Polysaccharides in Ocular Drug Delivery
Abstract
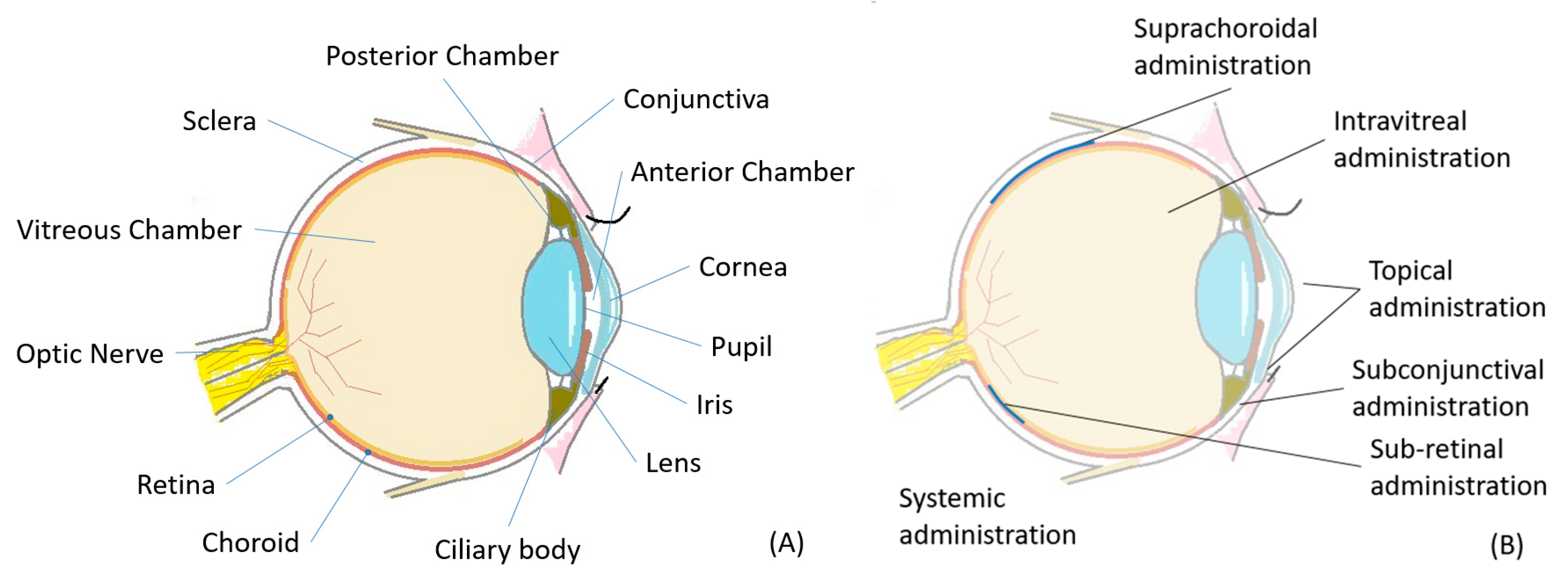
1. Introduction
2. Polysaccharides Used in Ophthalmology
3. Topical Administration
3.1. Barriers to Topical Delivery of Ocular Drugs
3.2. Eye Drops and Artificial Tears
3.3. Mucoadhesives
3.4. In-Situ-Forming Hydrogels
3.4.1. Features of In-Situ-Forming Hydrogels
3.4.2. In-Situ-Forming Gels Influenced by Ionic Strength
3.4.3. In-Situ-Forming Gels Influenced by Temperature
3.4.4. In-Situ-Forming Gels Influenced by pH
3.5. Inserts and Contact Lenses
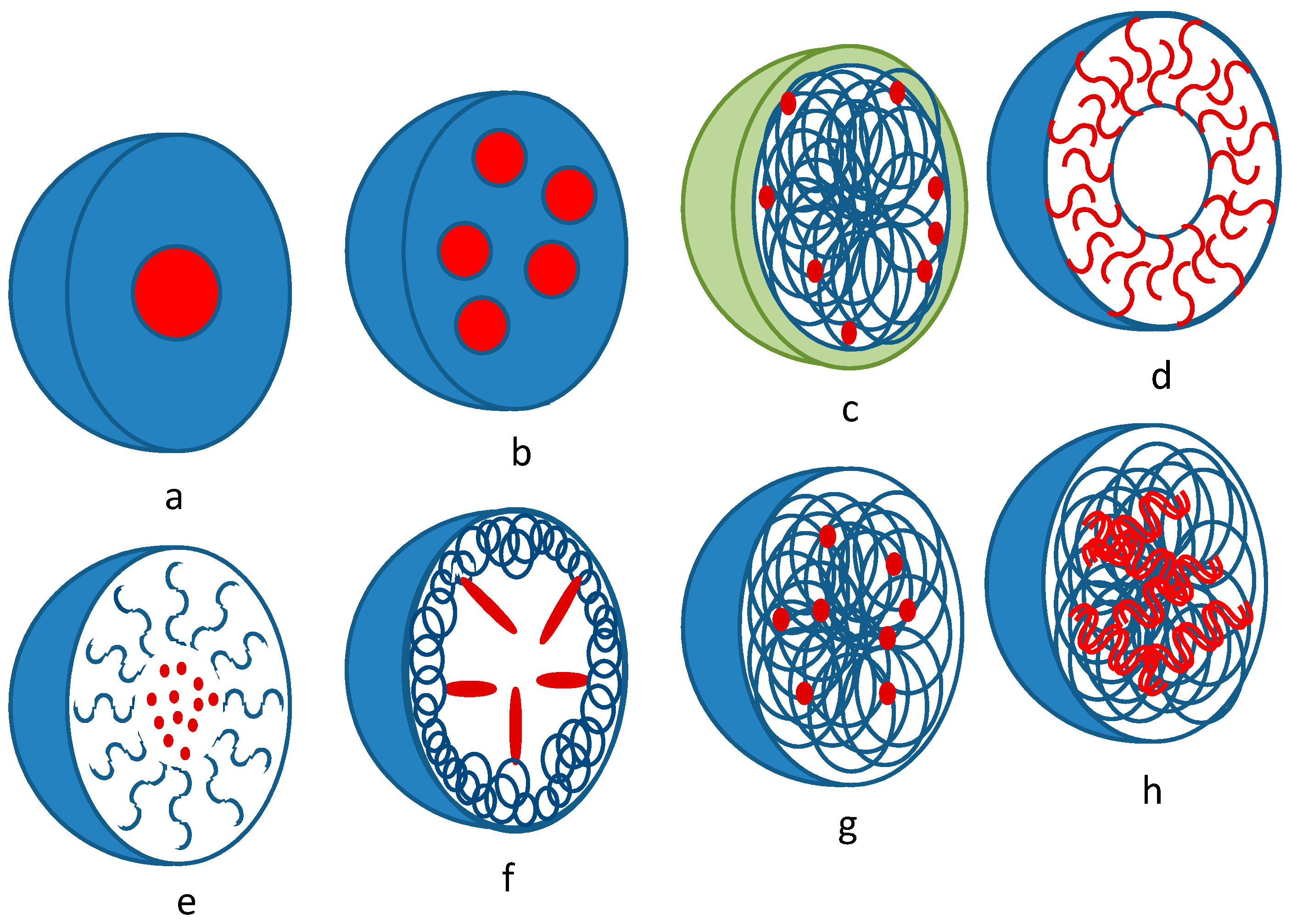
3.6. Dispersed Systems
3.6.1. Liposomes
3.6.2. Micro- and Nanoparticles
3.6.3. Inclusion Complexes (Clathrates)
3.7. Summary
4. Intravitreal Administration
4.1. Hydrogels
4.2. Dispersed Systems
4.2.1. Micro and Nanoparticles
4.2.2. Polyplexes
4.2.3. Self-Assembling Nanoparticles
4.3. Conjugates (Covalent Modification)
4.4. Intravitreal Implants
5. Periocular Administration
5.1. Subconjunctival Delivery
5.2. Suprachoroidal Delivery
6. Subretinal Delivery
7. Future Aspects
Author Contributions
Funding
Conflicts of Interest
Abbreviations
| ALG | alginic acid or sodium alginate |
| CMC | carboxymethyl cellulose or sodium carboxymethyl cellulose |
| CNAC | chitosan-N-acetyl-l-cysteine |
| DED | dry eye disease |
| HA | hyaluronic acid or sodium hyaluronate |
| hESCs | human embryonic stem cells |
| hiPSCs | human induced pluripotent stem cells |
| HPMC | hydroxypropyl methylcellulose |
| HUVECs | human umbilical vein endothelial cells |
| ILM | inner limiting membrane |
| IOP | intraocular pressure |
| MW | molecular weight |
| pDNA | plasmid DNA |
| PEG | polyethylene glycol |
| PLGA | poly(lactic-co-glycolic acid) |
| PNIPAAm | poly(N-isopropylacrylamide) |
| polysiRNA | multimerized small interfering RNA |
| RGD | adhesion peptide (Arg-Gly-Asp) |
| RPE | retinal pigment epithelial cells |
| RPCs | retinal progenitor cells |
| TPP | sodium tripolyphosphate |
| TSP | tamarind seed polysaccharides |
| VEGF | vascular endothelial growth factor |
References
- Formica, M.L.; Calles, J.A.; Palma, S.D. Polysaccharide-based nanocarriers for ocular drug delivery. Curr. Pharm. Des. 2015, 21, 4851–4868. [Google Scholar] [CrossRef] [PubMed]
- Nayak, K.; Misra, M. A review on recent drug delivery systems for posterior segment of eye. Biomed. Pharmacother. 2018, 107, 1564–1582. [Google Scholar] [CrossRef] [PubMed]
- Tsai, C.H.; Wang, P.Y.; Lin, I.C.; Huang, H.; Liu, G.S.; Tseng, C.L. Ocular drug delivery: Role of degradable polymeric nanocarriers for ophthalmic application. Int. J. Mol. Sci. 2018, 19, 2830. [Google Scholar] [CrossRef] [PubMed]
- Waite, D.; Wang, Y.; Jones, D.; Stitt, A.; Singh, T.R. Posterior drug delivery via periocular route: Challenges and opportunities. Ther. Deliv. 2017, 8, 685–699. [Google Scholar] [CrossRef]
- Kompella, U.B.; Amrite, A.C.; Pacha Ravi, R.; Durazo, S.A. Nanomedicines for back of the eye drug delivery, gene delivery, and imaging. Prog. Retin. Eye Res. 2013, 36, 172–198. [Google Scholar] [CrossRef]
- Cunha-Vaz, J.G. The blood-ocular barriers: Past, present, and future. Doc. Ophthalmol. 1997, 93, 149–157. [Google Scholar] [CrossRef]
- Weng, Y.; Liu, J.; Jin, S.; Guo, W.; Liang, X.; Hu, Z. Nanotechnology-based strategies for treatment of ocular disease. Acta Pharm. Sin. B 2017, 7, 281–291. [Google Scholar] [CrossRef]
- Poshina, D.N.; Raik, S.V.; Poshin, A.N.; Skorik, Y.A. Accessibility of chitin and chitosan in enzymatic hydrolysis: A review. Polym. Degrad. Stab. 2018, 156, 269–278. [Google Scholar] [CrossRef]
- Kritchenkov, A.S.; Andranovits, S.; Skorik, Y.A. Chitosan and its derivatives: Vectors in gene therapy. Russ. Chem. Rev. 2017, 86, 231–239. [Google Scholar] [CrossRef]
- Berezin, A.S.; Lomkova, E.A.; Skorik, Y.A. Chitosan conjugates with biologically active compounds: Design strategies, properties, and targeted drug delivery. Russ. Chem. Bull. 2012, 61, 781–795. [Google Scholar] [CrossRef]
- Tiwari, S.; Bahadur, P. Modified hyaluronic acid based materials for biomedical applications. Int. J. Biol. Macromol. 2019, 121, 556–571. [Google Scholar] [CrossRef] [PubMed]
- Fernando, I.P.S.; Kim, D.; Nah, J.W.; Jeon, Y.J. Advances in functionalizing fucoidans and alginates (bio) polymers by structural modifications: A review. Chem. Eng. J. 2019, 355, 33–48. [Google Scholar] [CrossRef]
- Pettignano, A.; Charlot, A.; Fleury, E. Carboxyl-functionalized derivatives of carboxymethyl cellulose: Towards advanced biomedical applications. Polym. Rev. 2019, 59, 510–560. [Google Scholar] [CrossRef]
- Siafaka, P.I.; Titopoulou, A.; Koukaras, E.N.; Kostoglou, M.; Koutris, E.; Karavas, E.; Bikiaris, D.N. Chitosan derivatives as effective nanocarriers for ocular release of timolol drug. Int. J. Pharm. 2015, 495, 249–264. [Google Scholar] [CrossRef]
- Zambito, Y.; Di Colo, G. Thiolated quaternary ammonium-chitosan conjugates for enhanced precorneal retention, transcorneal permeation and intraocular absorption of dexamethasone. Eur. J. Pharm. Biopharm. 2010, 75, 194–199. [Google Scholar] [CrossRef]
- Rassu, G.; Gavini, E.; Jonassen, H.; Zambito, Y.; Fogli, S.; Breschi, M.C.; Giunchedi, P. New chitosan derivatives for the preparation of rokitamycin loaded microspheres designed for ocular or nasal administration. J. Pharm. Sci. 2009, 98, 4852–4865. [Google Scholar] [CrossRef]
- Hume, L.R.; Lee, H.K.; Benedetti, L.; Sanzgiri, Y.D.; Topp, E.M.; Stella, V.J. Ocular sustained delivery of prednisolone using hyaluronic acid benzyl ester films. Int. J. Pharm. 1994, 111, 295–298. [Google Scholar] [CrossRef]
- Bongiovì, F.; Di Prima, G.; Palumbo, F.S.; Licciardi, M.; Pitarresi, G.; Giammona, G. Hyaluronic acid-based micelles as ocular platform to modulate the loading, release, and corneal permeation of corticosteroids. Macromol. Biosci. 2017, 17, 1700261. [Google Scholar] [CrossRef]
- Garhofer, G. Evaluation of the Corneal Residence Time of Chitosan–N-Acetylcysteine Eye Drops in Patients with Dry Eye Syndrome After Single and Multiple Instillation. 2014. Available online: https://clinicaltrials.gov/ct2/show/NCT01753752 (accessed on 24 December 2019).
- Duquesroix, B. Evaluation of the Efficacy and Safety of Iota-Carrageenan Eye Drops (ncx-4240) Versus Placebo in Patients with Adenoviral Conjunctivis. 2017. Available online: https://clinicaltrials.gov/ct2/show/NCT03009799 (accessed on 24 December 2019).
- Patchan, M.; Graham, J.; Xia, Z.; Maranchi, J.; McCally, R.; Schein, O.; Elisseeff, J.H.; Trexler, M. Synthesis and properties of regenerated cellulose-based hydrogels with high strength and transparency for potential use as an ocular bandage. Mater. Sci. Eng. 2013, 33, 3069–3076. [Google Scholar] [CrossRef]
- Urtti, A. Challenges and obstacles of ocular pharmacokinetics and drug delivery. Adv. Drug Deliv. Rev. 2006, 58, 1131–1135. [Google Scholar] [CrossRef]
- Necas, J.; Bartosikova, L.; Brauner, P.; Kolar, J. Hyaluronic acid (hyaluronan): A review. Vet. Med. 2008, 53, 397–411. [Google Scholar] [CrossRef]
- Price, R.D.; Berry, M.; Navsaria, H.A. Hyaluronic acid: The scientific and clinical evidence. J. Plast. Reconstr. Aesthetic Surg. 2007, 60, 1110–1119. [Google Scholar] [CrossRef] [PubMed]
- Aragona, P.; Papa, V.; Micali, A.; Santocono, M.; Milazzo, G. Long term treatment with sodium hyaluronate-containing artificial tears reduces ocular surface damage in patients with dry eye. Br. J. Ophthalmol. 2002, 86, 181–184. [Google Scholar] [CrossRef] [PubMed]
- Giri, T. Nanoarchitectured polysaccharide-based drug carrier for ocular therapeutics. In Nanoarchitectonics for Smart Delivery and Drug Targeting; William Andrew: Norwich, NY, USA, 2016; pp. 119–141. [Google Scholar]
- Irimia, T.; Ghica, M.; Popa, L.; Anuţa, V.; Arsene, A.-L.; Dinu-Pîrvu, C.-E. Strategies for improving ocular drug bioavailability and corneal wound healing with chitosan-based delivery systems. Polymers 2018, 10, 1221. [Google Scholar] [CrossRef] [PubMed]
- Felt, O.; Furrer, P.; Mayer, J.; Plazonnet, B.; Buri, P.; Gurny, R. Topical use of chitosan in ophthalmology: Tolerance assessment and evaluation of precorneal retention. Int. J. Pharm. 1999, 180, 185–193. [Google Scholar] [CrossRef]
- Silva, M.; Calado, R.; Marto, J.; Bettencourt, A.; Almeida, A.; Gonçalves, L. Chitosan nanoparticles as a mucoadhesive drug delivery system for ocular administration. Mar. Drugs 2017, 15, 370. [Google Scholar] [CrossRef]
- Chhonker, Y.S.; Prasad, Y.D.; Chandasana, H.; Vishvkarma, A.; Mitra, K.; Shukla, P.K.; Bhatta, R.S. Amphotericin-B entrapped lecithin/chitosan nanoparticles for prolonged ocular application. Int. J. Biol. Macromol. 2015, 72, 1451–1458. [Google Scholar] [CrossRef]
- Hunt, N.C.; Grover, L.M. Cell encapsulation using biopolymer gels for regenerative medicine. Biotechnol. Lett. 2010, 32, 733–742. [Google Scholar] [CrossRef]
- Hunt, N.C.; Smith, A.M.; Gbureck, U.; Shelton, R.M.; Grover, L.M. Encapsulation of fibroblasts causes accelerated alginate hydrogel degradation. Acta Biomater. 2010, 6, 3649–3656. [Google Scholar] [CrossRef]
- Goh, C.H.; Heng, P.W.S.; Chan, L.W. Alginates as a useful natural polymer for microencapsulation and therapeutic applications. Carbohydr. Polym. 2012, 88, 1–12. [Google Scholar] [CrossRef]
- Bidarra, S.J.; Barrias, C.C.; Granja, P.L. Injectable alginate hydrogels for cell delivery in tissue engineering. Acta Biomater. 2014, 10, 1646–1662. [Google Scholar] [CrossRef] [PubMed]
- Munarin, F.; Tanzi, M.C.; Petrini, P. Advances in biomedical applications of pectin gels. Int. J. Biol. Macromol. 2012, 51, 681–689. [Google Scholar] [CrossRef] [PubMed]
- Noreen, A.; Nazli, Z.I.; Akram, J.; Rasul, I.; Mansha, A.; Yaqoob, N.; Iqbal, R.; Tabasum, S.; Zuber, M.; Zia, K.M. Pectins functionalized biomaterials; a new viable approach for biomedical applications: A review. Int. J. Biol. Macromol. 2017, 101, 254–272. [Google Scholar] [CrossRef] [PubMed]
- Ceulemans, J.; Vinckier, I.; Ludwig, A. The use of xanthan gum in an ophthalmic liquid dosage form: Rheological characterization of the interaction with mucin. J. Pharm. Sci. 2002, 91, 1117–1127. [Google Scholar] [CrossRef]
- Bhowmik, M.; Kumari, P.; Sarkar, G.; Bain, M.K.; Bhowmick, B.; Mollick, M.M.R.; Mondal, D.; Maity, D.; Rana, D.; Bhattacharjee, D. Effect of xanthan gum and guar gum on in situ gelling ophthalmic drug delivery system based on poloxamer-407. Int. J. Biol. Macromol. 2013, 62, 117–123. [Google Scholar] [CrossRef]
- Burgalassi, S.; Chetoni, P.; Saettone, M.F. Hydrogels for ocular delivery of pilocarpine: Preliminary evaluation in rabbits of the influence of viscosity and of drug solubility. Eur. J. Pharm. Biopharm. 1996, 42, 385–392. [Google Scholar]
- Raghava, S.; Hammond, M.; Kompella, U.B. Periocular routes for retinal drug delivery. Expert Opin. Drug Deliv. 2004, 1, 99–114. [Google Scholar] [CrossRef]
- Urtti, A.; Salminen, L.; Miinalainen, O. Systemic absorption of ocular pilocarpine is modified by polymer matrices. Int. J. Pharm. 1985, 23, 147–161. [Google Scholar] [CrossRef]
- Battaglia, L.; Gallarate, M.; Serpe, L.; Foglietta, F.; Muntoni, E.; del Pozo Rodriguez, A.; Angeles Solinis Aspiazu, M. Chapter 7-ocular delivery of solid lipid nanoparticles. In Lipid Nanocarriers for Drug Targeting; Grumezescu, A.M., Ed.; William Andrew Publishing: Norwich, NY, USA, 2018; pp. 269–312. [Google Scholar]
- Maurice, D.M.; Mishima, S. Ocular pharmacokinetics. In Pharmacology of the Eye; Sears, M.L., Ed.; Springer: Berlin/Heidelberg, Germany, 1984; pp. 19–116. [Google Scholar]
- Kidron, H.; Vellonen, K.S.; del Amo, E.M.; Tissari, A.; Urtti, A. Prediction of the corneal permeability of drug-like compounds. Pharm. Res. 2010, 27, 1398–1407. [Google Scholar] [CrossRef]
- Huang, H.S.; Schoenwald, R.D.; Lach, J.L. Corneal penetration behavior of β-blocking agents ii: Assessment of barrier contributions. J. Pharm. Sci. 1983, 72, 1272–1279. [Google Scholar] [CrossRef]
- Fletcher, E.L.; Brennan, N.A. The effect of solution tonicity on the eye. Clin. Exp. Optom. 1993, 76, 17–21. [Google Scholar]
- Conrad, J.M.; Reay, W.A.; Polcyn, R.E.; Robinson, J.R. Influence of tonicity and pH on lacrimation and ocular drug bioavailability. J. Parenter. Drug Assoc. 1978, 32, 149–161. [Google Scholar] [PubMed]
- Garcia-Valldecabres, M.; López-Alemany, A.; Refojo, M.F. Ph stability of ophthalmic solutions. Optom. J. Am. Optom. Assoc. 2004, 75, 161–168. [Google Scholar] [CrossRef]
- Otero-Espinar, F.J.; Fernández-Ferreiro, A.; González-Barcia, M.; Blanco-Méndez, J.; Luzardo, A. Stimuli sensitive ocular drug delivery systems. In Drug Targeting and Stimuli Sensitive Drug Delivery Systems; Elsevier: Amsterdam, The Netherlands, 2018; pp. 211–270. [Google Scholar]
- Snibson, G.; Greaves, J.; Soper, N.; Prydal, J.; Wilson, C.; Bron, A. Precorneal residence times of sodium hyaluronate solutions studied by quantitative gamma scintigraphy. Eye 1990, 4, 594–602. [Google Scholar] [CrossRef]
- Paugh, J.R.; Nguyen, A.L.; Ketelson, H.A.; Christensen, M.T.; Meadows, D.L. Precorneal residence time of artificial tears measured in dry eye subjects. Optom. Vis. Sci. 2008, 85, 725–731. [Google Scholar] [CrossRef]
- Colo, G.D.; Zambito, Y.; Zaino, C.; Sansò, M. Selected polysaccharides at comparison for their mucoadhesiveness and effect on precorneal residence of different drugs in the rabbit model. Drug Dev. Ind. Pharm. 2009, 35, 941–949. [Google Scholar] [CrossRef]
- Burgalassi, S.; Nicosia, N.; Monti, D.; Falcone, G.; Boldrini, E.; Chetoni, P. Larch arabinogalactan for dry eye protection and treatment of corneal lesions: Investigations in rabbits. J. Ocul. Pharmacol. Ther. 2007, 23, 541–550. [Google Scholar] [CrossRef]
- Stolz, J.; Pinto-Bonilla, J.C.; Del Olmo-Jimeno, A.; Llovet Osuna, F.; Hernandez Galilea, E. A randomized crossover study comparing trehalose/hyaluronate eyedrops and standard treatment: Patient satisfaction in the treatment of dry eye syndrome. Ther. Clin. Risk Manag. 2015, 11, 595–603. [Google Scholar] [CrossRef][Green Version]
- Simmons, P.; Liu, H.; Carlisle-Wilcox, C.; Vehige, J. Efficacy and safety of two new formulations of artificial tears in subjects with dry eye disease: A 3-month, multicenter, active-controlled, randomized trial. Clin. Ophthalmol. 2015, 9, 665–675. [Google Scholar] [CrossRef]
- Asbell, P.; Fernandez, K.; Epstein, S.P.; Raynor, G.; Sheyman, A.; Massingale, M.; Dentone, P.; Landegger, L. Modulation of HLA-DR in dry eye patients following 30 days of treatment with a lubricant eyedrop solution. Clin. Ophthalmol. 2015, 2015, 1137–1145. [Google Scholar] [CrossRef][Green Version]
- Barabino, S.; Montaldo, E.; Solignani, F.; Valente, C.; Mingari, M.C.; Rolando, M. Immune response in the conjunctival epithelium of patients with dry eye. Exp. Eye Res. 2010, 91, 524–529. [Google Scholar] [CrossRef] [PubMed]
- Salzillo, R.; Schiraldi, C.; Corsuto, L.; D’Agostino, A.; Filosa, R.; De Rosa, M.; La Gatta, A. Optimization of hyaluronan-based eye drop formulations. Carbohydr. Polym. 2016, 153, 275–283. [Google Scholar] [CrossRef] [PubMed]
- Labetoulle, M.; Schmickler, S.; Galarreta, D.; Boehringer, D.; Ogundele, A.; Guillon, M.; Baudouin, C. Efficacy and safety of dual-polymer hydroxypropyl guar- and hyaluronic acid-containing lubricant eyedrops for the management of dry-eye disease: A randomized double-masked clinical study. Clin. Ophthalmol. 2018, 12, 2499–2508. [Google Scholar] [CrossRef] [PubMed]
- Grimaudo, M.A.; Pescina, S.; Padula, C.; Santi, P.; Concheiro, A.; Alvarez-Lorenzo, C.; Nicoli, S. Topical application of polymeric nanomicelles in ophthalmology: A review on research efforts for the non-invasive delivery of ocular therapeutics. Expert Opin. Drug Deliv. 2019, 16, 397–413. [Google Scholar] [CrossRef] [PubMed]
- Sharma, A.; Taniguchi, J. Review: Emerging strategies for antimicrobial drug delivery to the ocular surface: Implications for infectious keratitis. Ocul. Surf. 2017, 15, 670–679. [Google Scholar] [CrossRef] [PubMed]
- Kim, Y.C.; Chiang, B.; Wu, X.; Prausnitz, M.R. Ocular delivery of macromolecules. J. Control. Release 2014, 190, 172–181. [Google Scholar] [CrossRef]
- Dodou, D.; Breedveld, P.; Wieringa, P.A. Mucoadhesives in the gastrointestinal tract: Revisiting the literature for novel applications. Eur. J. Pharm. Biopharm. 2005, 60, 1–16. [Google Scholar] [CrossRef]
- Rossi, S.; Vigani, B.; Bonferoni, M.C.; Sandri, G.; Caramella, C.; Ferrari, F. Rheological analysis and mucoadhesion: A 30 year-old and still active combination. J. Pharm. Biomed. Anal. 2018, 156, 232–238. [Google Scholar] [CrossRef]
- Zambito, Y.; Colo, G.D. Polysaccharides as excipients for ocular topical formulations. In Biomaterials Applications for Nanomedicine; Pignatello, R., Ed.; InTech: London, UK, 2011; pp. 253–280. [Google Scholar]
- Rodriguez, I.; Vazquez, J.A.; Pastrana, L.; Khutoryanskiy, V.V. Enhancement and inhibition effects on the corneal permeability of timolol maleate: Polymers, cyclodextrins and chelating agents. Int. J. Pharm. 2017, 529, 168–177. [Google Scholar] [CrossRef]
- Bravo-Osuna, I.; Noiray, M.; Briand, E.; Woodward, A.; Argüeso, P.; Martínez, I.M.; Herrero-Vanrell, R.; Ponchel, G. Interfacial interaction between transmembrane ocular mucins and adhesive polymers and dendrimers analyzed by surface plasmon resonance. Pharm. Res. 2012, 29, 2329–2340. [Google Scholar] [CrossRef]
- Sogias, I.A.; Williams, A.C.; Khutoryanskiy, V.V. Why is chitosan mucoadhesive? Biomacromolecules 2008, 9, 1837–1842. [Google Scholar] [CrossRef] [PubMed]
- Menchicchi, B.; Fuenzalida, J.P.; Bobbili, K.B.; Hensel, A.; Swamy, M.J.; Goycoolea, F.M. Structure of chitosan determines its interactions with mucin. Biomacromolecules 2014, 15, 3550–3558. [Google Scholar] [CrossRef] [PubMed]
- Frohlich, E.; Roblegg, E. Mucus as barrier for drug delivery by nanoparticles. J. Nanosci. Nanotechnol. 2014, 14, 126–136. [Google Scholar] [CrossRef] [PubMed]
- Cao, Y.; Zhang, C.; Shen, W.; Cheng, Z.; Yu, L.L.; Ping, Q. Poly(n-isopropylacrylamide)–chitosan as thermosensitive in situ gel-forming system for ocular drug delivery. J. Control. Release 2007, 120, 186–194. [Google Scholar] [CrossRef] [PubMed]
- Mazumder, M.J.; Fitzpatrick, S.D.; Muirhead, B.; Sheardown, H. Cell-adhesive thermogelling pnipaam/hyaluronic acid cell delivery hydrogels for potential application as minimally invasive retinal therapeutics. J. Biomed. Mater. Res. Part A 2012, 100, 1877–1887. [Google Scholar] [CrossRef] [PubMed]
- Osmałek, T.; Froelich, A.; Tasarek, S. Application of gellan gum in pharmacy and medicine. Int. J. Pharm. 2014, 466, 328–340. [Google Scholar] [CrossRef]
- Janagam, D.R.; Wu, L.; Lowe, T.L. Nanoparticles for drug delivery to the anterior segment of the eye. Adv. Drug Deliv. Rev. 2017, 122, 31–64. [Google Scholar] [CrossRef]
- Patil, S.; Sharma, S.; Nimbalkar, A.; Pawar, A. Study of formulation variables on properties of drug-gellan beads by factorial design. Drug Dev. Ind. Pharm. 2006, 32, 315–326. [Google Scholar] [CrossRef]
- Miyazaki, S.; Aoyama, H.; Kawasaki, N.; Kubo, W.; Attwood, D. In situ-gelling gellan formulations as vehicles for oral drug delivery. J. Control. Release 1999, 60, 287–295. [Google Scholar] [CrossRef]
- Dwivedi, P.; Chand, P.; Gnanarajan, G.; Kotiyal, P. Review on ocular inserts. World J. Pharm. Res. 2015, 4, 493–523. [Google Scholar]
- Bhowmick, B.; Sarkar, G.; Rana, D.; Roy, I.; Saha, N.R.; Ghosh, S.; Bhowmik, M.; Chattopadhyay, D. Effect of carrageenan and potassium chloride on an in situ gelling ophthalmic drug delivery system based on methylcellulose. RSC Adv. 2015, 5, 60386–60391. [Google Scholar] [CrossRef]
- Yegappan, R.; Selvaprithiviraj, V.; Amirthalingam, S.; Jayakumar, R. Carrageenan based hydrogels for drug delivery, tissue engineering and wound healing. Carbohydr. Polym. 2018, 198, 385–400. [Google Scholar] [CrossRef] [PubMed]
- Jana, S.; Kumar Sen, K.; Gandhi, A. Alginate based nanocarriers for drug delivery applications. Curr. Pharm. Des. 2016, 22, 3399–3410. [Google Scholar] [CrossRef] [PubMed]
- Cohen, S.; Lobel, E.; Trevgoda, A.; Peled, Y. A novel in situ-forming ophthalmic drug delivery system from alginates undergoing gelation in the eye. J. Control. Release 1997, 44, 201–208. [Google Scholar] [CrossRef]
- Calles, J.A.; Bermúdez, J.; Vallés, E.; Allemandi, D.; Palma, S. Polymers in ophthalmology. In Advanced Polymers in Medicine; Puoci, F., Ed.; Springer International Publishing: Cham, Switzerland, 2015; pp. 147–176. [Google Scholar]
- Mittal, N.; Kaur, G. In situ gelling ophthalmic drug delivery system: Formulation and evaluation. J. Appl. Polym. Sci. 2014, 131, 39788. [Google Scholar] [CrossRef]
- Nagarwal, R.C.; Kumar, R.; Pandit, J. Chitosan coated sodium alginate–chitosan nanoparticles loaded with 5-FU for ocular delivery: In vitro characterization and in vivo study in rabbit eye. Eur. J. Pharm. Sci. 2012, 47, 678–685. [Google Scholar] [CrossRef]
- Ruel-Gariepy, E.; Leroux, J.-C. In situ-forming hydrogels—Review of temperature-sensitive systems. Eur. J. Pharm. Biopharm. 2004, 58, 409–426. [Google Scholar] [CrossRef]
- Dewan, M.; Bhowmick, B.; Sarkar, G.; Rana, D.; Bain, M.K.; Bhowmik, M.; Chattopadhyay, D. Effect of methyl cellulose on gelation behavior and drug release from poloxamer based ophthalmic formulations. Int. J. Biol. Macromol. 2015, 72, 706–710. [Google Scholar] [CrossRef]
- Marcos, X.; Pérez-Casas, S.; Llovo, J.; Concheiro, A.; Alvarez-Lorenzo, C. Poloxamer-hydroxyethyl cellulose-α-cyclodextrin supramolecular gels for sustained release of griseofulvin. Int. J. Pharm. 2016, 500, 11–19. [Google Scholar] [CrossRef]
- Soliman, K.A.; Ullah, K.; Shah, A.; Jones, D.S.; Singh, T.R.R. Poloxamer-based in situ gelling thermoresponsive systems for ocular drug delivery applications. Drug Discov. Today 2019, 24, 1575–1586. [Google Scholar] [CrossRef]
- Goyal, P.; Dhar, R.; Sagiri, S.S.; Uvanesh, K.; Senthilguru, K.; Shankar, G.; Samal, A.; Pramanik, K.; Banerjee, I.; Ray, S.S.; et al. Synthesis and characterization of novel dual environment-responsive hydrogels of hydroxyethyl methacrylate and methyl cellulose. Des. Monomers Polym. 2015, 18, 367–377. [Google Scholar] [CrossRef]
- García, M.C. Ionic-strength-responsive polymers for drug delivery applications. In Stimuli Responsive Polymeric Nanocarriers for Drug Delivery Applications; Elsevier: Amsterdam, The Netherlands, 2019; pp. 393–409. [Google Scholar]
- Gupta, S.; VYAS, S. Carbopol/chitosan based pH triggered in situ gelling system for ocular delivery of timolol maleate. Sci. Pharm. 2010, 78, 959–976. [Google Scholar] [CrossRef] [PubMed]
- Zaki, R.; Hosny, K.M.; Mohamed, A.K.; Abd-Elbary, A. Ketorolac tromethamine in-situ ocular hydro gel; preparation, characterization, and in-vivo evaluation. Int. J. Drug Deliv. 2011, 3, 535–545. [Google Scholar]
- Bertens, C.J.; Gijs, M.; van den Biggelaar, F.J.; Nuijts, R.M. Topical drug delivery devices: A review. Exp. Eye Res. 2018, 168, 149–160. [Google Scholar] [CrossRef] [PubMed]
- Jervis, L. A summary of recent advances in ocular inserts and implants. J. Bioequiv. Bioavailab. 2017, 9, 320–323. [Google Scholar]
- Al-Saedi, Z.H.; Alzhrani, R.M.; Boddu, S.H. Formulation and in vitro evaluation of cyclosporine—A inserts prepared using hydroxypropyl methylcellulose for treating dry eye disease. J. Ocul. Pharmacol. Ther. 2016, 32, 451–462. [Google Scholar] [CrossRef]
- Urtti, A.; Juslin, M.; Miinalainen, O. Pilocarpine release from hydroxypropyl-cellulose-polyvinylpyrrolidone matrices. Int. J. Pharm. 1985, 25, 165–178. [Google Scholar] [CrossRef]
- Everaert, A.; Wouters, Y.; Melsbach, E.; Zakaria, N.; Ludwig, A.; Kiekens, F.; Weyenberg, W. Optimisation of HPMC ophthalmic inserts with sustained release properties as a carrier for thermolabile therapeutics. Int. J. Pharm. 2017, 528, 395–405. [Google Scholar] [CrossRef]
- Khutoryanskaya, O.V.; Morrison, P.W.; Seilkhanov, S.K.; Mussin, M.N.; Ozhmukhametova, E.K.; Rakhypbekov, T.K.; Khutoryanskiy, V.V. Hydrogen-bonded complexes and blends of poly(acrylic acid) and methylcellulose: Nanoparticles and mucoadhesive films for ocular delivery of riboflavin. Macromol. Biosci. 2014, 14, 225–234. [Google Scholar] [CrossRef]
- Abilova, G.K.; Kaldybekov, D.B.; Ozhmukhametova, E.K.; Saimova, A.Z.; Kazybayeva, D.S.; Irmukhametova, G.S.; Khutoryanskiy, V.V. Chitosan/poly(2-ethyl-2-oxazoline) films for ocular drug delivery: Formulation, miscibility, in vitro and in vivo studies. Eur. Polym. J. 2019, 116, 311–320. [Google Scholar] [CrossRef]
- Gilhotra, R.; Mishra, D. Alginate-chitosan film for ocular drug delivery: Effect of surface cross-linking on film properties and characterization. Die Pharm. Int. J. Pharm. Sci. 2008, 63, 576–579. [Google Scholar]
- Mishra, D.; Gilhotra, R. Design and characterization of bioadhesive in-situ gelling ocular inserts of gatifloxacin sesquihydrate. Daru J. Pharm. Sci. 2008, 16, 1–8. [Google Scholar]
- Koelwel, C.; Rothschenk, S.; Fuchs-Koelwel, B.; Gabler, B.; Lohmann, C.; Göpferich, A. Alginate inserts loaded with epidermal growth factor for the treatment of keratoconjunctivitis sicca. Pharm. Dev. Technol. 2008, 13, 221–231. [Google Scholar] [CrossRef] [PubMed]
- Kaul, S.; Kumar, G.; Kothiyal, P. Design and evaluation of soluble ocular drug insert for controlled release of acyclovir. Int. J. Drug Res. Technol. 2017, 2, 393–398. [Google Scholar]
- Carvalho, I.M.; Marques, C.S.; Oliveira, R.S.; Coelho, P.B.; Costa, P.C.; Ferreira, D.C. Sustained drug release by contact lenses for glaucoma treatment—A review. J. Control. Release 2015, 202, 76–82. [Google Scholar] [CrossRef]
- Ali, M.; Byrne, M.E. Controlled release of high molecular weight hyaluronic acid from molecularly imprinted hydrogel contact lenses. Pharm. Res. 2009, 26, 714–726. [Google Scholar] [CrossRef]
- White, C.J.; McBride, M.K.; Pate, K.M.; Tieppo, A.; Byrne, M.E. Extended release of high molecular weight hydroxypropyl methylcellulose from molecularly imprinted, extended wear silicone hydrogel contact lenses. Biomaterials 2011, 32, 5698–5705. [Google Scholar] [CrossRef]
- Subrizi, A.; Del Amo, E.M.; Korzhikov-Vlakh, V.; Tennikova, T.; Ruponen, M.; Urtti, A. Design principles of ocular drug delivery systems: Importance of drug payload, release rate, and material properties. Drug Discov. Today 2019, 24, 1446–1457. [Google Scholar] [CrossRef]
- Tan, G.; Yu, S.; Pan, H.; Li, J.; Liu, D.; Yuan, K.; Yang, X.; Pan, W. Bioadhesive chitosan-loaded liposomes: A more efficient and higher permeable ocular delivery platform for timolol maleate. Int. J. Biol. Macromol. 2017, 94, 355–363. [Google Scholar] [CrossRef]
- Balguri, S.P.; Adelli, G.R.; Majumdar, S. Topical ophthalmic lipid nanoparticle formulations (SLN, NLC) of indomethacin for delivery to the posterior segment ocular tissues. Eur. J. Pharm. Biopharm. 2016, 109, 224–235. [Google Scholar] [CrossRef]
- Zeng, W.; Li, Q.; Wan, T.; Liu, C.; Pan, W.; Wu, Z.; Zhang, G.; Pan, J.; Qin, M.; Lin, Y. Hyaluronic acid-coated niosomes facilitate tacrolimus ocular delivery: Mucoadhesion, precorneal retention, aqueous humor pharmacokinetics, and transcorneal permeability. Colloids Surf. B 2016, 141, 28–35. [Google Scholar] [CrossRef] [PubMed]
- Zimmer, A.; Kreuter, J. Microspheres and nanoparticles used in ocular delivery systems. Adv. Drug Deliv. Rev. 1995, 16, 61–73. [Google Scholar] [CrossRef]
- Calvo, P.; Vila-Jato, J.L.; Alonso, M.A.J. Evaluation of cationic polymer-coated nanocapsules as ocular drug carriers. Int. J. Pharm. 1997, 153, 41–50. [Google Scholar] [CrossRef]
- Ibrahim, M.M.; Abd-Elgawad, A.-E.H.; Soliman, O.A.-E.; Jablonski, M.M. Natural bioadhesive biodegradable nanoparticle-based topical ophthalmic formulations for management of glaucoma. Transl. Vis. Sci. Technol. 2015, 4, 12. [Google Scholar] [CrossRef]
- Giunchedi, P.; Conte, U.; Chetoni, P.; Saettone, M.F. Pectin microspheres as ophthalmic carriers for piroxicam: Evaluation in vitro and in vivo in albino rabbits. Eur. J. Pharm. Sci. 1999, 9, 1–7. [Google Scholar] [CrossRef]
- Yuan, X.-B.; Li, H.; Yuan, Y.-B. Preparation of cholesterol-modified chitosan self-aggregated nanoparticles for delivery of drugs to ocular surface. Carbohydr. Polym. 2006, 65, 337–345. [Google Scholar] [CrossRef]
- De Campos, A.M.; Sánchez, A.; Alonso, M.A.J. Chitosan nanoparticles: A new vehicle for the improvement of the delivery of drugs to the ocular surface. Application to cyclosporin a. Int. J. Pharm. 2001, 224, 159–168. [Google Scholar] [CrossRef]
- Toropainen, E.; Hornof, M.; Kaarniranta, K.; Johansson, P.; Urtti, A. Corneal epithelium as a platform for secretion of transgene products after transfection with liposomal gene eyedrops. J. Gene Med. 2007, 9, 208–216. [Google Scholar] [CrossRef]
- De la Fuente, M.; Seijo, B.; Alonso, M. Bioadhesive hyaluronan–chitosan nanoparticles can transport genes across the ocular mucosa and transfect ocular tissue. Gene Ther. 2008, 15, 668–676. [Google Scholar] [CrossRef]
- Gudmundsdottir, E.; Stefansson, E.; Bjarnadottir, G.; Sigurjonsdottir, J.F.; Gudmundsdottir, G.; Masson, M.; Loftsson, T. Methazolamide 1% in cyclodextrin solution lowers iop in human ocular hypertension. Investig. Ophthalmol. Vis. Sci. 2000, 41, 3552–3554. [Google Scholar]
- Kristinsson, J.K.; Fridriksdottir, H.; Thorisdottir, S.; Sigurdardottir, A.M.; Stefansson, E.; Loftsson, T. Dexamethasone-cyclodextrin-polymer co-complexes in aqueous eye drops. Aqueous humor pharmacokinetics in humans. Investig. Ophthalmol. Vis. Sci. 1996, 37, 1199–1203. [Google Scholar]
- Palma, S.D.; Tartara, L.I.; Quinteros, D.; Allemandi, D.A.; Longhi, M.R.; Granero, G.E. An efficient ternary complex of acetazolamide with hp-ss-cd and tea for topical ocular administration. J. Control. Release 2009, 138, 24–31. [Google Scholar] [CrossRef] [PubMed]
- Jarho, P.; Urtti, A.; Pate, D.W.; Suhonen, P.; Järvinen, T. Increase in aqueous solubility, stability and in vitro corneal permeability of anandamide by hydroxypropyl-β-cyclodextrin. Int. J. Pharm. 1996, 137, 209–216. [Google Scholar] [CrossRef]
- Suhonen, P.; Jarvinen, T.; Lehmussaari, K.; Reunamaki, T.; Urtti, A. Ocular absorption and irritation of pilocarpine prodrug is modified with buffer, polymer, and cyclodextrin in the eyedrop. Pharm. Res. 1995, 12, 529–533. [Google Scholar] [CrossRef]
- Jarho, P.; Jarvinen, K.; Urtti, A.; Stella, V.J.; Jarvinen, T. Modified β-cyclodextrin (SBE7-β-CyD) with viscous vehicle improves the ocular delivery and tolerability of pilocarpine prodrug in rabbits. J. Pharm. Pharmacol. 1996, 48, 263–269. [Google Scholar] [CrossRef]
- Pate, D.W.; Järvinen, K.; Urtti, A.; Jarhol, P.; Fich, M.; Mahadevan, V.; Järvinen, T. Effects of topical anandamides on intraocular pressure in normotensive rabbits. Life Sci. 1996, 58, 1849–1860. [Google Scholar] [CrossRef]
- Loftsson, T.; Stefansson, E. Cyclodextrins and topical drug delivery to the anterior and posterior segments of the eye. Int. J. Pharm. 2017, 531, 413–423. [Google Scholar] [CrossRef]
- Wong, W.L.; Su, X.; Li, X.; Cheung, C.M.; Klein, R.; Cheng, C.Y.; Wong, T.Y. Global prevalence of age-related macular degeneration and disease burden projection for 2020 and 2040: A systematic review and meta-analysis. Lancet Glob. Health 2014, 2, e106–e116. [Google Scholar] [CrossRef]
- Villanueva, J.R.; Villanueva, L.R.; Navarro, M.G. Pharmaceutical technology can turn a traditional drug, dexamethasone into a first-line ocular medicine. A global perspective and future trends. Int. J. Pharm. 2017, 516, 342–351. [Google Scholar] [CrossRef]
- Michalska-Malecka, K.; Gaborek, A.; Nowak, M.; Halat, T.; Pawlowska, M.; Spiewak, D. Evaluation of the effectiveness and safety of glucocorticoids intravitreal implant therapy in macular edema due to retinal vein occlusion. Clin. Interv. Aging 2016, 11, 699–705. [Google Scholar] [CrossRef]
- Wang, X.Z.; Wang, S.R.; Zhang, Y. Advance of the application of nano-controlled release system in ophthalmic drug delivery. Drug Deliv. 2016, 23, 2897–2901. [Google Scholar] [CrossRef] [PubMed]
- Pearce, W.; Hsu, J.; Yeh, S. Advances in drug delivery to the posterior segment. Curr. Opin. Ophthalmol. 2015, 26, 233–239. [Google Scholar] [CrossRef] [PubMed]
- Kang-Mieler, J.J.; Osswald, C.R.; Mieler, W.F. Advances in ocular drug delivery: Emphasis on the posterior segment. Expert Opin. Drug Deliv. 2014, 11, 1647–1660. [Google Scholar] [CrossRef] [PubMed]
- Bisht, R.; Mandal, A.; Jaiswal, J.K.; Rupenthal, I.D. Nanocarrier mediated retinal drug delivery: Overcoming ocular barriers to treat posterior eye diseases. Wiley Interdiscip. Rev. Nanomed. Nanobiotechnol. 2018, 10, e1473. [Google Scholar] [CrossRef] [PubMed]
- Hennig, R.; Goepferich, A. Nanoparticles for the treatment of ocular neovascularizations. Eur. J. Pharm. Biopharm. 2015, 95, 294–306. [Google Scholar] [CrossRef] [PubMed]
- Shen, H.H.; Chan, E.C.; Lee, J.H.; Bee, Y.S.; Lin, T.W.; Dusting, G.J.; Liu, G.S. Nanocarriers for treatment of ocular neovascularization in the back of the eye: New vehicles for ophthalmic drug delivery. Nanomedicine 2015, 10, 2093–2107. [Google Scholar] [CrossRef]
- Shatz, W.; Aaronson, J.; Yohe, S.; Kelley, R.F.; Kalia, Y.N. Strategies for modifying drug residence time and ocular bioavailability to decrease treatment frequency for back of the eye diseases. Expert Opin. Drug Deliv. 2019, 16, 43–57. [Google Scholar] [CrossRef]
- Peynshaert, K.; Devoldere, J.; De Smedt, S.C.; Remaut, K. In vitro and ex vivo models to study drug delivery barriers in the posterior segment of the eye. Adv. Drug Deliv. Rev. 2018, 126, 44–57. [Google Scholar] [CrossRef]
- Kamaleddin, M.A. Nano-ophthalmology: Applications and considerations. Nanomed.-Nanotechnol. Biol. Med. 2017, 13, 1459–1472. [Google Scholar] [CrossRef]
- Joseph, R.R.; Venkatraman, S.S. Drug delivery to the eye: What benefits do nanocarriers offer? Nanomedicine 2017, 12, 683–702. [Google Scholar] [CrossRef]
- Jo, D.H.; Kim, J.H.; Lee, T.G.; Kim, J.H. Size, surface charge, and shape determine therapeutic effects of nanoparticles on brain and retinal diseases. Nanomed. Nanotechnol. Biol. Med. 2015, 11, 1603–1611. [Google Scholar] [CrossRef] [PubMed]
- Mains, J.; Wilson, C.G. The vitreous humor as a barrier to nanoparticle distribution. J. Ocul. Pharmacol. Ther. 2013, 29, 143–150. [Google Scholar] [CrossRef] [PubMed]
- Awwad, S.; Ahmed, A.; Sharma, G.; Heng, J.S.; Khaw, P.T.; Brocchini, S.; Lockwood, A. Principles of pharmacology in the eye. Br. J. Pharmacol. 2017, 174, 4205–4223. [Google Scholar] [CrossRef] [PubMed]
- Bishop, P.N. Structural macromolecules and supramolecular organisation of the vitreous gel. Prog. Retin. Eye Res. 2000, 19, 323–344. [Google Scholar] [CrossRef]
- Huang, D.; Chen, Y.S.; Green, C.R.; Rupenthal, I.D. Hyaluronic acid coated albumin nanoparticles for targeted peptide delivery in the treatment of retinal ischaemia. Biomaterials 2018, 168, 10–23. [Google Scholar] [CrossRef] [PubMed]
- Kaur, I.P.; Kakkar, S. Nanotherapy for posterior eye diseases. J. Control. Release 2014, 193, 100–112. [Google Scholar] [CrossRef] [PubMed]
- Lau, C.M.L.; Yu, Y.; Jahamir, G.; Chau, Y. Controlled release technology for anti-angiogenesis treatment of posterior eye diseases: Current status and challenges. Adv. Drug Deliv. Rev. 2018, 126, 145–161. [Google Scholar] [CrossRef]
- Thakur, S.S.; Barnett, N.L.; Donaldson, M.J.; Parekh, H.S. Intravitreal drug delivery in retinal disease: Are we out of our depth? Expert Opin. Drug Deliv. 2014, 11, 1575–1590. [Google Scholar] [CrossRef]
- Del Amo, E.M.; Rimpela, A.K.; Heikkinen, E.; Kari, O.K.; Ramsay, E.; Lajunen, T.; Schmitt, M.; Pelkonen, L.; Bhattacharya, M.; Richardson, D.; et al. Pharmacokinetic aspects of retinal drug delivery. Prog. Retin. Eye Res. 2017, 57, 134–185. [Google Scholar] [CrossRef]
- Del Amo, E.M.; Vellonen, K.S.; Kidron, H.; Urtti, A. Intravitreal clearance and volume of distribution of compounds in rabbits: In silico prediction and pharmacokinetic simulations for drug development. Eur. J. Pharm. Biopharm. 2015, 95, 215–226. [Google Scholar] [CrossRef]
- Kim, H.; Robinson, S.B.; Csaky, K.G. Investigating the movement of intravitreal human serum albumin nanoparticles in the vitreous and retina. Pharm. Res. 2009, 26, 329–337. [Google Scholar] [CrossRef] [PubMed]
- Koo, H.; Moon, H.; Han, H.; Na, J.H.; Huh, M.S.; Park, J.H.; Wood, S.J.; Park, K.H.; Kwon, I.C.; Kim, K.; et al. The movement of self-assembled amphiphilic polymeric nanoparticles in the vitreous and retina after intravitreal injection. Biomaterials 2012, 33, 3485–3493. [Google Scholar] [CrossRef] [PubMed]
- Pitkanen, L.; Pelkonen, J.; Ruponen, M.; Ronkko, S.; Urtti, A. Neural retina limits the nonviral gene transfer to retinal pigment epithelium in an in vitro bovine eye model. AAPS J. 2004, 6, e25. [Google Scholar] [CrossRef] [PubMed]
- Pitkanen, L.; Ruponen, M.; Nieminen, J.; Urtti, A. Vitreous is a barrier in nonviral gene transfer by cationic lipids and polymers. Pharm. Res. 2003, 20, 576–583. [Google Scholar] [CrossRef] [PubMed]
- Martens, T.F.; Vercauteren, D.; Forier, K.; Deschout, H.; Remaut, K.; Paesen, R.; Ameloot, M.; Engbersen, J.F.J.; Demeester, J.; De Smedt, S.C.; et al. Measuring the intravitreal mobility of nanomedicines with single-particle tracking microscopy. Nanomedicine 2013, 8, 1955–1968. [Google Scholar] [CrossRef]
- Manna, S.; Augsburger, J.J.; Correa, Z.M.; Landero, J.A.; Banerjee, R.K. Development of chitosan and polylactic acid based methotrexate intravitreal micro-implants to treat primary intraocular lymphoma: An in vitro study. J. Biomech. Eng. Trans. Asme 2014, 136, 021018. [Google Scholar] [CrossRef]
- Ramsay, E.; Hagstrom, M.; Vellonen, K.S.; Boman, S.; Toropainen, E.; del Amo, E.M.; Kidron, H.; Urtti, A.; Ruponen, M. Role of retinal pigment epithelium permeability in drug transfer between posterior eye segment and systemic blood circulation. Eur. J. Pharm. Biopharm. 2019, 143, 18–23. [Google Scholar] [CrossRef]
- Thrimawithana, T.R.; Young, S.; Bunt, C.R.; Green, C.; Alany, R.G. Drug delivery to the posterior segment of the eye. Drug Discov. Today 2011, 16, 270–277. [Google Scholar] [CrossRef]
- Kirchhof, S.; Goepferich, A.M.; Brandl, F.P. Hydrogels in ophthalmic applications. Eur. J. Pharm. Biopharm. 2015, 95, 227–238. [Google Scholar] [CrossRef]
- Yu, Y.; Lau, L.C.M.; Lo, A.C.Y.; Chau, Y. Injectable chemically crosslinked hydrogel for the controlled release of bevacizumab in vitreous: A 6-month in vivo study. Transl. Vis. Sci. Technol. 2015, 4, 5. [Google Scholar] [CrossRef]
- Gavini, E.; Bonferoni, M.C.; Rassu, G.; Obinu, A.; Ferrari, F.; Giunchedi, P. Biodegradable microspheres as intravitreal delivery systems for prolonged drug release. What is their eminence in the nanoparticle era? Curr. Drug Deliv. 2018, 15, 930–940. [Google Scholar] [CrossRef] [PubMed]
- Wang, F.X.; He, S.Z.; Chen, B. Retinoic acid-loaded alginate microspheres as a slow release drug delivery carrier for intravitreal treatment. Biomed. Pharmacother. 2018, 97, 722–728. [Google Scholar] [CrossRef] [PubMed]
- Elsaid, N.; Jackson, T.L.; Elsaid, Z.; Alqathania, A.; Somavarapu, S. Plga microparticles entrapping chitosan-based nanoparticles for the ocular delivery of ranibizumab. Mol. Pharm. 2016, 13, 2923–2940. [Google Scholar] [CrossRef] [PubMed]
- Huang, D.; Chen, Y.S.; Rupenthal, I.D. Hyaluronic acid coated albumin nanoparticles for targeted peptide delivery to the retina. Mol. Pharm. 2017, 14, 533–545. [Google Scholar] [CrossRef] [PubMed]
- Gan, L.; Wang, J.; Zhao, Y.N.; Chen, D.; Zhu, C.L.; Liu, J.P.; Gan, Y. Hyaluronan-modified core-shell liponanoparticles targeting CD44-positive retinal pigment epithelium cells via intravitreal injection. Biomaterials 2013, 34, 5978–5987. [Google Scholar] [CrossRef] [PubMed]
- Andrei, G.; Peptu, C.A.; Popa, M.; Desbrieres, J.; Peptu, C.; Gardikiotis, F.; Costuleanu, M.; Costin, D.; Dupin, J.C.; Uhart, A.; et al. Formulation and evaluation of cefuroxim loaded submicron particles for ophthalmic delivery. Int. J. Pharm. 2015, 493, 16–29. [Google Scholar] [CrossRef]
- Mitra, R.N.; Gao, R.J.; Zheng, M.; Wu, M.J.; Voinov, M.A.; Smirnov, A.I.; Smirnova, T.I.; Wang, K.; Chavala, S.; Han, Z.C. Glycol chitosan engineered autoregenerative antioxidant significantly attenuates pathological damages in models of age-related macular degeneration. ACS Nano 2017, 11, 4669–4685. [Google Scholar] [CrossRef]
- Lee, J.; Ryoo, N.K.; Han, H.; Hong, H.K.; Park, J.Y.; Park, S.J.; Kim, Y.K.; Sim, C.; Kim, K.; Woo, S.J.; et al. Anti-VEGF polysiRNA polyplex for the treatment of choroidal neovascularization. Mol. Pharm. 2016, 13, 1988–1995. [Google Scholar] [CrossRef]
- Martens, T.F.; Remaut, K.; Deschout, H.; Engbersen, J.F.J.; Hennink, W.E.; van Steenbergen, M.J.; Demeester, J.; De Smedt, S.C.; Braeckmans, K. Coating nanocarriers with hyaluronic acid facilitates intravitreal drug delivery for retinal gene therapy. J. Control. Release 2015, 202, 83–92. [Google Scholar] [CrossRef]
- Shatz, W.; Hass, P.E.; Mathieu, M.; Kim, H.S.; Leach, K.; Zhou, M.; Crawford, Y.; Shen, A.; Wang, K.; Chang, D.P.; et al. Contribution of antibody hydrodynamic size to vitreal clearance revealed through rabbit studies using a species-matched fab. Mol. Pharm. 2016, 13, 2996–3003. [Google Scholar] [CrossRef]
- Altiok, E.I.; Santiago-Ortiz, J.L.; Svedlund, F.L.; Zbinden, A.; Jha, A.K.; Bhatnagar, D.; Loskill, P.; Jackson, W.M.; Schaffer, D.V.; Healy, K.E. Multivalent hyaluronic acid bioconjugates improve sF1t-1 activity in vitro. Biomaterials 2016, 93, 95–105. [Google Scholar] [CrossRef] [PubMed]
- Altiok, E.I.; Browne, S.; Khuc, E.; Moran, E.P.; Qiu, F.F.; Zhou, K.L.; Santiago-Ortiz, J.L.; Ma, J.X.; Chan, M.F.; Healy, K.E. sFlt multivalent conjugates inhibit angiogenesis and improve half-life in vivo. PLoS ONE 2016, 11, e0155990. [Google Scholar] [CrossRef] [PubMed]
- Del Amo, E.M.; Urtti, A. Current and future ophthalmic drug delivery systems. A shift to the posterior segment. Drug Discov. Today 2008, 13, 135–143. [Google Scholar] [CrossRef] [PubMed]
- Van Kampen, E.; Vandervelden, C.; Fakhari, A.; Qian, J.; Berkland, C.; Gehrke, S.H. Design of hollow hyaluronic acid cylinders for sustained intravitreal protein delivery. J. Pharm. Sci. 2018, 107, 2354–2365. [Google Scholar] [CrossRef] [PubMed]
- Badiee, P.; Varshochian, R.; Rafiee-Tehrani, M.; Dorkoosh, F.A.; Khoshayand, M.R.; Dinarvand, R. Ocular implant containing bevacizumab-loaded chitosan nanoparticles intended for choroidal neovascularization treatment. J. Biomed. Mater. Res. Part A 2018, 106, 2261–2271. [Google Scholar] [CrossRef]
- Ranta, V.P.; Mannermaa, E.; Lummepuro, K.; Subrizi, A.; Laukkanen, A.; Antopolsky, M.; Murtomaki, L.; Hornof, M.; Urtti, A. Barrier analysis of periocular drug delivery to the posterior segment. J. Control. Release 2010, 148, 42–48. [Google Scholar] [CrossRef]
- Amrite, A.C.; Kompella, U.B. Size-dependent disposition of nanoparticles and microparticles following subconjunctival administration. J. Pharm. Pharmacol. 2005, 57, 1555–1563. [Google Scholar] [CrossRef]
- Wen, H.; Hao, J.; Li, S.K. Characterization of human sclera barrier properties for transscleral delivery of bevacizumab and ranibizumab. J. Pharm. Sci. 2013, 102, 892–903. [Google Scholar] [CrossRef]
- Voss, K.; Falke, K.; Bernsdorf, A.; Grabow, N.; Kastner, C.; Sternberg, K.; Minrath, I.; Eickner, T.; Wree, A.; Schmitz, K.-P. Development of a novel injectable drug delivery system for subconjunctival glaucoma treatment. J. Control. Release 2015, 214, 1–11. [Google Scholar] [CrossRef]
- Zarembinski, T.I.; Doty, N.J.; Erickson, I.E.; Srinivas, R.; Wirostko, B.M.; Tew, W.P. Thiolated hyaluronan-based hydrogels crosslinked using oxidized glutathione: An injectable matrix designed for ophthalmic applications. Acta Biomater. 2014, 10, 94–103. [Google Scholar] [CrossRef]
- Cheng, Y.-H.; Hung, K.-H.; Tsai, T.-H.; Lee, C.-J.; Ku, R.-Y.; Chiu, A.W.-h.; Chiou, S.-H.; Liu, C.J.-l. Sustained delivery of latanoprost by thermosensitive chitosan–gelatin-based hydrogel for controlling ocular hypertension. Acta Biomater. 2014, 10, 4360–4366. [Google Scholar] [CrossRef] [PubMed]
- Yang, L.-Q.; Lan, Y.-Q.; Guo, H.; Cheng, L.-Z.; Fan, J.-Z.; Cai, X.; Zhang, L.-M.; Chen, R.-F.; Zhou, H.-S. Ophthalmic drug-loaded N,O-carboxymethyl chitosan hydrogels: Synthesis, in vitro and in vivo evaluation. Acta Pharmacol. Sin. 2010, 31, 1625–1634. [Google Scholar] [CrossRef] [PubMed]
- Hsiao, M.-H.; Chiou, S.-H.; Larsson, M.; Hung, K.-H.; Wang, Y.-L.; Liu, C.J.-L.; Liu, D.-M. A temperature-induced and shear-reversible assembly of latanoprost-loaded amphiphilic chitosan colloids: Characterization and in vivo glaucoma treatment. Acta Biomater. 2014, 10, 3188–3196. [Google Scholar] [CrossRef] [PubMed]
- Thrimawithana, T.; Young, S.; Bunt, C.; Green, C.; Alany, R. In-vitro and in-vivo evaluation of carrageenan/methylcellulose polymeric systems for transscleral delivery of macromolecules. Eur. J. Pharm. Sci. 2011, 44, 399–409. [Google Scholar] [CrossRef]
- Wu, X.; Yang, X.; Jiang, H.; Xu, Y.; Liu, T.; Zang, X.; Gong, H. Safety evaluation of intracameral and subconjunctival injection of a novel mucoadhesive polysaccharide isolated from bletilla striata in rabbit eye. J. Ocul. Pharmacol. Ther. 2012, 28, 369–380. [Google Scholar] [CrossRef]
- Rong, X.; Yang, J.; Ji, Y.; Zhu, X.; Lu, Y.; Mo, X. Biocompatibility and safety of insulin-loaded chitosan nanoparticles/PLGA-PEG-PLGA hydrogel (ICNPH) delivered by subconjunctival injection in rats. J. Drug Deliv. Sci. Technol. 2019, 49, 556–562. [Google Scholar] [CrossRef]
- Chiang, B.; Venugopal, N.; Edelhauser, H.F.; Prausnitz, M.R. Distribution of particles, small molecules and polymeric formulation excipients in the suprachoroidal space after microneedle injection. Exp. Eye Res. 2016, 153, 101–109. [Google Scholar] [CrossRef]
- Jung, J.H.; Desit, P.; Prausnitz, M.R. Targeted drug delivery in the suprachoroidal space by swollen hydrogel pushing. Investig. Ophthalmol. Vis. Sci. 2018, 59, 2069–2079. [Google Scholar] [CrossRef]
- Wassmer, S.; Rafat, M.; Fong, W.G.; Baker, A.N.; Tsilfidis, C. Chitosan microparticles for delivery of proteins to the retina. Acta Biomater. 2013, 9, 7855–7864. [Google Scholar] [CrossRef]
- Mitra, R.N.; Han, Z.; Merwin, M.; Al Taai, M.; Conley, S.M.; Naash, M.I. Synthesis and characterization of glycol chitosan DNA nanoparticles for retinal gene delivery. ChemMedChem 2014, 9, 189–196. [Google Scholar] [CrossRef]
- Puras, G.; Zarate, J.; Diaz-Tahoces, A.; Avilés-Trigueros, M.; Fernandez, E.; Pedraz, J. Oligochitosan polyplexes as carriers for retinal gene delivery. Eur. J. Pharm. Sci. 2013, 48, 323–331. [Google Scholar] [CrossRef] [PubMed]
- Chen, S.; Yan, H.; Sun, B.; Zuo, A.; Liang, D. Subretinal transfection of chitosan-loaded TLR3-siRNA for the treatment of experimental autoimmune uveitis. Eur. J. Pharm. Biopharm. 2013, 85, 726–735. [Google Scholar] [CrossRef] [PubMed]
| Polysaccharide | Administration 1 | Drug Dosage Form | Max Potency 2 | Brand Names |
|---|---|---|---|---|
| Alginate sodium | T | insert | 1 mg | - |
| Carboxymethyl cellulose sodium | IVT, T | suspension, injection, solution | 0.5% | Refresh Tears |
| Guar gum | T | suspension | 0.2% | - |
| Hyaluronate sodium | IVT | injectable solution | 2.3% | Healon, Amvisc, Provisc, AMO Vitrax |
| Hydroxyethyl cellulose | T | solution, suspension | 0.25–1.6% | Rohto Hydra |
| Hydroxyethyl ethylcellulose | T | solution | 0.48% | - |
| Hyproxypropyl methylcellulose | T | solution, suspension, gel | 0.1–0.6%; 2.25% (gel) | Genteal, Nature’s Tears, Tearisol |
| Methylcellulose | T | solution, suspension | 0.05–0.5% | Murocel |
| Microcrystalline cellulose | IVT | implant | 1.66 mg | Retisert |
| Xanthan gum | T | solution, suspension | 0.6% | I-Dew Ultra |
© 2019 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Dubashynskaya, N.; Poshina, D.; Raik, S.; Urtti, A.; Skorik, Y.A. Polysaccharides in Ocular Drug Delivery. Pharmaceutics 2020, 12, 22. https://doi.org/10.3390/pharmaceutics12010022
Dubashynskaya N, Poshina D, Raik S, Urtti A, Skorik YA. Polysaccharides in Ocular Drug Delivery. Pharmaceutics. 2020; 12(1):22. https://doi.org/10.3390/pharmaceutics12010022
Chicago/Turabian StyleDubashynskaya, Natallia, Daria Poshina, Sergei Raik, Arto Urtti, and Yury A. Skorik. 2020. "Polysaccharides in Ocular Drug Delivery" Pharmaceutics 12, no. 1: 22. https://doi.org/10.3390/pharmaceutics12010022
APA StyleDubashynskaya, N., Poshina, D., Raik, S., Urtti, A., & Skorik, Y. A. (2020). Polysaccharides in Ocular Drug Delivery. Pharmaceutics, 12(1), 22. https://doi.org/10.3390/pharmaceutics12010022








