Ferritin and Encapsulin Nanoparticles as Effective Vaccine Delivery Systems: Boosting the Immunogenicity of the African Swine Fever Virus C129R Protein
Abstract
1. Introduction
2. Materials and Methods
2.1. Vector Design and Gene Synthesis
2.2. Preparation of Nanoparticle Proteins and Conjugated Antigens
2.3. Nanoparticle Structure Characterization
2.4. Nanoparticle Stability Studies
2.5. In Vivo Distribution of Nanoparticle Proteins
2.6. Evaluation of Antigen Uptake In Vitro
2.7. Animal Vaccination
2.8. Antibody and Antibody Isotype Assay
2.9. Flow Cytometry (FACS) and Analysis of Immune Cell Populations
2.10. Cytokine Assay
2.11. Safety Assessment
2.12. Statistical Analysis
3. Results
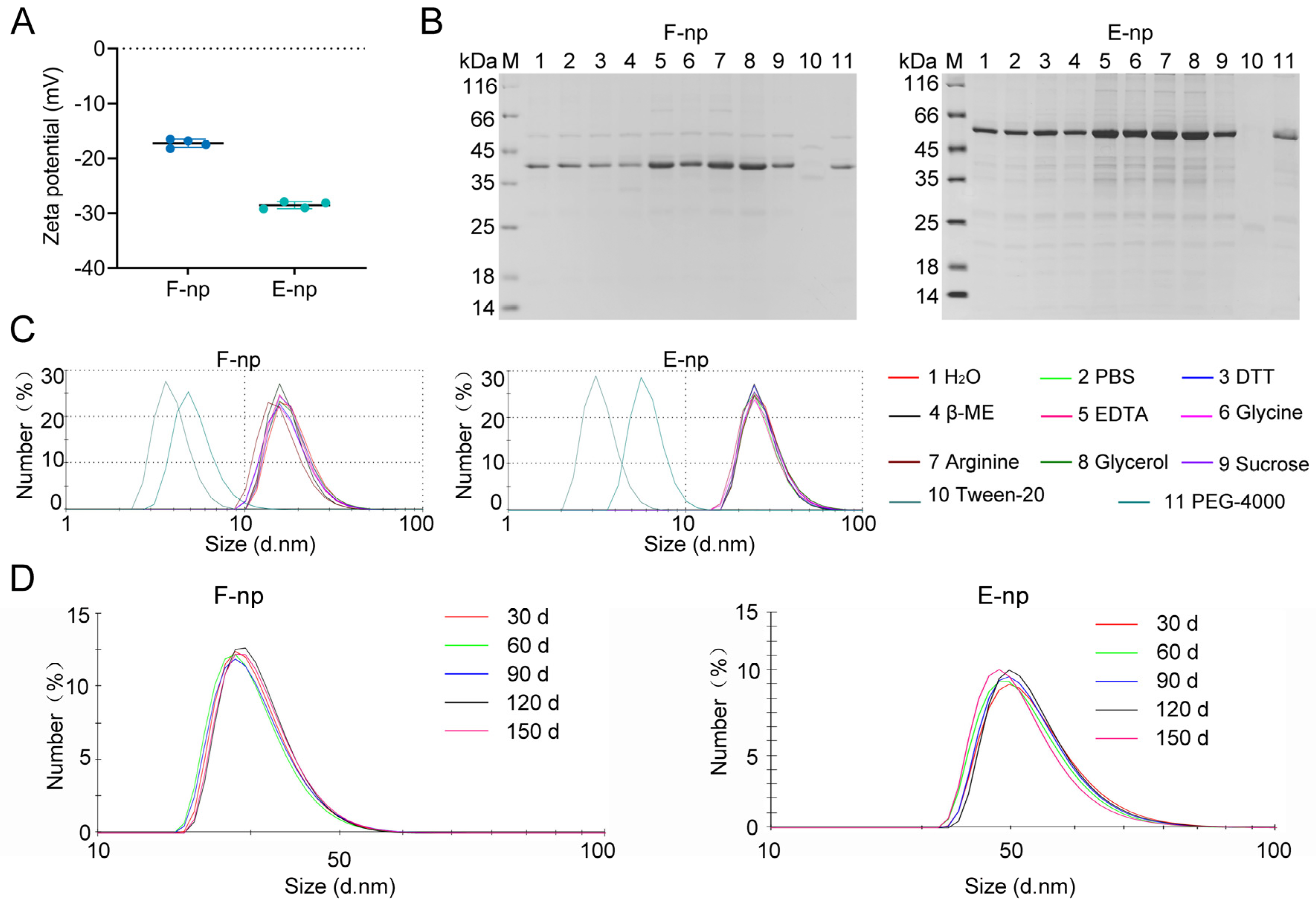
3.1. Design, Production, and Characterization of Protein Nanoparticles
3.2. Evaluation of Nanoparticle Stability
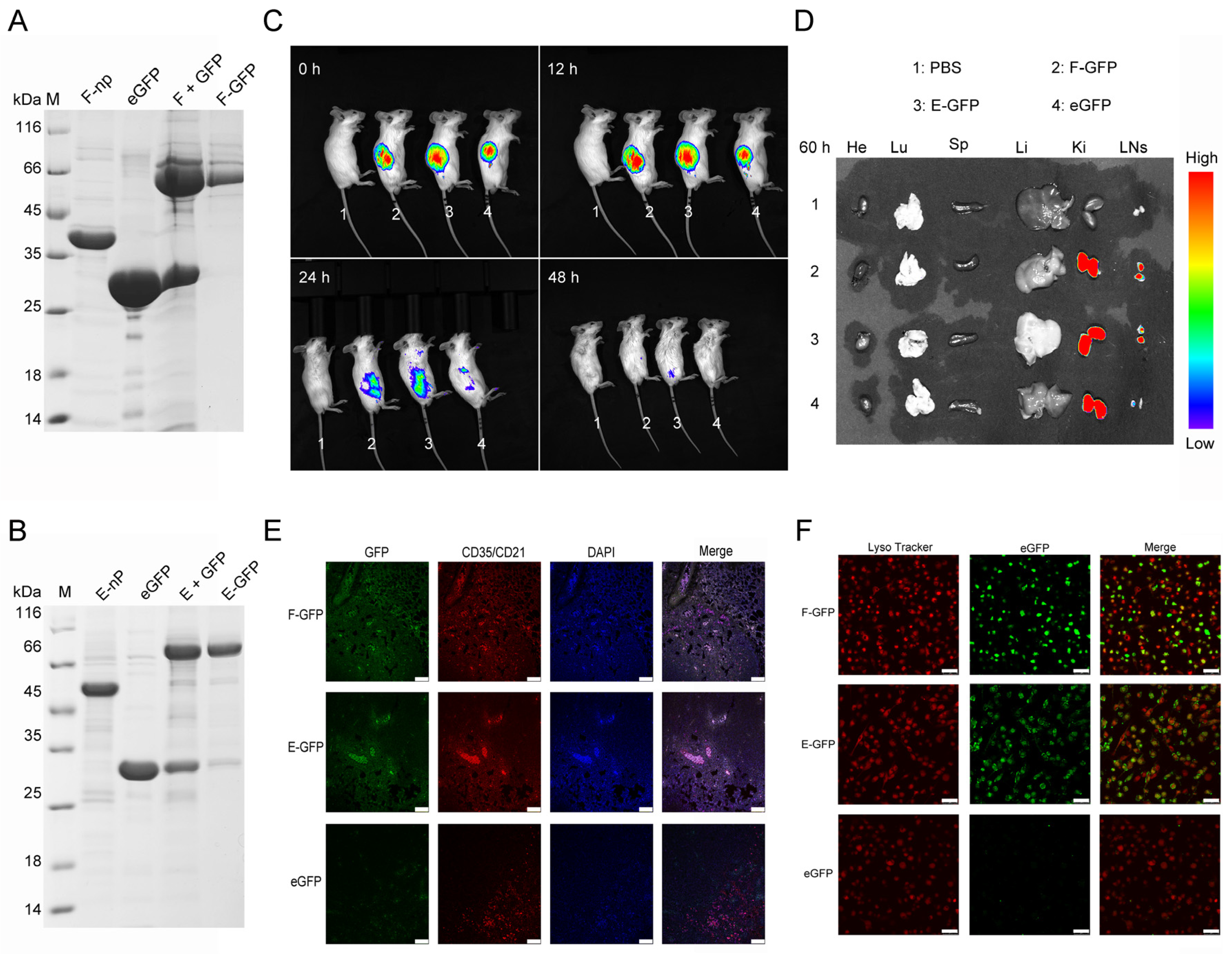
3.3. In Vivo and In Vivo Distribution of the Nanoparticles
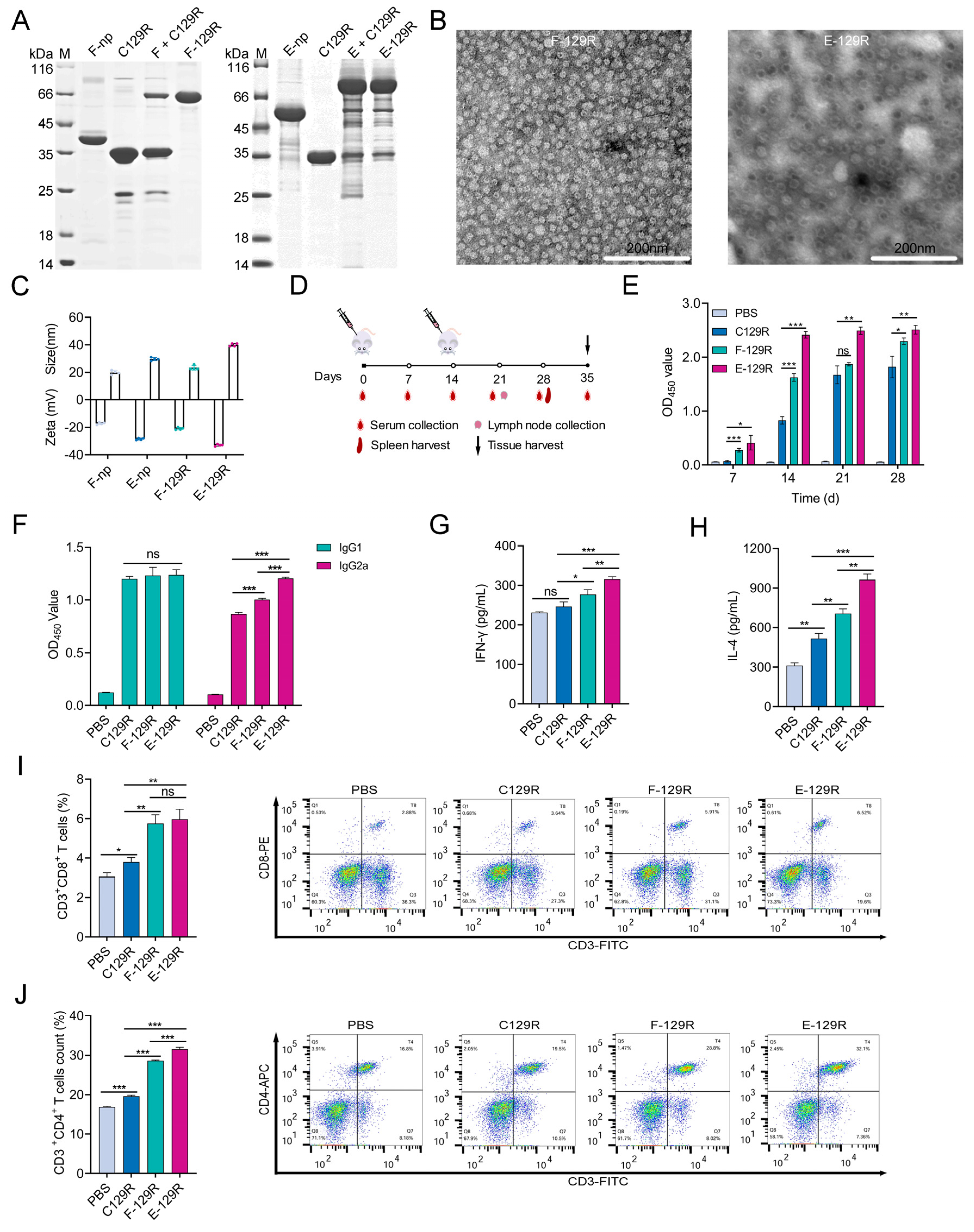
3.4. F/E-129R Nanoparticles Induce Strong Humoral and Cellular Immune Responses
3.5. F/E-C129 Nanoparticles Promote Immune Activation in Lymph Nodes
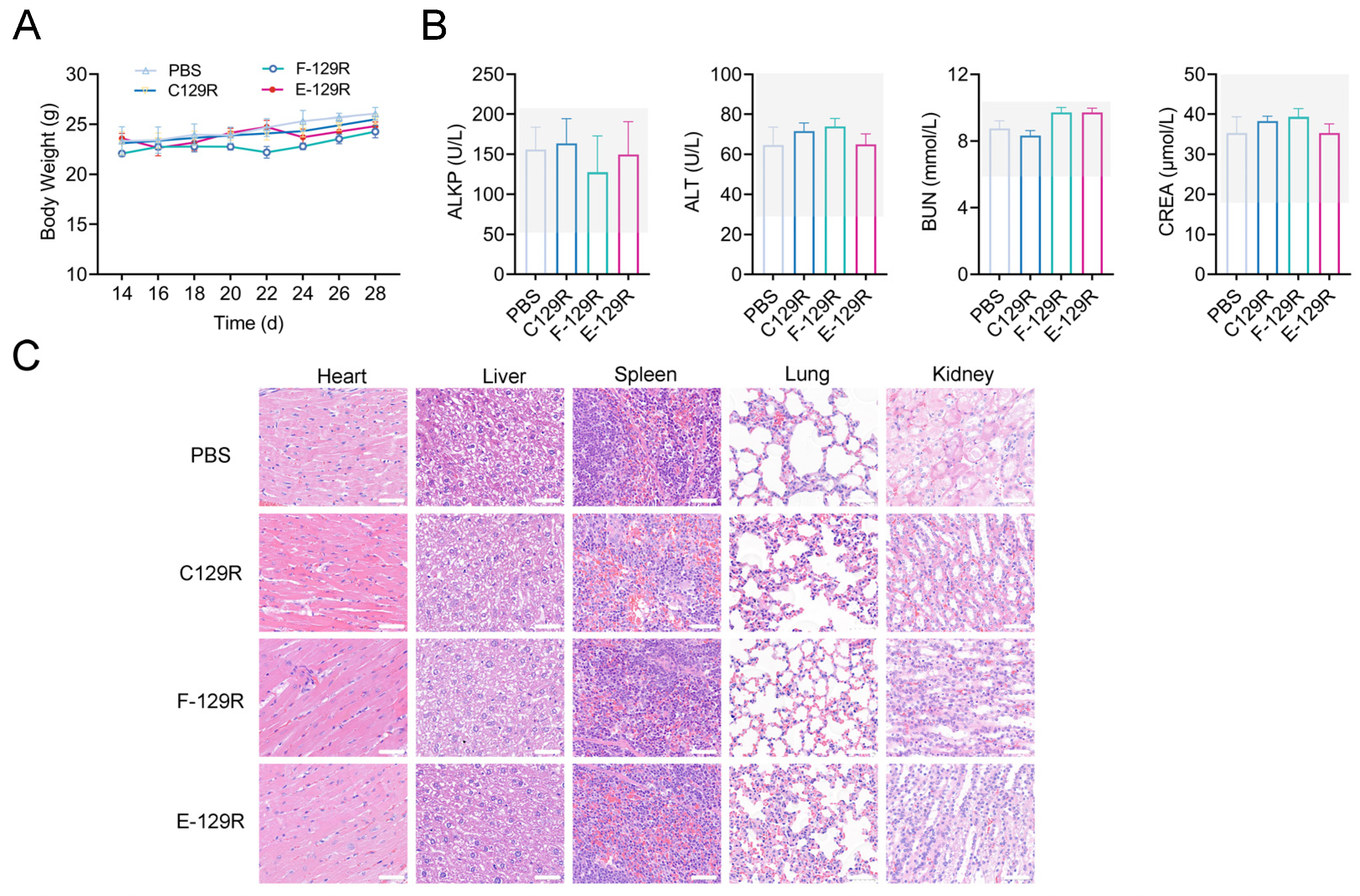
3.6. Safety Evaluation of F/E-129R Vaccines
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Yue, J.; Liu, Y.; Zhao, M.; Bi, X.; Li, G.; Liang, W. The R&D landscape for infectious disease vaccines. Nat. Rev. Drug Discov. 2023, 22, 867–868. [Google Scholar] [PubMed]
- Sun, S.; Cai, Y.; Song, T.-Z.; Pu, Y.; Cheng, L.; Xu, H.; Sun, J.; Meng, C.; Lin, Y.; Huang, H.; et al. Interferon-armed RBD dimer enhances the immunogenicity of RBD for sterilizing immunity against SARS-CoV-2. Cell Res. 2021, 31, 1011–1023. [Google Scholar] [CrossRef]
- Rodrigues, M.Q.; Alves, P.M.; Roldão, A. Functionalizing Ferritin Nanoparticles for Vaccine Development. Pharmaceutics. 2021, 13, 1621. [Google Scholar] [CrossRef]
- Yassine, H.M.; Boyington, J.C.; McTamney, P.M.; Wei, C.-J.; Kanekiyo, M.; Kong, W.-P.; Gallagher, J.R.; Wang, L.; Zhang, Y.; Joyce, M.G.; et al. Hemagglutinin-stem nanoparticles generate heterosubtypic influenza protection. Nat. Med. 2015, 21, 1065–1070. [Google Scholar] [CrossRef] [PubMed]
- Kanekiyo, M.; Joyce, M.G.; Gillespie, R.A.; Gallagher, J.R.; Andrews, S.F.; Yassine, H.M.; Wheatley, A.K.; Fisher, B.E.; Ambrozak, D.R.; Creanga, A.; et al. Mosaic nanoparticle display of diverse influenza virus hemagglutinins elicits broad B cell responses. Nat. Immunol. 2019, 20, 362–372. [Google Scholar] [CrossRef] [PubMed]
- Tan, T.K.; Rijal, P.; Rahikainen, R.; Keeble, A.H.; Schimanski, L.; Hussain, S.; Harvey, R.; Hayes, J.W.P.; Edwards, J.C.; McLean, R.K.; et al. A COVID-19 vaccine candidate using SpyCatcher multimerization of the SARS-CoV-2 spike protein receptor-binding domain induces potent neutralising antibody responses. Nat. Commun. 2021, 12, 542. [Google Scholar] [CrossRef]
- Chen, R.; Zhang, X.; Yuan, Y.; Deng, X.; Wu, B.; Xi, Z.; Wang, G.; Lin, Y.; Li, R.; Wang, X.; et al. Development of Receptor Binding Domain (RBD)-Conjugated Nanoparticle Vaccines with Broad Neutralization against SARS-CoV-2 Delta and Other Variants. Adv. Sci. 2022, 9, e2105378. [Google Scholar] [CrossRef]
- Li, Y.; Zhang, Y.; Zhou, Y.; Li, Y.; Xu, J.; Ai, Y.; Xu, L.; Xiao, X.; Zhang, B.; Jin, J. An RBD virus-like particle vaccine for SARS-CoV-2 induces cross-variant antibody responses in mice and macaques. Signal Transduct. Target. Ther. 2023, 8, 173. [Google Scholar] [CrossRef]
- Liu, T.; Li, M.; Tian, Y.; Dong, Y.; Liu, N.; Wang, Z.; Zhang, H.; Zheng, A.; Cui, C. Immunogenicity and safety of a self-assembling ZIKV nanoparticle vaccine in mice. Int. J. Pharm. 2024, 660, 124320. [Google Scholar] [CrossRef]
- Tokatlian, T.; Read, B.J.; Jones, C.A.; Kulp, D.W.; Menis, S.; Chang, J.Y.H.; Steichen, J.M.; Kumari, S.; Allen, J.D.; Dane, E.L.; et al. Innate immune recognition of glycans targets HIV nanoparticle immunogens to germinal centers. Science 2019, 363, 649–654. [Google Scholar] [CrossRef]
- Leggat, D.J.; Cohen, K.W.; Willis, J.R.; Fulp, W.J.; deCamp, A.C.; Kalyuzhniy, O.; Cottrell, C.A.; Menis, S.; Finak, G.; Ballweber-Fleming, L.; et al. Vaccination induces HIV broadly neutralizing antibody precursors in humans. Science 2022, 378, eadd6502. [Google Scholar] [CrossRef]
- Murji, A.A.; Qin, J.S.; Hermanus, T.; Morris, L.; Georgiev, I.S. Elicitation of Neutralizing Antibody Responses to HIV-1 Immunization with Nanoparticle Vaccine Platforms. Viruses 2021, 13, 1296. [Google Scholar] [CrossRef]
- Liao, Z.; Tu, L.; Li, X.; Liang, X.-J.; Huo, S. Virus-inspired nanosystems for drug delivery. Nanoscale 2021, 13, 18912–18924. [Google Scholar] [CrossRef] [PubMed]
- Huang, Z.; Zhu, Z.; Liu, L.; Song, W.; Chen, X. Preparation of viromimetic rod-like nanoparticle vaccines (RLNVax) and study of their humoral immune activation efficacy. Biomater. Sci. 2024, 12, 5115–5122. [Google Scholar] [CrossRef]
- Pan, C.; Wu, J.; Qing, S.; Zhang, X.; Zhang, L.; Yue, H.; Zeng, M.; Wang, B.; Yuan, Z.; Qiu, Y.; et al. Biosynthesis of Self-Assembled Proteinaceous Nanoparticles for Vaccination. Adv. Mater. 2020, 32, e2002940. [Google Scholar] [CrossRef] [PubMed]
- Li, M.; Yao, H.; Yi, K.; Lao, Y.-H.; Shao, D.; Tao, Y. Emerging nanoparticle platforms for CpG oligonucleotide delivery. Biomater. Sci. 2024, 12, 2203–2228. [Google Scholar] [CrossRef]
- Zakeri, B.; Fierer, J.O.; Celik, E.; Chittock, E.C.; Schwarz-Linek, U.; Moy, V.T.; Howarth, M. Peptide tag forming a rapid covalent bond to a protein, through engineering a bacterial adhesin. Proc. Natl. Acad. Sci. USA 2012, 109, E690–E697. [Google Scholar] [CrossRef] [PubMed]
- Vester, S.K.; Rahikainen, R.; Khairil Anuar, I.N.A.; Hills, R.A.; Tan, T.K.; Howarth, M. SpySwitch enables pH- or heat-responsive capture and release for plug-and-display nanoassembly. Nat. Commun. 2022, 13, 3714. [Google Scholar] [CrossRef]
- Lampinen, V.; Gröhn, S.; Soppela, S.; Blazevic, V.; Hytönen, V.P.; Hankaniemi, M.M. SpyTag/SpyCatcher display of influenza M2e peptide on norovirus-like particle provides stronger immunization than direct genetic fusion. Front. Cell Infect. Microbiol. 2023, 13, 1216364. [Google Scholar] [CrossRef]
- Rahikainen, R.; Rijal, P.; Tan, T.K.; Wu, H.J.; Andersson, A.M.C.; Barrett, J.R.; Bowden, T.A.; Draper, S.J.; Townsend, A.R.; Howarth, M. Overcoming Symmetry Mismatch in Vaccine Nanoassembly through Spontaneous Amidation. Angew. Chem. 2020, 133, 325–334. [Google Scholar] [CrossRef]
- Brune, K.D.; Howarth, M. New Routes and Opportunities for Modular Construction of Particulate Vaccines: Stick, Click, and Glue. Front. Immunol. 2018, 9, 1432. [Google Scholar] [CrossRef]
- Escolano, A.; Gristick, H.B.; Abernathy, M.E.; Merkenschlager, J.; Gautam, R.; Oliveira, T.Y.; Pai, J.; West, A.P.; Barnes, C.O.; Cohen, A.A.; et al. Immunization expands B cells specific to HIV-1 V3 glycan in mice and macaques. Nature 2019, 570, 468–473. [Google Scholar] [CrossRef] [PubMed]
- Kang, Y.-F.; Sun, C.; Zhuang, Z.; Yuan, R.-Y.; Zheng, Q.; Li, J.-P.; Zhou, P.-P.; Chen, X.-C.; Liu, Z.; Zhang, X.; et al. Rapid Development of SARS-CoV-2 Spike Protein Receptor-Binding Domain Self-Assembled Nanoparticle Vaccine Candidates. ACS Nano 2021, 15, 2738–2752. [Google Scholar] [CrossRef]
- Wang, W.J.; Zhou, X.X.; Bian, Y.J.; Wang, S.; Chai, Q.; Guo, Z.Q.; Wang, Z.N.; Zhu, P.; Peng, H.; Yan, X.Y.; et al. Dual-targeting nanoparticle vaccine elicits a therapeutic antibody response against chronic hepatitis B. Nat. Nanotechnol. 2020, 15, 406–416. [Google Scholar] [CrossRef] [PubMed]
- Chen, S.; Zhang, X.; Yao, Y.; Wang, S.; Li, K.; Zhang, B.; Ye, T.; Chen, L.; Wu, Y.; Li, E.; et al. Ferritin nanoparticle-based Nipah virus glycoprotein vaccines elicit potent protective immune responses in mice and hamsters. Virol. Sin. 2024, 39, 909–916. [Google Scholar] [CrossRef] [PubMed]
- Tennakoon, M.S.B.W.T.M.N.S.; Lee, K.-H.; Lee, H.-M.; Park, J.-Y.; Shin, H.-J. Optimization of Conditions for Expression of Dengue Serotype 2 EDIII Protein in Escherichia coli and Immune Responses of Adjuvant-Free EDIII Ferritin Nanoparticles Against Dengue Virus in BALB/c Mice. Viruses 2025, 17, 129. [Google Scholar] [CrossRef]
- Chang, X.; Ma, J.; Zhou, Y.; Xiao, S.; Xiao, X.; Fang, L. Development of a Ferritin Protein Nanoparticle Vaccine with PRRSV GP5 Protein. Viruses 2024, 16, 991. [Google Scholar] [CrossRef]
- Jones, J.A.; Andreas, M.P.; Giessen, T.W. Structural basis for peroxidase encapsulation inside the encapsulin from the Gram-negative pathogen Klebsiella pneumoniae. Nat. Commun. 2024, 15, 2558. [Google Scholar] [CrossRef]
- Jenkins, M.C.; Lutz, S. Encapsulin Nanocontainers as Versatile Scaffolds for the Development of Artificial Metabolons. ACS Synth. Biol. 2021, 10, 857–869. [Google Scholar] [CrossRef]
- Choi, H.; Eom, S.; Kim, H.-u.; Bae, Y.; Jung, H.S.; Kang, S. Load and Display: Engineering Encapsulin as a Modular Nanoplatform for Protein-Cargo Encapsulation and Protein-Ligand Decoration Using Split Intein and SpyTag/SpyCatcher. Biomacromolecules 2021, 22, 3028–3039. [Google Scholar] [CrossRef]
- Zhai, W.Z.; Huang, Y.; He, Y.H.; Chu, Y.Y.; Tao, C.H.; Pang, Z.B.; Wang, Z.; Zhu, H.F.; Jia, H. Immunogenicity Analysis and Identification of Potential T-Cell Epitopes in C129R Protein of African Swine Fever Virus. Microorganisms 2024, 12, 1056. [Google Scholar] [CrossRef] [PubMed]
- Dodantenna, N.; Ranathunga, L.; Chathuranga, W.A.G.; Weerawardhana, A.; Cha, J.W.; Subasinghe, A.; Gamage, N.; Haluwana, D.K.; Kim, Y.; Jheong, W.; et al. African Swine Fever Virus EP364R and C129R Target Cyclic GMP-AMP To Inhibit the cGAS-STING Signaling Pathway. J. Virol. 2022, 96, e0102222. [Google Scholar] [CrossRef] [PubMed]
- Kanekiyo, M.; Bu, W.; Joyce, M.G.; Meng, G.; Whittle, J.R.R.; Baxa, U.; Yamamoto, T.; Narpala, S.; Todd, J.-P.; Rao, S.S.; et al. Rational Design of an Epstein-Barr Virus Vaccine Targeting the Receptor-Binding Site. Cell 2015, 162, 1090–1100. [Google Scholar] [CrossRef] [PubMed]
- Keeble, A.H.; Turkki, P.; Stokes, S.; Khairil Anuar, I.N.A.; Rahikainen, R.; Hytönen, V.P.; Howarth, M. Approaching infinite affinity through engineering of peptide–protein interaction. Proc. Natl. Acad. Sci. USA 2019, 116, 26523–26533. [Google Scholar] [CrossRef]
- Bachmann, M.F.; Jennings, G.T. Vaccine delivery: A matter of size, geometry, kinetics and molecular patterns. Nat. Rev. Immunol. 2010, 10, 787–796. [Google Scholar] [CrossRef]
- Wang, S.; Li, F.; Ye, T.; Wang, J.; Lyu, C.; Qing, S.; Ding, Z.; Gao, X.; Jia, R.; Yu, D.; et al. Macrophage-tumor chimeric exosomes accumulate in lymph node and tumor to activate the immune response and the tumor microenvironment. Sci. Transl. Med. 2021, 13, eabb6981. [Google Scholar] [CrossRef]
- Qin, H.; Zhao, R.; Qin, Y.; Zhu, J.; Chen, L.; Di, C.; Han, X.; Cheng, K.; Zhang, Y.; Zhao, Y.; et al. Development of a Cancer Vaccine Using In Vivo Click-Chemistry-Mediated Active Lymph Node Accumulation for Improved Immunotherapy. Adv. Mater. 2021, 33, e2006007. [Google Scholar] [CrossRef]
- Liu, M.; Feng, Y.; Lu, Y.; Huang, R.; Zhang, Y.; Zhao, Y.; Mo, R. Lymph-targeted high-density lipoprotein-mimetic nanovaccine for multi-antigenic personalized cancer immunotherapy. Sci. Adv. 2024, 10, eadk2444. [Google Scholar] [CrossRef]
- Najibi, A.J.; Lane, R.S.; Sobral, M.C.; Bovone, G.; Kang, S.; Freedman, B.R.; Gutierrez Estupinan, J.; Elosegui-Artola, A.; Tringides, C.M.; Dellacherie, M.O.; et al. Durable lymph-node expansion is associated with the efficacy of therapeutic vaccination. Nat. Biomed. Eng. 2024, 8, 1226–1242. [Google Scholar] [CrossRef]
- Liu, H.P.; Moynihan, K.D.; Zheng, Y.R.; Szeto, G.L.; Li, A.V.; Huang, B.; Van Egeren, D.S.; Park, C.; Irvine, D.J. Structure-based programming of lymph-node targeting in molecular vaccines. Nature 2014, 507, 519–522. [Google Scholar] [CrossRef]
- Liang, J.; Yao, L.; Liu, Z.; Chen, Y.; Lin, Y.; Tian, T. Nanoparticles in Subunit Vaccines: Immunological Foundations, Categories, and Applications. Small 2024, 21, e2407649. [Google Scholar] [CrossRef] [PubMed]
- Nguyen, B.; Tolia, N.H. Protein-based antigen presentation platforms for nanoparticle vaccines. npj Vaccines 2021, 6, 70. [Google Scholar] [CrossRef] [PubMed]
- Öztürk, K.; Kaplan, M.; Çalış, S. Effects of nanoparticle size, shape, and zeta potential on drug delivery. Int. J. Pharm. 2024, 666, 124799. [Google Scholar] [CrossRef] [PubMed]
- Pan, J.D.; Wang, Q.H.; Qi, M.; Chen, J.J.; Wu, X.F.; Zhang, X.W.; Li, W.; Zhang, X.E.; Cui, Z.Q. An Intranasal Multivalent Epitope-Based Nanoparticle Vaccine Confers Broad Protection against Divergent Influenza Viruses. ACS Nano. 2023, 17, 13474–13487. [Google Scholar] [CrossRef]


Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Zhang, Y.; Ru, Y.; Zhao, L.; Hao, R.; Yang, Y.; Li, Y.; Zhang, R.; Jiang, C.; Zheng, H. Ferritin and Encapsulin Nanoparticles as Effective Vaccine Delivery Systems: Boosting the Immunogenicity of the African Swine Fever Virus C129R Protein. Viruses 2025, 17, 556. https://doi.org/10.3390/v17040556
Zhang Y, Ru Y, Zhao L, Hao R, Yang Y, Li Y, Zhang R, Jiang C, Zheng H. Ferritin and Encapsulin Nanoparticles as Effective Vaccine Delivery Systems: Boosting the Immunogenicity of the African Swine Fever Virus C129R Protein. Viruses. 2025; 17(4):556. https://doi.org/10.3390/v17040556
Chicago/Turabian StyleZhang, Yue, Yi Ru, Longhe Zhao, Rongzeng Hao, Yang Yang, Yajun Li, Rong Zhang, Chenghui Jiang, and Haixue Zheng. 2025. "Ferritin and Encapsulin Nanoparticles as Effective Vaccine Delivery Systems: Boosting the Immunogenicity of the African Swine Fever Virus C129R Protein" Viruses 17, no. 4: 556. https://doi.org/10.3390/v17040556
APA StyleZhang, Y., Ru, Y., Zhao, L., Hao, R., Yang, Y., Li, Y., Zhang, R., Jiang, C., & Zheng, H. (2025). Ferritin and Encapsulin Nanoparticles as Effective Vaccine Delivery Systems: Boosting the Immunogenicity of the African Swine Fever Virus C129R Protein. Viruses, 17(4), 556. https://doi.org/10.3390/v17040556





