Formulation and In-Vitro Characterization of Chitosan-Nanoparticles Loaded with the Iron Chelator Deferoxamine Mesylate (DFO)
Abstract
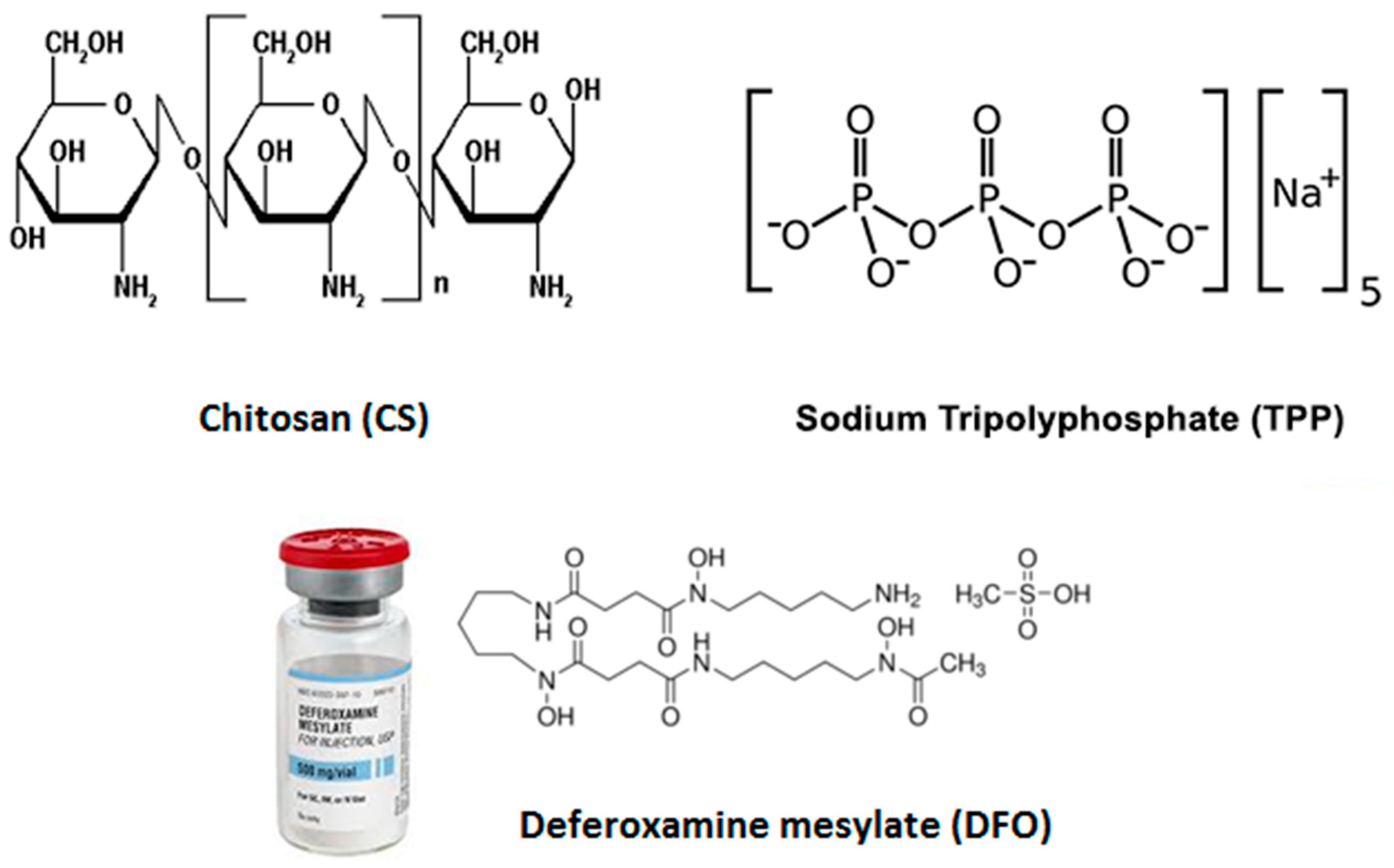
1. Introduction
2. Experimental
2.1. Materials
2.2. Preparation of CS Nanoparticles
2.3. Characterization of CS Nanoparticles
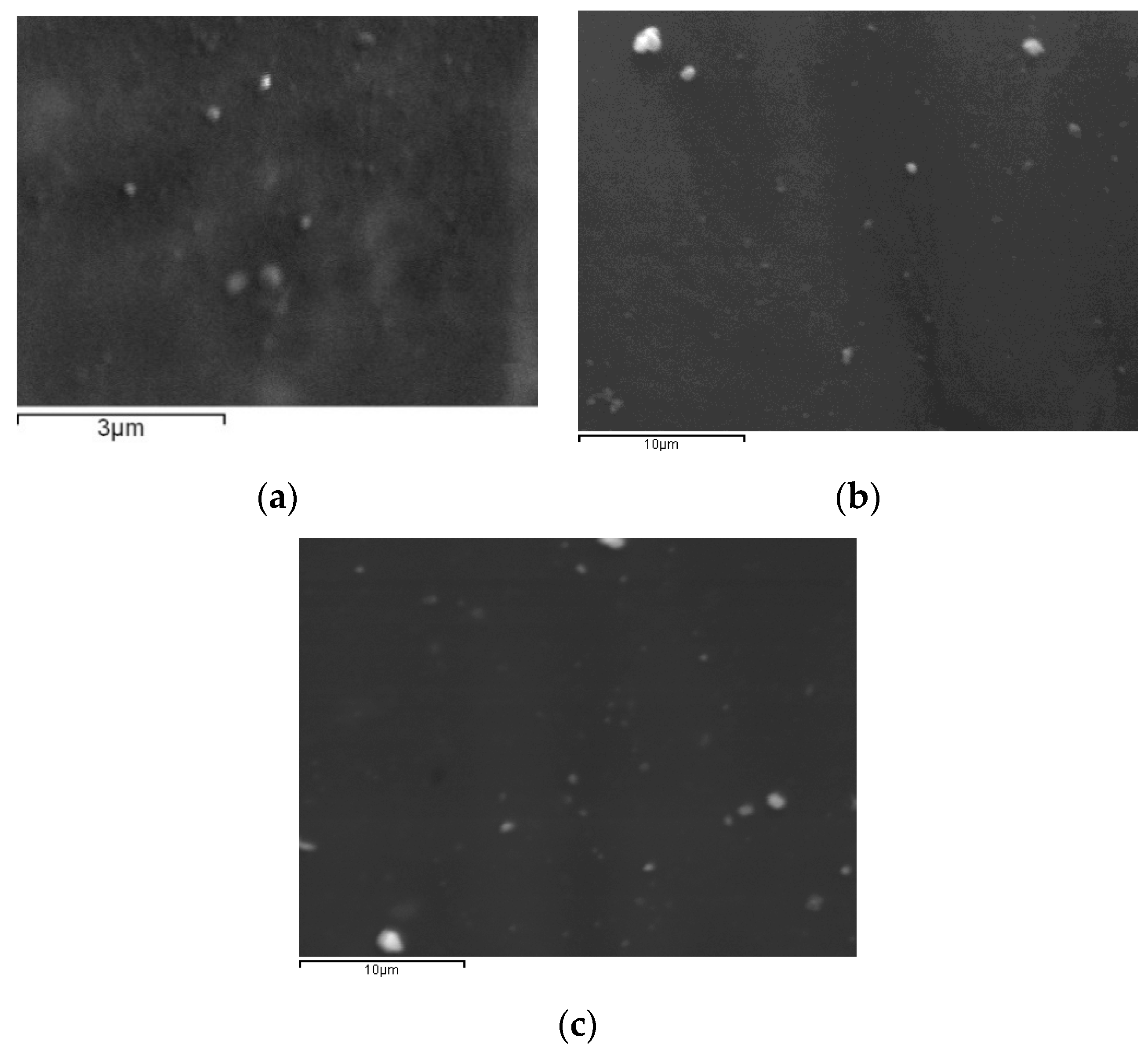
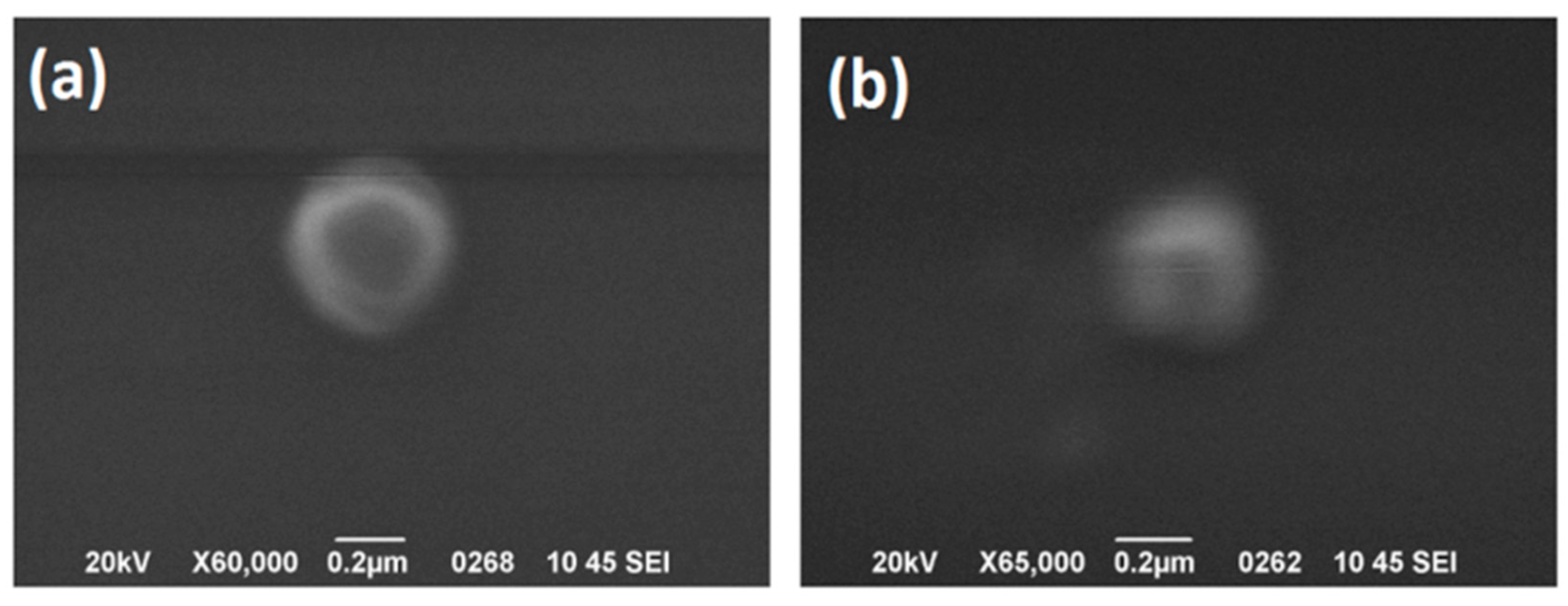
2.3.1. Morphological Characterization of Nanoparticles
2.3.2. Size Measurements of Nanoparticles
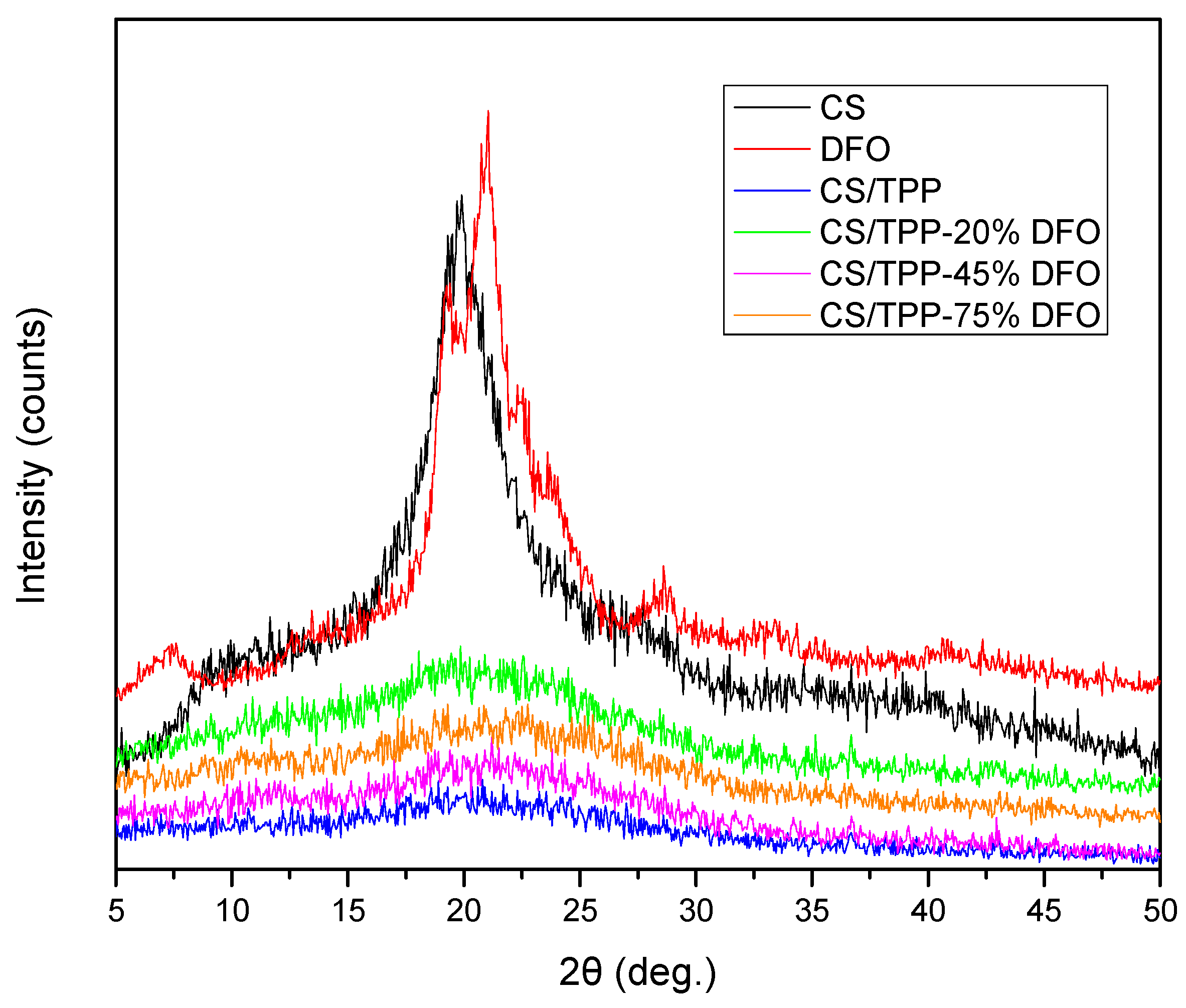
2.3.3. Wide Angle X-ray Diffractometry (WAXD)
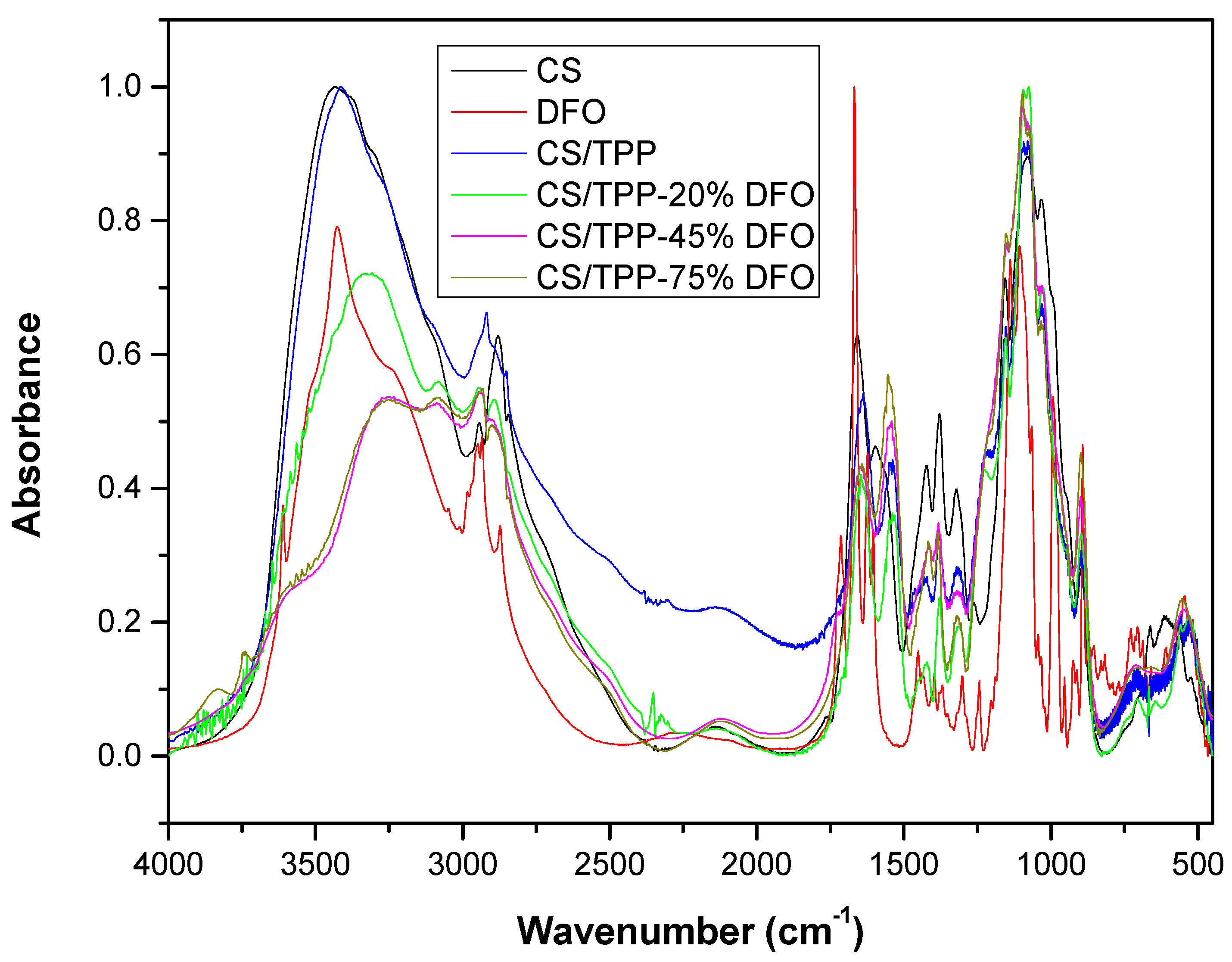
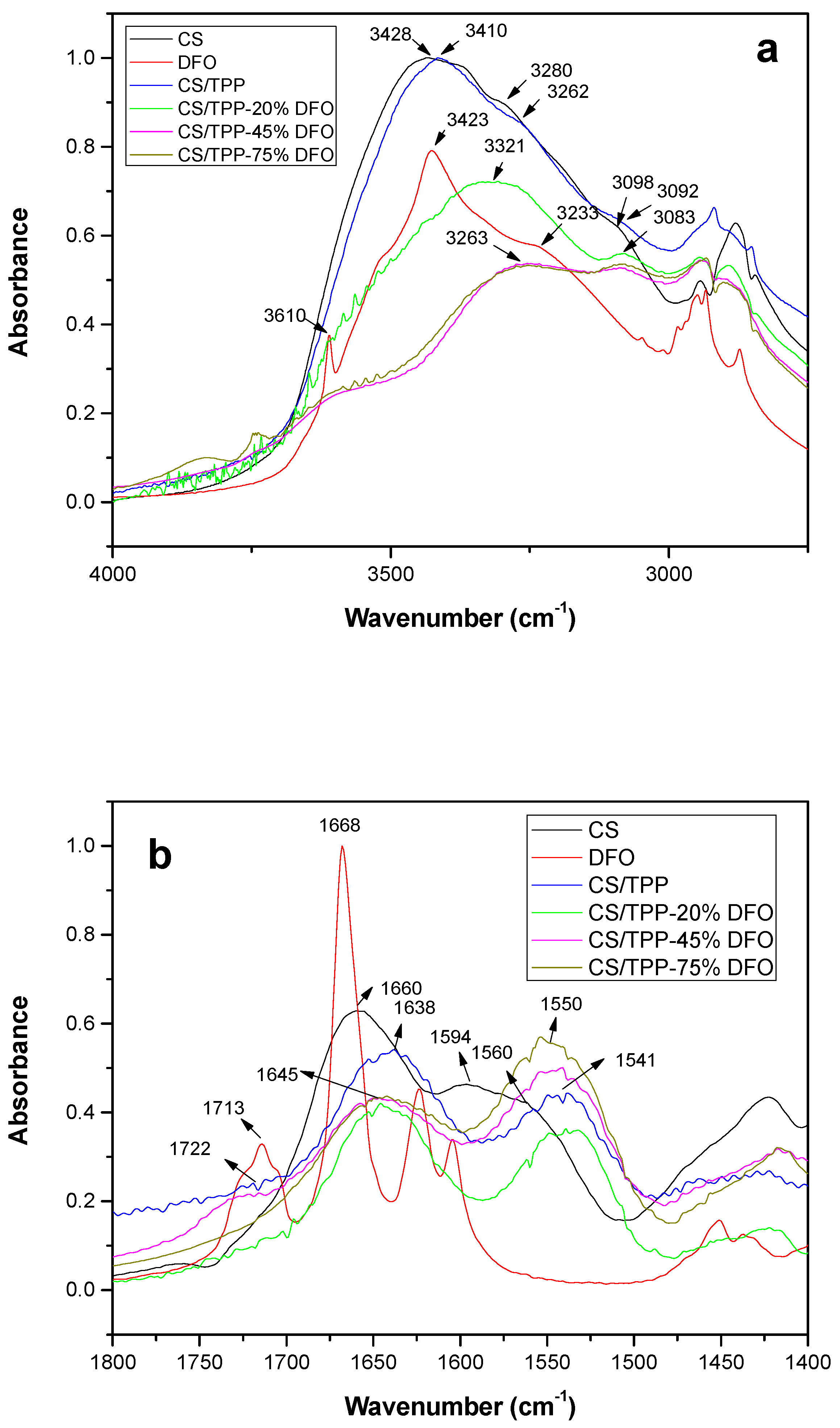
2.3.4. Fourier Transformation-Infrared Spectroscopy (FT-IR)
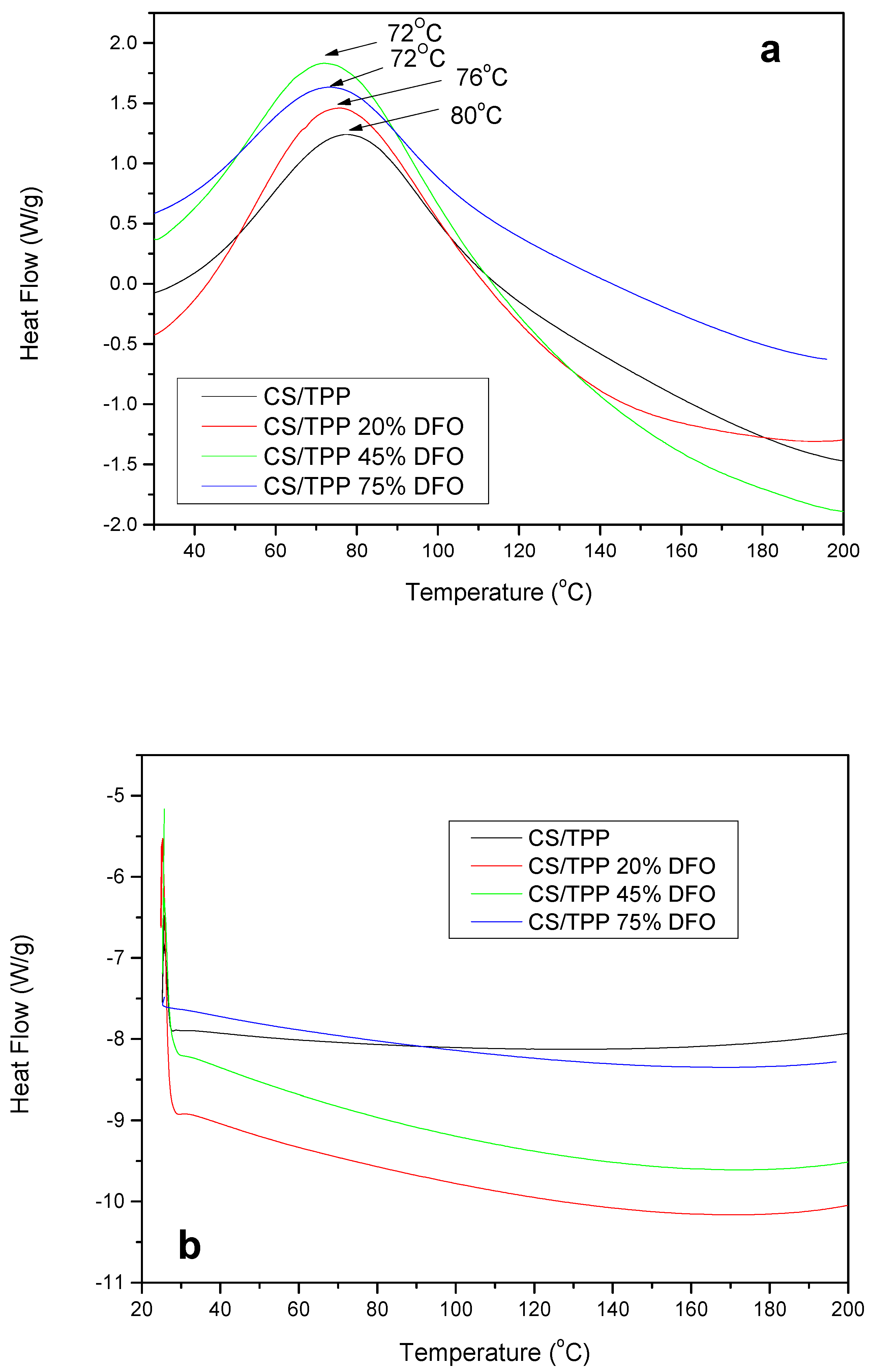
2.3.5. Differential Scanning Calorimeter (DSC)
2.3.6. Evaluation of Drug Encapsulation and Release Rates
2.3.7. Cell Culture
2.3.8. Quantitative Real-Time PCR (qPCR)
2.3.9. Statistical Analysis
3. Results and Discussion
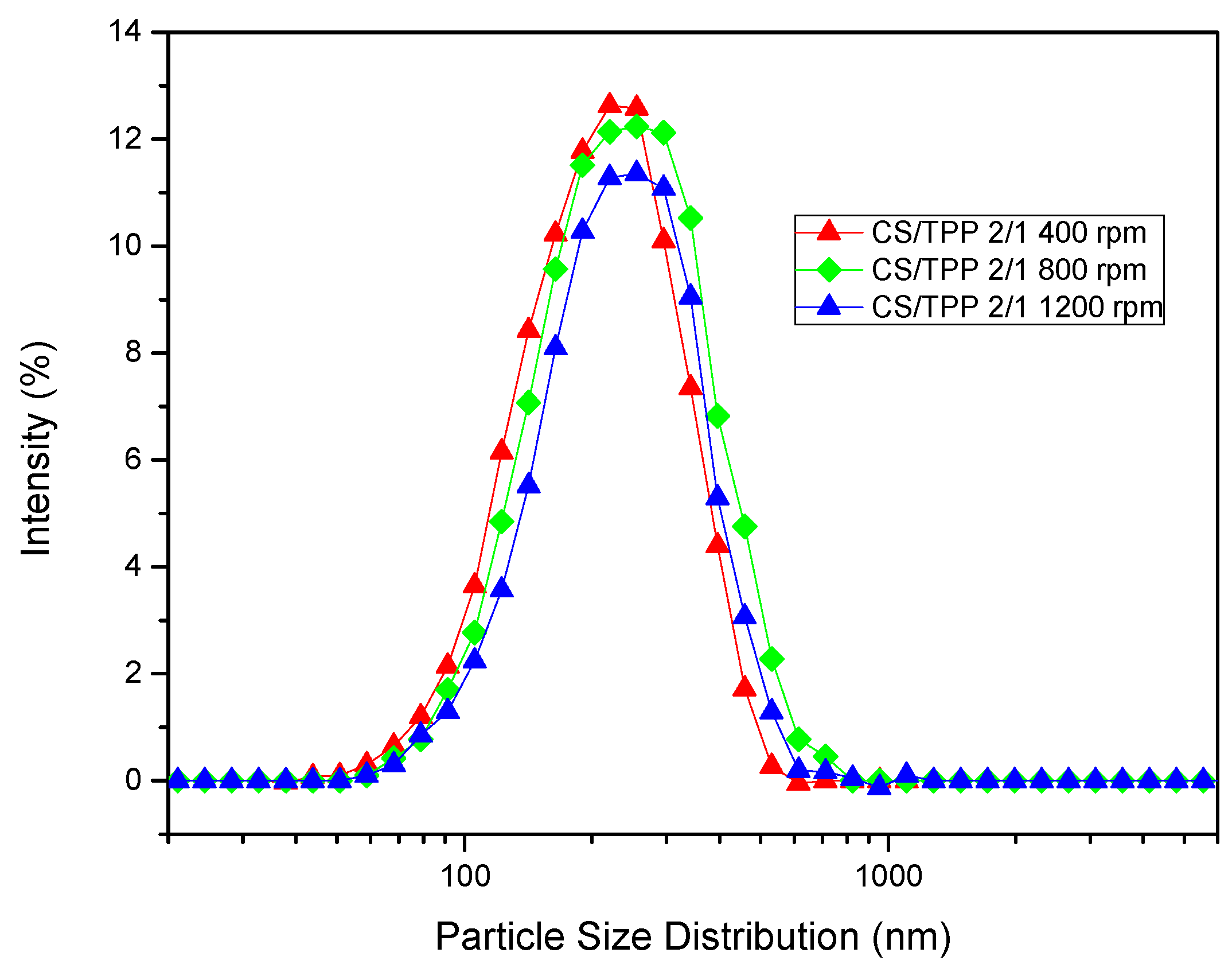
3.1. Size and Morphology of CS/TPP Nanoparticles
3.2. CS/TPP Nanoparticles Loaded with DFO
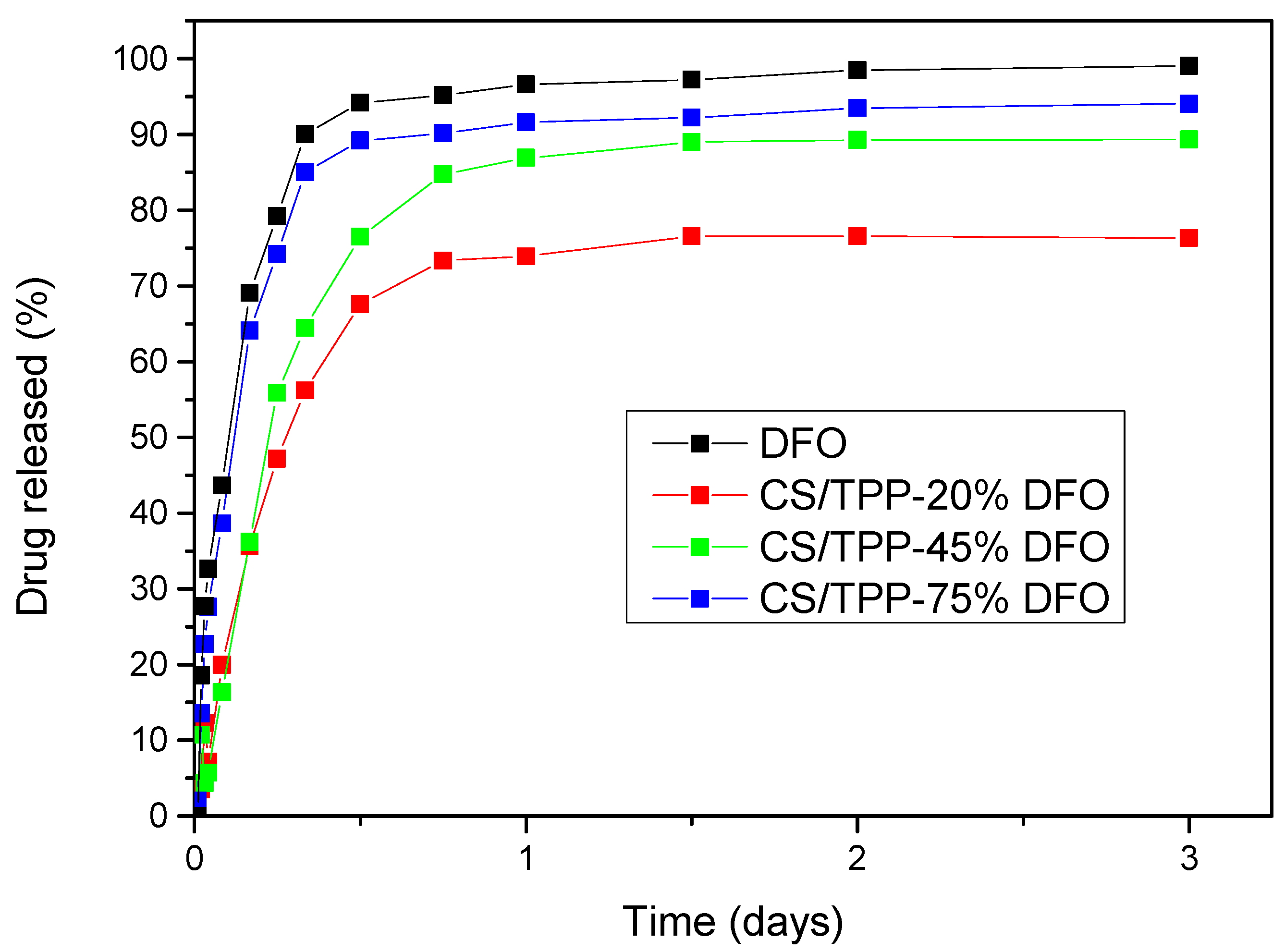
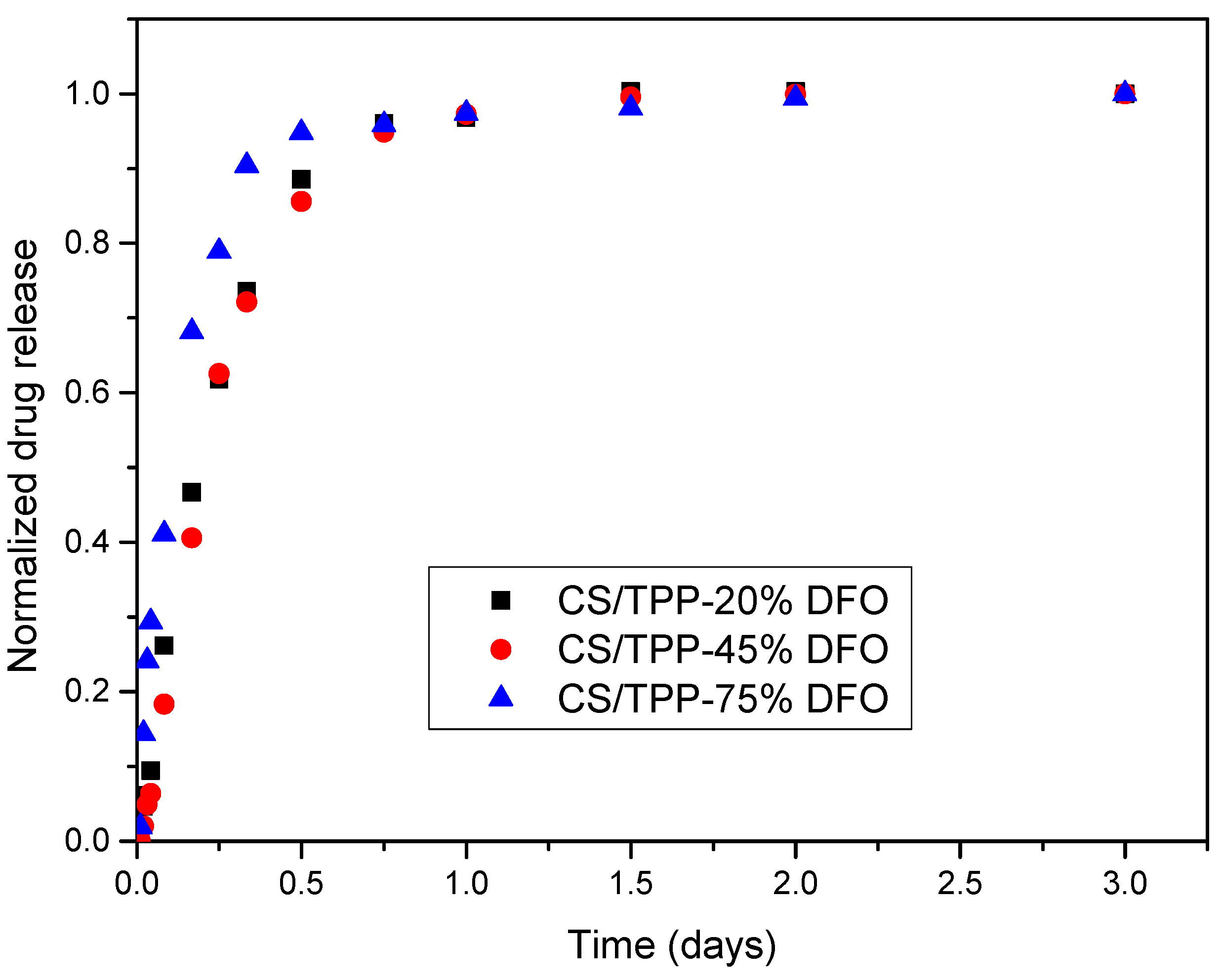
3.3. Drug Release from CS NPs
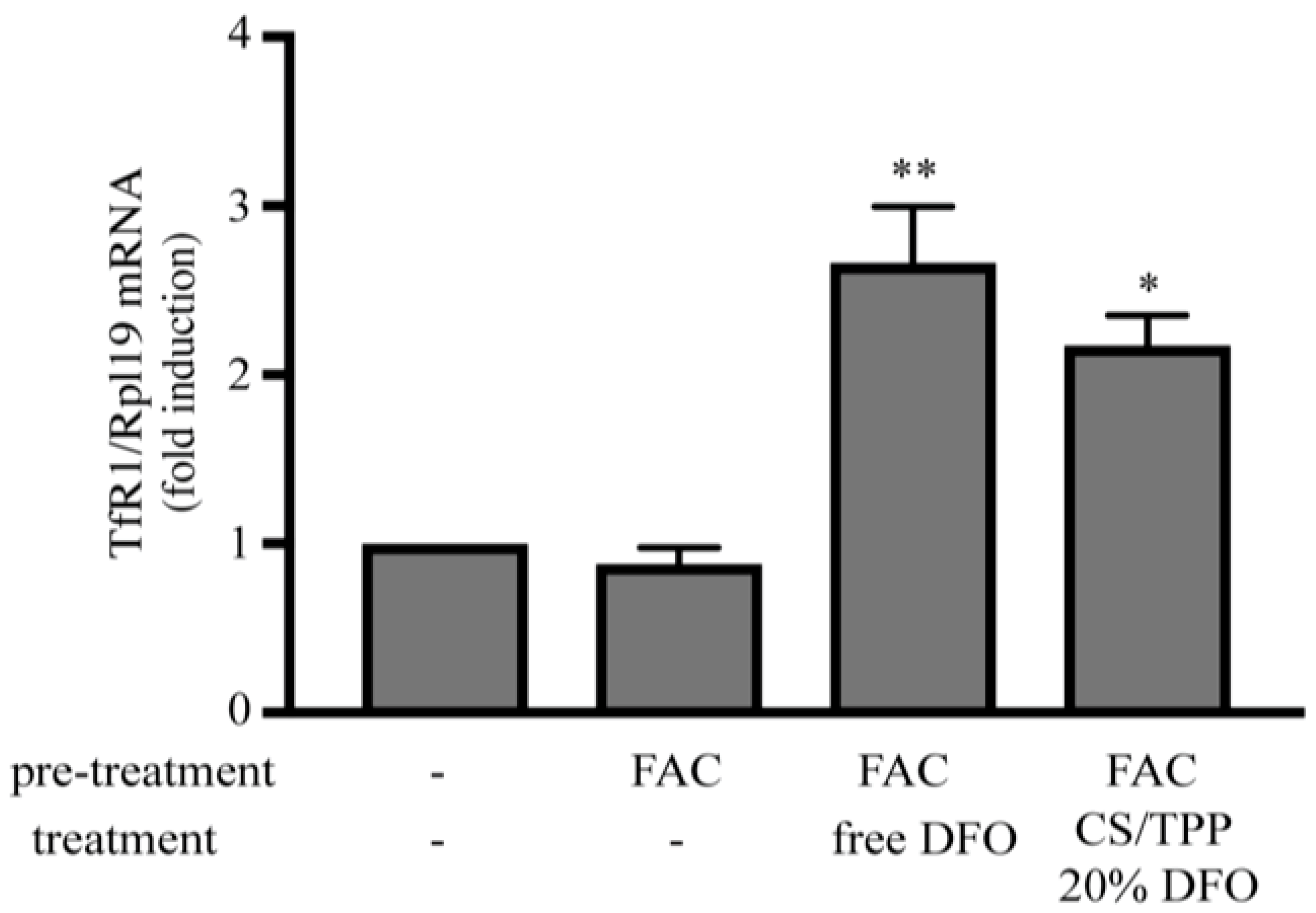
3.4. Evidence that DFO Released from CS NPs Operates as a Functional Iron Chelator in Cultured Cells
4. Conclusions
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- Musallam, K.M.; Angastiniotis, M.; Eleftheriou, A.; Porter, J.B. Cross-Talk between Available Guidelines for the Management of Patients with Beta-Thalassemia Major. Acta Haematol. 2013, 130, 64–73. [Google Scholar] [CrossRef] [PubMed]
- Cheng, C.J.; Tietjen, G.T.; Saucier-sawyer, J.K.; Mark, W.; Haven, N.; Haven, N. A holistic approach to targeting disease with polymer nanoparticles. Nat. Rev. Drug Discov. 2015, 14, 239–247. [Google Scholar] [CrossRef] [PubMed]
- Fangueiro, J.F.; Andreani, T.; Egea, M.A.; Garcia, M.L.; Souto, S.B.; Silva, A.M.; Souto, E.B. Design of cationic lipid nanoparticles for ocular delivery: Development, characterization and cytotoxicity. Int. J. Pharm. 2014, 461, 64–73. [Google Scholar] [CrossRef]
- Mishra, V.; Jain, N.K. Acetazolamide encapsulated dendritic nano-architectures for effective glaucoma management in rabbits. Int. J. Pharm. 2014, 461, 380–390. [Google Scholar] [CrossRef]
- Pahuja, P.; Arora, S.; Pawar, P.; Pahuja, P.; Arora, S.; Pawar, P. Ocular drug delivery system: A reference to natural polymers. Expert Opin. Drug Deliv. 2012, 9, 837–861. [Google Scholar] [CrossRef] [PubMed]
- Üstündag-Okur, N.; Gökçe, E.H.; Bozdiyik, D.I.; Egrilmez, S.; Özer, Ö.; Ertan, G. Preparation and in vitro–in vivo evaluation of ofloxacin loaded ophthalmic nano structured lipid carriers modified with chitosan oligosaccharide lactate for the treatment of bacterial keratitis. Eur. J. Pharm. Sci. 2014, 63, 204–215. [Google Scholar] [CrossRef] [PubMed]
- Chevalier, M.T.; Gonzalez, J.; Alvarez, V. Biodegradable Polymeric Microparticles as Drug Delivery Devices. Ifmbe Proc. 2015, 49, 187–190. [Google Scholar]
- Patel, J.K.; Jivani, N.P. Chitosan Based Nanoparticles in Drug Delivery. Int. J. Pharm. Sci. Nanotechnol. 2009, 2, 517–522. [Google Scholar]
- Keawchaoon, L.; Yoksan, R. Preparation, characterization and in vitro release study of carvacrol-loaded chitosan nanoparticles. Colloids Surf. B Biointerfaces 2011, 84, 163–171. [Google Scholar] [CrossRef]
- Frank, L.A.; Onzi, G.R.; Morawski, A.S.; Pohlmann, A.R.; Guterres, S.S.; Contri, R.V. Chitosan as a coating material for nanoparticles intended for biomedical applications. React. Funct. Polym. 2020, 147, 104459. [Google Scholar] [CrossRef]
- Arulmozhi, V.; Pandian, K.; Mirunalini, S. Ellagic acid encapsulated chitosan nanoparticles for drug delivery system in human oral cancer cell line (KB). Colloids Surf. B Biointerfaces 2013, 110, 313–320. [Google Scholar] [CrossRef] [PubMed]
- de Campos, A.M.; Diebold, Y.; Carvalho, E.L.S.; Sánchez, A.; Alonso, M.J. Chitosan Nanoparticles as New Ocular Drug Delivery Systems: In Vitro Stability, in Vivo Fate, and Cellular Toxicity. Pharm. Res. 2004, 21, 803–810. [Google Scholar] [CrossRef] [PubMed]
- Fàbregas, A.; Miñarro, M.; García-Montoya, E.; Pérez-Lozano, P.; Carrillo, C.; Sarrate, R.; Sánchez, N.; Ticó, J.R.; Suñé-Negre, J.M. Impact of physical parameters on particle size and reaction yield when using the ionic gelation method to obtain cationic polymeric chitosan–tripolyphosphate nanoparticles. Int. J. Pharm. 2013, 446, 199–204. [Google Scholar]
- Dash, M.; Chiellini, F.; Ottenbrite, R.M.; Chiellini, E. Chitosan—A versatile semi-synthetic polymer in biomedical applications. Prog. Polym. Sci. 2011, 36, 981–1014. [Google Scholar] [CrossRef]
- Bulmer, C.; Margaritis, A.; Xenocostas, A. Production and characterization of novel chitosan nanoparticles for controlled release of rHu-Erythropoietin. Biochem. Eng. J. 2012, 68, 61–69. [Google Scholar] [CrossRef]
- Fan, W.; Yan, W.; Xu, Z.; Ni, H. Formation mechanism of monodisperse, low molecular weight chitosan nanoparticles by ionic gelation technique. Colloids Surf. B Biointerfaces 2012, 90, 21–27. [Google Scholar] [CrossRef]
- Gaspar, V.M.; Sousa, F.; Queiroz, J.A.; Correia, I.J. Formulation of chitosan–TPP–pDNA nanocapsules for gene therapy applications. Nanotechnology 2011, 22, 015101. [Google Scholar] [CrossRef]
- Ji, A.M.; Su, D.; Che, O.; Li, W.S.; Sun, L.; Zhang, Z.Y.; Yang, B.; Xu, F. Functional gene silencing mediated by chitosan/siRNA nanocomplexes. Nanotechnology 2009, 20, 405103. [Google Scholar] [CrossRef]
- Tsai, M.; Chen, R.; Bai, S.; Chen, W. The storage stability of chitosan/tripolyphosphate nanoparticles in a phosphate buffer. Carbohydr. Polym. 2011, 84, 756–761. [Google Scholar] [CrossRef]
- Calvo, P.; Vila-Jato, J.L.; Alonso, M.J. Evaluation of cationic polymer-coated nanocapsules as ocular drug carriers. Int. J. Pharm. 1997, 153, 41–50. [Google Scholar] [CrossRef]
- Nanaki, S.G.; Kanaze, F.I.; Bikiaris, D.N. Development of a simple validated isocratic HPLC method for the assaying of desferrioxamine in nanoparticles based on poly(ε-caprolactone)-block-poly(propylene adipate) copolymers. Glob. J. Anal. Chem. 2011, 2. [Google Scholar]
- Maffettone, C.; Chen, G.; Drozdov, I.; Ouzounis, C.; Pantopoulos, K. Tumorigenic Properties of Iron Regulatory Protein 2 (IRP2) Mediated by Its Specific 73-Amino Acids Insert. PLoS ONE 2010, 5, e10163. [Google Scholar] [CrossRef]
- Pan, Y.; Zheng, J.; Zhao, H.; Li, Y.; Xu, H.; Wei, G. Relationship between drug effects and particle size of insulin-loaded bioadhesive microspheres. Acta Pharmacol. Sin. 2002, 23, 1051–1056. [Google Scholar]
- Papadimitriou, S.; Bikiaris, D.; Avgoustakis, K. Chitosan nanoparticles loaded with dorzolamide and pramipexole. Carbohydr. Polym. 2008, 73, 44–54. [Google Scholar] [CrossRef]
- Siafaka, P.I.; Titopoulou, A.; Koukaras, E.N.; Kostoglou, M.; Koutris, E.; Karavas, E.; Bikiaris, D.N. Chitosan derivatives as effective nanocarriers for ocular release of timolol drug. Int. J. Pharm. 2015, 495, 249–264. [Google Scholar] [CrossRef]
- Singh, K.H.; Shinde, U.A. Chitosan nanoparticles for controlled delivery of brimonidine tartrate to the ocular membrane. Die Pharm. Int. J. Pharm. Sci. 2011, 66, 594–599. [Google Scholar]
- Bozdag, S.; Dillen, K.; Vandervoort, J.; Ludwig, A. The effect of freeze-drying with different cryoprotectants and gamma-irradiation sterilization on the characteristics of ciprofloxacin HCl-loaded poly (D, L -lactide-glycolide) nanoparticles. J. Pharm. Pharmacol. 2005, 57, 699–707. [Google Scholar] [CrossRef]
- Abdelwahed, W.; Degobert, G.; Stainmesse, S.; Fessi, H. Freeze-drying of nanoparticles: Formulation, process and storage considerations. Adv. Drug Deliv. Rev. 2006, 58, 1688–1713. [Google Scholar] [CrossRef]
- Koutroumanis, K.P.; Avgoustakis, K.; Bikiaris, D. Synthesis of cross-linked N-(2-carboxybenzyl) chitosan pH sensitive polyelectrolyte and its use for drug controlled delivery. Carbohydr. Polym. 2010, 82, 181–188. [Google Scholar] [CrossRef]
- Kyzas, G.Z.; Bikiaris, D.N.; Lazaridis, N.K. Low-Swelling Chitosan Derivatives as Biosorbents for Basic Dyes. Langmuir 2008, 24, 4791–4799. [Google Scholar] [CrossRef]
- Dubey, A.; Prabhu, P. Formulation and evaluation of stimuli-sensitive hydrogels of timolol maleate and brimonidine tartrate. Int. J. Pharm. Investig. 2014, 4, 122. [Google Scholar] [CrossRef]
- Abdeen, Z.; Mohammad, S.G. Study of the Adsorption Efficiency of an Eco-Friendly Carbohydrate Polymer for Contaminated Aqueous Solution by Organophosphorus Pesticide. Open J. Org. Polym. Mater. 2014, 4, 16–28. [Google Scholar] [CrossRef]
- Karavas, E.; Georgarakis, M.; Docoslis, A.; Bikiaris, D. Combining SEM, TEM, and micro-Raman techniques to differentiate between the amorphous molecular level dispersions and nanodispersions of a poorly water-soluble drug within a polymer matrix. Int. J. Pharm. 2007, 340, 76–83. [Google Scholar] [CrossRef]
- Nanaki, S.G.; Pantopoulos, K.; Bikiaris, D.N. Synthesis of biocompatible poly(e-caprolactone)-block-poly(propylene adipate) copolymers appropriate for drug nanoencapsulation in the form of core-shell nanoparticles. Int. J. Nanomed. 2011, 6, 2981–2995. [Google Scholar]
- Hattori, Y.; Haruna, Y.; Otsuka, M. Dissolution process analysis using model-free Noyes–Whitney integral equation. Colloids Surf. B Biointerfaces 2013, 102, 227–231. [Google Scholar] [CrossRef]
- Korsmeyer, R.W.; Gurny, R.; Doelker, E.; Buri, P.; Peppas, N.A. Mechanisms of solute release from porous hydrophilic polymers. Int. J. Pharm. 1983, 15, 25–35. [Google Scholar]
- Crank, J. The Mathematics of Diffusion; Oxford University Press: Oxford, UK, 1975. [Google Scholar]
- Tien, C. Adsorption Calculations and Modeling; Butterworth-Heinemann: Boston, MA, USA, 1994. [Google Scholar]
- Wang, J.; Pantopoulos, K. Regulation of cellular iron metabolism. Biochem. J. 2011, 434, 365–381. [Google Scholar] [CrossRef]
- Pantopoulos, K.; Gray, N.K. Differential regulation of two related RNA-binding proteins, iron regulatory protein (IRP) and IRPB. RNA 1995, 1, 155–163. [Google Scholar]

| Gene | GenBank Accession | Forward Primer Sequence | Reverse Primer Sequence |
|---|---|---|---|
| TfR1 | NM_011638.4 | AGCCAGATCAGCATTCTCTAACT | GCCTTCATGTTATTGTCGGCAT |
| Rpl19 | NM_009078.2 | AGGCATATGGGCATAGGGAAGAG | TTGACCTTCAGGTACAGGCTGTG |
| a Sample | Nanoparticle Yield (%) | Nanoparticle Size (nm) | Pdi | Zeta Potential (mV) |
|---|---|---|---|---|
| CS/TPP 2/1 400 rpm | 77.50 ± 1.84 | 243 ± 15 | 0.62 | 38.45 |
| CS/TPP 2/1 800 rpm | 85.75 ± 1.12 | 287 ± 17 | 0.78 | 37.59 |
| CS/TPP 2/1 1200 rpm | 82.51 ± 0.93 | 269 ± 21 | 0.54 | 40.11 |
| a Sample | Nanoparticle Diameter (nm) | Nanoparticle Yield (%) | Drug Loading (%) | Entrapment Efficiency (%) |
|---|---|---|---|---|
| CS/TPP_blank | 287 ± 17 | 85.75 ± 1.12 | - | - |
| CS/TPP_20%DFO | 304 ± 25 | 76.88 ± 1.12 | 11.55 ± 1.47 | 44.45 ± 1.39 |
| CS/TPP_45%DFO | 448 ± 31 | 61.46 ± 0.87 | 17.02 ± 2.12 | 26.15 ± 1.05 |
| CS/TPP_75%DFO | 528 ± 35 | 35.47 ± 1.34 | 40.09 ± 4.22 | 18.96 ± 0.89 |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Lazaridou, M.; Christodoulou, E.; Nerantzaki, M.; Kostoglou, M.; Lambropoulou, D.A.; Katsarou, A.; Pantopoulos, K.; Bikiaris, D.N. Formulation and In-Vitro Characterization of Chitosan-Nanoparticles Loaded with the Iron Chelator Deferoxamine Mesylate (DFO). Pharmaceutics 2020, 12, 238. https://doi.org/10.3390/pharmaceutics12030238
Lazaridou M, Christodoulou E, Nerantzaki M, Kostoglou M, Lambropoulou DA, Katsarou A, Pantopoulos K, Bikiaris DN. Formulation and In-Vitro Characterization of Chitosan-Nanoparticles Loaded with the Iron Chelator Deferoxamine Mesylate (DFO). Pharmaceutics. 2020; 12(3):238. https://doi.org/10.3390/pharmaceutics12030238
Chicago/Turabian StyleLazaridou, Maria, Evi Christodoulou, Maria Nerantzaki, Margaritis Kostoglou, Dimitra A. Lambropoulou, Angeliki Katsarou, Kostas Pantopoulos, and Dimitrios N. Bikiaris. 2020. "Formulation and In-Vitro Characterization of Chitosan-Nanoparticles Loaded with the Iron Chelator Deferoxamine Mesylate (DFO)" Pharmaceutics 12, no. 3: 238. https://doi.org/10.3390/pharmaceutics12030238
APA StyleLazaridou, M., Christodoulou, E., Nerantzaki, M., Kostoglou, M., Lambropoulou, D. A., Katsarou, A., Pantopoulos, K., & Bikiaris, D. N. (2020). Formulation and In-Vitro Characterization of Chitosan-Nanoparticles Loaded with the Iron Chelator Deferoxamine Mesylate (DFO). Pharmaceutics, 12(3), 238. https://doi.org/10.3390/pharmaceutics12030238









