Construction and Immune Strategy Optimization of a Vaccine Strain for Influenza A (H5N8) Subtype
Abstract
1. Introduction
2. Materials and Methods
2.1. Construction of Candidate Vaccine Strain
2.2. Receptor-Binding Preference Assay
2.3. Virulence Evaluation of rH5N8/PR8
2.3.1. Intravenous Pathogenicity Test (IVPI)
2.3.2. Virulence of the rH5N8/PR8 in Mice
2.4. Immunization of Mice and Optimization of Vaccination Protocols
2.5. Testing of Immunoglobulin and Cytokines in Sera
2.6. Protective Efficacy Evaluation of H5N8 Vaccine in BALB/c Mice
2.7. Biosafety and Animal Ethics
3. Results
3.1. Construction of H5N8 CVV
3.2. Receptor-Binding Preference Analysis
3.3. Pathogenicity Assessment
3.4. Immunogenicity and Optimization of Immunization Protocols for rH5N8/PR8 Candidate Vaccine
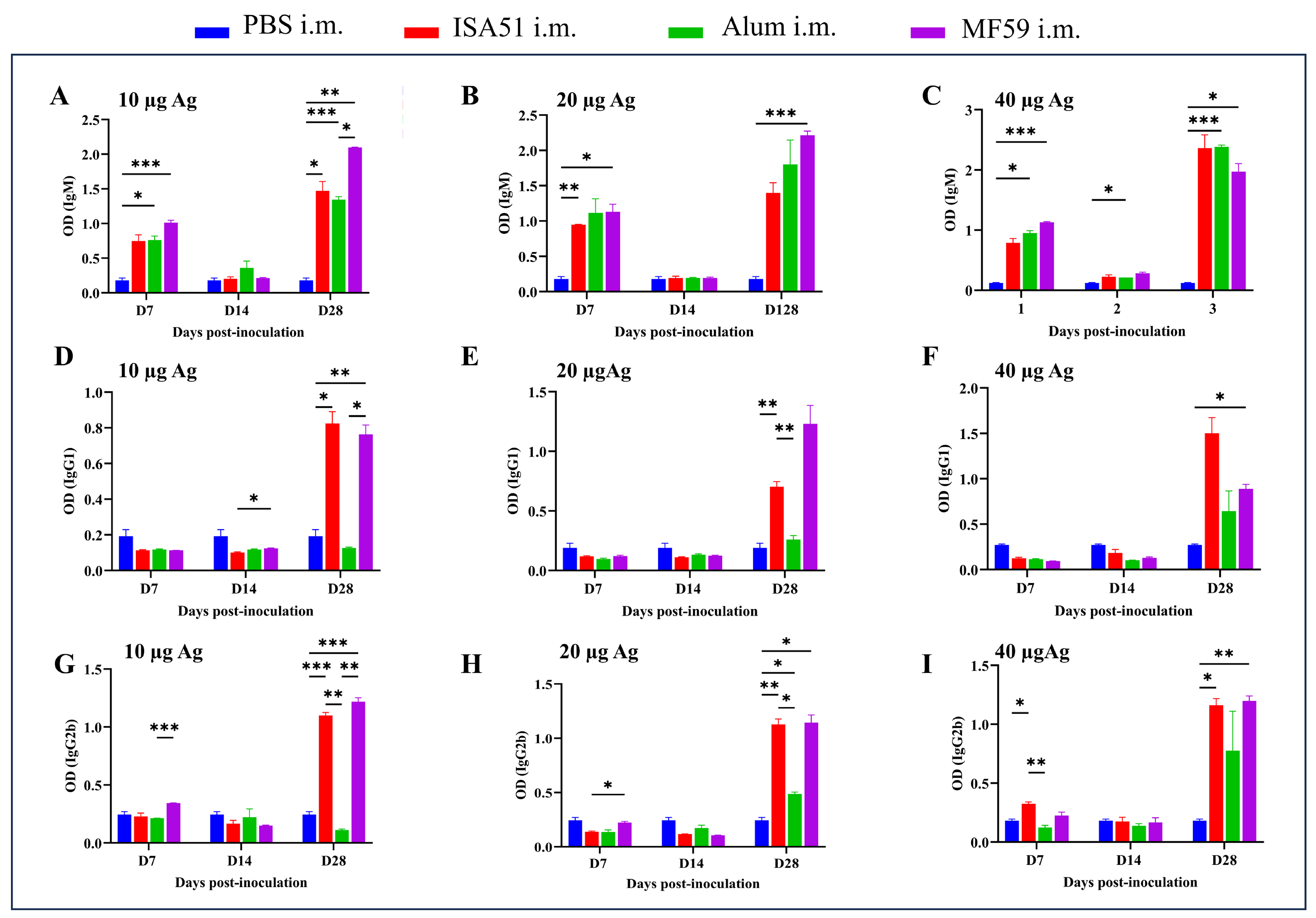
3.4.1. Immunogenicity Effect of Different Adjuvants and Dosage
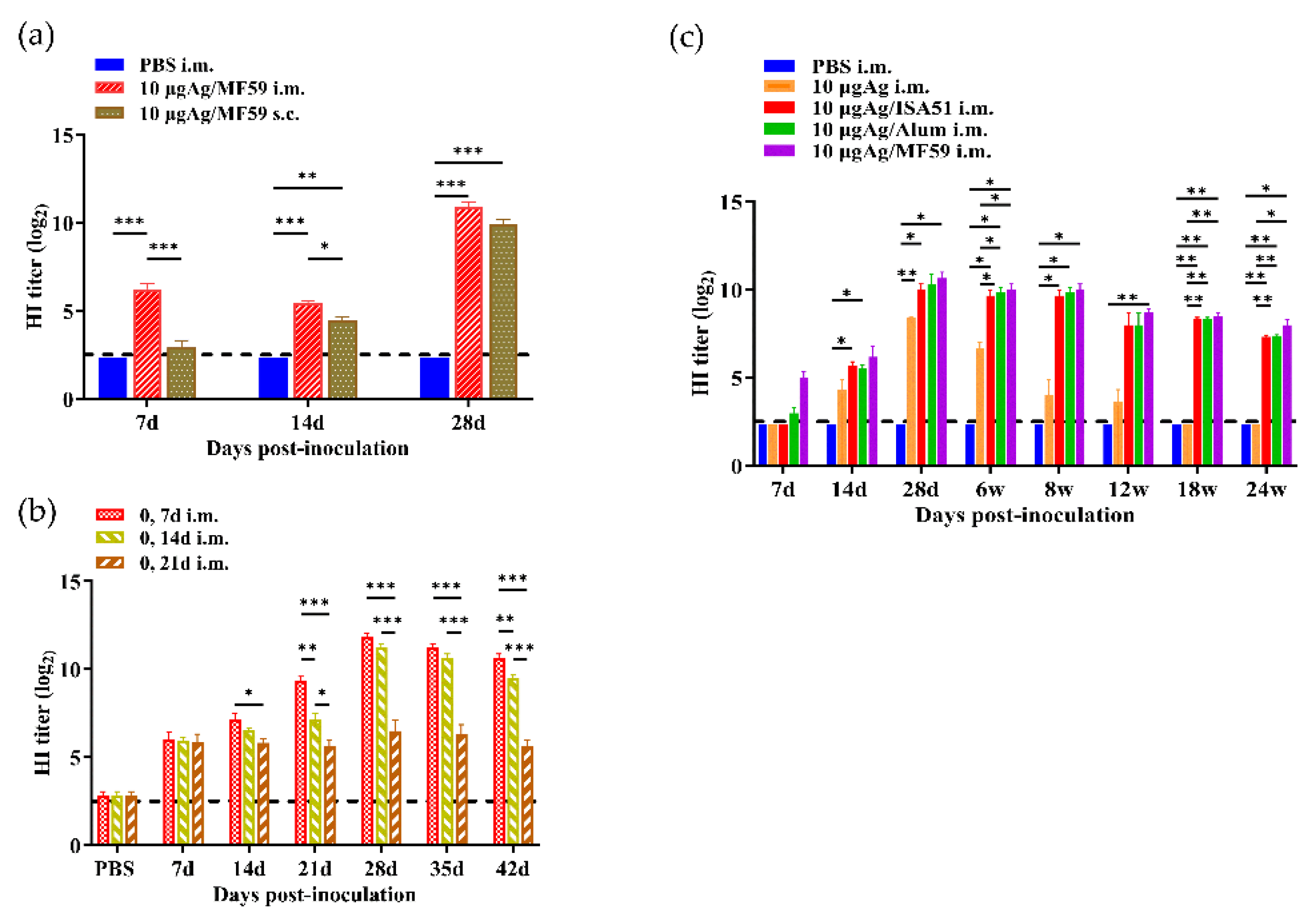
3.4.2. Immunogenicity Difference Between Intramuscular and Subcutaneous Administration
3.4.3. Comparison of Immunogenicity at Different Booster Intervals
3.4.4. Long-Term Immune Response Monitoring
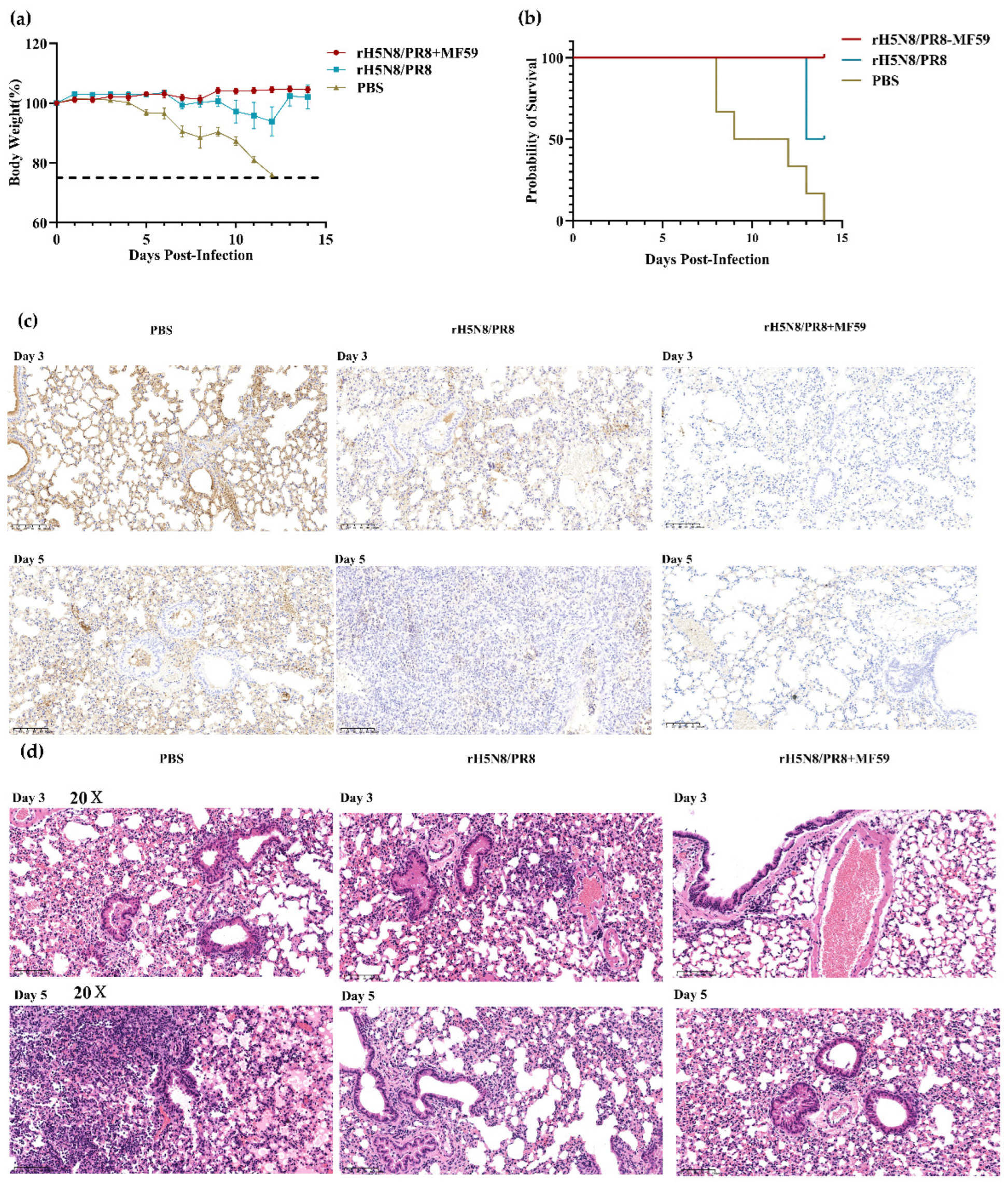
3.5. Evaluation of Protective Efficacy for MF59-Adjuvanted Inactivated rH5N8/PR8
4. Discussion
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Smith, G.J.; Donis, R.O.; World Health Organization/World Organisation for Animal Health/Food and Agriculture Organization (WHO/OIE/FAO) H5 Evolution Working Group. Nomenclature updates resulting from the evolution of avian influenza A(H5) virus clades 2.1.3.2a, 2.2.1, and 2.3.4 during 2013–2014. Influenza Other Respir. Viruses 2015, 9, 271–276. [Google Scholar] [CrossRef] [PubMed]
- World Health Organization. Antigenic and genetic characteristics of zoonotic influenza A viruses and development of candidate vaccine viruses for pandemic preparedness. Wkly. Epidemiol. Rec. 2020, 95, 525–539. [Google Scholar]
- Shi, W.; Gao, G.F. Emerging H5N8 avian influenza viruses. Science 2021, 372, 784–786. [Google Scholar] [CrossRef]
- European Food Safety Authority; European Centre for Disease Prevention and Control and European Union Reference Laboratory for Avian Influenza. Avian influenza overview November 2019–February2020. EFSA J. 2020, 18, e06096. [Google Scholar] [CrossRef]
- Liang, Y.; Nissen, J.N. Novel Clade 2.3.4.4b Highly Pathogenic Avian Influenza A H5N8 and H5N5 Viruses in Denmark, 2020. Viruses 2021, 13, 886. [Google Scholar] [CrossRef]
- Śmietanka, K.; Świętoń, E. Highly Pathogenic Avian Influenza H5N8 in Poland in 2019–2020. J. Vet. Res. 2020, 64, 469–476. [Google Scholar] [CrossRef]
- Jeong, S.; Lee, D.H. Highly Pathogenic Avian Influenza Clade 2.3.4.4b Subtype H5N8 Virus Isolated from Mandarin Duck in South Korea, 2020. Viruses 2020, 12, 1389. [Google Scholar] [CrossRef]
- European Food Safety Authority, European Centre for Disease Prevention and Control. Avian influenza overview June–September 2022. EFSA J. 2022, 20, e07597. [Google Scholar] [CrossRef]
- Pyankova, O.G.; Susloparov, I.M. Isolation of clade 2.3.4.4b A(H5N8), a highly pathogenic avian influenza virus, from a worker during an outbreak on a poultry farm, Russia, December 2020. Euro. Surveill. 2021, 26, 2100439. [Google Scholar] [CrossRef]
- Wille, M.; Barr, I.G. Resurgence of avian influenza virus. Science 2022, 376, 459–460. [Google Scholar] [CrossRef]
- Zeng, J.; Du, F. Spatiotemporal genotype replacement of H5N8 avian influenza viruses contributed to H5N1 emergence in 2021/2022 panzootic. J. Virol. 2024, 98, e0140123. [Google Scholar] [CrossRef] [PubMed]
- Plaza, P.I.; Gamarra-Toledo, V. Recent Changes in Patterns of Mammal Infection with Highly Pathogenic Avian Influenza A(H5N1) Virus Worldwide. Emerg. Infect. Dis. 2024, 30, 444–452. [Google Scholar] [CrossRef] [PubMed]
- Ye, H.; Zhang, J. Divergent Reassortment and Transmission Dynamics of Highly Pathogenic Avian Influenza A(H5N8) Virus in Birds of China During 2021. Front. Microbiol. 2022, 13, 913551. [Google Scholar] [CrossRef]
- Xiao, C.; Xu, J. Five independent cases of human infection with avian influenza H5N6—Sichuan province, China, 2021. China CDC Wkly. 2021, 3, 751–756. [Google Scholar] [CrossRef]
- European Food Safety Authority; European Centre for Disease Prevention and Control. Avian influenza overview September-December 2023. EFSA J. 2023, 21, e8539. [Google Scholar] [CrossRef]
- Zhu, W.; Li, X. Epidemiologic, Clinical, and Genetic Characteristics of Human Infections with Influenza A(H5N6) Viruses, China. Emerg. Infect. Dis. 2022, 28, 1332–1344. [Google Scholar] [CrossRef]
- Lewis, N.S.; Banyard, A.C. Emergence and spread of novel H5N8, H5N5 and H5N1 clade 2.3.4.4 highly pathogenic avian influenza in 2020. Emerg. Microbes. Infect. 2021, 10, 148–151. [Google Scholar] [CrossRef]
- Swayne, D.E.; Sims, L.D. Strategic challenges in the global control of high pathogenicity avian influenza. Rev. Sci. Tech. 2024, 89–102. (In English) [Google Scholar] [CrossRef]
- Zeng, X.; Deng, G. Protective Efficacy of the Inactivated H5N1 Influenza Vaccine Re-6 Against Different Clades of H5N1 Viruses Isolated in China and the Democratic People’s Republic of Korea. Avian. Dis. 2016, 60, 238–240. [Google Scholar] [CrossRef]
- Charostad, J.; Rezaei Zadeh Rukerd, M. A comprehensive review of highly pathogenic avian influenza (HPAI) H5N1: An imminent threat at doorstep. Travel Med. Infect. Dis. 2023, 55, 102638. [Google Scholar] [CrossRef]
- Ma, J.; Lee, J.; Liu, H. Newcastle disease virus-based H5 influenza vaccine protects chickens from lethal challenge with a highly pathogenic H5N2 avian influenza virus. NPJ Vaccines 2017, 2, 33. [Google Scholar] [CrossRef] [PubMed]
- Vogel, O.A.; Manicassamy, B. Broadly Protective Strategies Against Influenza Viruses: Universal Vaccines and Therapeutics. Front. Microbiol. 2020, 11, 135. [Google Scholar] [CrossRef] [PubMed]
- Bresson, J.L.; Perronne, C. Safety and immunogenicity of an inactivated split-virion influenza A/Vietnam/1194/2004 (H5N1) vaccine: Phase I randomized trial. Lancet 2006, 367, 1657–1664. [Google Scholar] [CrossRef]
- Sridhar, S.; Begom, S. Cellular immune correlate of protection against symptomatic pandemic influenza. Nat. Med. 2013, 19, 1305–1312. [Google Scholar] [CrossRef]
- Manzoli, L.; Salanti, G. Immunogenicity and adverse events of avian influenza A H5N1 vaccine in healthy adults: Multiple-treatments meta-analysis. Lancet Infect. Dis. 2009, 9, 482–492. [Google Scholar] [CrossRef]
- Stephenson, I.; Nicholson, K.G. Boosting immunity to influenza H5N1 with MF59-adjuvanted H5N3 A/Duck/Singapore/97 vaccine in a primed human population. Vaccine 2003, 21, 1687–1693. [Google Scholar] [CrossRef]
- Lin, S.; Chen, J. Evolutionary dynamics and comparative pathogenicity of clade 2.3.4.4b H5 subtype avian influenza viruses, China, 2021–2022. Virol. Sin. 2024, 39, 358–368. [Google Scholar] [CrossRef]
- Hoffmann, E.; Neumann, G. A DNA transfection system for generation of influenza A virus from eight plasmids. Proc. Natl. Acad. Sci. USA 2000, 97, 6108–6113. [Google Scholar] [CrossRef]
- Liu, L.Q.; Li, Z. Development and Assessment of Two Highly Pathogenic Avian Influenza (HPAI) H5N6 Candidate Vaccine Viruses for Pandemic Preparedness. Biomed. Environ. Sci. 2020, 33, 670–679. [Google Scholar] [CrossRef]
- Matsuoka, Y.; Lamirande, E.W. The mouse model for influenza. Curr. Protoc. Microbiol. 2009, 13, 15G.3. [Google Scholar] [CrossRef]
- Sahajpal, N.S.; Mondal, A.K. High-Throughput Next-Generation Sequencing Respiratory Viral Panel: A Diagnostic and Epidemiologic Tool for SARS-CoV-2 and Other Viruses. Viruses 2021, 13, 2063. [Google Scholar] [CrossRef] [PubMed]
- McGinnis, J.; Laplante, J. Next generation sequencing for whole genome analysis and surveillance of influenza A viruses. J. Clin. Virol. 2016, 79, 44–50. [Google Scholar] [CrossRef]
- Zou, S.; Tang, J. Molecular characterization of H3 subtype avian influenza viruses based on poultry-related environmental surveillance in China between 2014 and 2017. Virology 2020, 542, 8–19. [Google Scholar] [CrossRef]
- Díez, F.G.; León, F.C. Manual of Diagnostic Tests and Vaccines for Terrestrial Animals: Soluciones presentes y futuras [The Spanish translation of the Manual of Diagnostic Tests and Vaccines for Terrestrial Animals: Current and future solutions]. Rev. Sci. Tech. 2004, 23, 1023–1031. (In Spanish) [Google Scholar]
- Gao, F.; Yang, T. MiRNA Targeted NP Genome of Live Attenuated Influenza Vaccines Provide Cross-Protection against a Lethal Influenza Virus Infection. Vaccines 2020, 8, 65. [Google Scholar] [CrossRef]
- De Rosa, S.C.; Cohen, K.W. Whole-blood cytokine secretion assay as a high-throughput alternative for assessing the cell-mediated immunity profile after two doses of an adjuvanted SARS-CoV-2 recombinant protein vaccine candidate. Clin. Transl. Immunol. 2022, 11, e1360. [Google Scholar] [CrossRef]
- Hill, N.J.; Bishop, M.A. Ecological divergence of wild birds drives avian influenza spillover and global spread. PLoS Pathog. 2022, 18, e1010062. [Google Scholar] [CrossRef]
- Zost, S.J.; Wu, N.C. Immunodominance and Antigenic Variation of Influenza Virus Hemagglutinin: Implications for Design of Universal Vaccine Immunogens. J. Infect. Dis. 2019, 219, S38–S45. [Google Scholar] [CrossRef]
- Arinaminpathy, N.; Ratmann, O. Impact of cross-protective vaccines on epidemiological and evolutionary dynamics of influenza. Proc. Natl. Acad. Sci. USA 2012, 109, 3173–3177. [Google Scholar] [CrossRef]
- Martins, J.P.; Santos, M. Seasonal Influenza Vaccine Effectiveness in Persons Aged 15–64 Years: A Systematic Review and Meta-Analysis. Vaccines 2023, 11, 1322. [Google Scholar] [CrossRef]
- Van Doorn, E.; Liu, H. Safety and tolerability evaluation of the use of Montanide ISA™51 as vaccine adjuvant: A systematic review. Hum. Vaccin. Immunother. 2016, 12, 159–169. [Google Scholar] [CrossRef]
- Danielsson, R.; Eriksson, H. Aluminium adjuvants in vaccines–A way to modulate the immune response. Semin. Cell Dev. Biol. 2021, 115, 3–9. [Google Scholar] [CrossRef] [PubMed]
- O’Hagan, D.T. MF59 is a safe and potent vaccine adjuvant that enhances protection against influenza virus infection. Expert Rev. Vaccines 2007, 6, 699–710. [Google Scholar] [CrossRef] [PubMed]
- Gao, F.; Liu, X. AddaVax-Adjuvanted H5N8 Inactivated Vaccine Induces Robust Humoral Immune Response against Different Clades of H5 Viruses. Vaccines 2022, 10, 1683. [Google Scholar] [CrossRef]
- Winokur, P.L.; Hegmann, T.E. Safety and Immunogenicity of a monovalent inactivated influenza A/H5N8 virus vaccine given with and without AS03 or MF59 adjuvants in healthy adults. Clin. Infect. Dis. 2023, ciac983. [Google Scholar] [CrossRef]
- Zhang, S.X.; Liu, j. Characteristics of highly pathogenic avian influenza A (H5) viruses in clade 2.3.4.4b in China, 2010−2023. Dis. Surveill. 2024, 40, 226–231. [Google Scholar] [CrossRef]

Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Zhang, S.; Tang, J.; Liu, L.; Wei, H.; Xin, L.; Xiao, K.; Xiao, J.; Dong, J.; Li, Z.; Bai, H.; et al. Construction and Immune Strategy Optimization of a Vaccine Strain for Influenza A (H5N8) Subtype. Viruses 2025, 17, 544. https://doi.org/10.3390/v17040544
Zhang S, Tang J, Liu L, Wei H, Xin L, Xiao K, Xiao J, Dong J, Li Z, Bai H, et al. Construction and Immune Strategy Optimization of a Vaccine Strain for Influenza A (H5N8) Subtype. Viruses. 2025; 17(4):544. https://doi.org/10.3390/v17040544
Chicago/Turabian StyleZhang, Shuxia, Jing Tang, Liqi Liu, Hejiang Wei, Li Xin, Kang Xiao, Jinbo Xiao, Jie Dong, Zi Li, Hongyan Bai, and et al. 2025. "Construction and Immune Strategy Optimization of a Vaccine Strain for Influenza A (H5N8) Subtype" Viruses 17, no. 4: 544. https://doi.org/10.3390/v17040544
APA StyleZhang, S., Tang, J., Liu, L., Wei, H., Xin, L., Xiao, K., Xiao, J., Dong, J., Li, Z., Bai, H., Wang, S., Zhu, W., Yang, L., Zou, S., & Wang, D. (2025). Construction and Immune Strategy Optimization of a Vaccine Strain for Influenza A (H5N8) Subtype. Viruses, 17(4), 544. https://doi.org/10.3390/v17040544





