Convergence of Biofabrication Technologies and Cell Therapies for Wound Healing
Abstract
1. Introduction
2. Significant Cell Populations for Regenerative Skin Wound Therapies
2.1. Keratinocytes
2.2. Fibroblasts
2.3. Platelets
2.4. Stem/Progenitor Cell Therapies
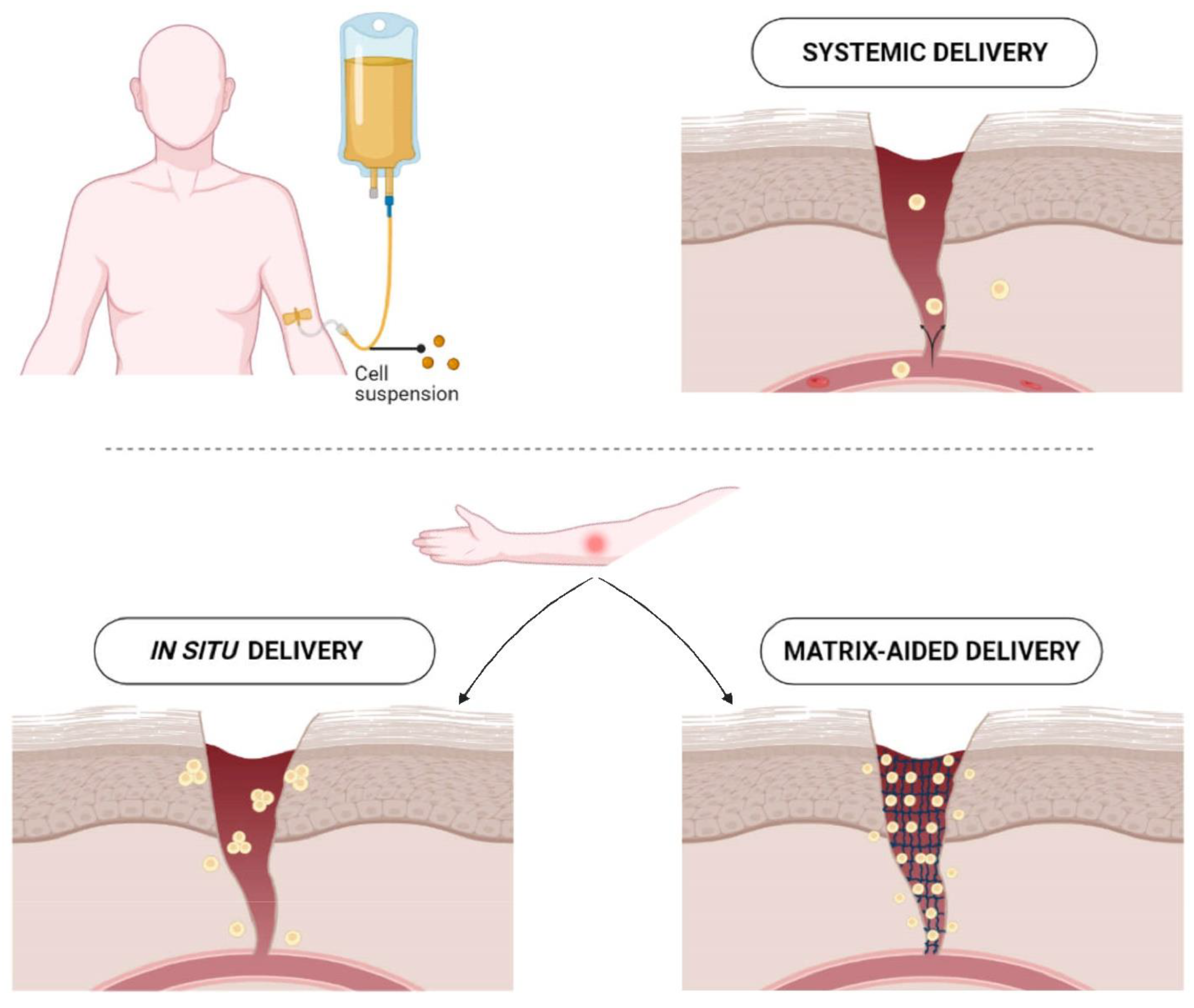
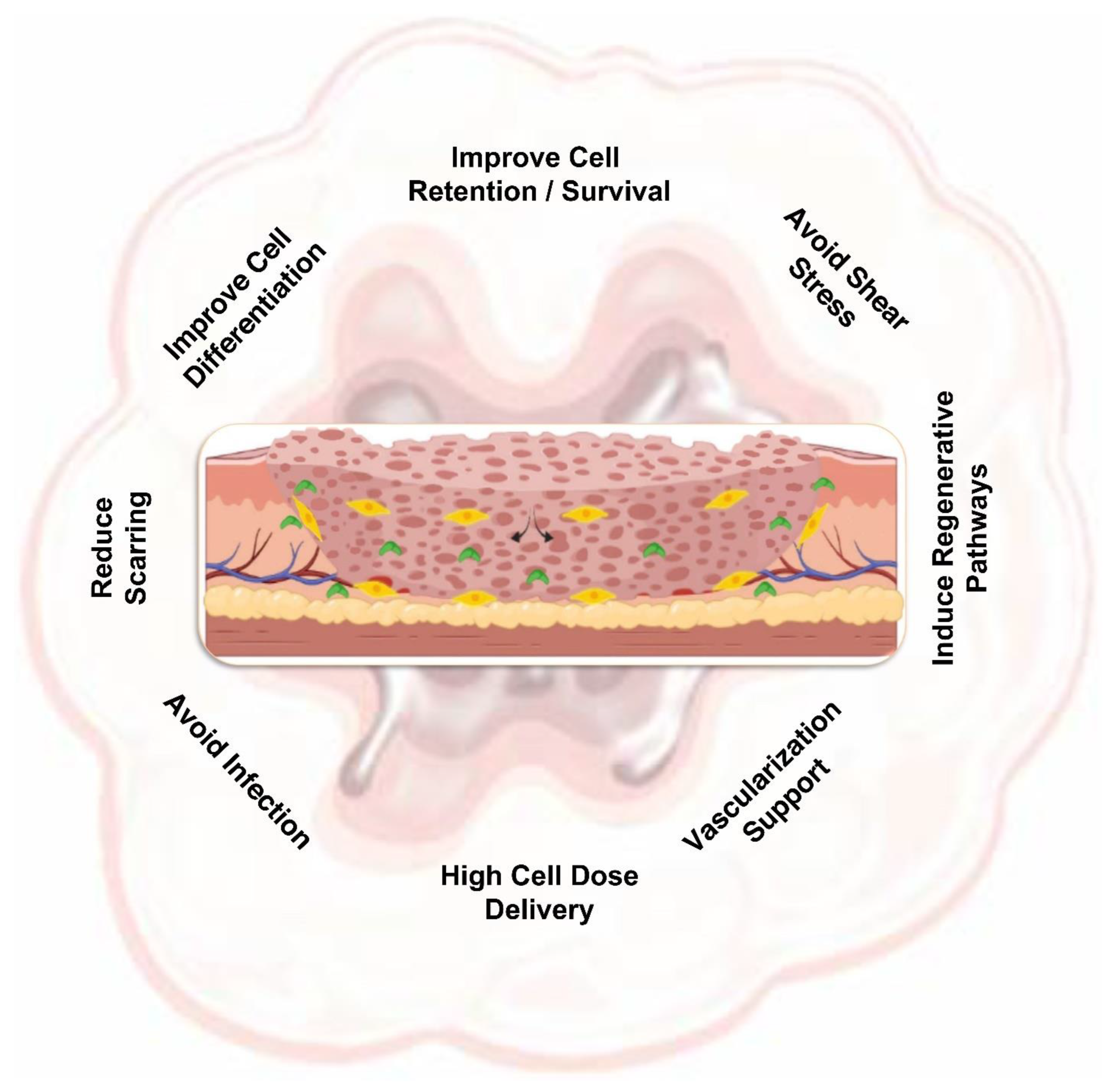
3. Contribution of Matrices to the Improvement of Cell Therapy
3.1. Biofabrication Technologies
3.2. Matrices as Supportive Carriers
3.3. Matrices as Inductive Substrates to Modulate the Biophysical and Biochemical Responses
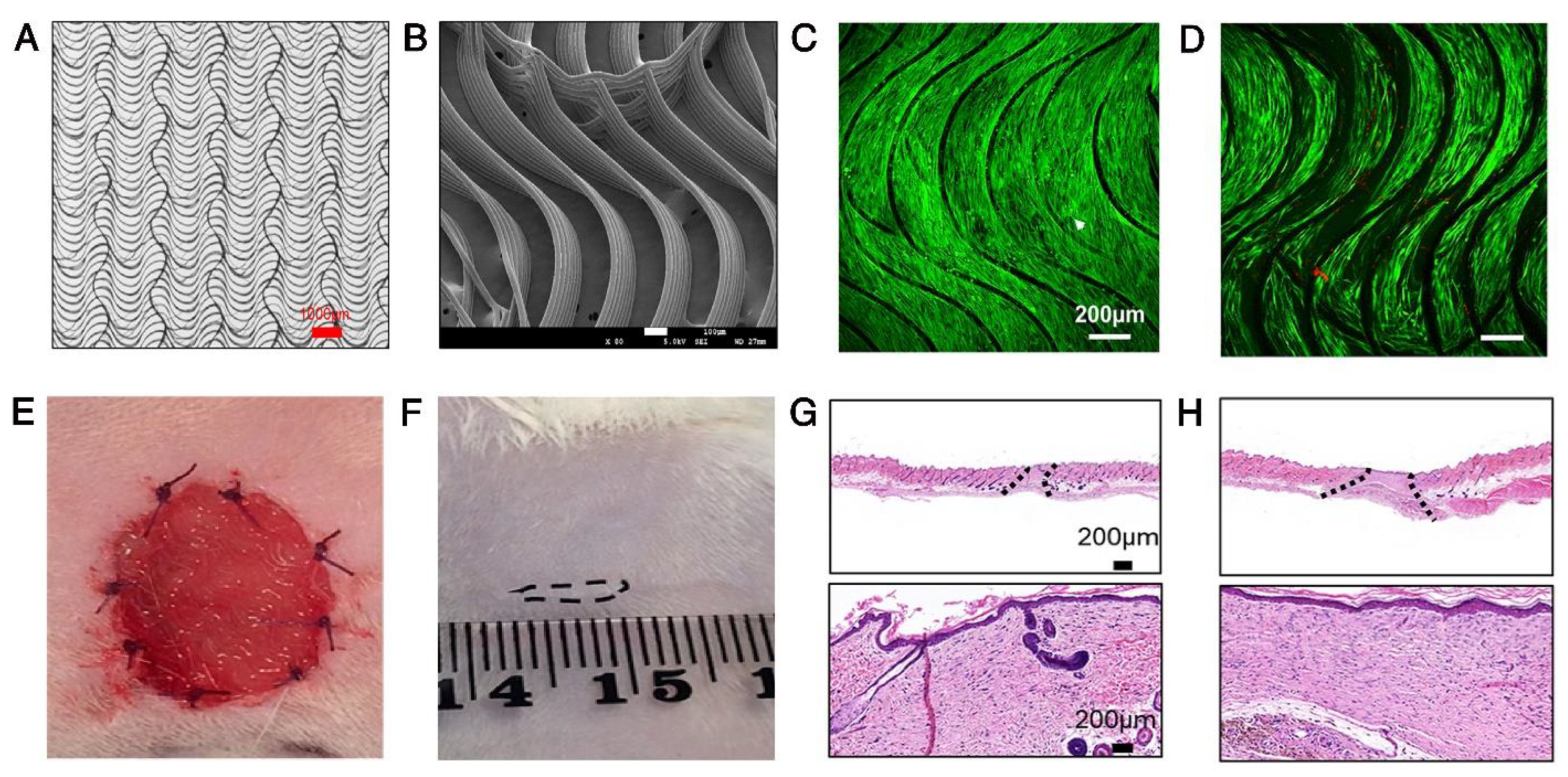
3.3.1. Biophysical Cues
3.3.2. Matrices for Efficient Delivery of Bioactive Molecules
4. Stem/Progenitor Cells Seeded Matrices in Clinical Settings
5. Current Limitations and Future Opportunities
6. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
Abbreviations
| (AMPs) | Antimicrobial peptides |
| (RGD) | Arg-Gly-Asp peptide |
| (CEA) | Cultured epithelial autograft |
| (EGF) | Epidermal growth factor |
| (ECM) | Extracellular matrix |
| (GelMA) | Gelatin-methacryloyl |
| (GHK) | Glycyl-Histidyl-Lysine |
| (GFs) | Growth factors |
| (HDPs) | Host defense peptides |
| (IL) | Interleukin |
| (MSCs) | Mesenchymal stem cells |
| (PDGF) | Platelet-derived growth factor |
| (PRP) | Platelet-rich plasma |
| (PCL) | Poly(caprolactone) |
| (PDLLA) | Poly(D, L-lactic acid) |
| (PLGA) | Poly(lactic-co-glycolic acid) |
| (PVA) | Poly(vinyl alcohol) |
| (3D) | Three dimensional |
| (TGF) | Transforming growth factor |
| (2D) | Two dimensional |
| (VEGF) | Vascular endothelial growth factor |
References
- Mathes, S.H.; Ruffner, H.; Graf-Hausner, U. The use of skin models in drug development. Adv. Drug Deliv. Rev. 2014, 69–70, 81–102. [Google Scholar] [CrossRef] [PubMed]
- Wilkinson, H.N.; Hardman, M.J. Wound healing: Cellular mechanisms and pathological outcomes. Open Biol. 2020, 10, 200223. [Google Scholar] [CrossRef] [PubMed]
- Gushiken, L.F.S.; Beserra, F.P.; Bastos, J.K.; Jackson, C.J.; Pellizzon, C.H. Cutaneous Wound Healing: An Update from Physiopathology to Current Therapies. Life 2021, 11, 665. [Google Scholar] [CrossRef] [PubMed]
- Rodrigues, M.; Kosaric, N.; Bonham, C.A.; Gurtner, G.C. Wound Healing: A Cellular Perspective. Physiol. Rev. 2019, 99, 665–706. [Google Scholar] [CrossRef] [PubMed]
- Dong, Y.; Yang, Q.; Sun, X. Comprehensive Analysis of Cell Therapy on Chronic Skin Wound Healing: A Meta-Analysis. Hum. Gene Ther. 2021, 32, 787–795. [Google Scholar] [CrossRef] [PubMed]
- Domaszewska-Szostek, A.; Krzyżanowska, M.; Siemionow, M. Cell-Based Therapies for Chronic Wounds Tested in Clinical Studies: Review. Ann. Plast. Surg. 2019, 83, e96–e109. [Google Scholar] [CrossRef] [PubMed]
- Domaszewska-Szostek, A.P.; Krzyżanowska, M.O.; Czarnecka, A.M.; Siemionow, M. Local Treatment of Burns with Cell-Based Therapies Tested in Clinical Studies. J. Clin. Med. 2021, 10, 396. [Google Scholar] [CrossRef]
- Fabbri, M.; García-Fernández, L.; Vázquez-Lasa, B.; Soccio, M.; Lotti, N.; Gamberini, R.; Rimini, B.; Munari, A.; Román, J.S. Micro-structured 3D-electrospun scaffolds of biodegradable block copolymers for soft tissue regeneration. Eur. Polym. J. 2017, 94, 33–42. [Google Scholar] [CrossRef]
- Lee, J.; Cuddihy, M.J.; Kotov, N.A. Three-dimensional cell culture matrices: State of the art. Tissue Eng. Part B Rev. 2008, 14, 61–86. [Google Scholar] [CrossRef]
- Farahani, M.; Shafiee, A. Wound Healing: From Passive to Smart Dressings. Adv. Healthc. Mater. 2021, 10, 2100477. [Google Scholar] [CrossRef]
- Hosseini, M.; Shafiee, A. Engineering Bioactive Scaffolds for Skin Regeneration. Small 2021, 17, 2101384. [Google Scholar] [CrossRef] [PubMed]
- Rheinwald, J.G.; Green, H. Serial cultivation of strains of human epidermal keratinocytes: The formation of keratinizing colonies from single cells. Cell 1975, 6, 331–343. [Google Scholar] [CrossRef] [PubMed]
- Grafting of burns with cultured epithelium prepared from autologous epidermal cells. Lancet 1981, 1, 75–78.
- You, H.J.; Han, S.K.; Lee, J.W.; Chang, H. Treatment of diabetic foot ulcers using cultured allogeneic keratinocytes—A pilot study. Wound Repair. Regen. 2012, 20, 491–499. [Google Scholar] [CrossRef]
- Gallego, L.; Junquera, L.; Villarreal, P.; Peña, I.; Meana, A. Use of cultured human epithelium for coverage: A defect of radial forearm free flap donor site. Med. Oral Patol. Oral Cir. Bucal. 2010, 15, e58–e60. [Google Scholar] [CrossRef]
- Yanaga, H.; Udoh, Y.; Yamauchi, T.; Yamamoto, M.; Kiyokawa, K.; Inoue, Y.; Tai, Y. Cryopreserved cultured epidermal allografts achieved early closure of wounds and reduced scar formation in deep partial-thickness burn wounds (DDB) and split-thickness skin donor sites of pediatric patients. Burns 2001, 27, 689–698. [Google Scholar] [CrossRef] [PubMed]
- Pastar, I.; Stojadinovic, O.; Yin, N.C.; Ramirez, H.; Nusbaum, A.G.; Sawaya, A.; Patel, S.B.; Khalid, L.; Isseroff, R.R.; Tomic-Canic, M. Epithelialization in Wound Healing: A Comprehensive Review. Adv. Wound Care 2014, 3, 445–464. [Google Scholar] [CrossRef] [PubMed]
- Piipponen, M.; Li, D.; Landén, N.X. The Immune Functions of Keratinocytes in Skin Wound Healing. Int. J. Mol. Sci. 2020, 21, 8790. [Google Scholar] [CrossRef] [PubMed]
- You, H.J.; Han, S.K. Cell therapy for wound healing. J. Korean Med. Sci. 2014, 29, 311–319. [Google Scholar] [CrossRef]
- Wood, F.M.; Kolybaba, M.L.; Allen, P. The use of cultured epithelial autograft in the treatment of major burn injuries: A critical review of the literature. Burns 2006, 32, 395–401. [Google Scholar] [CrossRef]
- Dominiak, M.; Łysiak-Drwal, K.; Saczko, J.; Kunert-Keil, C.; Gedrange, T. The clinical efficacy of primary culture of human fibroblasts in gingival augmentation procedures-a preliminary report. Ann. Anat. 2012, 194, 502–507. [Google Scholar] [CrossRef]
- Milinkovic, I.; Aleksic, Z.; Jankovic, S.; Popovic, O.; Bajic, M.; Cakic, S.; Lekovic, V. Clinical application of autologous fibroblast cell culture in gingival recession treatment. J. Periodontal. Res. 2015, 50, 363–370. [Google Scholar] [CrossRef] [PubMed]
- Munavalli, G.S.; Smith, S.; Maslowski, J.M.; Weiss, R.A. Successful treatment of depressed, distensible acne scars using autologous fibroblasts: A multi-site, prospective, double blind, placebo-controlled clinical trial. Dermatol. Surg. 2013, 39, 1226–1236. [Google Scholar] [CrossRef] [PubMed]
- Gomes, R.N.; Manuel, F.; Nascimento, D.S. The bright side of fibroblasts: Molecular signature and regenerative cues in major organs. NPJ Regen. Med. 2021, 6, 43. [Google Scholar] [CrossRef]
- Plikus, M.V.; Wang, X.; Sinha, S.; Forte, E.; Thompson, S.M.; Herzog, E.L.; Driskell, R.R.; Rosenthal, N.; Biernaskie, J.; Horsley, V. Fibroblasts: Origins, definitions, and functions in health and disease. Cell 2021, 184, 3852–3872. [Google Scholar] [CrossRef] [PubMed]
- Hart, C.E.; Loewen-Rodriguez, A.; Lessem, J. Dermagraft: Use in the Treatment of Chronic Wounds. Adv. Wound Care 2012, 1, 138–141. [Google Scholar] [CrossRef] [PubMed]
- Venugopal, S.S.; Yan, W.; Frew, J.W.; Cohn, H.I.; Rhodes, L.M.; Tran, K.; Melbourne, W.; Nelson, J.A.; Sturm, M.; Fogarty, J.; et al. A phase II randomized vehicle-controlled trial of intradermal allogeneic fibroblasts for recessive dystrophic epidermolysis bullosa. J. Am. Acad. Dermatol. 2013, 69, 898–908.e897. [Google Scholar] [CrossRef]
- Wong, T.; Gammon, L.; Liu, L.; Mellerio, J.E.; Dopping-Hepenstal, P.J.; Pacy, J.; Elia, G.; Jeffery, R.; Leigh, I.M.; Navsaria, H.; et al. Potential of fibroblast cell therapy for recessive dystrophic epidermolysis bullosa. J. Investig. Dermatol. 2008, 128, 2179–2189. [Google Scholar] [CrossRef]
- Han, S.K.; Choi, K.J.; Kim, W.K. Clinical application of fresh fibroblast allografts for the treatment of diabetic foot ulcers: A pilot study. Plast. Reconstr. Surg. 2004, 114, 1783–1789. [Google Scholar] [CrossRef]
- Han, S.K.; Kim, H.S.; Kim, W.K. Efficacy and safety of fresh fibroblast allografts in the treatment of diabetic foot ulcers. Dermatol. Surg. Off. Publ. Am. Soc. Dermatol. Surg. 2009, 35, 1342–1348. [Google Scholar] [CrossRef]
- Han, S.K.; Kim, W.K. Revisiting fresh fibroblast allograft as a treatment for diabetic foot ulcers. Plast. Reconstr. Surg. 2009, 123, 88e–89e. [Google Scholar] [CrossRef] [PubMed]
- Choi, J.; Minn, K.W.; Chang, H. The efficacy and safety of platelet-rich plasma and adipose-derived stem cells: An update. Arch. Plast. Surg. 2012, 39, 585–592. [Google Scholar] [CrossRef] [PubMed]
- Shin, H.S.; Oh, H.Y. The Effect of Platelet-rich Plasma on Wounds of OLETF Rats Using Expression of Matrix Metalloproteinase-2 and -9 mRNA. Arch. Plast. Surg. 2012, 39, 106–112. [Google Scholar] [CrossRef] [PubMed]
- Lacci, K.M.; Dardik, A. Platelet-rich plasma: Support for its use in wound healing. Yale J. Biol. Med. 2010, 83, 1–9. [Google Scholar]
- Menchisheva, Y.; Mirzakulova, U.; Yui, R. Use of platelet-rich plasma to facilitate wound healing. Int. Wound J. 2019, 16, 343–353. [Google Scholar] [CrossRef]
- Vidán-Estévez, J.; Sánchez-Herráez, S.; Escalante-Barrigón, F.; Seco-Calvo, J. Healing of Chronic Wounds with Platelet-Derived Growth Factors from Single Donor Platelet-Rich Plasma following One Freeze-Thaw Cycle. A Cross-Sectional Study. J. Clin. Med. 2021, 10, 5762. [Google Scholar] [CrossRef]
- Jain, N.K.; Gulati, M. Platelet-rich plasma: A healing virtuoso. Blood Res. 2016, 51, 3–5. [Google Scholar] [CrossRef]
- Nagamura-Inoue, T.; He, H. Umbilical cord-derived mesenchymal stem cells: Their advantages and potential clinical utility. World J. Stem Cells 2014, 6, 195–202. [Google Scholar] [CrossRef]
- da Silva, L.P.; Reis, R.L.; Correlo, V.M.; Marques, A.P. Hydrogel-Based Strategies to Advance Therapies for Chronic Skin Wounds. Annu. Rev. Biomed. Eng. 2019, 21, 145–169. [Google Scholar] [CrossRef]
- Isakson, M.; de Blacam, C.; Whelan, D.; McArdle, A.; Clover, A.J. Mesenchymal Stem Cells and Cutaneous Wound Healing: Current Evidence and Future Potential. Stem Cells Int. 2015, 2015, 831095. [Google Scholar] [CrossRef]
- Kosaric, N.; Kiwanuka, H.; Gurtner, G.C. Stem cell therapies for wound healing. Expert Opin. Biol. Ther. 2019, 19, 575–585. [Google Scholar] [CrossRef] [PubMed]
- Dabiri, G.; Heiner, D.; Falanga, V. The emerging use of bone marrow-derived mesenchymal stem cells in the treatment of human chronic wounds. Expert Opin. Emerg. Drugs 2013, 18, 405–419. [Google Scholar] [CrossRef] [PubMed]
- Hu, M.S.; Borrelli, M.R.; Lorenz, H.P.; Longaker, M.T.; Wan, D.C. Mesenchymal Stromal Cells and Cutaneous Wound Healing: A Comprehensive Review of the Background, Role, and Therapeutic Potential. Stem Cells Int. 2018, 2018, 6901983. [Google Scholar] [CrossRef]
- Lee, H.C.; Park, J.-S.; Choi, J.H. Safety and effect of adipose tissue-derived stem cell implantation in patients with critical limb ischemia: A pilot study. Circ. J. 2012, 76, 1750–1760. [Google Scholar] [CrossRef] [PubMed]
- Wettstein, R.; Savic, M.; Pierer, G.; Scheufler, O.; Haug, M.; Halter, J.; Gratwohl, A.; Baumberger, M.; Schaefer, D.J.; Kalbermatten, D.F. Progenitor cell therapy for sacral pressure sore: A pilot study with a novel human chronic wound model. Stem Cell Res. Ther. 2014, 5, 18. [Google Scholar] [CrossRef]
- Marino, G.; Moraci, M.; Armenia, E.; Orabona, C.; Sergio, R.; De Sena, G.; Capuozzo, V.; Barbarisi, M.; Rosso, F.; Giordano, G.; et al. Therapy with autologous adipose-derived regenerative cells for the care of chronic ulcer of lower limbs in patients with peripheral arterial disease. J. Surg. Res. 2013, 185, 36–44. [Google Scholar] [CrossRef]
- Bura, A.; Planat-Benard, V.; Bourin, P.; Silvestre, J.-S.; Gross, F.; Grolleau, J.-L.; Saint-Lebese, B.; Peyrafitte, J.-A.; Fleury, S.; Gadelorge, M.; et al. Phase I trial: The use of autologous cultured adipose-derived stroma/stem cells to treat patients with non-revascularizable critical limb ischemia. Cytotherapy 2014, 16, 245–257. [Google Scholar] [CrossRef]
- Carstens, M.H.; Gómez, A.; Cortés, R.; Turner, E.; Pérez, C.; Ocon, M.; Correa, D. Non-reconstructable peripheral vascular disease of the lower extremity in ten patients treated with adipose-derived stromal vascular fraction cells. Stem Cell Res. 2017, 18, 14–21. [Google Scholar] [CrossRef]
- Chopinaud, M.; Labbé, D.; Creveuil, C.; Marc, M.; Bénateau, H.; Mourgeon, B.; Chopinaud, E.; Veyssière, A.; Dompmartin, A. Autologous Adipose Tissue Graft to Treat Hypertensive Leg Ulcer: A Pilot Study. Dermatology 2017, 233, 234–241. [Google Scholar] [CrossRef]
- Konstantinow, A.; Arnold, A.; Djabali, K.; Kempf, W.; Gutermuth, J.; Fischer, T.; Biedermann, T. Therapy of ulcus cruris of venous and mixed venous arterial origin with autologous, adult, native progenitor cells from subcutaneous adipose tissue: A prospective clinical pilot study. J. Eur. Acad. Dermatol. Venereol. 2017, 31, 2104–2118. [Google Scholar] [CrossRef]
- Gupta, P.K.; Chullikana, A.; Parakh, R.; Desai, S.; Das, A.; Gottipamula, S.; Krishnamurthy, S.; Anthony, N.; Pherwani, A.; Majumdar, A.S. A double blind randomized placebo controlled phase I/II study assessing the safety and efficacy of allogeneic bone marrow derived mesenchymal stem cell in critical limb ischemia. J. Transl. Med. 2013, 11, 143. [Google Scholar] [CrossRef] [PubMed]
- Jain, P.; Perakath, B.; Jesudason, M.R.; Nayak, S. The effect of autologous bone marrow-derived cells on healing chronic lower extremity wounds: Results of a randomized controlled study. Ostomy Wound Manag. 2011, 57, 38–44. [Google Scholar]
- Lu, D.; Chen, B.; Liang, Z.; Deng, W.; Jiang, Y.; Li, S.; Xu, J.; Wu, Q.; Zhang, Z.; Xie, B.; et al. Comparison of bone marrow mesenchymal stem cells with bone marrow-derived mononuclear cells for treatment of diabetic critical limb ischemia and foot ulcer: A double-blind, randomized, controlled trial. Diabetes Res. Clin. Pract. 2011, 92, 26–36. [Google Scholar] [CrossRef] [PubMed]
- Sarasúa, J.G.; López, S.P.; Viejo, M.; Basterrechea, M.P.; Rodríguez, A.F.; Gutiérrez, A.F.; Gala, J.G.; Menéndez, Y.M.; Augusto, D.E.; Arias, A.P.; et al. Treatment of pressure ulcers with autologous bone marrow nuclear cells in patients with spinal cord injury. J. Spinal Cord Med. 2011, 34, 301–307. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Gupta, G.J.; Karki, K.; Jain, P.; Saxena, A.K. Autologous Bone Marrow Aspirate Therapy for Skin Tissue Engineering and Tissue Regeneration. Adv. Wound Care 2017, 6, 135–142. [Google Scholar] [CrossRef]
- Mavilio, F.; Pellegrini, G.; Ferrari, S.; Di Nunzio, F.; Di Iorio, E.; Recchia, A.; Maruggi, G.; Ferrari, G.; Provasi, E.; Bonini, M.C.; et al. Correction of junctional epidermolysis bullosa by transplantation of genetically modified epidermal stem cells. Nat. Med. 2006, 12, 1397–1402. [Google Scholar] [CrossRef]
- Hirsch, T.; Rothoeft, T.; Teig, N.; Bauer, J.W.; Pellegrini, G.; De Rosa, L.; Scaglione, D.; Reichelt, J.; Klausegger, A.; Kneisz, D.; et al. Regeneration of the entire human epidermis using transgenic stem cells. Nature 2017, 551, 327–332. [Google Scholar] [CrossRef]
- Humpert, P.; Bärtsch, U.; Konrade, I.; Hammes, H.-P.; Morcos, M.; Kasper, M.; Bierhaus, A.; Nawroth, P. Locally applied mononuclear bone marrow cells restore angiogenesis and promote wound healing in a type 2 diabetic patient. Exp. Clin. Endocrinol. Diabetes 2005, 113, 538–540. [Google Scholar] [CrossRef]
- Farivar, B.S.; Toursavadkohi, S.; Monahan, T.S.; Sharma, J.; Ucuzian, A.A.; Kundi, R.; Sarkar, R.; Lal, B.K. Prospective study of cryopreserved placental tissue wound matrix in the management of chronic venous leg ulcers. J. Vasc. Surg. Venous Lymphat. Disord. 2019, 7, 228–233. [Google Scholar] [CrossRef]
- Wu, S.C.; Pollak, R.; Frykberg, R.G.; Zhou, W.; Karnoub, M.; Jankovic, V.; Fischkoff, S.A.; Chitkara, D. Safety and efficacy of intramuscular human placenta-derived mesenchymal stromal-like cells (cenplacel [PDA-002]) in patients who have a diabetic foot ulcer with peripheral arterial disease. Int. Wound J. 2017, 14, 823–829. [Google Scholar] [CrossRef]
- Qin, H.L.; Zhu, X.H.; Zhang, B.; Zhou, L.; Wang, W.Y. Clinical Evaluation of Human Umbilical Cord Mesenchymal Stem Cell Transplantation After Angioplasty for Diabetic Foot. Exp. Clin. Endocrinol. Diabetes 2016, 124, 497–503. [Google Scholar] [CrossRef]
- Motamedi, S.; Esfandpour, A.; Babajani, A.; Jamshidi, E.; Bahrami, S.; Niknejad, H. The Current Challenges on Spray-Based Cell Delivery to the Skin Wounds. Tissue Eng. Part C Methods 2021, 27, 543–558. [Google Scholar] [CrossRef] [PubMed]
- Gurtner, G.C.; Chapman, M.A. Regenerative Medicine: Charting a New Course in Wound Healing. Adv. Wound Care 2016, 5, 314–328. [Google Scholar] [CrossRef] [PubMed]
- Dow, J.; Simkhovich, B.Z.; Kedes, L.; Kloner, R.A. Washout of transplanted cells from the heart: A potential new hurdle for cell transplantation therapy. Cardiovasc. Res. 2005, 67, 301–307. [Google Scholar] [CrossRef] [PubMed]
- Nie, Y.; Zhang, K.; Zhang, S.; Wang, D.; Han, Z.; Che, Y.; Kong, D.; Zhao, Q.; Han, Z.; He, Z.-X.; et al. Nitric oxide releasing hydrogel promotes endothelial differentiation of mouse embryonic stem cells. Acta Biomater. 2017, 63, 190–199. [Google Scholar] [CrossRef]
- Zhao, X.; Li, Q.; Guo, Z.; Li, Z. Constructing a cell microenvironment with biomaterial scaffolds for stem cell therapy. Stem Cell Res. Ther. 2021, 12, 583. [Google Scholar] [CrossRef]
- Moroni, L.; Boland, T.; Burdick, J.A.; De Maria, C.; Derby, B.; Forgacs, G.; Groll, J.; Li, Q.; Malda, J.; Mironov, V.A.; et al. Biofabrication: A Guide to Technology and Terminology. Trends Biotechnol. 2018, 36, 384–402. [Google Scholar] [CrossRef]
- Groll, J.; Boland, T.; Blunk, T.; Burdick, J.A.; Cho, D.-W.; Dalton, P.D.; Derby, B.; Forgacs, G.; Li, Q.; Mironov, V.A.; et al. Biofabrication: Reappraising the definition of an evolving field. Biofabrication 2016, 8, 013001. [Google Scholar] [CrossRef]
- Xu, S.; Lu, T.; Yang, L.; Luo, S.; Wang, Z.; Ye, C. In situ cell electrospun using a portable handheld electrospinning apparatus for the repair of wound healing in rats. Int. Wound J. 2022. [Google Scholar] [CrossRef]
- Pisani, S.; Dorati, R.; Genta, I.; Chiesa, E.; Modena, T.; Conti, B. High Efficiency Vibrational Technology (HEVT) for Cell Encapsulation in Polymeric Microcapsules. Pharmaceutics 2020, 12, 469. [Google Scholar] [CrossRef]
- Moyer, H.R.; Kinney, R.C.; Singh, K.A.; Williams, J.K.; Schwartz, Z.; Boyan, B.D. Alginate microencapsulation technology for the percutaneous delivery of adipose-derived stem cells. Ann. Plast. Surg. 2010, 65, 497–503. [Google Scholar] [CrossRef] [PubMed]
- Khademhosseini, A.; Eng, G.; Yeh, J.; Fukuda, J.; Blumling, J.; Langer, R.; Burdick, J.A. Micromolding of photocrosslinkable hyaluronic acid for cell encapsulation and entrapment. J. Biomed. Mater. Res. A 2006, 79, 522–532. [Google Scholar] [CrossRef] [PubMed]
- Shin, S.R.; Aghaei-Ghareh-Bolagh, B.; Dang, T.T.; Topkaya, S.N.; Gao, X.; Yang, S.Y.; Jung, S.M.; Oh, J.H.; Dokmeci, M.R.; Tang, X.; et al. Cell-laden microengineered and mechanically tunable hybrid hydrogels of gelatin and graphene oxide. Adv. Mater. 2013, 25, 6385–6391. [Google Scholar] [CrossRef] [PubMed]
- Celik, S.B.G.; Dominici, S.R.; Filby, B.W.; Das, A.A.K.; Madden, L.A.; Paunov, V.N. Fabrication of Human Keratinocyte Cell Clusters for Skin Graft Applications by Templating Water-in-Water Pickering Emulsions. Biomimetics 2019, 4, 50. [Google Scholar] [CrossRef]
- Yu, J.; Huang, T.-R.; Lim, Z.H.; Luo, R.; Pasula, R.R.; Liao, L.-D.; Lim, S.; Chen, C.-H. Production of Hollow Bacterial Cellulose Microspheres Using Microfluidics to Form an Injectable Porous Scaffold for Wound Healing. Adv. Healthc. Mater. 2016, 5, 2983–2992. [Google Scholar] [CrossRef]
- Griffin, D.R.; Weaver, W.M.; Scumpia, P.O.; Di Carlo, D.; Segura, T. Accelerated wound healing by injectable microporous gel scaffolds assembled from annealed building blocks. Nat. Mater. 2015, 14, 737–744. [Google Scholar] [CrossRef]
- Skardal, A.; Mack, D.; Kapetanovic, E.; Atala, A.; Jackson, J.D.; Yoo, J.; Soker, S. Bioprinted amniotic fluid-derived stem cells accelerate healing of large skin wounds. Stem Cells Transl. Med. 2012, 1, 792–802. [Google Scholar] [CrossRef]
- Kim, B.S.; Kwon, Y.W.; Kong, J.-S.; Park, G.T.; Gao, G.; Han, W.; Kim, M.-B.; Lee, H.; Kim, J.H.; Cho, D.-W. 3D cell printing of in vitro stabilized skin model and in vivo pre-vascularized skin patch using tissue-specific extracellular matrix bioink: A step towards advanced skin tissue engineering. Biomaterials 2018, 168, 38–53. [Google Scholar] [CrossRef]
- Albanna, M.; Binder, K.W.; Murphy, S.V.; Kim, J.; Qasem, S.A.; Zhao, W.; Tan, J.; El-Amin, I.B.; Dice, D.D.; Marco, J.; et al. In Situ Bioprinting of Autologous Skin Cells Accelerates Wound Healing of Extensive Excisional Full-Thickness Wounds. Sci. Rep. 2019, 9, 1856. [Google Scholar] [CrossRef]
- Cheng, R.Y.; Eylert, G.; Gariepy, J.-M.; He, S.; Ahmad, H.; Gao, Y.; Priore, S.; Hakimi, N.; Jeschke, M.G.; Günther, A. Handheld instrument for wound-conformal delivery of skin precursor sheets improves healing in full-thickness burns. Biofabrication 2020, 12, 025002. [Google Scholar] [CrossRef]
- Puertas-Bartolomé, M.; Mora-Boza, A.; García-Fernández, L. Emerging Biofabrication Techniques: A Review on Natural Polymers for Biomedical Applications. Polymers 2021, 13, 1209. [Google Scholar] [CrossRef] [PubMed]
- Bryksin, A.V.; Brown, A.C.; Baksh, M.M.; Finn, M.G.; Barker, T.H. Learning from nature—Novel synthetic biology approaches for biomaterial design. Acta Biomater. 2014, 10, 1761–1769. [Google Scholar] [CrossRef] [PubMed]
- Kamarul, T.; Krishnamurithy, G.; Salih, N.D.; Ibrahim, N.S.; Raghavendran HR, B.; Suhaeb, A.R.; Choon DS, K. Biocompatibility and toxicity of poly(vinyl alcohol)/N,O-carboxymethyl chitosan scaffold. Sci. World J. 2014, 2014, 905103. [Google Scholar] [CrossRef] [PubMed]
- Ma, K.; Kwon, S.H.; Padmanabhan, J.; Duscher, D.; Trotsyuk, A.A.; Dong, Y.; Inayathullah, M.; Rajadas, J.; Gurtner, G.C. Controlled Delivery of a Focal Adhesion Kinase Inhibitor Results in Accelerated Wound Closure with Decreased Scar Formation. J. Investig. Dermatol. 2018, 138, 2452–2460. [Google Scholar] [CrossRef]
- Rustad, K.C.; Gurtner, G.C. Mesenchymal Stem Cells Home to Sites of Injury and Inflammation. Adv. Wound Care 2012, 1, 147–152. [Google Scholar] [CrossRef]
- Rustad, K.C.; Wong, V.W.; Sorkin, M.; Glotzbach, J.; Major, M.R.; Rajadas, J.; Longaker, M.T.; Gurtner, G.C. Enhancement of mesenchymal stem cell angiogenic capacity and stemness by a biomimetic hydrogel scaffold. Biomaterials 2012, 33, 80–90. [Google Scholar] [CrossRef]
- Tartarini, D.; Mele, E. Adult Stem Cell Therapies for Wound Healing: Biomaterials and Computational Models. Front. Bioeng. Biotechnol. 2015, 3, 206. [Google Scholar] [CrossRef]
- Wu, Y.; Chen, L.; Scott, P.G.; Tredget, E.E. Mesenchymal stem cells enhance wound healing through differentiation and angiogenesis. Stem Cells 2007, 25, 2648–2659. [Google Scholar] [CrossRef]
- Li, J.; Mooney, D.J. Designing hydrogels for controlled drug delivery. Nat. Rev. Mater. 2016, 1, 16071. [Google Scholar] [CrossRef]
- Razavi, M.; Thakor, A.S. An oxygen plasma treated poly(dimethylsiloxane) bioscaffold coated with polydopamine for stem cell therapy. J. Mater. Sci. Mater. Med. 2018, 29, 54. [Google Scholar] [CrossRef]
- Xu, Q.; Sigen, A.; Gao, Y.; Guo, L.; Creagh-Flynn, J.; Zhou, D.; Greiser, U.; Dong, Y.; Wang, F.; Tai, H.; et al. A hybrid injectable hydrogel from hyperbranched PEG macromer as a stem cell delivery and retention platform for diabetic wound healing. Acta Biomater. 2018, 75, 63–74. [Google Scholar] [CrossRef] [PubMed]
- Sadeghi-Avalshahr, A.; Nokhasteh, S.; Molavi, A.M.; Khorsand-Ghayeni, M.; Mahdavi-Shahri, M. Synthesis and characterization of collagen/PLGA biodegradable skin scaffold fibers. Regen. Biomater. 2017, 4, 309–314. [Google Scholar] [CrossRef]
- Suzuki, R.; Kuroyanagi, Y. Safety and utility of a PMMA-based tissue adhesive for closure of surgical incision wounds. J. Biomater. Sci. Polym. Ed. 2013, 24, 287–300. [Google Scholar] [CrossRef] [PubMed]
- Huo, J.; Sun, S.; Geng, Z.; Sheng, W.; Chen, R.; Ma, K.; Sun, X.; Fu, X. Bone Marrow-Derived Mesenchymal Stem Cells Promoted Cutaneous Wound Healing by Regulating Keratinocyte Migration via β2-Adrenergic Receptor Signaling. Mol. Pharm. 2018, 15, 2513–2527. [Google Scholar] [CrossRef] [PubMed]
- Kuo, Y.R.; Wang, C.T.; Cheng, J.T.; Kao, G.S.; Chiang, Y.C.; Wang, C.J. Adipose-Derived Stem Cells Accelerate Diabetic Wound Healing Through the Induction of Autocrine and Paracrine Effects. Cell Transplant. 2016, 25, 71–81. [Google Scholar] [CrossRef] [PubMed]
- Gorecka, J.; Gao, X.; Fereydooni, A.; Dash, B.C.; Luo, J.; Lee, S.R.; Taniguchi, R.; Hsia, H.C.; Qyang, Y.; Dardik, A. Induced pluripotent stem cell-derived smooth muscle cells increase angiogenesis and accelerate diabetic wound healing. Regen. Med. 2020, 15, 1277–1293. [Google Scholar] [CrossRef] [PubMed]
- Laiva, A.L.; O’Brien, F.J.; Keogh, M.B. SDF-1α Gene-Activated Collagen Scaffold Restores Pro-Angiogenic Wound Healing Features in Human Diabetic Adipose-Derived Stem Cells. Biomedicines 2021, 9, 160. [Google Scholar] [CrossRef] [PubMed]
- Dang, H.P.; Vaquette, C.; Shabab, T.; Pérez, R.A.; Yang, Y.; Dargaville, T.R.; Shafiee, A.; Tran, P.A. Porous 3D Printed Scaffolds For Guided Bone Regeneration In a Rat Calvarial Defect Model. Appl. Mater. Today 2020, 20, 100706. [Google Scholar] [CrossRef]
- Zhu, Y.; Hideyoshi, S.; Jiang, H.; Matsumura, Y.; Dziki, J.L.; LoPresti, S.T.; Huleihel, L.; Faria, G.N.; Fuhrman, L.C.; Lodono, R.; et al. Injectable, porous, biohybrid hydrogels incorporating decellularized tissue components for soft tissue applications. Acta Biomater. 2018, 73, 112–126. [Google Scholar] [CrossRef]
- Sivaraj, D.; Chen, K.; Chattopadhyay, A.; Henn, D.; Wu, W.; Noishiki, C.; Magbual, N.J.; Mittal, S.; Mermin-Bunnell, A.M.; Bonham, C.A.; et al. Hydrogel Scaffolds to Deliver Cell Therapies for Wound Healing. Front. Bioeng. Biotechnol. 2021, 9, 660145. [Google Scholar] [CrossRef]
- Spiller, K.L.; Nassiri, S.; Witherel, C.E.; Anfang, R.R.; Ng, J.; Nakazawa, K.R.; Yu, T.; Vunjak-Novakovic, G. Sequential delivery of immunomodulatory cytokines to facilitate the M1-to-M2 transition of macrophages and enhance vascularization of bone scaffolds. Biomaterials 2015, 37, 194–207. [Google Scholar] [CrossRef] [PubMed]
- Shi, C.; Pamer, E.G. Monocyte recruitment during infection and inflammation. Nat. Rev. Immunol. 2011, 11, 762–774. [Google Scholar] [CrossRef] [PubMed]
- Gensel, J.C.; Zhang, B. Macrophage activation and its role in repair and pathology after spinal cord injury. Brain Res. 2015, 1619, 1–11. [Google Scholar] [CrossRef] [PubMed]
- Kim, C.C.; Nakamura, M.C.; Hsieh, C.L. Brain trauma elicits non-canonical macrophage activation states. J. Neuroinflammation 2016, 13, 117. [Google Scholar] [CrossRef] [PubMed]
- Makinde, H.M.; Cuda, C.M.; Just, T.B.; Perlman, H.R.; Schwulst, S.J. Nonclassical Monocytes Mediate Secondary Injury, Neurocognitive Outcome, and Neutrophil Infiltration after Traumatic Brain Injury. J. Immunol. 2017, 199, 3583–3591. [Google Scholar] [CrossRef]
- Monteiro, I.P.; Shukla, A.; Marques, A.P.; Reis, R.L.; Hammond, P.T. Spray-assisted layer-by-layer assembly on hyaluronic acid scaffolds for skin tissue engineering. J. Biomed. Mater. Res. A 2015, 103, 330–340. [Google Scholar] [CrossRef]
- Ng, W.L.; Wang, S.; Yeong, W.Y.; Naing, M.W. Skin Bioprinting: Impending Reality or Fantasy? Trends Biotechnol. 2016, 34, 689–699. [Google Scholar] [CrossRef]
- Poursamar, S.A.; Hatami, J.; Lehner, A.N.; da Silva, C.L.; Ferreira, F.C.; Antunes, A.P. Gelatin porous scaffolds fabricated using a modified gas foaming technique: Characterisation and cytotoxicity assessment. Mater. Sci. Eng. C Mater. Biol. Appl. 2015, 48, 63–70. [Google Scholar] [CrossRef]
- Pedde, R.D.; Mirani, B.; Navaei, A.; Styan, T.; Wong, S.; Mehrali, M.; Thakur, A.; Mohtaram, N.K.; Bayati, A.; Dolatshahi-Pirouz, A.; et al. Emerging Biofabrication Strategies for Engineering Complex Tissue Constructs. Adv. Mater. 2017, 29, 1606061. [Google Scholar] [CrossRef]
- Hosseini, M.; Brown, J.; Shafiee, A. Strategies to induce blood vessel ingrowth into skin grafts and tissue-engineered substitutes. Tissue Eng. Part C Methods 2022, 28, 113–126. [Google Scholar] [CrossRef]
- Yanez, M.; Rincon, J.; Dones, A.; De Maria, C.; Gonzales, R.; Boland, T. In vivo assessment of printed microvasculature in a bilayer skin graft to treat full-thickness wounds. Tissue Eng. Part A 2015, 21, 224–233. [Google Scholar] [CrossRef] [PubMed]
- Singh, S.; Choudhury, D.; Yu, F.; Mironov, V.; Naing, M.W. In situ bioprinting—Bioprinting from benchside to bedside? Acta Biomater. 2020, 101, 14–25. [Google Scholar] [CrossRef] [PubMed]
- Kyburz, K.A.; Anseth, K.S. Three-dimensional hMSC motility within peptide-functionalized PEG-based hydrogels of varying adhesivity and crosslinking density. Acta Biomater. 2013, 9, 6381–6392. [Google Scholar] [CrossRef]
- Schultz, K.M.; Kyburz, K.A.; Anseth, K.S. Measuring dynamic cell-material interactions and remodeling during 3D human mesenchymal stem cell migration in hydrogels. Proc. Natl. Acad. Sci. USA 2015, 112, E3757–E3764. [Google Scholar] [CrossRef] [PubMed]
- Daviran, M.; Catalano, J.; Schultz, K.M. Determining How Human Mesenchymal Stem Cells Change Their Degradation Strategy in Response to Microenvironmental Stiffness. Biomacromolecules 2020, 21, 3056–3068. [Google Scholar] [CrossRef]
- Lokhande, G.; Carrow, J.K.; Thakur, T.; Xavier, J.R.; Parani, M.; Bayless, K.J.; Gaharwar, A.K. Nanoengineered injectable hydrogels for wound healing application. Acta Biomater. 2018, 70, 35–47. [Google Scholar] [CrossRef]
- Lord, M.S.; Foss, M.; Besenbacher, F. Influence of nanoscale surface topography on protein adsorption and cellular response. Nano Today 2010, 5, 66–78. [Google Scholar] [CrossRef]
- Noro, A.; Kaneko, M.; Murata, I.; Yoshinari, M. Influence of surface topography and surface physicochemistry on wettability of zirconia (tetragonal zirconia polycrystal). J. Biomed. Mater. Res. B Appl. Biomater. 2013, 101, 355–363. [Google Scholar] [CrossRef]
- Kim, D.-H.; Han, K.; Gupta, K.; Kwon, K.W.; Suh, K.-Y.; Levchenko, A. Mechanosensitivity of fibroblast cell shape and movement to anisotropic substratum topography gradients. Biomaterials 2009, 30, 5433–5444. [Google Scholar] [CrossRef]
- Wang, X.; Nakamoto, T.; Dulińska-Molak, I.; Kawazoe, N.; Chen, G. Regulating the stemness of mesenchymal stem cells by tuning micropattern features. J. Mater. Chem. B 2016, 4, 37–45. [Google Scholar] [CrossRef]
- Oyama, T.G.; Oyama, K.; Kimura, A.; Yoshida, F.; Ishida, R.; Yamazaki, M.; Miyoshi, H.; Taguchi, M. Collagen hydrogels with controllable combined cues of elasticity and topography to regulate cellular processes. Biomed. Mater. 2021, 16, 045037. [Google Scholar] [CrossRef] [PubMed]
- Smith, A.G.; Din, A.; Denyer, M.; Crowther, N.J.; Eagland, D.; Vowden, K.; Vowden, P.; Britland, S.T. Microengineered surface topography facilitates cell grafting from a prototype hydrogel wound dressing with antibacterial capability. Biotechnol. Prog. 2006, 22, 1407–1415. [Google Scholar] [CrossRef] [PubMed]
- Hosseini, M.; Brown, J.; Khosrotehrani, K.; Bayat, A.; Shafiee, A. Skin biomechanics: A potential therapeutic intervention target to reduce scarring. Burns Trauma. 2022, 10, unpublished. [Google Scholar] [CrossRef] [PubMed]
- Huang, R.; Xu, L.; Wang, Y.; Zhang, Y.; Lin, B.; Lin, Z.; Li, J.; Li, X. Efficient fabrication of stretching hydrogels with programmable strain gradients as cell sheet delivery vehicles. Mater. Sci. Eng. C 2021, 129, 112415. [Google Scholar] [CrossRef]
- Shafiee, A.; Cavalcanti, A.S.; Saidy, N.T.; Schneidereit, D.; Friedrich, O.; Ravichandran, A.; De-Juan-Pardo, E.M.; Hutmacher, D.W. Convergence of 3D printed biomimetic wound dressings and adult stem cell therapy. Biomaterials 2021, 268, 120558. [Google Scholar] [CrossRef]
- Yannas, I.V.; Tzeranis, D.S.; So, P.T.C. Regeneration of injured skin and peripheral nerves requires control of wound contraction, not scar formation. Wound Repair. Regen. 2017, 25, 177–191. [Google Scholar] [CrossRef]
- Lotz, S.; Goderie, S.; Tokas, N.; Hirsch, S.E.; Ahmad, F.; Corneo, B.; Le, S.; Banerjee, A.; Kane, R.S.; Stern, J.H.; et al. Sustained levels of FGF2 maintain undifferentiated stem cell cultures with biweekly feeding. PLoS ONE 2013, 8, e56289. [Google Scholar] [CrossRef]
- Meng, X.T.; Li, C.; Dong, Z.Y.; Liu, J.M.; Li, W.; Liu, Y.; Xue, H.; Chen, D. Co-transplantation of bFGF-expressing amniotic epithelial cells and neural stem cells promotes functional recovery in spinal cord-injured rats. Cell Biol. Int. 2008, 32, 1546–1558. [Google Scholar] [CrossRef]
- Gümüşderelioğlu, M.; Dalkıranoğlu, S.; Aydın, R.S.T.; Çakmak, S. A novel dermal substitute based on biofunctionalized electrospun PCL nanofibrous matrix. J. Biomed. Mater. Res. Part A 2011, 98A, 461–472. [Google Scholar] [CrossRef]
- Tığlı, R.S.; Kazaroğlu, N.M.; Mavış, B.; Gümüşderelioğlu, M. Cellular Behavior on Epidermal Growth Factor (EGF)-Immobilized PCL/Gelatin Nanofibrous Scaffolds. J. Biomater. Sci. Polym. Ed. 2011, 22, 207–223. [Google Scholar] [CrossRef]
- Xie, Y.; Upton, Z.; Richards, S.; Rizzi, S.C.; Leavesley, D.I. Hyaluronic acid: Evaluation as a potential delivery vehicle for vitronectin:growth factor complexes in wound healing applications. J. Control. Release 2011, 153, 225–232. [Google Scholar] [CrossRef] [PubMed]
- Choi, J.S.; Leong, K.W.; Yoo, H.S. In vivo wound healing of diabetic ulcers using electrospun nanofibers immobilized with human epidermal growth factor (EGF). Biomaterials 2008, 29, 587–596. [Google Scholar] [CrossRef]
- Zhou, W.; Zhao, M.; Zhao, Y.; Mou, Y. A fibrin gel loaded with chitosan nanoparticles for local delivery of rhEGF: Preparation and in vitro release studies. J. Mater. Sci. Mater. Med. 2011, 22, 1221–1230. [Google Scholar] [CrossRef] [PubMed]
- Wang, F.; Wang, M.; She, Z.; Fan, K.; Xu, C.; Chu, B.; Chen, C.; Shi, S.; Tan, R. Collagen/chitosan based two-compartment and bi-functional dermal scaffolds for skin regeneration. Mater. Sci. Eng. C Mater. Biol. Appl. 2015, 52, 155–162. [Google Scholar] [CrossRef] [PubMed]
- Choi, J.S.; Yoo, H.S. Pluronic/chitosan hydrogels containing epidermal growth factor with wound-adhesive and photo-crosslinkable properties. J. Biomed. Mater. Res. A 2010, 95, 564–573. [Google Scholar] [CrossRef] [PubMed]
- Yang, Y.; Xia, T.; Chen, F.; Wei, W.; Liu, C.; He, S.; Li, X. Electrospun fibers with plasmid bFGF polyplex loadings promote skin wound healing in diabetic rats. Mol. Pharm. 2012, 9, 48–58. [Google Scholar] [CrossRef]
- ukomskyj, A.O.; Rao, N.; Yan, L.; Pye, J.S.; Li, H.; Wang, B.; Li, J.J. Stem Cell-Based Tissue Engineering for the Treatment of Burn Wounds: A Systematic Review of Preclinical Studies. Stem Cell Rev. Rep. 2022, 18, 1926–1955. [Google Scholar] [CrossRef]
- Elbialy, Z.I.; Assar, D.H.; Abdelnaby, A.; Asa, S.A.; Abdelhiee, E.Y.; Ibrahim, S.S.; Abdel-Daim, M.M.; Almeer, R.; Atiba, A. Healing potential of Spirulina platensis for skin wounds by modulating bFGF, VEGF, TGF-ß1 and α-SMA genes expression targeting angiogenesis and scar tissue formation in the rat model. Biomed. Pharmacother. 2021, 137, 111349. [Google Scholar] [CrossRef]
- Jung, S.-M.; Min, S.K.; Lee, H.C.; Kwon, Y.S.; Jung, M.H.; Shin, H.S. Spirulina-PCL Nanofiber Wound Dressing to Improve Cutaneous Wound Healing by Enhancing Antioxidative Mechanism. J. Nanomater. 2016, 2016, 6135727. [Google Scholar]
- Steffens, D.; Leonardi, D.; Soster, P.R.D.L.; Lersch, M.; Rosa, A.; Crestani, T.; Scher, C.; de Morais, M.G.; Costa, J.A.V.; Pranke, P. Development of a new nanofiber scaffold for use with stem cells in a third degree burn animal model. Burns 2014, 40, 1650–1660. [Google Scholar] [CrossRef]
- Vallejo, M.; Moura, N.; Gomes, A.; Joaquinito, A.; Faustino, M.; Almeida, A.; Gonçalves, I.; Serra, V.; Neves, M. The Role of Porphyrinoid Photosensitizers for Skin Wound Healing. Int. J. Mol. Sci. 2021, 22, 4121. [Google Scholar] [CrossRef] [PubMed]
- Koo, M.-A.; Hong, S.H.; Lee, M.H.; Kwon, B.-J.; Seon, G.M.; Kim, M.S.; Kim, D.; Nam, K.C.; Park, J.-C. Effective stacking and transplantation of stem cell sheets using exogenous ROS-producing film for accelerated wound healing. Acta Biomater. 2019, 95, 418–426. [Google Scholar] [CrossRef] [PubMed]
- Lei, J.; Sun, L.; Huang, S.; Zhu, C.; Li, P.; He, J.; Mackey, V.; Coy, D.H.; He, Q. The antimicrobial peptides and their potential clinical applications. Am. J. Transl. Res. 2019, 11, 3919–3931. [Google Scholar] [PubMed]
- Kasetty, G.; Kalle, M.; Mörgelin, M.; Brune, J.C.; Schmidtchen, A. Anti-endotoxic and antibacterial effects of a dermal substitute coated with host defense peptides. Biomaterials 2015, 53, 415–425. [Google Scholar] [CrossRef] [PubMed]
- Pickart, L.; Vasquez-Soltero, J.M.; Margolina, A. GHK Peptide as a Natural Modulator of Multiple Cellular Pathways in Skin Regeneration. BioMed Res. Int. 2015, 2015, 648108. [Google Scholar] [CrossRef]
- Arul, V.; Gopinath, D.; Gomathi, K.; Jayakumar, R. Biotinylated GHK peptide incorporated collagenous matrix: A novel biomaterial for dermal wound healing in rats. J. Biomed. Mater. Res. B Appl. Biomater. 2005, 73, 383–391. [Google Scholar] [CrossRef]
- Hosoyama, K.; Lazurko, C.; Muñoz, M.; McTiernan, C.D.; Alarcon, E.I. Peptide-Based Functional Biomaterials for Soft-Tissue Repair. Front. Bioeng. Biotechnol. 2019, 7, 205. [Google Scholar] [CrossRef] [PubMed]
- Krishna, O.D.; Kiick, K.L. Protein-and peptide-modified synthetic polymeric biomaterials. Pept. Sci. Orig. Res. Biomol. 2010, 94, 32–48. [Google Scholar] [CrossRef]
- Dong, Y.; Cui, M.; Qu, J.; Wang, X.; Kwon, S.H.; Barrera, J.; Elvassore, N.; Gurtner, G.C. Conformable hyaluronic acid hydrogel delivers adipose-derived stem cells and promotes regeneration of burn injury. Acta Biomater. 2020, 108, 56–66. [Google Scholar] [CrossRef]
- Parisi, L.; Toffoli, A.; Ghezzi, B.; Mozzoni, B.; Lumetti, S.; Macaluso, G.M. A glance on the role of fibronectin in controlling cell response at biomaterial interface. Jpn. Dent. Sci. Rev. 2020, 56, 50–55. [Google Scholar] [CrossRef]
- Zollinger, A.J.; Smith, M.L. Fibronectin, the extracellular glue. Matrix Biol. 2017, 61, 27–37. [Google Scholar] [CrossRef] [PubMed]
- Gomes, S.; Leonor, I.B.; Mano, J.F.; Reis, R.L.; Kaplan, D.L. Natural and Genetically Engineered Proteins for Tissue Engineering. Prog. Polym. Sci. 2012, 37, 1–17. [Google Scholar] [CrossRef] [PubMed]
- Pradhan, S.; Farach-Carson, M.C. Mining the extracellular matrix for tissue engineering applications. Regen. Med. 2010, 5, 961–970. [Google Scholar] [CrossRef]
- Kallmeyer, K.; André-Lévigne, D.; Baquié, M.; Krause, K.-H.; Pepper, M.S.; Pittet-Cuénod, B.; Modarressi, A. Fate of systemically and locally administered adipose-derived mesenchymal stromal cells and their effect on wound healing. Stem Cells Transl. Med. 2020, 9, 131–144. [Google Scholar] [CrossRef] [PubMed]
- Lee, C.; Shim, S.; Jang, H.; Myung, H.; Lee, J.; Bae, C.-H.; Myung, J.K.; Kim, M.-J.; Lee, S.B.; Jang, W.-S.; et al. Human umbilical cord blood-derived mesenchymal stromal cells and small intestinal submucosa hydrogel composite promotes combined radiation-wound healing of mice. Cytotherapy 2017, 19, 1048–1059. [Google Scholar] [CrossRef]
- Myung, H.; Jang, H.; Myung, J.K.; Lee, C.; Lee, J.; Kang, J.; Jang, W.; Lee, S.; Kim, H.; Kim, H.; et al. Platelet-rich plasma improves the therapeutic efficacy of mesenchymal stem cells by enhancing their secretion of angiogenic factors in a combined radiation and wound injury model. Exp. Dermatol. 2020, 29, 158–167. [Google Scholar] [CrossRef]
- Tausche, A.-K.; Skaria, M.; Bohlen, L.; Liebold, K.; Hafner, J.; Friedlein, H.; Meurer, M.; Goedkoop, R.J.; Wollina, U.; Salomon, D.; et al. An autologous epidermal equivalent tissue-engineered from follicular outer root sheath keratinocytes is as effective as split-thickness skin autograft in recalcitrant vascular leg ulcers. Wound Repair. Regen. 2003, 11, 248–252. [Google Scholar] [CrossRef]
- Ortega-Zilic, N.; Hunziker, T.; Läuchli, S.; Mayer, D.; Huber, C.; Conzett, K.B.; Sippel, K.; Borradori, L.; French, L.E.; Hafner, J. EpiDex® Swiss field trial 2004–2008. Dermatology 2010, 221, 365–372. [Google Scholar] [CrossRef]
- Hanft, J.R.; Surprenant, M.S. Healing of chronic foot ulcers in diabetic patients treated with a human fibroblast-derived dermis. J. Foot Ankle Surg. 2002, 41, 291–299. [Google Scholar] [CrossRef]
- Harding, K.; Sumner, M.; Cardinal, M. A prospective, multicentre, randomised controlled study of human fibroblast-derived dermal substitute (Dermagraft) in patients with venous leg ulcers. Int. Wound J. 2013, 10, 132–137. [Google Scholar] [CrossRef]
- Falanga, V.; Sabolinski, M. A bilayered living skin construct (APLIGRAF) accelerates complete closure of hard-to-heal venous ulcers. Wound Repair Regen. 1999, 7, 201–207. [Google Scholar] [CrossRef] [PubMed]
- Falanga, V.J. Tissue engineering in wound repair. Adv. Skin Wound Care 2000, 13, 15–19. [Google Scholar] [PubMed]
- Edmonds, M. Apligraf in the treatment of neuropathic diabetic foot ulcers. Int. J. Low Extrem. Wounds 2009, 8, 11–18. [Google Scholar] [CrossRef] [PubMed]
- Veves, A.; Falanga, V.; Armstrong, D.G.; Sabolinski, M.L. Graftskin, a human skin equivalent, is effective in the management of noninfected neuropathic diabetic foot ulcers: A prospective randomized multicenter clinical trial. Diabetes Care 2001, 24, 290–295. [Google Scholar] [CrossRef] [PubMed]
- Centanni, J.M.; Straseski, J.A.; Wicks, A.; Hank, J.A.; Rasmussen, C.A.; Lokuta, M.A.; Schurr, M.J.; Foster, K.N.; Faucher, L.D. StrataGraft skin substitute is well-tolerated and is not acutely immunogenic in patients with traumatic wounds: Results from a prospective, randomized, controlled dose escalation trial. Ann. Surg. 2011, 253, 672–683. [Google Scholar] [CrossRef] [PubMed]
- Gibson, A.L.; Holmes, J.H., IV; Shupp, J.W.; Smith, D.; Joe, V.; Carson, J.; Litt, J.; Kahn, S.; Short, T.; Cancio, L.; et al. A phase 3, open-label, controlled, randomized, multicenter trial evaluating the efficacy and safety of StrataGraft® construct in patients with deep partial-thickness thermal burns. Burns 2021, 47, 1024–1037. [Google Scholar] [CrossRef]
- Falanga, V.; Iwamoto, S.; Chartier, M.; Yufit, T.; Butmarc, J.; Kouttab, N.; Shrayer, D.; Carson, P. Autologous bone marrow-derived cultured mesenchymal stem cells delivered in a fibrin spray accelerate healing in murine and human cutaneous wounds. Tissue Eng. 2007, 13, 1299–1312. [Google Scholar] [CrossRef]
- Portas, M.; Mansilla, E.; Drago, H.; Dubner, D.; Radl, A.; Coppola, A.; Di Giorgio, M. Use of Human Cadaveric Mesenchymal Stem Cells for Cell Therapy of a Chronic Radiation-Induced Skin Lesion: A Case Report. Radiat. Prot. Dosim. 2016, 171, 99–106. [Google Scholar] [CrossRef]
- Iacono, E.; Merlo, B.; Pirrone, A.; Antonelli, C.; Brunori, L.; Romagnoli, N.; Castagnetti, C. Effects of mesenchymal stem cells isolated from amniotic fluid and platelet-rich plasma gel on severe decubitus ulcers in a septic neonatal foal. Res. Vet. Sci. 2012, 93, 1439–1440. [Google Scholar] [CrossRef]
- de Leon, J.M.; Driver, V.R.; Fylling, C.P.; Carter, M.J.; Anderson, C.; Wilson, J.; Dougherty, R.M.; Fuston, D.; Trigilia, D.; Valenski, V.; et al. The clinical relevance of treating chronic wounds with an enhanced near-physiological concentration of platelet-rich plasma gel. Adv. Skin Wound Care 2011, 24, 357–368. [Google Scholar] [CrossRef]
- Hess, L.H.; Jansen, M.; Maybeck, V.; Hauf, M.V.; Seifert, M.; Stutzmann, M.; Sharp, I.D.; Offenhäusser, A.; Garrido, J.A. Graphene transistor arrays for recording action potentials from electrogenic cells. Adv. Mater. 2011, 23, 5045–5049. [Google Scholar] [CrossRef] [PubMed]
- Dankerl, M.; Hauf, M.V.; Lippert, A.; Hess, L.H.; Birner, S.; Sharp, I.D.; Mahmood, A.; Mallet, P.; Veuillen, J.-Y.; Stutzmann, M.; et al. Graphene Solution-Gated Field-Effect Transistor Array for Sensing Applications. Adv. Funct. Mater. 2010, 20, 3117–3124. [Google Scholar] [CrossRef]
- Tian, B.; Liu, J.; Dvir, T.; Jin, L.; Tsui, J.H.; Qing, Q.; Suo, Z.; Langer, R.; Kohane, D.S.; Lieber, C.M. Macroporous nanowire nanoelectronic scaffolds for synthetic tissues. Nat. Mater. 2012, 11, 986–994. [Google Scholar] [CrossRef] [PubMed]
- Marshall, C.D.; Hu, M.S.; Leavitt, T.; Barnes, L.A.; Lorenz, H.P.; Longaker, M.T. Cutaneous Scarring: Basic Science, Current Treatments, and Future Directions. Adv. Wound Care 2018, 7, 29–45. [Google Scholar] [CrossRef]
| Stem/Progenitor Cells | Treatment Group(s) | Wound Type | Remarks | Reference |
|---|---|---|---|---|
| Adipose-derived MSCs | Adipose tissue derived MSCs | CLI | - 66.7% of patients showed ulcer healing - The treatment showed the formation of numerous vascular collateral networks | [44] * |
| 1: Autologous adipose-derived stem and regenerative cells plus traditional methods and advanced dressings 2: Only traditional methods and nonadherent dressings | Chronic ulcer of lower limbs | - There was a reduction in both the diameter and depth of the ulcer - In 6 of 10 cases, there was complete healing of the ulcer | [46] | |
| Autologous cultured adipose-derived stroma/SCs | Non-revascularizable critical limb ischemia | - Ulcer evolution and wound healing showed improvement | [47] ** | |
| Non-culture-expanded autologous, adipose-derived stromal vascular fraction cells | CLI | - 6 of the 10 patients with non-healing ulcers had a complete closure - There was evidence of neovascularization in 5 patients | [48] * | |
| Adipose-derived SCs | Hypertensive leg ulcers | - Wound surfaces constantly and significantly decreased (wound closure rate of 73.2% at month 3 and 93.1% at month 6) - Percentages of fibrin and necrosis decreased, whereas granulation tissue increased significantly - There was no recurrence | [49] * | |
| 1: Autologous stromal vascular fraction cells plus a wound dressing 2: A standard dressing | Chronic VLU and AVLU | - All VLU patients and 4 of 9 AVLU patients showed complete epithelialization of the ulcers within 71–174 days - In 3 patients with large ulcerations on both legs, ulcerations on the non-treated, contralateral leg also epithelialized (paracrine effects seemed to stimulate the regenerative changes even at a large distance) | [50] | |
| Bone marrow derived MSCs | 1: Allogeneic bone marrow-derived MSCs 2: PlasmaLyte A | CLI | - The use of allogeneic BM-MSCs was safe in patients with CLI - All ulcers at two-year follow-up healed in group 2, whereas one patient in group 1 continued to have ulcers but with reduced size | [51] |
| 1: Bone marrow-derived cells 2: Autologous peripheral blood plus regular wound care treatments | Chronic lower limb wounds due to diabetes mellitus | - The average decrease in wound area at 2 (17.4% vs. 4.84%) and 12 (36.4% vs. 27.32%) weeks was higher in group 1 compared to in group 2 | [52] | |
| 1: Bone marrow MSCs 2: Bone marrow-derived mononuclear cells 3: normal saline | Diabetic critical limb ischemia | - The ulcer healing rate was significantly higher in group 1 - They reached 100% four weeks earlier than group 2 - Ulcer healing rate in group 2 was significantly higher than in group 3, which appeared at 12 weeks | [53] | |
| Autologous bone marrow nuclear cells | Pressure ulcers | - Pressure ulcers had fully healed after a mean time of 21 days in 86.36% of the patients - During a mean follow-up of 19 months, none of the resolved ulcers recurred | [54] * | |
| 1: Autologous bone marrow aspirate 2: Saline dressings | Chronic wounds | - Group 1 achieved a significant reduction in the wound surface area | [55] | |
| Progenitor cells | CD34+ cells isolated from bone marrow | Sacral pressure sore | - The treatment positively affected granulation tissue formation and wound contraction, which showed about a 50% reduction in the pressure sore volume on the treated side versus a 40% reduction on the control side | [45] ** |
| Genetically modified epidermal stem cells | Junctional epidermolysis bullosa | - Complete engraftment was achieved following 8 days - Transduced stem cells enabled the regeneration of epidermis | [56] ** | |
| Genetically modified epidermal stem cells | Junctional epidermolysis bullosa | - The human epidermis is supported not by equipotent progenitors, but by long-lived stem cells with an extensive self-renewal ability so that they could generate progenitors to renew terminally differentiated keratinocytes | [57] ** | |
| Bone marrow-derived mononuclear cells | Mononuclear bone marrow cells | Chronic venous and neuro-ischemic wounds | - The treatment led to a wound size reduction, a markedly increased vascularization, and infiltration of mononuclear cells | [58] ** |
| Placental MSCs | 1: Cryopreserved human placental tissue in a human viable wound matrix plus standard compression therapy 2: Standard compression therapy | VLU | - Complete healing in 53% of the cases in group 1 - Reduction in wound size by half (80% in group 1 vs. 25% in group 2) | [59] |
| Human placenta-derived mesenchymal stromal-like cells (cenplacel) | DFUs with PAD | - There was preliminary evidence of ulcer healing in seven patients (five complete; two partial) within 3 months of cenplacel treatment - Circulating endothelial cell levels (a biomarker of vascular injury in PAD) were decreased within 1 month - Cenplacel was generally safe and well-tolerated in patients with chronic DFUs and PAD | [60] * | |
| Umbilical cord MSCs | 1: Human umbilical cord MSCs plus a percutaneous angioplasty treatment 2: A percutaneous angioplasty treatment | Ulcer wounds | - 3 months after treatment, there was a significant increase in neovessels accompanied by complete or gradual ulcer healing in group 1 | [61] |
| Technologies | Biofabrication Mode | Biomaterial Platforms | Biomaterial | Cell Type | Remarks | Reference |
|---|---|---|---|---|---|---|
| Cell electrospinning | Bioassembly | Nanofibers | Polyvinyl alcohol | Bone marrow-derived SCs | - Good infiltration and cell growth due to the even distribution of the cells throughout the fiber filaments - Acceleration of wound healing and appendage regeneration by promoting granulation tissue repair - Formation of dense and mature collagen fiber structure parallel to the epidermis | [69] |
| Extrusion | Bioassembly (vibrational modality) | Shell/core microcapsules | Poly(methyl-methacrylate) | Human dermal fibroblasts | - Decrease of cell viability as long as the number of microcapsules increased - After 72 h incubation, microcapsules did not interfere with cell growth - Slow cell proliferation inside the microcapsules | [70] |
| Bioassembly (electrostatic droplet modality) | Microcapsules | Alginate | Human adipose-derived SCs | - Growth of the encapsulated cells in static culture by 3 weeks - Cell survival after injection into a nude mouse - Protection of the cells during injection—potential deterrent to donor cell migration | [71] | |
| Soft lithography | Bioprinting | Microgels | Hyaluronic acid modified with photoreactive methacrylates | Fibroblasts | - Uniform distribution of the cells throughout the gel (depending on the crosslinking process) - Maintaining the cell viability (depending on the exposure time of the cells to ultra violet, photoinitiator concentration and exposure to dry air) - Cell-mediated degradation of hydrogels | [72] |
| Photolithography | Bioprinting | Microgels | GelMA and graphene oxide | Fibroblasts | - Support of cellular adhesion and spreading with improved viability and proliferation - Robust mechanical properties and excellent flexibility - Able to construct multilayer cell-laden hydrogels | [73] |
| Emulsion | Bioassembly | Hydrogels | Sodium alginate | Keratinocyte clusteroids | - Growth of the clusteroids in the hydrogels - Percolation of the clusteroids through the hydrogel and formation of an integral tissue | [74] |
| Microfluidics | Bioassembly | Hollow microspheres | Bacterial cellulose | Primary epidermal keratinocytes | - Increased proliferation due to the high porosity of the microsphere scaffold - Enhanced wound healing due to 3D mimicry of the native skin ECM and water retention | [75] |
| Bioassembly | Microporous annealed particle gels | Multi-armed poly(ethylene)glycol-vinyl sulfone functionalized with RGD | Dermal fibroblasts, adipose-derived MSCs; bone marrow-derived MSCs | - Cell proliferation and formation of extensive 3D networks by the incorporated cells - Facilitation of the cell migration, rapid cutaneous tissue regeneration and tissue structure formation due to a stably linked interconnected network of micropores | [76] | |
| Bioprinting | Bioprinting (inkjet modality) | Hydrogels | Fibrin and collagen | Amniotic fluid-derived SCs and bone marrow-derived MSCs | - Facilitation of quick wound and closure and angiogenesis due to delivery of secreted trophic factors - Greater re-epithelialization - Increased microvessel density - Transient integration of the cells with the surrounding tissue | [77] |
| In vitro bioprinting (extrusion modality) | 3D cell-printed full-thickness human skin equivalent | Decellularized ECM-based skin | Endothelial progenitor cells and adipose-derived SCs | - Sufficient recapitulation of the microenvironment physiologically relevant to the skin cells (dense and thick microstructure) - Improved epidermal organization, dermal ECM secretion and barrier function - Acceleration of wound closure, re-epithelization, neovascularization, and blood flow | [78] | |
| In vivo bioprinting (extrusion modality) | Two-layered skin construct (hydrogel) | Fibrinogen and collagen | Human fibroblasts and human keratinocytes | - Capable of delivering the cells to the specific target sites - Rapid wound closure, reduced contraction and accelerated re-epithelialization - Regeneration of tissues with a dermal structure and composition similar to healthy skin, with extensive collagen deposition arranged in large, organized fibers, extensive mature vascular formation and proliferating keratinocytes | [79] | |
| In vivo bioprinting (extrusion modality) | Skin precursor sheets | Fibrin and hyaluronic acid | Mesenchymal stem/stromal cells | - High cell viability and increased proliferation - Improved re-epithelialization, dermal cell repopulation and neovascularization | [80] |
| Growth Factor | Biomaterial Composition | Delivery System | Study Type | Remarks | Ref. |
|---|---|---|---|---|---|
| IGF and EGF (vitronectin: GF complexes) | HA hydrogel | Surface presentation, physical adsorption | In vitro culture of fibroblasts and keratinocytes Ex vivo model of 3D de-epidermized dermis human skin equivalent | In vitro: the combination of the complexes and HA activated the proliferation of human fibroblasts but not keratinocytes. Ex vivo: the combination improved the proliferative and differentiating layers. HA promoted absorption and transport. | [131] |
| EGF | Electrospun nanofibers of PCL-b-PEG | Surface presentation, chemical conjugation | In vitro culture of keratinocytes In vivo model of full-thickness diabetic wounds in mice | In vitro: the conjugation of EGF to nanofibers considerably enhanced the expression of keratinocyte-specific genes. In vivo: the conjugation led to better wound healing outcomes such as wound closure. The expression of EGF-receptor was on a significant rise. | [132] |
| EGF | Fibrin gel loaded within chitosan nanoparticles | Controlled sustained release | In vitro culture of fibroblasts | EGF released from the composite gel was bioactive for one week at most. It could activate the proliferation of fibroblasts. | [133] |
| VEGF | Two-compartment and bi-functional scaffold from chitosan/collagen-containing PLGA microspheres | Preprogrammed release | In vitro culture of fibroblasts | VEGF showed a linear release behavior over a long period (49 days). The scaffold could support cell adhesion and proliferation. | [134] |
| EGF | Photo-cross-linkable pluronic/chitosan hydrogel | Responsive release | In vitro culture of keratinocytes In vivo model of diabetic ulcers in mice | In vitro: EGF contributed to the retention of original phenotypes of keratinocytes. In vivo: EGF had high retention in the hydrogel at the wound site, which was in favor of the proliferation of keratinocytes. The slow release of EGF carried an effect on the keratinocytes proliferation of epidermal cells and supported wound recovery. EGF worked better in the differentiation of epidermal cells into keratinocytes, than in the acceleration of wound healing rates. | [135] |
| Polyplexes of bFGF | Electrospun core−sheath fibers from PELA | Gene transfection | In vitro culture of fibroblasts In vivo model of diabetic skin wounds | In vitro: bFGF improved cell proliferation. The transfection continued for over four weeks. In vivo: its release led to considerably high wound recovery with enhanced vascularization, collagen deposition and maturation, complete re-epithelialization and skin appendage restoration. | [136] |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Hosseini, M.; Dalley, A.J.; Shafiee, A. Convergence of Biofabrication Technologies and Cell Therapies for Wound Healing. Pharmaceutics 2022, 14, 2749. https://doi.org/10.3390/pharmaceutics14122749
Hosseini M, Dalley AJ, Shafiee A. Convergence of Biofabrication Technologies and Cell Therapies for Wound Healing. Pharmaceutics. 2022; 14(12):2749. https://doi.org/10.3390/pharmaceutics14122749
Chicago/Turabian StyleHosseini, Motaharesadat, Andrew J. Dalley, and Abbas Shafiee. 2022. "Convergence of Biofabrication Technologies and Cell Therapies for Wound Healing" Pharmaceutics 14, no. 12: 2749. https://doi.org/10.3390/pharmaceutics14122749
APA StyleHosseini, M., Dalley, A. J., & Shafiee, A. (2022). Convergence of Biofabrication Technologies and Cell Therapies for Wound Healing. Pharmaceutics, 14(12), 2749. https://doi.org/10.3390/pharmaceutics14122749







