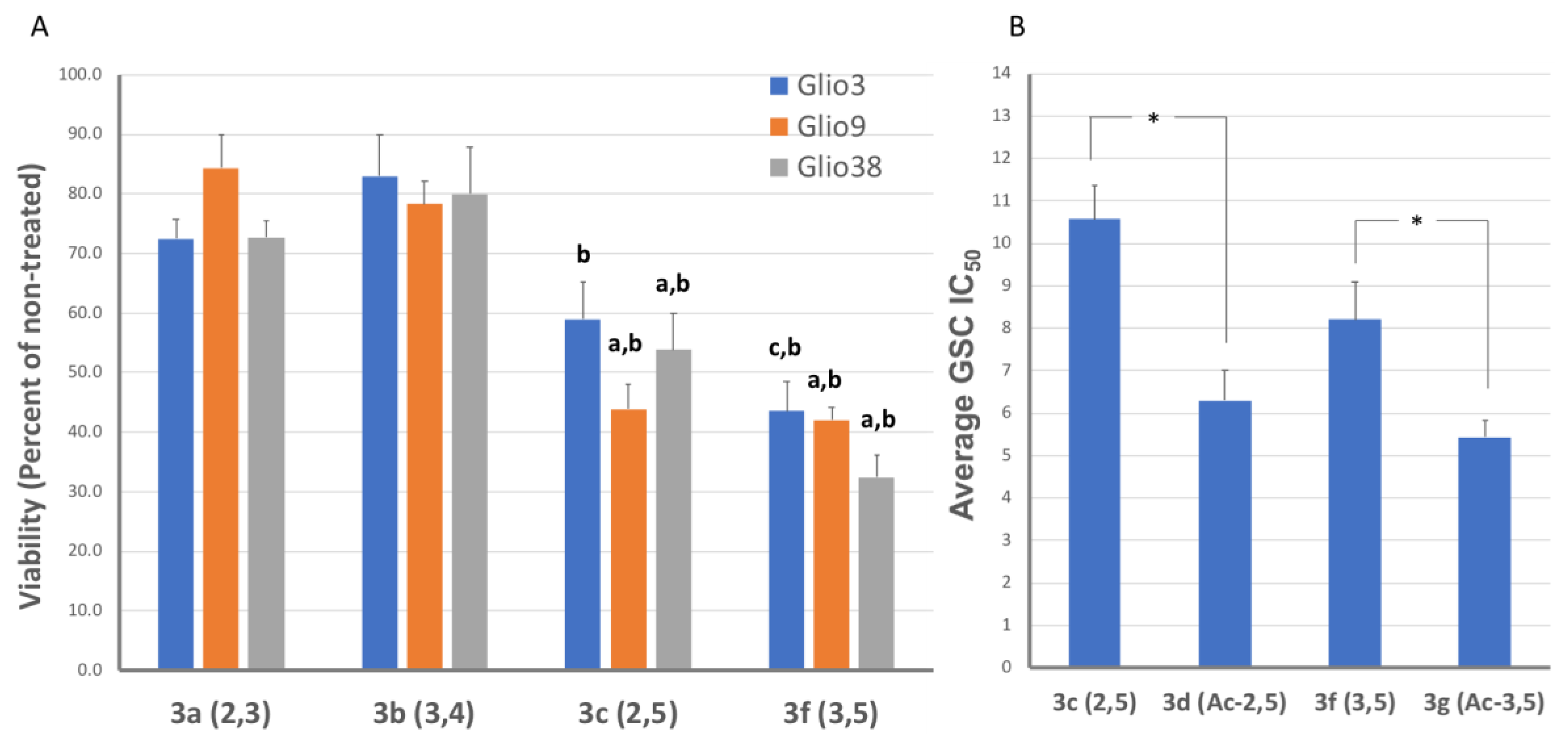
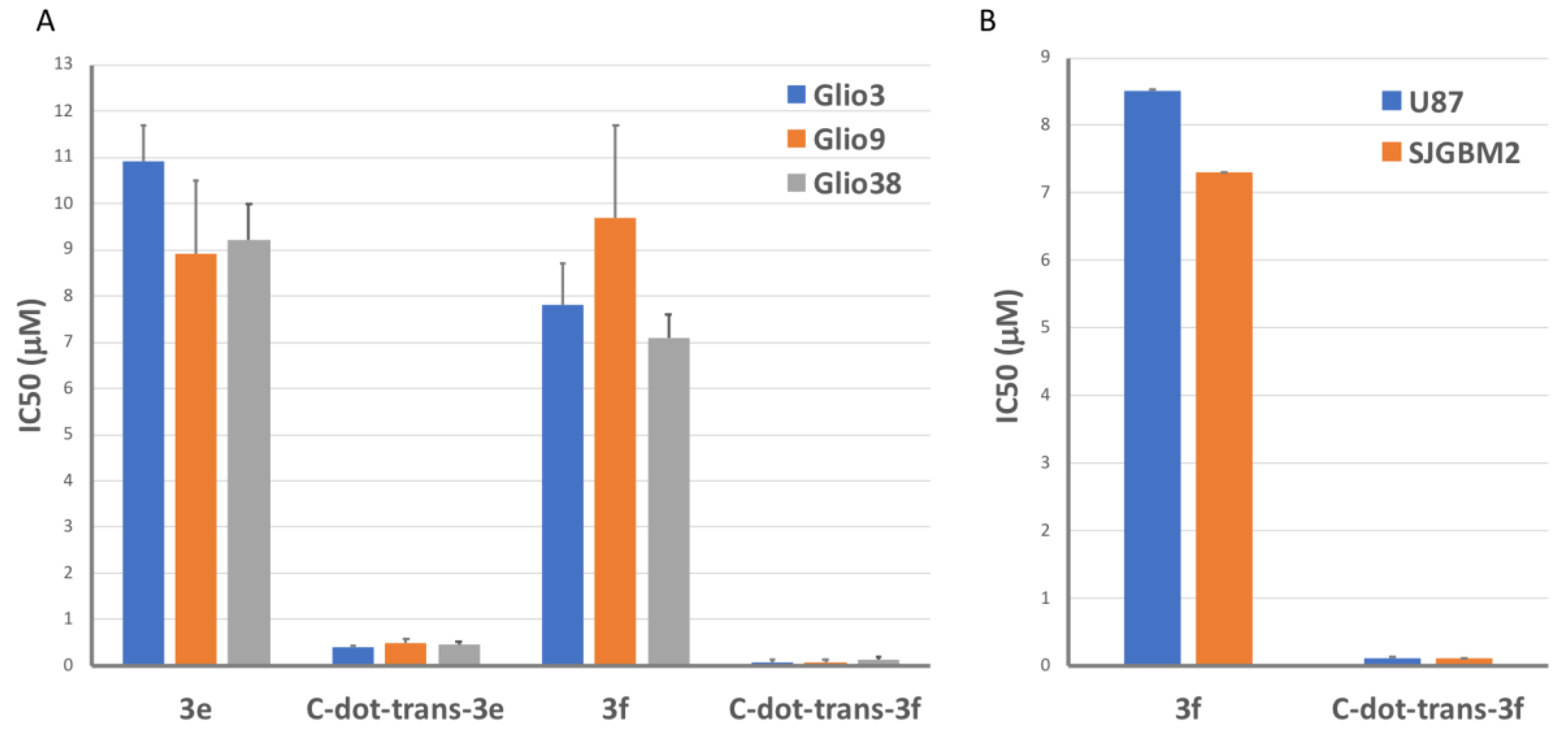
3.2.5. Methoxy Groups
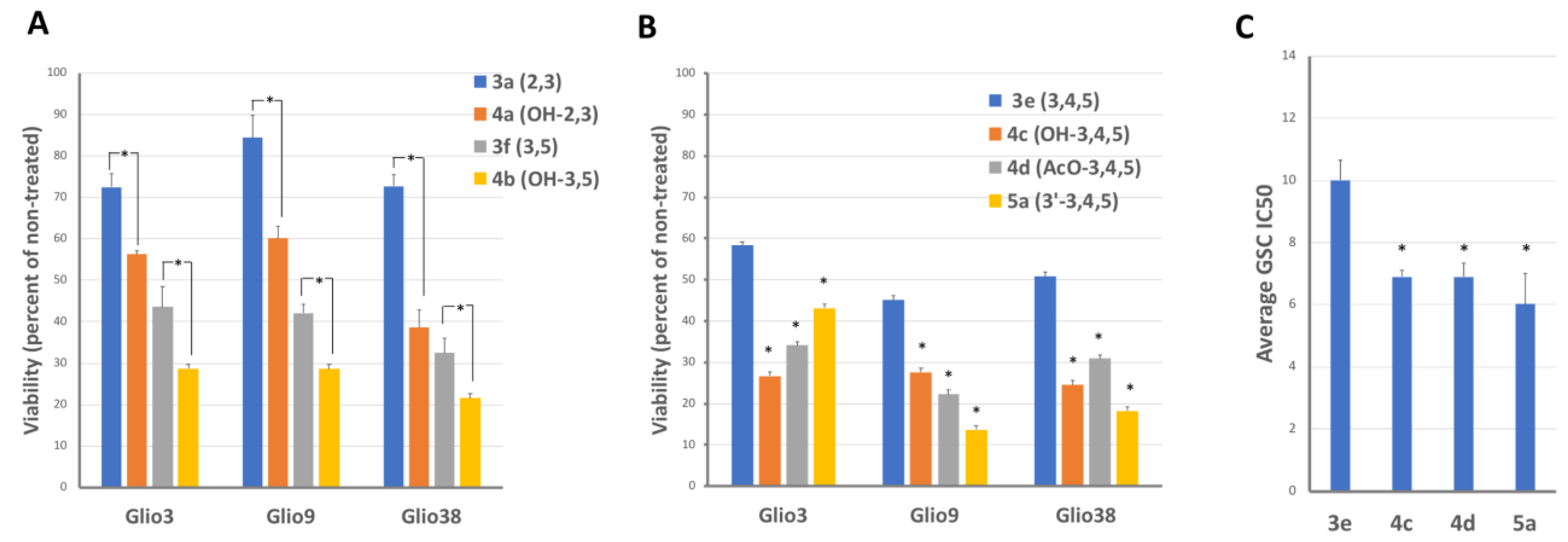
3.3. 4′-Hydroxyacetophenone Series and 3′-Amino Chalcone Derivatives
3.4. Chalcones Potential to Cross the Blood–Brain Barrier (BBB)
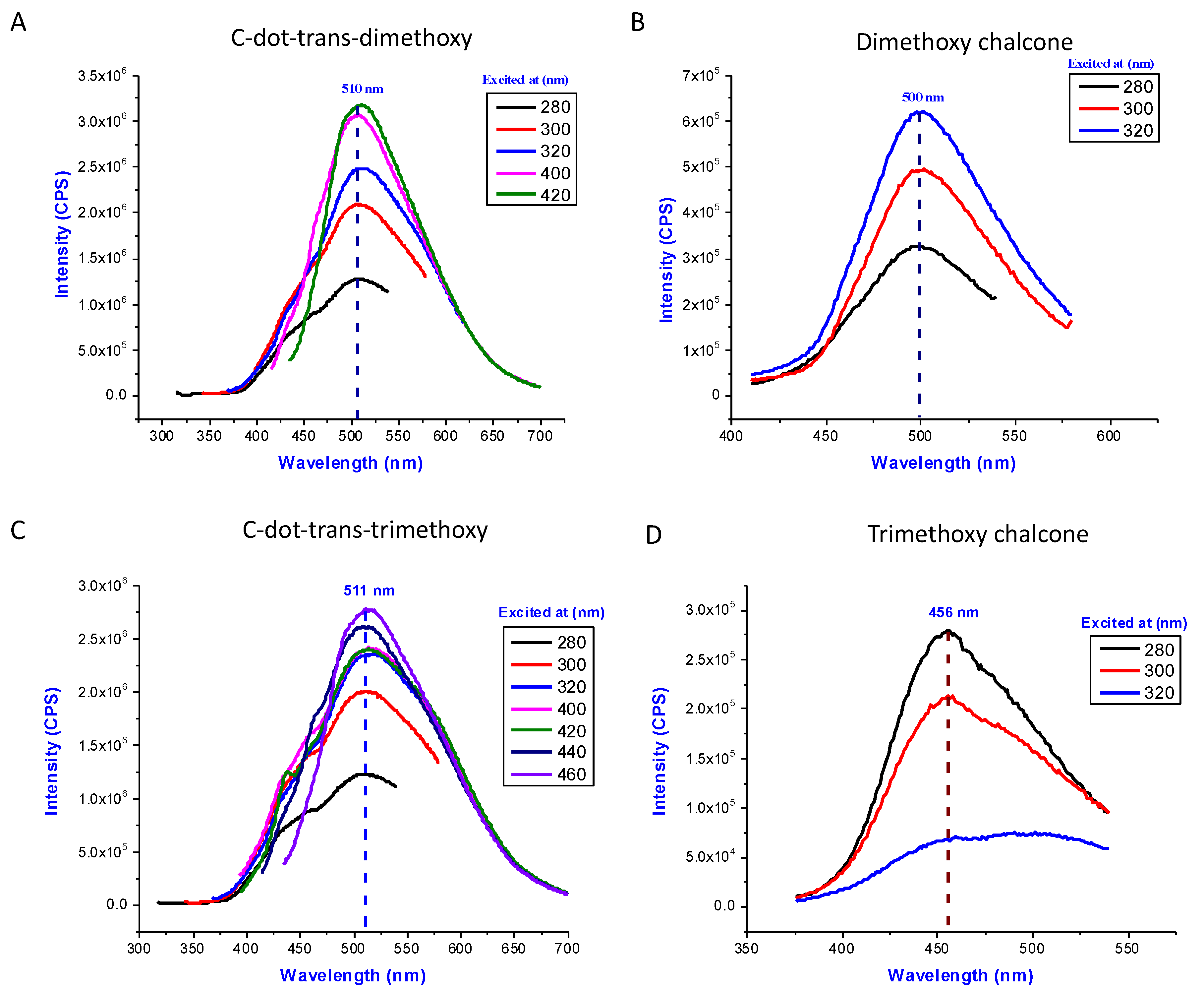
3.5. C-Dot-Trans-Chalcone Characterization
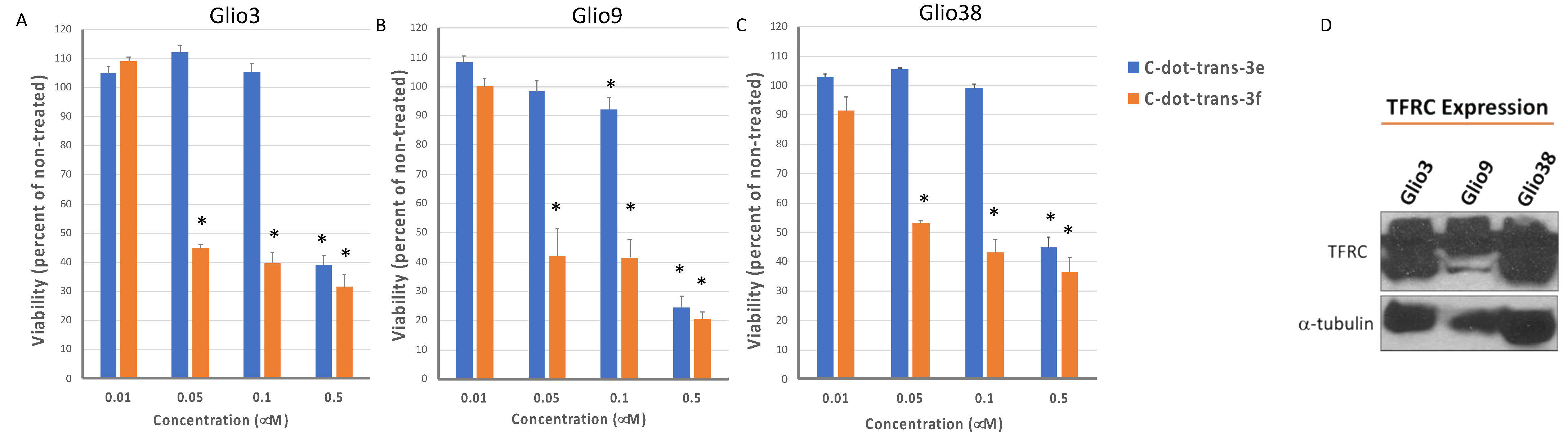
3.6. Effect of C-Dot-Trans-Chalcone Conjugate on GSC Viability and GSC Self-Renewal
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Stupp, R.; Hegi, M.E.; Mason, W.P.; Van Den Bent, M.J.; Taphoorn, M.J.; Janzer, R.C.; Ludwin, S.K.; Allgeier, A.; Fisher, B.; Belanger, K.; et al. Effects of radiotherapy with concomitant and adjuvant temozolomide versus radiotherapy alone on survival in glioblastoma in a randomised phase III study: 5-year analysis of the EORTC-NCIC trial. Lancet Oncol. 2009, 10, 459–466. [Google Scholar] [CrossRef]
- Safa, A.R.; Saadatzadeh, M.R.; Cohen-Gadol, A.A.; Pollok, K.E.; Bijangi-Vishehsaraei, K. Glioblastoma stem cells (GSCs) epigenetic plasticity and interconversion between differentiated non-GSCs and GSCs. Genes Dis. 2015, 2, 152–163. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Bao, S.; Wu, Q.; Sathornsumetee, S.; Hao, Y.; Li, Z.; Hjelmeland, A.B.; Shi, Q.; McLendon, R.E.; Bigner, D.D.; Rich, J.N. Stem Cell–like Glioma Cells Promote Tumor Angiogenesis through Vascular Endothelial Growth Factor. Cancer Res. 2006, 66, 7843–7848. [Google Scholar] [CrossRef] [Green Version]
- Wang, R.; Chadalavada, K.; Wilshire, J.; Kowalik, U.; Hovinga, K.E.; Geber, A.; Fligelman, B.; Leversha, M.; Brennan, C.; Tabar, V. Glioblastoma stem-like cells give rise to tumour endothelium. Nature 2010, 468, 829–833. [Google Scholar] [CrossRef] [PubMed]
- Hendrix, M.J.C.; Seftor, E.A.; Hess, A.R.; Seftor, R.E.B. Vasculogenic mimicry and tumour-cell plasticity: Lessons from melanoma. Nat. Rev. Cancer 2003, 3, 411–421. [Google Scholar] [CrossRef]
- Gersey, Z.C.; Rodriguez, G.A.; Barbarite, E.; Sanchez, A.; Walters, W.M.; Ohaeto, K.C.; Komotar, R.J.; Graham, R.M. Curcumin decreases malignant characteristics of glioblastoma stem cells via induction of reactive oxygen species. BMC Cancer 2017, 17, 99. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Shah, S.S.; Rodriguez, G.A.; Musick, A.; Walters, W.M.; de Cordoba, N.; Barbarite, E.; Marlow, M.M.; Marples, B.; Prince, J.S.; Komotar, R.J.; et al. Targeting Glioblastoma Stem Cells with 2-Deoxy-D-Glucose (2-DG) Potentiates Radiation-Induced Unfolded Protein Response (UPR). Cancers 2019, 11, 159. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Chen, J.; Li, Y.; Yu, T.-S.; McKay, R.M.; Burns, D.K.; Kernie, S.G.; Parada, L.F. A restricted cell population propagates glioblastoma growth after chemotherapy. Nature 2012, 488, 522–526. [Google Scholar] [CrossRef] [Green Version]
- Zhu, Z.; Khan, M.A.; Weiler, M.; Blaes, J.; Jestaedt, L.; Geibert, M.; Zou, P.; Gronych, J.; Bernhardt, O.; Korshunov, A.; et al. Targeting Self-Renewal in High-Grade Brain Tumors Leads to Loss of Brain Tumor Stem Cells and Prolonged Survival. Cell Stem Cell 2014, 15, 185–198. [Google Scholar] [CrossRef] [Green Version]
- Gimple, R.C.; Bhargava, S.; Dixit, D.; Rich, J.N. Glioblastoma stem cells: Lessons from the tumor hierarchy in a lethal cancer. Genes Dev. 2019, 33, 591–609. [Google Scholar] [CrossRef]
- Tang, X.; Zuo, C.; Fang, P.; Liu, G.; Qiu, Y.; Huang, Y.; Tang, R. Targeting Glioblastoma Stem Cells: A Review on Biomarkers, Signal Pathways and Targeted Therapy. Front. Oncol. 2021, 11, 701291. [Google Scholar] [CrossRef] [PubMed]
- Anselmo, A.C.; Mitragotri, S. Nanoparticles in the clinic. Bioeng. Transl. Med. 2016, 1, 10–29. [Google Scholar] [CrossRef]
- Liu, D.; Yang, F.; Xiong, F.; Gu, N. The Smart Drug Delivery System and Its Clinical Potential. Theranostics 2016, 6, 1306–1323. [Google Scholar] [CrossRef] [PubMed]
- Fukumura, D.; Jain, R.K. Tumor microenvironment abnormalities: Causes, consequences, and strategies to normalize. J. Cell. Biochem. 2006, 101, 937–949. [Google Scholar] [CrossRef]
- Tortorella, S.; Karagiannis, T.C. Transferrin Receptor-Mediated Endocytosis: A Useful Target for Cancer Therapy. J. Membr. Biol. 2014, 247, 291–307. [Google Scholar] [CrossRef] [PubMed]
- Schonberg, D.L.; Miller, E.T.; Wu, Q.; Flavahan, W.A.; Das, N.K.; Hale, J.S.; Hubert, C.G.; Mack, S.C.; Jarrar, A.M.; Karl, R.T.; et al. Preferential Iron Trafficking Characterizes Glioblastoma Stem-like Cells. Cancer Cell 2015, 28, 441–455. [Google Scholar] [CrossRef] [Green Version]
- Peng, Z.; Han, X.; Li, S.; Al-Youbi, A.O.; Bashammakh, A.S.; El-Shahawi, M.S.; Leblanc, R.M. Carbon dots: Biomacromolecule interaction, bioimaging and nanomedicine. Co-Ord. Chem. Rev. 2017, 343, 256–277. [Google Scholar] [CrossRef]
- Li, S.; Peng, Z.; Dallman, J.; Baker, J.; Othman, A.M.; Blackwelder, P.L.; Leblanc, R.M. Crossing the blood–brain–barrier with transferrin conjugated carbon dots: A zebrafish model study. Colloids Surfaces B Biointerfaces 2016, 145, 251–256. [Google Scholar] [CrossRef] [Green Version]
- Han, X.; Jing, Z.; Wu, W.; Zou, B.; Peng, Z.; Ren, P.; Leblanc, R.M. Biocompatible and blood-brain barrier permeable carbon dots for inhibition of Abeta fibrillation and toxicity, and BACE1 activity. Nanoscale 2017, 9, 12862–12866. [Google Scholar] [CrossRef]
- Zheng, M.; Ruan, S.; Liu, S.; Sun, T.; Qu, D.; Zhao, H.; Xie, Z.; Gao, H.; Jing, X.; Sun, Z. Self-Targeting Fluorescent Carbon Dots for Diagnosis of Brain Cancer Cells. ACS Nano 2015, 9, 11455–11461. [Google Scholar] [CrossRef]
- Li, S.; Amat, D.; Peng, Z.; Vanni, S.; Raskin, S.; De Angulo, G.; Othman, A.M.; Graham, R.M.; Leblanc, R.M. Transferrin conjugated nontoxic carbon dots for doxorubicin delivery to target pediatric brain tumor cells. Nanoscale 2016, 8, 16662–16669. [Google Scholar] [CrossRef] [PubMed]
- Hettiarachchi, S.; Graham, R.M.; Mintz, K.J.; Zhou, Y.; Vanni, S.; Peng, Z.; Leblanc, R.M. Triple conjugated carbon dots as a nano-drug delivery model for glioblastoma brain tumors. Nanoscale 2019, 11, 6192–6205. [Google Scholar] [CrossRef] [PubMed]
- Liyanage, P.Y.; Zhou, Y.; Al-Youbi, A.O.; Bashammakh, A.S.; El-Shahawi, M.S.; Vanni, S.; Graham, R.M.; Leblanc, R.M. Pediatric glioblastoma target-specific efficient delivery of gemcitabine across the blood–brain barrier via carbon nitride dots. Nanoscale 2020, 12, 7927–7938. [Google Scholar] [CrossRef] [PubMed]
- Graham, R.M.; Hernández, F.; Puerta, N.; De Angulo, G.; Webster, A.K.; Vanni, S. Resveratrol augments ER stress and the cytotoxic effects of glycolytic inhibition in neuroblastoma by downregulating Akt in a mechanism independent of SIRT1. Exp. Mol. Med. 2016, 48, e210. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Marlow, M.M.; Shah, S.S.; Véliz, E.A.; Ivan, M.E.; Graham, R.M. Treatment of adult and pediatric high-grade gliomas with Withaferin A: Antitumor mechanisms and future perspectives. J. Nat. Med. 2016, 71, 16–26. [Google Scholar] [CrossRef]
- Mann, J. Natural products in cancer chemotherapy: Past, present and future. Nat. Cancer 2002, 2, 143–148. [Google Scholar] [CrossRef]
- Champelovier, P.; Mininno, M.; Duchamp, E.; Nicolle, E.; Curri, V.; Boumendjel, A.; Boutonnat, J. Cytotoxicity of chalcone derivatives towards glioblastoma. Anticancer Res. 2011, 31, 3213–3218. [Google Scholar]
- Bittencourt, L.F.F.; de Oliveira, K.A.; Cardoso, C.B.; Lopes, F.G.; Dal-Cim, T.; Chiaradia-Delatorre, L.D.; Mascarello, A.; Maluf, S.W.; Yunes, R.A.; Garcez, R.C.; et al. Novel synthetic chalcones induces apoptosis in human glioblastoma cells. Chem. Interactions 2016, 252, 74–81. [Google Scholar] [CrossRef]
- Lu, W.J.; Wu, G.J.; Chen, R.J.; Chang, C.C.; Lien, L.M.; Chiu, C.C.; Lin, K.H. Licochalcone A attenuates glioma cell growth in vitro and in vivo through cell cycle arrest. Food Funct. 2018, 9, 4500–4507. [Google Scholar] [CrossRef]
- Du, S.; Sarver, J.G.; Trabbic, C.J.; Erhardt, P.W.; Schroering, A.; Maltese, W.A. 6-MOMIPP, a novel brain-penetrant anti-mitotic indolyl-chalcone, inhibits glioblastoma growth and viability. Cancer Chemother. Pharmacol. 2018, 83, 237–254. [Google Scholar] [CrossRef]
- Arai, M.A.; Ochi, F.; Makita, Y.; Chiba, T.; Higashi, K.; Suganami, A.; Tamura, Y.; Toida, T.; Iwama, A.; Sadhu, S.K.; et al. GLI1 Inhibitors Identified by Target Protein Oriented Natural Products Isolation (TPO-NAPI) with Hedgehog Inhibition. ACS Chem. Biol. 2018, 13, 2551–2559. [Google Scholar] [CrossRef] [PubMed]
- Shrivastava, S.; Jeengar, M.K.; Thummuri, D.; Koval, A.; Katanaev, V.L.; Marepally, S.; Naidu, V.G.M. Cardamonin, a chalcone, inhibits human triple negative breast cancer cell invasiveness by downregulation of Wnt/beta-catenin signaling cascades and reversal of epithelial-mesenchymal transition. Biofactors 2017, 43, 152–169. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Wu, N.; Liu, J.; Zhao, X.; Yan, Z.; Jiang, B.; Wang, L.; Cao, S.; Shi, D.; Lin, X. Cardamonin induces apoptosis by suppressing STAT3 signaling pathway in glioblastoma stem cells. Tumor Biol. 2015, 36, 9667–9676. [Google Scholar] [CrossRef]
- Lin, Y.; Sun, H.; Dang, Y.; Li, Z. Isoliquiritigenin inhibits the proliferation and induces the differentiation of human glioma stem cells. Oncol. Rep. 2017, 39, 687–694. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Romagnoli, R.; Baraldi, P.G.; Carrion, M.D.; Cruz-Lopez, O.; Cara, C.L.; Balzarini, J.; Viola, G. Hybrid alpha-bromoacryloylamido chalcones. Design, synthesis and biological evaluation. Bioorganic Med. Chem. Lett. 2009, 19, 2022–2028. [Google Scholar] [CrossRef] [Green Version]
- Suwito, H.; Jumina; Mustofa; Pudjiastuti, P.; Fanani, M.Z.; Kimata-Ariga, Y.; Katahira, R.; Kawakami, T.; Fujiwara, T.; Hase, T.; et al. Design and Synthesis of Chalcone Derivatives as Inhibitors of the Ferredoxin—Ferredoxin-NADP+ Reductase Interaction of Plasmodium falciparum: Pursuing New Antimalarial Agents. Molecules 2014, 19, 21473–21488. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Kim, E.-J.; Ryu, H.W.; Curtis-Long, M.J.; Han, J.; Kim, J.Y.; Cho, J.K.; Kang, D.; Park, K.H. Chemoselective regulation of TREK2 channel: Activation by sulfonate chalcones and inhibition by sulfonamide chalcones. Bioorg. Med. Chem. Lett. 2010, 20, 4237–4239. [Google Scholar] [CrossRef]
- Rammohan, A.; Bhaskar, B.V.; Venkateswarlu, N.; Gu, W.; Zyryanov, G.V. Design, synthesis, docking and biological evaluation of chalcones as promising antidiabetic agents. Bioorg. Chem. 2019, 95, 103527. [Google Scholar] [CrossRef]
- El-Sayed, R.; AlThagafi, I. Potential Biosignificant Interest and Surface Activity of Efficient Heterocyclic Derivatives. J. Oleo Sci. 2016, 65, 177–192. [Google Scholar] [CrossRef] [Green Version]
- Nazir, S.; Ansari, F.L.; Hussain, T.; Mazhar, K.; Muazzam, A.G.; Qasmi, Z.U.H.; Mirza, B. Brine shrimp lethality assay ‘an effective prescreen’: Microwave-assisted synthesis, BSL toxicity and 3DQSAR studies-based designing, docking and antitumor evaluation of potent chalcones. Pharm. Biol. 2013, 51, 1091–1103. [Google Scholar] [CrossRef] [Green Version]
- dos Santos, M.B.; Anselmo, D.B.; De Oliveira, J.G.; Jardim-Perassi, B.V.; Monteiro, D.A.; Silva, G.; Gomes, E.; Fachin, A.L.; Marins, M.; de Campos Zuccari, D.A.P.; et al. Antiproliferative activity and p53 upregulation effects of chalcones on human breast cancer cells. J. Enzym. Inhib. Med. Chem. 2019, 34, 1093–1099. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Arulkumaran, R.; Vijayakumar, S.; Sundararajan, R.; Sakthinathan, S.; Kamalakkannan, D.; Suresh, R.; Ranganathan, K.; Vanangamudi, G.; Thirunarayanan, G. Thionylchloride Catalyzed Aldol Condensation: Synthesis, Spectral Correlation and Antibacterial Activities of some 3,5-Dichloro-2-Hydroxyphenyl Chalcones. Int. Lett. Chem. Phys. Astron. 2013, 4, 17–38. [Google Scholar] [CrossRef] [Green Version]
- Divya, V.; Parasuraman, R.; Anjana, R.; Daisy Jones, P.; Murseena, K.P.; Anjitha, K. Synthesis and Characterization of Indole Derivatives as Potent Antibacterial Agents. Int. J. Pharm. Pharm. Res. 2020, 19, 964–965. [Google Scholar]
- Mokale, S.N.; Dube, P.N.; Bhavale, S.A.; Sayed, I.; Begum, A.; Nevase, M.C.; Shelke, V.R.; Mujaheed, A. Synthesis, in-vitro screening, and docking analysis of novel pyrrolidine and piperidine-substituted ethoxy chalcone as anticancer agents. Med. Chem. Res. 2014, 24, 1842–1856. [Google Scholar] [CrossRef]
- Liang, J.-H.; Yang, L.; Wu, S.; Liu, S.S.; Cushman, M.; Tian, J.; Qing, H. Discovery of efficient stimulators for adult hippocampal neurogenesis based on scaffolds in dragon’s blood. Eur. J. Med. Chem. 2017, 136, 382–392. [Google Scholar] [CrossRef]
- Acharya, B.N.; Saraswat, D.; Tiwari, M.; Shrivastava, A.K.; Ghorpade, R.; Bapna, S.; Kaushik, M.P. Synthesis and antimalarial evaluation of 1, 3, 5-trisubstituted pyrazolines. Eur. J. Med. Chem. 2010, 45, 430–438. [Google Scholar] [CrossRef]
- Bhat, B.A.; Dhar, K.L.; Puri, S.C.; Saxena, A.K.; Shanmugavel, M.; Qazi, G.N. Synthesis and biological evaluation of chalcones and their derived pyrazoles as potential cytotoxic agents. Bioorg. Med. Chem. Lett. 2005, 15, 3177–3180. [Google Scholar] [CrossRef]
- Singh, N.; Singh, R.; Malik, M.S.; Singh, R. Synthesis and Insecticidal Activity of 2-[4-(4, 5-di hydro-5-(substituted phenyl)-1H-Pyrazol-3-yl) phenoxy] Acetic Acid Hydrazides and Related Compounds. Pestic. Res. J. 2008, 20, 183–188. [Google Scholar]
- Kamal, A.; Ramakrishna, G.; Raju, P.; Viswanath, A.; Ramaiah, J.; Balakishan, G.; Pal-Bhadra, M. Synthesis and anti-cancer activity of chalcone linked imidazolones. Bioorg. Med. Chem. Lett. 2010, 20, 4865–4869. [Google Scholar] [CrossRef]
- Wuts, P.G.; Greene, T.W. Greene’s Protective Groups in Organic Synthesis; John Wiley & Sons: Hoboken, NJ, USA, 2006. [Google Scholar]
- Sansalone, L.; Veliz, E.A.; Myrthil, N.G.; Stathias, V.; Walters, W.; Torrens, I.I.; Schürer, S.C.; Vanni, S.; Leblanc, R.M.; Graham, R.M. Novel Curcumin Inspired Bis-Chalcone Promotes Endoplasmic Reticulum Stress and Glioblastoma Neurosphere Cell Death. Cancers 2019, 11, 357. [Google Scholar] [CrossRef] [Green Version]
- Vallejo, F.A.; Shah, S.S.; de Cordoba, N.; Walters, W.M.; Prince, J.; Khatib, Z.; Komotar, R.J.; Vanni, S.; Graham, R.M. The contribution of ketone bodies to glycolytic inhibition for the treatment of adult and pediatric glioblastoma. J. Neuro-Oncol. 2020, 147, 317–326. [Google Scholar] [CrossRef] [PubMed]
- Kang, M.H.; Smith, M.A.; Bs, C.L.M.; Keshelava, N.; Houghton, P.J.; Reynolds, C.P. National Cancer Institute pediatric preclinical testing program: Model description for in vitro cytotoxicity testing. Pediatr. Blood Cancer 2010, 56, 239–249. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Li, S.; Wang, L.; Chusuei, C.C.; Suarez, V.M.; Blackwelder, P.L.; Micic, M.; Orbulescu, J.; Leblanc, R.M. Nontoxic Carbon Dots Potently Inhibit Human Insulin Fibrillation. Chem. Mater. 2015, 27, 1764–1771. [Google Scholar] [CrossRef]
- Hettiarachchi, S.D.; Cilingir, E.K.; Maklouf, H.; Seven, E.S.; Paudyal, S.; Vanni, S.; Graham, R.M.; Leblanc, R.M. pH and redox triggered doxorubicin release from covalently linked carbon dots conjugates. Nanoscale 2021, 13, 5507–5518. [Google Scholar] [CrossRef] [PubMed]
- Wilcken, R.; Zimmermann, M.O.; Lange, A.; Joerger, A.C.; Boeckler, F.M. Principles and Applications of Halogen Bonding in Medicinal Chemistry and Chemical Biology. J. Med. Chem. 2013, 56, 1363–1388. [Google Scholar] [CrossRef] [PubMed]
- Wilcken, R.; Liu, X.; Zimmermann, M.O.; Rutherford, T.J.; Fersht, A.R.; Joerger, A.C.; Boeckler, F.M. Halogen-Enriched Fragment Libraries as Leads for Drug Rescue of Mutant p53. J. Am. Chem. Soc. 2012, 134, 6810–6818. [Google Scholar] [CrossRef] [PubMed]
- Miller, J.J.; Blanchet, A.; Orvain, C.; Nouchikian, L.; Reviriot, Y.; Clarke, R.M.; Martelino, D.; Wilson, D.; Gaiddon, C.; Storr, T. Bifunctional ligand design for modulating mutant p53 aggregation in cancer. Chem. Sci. 2019, 10, 10802–10814. [Google Scholar] [CrossRef] [Green Version]
- Cancer Genome Atlas Research Network. Comprehensive genomic characterization defines human glioblastoma genes and core pathways. Nature 2008, 455, 1061–1068. [Google Scholar] [CrossRef]
- Kim, M.; Ma, D.J.; Calligaris, D.; Zhang, S.; Feathers, R.W.; Vaubel, R.A.; Meaux, I.; Mladek, A.C.; Parrish, K.E.; Jin, F.; et al. Efficacy of the MDM2 Inhibitor SAR405838 in Glioblastoma Is Limited by Poor Distribution Across the Blood–Brain Barrier. Mol. Cancer Ther. 2018, 17, 1893–1901. [Google Scholar] [CrossRef] [Green Version]
- Nepali, K.; Lee, H.-Y.; Liou, J.-P. Nitro-Group-Containing Drugs. J. Med. Chem. 2018, 62, 2851–2893. [Google Scholar] [CrossRef]
- Kandoth, C.; McLellan, M.D.; Vandin, F.; Ye, K.; Niu, B.; Lu, C.; Xie, M.; Zhang, Q.; McMichael, J.F.; Wyczalkowski, M.A.; et al. Mutational landscape and significance across 12 major cancer types. Nature 2013, 502, 333–339. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Brennan, C.W.; Verhaak, R.G.W.; McKenna, A.; Campos, B.; Noushmehr, H.; Salama, S.R.; Zheng, S.; Chakravarty, D.; Sanborn, J.Z.; Berman, S.H.; et al. The Somatic Genomic Landscape of Glioblastoma. Cell 2013, 155, 462–477, Erratum in Cell 2014, 157, 753. [Google Scholar] [CrossRef] [PubMed]
- Lipinski, C.A.; Lombardo, F.; Dominy, B.W.; Feeney, P.J. Experimental and computational approaches to estimate solubility and permeability in drug discovery and development settings. Adv. Drug Deliv. Rev. 2001, 46, 3–26. [Google Scholar] [CrossRef]
- Veber, D.F.; Johnson, S.R.; Cheng, H.-Y.; Smith, B.R.; Ward, K.W.; Kopple, K.D. Molecular Properties That Influence the Oral Bioavailability of Drug Candidates. J. Med. Chem. 2002, 45, 2615–2623. [Google Scholar] [CrossRef] [PubMed]
- Pajouhesh, H.; Lenz, G.R. Medicinal chemical properties of successful central nervous system drugs. NeuroRX 2005, 2, 541–553. [Google Scholar] [CrossRef] [Green Version]
- Mintz, K.J.; Mercado, G.; Zhou, Y.; Ji, Y.; Hettiarachchi, S.D.; Liyanage, P.Y.; Pandey, R.R.; Chusuei, C.C.; Dallman, J.; Leblanc, R.M. Tryptophan carbon dots and their ability to cross the blood-brain barrier. Colloids Surfaces B Biointerfaces 2019, 176, 488–493. [Google Scholar] [CrossRef]
- Zhou, Y.; Peng, Z.; Seven, E.S.; Leblanc, R.M. Crossing the blood-brain barrier with nanoparticles. J. Control. Release 2017, 270, 290–303. [Google Scholar] [CrossRef]
- Cilingir, E.K.; Seven, E.S.; Zhou, Y.; Walters, B.M.; Mintz, K.J.; Pandey, R.R.; Wikramanayake, A.H.; Chusuei, C.C.; Vanni, S.; Graham, R.M.; et al. Metformin derived carbon dots: Highly biocompatible fluorescent nanomaterials as mitochondrial targeting and blood-brain barrier penetrating biomarkers. J. Colloid Interface Sci. 2021, 592, 485–497. [Google Scholar] [CrossRef]






| Chalcone | Structure | Glio3 | Glio9 | Glio38 | MSC |
|---|---|---|---|---|---|
| IC50 (µM) | |||||
| 3a |  | >10 | >10 | >10 | n.d. |
| 3b |  | >10 | >10 | >10 | n.d. |
| 3c |  | 12.0 ± 1.8 | 9.3 ± 0.6 | 10.4 ± 2.0 | >>10 |
| 3d |  | 6.9 ± 1.6 | 5.5 ± 1.1 | 7.9 ± 1.7 | 16.8 |
| 3e |  | 10.9 ± 0.8 | 8.9 ± 1.6 | 9.2 ± 0.8 | 46.7 |
| 3f |  | 7.8 ± 0.9 | 9.7 ± 2.0 | 6.5 ± 0.9 | 74.8 |
| 3g |  | 6.2 ± 1.3 | 4.8 ± 0.6 | 5.4 ± 0.6 | 7.4 |
| 3h |  | >10 | >10 | >10 | n.d. |
| 3i | 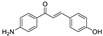 | >10 | >10 | >10 | n.d. |
| 3j |  | >10 | >10 | >10 | n.d. |
| 3k |  | >10 | >10 | >10 | n.d. |
| 3l | 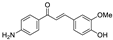 | >10 | >10 | >10 | n.d. |
| 3m |  | >10 | >10 | >10 | n.d. |
| 3n | 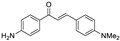 | >10 | >10 | >10 | n.d. |
| 3o | 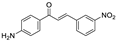 | 5.5 ± 0.6 | 6.2 ± 2.1 | 6.4 ± 0.6 | 41.5 |
| 3p |  | 6.6 ± 1.2 | 5.2 ± 0.5 | 6.4 ± 2.0 | 8.0 |
| 3q |  | 8.3 ± 0.7 | 6.6 ± 0.5 | 6.6 ± 0.7 | >>10 |
| 3r | 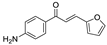 | >10 | >10 | >10 | n.d. |
| 3s | 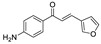 | >10 | >10 | >10 | n.d. |
| 3t |  | >10 | >10 | >10 | n.d. |
| 3u | 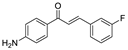 | 9.9 ± 0.3 | 7.2 ± 0.6 | 8.8 ± 1.4 | 15.6 |
| 3v | 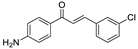 | 9.1 ± 0.6 | 5.8 ± 0.9 | 6.7 ± 0.6 | 25.7 |
| 3w | 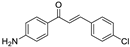 | 12.3 ± 1.1 | 7 ± 0.3 | 7.9 ± 0.6 | 80.1 |
| 3x | 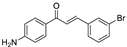 | 9.3 ± 1.1 | 7 ± 0.5 | 5.9 ± 0.8 | 28.1 |
| Chalcone | Structure | Glio3 | Glio9 | Glio38 | MSC |
|---|---|---|---|---|---|
| IC50 (µM) | |||||
| 4a | 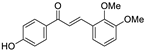 | 11.4 ± 0.9 | 14.2 ± 3 | 9.1 ± 0.7 | >>10 |
| 4b | 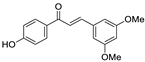 | 6.7 ± 0.2 | 7.0 ± 0.4 | 6.4 ± 0.4 | 17.1 |
| 4c | 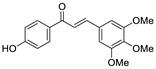 | 6.8 ± 0.5 | 6.9 ± 0.7 | 6.2 ± 1.2 | 15.7 |
| 4d | 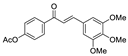 | 7.7 ± 0.4 | 6.2 ± 0.9 | 6.9 ± 0.3 | >>10 |
| 4e |  | 10.4 ± 1.4 | 7.0 ± 1.3 | 18.4 | n.d. |
| 4f | 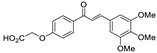 | >10 | >10 | >10 | n.d. |
| 5a | 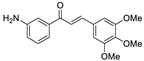 | 8.0 ± 1.5 | 5.1 ± 0.6 | 5.0 ± 0.8 | 5.5 |
| Chalcone | MW | TPSA | LogP | H-Bond Donors | H-Bond Acceptors | Rotatable Bonds |
|---|---|---|---|---|---|---|
| Optimal Values | ||||||
| <450 g/mol | ≤60–70 Å | <5 | <3 | <7 | <8 | |
| 3d | 325.36 | 64.64 | 2.89 | 1 | 5 | 6 |
| 3e | 313.35 | 70.80 | 2.52 | 2 | 5 | 6 |
| 3f | 283.33 | 61.56 | 2.93 | 2 | 4 | 5 |
| 3g | 325.36 | 64.64 | 3.07 | 1 | 5 | 6 |
| 3o | 268.27 | 88.92 | 2.82 | 2 | 5 | 4 |
| 3p | 224.26 | 55.99 | 1.54 | 2 | 3 | 3 |
| 3q | 224.26 | 55.99 | 1.47 | 2 | 3 | 3 |
| 3u | 241.26 | 43.09 | 3.03 | 2 | 2 | 3 |
| 3v | 257.72 | 43.09 | 3.54 | 2 | 2 | 3 |
| 3w | 257.72 | 43.09 | 3.56 | 2 | 2 | 3 |
| 3x | 302.17 | 43.09 | 3.67 | 2 | 2 | 3 |
| 4b | 284.31 | 55.77 | 3.37 | 1 | 4 | 5 |
| 4c | 314.34 | 65.00 | 2.96 | 1 | 5 | 6 |
| 4d | 356.37 | 71.08 | 2.99 | 0 | 6 | 8 |
| 5a | 313.35 | 70.80 | 2.50 | 2 | 5 | 6 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Veliz, E.A.; Kaplina, A.; Hettiarachchi, S.D.; Yoham, A.L.; Matta, C.; Safar, S.; Sankaran, M.; Abadi, E.L.; Cilingir, E.K.; Vallejo, F.A.; et al. Chalcones as Anti-Glioblastoma Stem Cell Agent Alone or as Nanoparticle Formulation Using Carbon Dots as Nanocarrier. Pharmaceutics 2022, 14, 1465. https://doi.org/10.3390/pharmaceutics14071465
Veliz EA, Kaplina A, Hettiarachchi SD, Yoham AL, Matta C, Safar S, Sankaran M, Abadi EL, Cilingir EK, Vallejo FA, et al. Chalcones as Anti-Glioblastoma Stem Cell Agent Alone or as Nanoparticle Formulation Using Carbon Dots as Nanocarrier. Pharmaceutics. 2022; 14(7):1465. https://doi.org/10.3390/pharmaceutics14071465
Chicago/Turabian StyleVeliz, Eduardo A., Anastasiia Kaplina, Sajini D. Hettiarachchi, Athina L. Yoham, Carolina Matta, Sabrin Safar, Meghana Sankaran, Esther L. Abadi, Emel Kirbas Cilingir, Frederic A. Vallejo, and et al. 2022. "Chalcones as Anti-Glioblastoma Stem Cell Agent Alone or as Nanoparticle Formulation Using Carbon Dots as Nanocarrier" Pharmaceutics 14, no. 7: 1465. https://doi.org/10.3390/pharmaceutics14071465
APA StyleVeliz, E. A., Kaplina, A., Hettiarachchi, S. D., Yoham, A. L., Matta, C., Safar, S., Sankaran, M., Abadi, E. L., Cilingir, E. K., Vallejo, F. A., Walters, W. M., Vanni, S., Leblanc, R. M., & Graham, R. M. (2022). Chalcones as Anti-Glioblastoma Stem Cell Agent Alone or as Nanoparticle Formulation Using Carbon Dots as Nanocarrier. Pharmaceutics, 14(7), 1465. https://doi.org/10.3390/pharmaceutics14071465







