Y-Site Physical Compatibility of Numeta G13E with Drugs Frequently Used at Neonatal Intensive Care
Abstract
1. Introduction
2. Materials and Methods
2.1. Materials
2.2. Selection of Test Materials
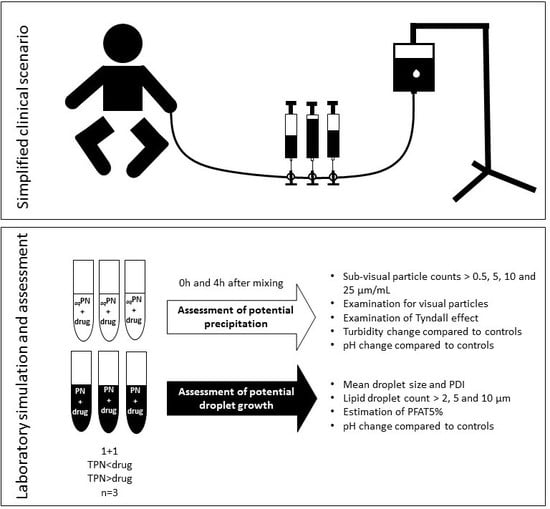
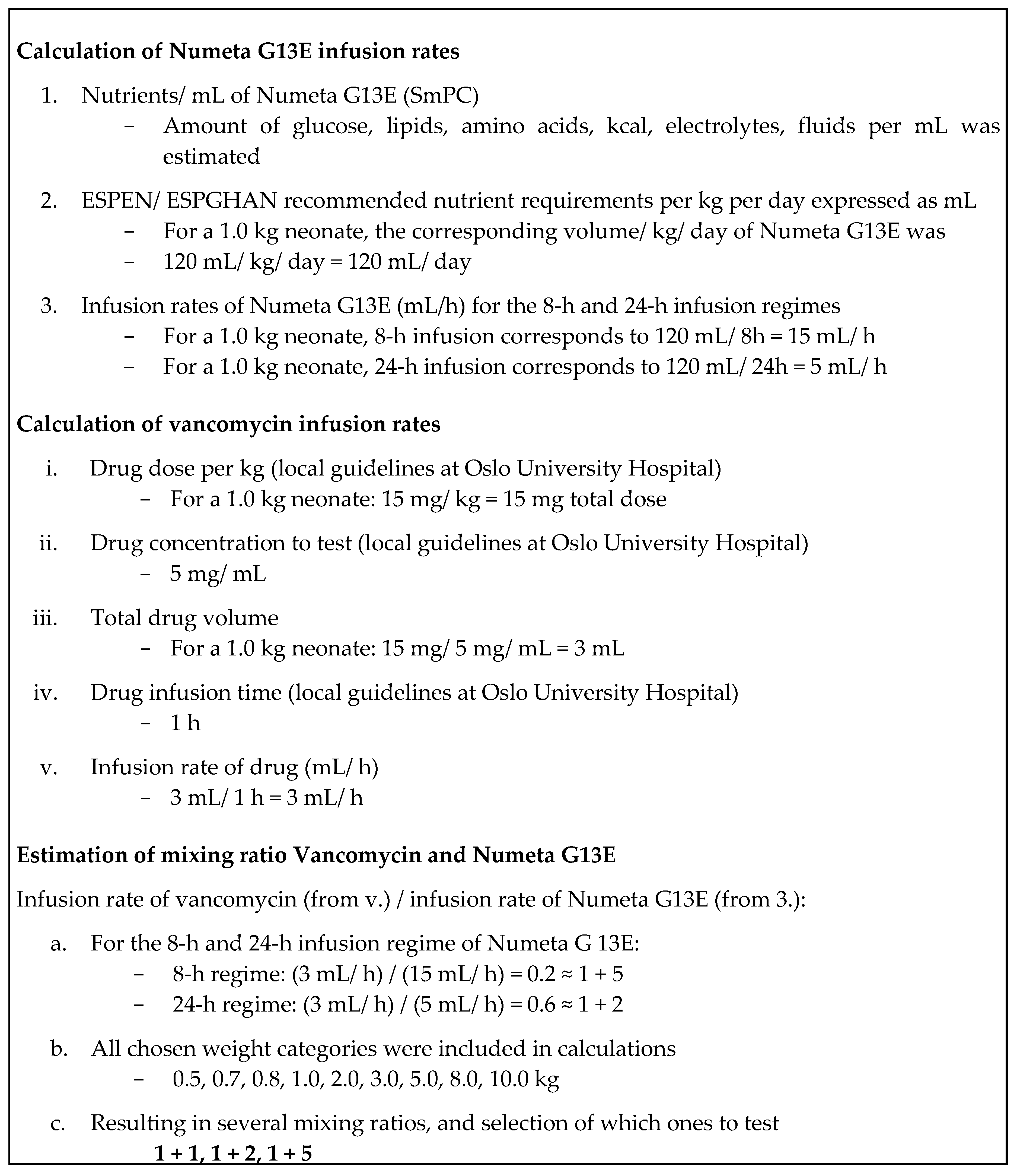
2.3. Study Design
2.4. Sample Preparation
2.5. Analyses
2.5.1. Methods and Assessment Criteria for the Detection of Potential Particle Precipitation
2.5.2. Methods and Assessment Criteria for the Evaluation of Emulsion Stability
3. Results
3.1. Detection of Potential Particle Precipitation
3.2. Evaluation of Emulsion Stability
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- Joosten, K.; Embleton, N.; Yan, W.; Senterre, T. ESPGHAN/ESPEN/ESPR/CSPEN guidelines on pediatric parenteral nutrition: Energy. Clin. Nutr. 2018, 37, 2309–2314. [Google Scholar] [CrossRef] [PubMed]
- Moyses, H.E.; Johnson, M.J.; Leaf, A.A.; Cornelius, V.R. Early parenteral nutrition and growth outcomes in preterm infants: A systematic review and meta-analysis. Am. J. Clin. Nutr. 2013, 97, 816–826. [Google Scholar] [CrossRef] [PubMed]
- Kolacek, S.; Puntis, J.W.L.; Hojsak, I. ESPGHAN/ESPEN/ESPR/CSPEN guidelines on pediatric parenteral nutrition: Venous access. Clin. Nutr. 2018, 37, 2379–2391. [Google Scholar] [CrossRef] [PubMed]
- Jack, T.; Brent, B.E.; Boehne, M.; Muller, M.; Sewald, K.; Braun, A.; Wessel, A.; Sasse, M. Analysis of particulate contaminations of infusion solutions in a pediatric intensive care unit. Intensive Care Med. 2010, 36, 707–711. [Google Scholar] [CrossRef] [PubMed]
- Boehne, M.; Jack, T.; Koditz, H.; Seidemann, K.; Schmidt, F.; Abura, M.; Bertram, H.; Sasse, M. In-line filtration minimizes organ dysfunction: New aspects from a prospective, randomized, controlled trial. BMC Pediatr. 2013, 13, 21. [Google Scholar] [CrossRef] [PubMed]
- Benlabed, M.; Perez, M.; Gaudy, R.; Genay, S.; Lannoy, D.; Barthelemy, C.; Odou, P.; Lebuffe, G.; Decaudin, B. Clinical implications of intravenous drug incompatibilities in critically ill patients. Anaesth. Crit. Care Pain Med. 2019, 38, 173–180. [Google Scholar] [CrossRef] [PubMed]
- Bradley, J.S.; Wassel, R.T.; Lee, L.; Nambiar, S. Intravenous ceftriaxone and calcium in the neonate: Assessing the risk for cardiopulmonary adverse events. Pediatrics 2009, 123, e609–e613. [Google Scholar] [CrossRef] [PubMed]
- European Medicines Agency. Guideline on Pharmaceutical Development of Medicines for Paediatric Use. Available online: https://www.ema.europa.eu/en/documents/scientific-guideline/guideline-pharmaceutical-development-medicines-paediatric-use_en.pdf (accessed on 28 June 2020).
- U.S. Food and Drug Administration. General Clinical Pharmacology Considerations for Neonatal Studies for Drugs and Biological Products Guidance for Industry. Available online: https://www.fda.gov/media/129532/download (accessed on 28 June 2020).
- Staven, V.; Iqbal, H.; Wang, S.; Grønlie, I.; Tho, I. Physical compatibility of Total Parenteral Nutrition (TPN) and drugs in Y-site administration to children from neonates to adolescents. J. Pharm. Pharmacol. 2017, 69, 448–462. [Google Scholar] [CrossRef] [PubMed]
- Staven, V.; Wang, S.; Grønlie, I.; Tho, I. Physical stability of an all-in-one parenteral nutrition admixture for preterm infants upon mixing with micronutrients and drugs. Eur. J. Hosp. Pharm. 2018. [Google Scholar] [CrossRef] [PubMed]
- Fox, L.M.; Wilder, A.G.; Foushee, J.A. Physical compatibility of various drugs with neonatal total parenteral nutrient solution during simulated Y-site administration. Am. J. Health Syst. Pharm. 2013, 70, 520–524. [Google Scholar] [CrossRef] [PubMed]
- Greenhill, K.; Hornsby, E.; Gorman, G. Investigations of Physical Compatibilities of Commonly Used Intravenous Medications with and without Parenteral Nutrition in Pediatric Cardiovascular Intensive Care Unit Patients. Pharm 2019, 12, 67. [Google Scholar] [CrossRef] [PubMed]
- Veltri, M.; Lee, C.K. Compatibility of neonatal parenteral nutrient solutions with selected intravenous drugs. Am. J. Health Syst. Pharm. 1996, 53, 2611–2613. [Google Scholar] [CrossRef] [PubMed]
- Watson, D. Piggyback compatibility of antibiotics with pediatric parenteral nutrition solutions. JPEN J. Parenter. Enter. Nutr. 1985, 9, 220–224. [Google Scholar] [CrossRef] [PubMed]
- European Medicines Agency. Maximum Shelf-Life of Sterile Products. Available online: https://www.ema.europa.eu/en/documents/scientific-guideline/note-guidance-maximum-shelf-life-sterile-products-human-use-after-first-opening-following_en.pdf (accessed on 28 June 2020).
- MÖJLIGA TILLSATSER I NUMETA G13E, G16E och G19E; Baxter: Friendswood, TX, USA, 2019.
- BNF for Children; BMJ Group and Pharmaceutical Press: London, UK, 2016.
- NeoFax; American Society of Hospital Pharmacists: Bethesda, MD, USA, 2019.
- Taketomo, C. Pediatric and Neonatal Dosage Handbook, 25th ed.; Wolters Kluwer: Alphen aan den Rijn, The Netherlands, 2018. [Google Scholar]
- Nasjonalt Kompetansenettverk for Legemidler til Barn. Legemidler til Barn. Available online: https://www.legemidlertilbarn.no/omoss/Sider/About-the-Network.aspx (accessed on 28 June 2020).
- Staven, V.; Wang, S.; Gronlie, I.; Tho, I. Development and evaluation of a test program for Y-site compatibility testing of total parenteral nutrition and intravenous drugs. Nutr. J. 2016, 15, 29. [Google Scholar] [CrossRef] [PubMed]
- SmPC Numeta Baxter. Available online: https://www.legemiddelsok.no/_layouts/15/Preparatomtaler/Spc/15-10661.pdf (accessed on 28 June 2020).
- Particulate Contamination: Sub-Visible Particles. Available online: http://www.uspbpep.com/ep60/2.9.19.%20particulate%20contamination-%20sub-visible%20particles%2020919e.pdf (accessed on 28 June 2020).
- Hall, M.; Noble, A.; Smith, S. (Eds.) A Foundation for Neonatal Care: A Multi-disciplinary Guide; Radcliffe Publishing: Abingdon, Oxon, UK, 2009. [Google Scholar]
- Staven, V.; Waaseth, M.; Wang, S.; Gronlie, I.; Tho, I. Utilization of the tyndall effect for enhanced visual detection of particles in compatibility testing of intravenous fluids: Validity and reliability. PDA J. Pharm. Sci. Technol. 2015, 69, 270–283. [Google Scholar] [CrossRef] [PubMed]
- Newton, D.W.; Driscoll, D.F. Calcium and phosphate compatibility: Revisited again. Am. J. Health Syst. Pharm. 2008, 65, 73–80. [Google Scholar] [CrossRef] [PubMed]
- Globule Size Distribution in Lipid Injectable Emulsions. Available online: https://www.drugfuture.com/Pharmacopoeia/USP32/pub/data/v32270/usp32nf27s0_c729.html (accessed on 28 June 2020).
- Driscoll, D.F.; Bhargava, H.N.; Li, L.; Zaim, R.H.; Babayan, V.K.; Bistrian, B.R. Physicochemical stability of total nutrient admixtures. Am. J. Health Syst. Pharm. 1995, 52, 623–634. [Google Scholar] [CrossRef] [PubMed]
- PhEur. The European Pharmacopoeia; The European Pharmacopoeia Commission: Strasbourg, France, 2016. [Google Scholar]
- Medicines Complete. Clarke’s Analysis of Drugs and Poisons. Available online: https://www.medicinescomplete.com/#/search/all/Clarke%E2%80%99s%20Analysis%20of%20Drugs%20and%20Poisons?offset=0 (accessed on 28 June 2020).
- Roy, S.D.; Flynn, G.L. Solubility behavior of narcotic analgesics in aqueous media: Solubilities and dissociation constants of morphine, fentanyl, and sufentanil. Pharm. Res. 1989, 6, 147–151. [Google Scholar] [CrossRef] [PubMed]
| Product Type | Name | Manufacturer | Lot no. |
|---|---|---|---|
| Three-in-one PN admixture | Numeta G13E | Baxter | 17E15N44 16K22N40 |
| Trace elements | Peditrace | Fresenius Kabi | 12LBL19 12LFL99 |
| Vitamins—water soluble | Soluvit | Fresenius Kabi | 10LF1840 10LK6141 |
| Vitamins—lipid soluble | Vitalipid Infant | Fresenius Kabi | 10LA5346 10LH3632 |
| Drug | Manufacturer | Lot no. | Dilution Medium | Concentration after Dilution |
|---|---|---|---|---|
| Paracetamol Excipients: mannitol, sodium citrate trihydrate, glacial acetic acid, aqua purificata pH: 4.5–5.5 | B.Braun | 17233450 | Undiluted | 10 mg/mL |
| Vancomycin Excipients: none pH: not stated | MIP | 2725616 | Glucose 50 mg/mL | 5 mg/mL |
| Fentanyl Excipients: sodium chloride, hydrochloric acid/sodium hydroxide, aqua purificata pH: 5.0–7.5 | Hameln | 07400817A | Glucose 50 mg/mL | 10 μg/mL |
| Drug | Selected Mixing Ratio Drug + Numeta G13E+ |
|---|---|
| Paracetamol | 1 + 1, 1 + 10, 3 + 2 |
| Vancomycin | 1 + 1, 1 + 2, 1 + 5 |
| Fentanyl | 1 + 1, 1 + 10, 1 + 20 |
| Component (Amount) | Numeta G13E+ | aqNumeta G13E+ |
|---|---|---|
| Olive oil (80%) (g) | 17.4 | - |
| Soy bean oil a (20%) (g) | 13.0 | - |
| Glucose monohydrate (g) | 127.5 | 139.7 |
| Alanine (g) | 2.2 | 2.4 |
| Arginine (g) | 2.3 | 2.5 |
| Aspartic acid (g) | 1.6 | 1.8 |
| Cysteine (g) | 0.5 | 0.6 |
| Glutamic acid (g) | 2.7 | 3.0 |
| Glycine (g) | 1.1 | 1.2 |
| Histidine (g) | 1.0 | 1.1 |
| Isoleucine (g) | 1.8 | 2.0 |
| Leucine (g) | 2.7 | 3.0 |
| Lysine (g) | 3.0 | 3.3 |
| Methionine (g) | 0.6 | 0.7 |
| Ornithine (g) | 0.7 | 0.7 |
| Phenylalanine (g) | 1.1 | 1.2 |
| Proline (g) | 0.8 | 0.9 |
| Serine(g) | 1.1 | 1.2 |
| Taurine (g) | 0.2 | 0.2 |
| Threonine (g) | 1.0 | 1.1 |
| Tryptophan (g) | 0.6 | 0.6 |
| Tyrosine (g) | 0.2 | 0.2 |
| Valine (g) | 2.1 | 2.3 |
| Sodium (mmol) | 19.1 | 21.0 |
| Potassium (mmol) | 18.0 | 19.7 |
| Magnesium (mmol) | 1.4 | 1.5 |
| Calcium b (mmol) | 11.0 | 12.1 |
| Phosphate c (mmol) | 11.0 | 12.1 |
| Acetate (mmol) | 20.9 | 22.9 |
| Chloride (mmol) | 27.4 | 29.5 |
| Malate (mmol) | 9.3 | 10.2 |
| Zinc (mg) | 10.0 | 11.9 |
| Copper (mg) | 0.9 | 1.0 |
| Manganese (mg) | 0.04 | 0.05 |
| Selenium (mg) | 0.1 | 0.1 |
| Fluoride (mg) | 2.5 | 2.7 |
| Iodide (mg) | 0.04 | 0.05 |
| Thiamine mononitrate (mg) | 27.0 | - |
| Riboflavin sodium phosphate (mg) | 42.6 | - |
| Nicotinamide (mg) | 347.8 | - |
| Pyridoxine hydrochloride (mg) | 42.6 | - |
| Sodium pantothenate (mg) | 143.5 | - |
| Sodium ascorbate (mg) | 982.6 | - |
| Biotin (mg) | 0.5 | - |
| Folic acid (mg) | 3.5 | - |
| Cyanocobalamine (mg) | 0.04 | - |
| α-Tocopherol (mg) | 55.7 | - |
| Retinol (mg) | 6.0 | - |
| Phytomenadione (mg) | 1.7 | - |
| Ergocholecalciferol (mg) | 0.1 | - |
| Control | Particles/mL ≥ 0.5 μm | Turbidity (FNU) | Visible Particles or Tyndall Effect (+/−) | pH | ||||
|---|---|---|---|---|---|---|---|---|
| 0 h | 4 h | 0 h | 4 h | 0 h | 4 h | 0 h | 4 h | |
| aqNumeta G13E+ | 12 ± 5 | 25 ± 32 | 0.02 | 0.05 | + | + | 5.40 | 5.39 |
| Paracetamol | 9 ± 2 | 12 ± 9 | 0.03 | 0.01 | − | − | 5.24 | 5.23 |
| Vancomycin | 15 ± 9 | 8 ± 3 | 0.02 | 0.06 | + | + | 3.20 | 3.19 |
| Fentanyl | N/A 1 | N/A 1 | 0.16 | N/A 1 | − | − | 4.81 | N/A 1 |
| Drug | Mix Ratio | Particles/mL ≥ 0.5 μm | Turbidity (FNU) | Visible Particles or Tyndall Effect (+/−) | pH | ||||
|---|---|---|---|---|---|---|---|---|---|
| 0 h | 4 h | 0 h | 4 h | 0 h | 4 h | 0 h | 4 h | ||
| Paracetamol | 1 + 1 | 52 ± 26 | 78 ± 31 | 0.01 ± 0.01 | 0.01 ± 0.01 | − | + | 5.45 ± 0.02 | 5.47 ± 0.01 |
| 1 + 10 | 18 ± 7 | 11 ± 2 | 0.08 ± 0.05 | 0.01 ± 0.02 | + | − | 5.45 ± 0.01 | 5.42 ± 0.01 | |
| 3 + 2 | 22 ± 4 | 9 ± 2 | 0.01 ± 0.01 | 0.05 ± 0.03 | + | − | 5.46 ± 0.04 | 5.45 ± 0.01 | |
| Vancomycin | 1 + 1 | 36 ± 37 | 12 ± 5 | 0.00 ± 0.01 | 0.03 ± 0.03 | + | + | 5.41 ± 0.02 | 5.41 ± 0.01 |
| 1 + 2 | 12 ± 2 | 12 ± 1 | 0.01 ± 0.02 | 0.02 ± 0.01 | + | + | 5.39 ± 0.01 | 5.39 ± 0.02 | |
| 1 + 5 | 18 ± 11 | 20 ± 10 | 0.01 ± 0.02 | 0.01 ± 0.01 | − | − | 5.45 ± 0.01 | 5.45 ± 0.01 | |
| Fentanyl | 1 + 1 | 23 ± 3 | 16 ± 4 | 0.12 ± 0.00 | 0.14 ± 0.01 | + | + | 5.52 ± 0.01 | 5.50 ± 0.01 |
| 1 + 10 | 20 ± 14 | 21 ± 5 | 0.19 ± 0.02 | 0.17 ± 0.04 | − | − | 5.39 ± 0.02 | 5.41 ± 0.01 | |
| 1 + 20 | 13 ± 3 | 18 ± 7 | 0.17 ± 0.03 | 0.14 ± 0.01 | + | + | 5.47 ± 0.02 | 5.44 ± 0.01 | |
| Drug | Mix Ratio | Z-Average (nm) | PDI | %PFAT5 | pH | ||
|---|---|---|---|---|---|---|---|
| 0 h | 4 h | 0 h | 4 h | ||||
| Numeta G13E+ | - | 266 ± 1 | 0.12 ± 0.01 | 0.20 ± 0.09 | 0.28 ± 0.08 | 5.50 | 5.50 |
| Paracetamol | 1 + 1 | 236 ± 1 | 0.15 ± 0.02 | 0.24 ± 0.08 | 0.34 ± 0.00 | 5.56 ± 0.04 | 5.54 ± 0.02 |
| 1 + 10 | 240 ± 3 | 0.12 ± 0.01 | 0.24 ± 0.21 | 0.66 ± 0.36 | 5.49 ± 0.03 | 5.50 ± 0.03 | |
| 3 + 2 | 239 ± 1 | 0.12 ± 0.01 | 0.41 ± 0.18 | 0.57 ± 0.41 | 5.50 ± 0.05 | 5.47 ± 0.04 | |
| Vancomycin | 1 + 1 | 241 ± 2 | 0.12 ± 0.04 | 0.49 ± 0.22 | 0.29 ± 0.10 | 5.50 ± 0.02 | 5.49 ± 0.02 |
| 1 + 2 | 238 ± 4 | 0.13 ± 0.02 | 0.16 ± 0.02 | 0.46 ± 0.35 | 5.48 ± 0.01 | 5.47 ± 0.02 | |
| 1 + 5 | 240 ± 1 | 0.12 ± 0.01 | 0.17 ± 0.03 | 0.25 ± 0.05 | 5.52 ± 0.01 | 5.50 ± 0.01 | |
| Fentanyl | 1 + 1 | 241 ± 2 | 0.10 ± 0.00 | 0.16 ± 0.04 | 0.09 ± 0.04 | 5.58 ± 0.03 | 5.59 ± 0.05 |
| 1 + 10 | 240 ± 1 | 0.10 ± 0.01 | 0.13 ± 0.04 | 0.12 ± 0.04 | 5.58 ± 0.10 | 5.54 ± 0.03 | |
| 1 + 20 | 221 ± 1 | 0.12 ± 0.03 | 0.23 ± 0.06 | 0.16 ± 0.03 | 5.53 ± 0.02 | 5.47 ± 0.02 | |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Nezvalova-Henriksen, K.; Nilsson, N.; Østerberg, C.T.; Staven Berge, V.; Tho, I. Y-Site Physical Compatibility of Numeta G13E with Drugs Frequently Used at Neonatal Intensive Care. Pharmaceutics 2020, 12, 677. https://doi.org/10.3390/pharmaceutics12070677
Nezvalova-Henriksen K, Nilsson N, Østerberg CT, Staven Berge V, Tho I. Y-Site Physical Compatibility of Numeta G13E with Drugs Frequently Used at Neonatal Intensive Care. Pharmaceutics. 2020; 12(7):677. https://doi.org/10.3390/pharmaceutics12070677
Chicago/Turabian StyleNezvalova-Henriksen, Katerina, Niklas Nilsson, Camilla Tomine Østerberg, Vigdis Staven Berge, and Ingunn Tho. 2020. "Y-Site Physical Compatibility of Numeta G13E with Drugs Frequently Used at Neonatal Intensive Care" Pharmaceutics 12, no. 7: 677. https://doi.org/10.3390/pharmaceutics12070677
APA StyleNezvalova-Henriksen, K., Nilsson, N., Østerberg, C. T., Staven Berge, V., & Tho, I. (2020). Y-Site Physical Compatibility of Numeta G13E with Drugs Frequently Used at Neonatal Intensive Care. Pharmaceutics, 12(7), 677. https://doi.org/10.3390/pharmaceutics12070677