A Screening Study for the Development of Simvastatin-Doxorubicin Liposomes, a Co-Formulation with Future Perspectives in Colon Cancer Therapy
Abstract
:1. Introduction
2. Materials and Methods
2.1. Materials
2.2. Methods
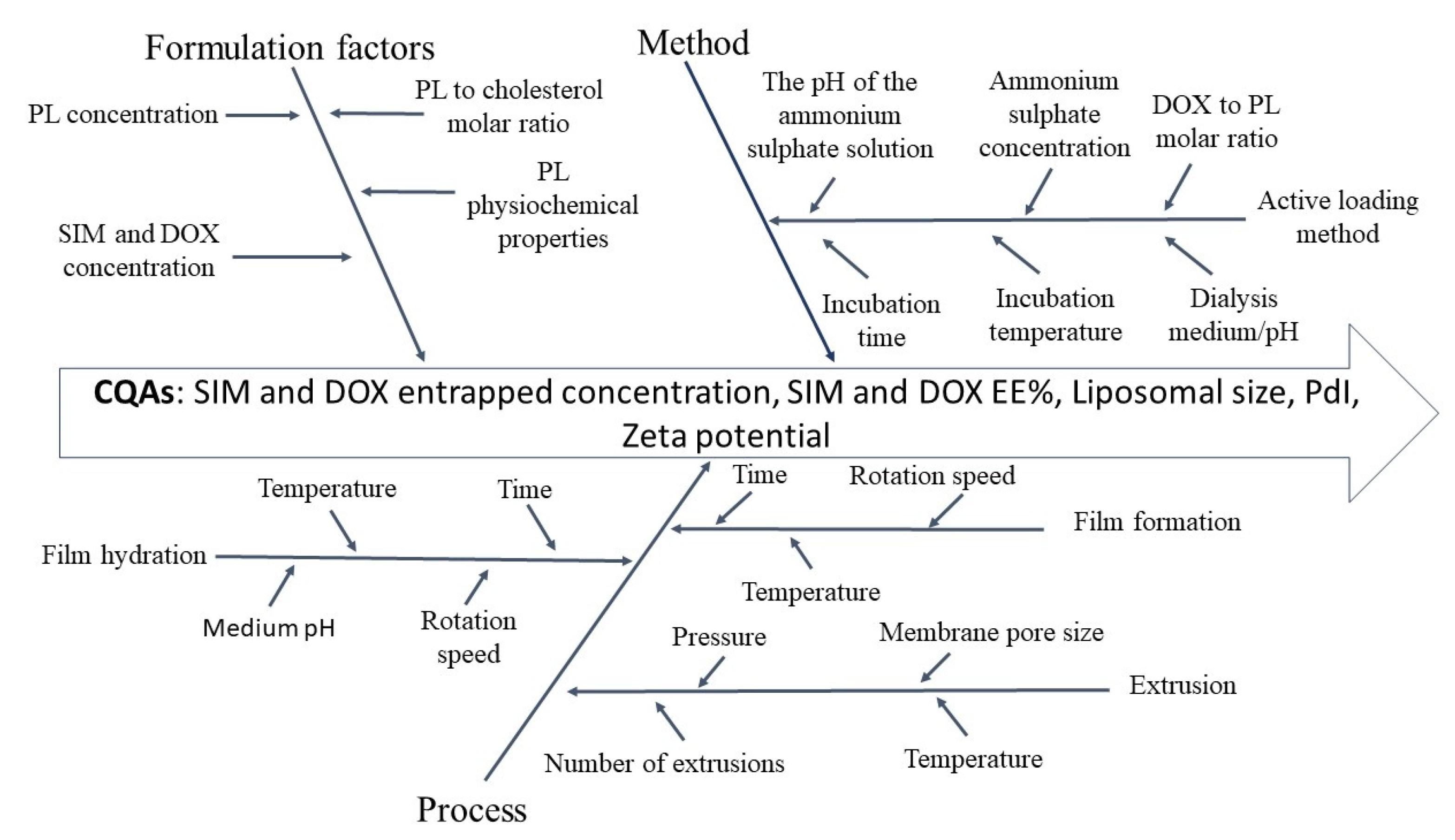
2.2.1. Implementation of the QbD Concept
2.2.2. Liposomes Preparation
2.2.3. Characterization of Liposomes
Determination of SIM and DOX Entrapped Concentration
Determination of Liposomal Size and PdI
Determination of Liposomal Morphology using Transmission Electron Microscopy (TEM) Analysis
In Vitro Release Study
2.2.4. Cell Co-Culture
2.2.5. Cell Proliferation Assay
3. Results and Discussions
3.1. Setting the QTPP and the CQAs
3.2. Risk Analysis
3.3. DoE
3.4. DoE Analysis
3.4.1. The Influence of the Formulation Factors on Drug Entrapped Concentration
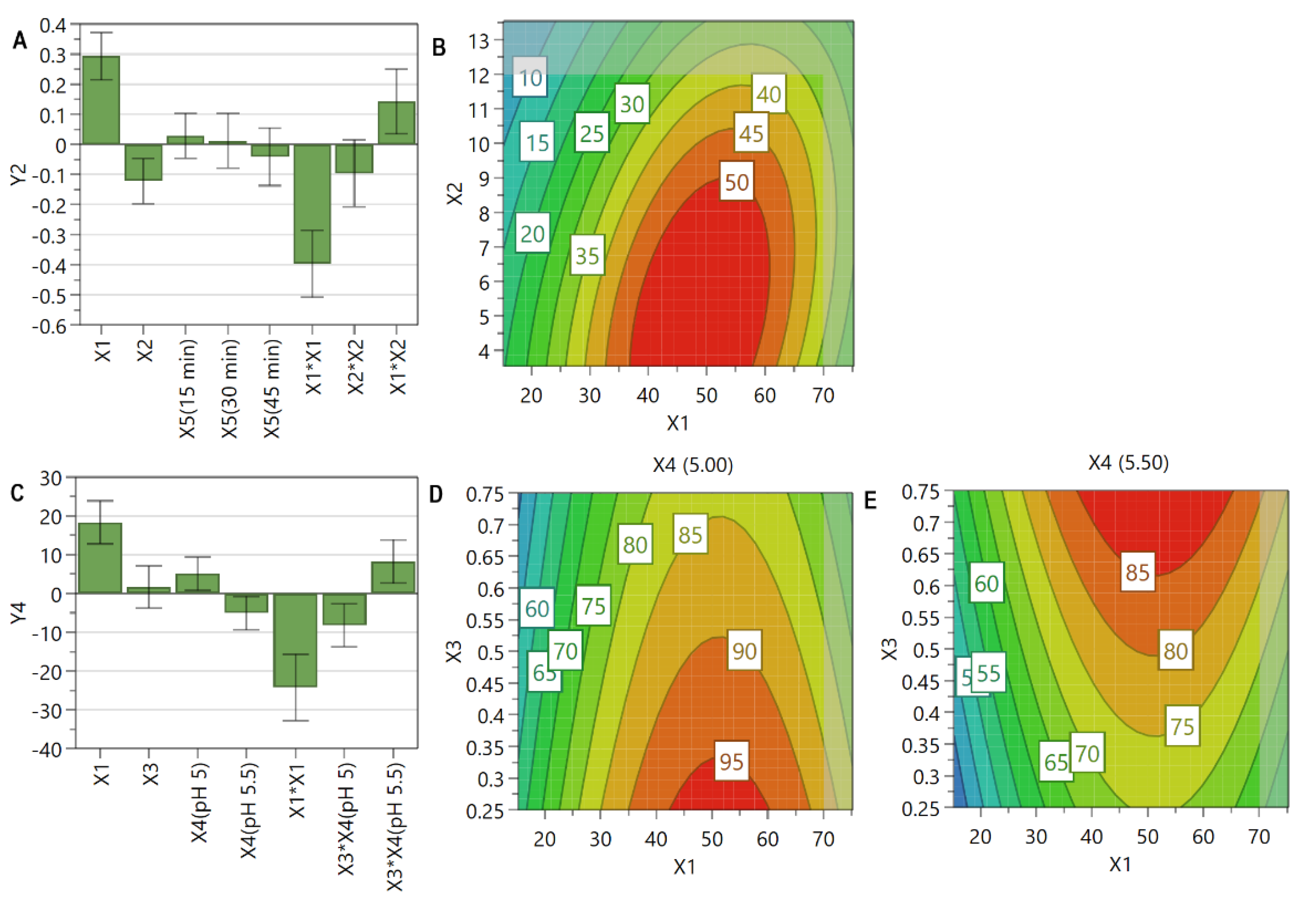
3.4.2. The Influence of the Formulation Factors on EE%
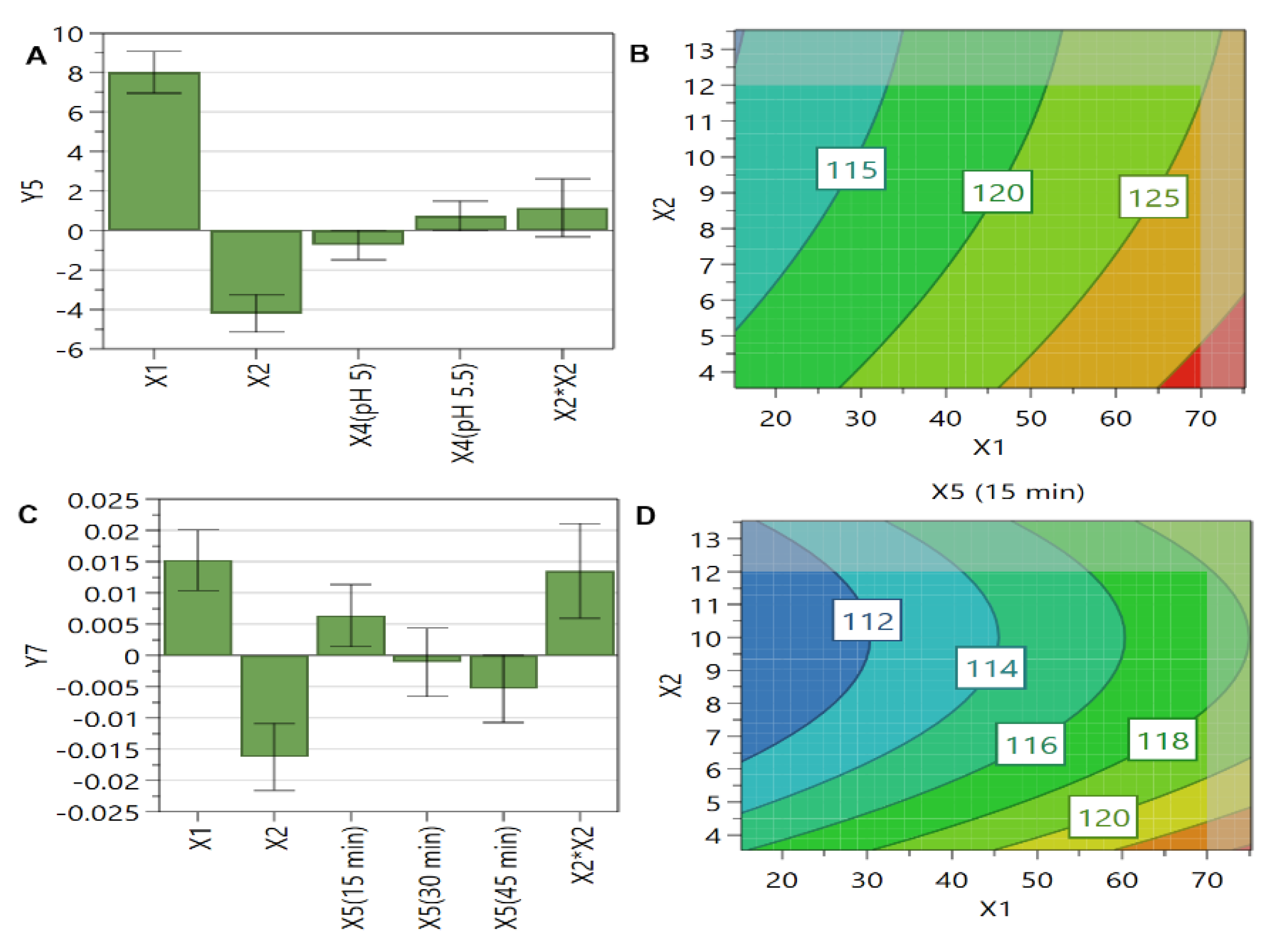
3.4.3. The Influence of the Formulation Factors on Liposomal Size
3.4.4. The Influence of the Formulation Factors on PdI
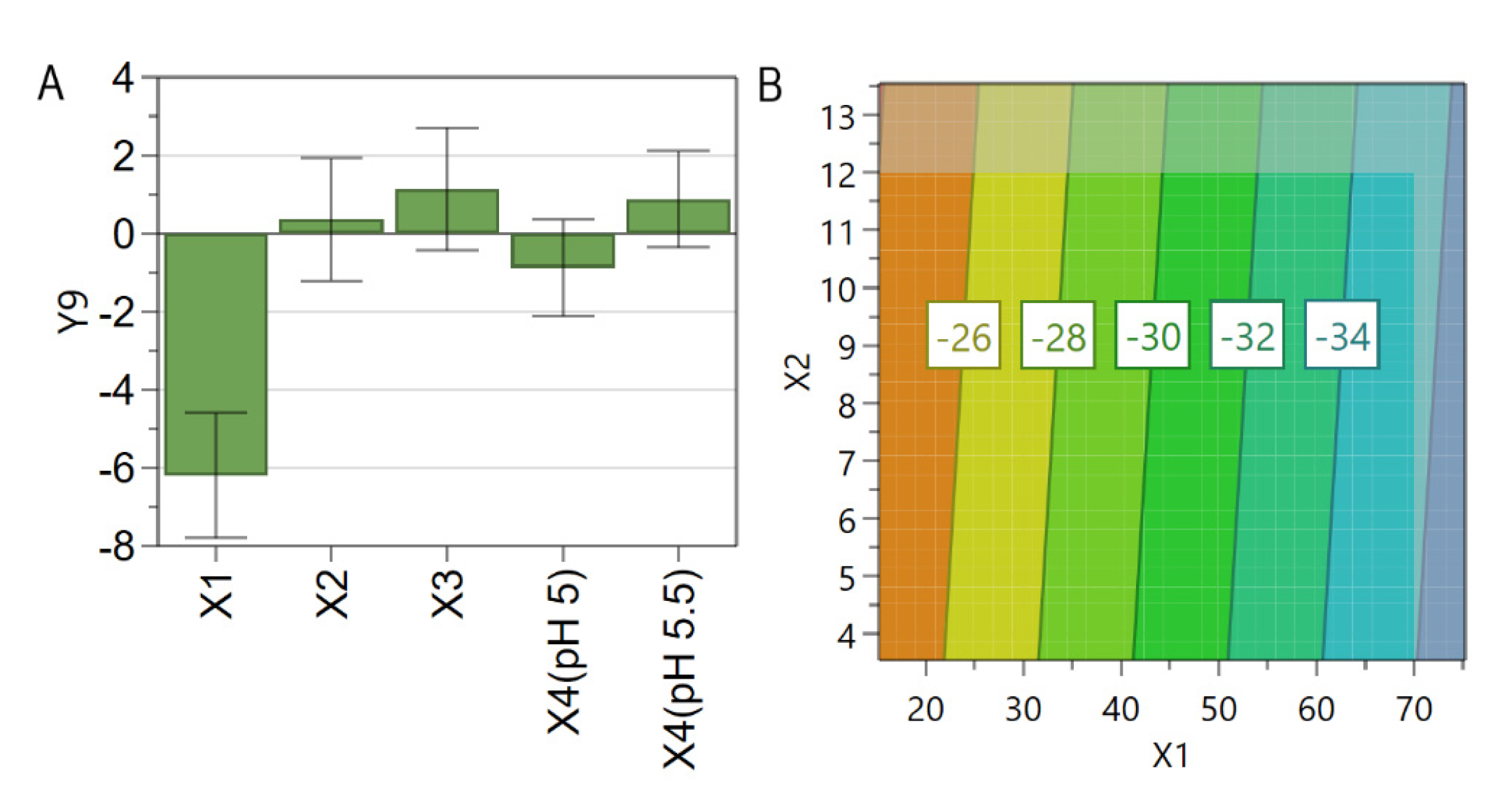
3.4.5. The Influence of the Formulation Factors on Zeta Potential
3.5. TEM Analysis
3.6. In Vitro Release Study
3.7. The Effects of SIM and DOX on the Proliferation of C26 Murine Colon Carcinoma Cells Co-Cultured with Murine Macrophages
4. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Data Availability Statement
Conflicts of Interest
References
- WHO. WHO|Cancer. Available online: https://www.who.int/news-room/fact-sheets/detail/cancer (accessed on 21 February 2021).
- Hatcher, O.; Kumar, A.A. Chemotherapy and radiotherapy for colorectal cancers. Surgery 2014, 32, 179–184. [Google Scholar] [CrossRef]
- Maranhão, R.C.; Vital, C.G.; Tavoni, T.M.; Graziani, S.R. Clinical experience with drug delivery systems as tools to decrease the toxicity of anticancer chemotherapeutic agents. Expert Opin. Drug Deliv. 2017, 14, 1217–1226. [Google Scholar] [CrossRef] [PubMed]
- Capelôa, T.; Benyahia, Z.; Zampieri, L.X.; Blackman, M.C.; Sonveaux, P. Metabolic and non-metabolic pathways that control cancer resistance to anthracyclines. Semin. Cell Dev. Biol. 2019, 98, 181–191. [Google Scholar] [CrossRef] [PubMed]
- Vahed, S.Z.; Salehi, R.; Davaran, S.; Sharifi, S. Liposome-based drug co-delivery systems in cancer cells. Mater. Sci. Eng. C 2017, 71, 1327–1341. [Google Scholar] [CrossRef] [PubMed]
- Argilés, G.; Tabernero, J.; Labianca, R.; Hochhauser, D.; Salazar, R.; Iveson, T.; Laurent-Puig, P.; Quirke, P.; Yoshino, T.; Taieb, J.; et al. Localised colon cancer: ESMO Clinical Practice Guidelines for diagnosis, treatment and follow-up. Ann. Oncol. 2020, 31, 1291–1305. [Google Scholar] [CrossRef] [PubMed]
- Catarina, A.; Nuno, J.; Simões, S. Combination Chemotherapy in Cancer: Principles, Evaluation and Drug Delivery Strategies; IntechOpen: London, UK, 2011. [Google Scholar] [CrossRef] [Green Version]
- Mayer, L.D.; Tardi, P.; Louie, A.C. CPX-351: A nanoscale liposomal co-formulation of daunorubicin and cytarabine with unique biodistribution and tumor cell uptake properties. Int. J. Nanomed. 2019, 14, 3819–3830. [Google Scholar] [CrossRef] [Green Version]
- Gonçalves, M.; Mignani, S.; Rodrigues, J.; Tomás, H. A glance over doxorubicin based-nanotherapeutics: From proof-of-concept studies to solutions in the market. J. Control. Release 2019, 317, 347–374. [Google Scholar] [CrossRef] [PubMed]
- Cagel, M.; Grotz, E.; Bernabeu, E.; Moretton, M.A.; Chiappetta, D.A. Doxorubicin: Nanotechnological overviews from bench to bedside. Drug Discov. Today 2017, 22, 270–281. [Google Scholar] [CrossRef]
- Gabizon, A.A.; Patil, Y.; La-Beck, N.M. New insights and evolving role of pegylated liposomal doxorubicin in cancer therapy. Drug Resist. Updat. 2016, 29, 90–106. [Google Scholar] [CrossRef]
- Pugazhendhi, A.; Edison, T.N.J.I.; Velmurugan, B.K.; Jacob, J.A.; Karuppusamy, I. Toxicity of Doxorubicin (Dox) to different experimental organ systems. Life Sci. 2018, 200, 26–30. [Google Scholar] [CrossRef]
- Barenholz, Y. Doxil®—The first FDA-approved nano-drug: Lessons learned. J. Control. Release 2012, 160, 117–134. [Google Scholar] [CrossRef] [PubMed]
- Phase 2 Study of Thermodox as Adjuvant Therapy With Thermal Ablation (RFA) in Treatment of Metastatic Colorectal Can-cer(mCRC) (ABLATE). Available online: https://clinicaltrials.gov/ct2/show/NCT01464593?term=doxorubicin&cond=Colorectal+Cancer&draw=2&rank=1 (accessed on 26 August 2021).
- Effects of STM 434 Alone or in Combination with Liposomal Doxorubicin in Patients with Ovarian Cancer or Other Advanced Solid Tumors. Available online: https://clinicaltrials.gov/ct2/show/NCT02262455?term=doxorubicin&cond=Colorectal+Cancer&draw=3&rank=11 (accessed on 26 August 2021).
- PIPAC for the Treatment of Peritoneal Carcinomatosis in Patients With Ovarian, Uterine, Appendiceal, Colorectal, or Gastric Cancer. Available online: https://clinicaltrials.gov/ct2/show/NCT04329494?term=doxorubicin&cond=Colorectal+Cancer&draw=6&rank=4 (accessed on 26 August 2021).
- Motexafin Gadolinium and Doxorubicin in Treating Patients with Advanced Cancer. Available online: https://clinicaltrials.gov/ct2/show/NCT00036790?term=doxorubicin&cond=Colorectal+Cancer&draw=2&rank=5 (accessed on 26 August 2021).
- Combination Chemotherapy with or without Chemoembolization in Treating Patients with Colorectal Cancer Metastatic to the Liver (6655). Available online: https://clinicaltrials.gov/ct2/show/NCT00023868?term=doxorubicin&cond=Colorectal+Cancer&draw=2&rank=7 (accessed on 26 August 2021).
- Xiong, Y.; Wang, Y.; Tiruthani, K. Tumor immune microenvironment and nano-immunotherapeutics in colorectal cancer. Nanomed. Nanotechnol. Biol. Med. 2019, 21, 102034. [Google Scholar] [CrossRef] [PubMed]
- Li, N.; Xie, X.; Hu, Y.; He, H.; Fu, X.; Fang, T.; Li, C. Herceptin-conjugated liposomes co-loaded with doxorubicin and simvastatin in targeted prostate cancer therapy. Am. J. Transl. Res. 2019, 11, 1255–1269. [Google Scholar]
- Sadeghi-Abandansari, H.; Pakian, S.; Nabid, M.-R.; Ebrahimi, M.; Rezalotfi, A. Local co-delivery of 5-fluorouracil and curcumin using Schiff’s base cross-linked injectable hydrogels for colorectal cancer combination therapy. Eur. Polym. J. 2021, 157, 110646. [Google Scholar] [CrossRef]
- Psurski, M.; Filip-Psurska, B.; Cuprych, M.; Wietrzyk, J.; Oleksyszyn, J. 3,4-dimethoxybenzyl isothiocyanate enhances doxorubicin efficacy in LoVoDX doxorubicin-resistant colon cancer and attenuates its toxicity in vivo. Life Sci. 2019, 231, 116530. [Google Scholar] [CrossRef]
- Mohammadkhani, N.; Gharbi, S.; Rajani, H.; Farzaneh, A.; Mahjoob, G.; Hoseinsalari, A.; Korsching, E. Statins: Complex outcomes but increasingly helpful treatment options for patients. Eur. J. Pharmacol. 2019, 863, 172704. [Google Scholar] [CrossRef] [PubMed]
- Murtola, T.J.; Visvanathan, K.; Artama, M.; Vainio, H.; Kala, V. Statin Use and Breast Cancer Survival: A Nationwide Cohort Study from Finland. PLoS ONE 2014, 9, e110231. [Google Scholar] [CrossRef] [Green Version]
- Kim, J.; Choi, E.-A.; Han, Y.-E.; Lee, J.-W.; Kim, Y.-S.; Kim, Y.; You, H.-S.; Hyun, H.-J.; Kang, H.-T. Association between statin use and all-cause mortality in cancer survivors, based on the Korean health insurance service between 2002 and 2015. Nutr. Metab. Cardiovasc. Dis. 2019, 30, 434–440. [Google Scholar] [CrossRef]
- Abdel-Qadir, H.; Bobrowski, D.; Zhou, L.; Austin, P.C.; Calvillo-Argüelles, O.; Amir, E.; Lee, D.S.; Thavendiranathan, P. Statin Exposure and Risk of Heart Failure After Anthracycline- or Trastuzumab-Based Chemotherapy for Early Breast Cancer: A Propensity Score‒Matched Cohort Study. J. Am. Heart Assoc. 2021, 10, e018393. [Google Scholar] [CrossRef]
- Henslee, A.B.; Steele, T.A. Combination statin and chemotherapy inhibits proliferation and cytotoxicity of an aggressive natural killer cell leukemia. Biomark. Res. 2018, 6, 1–11. [Google Scholar] [CrossRef]
- Anderson, C.C.; Khatri, M.; Roede, J.R. Time-dependent simvastatin administration enhances doxorubicin toxicity in neuroblastoma. Toxicol. Rep. 2020, 7, 520–528. [Google Scholar] [CrossRef] [PubMed]
- Buranrat, B.; Suwannaloet, W.; Naowaboot, J. Simvastatin potentiates doxorubicin activity against MCF-7 breast cancer cells. Oncol. Lett. 2017, 14, 6243–6250. [Google Scholar] [CrossRef]
- Tefas, L.R.; Sylvester, B.; Tomuta, I.; Sesarman, A.; Licarete, E.; Banciu, M.; Porfire, A. Development of antiproliferative long-circulating liposomes co-encapsulating doxorubicin and curcumin, through the use of a quality-by-design approach. Drug Des. Dev. Ther. 2017, 11, 1605–1621. [Google Scholar] [CrossRef] [Green Version]
- Gkionis, L.; Campbell, R.A.; Aojula, H.; Harris, L.K.; Tirella, A. Manufacturing drug co-loaded liposomal formulations targeting breast cancer: Influence of preparative method on liposomes characteristics and in vitro toxicity. Int. J. Pharm. 2020, 590, 119926. [Google Scholar] [CrossRef] [PubMed]
- Shaikh, I.M.; Tan, K.B.; Chaudhury, A.; Liu, Y.; Tan, B.-J.; Tan, B.M.; Chiu, G.N. Liposome co-encapsulation of synergistic combination of irinotecan and doxorubicin for the treatment of intraperitoneally grown ovarian tumor xenograft. J. Control. Release 2013, 172, 852–861. [Google Scholar] [CrossRef]
- Haran, G.; Cohen, R.; Bar, L.K.; Barenholz, Y. Transmembrane ammonium sulfate gradients in liposomes produce efficient and stable entrapment of amphipathic weak bases. Biochim. et Biophys. Acta (BBA)—Biomembr. 1993, 1151, 201–215. [Google Scholar] [CrossRef]
- Zucker, D.; Marcus, D.; Barenholz, Y.; Goldblum, A. Liposome drugs’ loading efficiency: A working model based on loading conditions and drug’s physicochemical properties. J. Control. Release 2009, 139, 73–80. [Google Scholar] [CrossRef] [PubMed]
- Sun, J.; Song, Y.; Lu, M.; Lin, X.; Liu, Y.; Zhou, S.; Su, Y.; Deng, Y. Evaluation of the antitumor effect of dexamethasone palmitate and doxorubicin co-loaded liposomes modified with a sialic acid–octadecylamine conjugate. Eur. J. Pharm. Sci. 2016, 93, 177–183. [Google Scholar] [CrossRef]
- Wang, T.; Jiang, Y.; Chu, H.; Liu, X.; Dai, Y.; Wang, D. Doxorubicin and Lovastatin co-delivery liposomes for synergistic therapy of liver cancer. J. Drug Deliv. Sci. Technol. 2019, 52, 452–459. [Google Scholar] [CrossRef]
- The International Council for Harmonisation of Technical Requirements for Pharmaceuticals for Human Use (ICH). ICH Harmonised Tripartite Guideline, Pharmaceutical Development Q8(R2). Available online: https://database.ich.org/sites/default/files/Q8%28R2%29%20Guideline.pdf (accessed on 10 February 2021).
- Grangeia, H.B.; Silva, C.; Simões, S.P.; Reis, M.S. Quality by design in pharmaceutical manufacturing: A systematic review of current status, challenges and future perspectives. Eur. J. Pharm. Biopharm. 2019, 147, 19–37. [Google Scholar] [CrossRef] [PubMed]
- U.S. Department of Health and Human Services Food and Drug Administration Center for Drug Evaluation and Research. Guidance for Industry: Liposome Drug Products: Chemistry, Manufacturing, and Controls; Human Pharmacokinetics and Bioavailability; and Labeling Documentation. Available online: https://www.fda.gov/media/70837/download (accessed on 1 March 2021).
- Farzaneh, H.; Nik, M.E.; Mashreghi, M.; Saberi, Z.; Jaafari, M.R.; Teymouri, M. A study on the role of cholesterol and phosphatidylcholine in various features of liposomal doxorubicin: From liposomal preparation to therapy. Int. J. Pharm. 2018, 551, 300–308. [Google Scholar] [CrossRef]
- Chen, Y.; Cheng, Y.; Zhao, P.; Zhang, S.; Li, M.; He, C.; Zhang, X.; Yang, T.; Yan, R.; Ye, P.; et al. Co-delivery of doxorubicin and imatinib by pH sensitive cleavable PEGylated nanoliposomes with folate-mediated targeting to overcome multidrug resistance. Int. J. Pharm. 2018, 542, 266–279. [Google Scholar] [CrossRef]
- Dash, T.K.; Konkimalla, V.B. Formulation and Optimization of Doxorubicin and Biochanin A Combinational Liposomes for Reversal of Chemoresistance. AAPS PharmSciTech. 2016, 18, 1116–1124. [Google Scholar] [CrossRef]
- Porfire, A.; Tomuta, I.; Muntean, D.; Luca, L.; Licarete, E.; Alupei, M.C.; Achim, M.; Vlase, L.; Banciu, M. Optimizing long-circulating liposomes for delivery of simvastatin to C26 colon carcinoma cells. J. Liposome Res. 2014, 25, 1–9. [Google Scholar] [CrossRef]
- Nam, J.H.; Kim, S.-Y.; Seong, H. Investigation on Physicochemical Characteristics of a Nanoliposome-Based System for Dual Drug Delivery. Nanoscale Res. Lett. 2018, 13, 101. [Google Scholar] [CrossRef] [PubMed]
- Știufiuc, G.F.; Nițică, Ș.; Toma, V.; Iacoviță, C.; Zahn, D.; Tetean, R.; Burzo, E.; Lucaciu, C.M.; Știufiuc, R.I. Synergistical Use of Electrostatic and Hydrophobic Interactions for the Synthesis of a New Class of Multifunctional Nanohybrids: Plasmonic Magneto-Liposomes. Nanomaterials 2019, 9, 1623. [Google Scholar] [CrossRef] [Green Version]
- Stiufiuc, R.; Iacovita, C.; Stiufiuc, G.; Florea, A.; Achim, M.; Lucaciu, C.M. A new class of pegylated plasmonic liposomes: Synthesis and characterization. J. Colloid Interface Sci. 2015, 437, 17–23. [Google Scholar] [CrossRef] [PubMed]
- Ali, H.; Shirode, A.B.; Sylvester, P.W.; Nazzal, S. Preparation, characterization, and anticancer effects of simvastatin–tocotrienol lipid nanoparticles. Int. J. Pharm. 2010, 389, 223–231. [Google Scholar] [CrossRef] [PubMed]
- Zhang, Y.; Huo, M.; Zhou, J.; Zou, A.; Li, W.; Yao, C.; Xie, S. DDSolver: An Add-In Program for Modeling and Comparison of Drug Dissolution Profiles. AAPS J. 2010, 12, 263–271. [Google Scholar] [CrossRef] [Green Version]
- Zhang, X.; Goncalves, R.; Mosser, D.M. The Isolation and Characterization of Murine Macrophages. Curr. Protoc. Immunol. 2008, 83, 14.1.1–14.1.14. [Google Scholar] [CrossRef]
- Herbeuval, J.-P.; Lelievre, E.; Lambert, C.; Dy, M.; Genin, C. Recruitment of STAT3 for Production of IL-10 by Colon Carcinoma Cells Induced by Macrophage-Derived IL-6. J. Immunol. 2004, 172, 4630–4636. [Google Scholar] [CrossRef] [Green Version]
- Luput, L.; Licarete, E.; Sesarman, A.; Patras, L.; Alupei, M.C.; Banciu, M. Tumor-associated macrophages favor C26 murine colon carcinoma cell proliferation in an oxidative stress-dependent manner. Oncol. Rep. 2017, 37, 2472–2480. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Cell Proliferation ELISA, BrdU (Colorimetric). Available online: https://www.sigmaaldrich.com/deepweb/assets/sigmaaldrich/product/documents/229/033/11647229001bul.pdf (accessed on 10 July 2021).
- Eloy, J.O.; de Souza, M.C.; Petrilli, R.; Barcellos, J.P.A.; Lee, R.J.; Marchetti, J.M. Liposomes as carriers of hydrophilic small molecule drugs: Strategies to enhance encapsulation and delivery. Colloids Surf. B Biointerfaces 2014, 123, 345–363. [Google Scholar] [CrossRef]
- Li, J.; Wang, X.; Zhang, T.; Wang, C.; Huang, Z.; Luo, X.; Deng, Y. A review on phospholipids and their main applications in drug delivery systems. Asian. J. Pharm. Sci. 2015, 10, 81–98. [Google Scholar] [CrossRef]
- Lee, M.-K. Clinical usefulness of liposomal formulations in cancer therapy: Lessons from the experiences of doxorubicin. J. Pharm. Investig. 2018, 49, 203–214. [Google Scholar] [CrossRef]
- Fatima, M.T.; Islam, Z.; Ahmad, E.; Barreto, G.E.; Ashraf, G.M. Ionic gradient liposomes: Recent advances in the stable entrapment and prolonged released of local anesthetics and anticancer drugs. Biomed. Pharmacother. 2018, 107, 34–43. [Google Scholar] [CrossRef]
- Tazina, E.V.; Kostin, K.V.; Oborotova, N. Specific features of drug encapsulation in liposomes (A review). Pharm. Chem. J. 2011, 45, 481–490. [Google Scholar] [CrossRef]
- Takahashi, N.; Higashi, K.; Ueda, K.; Yamamoto, K.; Moribe, K. Determination of Nonspherical Morphology of Doxorubicin-Loaded Liposomes by Atomic Force Microscopy. J. Pharm. Sci. 2018, 107, 717–726. [Google Scholar] [CrossRef] [PubMed]
- Abraham, S.A.; Waterhouse, D.N.; Mayer, L.D.; Cullis, P.R.; Madden, T.D.; Bally, M.B. The Liposomal Formulation of Doxorubicin. Methods Enzymol. 2005, 391, 71–97. [Google Scholar] [CrossRef] [PubMed]
- Bolotin, E.M.; Cohen, R.; Bar, L.K.; Emanuel, N.; Ninio, S.; Barenholz, Y.; Lasic, D.D. Ammonium Sulfate Gradients for Efficient and Stable Remote Loading of Amphipathic Weak Bases into Liposomes and Ligandoliposomes. J. Liposome Res. 1994, 4, 455–479. [Google Scholar] [CrossRef]
- Chibowski, E.; Szcześ, A. Zeta potential and surface charge of DPPC and DOPC liposomes in the presence of PLC enzyme. Adsorption 2016, 22, 755–765. [Google Scholar] [CrossRef] [Green Version]
- Gubernator, J. Active methods of drug loading into liposomes: Recent strategies for stable drug entrapment and increasedin vivoactivity. Expert Opin. Drug Deliv. 2011, 8, 565–580. [Google Scholar] [CrossRef] [PubMed]
- Bozzuto, G.; Molinari, A. Liposomes as nanomedical devices. Int. J. Nanomed. 2015, 10, 975–999. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Er, Y.; Barnes, T.; Fornasiero, D.; Prestidge, C.A. The encapsulation and release of guanosine from PEGylated liposomes. J. Liposome Res. 2009, 19, 29–36. [Google Scholar] [CrossRef]
- Honary, S.; Zahir, F. Effect of Zeta Potential on the Properties of Nano-Drug Delivery Systems—A Review (Part 2). Trop. J. Pharm. Res. 2013, 12, 265–273. [Google Scholar] [CrossRef]
- Honary, S.; Zahir, F. Effect of Zeta Potential on the Properties of Nano-Drug Delivery Systems—A Review (Part 1). Trop. J. Pharm. Res. 2013, 12, 255–264. [Google Scholar] [CrossRef]
- Li, T.; Clulow, A.J.; Nowell, C.J.; Hawley, A.; Cipolla, D.; Rades, T.; Boyd, B.J. Controlling the size and shape of liposomal ciprofloxacin nanocrystals by varying the lipid bilayer composition and drug to lipid ratio. J. Colloid Interface Sci. 2019, 555, 361–372. [Google Scholar] [CrossRef] [PubMed]
- Shah, S.; Dhawan, V.; Holm, R.; Nagarsenker, M.S.; Perrie, Y. Liposomes: Advancements and innovation in the manufacturing process. Adv. Drug Deliv. Rev. 2020, 154-155, 102–122. [Google Scholar] [CrossRef]
- Ong, S.G.M.; Chitneni, M.; Lee, K.S.; Ming, L.C.; Yuen, K.H. Evaluation of Extrusion Technique for Nanosizing Liposomes. Pharmaceutics 2016, 8, 36. [Google Scholar] [CrossRef]
- Bhandary, S.; Basu, R.; Das, S.; Nandy, P. Effect of some statin group of drugs on the phase profile of liposomal membrane—a fluorescence anisotropy study. Phase Transit. 2009, 82, 821–830. [Google Scholar] [CrossRef]
- Jousma, H.; Talsma, H.; Spies, F.; Joosten, J.G.H.; Junginger, H.E.; Crommelin, D.J.A. Characterization of liposomes. The in-fluence of extrusion of multilamellar vesicles through polycarbonate membranes on particle size, particle size distribution and number of bilayers. Int. J. Pharm. 1987, 35, 263–274. [Google Scholar] [CrossRef]
- Johnston, M.J.W.; Edwards, K.; Karlsson, G.; Cullis, P.R. Influence of Drug-to-Lipid Ratio on Drug Release Properties and Liposome Integrity in Liposomal Doxorubicin Formulations. J. Liposome Res. 2008, 18, 145–157. [Google Scholar] [CrossRef]
- Alves, A.C.; Magarkar, A.; Horta, M.; Lima, J.L.F.C.; Bunker, A.; Nunes, C.; Reis, S. Influence of doxorubicin on model cell membrane properties: Insights from in vitro and in silico studies. Sci. Rep. 2017, 7, 6343. [Google Scholar] [CrossRef] [Green Version]
- Sułkowski, W.; Pentak, D.; Nowak, K.; Sułkowska, A. The influence of temperature, cholesterol content and pH on liposome stability. J. Mol. Struct. 2005, 744-747, 737–747. [Google Scholar] [CrossRef]
- Sariişik, E.; Koçak, M.; Baloglu, F.K.; Severcan, F. Interaction of the cholesterol reducing agent simvastatin with zwitterionic DPPC and charged DPPG phospholipid membranes. Biochim. et Biophys. Acta (BBA)—Biomembr. 2019, 1861, 810–818. [Google Scholar] [CrossRef]
- Xu, X.; Khan, M.; Burgess, D.J. A quality by design (QbD) case study on liposomes containing hydrophilic API: I. Formulation, processing design and risk assessment. Int. J. Pharm. 2011, 419, 52–59. [Google Scholar] [CrossRef] [PubMed]
- Kotouček, J.; Hubatka, F.; Mašek, J.; Kulich, P.; Velínská, K.; Bezděková, J.; Fojtíková, M.; Bartheldyová, E.; Tomečková, A.; Stráská, J.; et al. Preparation of nanoliposomes by microfluidic mixing in herring-bone channel and the role of membrane fluidity in liposomes formation. Sci. Rep. 2020, 10, 1–11. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Doskocz, J.; Dałek, P.; Przybyło, M.; Trzebicka, B.; Foryś, A.; Kobyliukh, A.; Iglic, A.; Langner, M. The Elucidation of the Mo-lecular Mechanism of the Extrusion Process. Materials 2021, 14, 4278. [Google Scholar] [CrossRef] [PubMed]
- Wiącek, A.E. Effect of ionic strength on electrokinetic properties of oil/water emulsions with dipalmitoylphosphatidylcholine. Colloids Surfaces A Physicochem. Eng. Asp. 2007, 302, 141–149. [Google Scholar] [CrossRef]
- Otto, F.; Brezesinski, G.; van Hoogevest, P.; Neubert, R. Physicochemical characterization of natural phospholipid excipients with varying PC content. Colloids Surfaces A Physicochem. Eng. Asp. 2018, 558, 291–296. [Google Scholar] [CrossRef]
- Ruiz, A.; Ma, G.; Seitsonen, J.; Pereira, S.G.; Ruokolainen, J.; Al-Jamal, W.T. Encapsulated doxorubicin crystals influence lysolipid temperature-sensitive liposomes release and therapeutic efficacy in vitro and in vivo. J. Control. Release 2020, 328, 665–678. [Google Scholar] [CrossRef]
- Murtaza, G. Solubility enhancement of simvastatin: A review. Acta Pol. Pharm.—Drug Res. 2012, 69, 581–590. [Google Scholar]
- Wu, D.C.; Ofner, C.M. Adsorption and Degradation of Doxorubicin from Aqueous Solution in Polypropylene Containers. AAPS PharmSciTech. 2012, 14, 74–77. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Li, T.; Cipolla, D.; Rades, T.; Boyd, B.J. Drug nanocrystallisation within liposomes. J. Control. Release 2018, 288, 96–110. [Google Scholar] [CrossRef] [PubMed]
- Zhigaltsev, I.V.; Maurer, N.; Edwards, K.; Karlsson, G.; Cullis, P.R. Formation of drug–arylsulfonate complexes inside liposomes: A novel approach to improve drug retention. J. Control. Release 2006, 110, 378–386. [Google Scholar] [CrossRef]
- Russell, L.; Hultz, M.; Searson, P.C. Leakage kinetics of the liposomal chemotherapeutic agent Doxil: The role of dissolution, protonation, and passive transport, and implications for mechanism of action. J. Control. Release 2017, 269, 171–176. [Google Scholar] [CrossRef]
- Patra, M.; Salonen, E.; Terama, E.; Vattulainen, I.; Faller, R.; Lee, B.W.; Holopainen, J.; Karttunen, M. Under the Influence of Alcohol: The Effect of Ethanol and Methanol on Lipid Bilayers. Biophys. J. 2006, 90, 1121–1135. [Google Scholar] [CrossRef] [Green Version]
- Fugit, K.D.; Anderson, B.D. Dynamic, Nonsink Method for the Simultaneous Determination of Drug Permeability and Binding Coefficients in Liposomes. Mol. Pharm. 2014, 11, 1314–1325. [Google Scholar] [CrossRef] [PubMed]
- Rizvi, S.Z.H.; Shah, F.A.; Khan, N.; Muhammad, I.; Ali, K.H.; Ansari, M.M.; Din, F.U.; Qureshi, O.S.; Kim, K.-W.; Choe, Y.-H.; et al. Simvastatin-loaded solid lipid nanoparticles for enhanced anti-hyperlipidemic activity in hyperlipidemia animal model. Int. J. Pharm. 2019, 560, 136–143. [Google Scholar] [CrossRef]
- Galiullina, L.F.; Scheidt, H.A.; Huster, D.; Aganov, A.; Klochkov, V. Interaction of statins with phospholipid bilayers studied by solid-state NMR spectroscopy. Biochim. et Biophys. Acta (BBA)—Biomembr. 2018, 1861, 584–593. [Google Scholar] [CrossRef]
- Labani-Motlagh, A.; Ashja-Mahdavi, M.; Loskog, A. The Tumor Microenvironment: A Milieu Hindering and Obstructing Antitumor Immune Responses. Front. Immunol. 2020, 11, 940. [Google Scholar] [CrossRef]
- Baghban, R.; Roshangar, L.; Jahanban-Esfahlan, R.; Seidi, K.; Ebrahimi-Kalan, A.; Jaymand, M.; Kolahian, S.; Javaheri, T.; Zare, P. Tumor microenvironment complexity and therapeutic implications at a glance. Cell Commun. Signal. 2020, 18, 1–19. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Wei, C.; Yang, C.; Wang, S.; Shi, D.; Zhang, C.; Lin, X.; Liu, Q.; Dou, R.; Xiong, B. Crosstalk between cancer cells and tumor associated macrophages is required for mesenchymal circulating tumor cell-mediated colorectal cancer metastasis. Mol. Cancer. 2019, 18, 1–23. [Google Scholar] [CrossRef] [PubMed]
- Mallappa, S.; Neeli, P.K.; Karnewar, S.; Kotamraju, S. Doxorubicin induces prostate cancer drug resistance by upregulation of ABCG4 through GSH depletion and CREB activation: Relevance of statins in chemosensitization. Mol. Carcinog. 2019, 58, 1118–1133. [Google Scholar] [CrossRef] [PubMed]
- Hamanaka, R.B.; Chandel, N.S. Mitochondrial reactive oxygen species regulate cellular signaling and dictate biological outcomes. Trends Biochem. Sci. 2010, 35, 505–513. [Google Scholar] [CrossRef] [Green Version]
- Horowitz, A.T.; Barenholz, Y.; Gabizon, A.A. In vitro cytotoxicity of liposome-encapsulated doxorubicin: Dependence on liposome composition and drug release. Biochim. et Biophys. Acta (BBA)—Biomembr. 1992, 1109, 203–209. [Google Scholar] [CrossRef]






| PL (mM) | 44 | 77 |
|---|---|---|
| DOX (µg/mL) | 176.86 ± 25.39 | 194.9 ± 66.43 |
| SIM (µg/mL) | 1267.42 ± 121.96 | 1552.44 ± 76.13 |
| Quality Target Product Profile | Target | Justification | |
|---|---|---|---|
| Formulation | Liposomes | - | To deliver simultaneously SIM and DOX at the tumor site |
| Route of administration | Intravenous | - | To increase the bioavailability of both active substances at the tumor site |
| Quality attributes | Pegylated liposomes | - | To ensure prolonged blood circulation time for liposomes |
| Zeta potential | ≤−30 mV | Values higher than +30 mV or lower than −30 mV are required for a good colloidal stability of the formulation | |
| EE% | 50–100% | Reduced production losses | |
| Drug entrapped concentrations | DOX > 120 µg/mL | Increased dosing intervals | |
| SIM > 1200 µg/mL | |||
| SIM to DOX molar ratio | 12 to 1 | Securing the right ratio between the two active substances in liposomal formulation is essential to achieve the desired cytotoxic effect at the tumor site | |
| Spherical shape | - | Active loading of DOX into liposomes may lead to a deformation of liposomes shape and membrane disruption | |
| Size | 50–200 nm | Enhanced permeability retention effect is dependent on the liposomal size, values smaller than 200 nm being indicated; Liposomes smaller than 50 nm are quickly eliminated by the spleen and through kidney filtration | |
| PdI | <0.2 | A monodisperse liposomal suspension is critical for predictable in vivo behavior | |
| Prolonged in vitrorelease profile | - | Required in order to increase the dosing interval and to prevent off-site drug release | |
| Parameter | Failure Mode | Failure Effects | Potential Causes | Control Methods | S | D | O | RPN |
|---|---|---|---|---|---|---|---|---|
| Drug entrapped concentration and EE% | -Reduced drug entrapped concentration; -Reduced EE% | -Drug losses; -Increased production costs; -Frequent dosing required; -Enhanced administered doses; -Reduced patient compliance; -Diminished therapeutic effect | PL physiochemical properties | Use of PL with an increased Tm | 3 | 1 | 5 | 15 |
| PL concentration | Identification of an appropriate concentration range | 5 | 4 | 5 | 100 | |||
| SIM concentration | 5 | 4 | 5 | 100 | ||||
| DOX concentration | 5 | 4 | 5 | 100 | ||||
| PL to cholesterol molar ratio | 5 | 1 | 1 | 5 | ||||
| DOX loading method | Use of active loading method | 5 | 1 | 1 | 5 | |||
| Type of sulphate salt | Use of AS salt | 5 | 1 | 3 | 15 | |||
| Sulphate salt concentration | Use of a 250 mM salt concentration | 3 | 1 | 3 | 9 | |||
| The pH of the hydration medium | Optimization of the pH of the AS solution | 3 | 4 | 5 | 60 | |||
| Establishing a pH gradient | Optimization of liposomes purification step | 1 | 1 | 1 | 1 | |||
| DOX to PL molar ratio | Use of a DOX to PL molar ratio smaller than 0.95 | 4 | 1 | 2 | 8 | |||
| Incubation time | Optimization of incubation time of SIM-LCL with DOX | 5 | 4 | 5 | 100 | |||
| Incubation temperature | Performing the incubation step at 60 °C | 4 | 1 | 1 | 4 | |||
| Size and PdI | -Multilamellar vesicles; -Polydisperse suspension; -Increased liposomal size | -Reduced internal liposomal volume for DOX encapsulation; -Diminished therapeutic effect; -Fast elimination through reticuloendothelial system; -Reduced colloidal stability | Size reduction method | Application of extrusion process | 1 | 1 | 1 | 1 |
| Optimizing the number of extrusion cycles | 5 | 1 | 3 | 15 | ||||
| Use of membranes with a reduced pore size | 4 | 1 | 4 | 16 | ||||
| Prolonged blood circulation time | Rapid removal from blood circulation | -Frequent dosing required; -Diminished therapeutic effect | Formulation of conventional liposomes | Use of pegylated PL | 5 | 1 | 4 | 20 |
| Prolonged release profile | Fast drug release rate | -Diminished therapeutic effect; -Frequent dosing required; -Off-site drug release; -Increased number of side effects; -Reduced patient compliance; -Increased health care costs | Use of reduced PL concentration | Optimization of PL concentration | 4 | 4 | 5 | 80 |
| SIM and DOX concentration | Optimization of drug concentration | 2 | 2 | 5 | 20 | |||
| Use of PL with a reduced Tm | Use of PL with an increased Tm | 3 | 1 | 4 | 12 | |||
| Zeta potential | Values in the range of −20 mV to +20 mV | -Reduced colloidal stability; -Interactions with blood constituents and rapid removal from blood circulation; -Vesicle agglomeration; -Sedimentation | PL concentration | Optimization of PL concentration | 5 | 4 | 5 | 100 |
| Ionic strength of the liposomes external medium; | Use of NaCl for dialysis | 3 | 2 | 2 | 12 | |||
| Type of PL | Use of charged PL | 3 | 3 | 2 | 18 |
| Exp Name | X1 | X2 | X3 | X4 | X5 | Y1 | Y2 | Y3 | Y4 | Y5 | Y6 | Y7 | Y8 | Y9 |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| N1 | 11 | 2 | 0.25 | 5.00 | 15 | 157.67 | 18.77 | 59.64 | 28.67 | 118.46 | 0.023 | 110.33 | 0.028 | −22.56 |
| N2 | 11 | 7 | 0.50 | 5.00 | 30 | 297.51 | 10.20 | 123.95 | 42.59 | 111.86 | 0.060 | 106.76 | 0.091 | −20.70 |
| N3 | 11 | 12 | 0.75 | 5.00 | 45 | 126.60 | 2.52 | 173.84 | 38.14 | 108.86 | 0.047 | 105.83 | 0.066 | −25.16 |
| N4 | 44 | 2 | 0.25 | 5.00 | 30 | 364.58 | 44.05 | 156.66 | 91.45 | 123.33 | 0.014 | 122.00 | 0.036 | −34.66 |
| N5 | 44 | 7 | 0.50 | 5.00 | 45 | 1129.08 | 38.66 | 325.19 | 84.20 | 118.06 | 0.030 | 110.16 | 0.056 | −31.20 |
| N6 | 44 | 12 | 0.75 | 5.00 | 15 | 1809.98 | 35.80 | 378.42 | 75.07 | 117.93 | 0.025 | 115.16 | 0.051 | −36.46 |
| N7 | 77 | 2 | 0.50 | 5.00 | 15 | 224.54 | 27.03 | 285.83 | 74.00 | 132.93 | 0.050 | 125.53 | 0.039 | −35.53 |
| N8 | 77 | 7 | 0.75 | 5.00 | 30 | 1130.26 | 38.61 | 439.40 | 87.16 | 122.50 | 0.031 | 117.10 | 0.060 | −34.46 |
| N9 | 77 | 12 | 0.25 | 5.00 | 45 | 1384.17 | 27.61 | 202.12 | 97.16 | 125.16 | 0.020 | 116.80 | 0.034 | −37.00 |
| N10 | 11 | 2 | 0.75 | 5.50 | 45 | 232.02 | 25.66 | 189.37 | 41.55 | 117.26 | 0.046 | 115.30 | 0.075 | −21.13 |
| N11 | 11 | 7 | 0.25 | 5.50 | 15 | 185.80 | 6.31 | 61.30 | 29.47 | 114.56 | 0.040 | 110.36 | 0.079 | −37.93 |
| N12 | 11 | 12 | 0.50 | 5.50 | 30 | 238.31 | 4.74 | 167.75 | 57.64 | 116.03 | 0.057 | 110.70 | 0.068 | −28.50 |
| N13 | 44 | 2 | 0.50 | 5.50 | 45 | 336.65 | 39.76 | 275.85 | 88.19 | 128.20 | 0.065 | 126.00 | 0.056 | −30.93 |
| N14 | 44 | 7 | 0.75 | 5.50 | 15 | 1335.59 | 45.73 | 410.57 | 88.31 | 120.60 | 0.046 | 115.33 | 0.062 | −25.70 |
| N15 | 44 | 12 | 0.25 | 5.50 | 30 | 1200.86 | 23.97 | 66.84 | 39.88 | 116.86 | 0.045 | 109.43 | 0.059 | −27.60 |
| N16 | 77 | 2 | 0.75 | 5.50 | 30 | 244.61 | 29.22 | 401.70 | 79.68 | 135.76 | 0.029 | 132.36 | 0.040 | −31.96 |
| N17 | 77 | 7 | 0.25 | 5.50 | 45 | 1130.51 | 37.73 | 111.75 | 53.72 | 121.06 | 0.045 | 116.03 | 0.052 | −35.53 |
| N18 | 77 | 12 | 0.50 | 5.50 | 15 | 1361.95 | 27.09 | 251.59 | 65.14 | 120.53 | 0.052 | 115.50 | 0.022 | −33.34 |
| N19 | 44 | 7 | 0.50 | 5.00 | 15 | 1969.29 | 67.21 | 228.17 | 78.40 | 120.86 | 0.028 | 114.36 | 0.054 | −29.03 |
| N20 | 44 | 7 | 0.50 | 5.00 | 15 | 2066.85 | 70.71 | 274.19 | 94.21 | 120.43 | 0.021 | 115.76 | 0.050 | −34.63 |
| N21 | 44 | 7 | 0.50 | 5.00 | 15 | 1392.23 | 47.50 | 253.12 | 86.97 | 119.83 | 0.045 | 115.40 | 0.045 | −26.70 |
| Liposomal Formulation | X1 | X2 | X3 | Y1 | Y2 | Y3 | Y4 | Y7 | Y8 | Y9 |
|---|---|---|---|---|---|---|---|---|---|---|
| DOX-LCL | 44 | - | 0.5 | - | - | 165.47 | 56.08 | 129.4 | 0.055 | −28.7 |
| SIM1-DOX-LCL | 44 | 2 | 0.25 | 260.74 | 35.59 | 89.90 | 62.33 | 119.8 | 0.050 | −28.3 |
| SIM2-DOX-LCL | 44 | 12 | 0.5 | 998.49 | 19.92 | 115.37 | 37.27 | 104.3 | 0.071 | −27 |
| Pharmaceutical Formulation | Tested Drug Concentration | IC50 (μM) |
|---|---|---|
| SIM solution | 0.041–20.7 μM | 3 ± 0.560 |
| DOX solution | 0.007–10 μM | 0.25 ± 0.047 |
| SIM1 + DOX (variable) | 0.934 μM SIM + (0.015–8 μM) DOX | 0.06 ± 0.036 |
| SIM2 + DOX (variable) | 3 μM SIM+ (0.019–8 μM) DOX | 0.27 ± 0.114 |
| DOX-LCL | 0.007–5 μM DOX | 0.27 ± 0.127 |
| SIM1-DOX-LCL | 0.934 μM SIM + (0.007–5) μM DOX | 0.37 ± 0.086 |
| SIM2-DOX-LCL | 3 μM SIM + (0.007–5) μM DOX | 0.08 ± 0.044 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Barbălată, C.I.; Porfire, A.S.; Sesarman, A.; Rauca, V.-F.; Banciu, M.; Muntean, D.; Știufiuc, R.; Moldovan, A.; Moldovan, C.; Tomuță, I. A Screening Study for the Development of Simvastatin-Doxorubicin Liposomes, a Co-Formulation with Future Perspectives in Colon Cancer Therapy. Pharmaceutics 2021, 13, 1526. https://doi.org/10.3390/pharmaceutics13101526
Barbălată CI, Porfire AS, Sesarman A, Rauca V-F, Banciu M, Muntean D, Știufiuc R, Moldovan A, Moldovan C, Tomuță I. A Screening Study for the Development of Simvastatin-Doxorubicin Liposomes, a Co-Formulation with Future Perspectives in Colon Cancer Therapy. Pharmaceutics. 2021; 13(10):1526. https://doi.org/10.3390/pharmaceutics13101526
Chicago/Turabian StyleBarbălată, Cristina Ioana, Alina Silvia Porfire, Alina Sesarman, Valentin-Florian Rauca, Manuela Banciu, Dana Muntean, Rareș Știufiuc, Alin Moldovan, Cristian Moldovan, and Ioan Tomuță. 2021. "A Screening Study for the Development of Simvastatin-Doxorubicin Liposomes, a Co-Formulation with Future Perspectives in Colon Cancer Therapy" Pharmaceutics 13, no. 10: 1526. https://doi.org/10.3390/pharmaceutics13101526
APA StyleBarbălată, C. I., Porfire, A. S., Sesarman, A., Rauca, V.-F., Banciu, M., Muntean, D., Știufiuc, R., Moldovan, A., Moldovan, C., & Tomuță, I. (2021). A Screening Study for the Development of Simvastatin-Doxorubicin Liposomes, a Co-Formulation with Future Perspectives in Colon Cancer Therapy. Pharmaceutics, 13(10), 1526. https://doi.org/10.3390/pharmaceutics13101526









