Liposomes to Augment Dialysis in Preclinical Models: A Structured Review
Abstract
1. Introduction
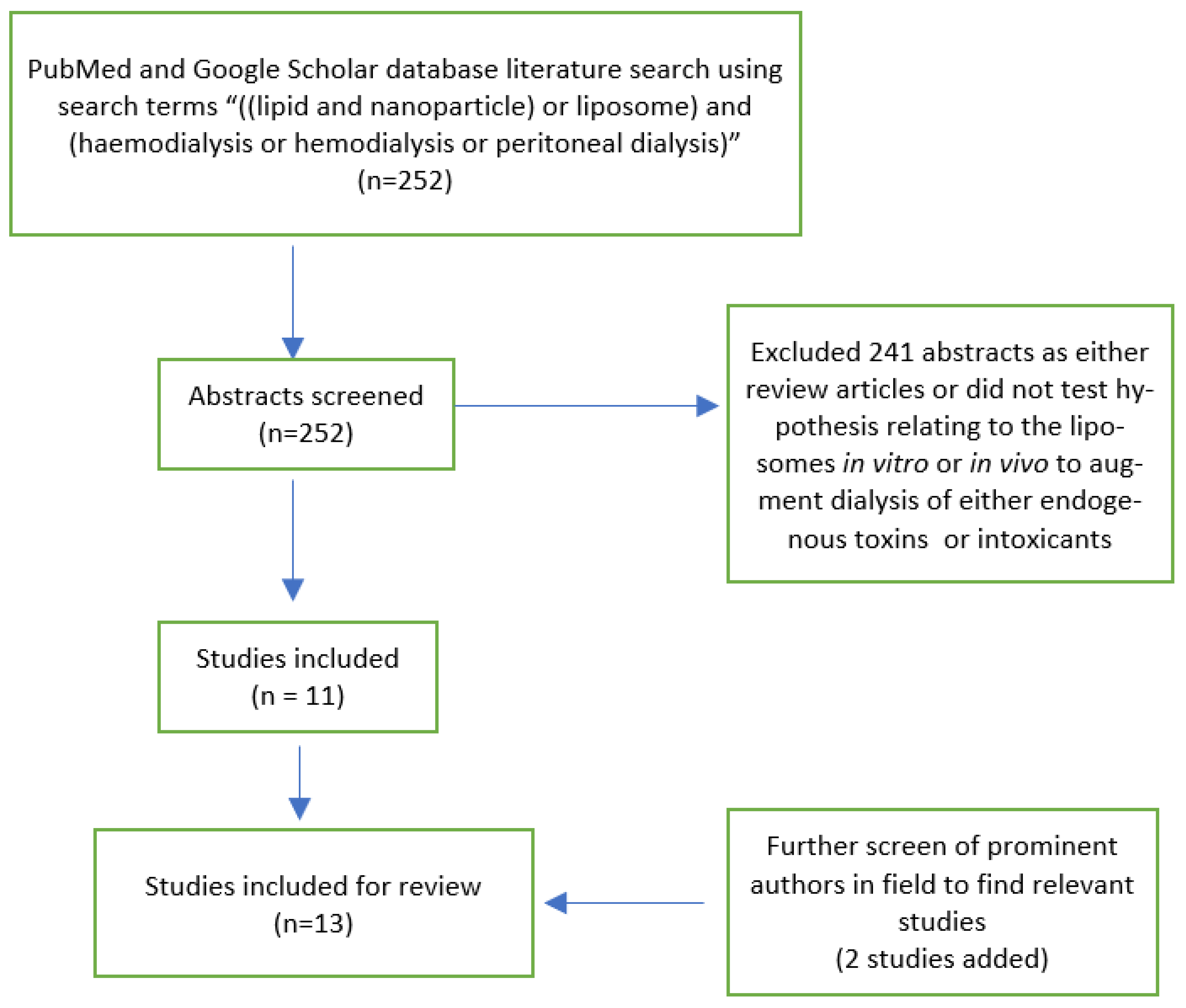
2. Methods
3. Results
4. Discussion
4.1. Endogenous Toxic Substances
4.2. Endogenous Protein-Bound Solute Dialysis
4.3. Exogenous Toxic Substances
4.4. Enzymatic Liposome Dialysis
4.5. Liposome Formulation and Modifications
4.6. Challenges/Perspective
5. Conclusions
Funding
Conflicts of Interest
References
- Devuyst, O.; Schumann, A. Peritoneal dialysis: Nanoparticles have entered the game. Perit. Dial. Int. 2015, 35, 240. [Google Scholar] [CrossRef]
- Allen, T.M.; Cullis, P.R. Liposomal drug delivery systems: From concept to clinical applications. Adv. Drug Deliv. Rev. 2013, 65, 36–48. [Google Scholar] [CrossRef]
- Cave, G. Drug Scavenging Lipid Based Nanoparticles for Detoxification In Vivo. Ph.D. Thesis, University of Auckland, Auckland, New Zealand, 2018. [Google Scholar]
- Cave, G.; Harvey, M.; Wu, Z. Drug scavenging lipid based nanoparticles as detoxifying agents in vivo. In Fundamentals of Nanoparticles, 1st ed.; Barhoum, A., Makhlouf, A.S.H., Eds.; Elsevier: Amsterdam, The Netherlands, 2018; pp. 425–450. [Google Scholar]
- Forster, V.; Luciani, P.; Leroux, J.C. Treatment of calcium channel blocker-induced cardiovascular toxicity with drug scavenging liposomes. Biomaterials 2012, 33, 3578–3585. [Google Scholar] [CrossRef] [PubMed]
- Szebeni, J. Complement activation-related pseudoallergy: A stress reaction in blood triggered by nanomedicines and biologicals. Mol. Immunol. 2014, 61, 163–173. [Google Scholar] [CrossRef]
- Ronco, C.; Clark, W.R. Haemodialysis membranes. Nat. Rev. Nephrol. 2018, 14, 394–410. [Google Scholar] [CrossRef]
- De Vriese, A.S.; Langlois, M.; Bernard, D.; Geerolf, I.; Stevens, L.; Boelaert, J.R.; Schurgers, M.; Matthys, E. Effect of dialyser membrane pore size on plasma homocysteine levels in haemodialysis patients. Nephrol. Dial. Transplant. 2003, 18, 2596–2600. [Google Scholar] [CrossRef]
- Forneris, F.; Wu, J.; Xue, X.; Ricklin, D.; Lin, Z.; Sfyroera, G.; Tzekou, A.; Volokhina, E.; Granneman, J.C.; Hauhart, R.; et al. Regulators of complement activity mediate inhibitory mechanisms through a common C3b-binding mode. EMBO J. 2016, 35, 1133–1149. [Google Scholar] [CrossRef]
- Devuyst, O.; Goffin, E. Water and solute transport in peritoneal dialysis: Models and clinical applications. Nephrol. Dial. Transplant. 2008, 23, 2120–2123. [Google Scholar] [CrossRef]
- Forster, V.; Signorell, R.D.; Roveri, M.; Leroux, J.C. Liposome-supported peritoneal dialysis for detoxification of drugs and endogenous metabolites. Sci. Transl. Med. 2014, 6, 258ra141. [Google Scholar] [CrossRef]
- Ghannoum, M.; Roberts, D.M.; Hoffman, R.S.; Ouellet, G.; Roy, L.; Decker, B.S.; Bouchard, J. A stepwise approach for the management of poisoning with extracorporeal treatments. Semin. Dial. 2014, 27, 362–370. [Google Scholar] [CrossRef]
- Dean, L. Amitriptyline therapy and CYP2D6 and CYP2C19 genotype. In Medical Genetics Summaries [Internet]; Pratt, V., Scott, S., Pirmohamed, M., Esquivel, B., Kane, M., Kattman, B., Malheiro, A., Eds.; National Center for Biotechnology: Bethesda, MD, USA, 2017. Available online: https://www.ncbi.nlm.nih.gov/books/NBK425165/ (accessed on 30 January 2021).
- Agostoni, V.; Lee, S.H.; Forster, V.; Kabbaj, M.; Bosoi, C.R.; Tremblay, M.; Zadory, M.; Rose, C.F.; Leroux, J.-C. Liposome-Supported Peritoneal Dialysis for the Treatment of Hyperammonemia-Associated Encephalopathy. Adv. Funct. Mater. 2016, 26, 8382–8389. [Google Scholar] [CrossRef]
- Giacalone, G.; Matoori, S.; Agostoni, V.; Forster, V.; Kabbaj, M.; Eggenschwiler, S.; Lussi, M.; De Gottardi, A.; Zamboni, N.; Leroux, J.C. Liposome-supported peritoneal dialysis in the treatment of severe hyperammonemia: An investigation on potential interactions. J. Control. Release 2018, 278, 57–65. [Google Scholar] [CrossRef] [PubMed]
- Matoori, S.; Forster, V.; Agostoni, V.; Bettschart-Wolfensberger, R.; Bektas, R.N.; Thöny, B.; Häberle, J.; Leroux, J.C.; Kabbaj, M. Preclinical evaluation of liposome-supported peritoneal dialysis for the treatment of hyperammonemic crises. J. Control. Release Off. J. Control. Release Soc. 2020, 328, 503–513. [Google Scholar] [CrossRef] [PubMed]
- Shi, Y.; Wang, Y.; Ma, S.; Liu, T.; Tian, H.; Zhu, Q.; Wang, W.; Li, Y.; Ding, F. Increasing the removal of protein-bound uremic toxins by liposome-supported hemodialysis. Artif. Organs 2019, 43, 490–503. [Google Scholar] [CrossRef] [PubMed]
- Shi, Y.; Tian, H.; Wang, Y.; Shen, Y.; Zhu, Q.; Ding, F. Removal of Protein-Bound Uremic Toxins by Liposome-Supported Peritoneal Dialysis. Perit. Dial Int. 2019, 39, 509–518. [Google Scholar] [CrossRef] [PubMed]
- Shen, Y.; Shen, Y.; Bi, X.; Li, J.; Chen, Y.; Zhu, Q.; Wang, Y.; Ding, F. Linoleic acid-modified liposomes for the removal of protein-bound toxins: An in vitro study. Int. J. Artif. Organs 2020, 391398820968837. [Google Scholar] [CrossRef] [PubMed]
- Shen, Y.; Wang, Y.; Shi, Y.; Bi, X.; Xu, J.; Zhu, Q.; Ding, F. Improving the clearance of protein-bound uremic toxins using cationic liposomes as an adsorbent in dialysate. Colloids Surf. B Biointerfaces 2020, 186, 110725. [Google Scholar] [CrossRef] [PubMed]
- Shen, Y.; Wang, Y.; Shi, Y.; Tian, H.; Zhu, Q.; Ding, F. Development of liposome as a novel adsorbent for artificial liver support system in liver failure. J. Liposome Res. 2020, 30, 246–254. [Google Scholar] [CrossRef]
- Zhang, W.; Wang, G.; Falconer, J.R.; Baguley, B.C.; Shaw, J.P.; Liu, J.; Xu, H.; See, E.; Sun, J.; Aa, J.; et al. Strategies to maximize liposomal drug loading for a poorly water-soluble anticancer drug. Pharm. Res. 2015, 31, 1451–1461. [Google Scholar] [CrossRef]
- Chapman, R.; Harvey, M.; Davies, P.; Wu, Z.; Cave, G. Liposome supported peritoneal dialysis in rat amitriptyline exposure with and without intravenous lipid emulsion. J. Liposome Res. 2019, 29, 114–120. [Google Scholar] [CrossRef]
- Cave, G.; Harvey, M.; Pianca, N.; Robertson, I.; Sleigh, J.; Wu, Z. Intravenous DOPG liposomes do not augment pH gradient liposome supported peritoneal dialysis in treatment of acute intravenous amitriptyline intoxication in rats. Toxicol. Commun. 2018, 1, 113–120. [Google Scholar] [CrossRef]
- Pratsinis, A.; Zuercher, S.; Forster, V.; Fischer, E.J.; Luciani, P.; Leroux, J.C. Liposome-supported enzymatic peritoneal dialysis. Biomaterials 2017, 145, 128–137. [Google Scholar] [CrossRef] [PubMed]
- Pratsinis, A. Liposome-Supported Enzymatic Peritoneal Dialysis for Alcohol Detoxification. Ph.D. Thesis, ETH Zurich, Zurich, Switzerland, 2017. Available online: http://www.research-collection.ethz.ch (accessed on 30 January 2021).
- Kidney Health New Zealand: Renal Statistics. Available online: https://www.kidney.health.nz/Kidney-Disease/Facts-and-Figures (accessed on 30 January 2021).
- Versantis Products. Available online: https://www.versantis.ch/products.php (accessed on 30 January 2021).
| Authors | Experimental Model | Target Molecule | Liposome Type | Results: In Vitro | Results: In Vivo |
|---|---|---|---|---|---|
| Exogenous toxic substances | |||||
| Forster et al. (2014) | pH-gradient liposomes in vitro and LSPD in vivo (rat model) Pharmacodynamic endpoints also for verapamil in vivo (rat model) | Verapamil, Propranolol, Amitriptyline, Phenobarbital | Liposome with acidic core (except phenobarbital where core basic) Liposomes bind via ionisation of weak base/acid in liposome core to become lipid insoluble, thus entrapped | 90% of verapamil was sequestered in Liposomes within 8 h in presence of plasma proteins | Verapamil: >80-fold increased extraction of drug over a 12-h peritoneal dwell time versus conventional icodextrin dialysate control. † LSPD in a rat model of verapamil intoxication resulted in 3-fold reduction in time to blood pressure recovery. † Other drugs: LSPD in vivo showed increased extraction versus conventional dialysate: Phenobarbital 1.25-fold, haloperidol > 100-fold, propranolol > 100-fold. † |
| Chapman et al. (2019) | LSPD in vivo ± ILE (rat models) | Amitriptyline | Liposomes with acidic core | Nil | 12-fold increase in dialysate amitriptyline concentration with LSPD. † Hypothesis generating finding of estimated extraction ratio for amitriptyline from peritoneal blood flow for LSPD 30%—much greater than reported free fraction amitriptyline (5–10%) [13] |
| Cave et al. (2018) | LSPD in vivo ± IV DOPG liposomes (rat models) | Amitriptyline | Liposomes with acidic core for liposomes in peritoneal dialysate IV DOPG liposomes (DOPG: 1,2-dioleoyl-sn-glycero-3-phosphoglycerol) DOPG liposomes bind via electrostatic/lipophilic interaction in liposome membrane | Nil | DOPG liposomes increased blood amitriptyline concentrations by 50%. No corresponding increase in LSPD dialysate amitriptyline concentrations at the end of the dwell time; control median 430 nmol/L vs. IV DOPG 414 nmol/L. |
| Enzymatic liposome dialysis | |||||
| Pratsinis et al. (2017) | LSPD in vivo (rat models) | Ethanol | Enzyme-loaded Liposomes (containing ethanol metabolising enzymes) compared with free enzymes in dialysate | Nil | E-liposomes enhanced ethanol metabolism, as evidenced by increased ethanol metabolites in both plasma and dialysate. |
| Endogenous toxic substances | |||||
| Forster et al. (2014) | LSPD both in vitro and in vivo (rat model) | Ammonia | Liposomes with acidic core | Liposomes extracted 95% of ammonia added to an in vitro diffusion system in 8 hr. When serum was added to mimic physiological conditions, the uptake into liposomes exceeded the total ammonia added. | 20-fold increase in ammonia concentration in dialysate with a 3-hr. LSPD treatment in rats. † |
| Agostoni et al. (2016) | In vitro: study on effect of concentration of citrate in liposome on ammonia removal capacity. In vivo: LSPD in rat and pig models | Ammonia | Liposomes with acidic core Large liposomes, prepared by osmotic shock technique | Acidic core of liposome confirmed as an influx driver of ammonia to liposomes, proportional to concentration of citrate in liposome. | One week of LSPD in rat models of induced hepatic failure: 10-fold increase in dialysate ammonia, reduced plasma ammonia concentration and brain water concentration versus conventional peritoneal dialysis. † LSPD with liposomes from this experiment did not cause CARPA in pigs. |
| Giacalone et al. (2018) | In vitro: capacity of liposomes for ammonia uptake and drug interactions in human ascitic fluid was assessed; in vivo: LSPD to assess uptake of important metabolites in a rat model | Ammonia | Liposomes with acidic core | LSPD maintained its ammonia uptake when combined with ascitic fluid from liver disease patients, with limited interaction effects when combined with drugs commonly co-administered to this patient group, except the lipophilic weakly basic propranolol and fluoroquinolones | LSPD did not remove important metabolites more than conventional PD fluid |
| Matoori et al. (2020) | LSPD in vivo (minipig models) Experiment undertaken to ascertain safety of the model prior to first in human study | Ammonia | Liposomes with acidic core | Nil | Increased dialytic clearance of ammonia in ammonium chloride infusion with LSPD. † LSPD model in pigs demonstrated low plasma citrate (driver of liposome pH gradient) concentrations and, low DPPC absorption and no CARPA with daily doses for 10 days (safety endpoints). |
| Endogenous bound solutes | |||||
| Shi et al. (2019) | Liposomes both in vitro and an in vivo rat peritoneal dialysis model Albumin both in vitro and an in vivo rat periotneal dialysis model | p-cresyl sulphate (PCS), indoxyl sulphate (IS) and indole-3-acetic acid (3-IAA) | Soy phospholipid liposomes Mechanism of binding electrostatic/lipophilic interaction in liposome membrane | Adding liposomes or albumin to dialysate markedly increased removal of PCS and IS. Albumin Markedly increased removal of 3-IAA. | Both LSPD and albumin resulted in higher concentrations of intraperitoneal PBUTs. † |
| Shi et al. (2019) | Liposome-supported HD both in vitro and in vivo (rat models) | PCS, IS and Hippuric acid (HA) | Soy phospholipid liposomes | Percentage removal of both PCS and IS, but not HA, increased as the liposome dose increased in a dose-response relationship. Adding liposomes to dialysate markedly increased removal of PBUTs without significantly altering urea and creatinine clearance | Adding liposomes resulted in higher reduction ratios and more total solute removal for several PBUTs when compared to conventional dialysate. † |
| Shen et al. (2020) | In vitro—rapid equilibrium dialysis (RED) device. | PCS and IS | Cationic liposomes (modified) vs. SP liposomes Cationic liposome exhibit increased electrostatic attraction in membrane | Cationic showed higher binding rate with IS (1.24–1.38 fold higher) and PCS (1.07–1.09 fold higher) compared with plain liposomes. Cationic liposome-supported dialysis had a better clearing efficiency for PCS and IS when compared with conventional dialysate and with dialysate containing bovine serum albumin. | Nil |
| Shen et al. (2020) | Liposome-supported haemodialysis both in vitro and in vivo (rat model) | Unconjugated bilirubin and bile salts | Soy phospholipid liposomes | Unconjugated bilirubin (52.83%–99.87%) and bile salts (50.54%–94.75%) were bound by liposomes in a dose–response relationship. Concentrations of both were significantly decreased in the liposome dialysis group vs. phosphate buffered saline group. | Liposome-containing dialysate resulted in a significantly higher reduction ratio in total bilirubin (6.56% ± 5.72% vs. −1.86% ± 5.99%, p < 0.05) and more total bile acids (7.63 ± 5.27 μmol vs. 2.13 ± 2.32 μmol, p < 0.05) extracted compared with conventional dialysate. † |
| Shen et al. (2020) | In vitro dialysis (Ultrafiltration column) | representative PBUTs and liver failure-related solutes | Linoleic acid-modified liposomes (LA-liposomes) Linoleic acid acts as displacer of target molecule from albumin to increase free fraction available | LA-liposomes exhibited binding to PBUTs, bilirubin and bile acids. Dialysate containing LA-liposomes showed higher reduction rates of these compounds compared with traditional dialysate and when compared with dialysate containing plain liposomes. Additionally, adding LA resulted in the significant inhibition of albumin binding PBUTs, so removal efficiency of PBUTs was greatly enhanced with LA as a competitive displacer. | Nil |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Hart, K.; Harvey, M.; Tang, M.; Wu, Z.; Cave, G. Liposomes to Augment Dialysis in Preclinical Models: A Structured Review. Pharmaceutics 2021, 13, 395. https://doi.org/10.3390/pharmaceutics13030395
Hart K, Harvey M, Tang M, Wu Z, Cave G. Liposomes to Augment Dialysis in Preclinical Models: A Structured Review. Pharmaceutics. 2021; 13(3):395. https://doi.org/10.3390/pharmaceutics13030395
Chicago/Turabian StyleHart, Kevin, Martyn Harvey, Mingtan Tang, Zimei Wu, and Grant Cave. 2021. "Liposomes to Augment Dialysis in Preclinical Models: A Structured Review" Pharmaceutics 13, no. 3: 395. https://doi.org/10.3390/pharmaceutics13030395
APA StyleHart, K., Harvey, M., Tang, M., Wu, Z., & Cave, G. (2021). Liposomes to Augment Dialysis in Preclinical Models: A Structured Review. Pharmaceutics, 13(3), 395. https://doi.org/10.3390/pharmaceutics13030395







