Intravitreal Dexamethasone Implant as a Sustained Release Drug Delivery Device for the Treatment of Ocular Diseases: A Comprehensive Review of the Literature
Abstract
1. Introduction
2. Methods
3. Dex Implant Mechanism of Action and Pharmacokinetic
4. Dex Implant in Retinal Vein Occlusion
4.1. Pathogenesis of Retinal Vein Occlusion and Inflammation
4.2. Evidence of the Efficacy of Dex Implant in RVO
5. Dex Implant in Posterior Non-Infectious Uveitis
5.1. Pathogenesis of Posterior Non-Infectious Uveitis
5.2. Evidence of the Efficacy of Dex in Posterior Non-Infectious Uveitis
6. Dex Implant in Diabetic Retinopathy
6.1. Pathogenesis of Diabetic Macular Edema and Inflammation
6.2. Evidence of the Efficacy of Dex in Diabetic Macular Edema
7. Dex Implant in Neovascular Age-Related Macular Degeneration
Evidence of the Efficacy of Dex in Age-Related Macular Degeneration
8. Dex Implant in Inherited Retinal Disorders
Evidence of the Efficacy of Dex in Inherited Retinal Disorders
9. Dex Implant in Other Conditions
Evidence of the Efficacy of Dex in Other Conditions
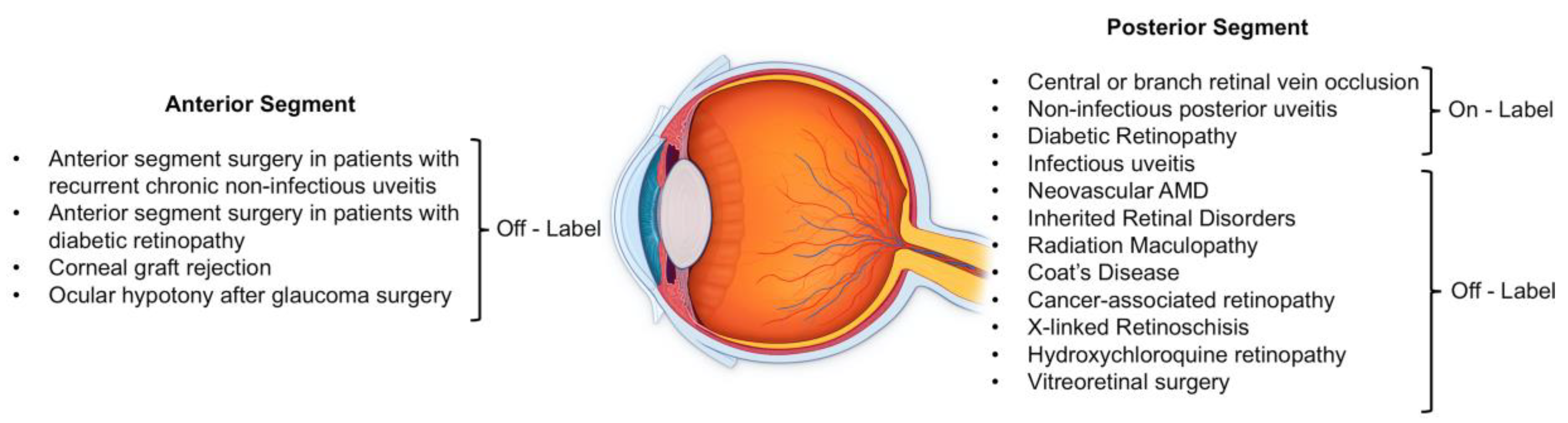
10. Dex Implant in Ocular Surgery
10.1. Evidence of the Efficacy of Dex in Anterior Segment Surgery
10.2. Evidence of the Efficacy of Dex in Vitreoretinal Surgery
11. Safety Profile of Dex Implant
11.1. Dex Implant and IOP
11.2. Dex Implant and Anterior Segment Complications
11.3. Dex Implant and Posterior Segment Complications
11.4. Dex Implant and Adnexa
11.5. Dex Implant and Pregnancy
12. Conclusions
Author Contributions
Funding
Conflicts of Interest
References
- Kuno, N.; Fujii, S. Biodegradable intraocular therapies for retinal disorders: Progress to date. Drugs Aging 2010, 27, 117–134. [Google Scholar] [CrossRef] [PubMed]
- Lowder, C.; Belfort, R.; Lightman, S.; Foster, C.S.; Robinson, M.R.; Schiffman, R.M.; Li, X.Y.; Cui, H.; Whitcup, S.M. Dexamethasone intravitreal implant for noninfectious intermediate or posterior uveitis. Arch. Ophthalmol. 2011, 129, 545–553. [Google Scholar] [CrossRef] [PubMed]
- Coscas, G.; Augustin, A.; Bandello, F.; De Smet, M.D.; Lanzetta, P.; Staurenghi, G.; Parravano, M.C.; Udaondo, P.; Moisseiev, E.; Soubrane, G.; et al. Retreatment with Ozurdex for macular edema secondary to retinal vein occlusion. Eur. J. Ophthalmol. 2013, 24, 1–9. [Google Scholar] [CrossRef] [PubMed]
- Dugel, P.U.; Bandello, F.; Loewenstein, A. Dexamethasone intravitreal implant in the treatment of diabetic macular edema. Clin. Ophthalmol. 2015, 9, 1321–1335. [Google Scholar] [CrossRef]
- Koronis, S.; Stavrakas, P.; Balidis, M.; Kozeis, N.; Tranos, P.G. Update in treatment of uveitic macular edema. Drug Des. Devel. Ther. 2019, 13, 667–680. [Google Scholar] [CrossRef]
- He, Y.; Ren, X.J.; Hu, B.J.; Lam, W.C.; Li, X.R. A meta-analysis of the effect of a dexamethasone intravitreal implant versus intravitreal anti-vascular endothelial growth factor treatment for diabetic macular edema. BMC Ophthalmol. 2018, 18, 121. [Google Scholar] [CrossRef]
- Campochiaro, P.A.; Hafiz, G.; Mir, T.A.; Scott, A.W.; Sophie, R.; Shah, S.M.; Ying, H.S.; Lu, L.; Chen, C.; Campbell, J.P.; et al. Pro-Permeability Factors after Dexamethasone Implant in Retinal Vein Occlusion; The Ozurdex for Retinal Vein Occlusion (ORVO) Study. Am. J. Ophthalmol. 2015, 160, 313–321. [Google Scholar] [CrossRef]
- Chang-Lin, J.E.; Attar, M.; Acheampong, A.A.; Robinson, M.R.; Whitcup, S.M.; Kuppermann, B.D.; Welty, D. Pharmacokinetics and pharmacodynamics of a sustained-release dexamethasone intravitreal implant. Investig. Ophthalmol. Vis. Sci. 2011, 52, 80–86. [Google Scholar] [CrossRef]
- Chin, E.K.; Almeida, D.R.; Velez, G.; Xu, K.; Peraire, M.; Corbella, M.; Elshatory, Y.M.; Kwon, Y.H.; Gehrs, K.M.; Culver Boldt, H.; et al. Ocular Hypertension after Intravitreal Dexamethasone (Ozurdex) Sustained-Release Implant. Retina 2017, 37, 1345–1351. [Google Scholar] [CrossRef]
- Yau, J.W.Y.; Lee, P.; Wong, T.Y.; Best, J.; Jenkins, A. Retinal vein occlusion: An approach to diagnosis, systemic risk factors and management. Intern. Med. J. 2008, 38, 904–910. [Google Scholar] [CrossRef]
- Campochiaro, P.A.; Choy, D.F.; Do, D.V.; Hafiz, G.; Shah, S.M.; Nguyen, Q.D.; Rubio, R.; Arron, J.R. Monitoring ocular drug therapy by analysis of aqueous samples. Ophthalmology 2009, 116, 2158–2164. [Google Scholar] [CrossRef] [PubMed]
- Rehak, M.; Wiedemann, P. Retinal vein thrombosis: Pathogenesis and management. J. Thromb. Haemost. 2010, 8, 1886–1894. [Google Scholar] [CrossRef] [PubMed]
- Au, A.; Hilely, A.; Scharf, J.; Gunnemann, F.; Wang, D.; Chehaibou, I.; Iovino, C.; Grondin, C.; Farecki, M.-L.; Falavarjani, K.G.; et al. Relationship between nerve fiber layer hemorrhages and outcomes in central retinal vein occlusion. Invest. Ophthalmol. Vis. Sci. 2020, 61, 54. [Google Scholar] [CrossRef] [PubMed]
- Haller, J.A.; Bandello, F.; Belfort, R.; Blumenkranz, M.S.; Gillies, M.; Heier, J.; Loewenstein, A.; Yoon, Y.H.; Jiao, J.; Li, X.Y.; et al. Dexamethasone intravitreal implant in patients with macular edema related to branch or central retinal vein occlusion: Twelve-month study results. Ophthalmology 2011, 118, 2453–2460. [Google Scholar] [CrossRef]
- Rezar-Dreindl, S.; Eibenberger, K.; Pollreisz, A.; Bühl, W.; Georgopoulos, M.; Krall, C.; Dunavölgyi, R.; Weigert, G.; Kroh, M.E.; Schmidt-Erfurth, U.; et al. Effect of intravitreal dexamethasone implant on intra-ocular cytokines and chemokines in eyes with retinal vein occlusion. Acta Ophthalmol. 2017, 95, e119–e127. [Google Scholar] [CrossRef]
- Tadayoni, R.; Waldstein, S.M.; Boscia, F.; Gerding, H.; Gekkieva, M.; Barnes, E.; Das Gupta, A.; Wenzel, A.; Pearce, I. Sustained Benefits of Ranibizumab with or without Laser in Branch Retinal Vein Occlusion: 24-Month Results of the BRIGHTER Study. Ophthalmology 2017, 124, 1778–1787. [Google Scholar] [CrossRef]
- Noma, H.; Funatsu, H.; Mimura, T.; Eguchi, S.; Hori, S. Soluble vascular endothelial growth factor receptor-2 and inflammatory factors in macular edema with branch retinal vein occlusion. Am. J. Ophthalmol. 2011, 152, 669–677. [Google Scholar] [CrossRef]
- Campochiaro, P.A.; Heier, J.S.; Feiner, L.; Gray, S.; Saroj, N.; Rundle, A.C.; Murahashi, W.Y.; Rubio, R.G. Ranibizumab for Macular Edema following Branch Retinal Vein Occlusion. Six-Month Primary End Point Results of a Phase III Study. Ophthalmology 2010, 117, 1102–1112. [Google Scholar] [CrossRef]
- Haller, J.A.; Bandello, F.; Belfort, R.; Blumenkranz, M.S.; Gillies, M.; Heier, J.; Loewenstein, A.; Yoon, Y.H.; Jacques, M.L.; Jiao, J.; et al. Randomized, Sham-Controlled Trial of Dexamethasone Intravitreal Implant in Patients with Macular Edema Due to Retinal Vein Occlusion. Ophthalmology 2010, 117, 1134–1146. [Google Scholar] [CrossRef]
- Li, X.; Wang, N.; Liang, X.; Xu, G.; Li, X.Y.; Jiao, J.; Lou, J.; Hashad, Y. Safety and efficacy of dexamethasone intravitreal implant for treatment of macular edema secondary to retinal vein occlusion in Chinese patients: Randomized, sham-controlled, multicenter study. Graefe’s Arch. Clin. Exp. Ophthalmol. 2018, 256, 59–69. [Google Scholar] [CrossRef]
- Danis, R.P.; Sadda, S.; Jiao, J.; Li, X.Y.; Whitcup, S.M. Relationship between retinal thickness and visual acuity in eyes with retinal vein occlusion treated with dexamethasone implant. Retina 2016, 36, 1170–1176. [Google Scholar] [CrossRef] [PubMed]
- Bezatis, A.; Spital, G.; Höhn, F.; Maier, M.; Clemens, C.R.; Wachtlin, J.; Lehmann, F.; Hattenbach, L.O.; Feltgen, N.; Meyer, C.H. Functional and anatomical results after a single intravitreal Ozurdex injection in retinal vein occlusion: A 6-month follow-up—The SOLO study. Acta Ophthalmol. 2013, 91, e340–e347. [Google Scholar] [CrossRef]
- Kuppermann, B.D.; Haller, J.A.; Bandello, F.; Loewenstein, A.; Jiao, J.; Li, X.Y.; Whitcup, S.M. Onset and duration of visual acuity improvement after dexamethasone intravitreal implant in eyes with macular edema due to retinal vein occlusion. Retina 2014, 34, 1743–1749. [Google Scholar] [CrossRef]
- Ferrini, W.; Ambresin, A. Intravitreal dexamethasone implant for the treatment of macular edema after retinal vein occlusion in a clinical setting. Klin. Monbl. Augenheilkd. 2013, 230, 423–426. [Google Scholar] [CrossRef] [PubMed]
- Yeh, W.S.; Haller, J.A.; Lanzetta, P.; Kuppermann, B.D.; Wong, T.Y.; Mitchell, P.; Whitcup, S.M.; Kowalski, J.W. Effect of the duration of macular edema on clinical outcomes in retinal vein occlusion treated with dexamethasone intravitreal implant. Ophthalmology 2012, 119, 1190–1198. [Google Scholar] [CrossRef] [PubMed]
- Singer, M.A.; Capone, A.; Dugel, P.U.; Dreyer, R.F.; Dodwell, D.G.; Roth, D.B.; Shi, R.; Walt, J.G.; Scott, L.C.; Hollander, D.A. Two or more dexamethasone intravitreal implants as monotherapy or in combination therapy for macular edema in retinal vein occlusion: Subgroup analysis of a retrospective chart review study retina. BMC Ophthalmol. 2015, 15, 33. [Google Scholar] [CrossRef]
- Querques, L.; Querques, G.; Lattanzio, R.; Gigante, S.R.; Del Turco, C.; Corradetti, G.; Cascavilla, M.L.; Bandello, F. Repeated intravitreal dexamethasone implant (Ozurdex®) for retinal vein occlusion. Ophthalmologica 2012, 229, 21–25. [Google Scholar] [CrossRef] [PubMed]
- Sadda, S.; Danis, R.P.; Pappuru, R.R.; Keane, P.A.; Jiao, J.; Li, X.Y.; Whitcup, S.M. Vascular changes in eyes treated with dexamethasone intravitreal implant for macular edema after retinal vein occlusion. Ophthalmology 2013, 120, 1423–1431. [Google Scholar] [CrossRef]
- Campochiaro, P.A.; Sophie, R.; Pearlman, J.; Brown, D.M.; Boyer, D.S.; Heier, J.S.; Marcus, D.M.; Feiner, L.; Patel, A. Long-term outcomes in patients with retinal vein occlusion treated with ranibizumab: The RETAIN study. Ophthalmology 2014, 121, 209–219. [Google Scholar] [CrossRef] [PubMed]
- Hoerauf, H.; Feltgen, N.; Weiss, C.; Paulus, E.M.; Schmitz-Valckenberg, S.; Pielen, A.; Puri, P.; Berk, H.; Eter, N.; Wiedemann, P.; et al. Clinical Efficacy and Safety of Ranibizumab Versus Dexamethasone for Central Retinal Vein Occlusion (COMRADE C): A European Label Study. Am. J. Ophthalmol. 2016, 169, 258–267. [Google Scholar] [CrossRef]
- Hattenbach, L.O.; Feltgen, N.; Bertelmann, T.; Schmitz-Valckenberg, S.; Berk, H.; Eter, N.; Lang, G.E.; Rehak, M.; Taylor, S.R.; Wolf, A.; et al. Head-to-head comparison of ranibizumab PRN versus single-dose dexamethasone for branch retinal vein occlusion (COMRADE-B). Acta Ophthalmol. 2018, 96, e10–e18. [Google Scholar] [CrossRef] [PubMed]
- Feltgen, N.; Hattenbach, L.O.; Bertelmann, T.; Callizo, J.; Rehak, M.; Wolf, A.; Berk, H.; Eter, N.; Lang, G.E.; Pielen, A.; et al. Comparison of ranibizumab versus dexamethasone for macular oedema following retinal vein occlusion: 1-year results of the COMRADE extension study. Acta Ophthalmol. 2018, 96, e933–e941. [Google Scholar] [CrossRef] [PubMed]
- Eter, N.; Mohr, A.; Wachtlin, J.; Feltgen, N.; Shirlaw, A.; Leaback, R. Dexamethasone intravitreal implant in retinal vein occlusion: Real-life data from a prospective, multicenter clinical trial. Graefe’s Arch. Clin. Exp. Ophthalmol. 2017, 255, 77–87. [Google Scholar] [CrossRef] [PubMed]
- Yoon, Y.H.; Kim, J.W.; Lee, J.Y.; Kim, I.T.; Kang, S.W.; Yu, H.G.; Koh, H.J.; Kim, S.S.; Chang, D.J.; Simonyi, S. Dexamethasone intravitreal implant for early treatment and retreatment of macular edema related to branch retinal vein occlusion: The multicenter COBALT Study. Ophthalmologica 2018, 240, 81–89. [Google Scholar] [CrossRef] [PubMed]
- Georgalas, L.; Tservakis, I.; Kiskira, E.E.; Petrou, P.; Papaconstantinou, D.; Kanakis, M. Efficacy and safety of dexamethasone intravitreal implant in patients with retinal vein occlusion resistant to anti-VEGF therapy: A 12-month prospective study. Cutan. Ocul. Toxicol. 2019, 38, 330–337. [Google Scholar] [CrossRef] [PubMed]
- Bandello, F.; Augustin, A.; Tufail, A.; Leaback, R. A 12-month, multicenter, parallel group comparison of dexamethasone intravitreal implant versus ranibizumab in branch retinal vein occlusion. Eur. J. Ophthalmol. 2018, 28, 697–705. [Google Scholar] [CrossRef]
- Kumar, P.; Sharma, Y.R.; Chandra, P.; Azad, R.; Meshram, G.G. Comparison of the Safety and Efficacy of Intravitreal Ranibizumab with or without Laser Photocoagulation Versus Dexamethasone Intravitreal Implant with or without Laser Photocoagulation for Macular Edema Secondary to Branch Retinal Vein Occlusion. Folia Med. (Plovdiv.) 2019, 61, 240–248. [Google Scholar] [CrossRef]
- Chatziralli, I.; Theodossiadis, G.; Kabanarou, S.A.; Parikakis, E.; Xirou, T.; Mitropoulos, P.; Theodossiadis, P. Ranibizumab versus dexamethasone implant for central retinal vein occlusion: The RANIDEX study. Graefe’s Arch. Clin. Exp. Ophthalmol. 2017, 255, 1899–1905. [Google Scholar] [CrossRef]
- Gado, A.S.; Macky, T.A. Dexamethasone intravitreous implant versus bevacizumab for central retinal vein occlusion-related macular oedema: A prospective randomized comparison. Clin. Exp. Ophthalmol. 2014, 42, 650–655. [Google Scholar] [CrossRef]
- Accorinti, M.; Okada, A.A.; Smith, J.R.; Gilardi, M. Epidemiology of Macular Edema in Uveitis. Ocul. Immunol. Inflamm. 2019, 27, 169–180. [Google Scholar] [CrossRef]
- Carnahan, M.C.; Goldstein, D.A. Ocular complications of topical, peri-ocular, and systemic corticosteroids. Curr. Opin. Ophthalmol. 2000, 11, 478–483. [Google Scholar] [CrossRef] [PubMed]
- Varela-Fernández, R.; Díaz-Tomé, V.; Luaces-Rodríguez, A.; Conde-Penedo, A.; García-Otero, X.; Luzardo-álvarez, A.; Fernández-Ferreiro, A.; Otero-Espinar, F.J. Drug delivery to the posterior segment of the eye: Biopharmaceutic and pharmacokinetic considerations. Pharmaceutics 2020, 12, 269. [Google Scholar] [CrossRef]
- Lightman, S.; Belfort, R.; Naik, R.K.; Lowder, C.; Foster, C.S.; Rentz, A.M.; Cui, H.; Whitcup, S.M.; Kowalski, J.W.; Revicki, D.A. Vision-related functioning outcomes of dexamethasone intravitreal implant in noninfectious intermediate or posterior uveitis. Investig. Ophthalmol. Vis. Sci. 2013, 54, 4864–4870. [Google Scholar] [CrossRef] [PubMed]
- Williams, G.A.; Haller, J.A.; Kuppermann, B.D.; Blumenkranz, M.S.; Weinberg, D.V.; Chou, C.; Whitcup, S.M. Dexamethasone Posterior-Segment Drug Delivery System in the Treatment of Macular Edema Resulting from Uveitis or Irvine-Gass Syndrome. Am. J. Ophthalmol. 2009, 147, 1048–1054. [Google Scholar] [CrossRef] [PubMed]
- Myung, J.S.; Aaker, G.D.; Kiss, S. Treatment of noninfectious posterior uveitis with dexamethasone intravitreal implant. Clin. Ophthalmol. 2010, 4, 1423–1426. [Google Scholar] [PubMed]
- Hasanreisoğlu, M.; Özdemir, H.B.; Özkan, K.; Yüksel, M.; Aktaş, Z.; Atalay, H.T.; Özdek, Ş.; Gürelik, G. Intravitreal Dexamethasone Implant in the Treatment of Non-infectious Uveitis. Turkish J. Ophthalmol. 2019, 49, 250–257. [Google Scholar] [CrossRef]
- Pohlmann, D.; vom Brocke, G.A.; Winterhalter, S.; Steurer, T.; Thees, S.; Pleyer, U. Dexamethasone Inserts in Noninfectious Uveitis: A Single-Center Experience. Ophthalmology 2018, 125, 1088–1099. [Google Scholar] [CrossRef]
- Tomkins-Netzer, O.; Taylor, S.R.J.; Bar, A.; Lula, A.; Yaganti, S.; Talat, L.; Lightman, S. Treatment with repeat dexamethasone implants results in long-term disease control in eyes with noninfectious uveitis. Ophthalmology 2014, 121, 1649–1654. [Google Scholar] [CrossRef]
- Zarranz-Ventura, J.; Carreño, E.; Johnston, R.L.; Mohammed, Q.; Ross, A.H.; Barker, C.; Fonollosa, A.; Artaraz, J.; Pelegrin, L.; Adan, A.; et al. Multicenter study of intravitreal dexamethasone implant in noninfectious uveitis: Indications, outcomes, and reinjection frequency. Am. J. Ophthalmol. 2014, 158, 1136–1145. [Google Scholar] [CrossRef]
- Saraiya, N.V.; Goldstein, D.A. Dexamethasone for ocular inflammation. Expert Opin. Pharmacother. 2011, 12, 1127–1131. [Google Scholar] [CrossRef]
- Sallam, A.; Taylor, S.R.J.; Lightman, S. Review and update of intraocular therapy in noninfectious uveitis. Curr. Opin. Ophthalmol. 2011, 22, 517–522. [Google Scholar] [CrossRef] [PubMed]
- Thorne, J.E.; Sugar, E.A.; Holbrook, J.T.; Burke, A.E.; Altaweel, M.M.; Vitale, A.T.; Acharya, N.R.; Kempen, J.H.; Jabs, D.A. Periocular Triamcinolone vs. Intravitreal Triamcinolone vs. Intravitreal Dexamethasone Implant for the Treatment of Uveitic Macular Edema: The PeriOcular vs. INTravitreal corticosteroids for uveitic macular edema (POINT) Trial. Ophthalmology 2019, 126, 283–295. [Google Scholar] [CrossRef] [PubMed]
- Khurana, R.N.; Bansal, A.S.; Chang, L.K.; Palmer, J.D.; Wu, C.; Wieland, M.R. Prospective evaluation of a sustained-release dexamethasone intravitreal implant for cystoid macular edema in quiescent uveitis. Retina 2017, 37, 1692–1699. [Google Scholar] [CrossRef] [PubMed]
- Cao, J.H.; Mulvahill, M.; Zhang, L.; Joondeph, B.C.; Dacey, M.S. Dexamethasone intravitreal implant in the treatment of persistent uveitic macular edema in the absence of active inflammation. Ophthalmology 2014, 121, 1871–1876. [Google Scholar] [CrossRef] [PubMed]
- Miserocchi, E.; Modorati, G.; Pastore, M.R.; Bandello, F. Dexamethasone intravitreal implant: An effective adjunctive treatment for recalcitrant noninfectious uveitis. Ophthalmologica 2012, 228, 229–233. [Google Scholar] [CrossRef]
- Fabiani, C.; Vitale, A.; Emmi, G.; Lopalco, G.; Vannozzi, L.; Bacherini, D.; Guerriero, S.; Favale, R.A.; Fusco, F.; Franceschini, R.; et al. Systemic Steroid Sparing Effect of Intravitreal Dexamethasone Implant in Chronic Noninfectious Uveitic Macular Edema. J. Ocul. Pharmacol. Ther. 2017, 33, 549–555. [Google Scholar] [CrossRef]
- Ratra, D.; Barh, A.; Banerjee, M.; Ratra, V.; Biswas, J. Safety and Efficacy of Intravitreal Dexamethasone Implant for Refractory Uveitic Macular Edema in Adults and Children. Ocul. Immunol. Inflamm. 2018, 26, 1034–1040. [Google Scholar] [CrossRef]
- Coşkun, E.; Celemler, P.; Kimyon, G.; Öner, V.; Kisacik, B.; Erbagci, I.; Onat, A.M. Intravitreal Dexamethasone Implant for Treatment of Refractory Behçet Posterior Uveitis: One-year Follow-up Results. Ocul. Immunol. Inflamm. 2015, 23, 437–443. [Google Scholar] [CrossRef]
- Fabiani, C.; Emmi, G.; Lopalco, G.; Vannozzi, L.; Bacherini, D.; Guerriero, S.; Franceschini, R.; Frediani, B.; Iannone, F.; Marco Tosi, G.; et al. Intravitreal Dexamethasone Implant as an Adjunct Weapon for Severe and Refractory Uveitis in Behçet’s Disease. Isr. Med. Assoc. J. 2017, 19, 415–419. [Google Scholar]
- Kim, M.; Kim, S.A.; Park, W.; Kim, R.Y.; Park, Y.H. Intravitreal Dexamethasone Implant for Treatment of Sarcoidosis-Related Uveitis. Adv. Ther. 2019, 36, 2137–2146. [Google Scholar] [CrossRef]
- Pelegrín, L.; De La Maza, M.S.; Molins, B.; Ríos, J.; Adán, A. Long-term evaluation of dexamethasone intravitreal implant in vitrectomized and non-vitrectomized eyes with macular edema secondary to non-infectious uveitis. Eye 2015, 29, 943–950. [Google Scholar] [CrossRef] [PubMed]
- Kim, J.T.; Yoon, Y.H.; Lee, D.H.; Joe, S.G.; Kim, J.G. Dexamethasone intravitreal implant in the silicone oil-filled eye for the treatment for recurrent macular oedema associated with ankylosing spondylitis: A case report. Acta Ophthalmol. 2013, 91, e331–e332. [Google Scholar] [CrossRef] [PubMed]
- Nguyen, T.; Kim, H.; Mielke, C.; Momont, A.C.; Brandt, J.D.; Liu, Y. Combined Dexamethasone Intravitreal Implant and Glaucoma Drainage Device Placement for Uveitic Glaucoma. J. Glaucoma 2020, 29, 252–257. [Google Scholar] [CrossRef] [PubMed]
- Tomkins-Netzer, O.; Talat, L.; Seguin-Greenstein, S.; Bar, A.; Lightman, S. Outcome of Treating Pediatric Uveitis with Dexamethasone Implants. Am. J. Ophthalmol. 2016, 161, 110–115. [Google Scholar] [CrossRef] [PubMed]
- Bratton, M.L.; He, Y.G.; Weakley, D.R. Dexamethasone intravitreal implant (Ozurdex) for the treatment of pediatric uveitis. J. AAPOS 2014, 18, 110–113. [Google Scholar] [CrossRef] [PubMed]
- Pichi, F.; Nucci, P.; Baynes, K.; Lowder, C.Y.; Srivastava, S.K. Sustained-release dexamethasone intravitreal implant in juvenile idiopathic arthritis-related uveitis. Int. Ophthalmol. 2017, 37, 221–228. [Google Scholar] [CrossRef]
- Sella, R.; Oray, M.; Friling, R.; Umar, L.; Tugal-Tutkun, I.; Kramer, M. Dexamethasone intravitreal implant (Ozurdex®) for pediatric uveitis. Graefe’s Arch. Clin. Exp. Ophthalmol. 2015, 253, 1777–1782. [Google Scholar] [CrossRef]
- Miserocchi, E.; Berchicci, L.; Iuliano, L.; Modorati, G.; Bandello, F. Dexamethasone intravitreal implant in serpiginous choroiditis. Br. J. Ophthalmol. 2017, 101, 327–332. [Google Scholar] [CrossRef]
- Walsh, J.; Reddy, A.K. Intravitreal dexamethasone implantation for birdshot chorioretinopathy. Retin. Cases Br. Rep. 2017, 11, 51–55. [Google Scholar] [CrossRef]
- Bajwa, A.; Peck, T.; Reddy, A.K.; Netland, P.A.; Shildkrot, Y. Dexamethasone implantation in birdshot chorioretinopathy—Long-term outcome. Int. Med. Case Rep. J. 2018, 11, 349–358. [Google Scholar] [CrossRef]
- Barnes, A.C.; Lowder, C.Y.; Bessette, A.P.; Baynes, K.; Srivastava, S.K. Treatment of acute zonal occult outer retinopathy with intravitreal steroids. Ophthalmic Surg. Lasers Imaging Retin. 2018, 49, 504–509. [Google Scholar] [CrossRef] [PubMed]
- Mora-Cantallops, A.; Pérez, M.D.; Revenga, M.; González-López, J.J. Ellipsoid layer restoration after Ozurdex® treatment in a patient with acute posterior multifocal placoid pigment epitheliopathy. Eur. J. Ophthalmol. 2019. [Google Scholar] [CrossRef] [PubMed]
- Empeslidis, T.; Banerjee, S.; Vardarinos, A.; Konstas, A.G.P. Dexamethasone intravitreal implant for idiopathic retinal vasculitis, aneurysms, and neuroretinitis. Eur. J. Ophthalmol. 2013, 23, 757–760. [Google Scholar] [CrossRef] [PubMed]
- Saatci, A.O.; Ayhan, Z.; Takeş, Ö.; Yaman, A.; Söylev Bajin, F.M. Single bilateral dexamethasone implant in addition to panretinal photocoagulation and oral azathioprine treatment in IRVAN syndrome. Case Rep. Ophthalmol. 2015, 6, 56–62. [Google Scholar] [CrossRef]
- Klein, R.; Klein, B.E.K.; Moss, S.E.; Davis, M.D.; DeMets, D.L. The Wisconsin Epidemiologic Study of Diabetic Retinopathy: IV. Diabetic Macular Edema. Ophthalmology 1984, 91, 1464–1474. [Google Scholar] [CrossRef]
- Boyer, D.S.; Yoon, Y.H.; Belfort, R.; Bandello, F.; Maturi, R.K.; Augustin, A.J.; Li, X.Y.; Cui, H.; Hashad, Y.; Whitcup, S.M. Three-year, randomized, sham-controlled trial of dexamethasone intravitreal implant in patients with diabetic macular edema. Ophthalmology 2014, 121, 1904–1914. [Google Scholar] [CrossRef]
- Schmidt-Erfurth, U.; Garcia-Arumi, J.; Bandello, F.; Berg, K.; Chakravarthy, U.; Gerendas, B.S.; Jonas, J.; Larsen, M.; Tadayoni, R.; Loewenstein, A. Guidelines for the management of diabetic macular edema by the European Society of Retina Specialists (EURETINA). Ophthalmologica 2017, 237, 185–222. [Google Scholar] [CrossRef]
- Bandello, F.; Toni, D.; Porta, M.; Varano, M. Diabetic retinopathy, diabetic macular edema, and cardiovascular risk: The importance of a long-term perspective and a multidisciplinary approach to optimal intravitreal therapy. Acta Diabetol. 2020, 57, 513–526. [Google Scholar] [CrossRef]
- Danis, R.P.; Sadda, S.; Li, X.Y.; Cui, H.; Hashad, Y.; Whitcup, S.M. Anatomical effects of dexamethasone intravitreal implant in diabetic macular oedema: A pooled analysis of 3-year phase III trials. Br. J. Ophthalmol. 2016, 100, 796–801. [Google Scholar] [CrossRef]
- Maturi, R.K.; Pollack, A.; Uy, H.S.; Varano, M.; Gomes, A.M.V.; Li, X.Y.; Cui, H.; Lou, J.; Hashad, Y.; Whitcup, S.M. Intraocular pressure in patients with diabetic macular edema treated with dexamethasone intravitreal implant in the 3-year mead study. Retina 2016, 36, 1143–1152. [Google Scholar] [CrossRef]
- Augustin, A.J.; Kuppermann, B.D.; Lanzetta, P.; Loewenstein, A.; Li, X.Y.; Cui, H.; Hashad, Y.; Whitcup, S.M.; Abujamra, S.; Acton, J.; et al. Dexamethasone intravitreal implant in previously treated patients with diabetic macular edema: Subgroup analysis of the MEAD study. BMC Ophthalmol. 2015, 15, 150. [Google Scholar] [CrossRef] [PubMed]
- Mastropasqua, R.; Toto, L.; Borrelli, E.; Di Antonio, L.; De Nicola, C.; Mastrocola, A.; Di Nicola, M.; Carpineto, P. Morphology and function over a one-year follow up period after intravitreal dexamethasone implant (Ozurdex) in patients with diabetic macular edema. PLoS ONE 2015, 10, e0145663. [Google Scholar] [CrossRef] [PubMed]
- Sarao, V.; Veritti, D.; Furino, C.; Giancipoli, E.; Alessio, G.; Boscia, F.; Lanzetta, P. Dexamethasone implant with fixed or individualized regimen in the treatment of diabetic macular oedema: Six-month outcomes of the UDBASA study. Acta Ophthalmol. 2017, 95, e255–e260. [Google Scholar] [CrossRef] [PubMed]
- Lo Giudice, G.; Avarello, A.; Campana, G.; Galan, A. Rapid response to dexamethasone intravitreal implant in diabetic macular edema. Eur. J. Ophthalmol. 2018, 28, 74–79. [Google Scholar] [CrossRef] [PubMed]
- Abdel-Hay, A.; Sivaprasad, S.; Subramanian, A.; Barbur, J.L. Acuity and colour vision changes post intravitreal dexamethasone implant injection in patients with diabetic macular oedema. PLoS ONE 2018, 13, e0199693. [Google Scholar] [CrossRef] [PubMed]
- Gillies, M.C.; Lim, L.L.; Campain, A.; Quin, G.J.; Salem, W.; Li, J.; Goodwin, S.; Aroney, C.; McAllister, I.L.; Fraser-Bell, S. A randomized clinical trial of intravitreal bevacizumab versus intravitreal dexamethasone for diabetic macular edema: The BEVORDEX study. Ophthalmology 2014, 121, 2473–2481. [Google Scholar] [CrossRef]
- Mehta, H.; Fraser-Bell, S.; Yeung, A.; Campain, A.; Lim, L.L.; Quin, G.J.; McAllister, I.L.; Keane, P.A.; Gillies, M.C. Efficacy of dexamethasone versus bevacizumab on regression of hard exudates in diabetic maculopathy: Data from the BEVORDEX randomised clinical trial. Br. J. Ophthalmol. 2016, 100, 1000–1004. [Google Scholar] [CrossRef]
- Aroney, C.; Fraser-Bell, S.; Lamoureux, E.L.; Gillies, M.C.; Lim, L.L.; Fenwick, E.K. Vision-related quality of life outcomes in the BEVORDEX study: A clinical trial comparing ozurdex sustained release dexamethasone intravitreal implant and bevacizumab treatment for diabetic macular edema. Investig. Ophthalmol. Vis. Sci. 2016, 57, 5541–5546. [Google Scholar] [CrossRef]
- Mehta, H.; Fraser-Bell, S.; Nguyen, V.; Lim, L.L.; Gillies, M.C. The Interval between Treatments of Bevacizumab and Dexamethasone Implants for Diabetic Macular Edema Increased over Time in the BEVORDEX Trial. Ophthalmol. Retin. 2018, 2, 231–234. [Google Scholar] [CrossRef]
- Callanan, D.G.; Loewenstein, A.; Patel, S.S.; Massin, P.; Corcóstegui, B.; Li, X.Y.; Jiao, J.; Hashad, Y.; Whitcup, S.M. A multicenter, 12-month randomized study comparing dexamethasone intravitreal implant with ranibizumab in patients with diabetic macular edema. Graefe’s Arch. Clin. Exp. Ophthalmol. 2017, 255, 463–473. [Google Scholar] [CrossRef]
- Lazic, R.; Lukic, M.; Boras, I.; Draca, N.; Vlasic, M.; Gabric, N.; Tomic, Z. Treatment of anti-vascular endothelial growth factor-resistant diabetic macular edema with dexamethasone intravitreal implant. Retina 2014, 34, 719–724. [Google Scholar] [CrossRef] [PubMed]
- Busch, C.; Zur, D.; Fraser-Bell, S.; Laíns, I.; Santos, A.R.; Lupidi, M.; Cagini, C.; Gabrielle, P.H.; Couturier, A.; Mané-Tauty, V.; et al. Shall we stay, or shall we switch? Continued anti-VEGF therapy versus early switch to dexamethasone implant in refractory diabetic macular edema. Acta Diabetol. 2018, 55, 789–796. [Google Scholar] [CrossRef] [PubMed]
- Busch, C.; Fraser-Bell, S.; Iglicki, M.; Lupidi, M.; Couturier, A.; Chaikitmongkol, V.; Giancipoli, E.; Rodríguez-Valdés, P.J.; Gabrielle, P.H.; Laíns, I.; et al. Real-world outcomes of non-responding diabetic macular edema treated with continued anti-VEGF therapy versus early switch to dexamethasone implant: 2-year results. Acta Diabetol. 2019, 56, 1341–1350. [Google Scholar] [CrossRef] [PubMed]
- Boyer, D.S.; Faber, D.; Gupta, S.; Patel, S.S.; Tabandeh, H.; Li, X.Y.; Liu, C.C.; Lou, J.; Whitcup, S.M. Dexamethasone intravitreal implant for treatment of diabetic macular edema in vitrectomized patients. Retina 2011, 31, 915–923. [Google Scholar] [CrossRef] [PubMed]
- Maturi, R.K.; Bleau, L.; Saunders, J.; Mubasher, M.; Stewart, M.W. A 12-Month, Single-Masked, Randomized Controlled Study of Eyes with Persistent Diabetic Macular Edema after Multiple Anti-Vegf Injections to Assess the Efficacy of the Dexamethasone-Delayed Delivery System as an Adjunct to Bevacizumab Compared with Continued Bevacizumab Monotherapy. Retina 2015, 35, 1604–1614. [Google Scholar] [PubMed]
- Maturi, R.K.; Glassman, A.R.; Liu, D.; Beck, R.W.; Bhavsar, A.R.; Bressler, N.M.; Jampol, L.M.; Melia, M.; Punjabi, O.S.; Salehi-Had, H.; et al. Effect of adding dexamethasone to continued ranibizumab treatment in patients with persistent diabetic macular edema: A DRCR network phase 2 randomized clinical trial. JAMA Ophthalmol. 2018, 136, 29–38. [Google Scholar] [CrossRef] [PubMed]
- Callanan, D.G.; Gupta, S.; Boyer, D.S.; Ciulla, T.A.; Singer, M.A.; Kuppermann, B.D.; Liu, C.C.; Li, X.Y.; Hollander, D.A.; Schiffman, R.M.; et al. Dexamethasone intravitreal implant in combination with laser photocoagulation for the treatment of diffuse diabetic macular edema. Ophthalmology 2013, 120, 1843–1851. [Google Scholar] [CrossRef]
- Podkowinski, D.; Orlowski-Wimmer, E.; Zlabinger, G.; Pollreisz, A.; Mursch-Edlmayr, A.S.; Mariacher, S.; Ring, M.; Bolz, M. Aqueous humour cytokine changes during a loading phase of intravitreal ranibizumab or dexamethasone implant in diabetic macular oedema. Acta Ophthalmol. 2020, 98, e407–e415. [Google Scholar] [CrossRef]
- Borrelli, E.; Sarraf, D.; Freund, K.B.; Sadda, S.R. OCT angiography and evaluation of the choroid and choroidal vascular disorders. Prog. Retin. Eye Res. 2018, 67, 30–55. [Google Scholar] [CrossRef]
- Ferris, F.L.; Wilkinson, C.P.; Bird, A.; Chakravarthy, U.; Chew, E.; Csaky, K.; Sadda, S.R. Clinical classification of age-related macular degeneration. Ophthalmology 2013, 120, 844–851. [Google Scholar] [CrossRef]
- Kuppermann, B.D.; Goldstein, M.; Maturi, R.K.; Pollack, A.; Singer, M.; Tufail, A.; Weinberger, D.; Li, X.Y.; Liu, C.C.; Lou, J.; et al. Dexamethasone Intravitreal Implant as Adjunctive Therapy to Ranibizumab in Neovascular Age-Related Macular Degeneration: A Multicenter Randomized Controlled Trial. Ophthalmologica 2015, 234, 40–54. [Google Scholar] [CrossRef]
- Chaudhary, V.; Barbosa, J.; Lam, W.C.; Mak, M.; Mavrikakis, E.; Mohaghegh, P.S.M. Ozurdex in age-related macular degeneration as adjunct to ranibizumab (The OARA Study). Can. J. Ophthalmol. 2016, 51, 302–305. [Google Scholar] [CrossRef] [PubMed]
- Rezar-Dreindl, S.; Sacu, S.; Eibenberger, K.; Pollreisz, A.; Bühl, W.; Georgopoulos, M.; Krall, C.; Weigert, G.; Schmidt-Erfurth, U. The intraocular cytokine profile and therapeutic response in persistent neovascular age-related macular degeneration. Investig. Ophthalmol. Vis. Sci. 2016, 57, 4144–4150. [Google Scholar] [CrossRef] [PubMed]
- Rezar-Dreindl, S.; Eibenberger, K.; Buehl, W.; Georgopoulos, M.; Weigert, G.; Krall, C.; Dunavoelgyi, R.; Schmidt-Erfurth, U.; Sacu, S. Role of additional dexamethasone for the management of persistent or recurrent neovascular agerelated macular degeneration under ranibizumab treatment. Retina 2017, 37, 962–970. [Google Scholar] [CrossRef] [PubMed]
- Giancipoli, E.; Pinna, A.; Boscia, F.; Zasa, G.; Sotgiu, G.; Dore, S.; D’Amico Ricci, G. Intravitreal Dexamethasone in Patients with Wet Age-Related Macular Degeneration Resistant to Anti-VEGF: A Prospective Pilot Study. J. Ophthalmol. 2018, 2018, 5612342. [Google Scholar] [CrossRef] [PubMed]
- Kaya, C.; Zandi, S.; Pfister, I.B.; Gerhardt, C.; Garweg, J.G. Adding a corticosteroid or switching to another anti-VEGF in insufficiently responsive wet age-related macular degeneration. Clin. Ophthalmol. 2019, 13, 2403–2409. [Google Scholar] [CrossRef]
- Calvo, P.; Ferreras, A.; Al Adel, F.; Wang, Y.; Brent, M.H. Dexamethasone intravitreal implant as adjunct therapy for patients with wet age-related macular degeneration with incomplete response to ranibizumab. Br. J. Ophthalmol. 2015, 99, 723–726. [Google Scholar] [CrossRef]
- Querques, G.; Rosenfeld, P.J.P.J.; Cavallero, E.; Borrelli, E.; Corvi, F.; Querques, L.; Bandello, F.M.F.M.; Zarbin, M.A.M.A. Treatment of dry age-related macular degeneration. Ophthalmic Res. 2014, 52, 107–115. [Google Scholar] [CrossRef]
- Chung, H.; Hwang, J.-U.; Kim, J.-G.; Yoon, Y.H. Optical coherence tomography in the diagnosis and monitoring of cystoid macular edema in patients with retinitis pigmentosa. Retina 2006, 26, 922–927. [Google Scholar] [CrossRef]
- Iovino, C.; Au, A.; Hilely, A.; Violanti, S.; Peiretti, E.; Gorin, M.B.; Sarraf, D. Evaluation of the Choroid in Eyes with Retinitis Pigmentosa and Cystoid Macular Edema. Investig. Opthalmology Vis. Sci. 2019, 60, 5000. [Google Scholar] [CrossRef]
- Srour, M.; Querques, G.; Leveziel, N.; Zerbib, J.; Tilleul, J.; Boulanger-Scemama, E.; Souied, E.H. Intravitreal dexamethasone implant (Ozurdex) for macular edema secondary to retinitis pigmentosa. Graefe’s Arch. Clin. Exp. Ophthalmol. 2013, 251, 1501–1506. [Google Scholar] [CrossRef] [PubMed]
- Ahn, S.J.; Kim, K.E.; Woo, S.J.; Park, K.H. The effect of an intravitreal dexamethasone implant for cystoid macular edema in retinitis pigmentosa: A case report and literature review. Ophthalmic Surg. Lasers Imaging Retin. 2014, 45, 160–164. [Google Scholar] [CrossRef] [PubMed]
- Örnek, N.; Örnek, K.; Erbahçeci, İ.E. Intravitreal dexamethasone implant (Ozurdex) for refractory macular edema secondary to retinitis pigmentosa. Turk Oftalmoloiji Derg. 2016, 46, 179–181. [Google Scholar] [CrossRef] [PubMed]
- Saatci, A.O.; Selver, O.B.; Seymenoglu, G.; Yaman, A. Bilateral Intravitreal Dexamethasone Implant for Retinitis Pigmentosa-Related Macular Edema. Case Rep. Ophthalmol. 2013, 4, 53–58. [Google Scholar] [CrossRef]
- Mansour, A.M.; Sheheitli, H.; Kucukerdonmez, C.; Sisk, R.A.; Moura, R.; Moschos, M.M.; Lima, L.H.; Al-Shaar, L.; Arevalo, J.F.; Maia, M.; et al. Intravitreal Dexamethasone Implant in Retinitis Pigmentosa-related Cystoid Macular Edema. Retina 2018, 38, 416–423. [Google Scholar] [CrossRef]
- Park, U.C.; Park, J.H.; Ma, D.J.; Cho, I.H.; Oh, B.-L.; Yu, H.G. A randomized paired-eye trial of intravitreal dexamethasone implant for cystoid macular edema in retinitis pigmentosa. Retina 2020, 40, 1359–1366. [Google Scholar] [CrossRef]
- Veritti, D.; Sarao, V.; De Nadai, K.; Chizzolini, M.; Parmeggiani, F.; Perissin, L.; Lanzetta, P. Dexamethasone Implant Produces Better Outcomes than Oral Acetazolamide in Patients with Cystoid Macular Edema Secondary to Retinitis Pigmentosa. J. Ocul. Pharmacol. Ther. 2020, 36, 190–197. [Google Scholar] [CrossRef]
- Fonollosa, A.; Llorenç, V.; Artaraz, J.; Jimenez, B.; Ruiz-Arruza, I.; Agirrebengoa, K.; Cordero-Coma, M.; Costales-Mier, F.; Adan, A. Safety and efficacy of intravitreal dexamethasone implants in the management of macular edema secondary to infectious uveitis. Retina 2016, 36, 1778–1785. [Google Scholar] [CrossRef]
- Agarwal, A.; Handa, S.; Aggarwal, K.; Sharma, M.; Singh, R.; Sharma, A.; Agrawal, R.; Sharma, K.; Gupta, V. The Role of Dexamethasone Implant in the Management of Tubercular Uveitis. Ocul. Immunol. Inflamm. 2018, 26, 884–892. [Google Scholar] [CrossRef]
- Jain, L.; Panda, K.G.; Basu, S. Clinical Outcomes of Adjunctive Sustained-Release Intravitreal Dexamethasone Implants in Tuberculosis-Associated Multifocal Serpigenoid Choroiditis. Ocul. Immunol. Inflamm. 2018, 26, 877–883. [Google Scholar] [CrossRef]
- Lautredou, C.C.; Hardin, J.S.; Chancellor, J.R.; Uwaydat, S.H.; Ellabban, A.A.; Sallam, A.B. Repeat Intravitreal Dexamethasone Implant for Refractory Cystoid Macular Edema in Syphilitic Uveitis. Case Rep. Ophthalmol. Med. 2018, 2018, 7419823. [Google Scholar] [CrossRef] [PubMed]
- Dutta Majumder, P.; Mayilvakanam, L.; Palker, A.; Sridharan, S.; Biswas, J. Intravitreal sustained-release dexamethasone implant for the treatment of persistent cystoid macular edema in ocular syphilis. Indian J. Ophthalmol. 2019, 67, 1487–1490. [Google Scholar] [PubMed]
- Majumder, P.D.; Biswas, J.; Ambreen, A.; Amin, R.; Pannu, Z.R.; Bedda, A.M. Intravitreal dexamethasone implant for the treatment of cystoid macular oedema associated with acute retinal necrosis. J. Ophthalmic Inflamm. Infect. 2016, 6, 49. [Google Scholar] [CrossRef] [PubMed]
- Seibel, I.; Hager, A.; Riechardt, A.I.; Davids, A.M.; Böker, A.; Joussen, A.M. Antiangiogenic or Corticosteroid Treatment in Patients with Radiation Maculopathy after Proton Beam Therapy for Uveal Melanoma. Am. J. Ophthalmol. 2016, 168, 31–39. [Google Scholar] [CrossRef]
- Frizziero, L.; Parrozzani, R.; Trainiti, S.; Pilotto, E.; Miglionico, G.; Pulze, S.; Midena, E. Intravitreal dexamethasone implant in radiation-induced macular oedema. Br. J. Ophthalmol. 2017, 101, 1699–1703. [Google Scholar] [CrossRef]
- Russo, A.; Reibaldi, M.; Avitabile, T.; Uva, M.G.; Franco, L.M.; Gagliano, C.; Bonfiglio, V.; Spatola, C.; Privitera, G.; Longo, A. Dexamethasone intravitreal implant vs. ranibizumab in the treatment of macular edema secondary to brachytherapy for choroidal melanoma. Retina 2018, 38, 788–794. [Google Scholar] [CrossRef]
- Arrigo, A.; Knutsson, K.A.; Rajabjan, F.; Augustin, V.A.; Bandello, F.; Parodi, M.B. Combined central retinal vein occlusion and branch retinal artery occlusion treated with intravitreal dexamethasone implant: A case report. Eur. J. Ophthalmol. 2020. [Google Scholar] [CrossRef]
- Ozturk, T.; Takes, O.; Saatci, A.O. Dexamethasone implant (ozurdex) in a case with unilateral simultaneous central retinal vein and branch retinal artery occlusion. Case Rep. Ophthalmol. 2015, 6, 76–81. [Google Scholar] [CrossRef]
- Fenicia, V.; Balestrieri, M.; Perdicchi, A.; Maraone, G.; Recupero, S.M. Intravitreal injection of dexamethasone implant in serous macular detachment associated with Waldenström’s disease. Case Rep. Ophthalmol. 2013, 4, 64–69. [Google Scholar] [CrossRef]
- Georgakopoulos, C.D.; Plotas, P.; Angelakis, A.; Kagkelaris, K.; Tzouvara, E.; Makri, O.E. Dexamethasone implant for immunogammopathy maculopathy associated with IgA multiple myeloma. Ther. Adv. Ophthalmol. 2019, 11, 251584141882044. [Google Scholar] [CrossRef]
- Nuzzi, R.; Monteu, F. Use of Intravitreal Dexamethasone in a Case of Anterior Ischemic Optic Neuropathy. Case Rep. Ophthalmol. 2017, 8, 452–458. [Google Scholar] [CrossRef] [PubMed]
- Saatci, A.O.; Ayhan, Z.; Yaman, A.; Bora, E.; Ulgenalp, A.; Kavukcu, S. A 12-Year-Old Girl with Bilateral Coats Disease and ABCA4 Gene Mutation. Case Rep. Ophthalmol. 2018, 9, 375–380. [Google Scholar] [CrossRef] [PubMed]
- Kumar, K.; Raj, P.; Chandnani, N.; Agarwal, A. Intravitreal dexamethasone implant with retinal photocoagulation for adult-onset Coats’ disease. Int. Ophthalmol. 2019, 39, 465–470. [Google Scholar] [CrossRef] [PubMed]
- Cebeci, Z.; Oray, M.; Tuncer, S.; Tugal Tutkun, I.; Kir, N. Intravitreal dexamethasone implant (Ozurdex) and photodynamic therapy for vasoproliferative retinal tumours. Can. J. Ophthalmol. 2014, 49, e83–e84. [Google Scholar] [CrossRef] [PubMed]
- Kong, X.; Psaras, C.; Stewart, J.M. Dexamethasone Intravitreal Implant Injection in Eyes with Comorbid Hypotony. Ophthalmol. Retin. 2019, 3, 993–997. [Google Scholar] [CrossRef] [PubMed]
- Ahn, S.J.; Joung, J.; Lee, S.H.; Lee, B.R. Intravitreal dexamethasone implant therapy for the treatment of cystoid macular Oedema due to hydroxychloroquine retinopathy: A case report and literature review. BMC Ophthalmol. 2018, 18, 310. [Google Scholar] [CrossRef]
- Kim, M.S.; Hong, H.K.; Park, K.H.; Woo, S.J. Intravitreal Dexamethasone Implant with Plasma Autoantibody Monitoring for Cancer-associated Retinopathy. Korean J. Ophthalmol. 2019, 33, 298. [Google Scholar] [CrossRef]
- Mukhtar, S.; Potter, S.M.; Khurshid, S.G. Dexamethasone intravitreal implant for X-linked (juvenile) retinoschisis. Retin. Cases Brief Rep. 2019, 13, 18–20. [Google Scholar] [CrossRef]
- Bulut, M.N.; Çalll, Ü.; Göktaş, E.; Bulut, K.; Kandemir, B.; Özertürk, Y. Use of an Intravitreal Dexamethasone Implant (Ozurdex) in a Case with Accidental Foveal Photocoagulation by Alexandrite Laser. Case Rep. Ophthalmol. 2016, 7, 130–134. [Google Scholar] [CrossRef]
- Corbelli, E.; Fasce, F.; Iuliano, L.; Sacconi, R.; Lattanzio, R.; Bandello, F.; Querques, G. Cataract surgery with combined versus deferred intravitreal dexamethasone implant for diabetic macular edema: Long-term outcomes from a real-world setting. Acta Diabetol. 2020. [Google Scholar] [CrossRef]
- Panozzo, G.A.; Gusson, E.; Panozzo, G.; Dalla Mura, G. Dexamethasone intravitreal implant at the time of cataract surgery in eyes with diabetic macular edema. Eur. J. Ophthalmol. 2017, 27, 433–437. [Google Scholar] [CrossRef] [PubMed]
- Furino, C.; Boscia, F.; Niro, A.; Giancipoli, E.; Grassi, M.O.; D’amico Ricci, G.; Blasetti, F.; Reibaldi, M.; Alessio, G. Combined Phacoemulsification and Intravitreal Dexamethasone Implant (Ozurdex®) in Diabetic Patients with Coexisting Cataract and Diabetic Macular Edema. J. Ophthalmol. 2017, 2017, 4896036. [Google Scholar] [CrossRef] [PubMed]
- Ragam, A.P.; Kolomeyer, A.M.; Nayak, N.V.; Chu, D.S. The use of ozurdex (dexamethasone intravitreal implant) during anterior segment surgery in patients with chronic recurrent uveitis. J. Ocul. Pharmacol. Ther. 2015, 31, 344–349. [Google Scholar] [CrossRef] [PubMed]
- Jinagal, J.; Gupta, G.; Agarwal, A.; Aggarwal, K.; Akella, M.; Gupta, V.; Suri, D.; Gupta, A.; Singh, S.; Ram, J. Safety and efficacy of dexamethasone implant along with phacoemulsification and intraocular lens implantation in children with juvenile idiopathic arthritis associated uveitis. Indian J. Ophthalmol. 2019, 67, 69–74. [Google Scholar] [PubMed]
- Giannaccare, G.; Fresina, M.; Pazzaglia, A.; Versura, P. Long-lasting corneal endothelial graft rejection successfully reversed after dexamethasone intravitreal implant. Int. Med. Case Rep. J. 2016, 9, 187–191. [Google Scholar] [CrossRef] [PubMed]
- Vinciguerra, P.; Albé, E.; Vinciguerra, R.; Romano, M.M.; Trazza, S.; Mastropasqua, L.; Epstein, D. Long-term resolution of immunological graft rejection after a dexamethasone intravitreal implant. Cornea 2015, 34, 471–474. [Google Scholar] [CrossRef]
- Pastor, J.C.; Rojas, J.; Pastor-Idoate, S.; Di Lauro, S.; Gonzalez-Buendia, L.; Delgado-Tirado, S. Proliferative vitreoretinopathy: A new concept of disease pathogenesis and practical consequences. Prog. Retin. Eye Res. 2016, 51, 125–155. [Google Scholar] [CrossRef]
- Govetto, A.; Sarraf, D.; Hubschman, J.P.; Tadayoni, R.; Couturier, A.; Chehaibou, I.; Au, A.; Grondin, C.; Virgili, G.; Romano, M.R. Distinctive Mechanisms and Patterns of Exudative Versus Tractional Intraretinal Cystoid Spaces as Seen with Multimodal Imaging. Am. J. Ophthalmol. 2020, 212, 43–56. [Google Scholar] [CrossRef]
- Banerjee, P.J.; Quartilho, A.; Bunce, C.; Xing, W.; Zvobgo, T.M.; Harris, N.; Charteris, D.G. Slow-Release Dexamethasone in Proliferative Vitreoretinopathy: A Prospective, Randomized Controlled Clinical Trial. Ophthalmology 2017, 124, 757–767. [Google Scholar] [CrossRef]
- Iovino, C.; Giannaccare, G.; Pellegrini, M.; Bernabei, F.; Braghiroli, M.; Caporossi, T.; Peiretti, E. Efficacy and safety of combined vitrectomy with intravitreal dexamethasone implant for advanced stage epiretinal membrane. Drug Des. Devel. Ther. 2019, 13, 4107–4114. [Google Scholar] [CrossRef]
- Hostovsky, A.; Muni, R.H.; Eng, K.T.; Mulhall, D.; Leung, C.; Kertes, P.J. Intraoperative Dexamethasone Intravitreal Implant (Ozurdex) in Vitrectomy Surgery for Epiretinal Membrane. Curr. Eye Res. 2019, 45, 737–741. [Google Scholar] [CrossRef] [PubMed]
- Kim, K.T.; Jang, J.W.; Kang, S.W.; Chae, J.B.; Cho, K.; Bae, K. Vitrectomy Combined with Intraoperative Dexamethasone Implant for the Management of Refractory Diabetic Macular Edema. Korean J. Ophthalmol. 2019, 33, 249. [Google Scholar] [CrossRef] [PubMed]
- Cakir, A.; Erden, B.; Bolukbasi, S.; Aydin, A.; Yurttaser Ocak, S.; Maden, G.; Elcioglu, M.N. Comparison of the effect of ranibizumab and dexamethasone implant in diabetic macular edema with concurrent epiretinal membrane. J. Fr. Ophtalmol. 2019, 42, 683–689. [Google Scholar] [CrossRef] [PubMed]
- Jung, Y.H.; Lee, Y. Efficacy of vitrectomy combined with an intraoperative dexamethasone implant in refractory diabetic macular edema. Acta Diabetol. 2019, 56, 691–696. [Google Scholar] [CrossRef]
- Uwaydat, S.H.; Wang, H.; Sallam, A.B. Intraoperative Injection of Intravitreal Dexamethasone Implant Using a Vitrectomy Trocar-Assisted Technique. Retina 2019, 39, S123–S124. [Google Scholar] [CrossRef]
- Miele, A.; Govetto, A.; Fumagalli, C.; Donati, S.; Biagini, I.; Azzolini, C.; Rizzo, S.; Virgili, G. Ocular hypertension and glaucoma following vitrectomy: A systematic review. Retina 2018, 38, 1–8. [Google Scholar] [CrossRef]
- Govetto, A.; Domínguez, R.; Landaluce, M.L.; Álves, M.T.; Lorente, R. Prevalence of open angle glaucoma in vitrectomized eyes: A cross-sectional study. Retina 2014, 34, 1623–1629. [Google Scholar] [CrossRef]
- Pang, J.P.; Son, G.; Yoon, Y.H.; Kim, J.-G.; Lee, J.Y. Combined vitrectomy with intravitreal dexamethasone implant for refractory macular edema secondary to diabetic retinopathy, retinal vein occlusion, and noninfectious posterior uveitis. Retina 2020, 40, 56–65. [Google Scholar] [CrossRef]
- Govetto, A.; Su, D.; Farajzadeh, M.; Megerdichian, A.; Platner, E.; Ducournau, Y.; Virgili, G.; Hubschman, J.P. Microcystoid Macular Changes in Association with Idiopathic Epiretinal Membranes in Eyes With and Without Glaucoma: Clinical Insights. Am. J. Ophthalmol. 2017, 181, 156–165. [Google Scholar] [CrossRef]
- Iglicki, M.; Zur, D.; Fung, A.; Gabrielle, P.H.; Lupidi, M.; Santos, R.; Busch, C.; Rehak, M.; Cebeci, Z.; Charles, M.; et al. TRActional DIabetic reTInal detachment surgery with co-adjuvant intravitreal dexamethasONe implant: The tradition study. Acta Diabetol. 2019, 56, 1141–1147. [Google Scholar] [CrossRef]
- Tunc, M.; Lahey, J.M.; Kearney, J.J.; Lewis, J.M.; Francis, R. Cystoid macular oedema following pneumatic retinopexy vs. scleral buckling. Eye 2007, 21, 831–834. [Google Scholar] [CrossRef] [PubMed]
- Bonfiglio, V.; Fallico, M.R.; Russo, A.; De Grande, V.; Longo, A.; Uva, M.G.; Reibaldi, M.; Avitabile, T. Intravitreal dexamethasone implant for cystoid macular edema and inflammation after scleral buckling. Eur. J. Ophthalmol. 2015, 25, e98–e100. [Google Scholar] [CrossRef] [PubMed]
- Thanos, A.; Todorich, B.; Yonekawa, Y.; Papakostas, T.D.; Khundkar, T.; Eliott, D.; Dass, A.B.; Williams, G.A.; Capone, A.; Faia, L.J.; et al. Dexamethasone intravitreal implant for the treatment of recalcitrant macular edema after rhegmatogenous retinal detachment repair. Retina 2018, 38, 1084–1090. [Google Scholar] [CrossRef] [PubMed]
- Nehmé, A.; Lobenhofer, E.K.; Stamer, W.D.; Edelman, J.L. Glucocorticoids with different chemical structures but similar glucocorticoid receptor potency regulate subsets of common and unique genes in human trabecular meshwork cells. BMC Med. Genomics 2009. [Google Scholar] [CrossRef]
- Rajesh, B.; Zarranz-Ventura, J.; Fung, A.T.; Busch, C.; Sahoo, N.K.; Rodriguez-Valdes, P.J.; Sarao, V.; Mishra, S.K.; Saatci, A.O.; Udaondo Mirete, P.; et al. Safety of 6000 intravitreal dexamethasone implants. Br. J. Ophthalmol. 2019, 104, 39–46. [Google Scholar] [CrossRef]
- Rosenblatt, A.; Udaondo, P.; Cunha-Vaz, J.; Sivaprasad, S.; Bandello, F.; Lanzetta, P.; Kodjikian, L.; Goldstein, M.; Habot-Wilner, Z.; Loewenstein, A.; et al. A Collaborative Retrospective Study on the Efficacy and Safety of Intravitreal Dexamethasone Implant (Ozurdex) in Patients with Diabetic Macular Edema: The European DME Registry Study. Ophthalmology 2020, 127, 377–393. [Google Scholar] [CrossRef]
- Srinivasan, R.; Sharma, U.; George, R.; Raman, R.; Sharma, T. Intraocular pressure changes after dexamethasone implant in patients with glaucoma and steroid responders. Retina 2019, 39, 157–162. [Google Scholar] [CrossRef]
- Sharma, A.; Kuppermann, B.D.; Bandello, F.; Lanzetta, P.; Zur, D.; Park, S.W.; Yu, H.G.; Saravanan, V.R.; Zacharias, L.C.; Barreira, A.K.; et al. Intraocular pressure (IOP) after intravitreal dexamethasone implant (Ozurdex) amongst different geographic populations—GEODEX-IOP study. Eye 2019, 34, 1063–1068. [Google Scholar] [CrossRef]
- Wannamaker, K.W.; Kenny, S.; Das, R.; Mendlovitz, A.; Comstock, J.M.; Chu, E.R.; Bahadorani, S.; Gresores, N.J.; Beck, K.D.; Krambeer, C.J.; et al. The effects of temporary intraocular pressure spikes after intravitreal dexamethasone implantation on the retinal nerve fiber layer. Clin. Ophthalmol. 2019, 13, 1079–1086. [Google Scholar] [CrossRef]
- Ayar, O.; Alpay, A.; Koban, Y.; Akdemir, M.O.; Yazgan, S.; Canturk Ugurbas, S.; Ugurbas, S.H. The Effect of Dexamethasone Intravitreal Implant on Retinal Nerve Fiber Layer in Patients Diagnosed with Branch Retinal Vein Occlusion. Curr. Eye Res. 2017, 42, 1287–1292. [Google Scholar] [CrossRef]
- Rahimy, E.; Khurana, R.N. Anterior segment migration of dexamethasone implant: Risk factors, complications, and management. Curr. Opin. Ophthalmol. 2017, 28, 246–251. [Google Scholar] [CrossRef] [PubMed]
- Röck, D.; Bartz-Schmidt, K.U.; Röck, T. Risk factors for and management of anterior chamber intravitreal dexamethasone implant migration. BMC Ophthalmol. 2019, 19, 120. [Google Scholar] [CrossRef] [PubMed]
- Sherman, T.; Raman, V. Incomplete scleral penetration of dexamethasone (Ozurdex) intravitreal implant. BMJ Case Rep. 2018. [Google Scholar] [CrossRef] [PubMed]
- Fasce, F.; Battaglia Parodi, M.; Knutsson, K.A.; Spinelli, A.; Mauceri, P.; Bolognesi, G.; Bandello, F. Accidental injection of dexamethasone intravitreal implant in the crystalline lens. Acta Ophthalmol. 2014, 92, e330–e331. [Google Scholar] [CrossRef]
- Luaces-Rodríguez, A.; González-Barcia, M.; Blanco-Teijeiro, M.J.; Gil-Martínez, M.; Gonzalez, F.; Gómez-Ulla, F.; Lamas, M.J.; Otero-Espinar, F.J.; Fernández-Ferreiro, A. Review of intraocular pharmacokinetics of anti-infectives commonly used in the treatment of infectious endophthalmitis. Pharmaceutics 2018, 10, 66. [Google Scholar] [CrossRef]
- Kang, Y.K.; Park, H.S.; Park, D.H.; Shin, J.P. Incidence and treatment outcomes of secondary epiretinal membrane following intravitreal injection for diabetic macular edema. Sci. Rep. 2020, 10, 528. [Google Scholar] [CrossRef]
- Kucukevcilioglu, M.; Eren, M.; Yolcu, U.; Sobaci, G. Acute retinal necrosis following intravitreal dexamethasone (Ozurdex®) implant. Arq. Bras. Oftalmol. 2015, 78, 118–119. [Google Scholar] [CrossRef]
- Thrane, A.S.; Hove, M.; Kjersem, B.; Krohn, J. Acute retinal necrosis and ocular neovascularization caused by cytomegalovirus following intravitreal dexamethasone implant (Ozurdex®) in an immunocompetent patient. Acta Ophthalmol. 2016, 94, e813–e814. [Google Scholar] [CrossRef]
- Uwaydat, S.H.; Sallam, A.B.; Wang, H.; Goyal, S. Retinal indentation by a dexamethasone implant in a gas-filled eye: Report of an unusual complication. JAMA Ophthalmol. 2017, 135, 1125–1127. [Google Scholar] [CrossRef]
- Agrawal, R.; Fernandez-Sanz, G.; Bala, S.; Addison, P.K.F. Desegmentation of Ozurdex implant in vitreous cavity: Report of two cases. Br. J. Ophthalmol. 2014, 98, 961–963. [Google Scholar] [CrossRef]
- Danan, J.; Heitz, A.; Bourcier, T. Periorbital necrotizing fasciitis following dexamethasone intravitreal implant injection. JAMA Ophthalmol. 2016, 134, 110–111. [Google Scholar] [CrossRef] [PubMed]
- Polizzi, S.; Mahajan, V.B. Intravitreal Anti-VEGF Injections in Pregnancy: Case Series and Review of Literature. J. Ocul. Pharmacol. Ther. 2015, 31, 605–610. [Google Scholar] [CrossRef] [PubMed]
- Capuano, V.; Serra, R.; Oubraham, H.; Zambrowski, O.; Amana, D.; Zerbib, J.; Souied, E.H.; Querques, G. Dexamethasone intravitreal implant for choroidal neovascularization during pregnancy. Retin. Cases Brief Rep. 2019, 13, 300–307. [Google Scholar] [CrossRef] [PubMed]
- Concillado, M.; Lund-Andersen, H.; Mathiesen, E.R.; Larsen, M. Dexamethasone Intravitreal Implant for Diabetic Macular Edema during Pregnancy. Am. J. Ophthalmol. 2016, 165, 7–15. [Google Scholar] [CrossRef] [PubMed]
- Hodzic-Hadzibegovic, D.; Ba-Ali, S.; Valerius, M.; Lund-Andersen, H. Quantification of fluid resorption from diabetic macular oedema with foveal serous detachment after dexamethasone intravitreal implant (Ozurdex®) in a pregnant diabetic. Acta Ophthalmol. 2017, 95, 324–325. [Google Scholar] [CrossRef] [PubMed]
| Author (Year) | Design | Condition | Eyes (n) | DEX Injections (Time Interval Range) | Follow up (Months) | Main Outcomes | Complications |
|---|---|---|---|---|---|---|---|
| Miserocchi et al. (2017) [68] | Retrospective case series | Serpiginous Choroiditis | 8 | Single (5 eyes), Repeated (3 eyes; 5–8 months) | 18 | Stabilization of serpiginous lesions, Decrease in systemic corticosteroids | Transient IOP increase (3 eyes), Cataract progression (2 eyes) |
| Mora-Cantallops et al. (2019) [72] | Case report | Acute Posterior Multifocal Placoid Pigment Epitheliopathy | 1 | Single | 6 | Stabilization of inflammatory lesions, Increased BCVA | Transient IOP increase |
| Barnes et al. (2018) [71] | Retrospective case series | Acute Zonal Occult Outer Retinopathy | 6 | Single | 14–63 | Stabilization of inflammatory lesions, Increased BCVA | Transient IOP increase, Cataract progression |
| Walsh et al. (2017) [69] | Retrospective case series | Birdshot Chorioretinopathy | 6 | Single (2 eyes), Repeated (4 eyes; 4–6 months) | 12–36 | Stabilization of inflammatory lesions, Reduced macular edema, Increased BCVA | IOP increase (2 eyes) |
| Bajwa et al. (2018) [70] | Retrospective case series | Birdshot Chorioretinopathy | 6 | Single (2 eyes), Repeated (4 eyes; 4–6 months) | 12–36 | Stabilization of the disease (2 eyes), Increased BCVA | IOP increase (2 eyes), Cataract progression (3 eyes) |
| Author (Year) | Design | Clinical Condition | Eyes (n) | DEX Injection | Follow up (Months) | Main Outcomes | Complications |
|---|---|---|---|---|---|---|---|
| Srour (2013) [111] | Retrospective case series | ME in RP | 4 | Single (2 eyes), Repeated (2 eyes, after 3 months) | 6 | Improved BCVA, Reduced CFT | None |
| Ahn (2014) [112] | Case report | ME in RP | 2 | Single | 6 | Improved BCVA, Reduced CFT | None |
| Ornek (2016) [113] | Case report | ME in RP | 2 | Single | 6 | Improved BCVA, Resolution of ME | None |
| Saatci (2013) [114] | Case report | ME in RP | 2 | Repeated after 3 months | 7 | Improved BCVA, Reduced CFT | None |
| Mansour (2018) [115] | Retrospective case series | ME in RP | 45 | Repeated (range 2–14 months) | Variable (15.5 ± 13.0) | Improved BCVA, Reduced CFT | Transient IOP elevation in 20 eyes, Cataract in 7 eyes |
| Author (Year) | Design | Etiology | Eyes (n) | DEX Injections | Follow up (Months) | Main Outcomes | Complications |
|---|---|---|---|---|---|---|---|
| Fonollosa (2016) [118] | Retrospective case series | Herpes simplex virus-type 1, Varicella-Zoster virus, Treponema Pallidum, Brucella Mellitensis, Borrelia Burgdorferi, Toxoplasma Gondii, Cytomegalovirus | 8 | Repeated (except 2 eyes) | 6–31 | Resolved ME, Improved BCVA, No reactivation of infectious disease | Transient IOP increase (1 eye) |
| Agarwal (2018) [119] | Retrospective case series | Mycobacterium tuberculosis | 19 | Single | 3–4 | Decreased ME, vitritis and progression of choroiditis lesions | Transient IOP increase (4 eyes), Cataract progression (2 eyes) |
| Jain (2018) [120] | Retrospective case series | Mycobacterium tuberculosis | 9 | Repeated | 6–24 | Stabilization of inflammatory lesions, Increased BCVA | IOP increase (2 eyes) |
| Lautredou (2018) [121] | Case report | Treponema pallidum and HIV | 1 | Repeated | 15 | Resolved ME, Improved BCVA | None |
| Majumder (2019) [122] | Case report | Treponema pallidum and HIV | 1 | Repeated | 4 | Resolved ME, Improved BCVA | Transient IOP increase |
| Majumder (2016) [123] | Retrospective case series | Herpes Virus | 4 | Repeated | 6–24 | Resolved ME, Improved BCVA, No reactivation of retinitis | None |
| Author (Year) | Design | Clinical Condition | Eyes (n) | DEX Injection | Follow up (Months) | Main Outcomes | Complications |
|---|---|---|---|---|---|---|---|
| Frizziero (2017) [125] | Retrospective case series | Radiation Maculopathy following Iodine-125 brachytherapy | 13 | Single | 6 | Improved BCVA, Reduced CFT | None |
| Russo (2018) [126] | Retrospective case series | Radiation Maculopathy following plaque brachytherapy | 8 | Repeated | 22 | Improved BCVA, Reduced CFT | None |
| Seibel (2016) [124] | Retrospective case series | Radiation Maculopathy following proton beam therapy | 5 | Single | 1 | Stable BCVA in 80% of patients, Reduced CFT | None |
| Arrigo (2020) [127] | Case report | Combined CRVO and branch retinal artery occlusion | 1 | Single | 24 | Recovery of BCVA, Resolution of ME | None |
| Oztrurk (2015) [128] | Case report | Combined CRVO and branch retinal artery occlusion | 1 | Single | 6 | Improved BCVA, Resolution of ME | None |
| Fenicia (2013) [129] | Case report | CRAO associated with Waldenström’s macroglobulinemia | 1 | Single | 6 | Resolution of ME | None |
| Georgakopoulos (2019) [130] | Case report | Bilateral CRAO associated with ImmunoglobulinA multiple myeloma | 2 | Single | 9 | Improved BCVA, Resolution of ME | None |
| Nuzzi (2017) [131] | Case report | Anterior Ischemic Optic Neuropathy | 1 | Single | 1 | Improved BCVA and visual field | None |
| Saatci (2018) [132] | Case report | Coats’ disease | 2 | Single + Photocoagulation | 50 | Improved BCVA, Resolution of ME | None |
| Kumar (2019) [133] | Case report | Coats’ disease | 1 | Single + Photocoagulation | 4 | Improved BCVA, Resolution of ME | None |
| Cebeci (2014) [134] | Case report | Coats’ disease associated with vasoproliferative retinal tumor | 1 | Single + Photodynamic Therapy | 12 | Improved BCVA, Resolution of exudation | Subcapsular cataract |
| Kong (2019) [135] | Retrospective case series | Hypotony | 15 | Repeated | 27 | Increased intraocular pressure | Vitreous hemorrhage |
| Ahn (2018) [136] | Case report | Hydroxychloroquine Retinopathy | 1 | Single | 2 | Improvement of ME | None |
| Kim (2019) [137] | Case report | Cancer-associated retinopathy | 2 | Repeated (every 4 months) | 48 | Preservation of foveal photoreceptors | None |
| Mukhtar (2017) [138] | Case report | Subretinal fluid associated with X-linked retinoschisis | 2 | Single | 6 | Resolution of subretinal fluid | None |
| Bulut (2016) [139] | Case report | Accidental Foveal Photocoagulation by Alexandrite Laser | 1 | Single | 3 | Recovery of BCVA, Resolution of ME | Transient IOP elevation |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Iovino, C.; Mastropasqua, R.; Lupidi, M.; Bacherini, D.; Pellegrini, M.; Bernabei, F.; Borrelli, E.; Sacconi, R.; Carnevali, A.; D’Aloisio, R.; et al. Intravitreal Dexamethasone Implant as a Sustained Release Drug Delivery Device for the Treatment of Ocular Diseases: A Comprehensive Review of the Literature. Pharmaceutics 2020, 12, 703. https://doi.org/10.3390/pharmaceutics12080703
Iovino C, Mastropasqua R, Lupidi M, Bacherini D, Pellegrini M, Bernabei F, Borrelli E, Sacconi R, Carnevali A, D’Aloisio R, et al. Intravitreal Dexamethasone Implant as a Sustained Release Drug Delivery Device for the Treatment of Ocular Diseases: A Comprehensive Review of the Literature. Pharmaceutics. 2020; 12(8):703. https://doi.org/10.3390/pharmaceutics12080703
Chicago/Turabian StyleIovino, Claudio, Rodolfo Mastropasqua, Marco Lupidi, Daniela Bacherini, Marco Pellegrini, Federico Bernabei, Enrico Borrelli, Riccardo Sacconi, Adriano Carnevali, Rossella D’Aloisio, and et al. 2020. "Intravitreal Dexamethasone Implant as a Sustained Release Drug Delivery Device for the Treatment of Ocular Diseases: A Comprehensive Review of the Literature" Pharmaceutics 12, no. 8: 703. https://doi.org/10.3390/pharmaceutics12080703
APA StyleIovino, C., Mastropasqua, R., Lupidi, M., Bacherini, D., Pellegrini, M., Bernabei, F., Borrelli, E., Sacconi, R., Carnevali, A., D’Aloisio, R., Cerquaglia, A., Finocchio, L., Govetto, A., Erba, S., Triolo, G., Di Zazzo, A., Forlini, M., Vagge, A., & Giannaccare, G. (2020). Intravitreal Dexamethasone Implant as a Sustained Release Drug Delivery Device for the Treatment of Ocular Diseases: A Comprehensive Review of the Literature. Pharmaceutics, 12(8), 703. https://doi.org/10.3390/pharmaceutics12080703











