Physicochemical, Pharmacokinetic, and Toxicity Evaluation of Methoxy Poly(ethylene glycol)-b-Poly(d,l-Lactide) Polymeric Micelles Encapsulating Alpinumisoflavone Extracted from Unripe Cudrania tricuspidata Fruit
Abstract
:1. Introduction
2. Materials and Methods
2.1. Materials and Reagents
2.2. Methods
2.2.1. Collection of Unripe C. Tricuspidata Fruit and Isolation of AIF
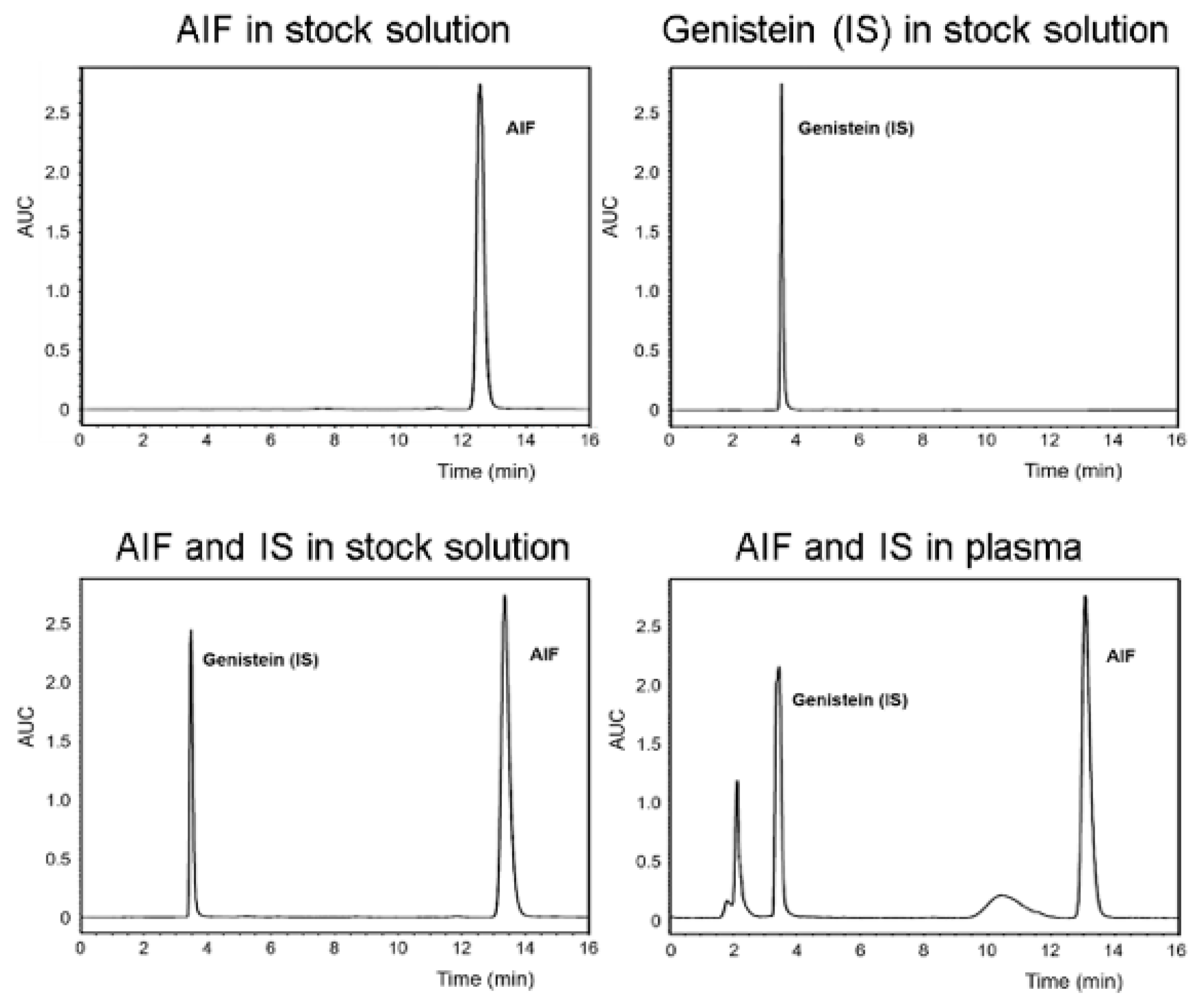
2.2.2. High-Performance Liquid Chromatography (HPLC) Analysis
2.2.3. Determination of AIF Solubility
2.2.4. Preparation of AIF-Loaded Micelles
2.2.5. Physicochemical Characterization of Micelles
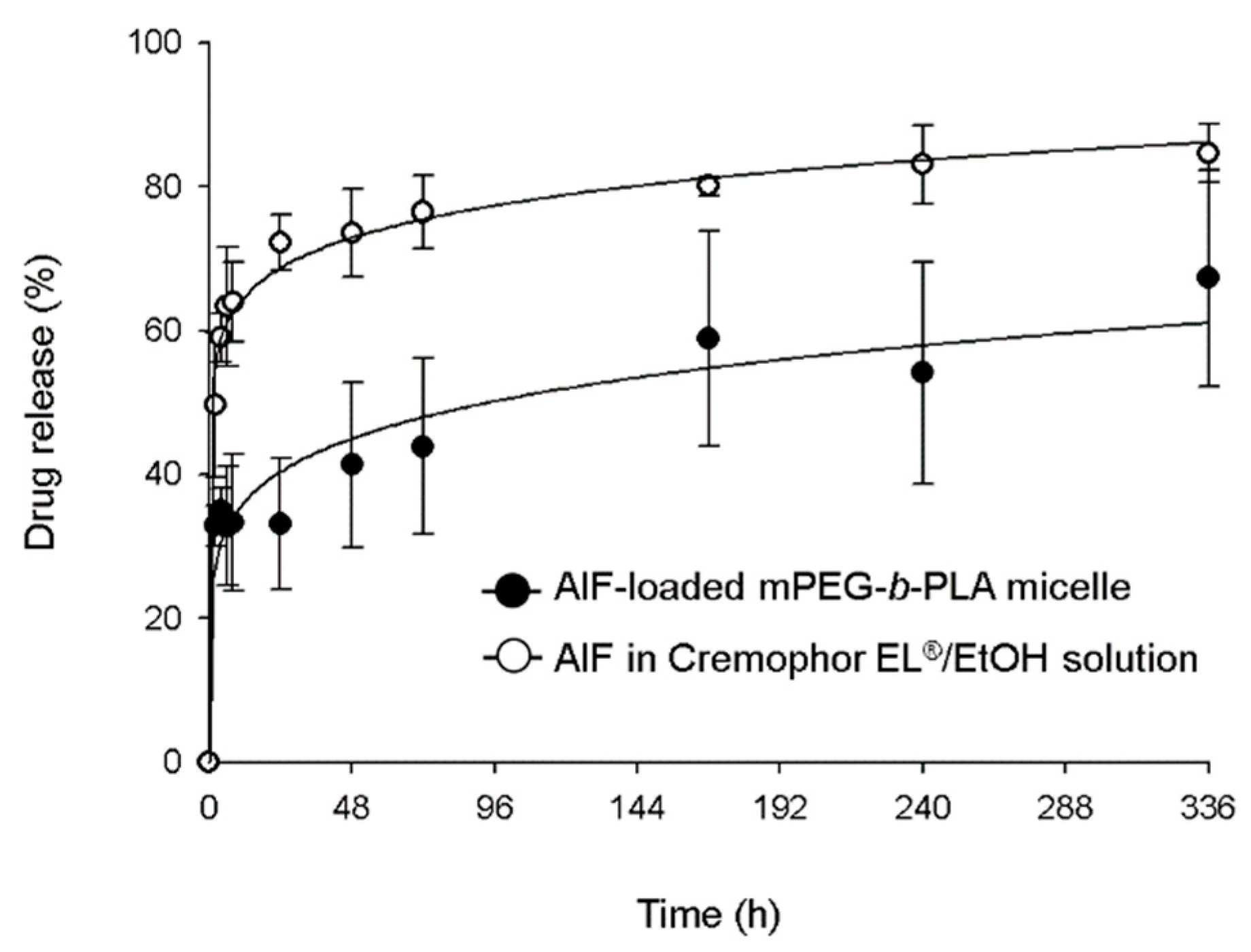
2.2.6. In Vitro Drug Release Assay
2.2.7. Pharmacokinetic Study
2.2.8. Biodistribution Study
2.2.9. Pre-Treatment of Biological Samples for HPLC Analysis
2.2.10. In Vivo Toxicity Assay
2.2.11. Statistical Analysis
3. Results and Discussion
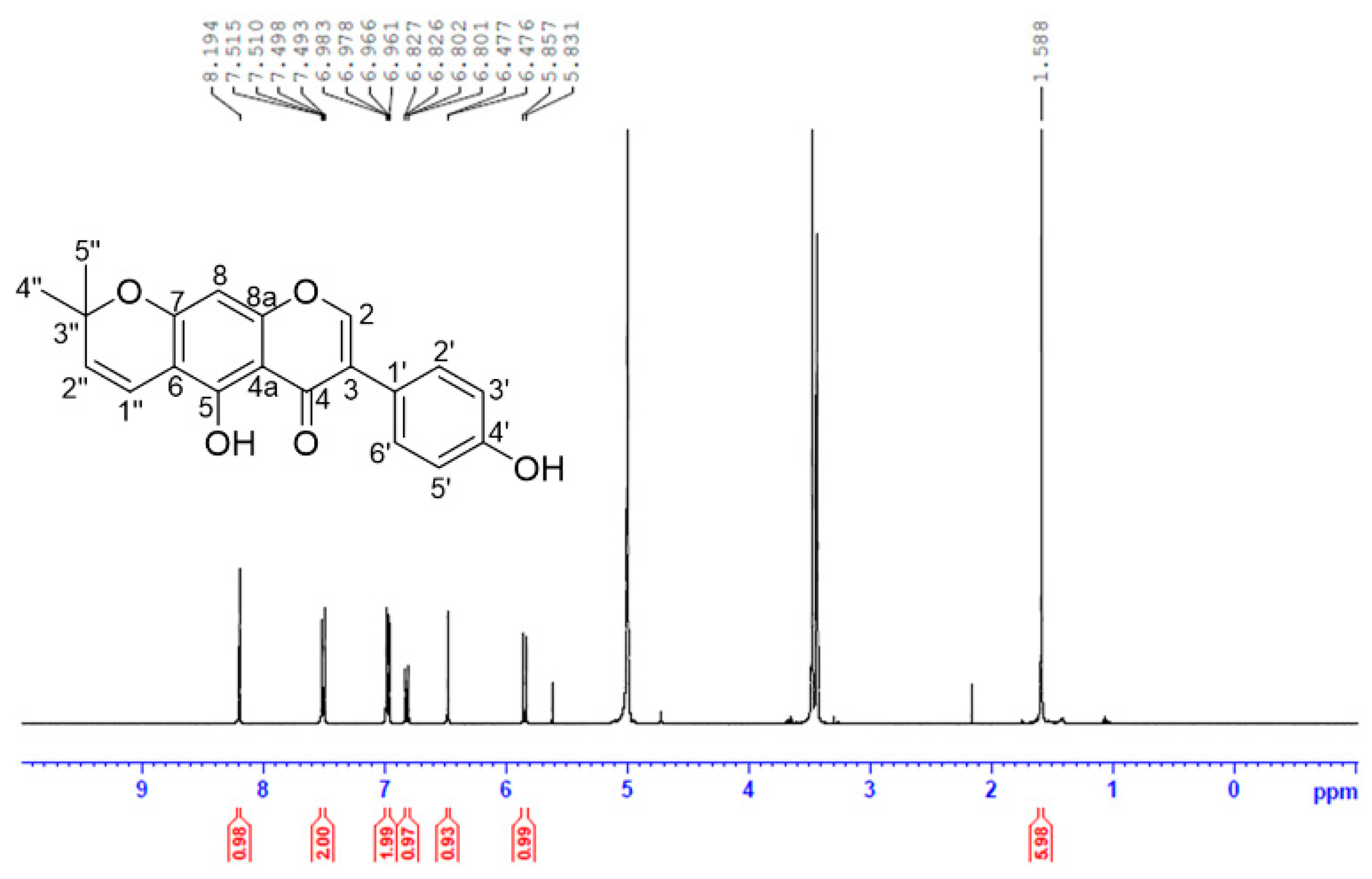
3.1. Isolation and Identification of AIF
3.2. Determination of AIF Solubility
3.3. Physicochemical Characterization of AIF-Loaded Micelles
3.4. In Vitro Drug Release Profile
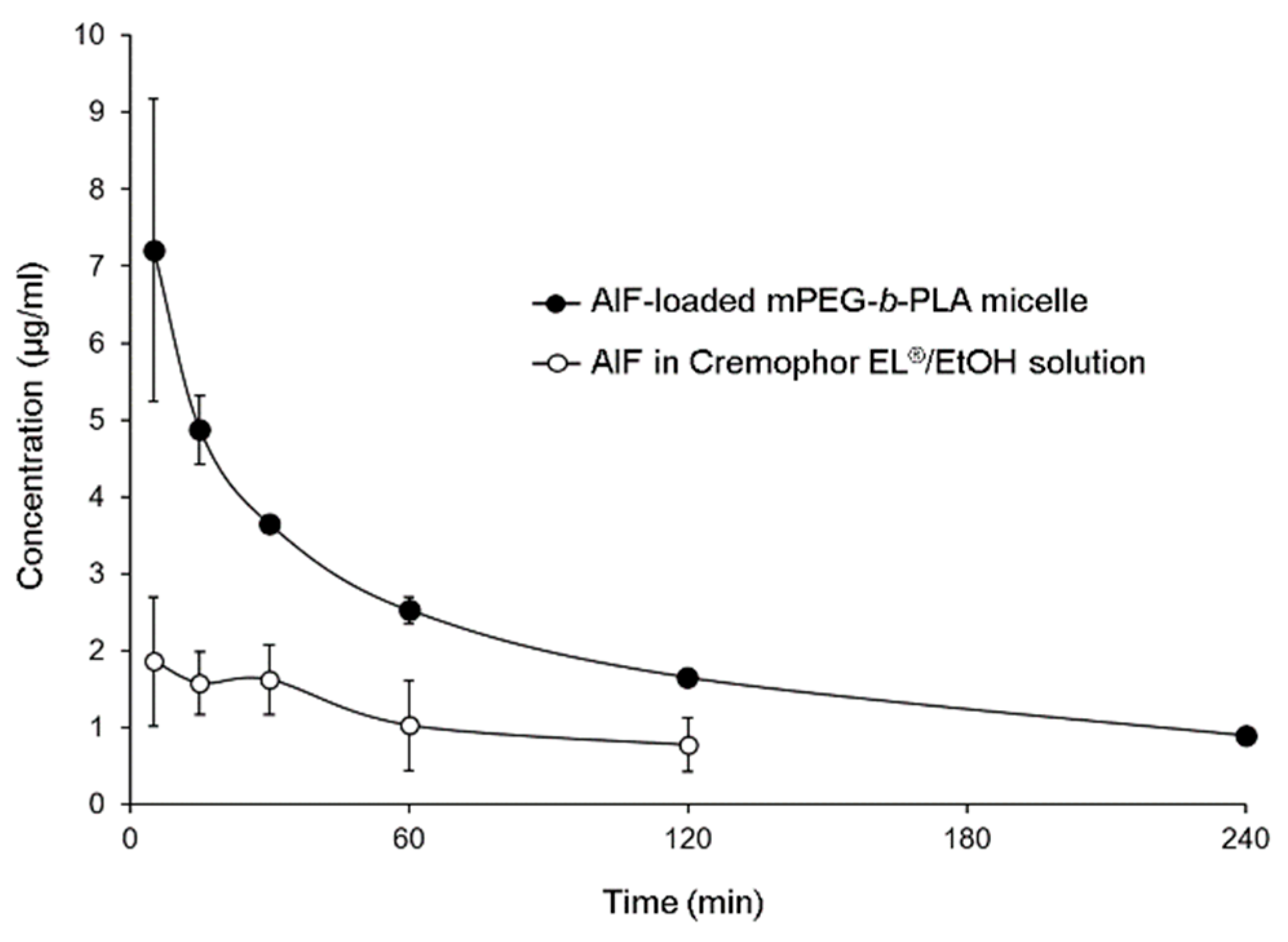
3.5. Pharmacokinetics of AIF in Rats
3.6. Biodistribution of Micelles in Rats
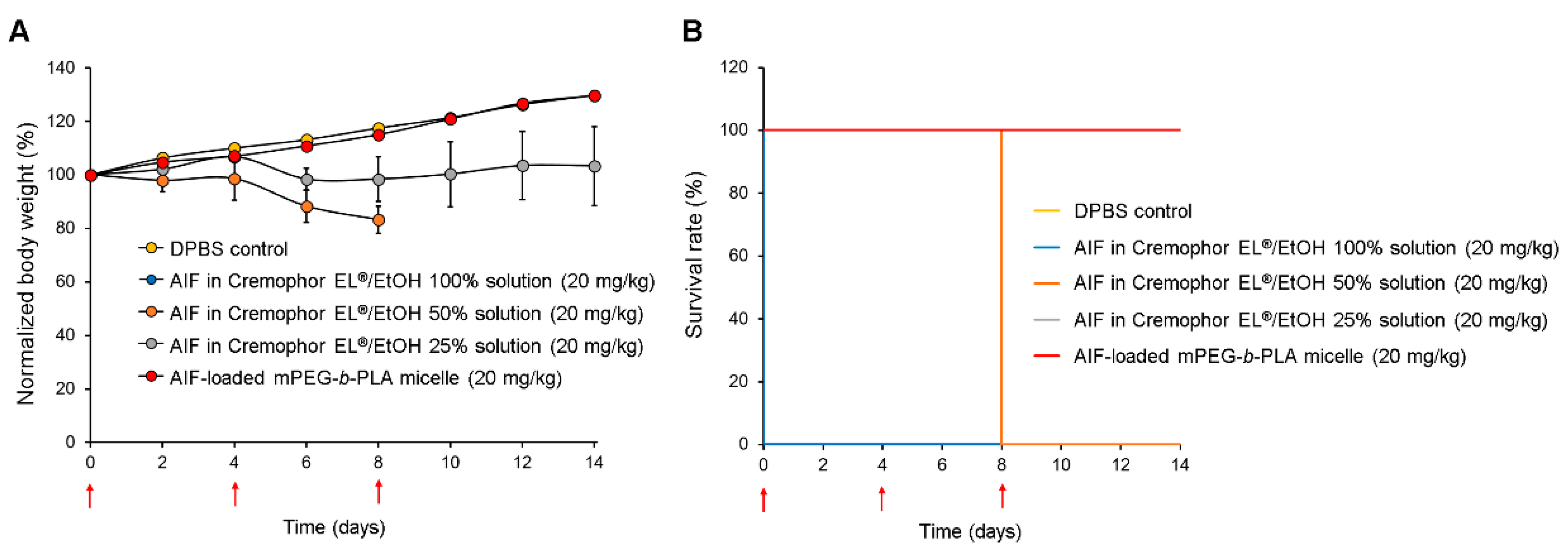
3.7. In Vivo Toxicity Assay
4. Conclusions
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- Xin, L.T.; Yue, S.J.; Fan, Y.C.; Wu, J.S.; Yan, D.; Guan, H.S.; Wang, C.Y. Cudrania tricuspidata: An updated review on ethnomedicine, phytochemistry and pharmacology. RSC Adv. 2017, 7, 31807–31832. [Google Scholar] [CrossRef]
- Jo, Y.H.; Kim, S.B.; Liu, Q.; Do, S.G.; Hwang, B.Y.; Lee, M.K. Comparison of pancreatic lipase inhibitory isoflavonoids from unripe and ripe fruits of Cudrania tricuspidata. PLoS ONE 2017, 12, e0172069. [Google Scholar] [CrossRef] [PubMed]
- Namkoong, S.; Kim, T.J.; Jang, I.S.; Kang, K.W.; Oh, W.K.; Park, J. Alpinumisoflavone Induces Apoptosis and Suppresses Extracellular Signal-Regulated Kinases/Mitogen Activated Protein Kinase and Nuclear Factor-Kappa; B Pathways in Lung Tumor Cells. Biol. Pharm. Bull. 2011, 34, 203–208. [Google Scholar] [CrossRef] [PubMed]
- Gao, M.; Chang, Y.; Wang, X.; Ban, C.; Zhang, F. Reduction of COX-2 through modulating miR-124/SPHK1 axis contributes to the antimetastatic effect of alpinumisoflavone in melanoma. Am. J. Transl. Res. 2017, 9, 986–998. [Google Scholar] [PubMed]
- Kingsford-Adaboh, R.; Dittrich, B.; Hubschle, C.B.; Gbewonyo, W.S.; Okamoto, H.; Kimura, M.; Ishida, H. Invariom structure refinement, electrostatic potential and toxicity of 4-O-methylalpinumisoflavone, O,O-dimethylalpinumisoflavone and 5-O-methyl-4-O-(3-methylbut-2-en-1-yl)alpinumisoflavone. Acta Crystallogr. Sect. B Struct. Sci. 2006, 62, 843–849. [Google Scholar] [CrossRef] [PubMed]
- Han, X.H.; Hong, S.S.; Hwang, J.S.; Jeong, S.H.; Hwang, J.H.; Lee, M.H.; Lee, M.K.; Lee, D.; Ro, J.S.; Hwang, B.Y. Monoamine oxidase inhibitory constituents from the fruits of Cudrania tricuspidata. Arch. Pharmacal Res. 2005, 28, 1324. [Google Scholar] [CrossRef]
- Cong, W.; Zhou, C.; Yin, J. Alpinumisoflavone inhibits osteoclast differentiation and exerts anti-osteoporotic effect in ovariectomized mice. Biomed. Pharmacother. 2017, 93, 344–351. [Google Scholar] [CrossRef] [PubMed]
- Chukwujekwu, J.C.; Van Heerden, F.R.; Van Staden, J. Antibacterial activity of flavonoids from the stem bark of Erythrina caffra thunb. Phytother. Res. PTR 2011, 25, 46–48. [Google Scholar] [CrossRef] [PubMed]
- Mvondo, M.A.; Njamen, D.; Tanee Fomum, S.; Wandji, J. Effects of alpinumisoflavone and abyssinone V-4’-methyl ether derived from Erythrina lysistemon (Fabaceae) on the genital tract of ovariectomized female Wistar rat. Phytother. Res. PTR 2012, 26, 1029–1036. [Google Scholar] [CrossRef]
- Wang, T.; Jiang, Y.; Chu, L.; Wu, T.; You, J. Alpinumisoflavone suppresses tumour growth and metastasis of clear-cell renal cell carcinoma. Am. J. Cancer Res. 2017, 7, 999–1015. [Google Scholar]
- Mvondo, M.A.; Njamen, D.; Kretzschmar, G.; Imma Bader, M.; Tanee Fomum, S.; Wandji, J.; Vollmer, G. Alpinumisoflavone and abyssinone V 4’-methylether derived from Erythrina lysistemon (Fabaceae) promote HDL-cholesterol synthesis and prevent cholesterol gallstone formation in ovariectomized rats. J. Pharm. Pharmacol. 2015, 67, 990–996. [Google Scholar] [CrossRef] [PubMed]
- Li, P.Y.; Liang, Y.C.; Sheu, M.J.; Huang, S.S.; Chao, C.Y.; Kuo, Y.H.; Huang, G.J. Alpinumisoflavone attenuates lipopolysaccharide-induced acute lung injury by regulating the effects of anti-oxidation and anti-inflammation both in vitro and in vivo. RSC Adv. 2018, 8, 31515–31528. [Google Scholar] [CrossRef]
- Kuete, V.; Mbaveng, A.T.; Nono, E.C.; Simo, C.C.; Zeino, M.; Nkengfack, A.E.; Efferth, T. Cytotoxicity of seven naturally occurring phenolic compounds towards multi-factorial drug-resistant cancer cells. Phytomedi. Int. J. Phytother. Phytopharm. 2016, 23, 856–863. [Google Scholar] [CrossRef] [PubMed]
- Shin, D.H.; Tam, Y.T.; Kwon, G.S. Polymeric micelle nanocarriers in cancer research. Front. Chem. Sci. Eng. 2016, 10, 348–359. [Google Scholar] [CrossRef]
- Varma, R.K.; Kaushal, R.; Junnarkar, A.Y.; Thomas, G.P.; Naidu, M.U.; Singh, P.P.; Tripathi, R.M.; Shridhar, D.R. Polysorbate 80: A pharmacological study. Arzneim. Forsch. 1985, 35, 804–808. [Google Scholar]
- Tam, Y.T.; Shin, D.H.; Chen, K.E.; Kwon, G.S. Poly(ethylene glycol)-block-poly(d,l-lactic acid) micelles containing oligo(lactic acid)8-paclitaxel prodrug: In Vivo conversion and antitumor efficacy. J. Control. Release Off. J. Control. Release Soc. 2019, 298, 186–193. [Google Scholar] [CrossRef] [PubMed]
- Shin, D.H.; Kwon, G.S. Epothilone B-based 3-in-1 polymeric micelle for anticancer drug therapy. Int. J. Pharm. 2017, 518, 307–311. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Soliman, G.M.; Attia, M.A.; Mohamed, R.A. Poly(ethylene glycol)-block-poly(epsilon-caprolactone) nanomicelles for the solubilization and enhancement of antifungal activity of sertaconazole. Curr. Drug Deliv. 2014, 11, 753–762. [Google Scholar] [CrossRef] [PubMed]
- Vasconcelos, T.; Sarmento, B.; Costa, P. Solid dispersions as strategy to improve oral bioavailability of poor water soluble drugs. Drug Discov. Today 2007, 12, 1068–1075. [Google Scholar] [CrossRef]
- Niwa, T.; Miura, S.; Danjo, K. Design of Dry Nanosuspension with Highly Spontaneous Dispersible Characteristics to Develop Solubilized Formulation for Poorly Water-Soluble Drugs. Pharm. Res. 2011, 28, 2339. [Google Scholar] [CrossRef] [PubMed]
- Kawakami, K.; Yoshikawa, T.; Moroto, Y.; Kanaoka, E.; Takahashi, K.; Nishihara, Y.; Masuda, K. Microemulsion formulation for enhanced absorption of poorly soluble drugs: I. Prescription design. J. Control. Release 2002, 81, 65–74. [Google Scholar] [CrossRef]
- Mohammed, A.R.; Weston, N.; Coombes, A.G.A.; Fitzgerald, M.; Perrie, Y. Liposome formulation of poorly water soluble drugs: Optimisation of drug loading and ESEM analysis of stability. Int. J. Pharm. 2004, 285, 23–34. [Google Scholar] [CrossRef] [PubMed]
- Zhao, J.; Xu, Y.; Wang, C.; Ding, Y.; Chen, M.; Wang, Y.; Peng, J.; Li, L.; Lv, L. Soluplus/TPGS mixed micelles for dioscin delivery in cancer therapy. Drug Dev. Ind. Pharm. 2017, 43, 1197–1204. [Google Scholar] [CrossRef] [PubMed]
- Cho, H.; Lai, T.C.; Tomoda, K.; Kwon, G.S. Polymeric micelles for multi-drug delivery in cancer. AAPS PharmSciTech 2015, 16, 10–20. [Google Scholar] [CrossRef] [PubMed]
- Sezgin, Z.; Yuksel, N.; Baykara, T. Preparation and characterization of polymeric micelles for solubilization of poorly soluble anticancer drugs. Eur. J. Pharm. Biopharm. 2006, 64, 261–268. [Google Scholar] [CrossRef] [PubMed]
- Kwon, G.S.; Okano, T. Polymeric micelles as new drug carriers. Adv. Drug Deliv. Rev. 1996, 21, 107–116. [Google Scholar] [CrossRef]
- Yokoyama, M.; Satoh, A.; Sakurai, Y.; Okano, T.; Matsumura, Y.; Kakizoe, T.; Kataoka, K. Incorporation of water-insoluble anticancer drug into polymeric micelles and control of their particle size. J. Control. Release 1998, 55, 219–229. [Google Scholar] [CrossRef]
- Koenhen, D.M.; Smolders, C.A. The determination of solubility parameters of solvents and polymers by means of correlations with other physical quantities. J. Appl. Polym. Sci. 1975, 19, 1163–1179. [Google Scholar] [CrossRef] [Green Version]
- Zhao, L.; Du, J.; Duan, Y.; Zang, Y.N.; Zhang, H.; Yang, C.; Cao, F.; Zhai, G. Curcumin loaded mixed micelles composed of Pluronic P123 and F68: Preparation, optimization and in vitro characterization. Colloids Surf. B. Biointerfaces 2012, 97, 101–108. [Google Scholar] [CrossRef]
- Kim, H.J.; Shin, D.H.; Lim, E.A.; Kim, J.-S. Sustained-release formulation of sarpogrelate hydrochloride. Arch. Pharm. Res. 2015, 38, 35–41. [Google Scholar] [CrossRef]
- Shin, D.H.; Park, S.H.; Jeong, S.W.; Park, C.W.; Han, K.; Chung, Y.B. Hepatic uptake of epirubicin by isolated rat hepatocytes and its biliary excretion after intravenous infusion in rats. Arch. Pharm. Res. 2014, 37, 1599–1606. [Google Scholar] [CrossRef] [PubMed]
- Toth, L.A. Defining the Moribund Condition as an Experimental Endpoint for Animal Research. ILAR J. 2000, 41, 72–79. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Bookman, M.A.; Kloth, D.D.; Kover, P.E.; Smolinski, S.; Ozols, R.F. Short-course intravenous prophylaxis for paclitaxel-related hypersensitivity reactions. Ann. Oncol. 1997, 8, 611–614. [Google Scholar] [CrossRef] [PubMed]
- Scripture, C.D.; Figg, W.D.; Sparreboom, A. Peripheral neuropathy induced by paclitaxel: Recent insights and future perspectives. Curr. Neuropharmacol. 2006, 4, 165–172. [Google Scholar] [CrossRef] [PubMed]
- Weiss, R.B.; Donehower, R.C.; Wiernik, P.H.; Ohnuma, T.; Gralla, R.J.; Trump, D.L.; Baker, J.R., Jr.; Van Echo, D.A.; Von Hoff, D.D.; Leyland-Jones, B. Hypersensitivity reactions from taxol. J. Clin. Oncol. 1990, 8, 1263–1268. [Google Scholar] [CrossRef]
- Tomoda, K.; Tam, Y.T.; Cho, H.; Buehler, D.; Kozak, K.R.; Kwon, G.S. Triolimus: A Multi-Drug Loaded Polymeric Micelle Containing Paclitaxel, 17-AAG, and Rapamycin as a Novel Radiosensitizer. Macromol. Biosci. 2017, 17. [Google Scholar] [CrossRef]
- Yin, H.; Lee, E.S.; Kim, D.; Lee, K.H.; Oh, K.T.; Bae, Y.H. Physicochemical characteristics of pH-sensitive poly(l-histidine)-b-poly(ethylene glycol)/poly(l-lactide)-b-poly(ethylene glycol) mixed micelles. J. Control. Release 2008, 126, 130–138. [Google Scholar] [CrossRef]
- Wei, Z.; Hao, J.; Yuan, S.; Li, Y.; Juan, W.; Sha, X.; Fang, X. Paclitaxel-loaded Pluronic P123/F127 mixed polymeric micelles: Formulation, optimization and in vitro characterization. Int. J. Pharm. 2009, 376, 176–185. [Google Scholar] [CrossRef]
- Zhang, C.; Qu, G.; Sun, Y.; Wu, X.; Yao, Z.; Guo, Q.; Ding, Q.; Yuan, S.; Shen, Z.; Ping, Q.; et al. Pharmacokinetics, biodistribution, efficacy and safety of N-octyl-O-sulfate chitosan micelles loaded with paclitaxel. Biomaterials 2008, 29, 1233–1241. [Google Scholar] [CrossRef]
- Yeh, T.K.; Lu, Z.; Wientjes, M.G.; Au, J.L.S. Formulating Paclitaxel in Nanoparticles Alters Its Disposition. Pharm. Res. 2005, 22, 867–874. [Google Scholar] [CrossRef]
- Gao, H.; Xiong, J.; Cheng, T.; Liu, J.; Chu, L.; Liu, J.; Ma, R.; Shi, L. In Vivo Biodistribution of Mixed Shell Micelles with Tunable Hydrophilic/Hydrophobic Surface. Biomacromolecules 2013, 14, 460–467. [Google Scholar] [CrossRef] [PubMed]
- Efron, B. Logistic Regression, Survival Analysis, and the Kaplan–Meier Curve. J. Am. Stat. Assoc. 1988, 83, 414–425. [Google Scholar] [CrossRef]



| Solvent | AIF Solubility (μg/mL) |
|---|---|
| DW | 0.178 ± 0.121 |
| Cremophor EL®/EtOH (5:5, v/v) | 82,143 ± 9989 |
| Cremophor EL®/EtOH (0:10, v/v) | 32,500 ± 6802 |
| Formulation | Polymer Amount Used (mg) | AIF Amount Used (mg) | AIF Final Concentration (mg/mL) | Encapsulation Efficiency (EE %) | Drug Loading (DL %) | Particle Size (nm) | Polydispersity Index (PDI) |
|---|---|---|---|---|---|---|---|
| AIF-loaded Pluronics® F127 micelle | 100 | 6 | 4.63 ± 0.08 | 77.2 ± 1.4 | 4.37 ± 0.08 | 1385 ± 430 | 0.45 ± 0.21 |
| 135 | 6 | 4.86 ± 0.50 | 81.0 ± 8.4 | 4.59 ± 0.47 | 9993 ± 8616 | 0.60 ± 0.36 | |
| 150 | 6 | 4.52 ± 0.02 | 75.4 ± 0.3 | 4.27 ± 0.02 | 1102 ± 1170 | 0.59 ± 0.45 | |
| AIF-loaded Soluplus® micelle | 100 | 6 | 0.01 ± 0.01 | 0.24 ± 0.23 | 0.01 ± 0.01 | 138 ± 143 | 0.39 ± 0.18 |
| 135 | 6 | 0.01 ± 0.00 | 0.09 ± 0.05 | 0.01 ± 0.00 | N.D. a | N.D. a | |
| 150 | 6 | 0.06 ± 0.09 | 0.94 ± 1.45 | 0.05 ± 0.08 | 78.7 ± 6.0 | 0.02 ± 026 | |
| AIF-loaded mPEG-b-PLA micelle | 100 | 6 | 2.37 ± 2.16 | 39.5 ± 36.0 | 2.24 ± 2.04 | 28.0 ± 1.8 | 0.15 ± 0.05 |
| 135 | 6 | 4.39 ± 0.09 | 73.1 ± 1.4 | 4.14 ± 0.08 | 34.1 ± 1.8 | 0.21 ± 0.02 | |
| 150 | 6 | 4.50 ± 0.15 | 74.9 ± 2.5 | 4.24 ± 0.14 | 31.2 ± 5.5 | 0.21 ± 0.01 |
| Parameters | AIF in 25% Cremophor EL®/EtOH Solution | AIF-Loaded mPEG-b-PLA Micelle |
|---|---|---|
| AUC a (min·μg·mL−1) | 326 ± 168 | 876 ± 103 * |
| C0 b (μg·mL−1) | 1.89 ± 0.63 | 7.86 ± 1.79 |
| CLt c (mL·kg−1·min) | 94.6 ± 56.1 | 23.1 ± 2.7 |
| Vd d (mL·kg−1) | 13903 ± 5274 | 2940 ± 867 |
| BA e (%) | 100 ± 51 | 269 ± 18 * |
© 2019 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Jo, M.J.; Jo, Y.H.; Lee, Y.J.; Park, C.-W.; Kim, J.-S.; Hong, J.T.; Chung, Y.B.; Lee, M.K.; Shin, D.H. Physicochemical, Pharmacokinetic, and Toxicity Evaluation of Methoxy Poly(ethylene glycol)-b-Poly(d,l-Lactide) Polymeric Micelles Encapsulating Alpinumisoflavone Extracted from Unripe Cudrania tricuspidata Fruit. Pharmaceutics 2019, 11, 366. https://doi.org/10.3390/pharmaceutics11080366
Jo MJ, Jo YH, Lee YJ, Park C-W, Kim J-S, Hong JT, Chung YB, Lee MK, Shin DH. Physicochemical, Pharmacokinetic, and Toxicity Evaluation of Methoxy Poly(ethylene glycol)-b-Poly(d,l-Lactide) Polymeric Micelles Encapsulating Alpinumisoflavone Extracted from Unripe Cudrania tricuspidata Fruit. Pharmaceutics. 2019; 11(8):366. https://doi.org/10.3390/pharmaceutics11080366
Chicago/Turabian StyleJo, Min Jeong, Yang Hee Jo, Yu Jin Lee, Chun-Woong Park, Jin-Seok Kim, Jin Tae Hong, Youn Bok Chung, Mi Kyeong Lee, and Dae Hwan Shin. 2019. "Physicochemical, Pharmacokinetic, and Toxicity Evaluation of Methoxy Poly(ethylene glycol)-b-Poly(d,l-Lactide) Polymeric Micelles Encapsulating Alpinumisoflavone Extracted from Unripe Cudrania tricuspidata Fruit" Pharmaceutics 11, no. 8: 366. https://doi.org/10.3390/pharmaceutics11080366
APA StyleJo, M. J., Jo, Y. H., Lee, Y. J., Park, C.-W., Kim, J.-S., Hong, J. T., Chung, Y. B., Lee, M. K., & Shin, D. H. (2019). Physicochemical, Pharmacokinetic, and Toxicity Evaluation of Methoxy Poly(ethylene glycol)-b-Poly(d,l-Lactide) Polymeric Micelles Encapsulating Alpinumisoflavone Extracted from Unripe Cudrania tricuspidata Fruit. Pharmaceutics, 11(8), 366. https://doi.org/10.3390/pharmaceutics11080366








