Emerging Arboviral Diseases in Pakistan: Epidemiology and Public Health Implications
Abstract
1. Introduction
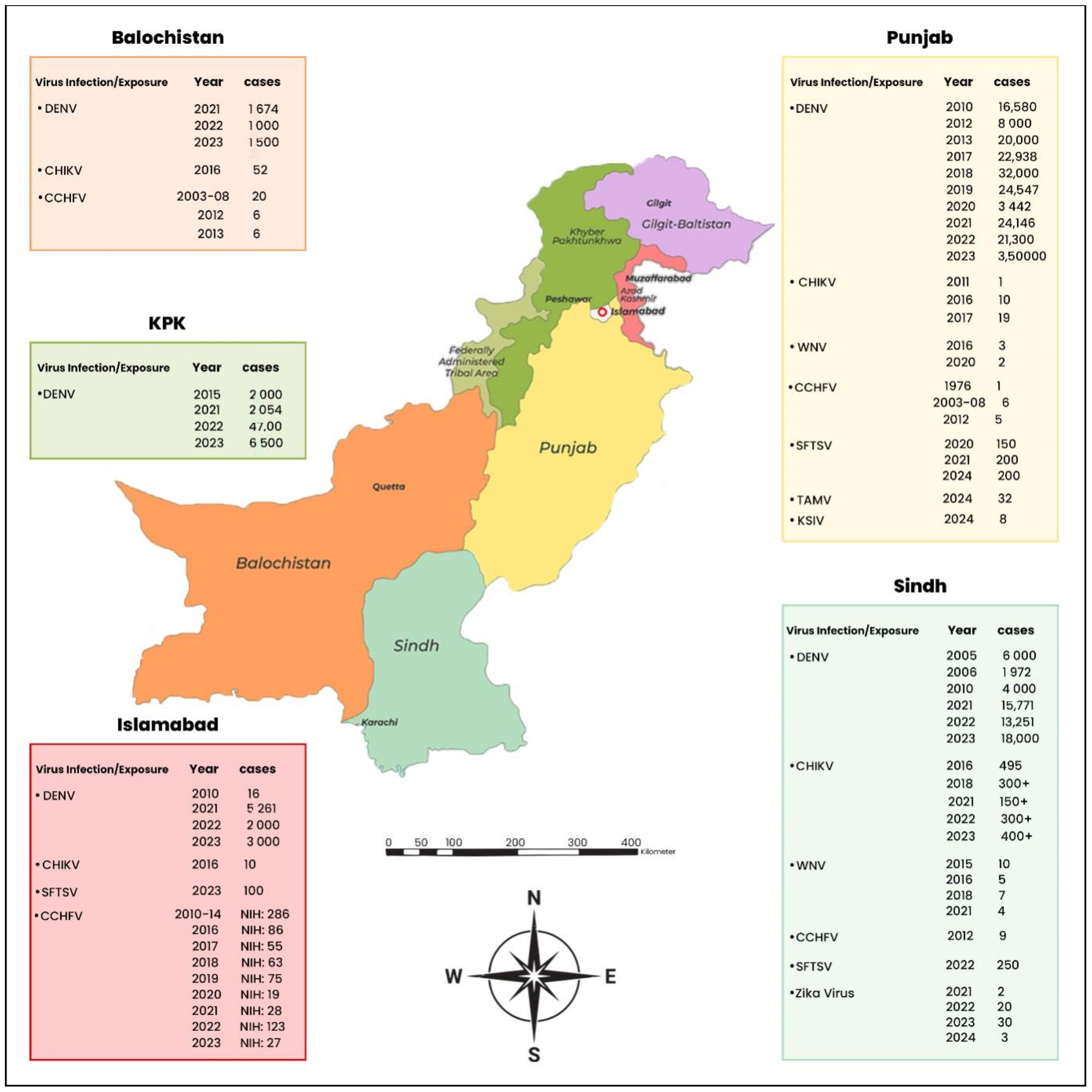
2. Epidemiological Trends of Arboviral Diseases in Pakistan: Mosquito-Borne and Tick-Borne Infections
2.1. Epidemiological Trends of Mosquito-Borne Diseases in Pakistan
2.1.1. Dengue Fever
2.1.2. Chikungunya Virus
2.1.3. West Nile Virus (WNV)
2.1.4. Japanese Encephalitis (JE)
2.1.5. Zika Virus (ZIKV)
2.2. Epidemiological Trends of Tick-Borne Diseases in Pakistan
2.2.1. Severe Fever with Thrombocytopenia Syndrome Virus (SFTSV)
2.2.2. Crimean–Congo Hemorrhagic Fever Virus (CCHFV): An Emerging Health Threat in Pakistan
2.2.3. Tamdy Virus (TAMV) and Karshi Virus (KSIV)
| Arbovirus | Year | Reported Cases | Reported Deaths | Case Fatality Rate % | Vectors | Host Species | References |
|---|---|---|---|---|---|---|---|
| Dengue Fever (DENV) | 1994–2024 | 134985 | 360 | 0.26 | A. aegypti & A. albopictus | Humans, Buffaloes, Rodents, Sheep, Cattle | [2,22,25] |
| Chikungunya Virus (CHIKV) | 1983–2018 | 31771 | - | - | A. aegypti & A. albopictus | Humans, Rodents | [30,31,32] |
| West Nile Virus (WNV) | 1980–2024 | 398 | 1 | 0.25 | B. pipiens & C. quinquefasciatus | Human, horses | [41,42,44] |
| Japanese Encephalitis (JE) | 1980–2018 | 28 | 9 | 32.14 | C. tritaeniorhynchus. | Humans | [49,50,51] |
| Zika Virus (ZIKV) | 2021–2024 | 86 | - | - | A. aegypti & A. albopictus | Humans, livestock | [53,55,86] |
| Severe Fever with Thrombocytopenia Syndrome (SFTSV) | 2020–2024 | 900 | - | - | - | Humans, livestock | [57,86] |
| Crimean-Congo Hemorrhagic Fever Virus (CCHFV) | 1976–2024 | 1314 | 247 | 18.79 | H. anatolicum H. marginatum H. dromedarii Rhipicephalus Spp. | Humans, Cattle, Sheep, goat | [72,77,86] |
| Tamdy Virus (TAMV) | 2019–2014 | 32 | - | - | - | Humans | [86] |
| Karshi Virus (KSIV) | 2019–2014 | 8 | - | - | - | Humans | [86] |
3. Discussion
4. Future Perspectives
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Butt, M.H.; Safdar, A.; Amir, A.; Zaman, M.; Ahmad, A.; Saleem, R.T.; Misbah, S.; Khan, Y.H.; Mallhi, T.H. Arboviral diseases and COVID-19 coincidence: Challenges for Pakistan’s derelict healthcare system. J. Med. Virol. 2021, 93, 6465–6467. [Google Scholar] [CrossRef] [PubMed]
- Khan, U.; Azeem, S. The rising toll of dengue cases in Pakistan every year: An incipient crisis. Ann. Med. Surg. 2022, 76, 103549. [Google Scholar] [CrossRef]
- Awan, U.A.; Zahoor, S.; Ayub, A.; Ahmed, H.; Aftab, N.; Aftab, N.; Afzal, M.S. COVID-19 and arboviral diseases: Another challenge for Pakistan’s dilapidated healthcare system. J. Med. Virol. 2020, 93, 4065. [Google Scholar] [CrossRef] [PubMed]
- Badar, N.; Salman, M.; Ansari, J.; Aamir, U.; Alam, M.M.; Arshad, Y.; Mushtaq, N.; Ikram, A.; Qazi, J. Emergence of Chikungunya Virus, Pakistan, 2016–2017. Emerg. Infect. Dis. 2020, 26, 307–310. [Google Scholar] [CrossRef]
- Kasi, K.K.; von Arnim, F.; Schulz, A.; Rehman, A.; Chudhary, A.; Oneeb, M.; Sas, M.A.; Jamil, T.; Maksimov, P.; Sauter-Louis, C.; et al. Crimean-Congo haemorrhagic fever virus in ticks collected from livestock in Balochistan, Pakistan. Transbound. Emerg. Dis. 2020, 67, 1543–1552. [Google Scholar] [CrossRef] [PubMed]
- Waris, A.; Anwar, F.; Asim, M.; Bibi, F. Is the bell ringing for another outbreak of Crimean-Congo hemorrhagic fever in Pakistan? Public Heal. Pr. 2022, 4, 100319. [Google Scholar] [CrossRef]
- Zohaib, A.; Saqib, M.; Athar, M.; Hussain, M.; Sial, A.-U.-R.; Tayyab, M.; Batool, M.; Sadia, H.; Taj, Z.; Tahir, U.; et al. Crimean-Congo Hemorrhagic Fever Virus in Humans and Livestock, Pakistan, 2015–2017. Emerg. Infect. Dis. J. 2020, 26, 773. [Google Scholar] [CrossRef]
- Mordecai, E.A.; Cohen, J.M.; Evans, M.V.; Gudapati, P.; Johnson, L.R.; Lippi, C.A.; Miazgowicz, K.; Murdock, C.C.; Rohr, J.R.; Ryan, S.J.; et al. Detecting the impact of temperature on transmission of Zika, dengue, and chikungunya using mechanistic models. PLoS Neglected Trop. Dis. 2017, 11, e0005568. [Google Scholar] [CrossRef] [PubMed]
- Rasheed, S.B.; Butlin, R.K.; Boots, M. A review of dengue as an emerging disease in Pakistan. Public. Health 2013, 127, 11–17. [Google Scholar] [CrossRef]
- Saeed, U.; Piracha, Z.Z. Viral outbreaks and communicable health hazards due to devastating floods in Pakistan. World J. Virol. 2016, 5, 82–84. [Google Scholar] [CrossRef]
- Aamir, U.B.; Badar, N.; Salman, M.; Ahmed, M.; Alam, M.M. Outbreaks of chikungunya in Pakistan. Lancet Infect. Dis. 2017, 17, 483. [Google Scholar] [CrossRef]
- Suleman, M.; Arshad, M.; Khan, K. Yellowfever mosquito (Diptera: Culicidae) introduced into Landi Kotal, Pakistan, by tire importation. J. Med. Entomol. 1996, 33, 689–693. [Google Scholar] [CrossRef] [PubMed]
- Imran, M.; Saleemi, M.K.; Chen, Z.; Wang, X.; Zhou, D.; Li, Y.; Zhao, Z.; Zheng, B.; Li, Q.; Cao, S.; et al. Decanoyl-Arg-Val-Lys-Arg-Chloromethylketone: An Antiviral Compound That Acts against Flaviviruses through the Inhibition of Furin-Mediated prM Cleavage. Viruses 2019, 11, 1011. [Google Scholar] [CrossRef] [PubMed]
- Roberts, A.; Kemp, C. Infectious diseases of refugees and immigrants: Dengue fever. J. Am. Acad. Nurse Pract. 2001, 13, 243–245. [Google Scholar] [CrossRef]
- Khan, J.; Khan, I.; Amin, I. A Comprehensive Entomological, Serological and Molecular Study of 2013 Dengue Outbreak of Swat, Khyber Pakhtunkhwa, Pakistan. PLoS ONE 2016, 11, e0147416. [Google Scholar] [CrossRef] [PubMed]
- Samsudin, N.A.; Othman, H.; Siau, C.S.; Zaini, Z.-I.I. Exploring community needs in combating aedes mosquitoes and dengue fever: A study with urban community in the recurrent hotspot area. BMC Public. Health 2024, 24, 1651. [Google Scholar] [CrossRef]
- Imran, M.; Ye, J.; Saleemi, M.K.; Shaheen, I.; Zohaib, A.; Chen, Z.; Cao, S. Epidemiological trends of mosquito-borne viral diseases in Pakistan. Anim. Dis. 2022, 2, 5. [Google Scholar] [CrossRef]
- Khan, J.; Khan, I.; Ghaffar, A.; Khalid, B. Epidemiological trends and risk factors associated with dengue disease in Pakistan (1980–2014): A systematic literature search and analysis. BMC Public Health 2018, 18, 745. [Google Scholar] [CrossRef] [PubMed]
- Zohra, T.; Din, M.; Ikram, A.; Bashir, A.; Jahangir, H.; Baloch, I.S.; Irshad, S.; Waris, A.; Salman, M.; Iqtadar, S.; et al. Demographic and clinical features of dengue fever infection in Pakistan: A cross-sectional epidemiological study. Trop. Dis. Travel Med. Vaccines 2024, 10, 11. [Google Scholar] [CrossRef] [PubMed]
- Khan, M.A.; Imtiaz, K.; Shafaq, H.; Farooqi, J.; Hassan, M.; Zafar, A.; Long, M.T.; Barr, K.L.; Khan, E.J.V.S. Screening for arboviruses in healthy blood donors: Experience from Karachi, Pakistan. Virol. Sin. 2022, 37, 774. [Google Scholar] [CrossRef]
- Tabassum, S.; Naeem, A.; Nazir, A.; Naeem, F.; Gill, S.; Tabassum, S. Year-round dengue fever in Pakistan, highlighting the surge amidst ongoing flood havoc and the COVID-19 pandemic: A comprehensive review. Ann. Med. Surg. 2023, 85, 908–912. [Google Scholar] [CrossRef] [PubMed]
- World Health Organization. Dengue-Global Situation. 2024. Available online: https://www.who.int/emergencies/disease-outbreak-news/item/2024-DON518 (accessed on 30 May 2024).
- Abdulsalam, F.I.; Antunez, P.; Yimthiang, S.; Jawjit, W. Influence of climate variables on dengue fever occurrence in the southern region of Thailand. PLoS Glob. Public Health 2022, 2, e0000188. [Google Scholar] [CrossRef] [PubMed]
- Ladner, J.; Rodrigues, M.; Davis, B.; Besson, M.-H.; Audureau, E.; Saba, J. Societal impact of dengue outbreaks: Stakeholder perceptions and related implications. A qualitative study in Brazil, 2015. PLoS Neglected Trop. Dis. 2017, 11, e0005366. [Google Scholar] [CrossRef] [PubMed]
- Aftab, S.; Yaqoob, E.; Javed, S. Dengue epidemic: Pakistan on alert. Lancet 2024, 404, 1807. [Google Scholar] [CrossRef] [PubMed]
- Dengue—Pakistan. 2024. Available online: https://www.nhsrc.gov.pk/LatestNews (accessed on 21 March 2024).
- Overgaard, H.J.; Dada, N.; Lenhart, A.; Stenström, T.A.B.; Alexander, N. Integrated disease management: Arboviral infections and waterborne diarrhoea. Bull. World Health Organ. 2021, 99, 583–592. [Google Scholar] [CrossRef]
- Feng, X.; Jiang, N.; Zheng, J.; Zhu, Z.; Chen, J.; Duan, L.; Song, P.; Sun, J.; Zhang, X.; Hang, L.; et al. Advancing knowledge of One Health in China: Lessons for One Health from China’s dengue control and prevention programs. Sci. One Health 2024, 3, 100087. [Google Scholar] [CrossRef] [PubMed]
- Lu, H.Z.; Sui, Y.; Lobo, N.F.; Fouque, F.; Gao, C.; Lu, S.; Lv, S.; Deng, S.Q.; Wang, D.Q. Challenge and opportunity for vector control strategies on key mosquito-borne diseases during the COVID-19 pandemic. Front. Public Health 2023, 11, 1207293. [Google Scholar] [CrossRef] [PubMed]
- Rauf, M.; Fatima Tuz, Z.; Manzoor, S.; Mehmood, A.; Bhatti, S. Outbreak of chikungunya in Pakistan. Lancet Infect. Dis. 2017, 17, 258. [Google Scholar] [CrossRef]
- Barr, K.L.; Khan, E.; Farooqi, J.Q.; Imtiaz, K.; Prakoso, D.; Malik, F.; Lednicky, J.A.; Long, M.T. Evidence of Chikungunya Virus Disease in Pakistan Since 2015 With Patients Demonstrating Involvement of the Central Nervous System. Front. Public Health 2018, 6, 186. [Google Scholar] [CrossRef]
- Khongwichit, S.; Chansaenroj, J.; Chirathaworn, C.; Poovorawan, Y. Chikungunya virus infection: Molecular biology, clinical characteristics, and epidemiology in Asian countries. J. Biomed. Sci. 2021, 28, 84. [Google Scholar] [CrossRef] [PubMed]
- Iqtadar, S.; Akram, J.; Khan, A. The Urgent Need for Dengue Vaccination: Combating an Escalating Public Health Crisis in Pakistan. Vaccines 2024, 12, 913. [Google Scholar] [CrossRef]
- Badar, N.; Salman, M.; Ansari, J.; Ikram, A.; Qazi, J.; Alam, M.M. Epidemiological trend of chikungunya outbreak in Pakistan: 2016–2018. PLoS Neglected Trop. Dis. 2019, 13, e0007118. [Google Scholar] [CrossRef]
- Abdul-Ghani, R.; Fouque, F.; Mahdy, M.A.K.; Zhong, Q.; Al-Eryani, S.M.A.; Alkwri, A.; Beier, J.C. Multisectoral Approach to Address Chikungunya Outbreaks Driven by Human Mobility: A Systematic Review and Meta-Analysis. J. Infect. Dis. 2020, 222, S709–S716. [Google Scholar] [CrossRef]
- Côrtes, N.; Lira, A.; Prates-Syed, W.; Dinis Silva, J.; Vuitika, L.; Cabral-Miranda, W.; Durães-Carvalho, R.; Balan, A.; Cabral-Marques, O.; Cabral-Miranda, G. Integrated control strategies for dengue, Zika, and Chikungunya virus infections. Front. Immunol. 2023, 14, 1281667. [Google Scholar] [CrossRef] [PubMed]
- Mourad, O.; Makhani, L.; Chen, L.H. Chikungunya: An Emerging Public Health Concern. Curr. Infect. Dis. Rep. 2022, 24, 217–228. [Google Scholar] [CrossRef] [PubMed]
- Zhang, L.; Guo, W.; Lv, C. Modern technologies and solutions to enhance surveillance and response systems for emerging zoonotic diseases. Sci. One Health 2024, 3, 100061. [Google Scholar] [CrossRef] [PubMed]
- Morrison, C.R.; Plante, K.S.; Heise, M.T. Chikungunya Virus: Current Perspectives on a Reemerging Virus. Microbiol. Spectr. 2016, 4, 143–161. [Google Scholar] [CrossRef]
- Silva, L.A.; Dermody, T.S. Chikungunya virus: Epidemiology, replication, disease mechanisms, and prospective intervention strategies. J. Clin. Investig. 2017, 127, 737–749. [Google Scholar] [CrossRef]
- Burney, M.; Munir, A. Role of arthropod borne viruses in human diseases in Rawalpindi and Peshawar area. II. Isolation of West Nile virus from human blood and culicine mosquitoes in Rawalpindi area. Pak. J. Med. Res. 1966, 5, 271–284. [Google Scholar]
- Hayes, C.G.; Baqar, S.; Ahmed, T.; Chowdhry, M.A.; Reisen, W.K. West Nile virus in Pakistan. 1. Sero-epidemiological studies in Punjab Province. Trans. R. Soc. Trop. Med. Hyg. 1982, 76, 431–436. [Google Scholar] [CrossRef]
- Chowdhury, P.; Khan, S.A. Global emergence of West Nile virus: Threat & preparedness in special perspective to India. Indian J. Med. Res. 2021, 154, 36–50. [Google Scholar] [CrossRef] [PubMed]
- Khan, E.; Barr, K.L.; Farooqi, J.Q.; Prakoso, D.; Abbas, A.; Khan, Z.Y.; Ashi, S.; Imtiaz, K.; Aziz, Z.; Malik, F.; et al. Human West Nile Virus Disease Outbreak in Pakistan, 2015–2016. Front. Public Health 2018, 6, 20. [Google Scholar] [CrossRef] [PubMed]
- Wang, H.-R.; Liu, T.; Gao, X.; Wang, H.-B.; Xiao, J.-H. Impact of climate change on the global circulation of West Nile virus and adaptation responses: A scoping review. Infect. Dis. Poverty 2024, 13, 38. [Google Scholar] [CrossRef] [PubMed]
- Singh, G.; Kumar, S.; Kumar, D.; Mishra, G. Biological control of the mosquito: An analysis of the impediments and possibilities. Int. J. Mosq. Res. 2023, 10, 117–126. [Google Scholar] [CrossRef]
- Bugshan, W.; Qahtani, S.; Alwagdani, N.; Alharthi, M.; Alqarni, A.; Alsuat, H.; Alqahtani, N.; Alshammari, M.; Albaqami, R.; Almotairi, A. Role of Health Awareness Campaigns in Improving Public Health:A Systematic Review: Life Sciences-Public Health. Int. J. Life Sci. Pharma Res. 2022, 12, L29–L35. [Google Scholar] [CrossRef]
- Singh, P.; Khatib, M.N.; Ballal, S.; Kaur, M.; Nathiya, D.; Sharma, S.; Siva Prasad, G.V.; Sinha, A.; Gaidhane, A.M.; Mohapatra, P.; et al. West Nile Virus in a Changing Climate: Epidemiology, pathology, advances in diagnosis and treatment, vaccine designing and control strategies, emerging public health challenges—A comprehensive review. Emerg. Microbes Infect. 2025, 14, 2437244. [Google Scholar] [CrossRef]
- Fatima, T.; Rais, A.; Khan, E.; Hills, S.L.; Chambers, T.V.; Hotwani, A.; Qureshi, S.; Shafquat, S.; Malik, S.; Qamar, F.; et al. Investigation of Japanese encephalitis virus as a cause of acute encephalitis in southern Pakistan, April 2015-January 2018. PLoS ONE 2020, 15, e0234584. [Google Scholar] [CrossRef] [PubMed]
- Vannice, K.S.; Hills, S.L.; Schwartz, L.M.; Barrett, A.D.; Heffelfinger, J.; Hombach, J.; Letson, G.W.; Solomon, T.; Marfin, A.A. The future of Japanese encephalitis vaccination: Expert recommendations for achieving and maintaining optimal JE control. NPJ Vaccines 2021, 6, 82. [Google Scholar] [CrossRef] [PubMed]
- Sugamata, M.; Ahmed, A.; Miura, T.; Takasu, T.; Kono, R.; Ogata, T.; Kimura-Kuroda, J.; Yasui, K. Seroepidemiological study of infection with West Nile virus in Karachi, Pakistan, in 1983 and 1985. J. Med. Virol. 1988, 26, 243–247. [Google Scholar] [CrossRef]
- Campbell, G.L.; Hills, S.L.; Fischer, M.; Jacobson, J.A.; Hoke, C.H.; Hombach, J.M.; Marfin, A.A.; Solomon, T.; Tsai, T.F.; Tsu, V.D.; et al. Estimated global incidence of Japanese encephalitis: A systematic review. Bull. World Health Organ. 2011, 89, 766–774, 774a–774e. [Google Scholar] [CrossRef] [PubMed]
- Hughes, R.A.; Cornblath, D.R. Guillain-barre syndrome. Lancet 2005, 366, 1653–1666. [Google Scholar] [CrossRef] [PubMed]
- Wahid, B.; Ali, A.; Rafique, S.; Idrees, M. Zika: As an emergent epidemic. Asian Pac. J. Trop. Med. 2016, 9, 723–729. [Google Scholar] [CrossRef]
- Butt, A.M.; Siddique, S.; Gardner, L.M.; Sarkar, S.; Lancelot, R.; Qamar, R. Zika virus in Pakistan: The tip of the iceberg? Lancet Glob. Health 2016, 4, e913–e914. [Google Scholar] [CrossRef] [PubMed]
- Dhimal, M.; Dahal, S.; Dhimal, M.L.; Mishra, S.R.; Karki, K.B.; Aryal, K.K.; Haque, U.; Kabir, M.I.; Guin, P.; Butt, A.M.; et al. Threats of Zika virus transmission for Asia and its Hindu-Kush Himalayan region. Infect. Dis. Poverty 2018, 7, 40. [Google Scholar] [CrossRef] [PubMed]
- Darwish, M.A.; Hoogstraal, H.; Roberts, T.J.; Ahmed, I.P.; Omar, F. A sero-epidemiological survey for certain arboviruses (Togaviridae) in Pakistan. Trans. R. Soc. Trop. Med. Hyg. 1983, 77, 442–445. [Google Scholar] [CrossRef]
- Zohaib, A.; Zhang, J.; Saqib, M.; Athar, M.A.; Hussain, M.H.; Chen, J.; Sial, A.-u.-R.; Tayyab, M.H.; Batool, M.; Khan, S.; et al. Serologic Evidence of Severe Fever with Thrombocytopenia Syndrome Virus and Related Viruses in Pakistan. Emerg. Infect. Dis. J. 2020, 26, 1513. [Google Scholar] [CrossRef] [PubMed]
- Casel, M.A.; Park, S.J.; Choi, Y.K. Severe fever with thrombocytopenia syndrome virus: Emerging novel phlebovirus and their control strategy. Exp. Mol. Med. 2021, 53, 713–722. [Google Scholar] [CrossRef] [PubMed]
- Luo, N.; Li, M.; Xu, M.; Shi, C.; Shi, X.; Ni, R.; Chen, Y.; Zheng, L.; Tu, Y.; Hu, D.; et al. Research Progress of Fever with Thrombocytopenia Syndrome. Intensive Care Res. 2023, 3, 172–181. [Google Scholar] [CrossRef] [PubMed]
- Bopp, N.E.; Kaiser, J.A.; Strother, A.E.; Barrett, A.D.T.; Beasley, D.W.C.; Benassi, V.; Milligan, G.N.; Preziosi, M.P.; Reece, L.M. Baseline mapping of severe fever with thrombocytopenia syndrome virology, epidemiology and vaccine research and development. NPJ Vaccines 2020, 5, 111. [Google Scholar] [CrossRef]
- Maslow, J.N.; Kwon, J.J.; Mikota, S.K.; Spruill, S.; Cho, Y.; Jeong, M. Severe fever and thrombocytopenia syndrome virus infection: Considerations for vaccine evaluation of a rare disease. Human Vaccines Immunother. 2019, 15, 2249–2257. [Google Scholar] [CrossRef]
- Linsuwanon, P.; Poovorawan, Y.; Lee, K.H.; Auysawasdi, N.; Wongwairot, S.; Limsuwan, C.; Vuthitanachot, V.; Leepitakrat, S.; Vongpunsawasdi, S.; Nilyanimit, P.; et al. Comprehensive Surveillance of Severe Fever with Thrombocytopenia Syndrome Virus in Patients with Acute Febrile Illness, Wild Rodents, and Trombiculid Larval Mites, Thailand. Emerg. Infect. Dis. J. 2024, 30, 111. [Google Scholar] [CrossRef]
- Wang, Y.; Li, K.; Li, P.; Sun, J.; Ye, L.; Dai, Y.; Tang, A.; Jiang, J.; Chen, C.; Tong, Z.; et al. Community-based comprehensive measures to prevent severe fever with thrombocytopenia syndrome, China. Int. J. Infect. Dis. 2018, 73, 63–66. [Google Scholar] [CrossRef]
- Ai, L.; Wang, W.; Teng, Z. Advancements in the Worldwide Detection of Severe Fever with Thrombocytopenia Syndrome Virus Infection from 2009 to 2023. China CDC Wkly. 2023, 5, 687–693. [Google Scholar] [CrossRef] [PubMed]
- Li, J.C.; Zhao, J.; Li, H.; Fang, L.Q.; Liu, W. Epidemiology, clinical characteristics, and treatment of severe fever with thrombocytopenia syndrome. Infect. Med. 2022, 1, 40–49. [Google Scholar] [CrossRef]
- Burney, M.I.; Ghafoor, A.; Saleen, M.; Webb, P.A.; Casals, J. Nosocomial outbreak of viral hemorrhagic fever caused by Crimean Hemorrhagic fever-Congo virus in Pakistan, January 1976. Am. J. Trop. Med. Hyg. 1980, 29, 941–947. [Google Scholar] [CrossRef] [PubMed]
- Alam, M.M.; Khurshid, A.; Sharif, S.; Shaukat, S.; Rana, M.S.; Angez, M.; Zaidi, S.S. Genetic analysis and epidemiology of Crimean Congo Hemorrhagic fever viruses in Baluchistan province of Pakistan. BMC Infect. Dis. 2013, 13, 201. [Google Scholar] [CrossRef] [PubMed]
- Wahid, B.; Altaf, S.; Naeem, N.; Ilyas, N.; Idrees, M. Scoping Review of Crimean-Congo Hemorrhagic Fever (CCHF) Literature and Implications of Future Research. J. Coll. Physicians Surg. Pak. 2019, 29, 563–573. [Google Scholar] [CrossRef] [PubMed]
- Saleem, J.; Usman, M.; Nadeem, A.; Sethi, S.A.; Salman, M. Crimean–Congo hemorrhagic fever: A first case from Abbottabad, Pakistan. Int. J. Infect. Dis. 2009, 13, e121–e123. [Google Scholar] [CrossRef] [PubMed]
- Sahito, A.M.; Mir, S.L.; Waseem, M.; Awan, M.A.E.; Shaikh, S.; Essar, M.Y. The possibility of the emergence of Crimean-Congo virus cases during Eid ul Adha: A troubling situation during a blessed festival. Ann. Med. Surg. 2022, 81, 104379. [Google Scholar] [CrossRef] [PubMed]
- Umair, M.; Rehman, Z.; Haider, S.A.; Ali, Q.; Hakim, R.; Bibi, S.; Salman, M.; Ikram, A. Whole-genome sequencing of Crimean-Congo hemorrhagic fever virus circulating in Pakistan during 2022. J. Med. Virol. 2023, 95, e28604. [Google Scholar] [CrossRef] [PubMed]
- Umair, M.; Haider, S.A.; Ali, Q.; Hakim, R.; Raisani, M.A.; Ayub, A.; Salman, M. Genomic characterization of Crimean-Congo Hemorrhagic Fever Virus detected during nosocomial outbreak (2023) in Balochistan province of Pakistan. medRxiv, 2023; preprint. [Google Scholar] [CrossRef]
- Field Epidemiology & Disease Surveillance Division, National Institute of Health, Islamabad. FELTP Pakistan Weekly Epidemiological Report, August 15–21, 2021. Available online: https://www.nih.org.pk/ (accessed on 30 May 2024).
- Tabassum, S.; Naeem, A.; Khan, M.Z.; Mumtaz, N.; Gill, S.; Ohadi, L. Crimean-Congo hemorrhagic fever outbreak in Pakistan, 2022: A warning bell amidst unprecedented floods and COVID 19 pandemic. Health Sci. Rep. 2023, 6, e1055. [Google Scholar] [CrossRef] [PubMed]
- Srivastava, S.; Kumar, S.; Sharma, P.K.; Rustagi, S.; Mohanty, A.; Donovan, S.; Henao-Martinez, A.F.; Sah, R.; Franco-Paredes, C. Control strategies for emerging infectious diseases: Crimean-Congo hemorrhagic fever management. Health Sci. Rep. 2024, 7, e70053. [Google Scholar] [CrossRef]
- de la Fuente, J.; Ghosh, S.; Lempereur, L.; Garrison, A.; Sprong, H.; Lopez-Camacho, C.; Maritz-Olivier, C.; Contreras, M.; Moraga-Fernández, A.; Bente, D.A. Interventions for the control of Crimean-Congo hemorrhagic fever and tick vectors. NPJ Vaccines 2024, 9, 181. [Google Scholar] [CrossRef]
- Sorvillo, T.E.; Rodriguez, S.E.; Hudson, P.; Carey, M.; Rodriguez, L.L.; Spiropoulou, C.F.; Bird, B.H.; Spengler, J.R.; Bente, D.A. Towards a Sustainable One Health Approach to Crimean-Congo Hemorrhagic Fever Prevention: Focus Areas and Gaps in Knowledge. Trop. Med. Infect. Dis. 2020, 5, 113. [Google Scholar] [CrossRef]
- Verbeek, J.H.; Rajamaki, B.; Ijaz, S.; Sauni, R.; Toomey, E.; Blackwood, B.; Tikka, C.; Ruotsalainen, J.H.; Kilinc Balci, F.S. Personal protective equipment for preventing highly infectious diseases due to exposure to contaminated body fluids in healthcare staff. Cochrane Database Syst. Rev. 2020, 4, Cd011621. [Google Scholar] [CrossRef]
- Okesanya, O.J.; Olatunji, G.D.; Kokori, E.; Olaleke, N.O.; Adigun, O.A.; Manirambona, E.; Lucero-Prisno, D.E., 3rd. Looking Beyond the Lens of Crimean-Congo Hemorrhagic Fever in Africa. Emerg. Infect. Dis. 2024, 30, 1319–1325. [Google Scholar] [CrossRef]
- Eisen, L.; Stafford, K.C. Barriers to Effective Tick Management and Tick-Bite Prevention in the United States (Acari: Ixodidae). J. Med. Entomol. 2021, 58, 1588–1600. [Google Scholar] [CrossRef] [PubMed]
- Patel, A.A.; Dalal, Y.D.; Parikh, A.; Gandhi, R.; Shah, A. Crimean-Congo Hemorrhagic Fever: An Emerging Viral Infection in India, Revisited and Lessons Learned. Cureus 2023, 15, e43315. [Google Scholar] [CrossRef]
- Girard, M.; Nelson, C.B.; Picot, V.; Gubler, D.J. Arboviruses: A global public health threat. Vaccine 2020, 38, 3989–3994. [Google Scholar] [CrossRef] [PubMed]
- Nejati, J.; Mohammadi, M.; Okati-Aliabad, H. Knowledge, attitudes, and practices regarding Crimean-Congo hemorrhagic fever in a high-prevalence suburban community, southeast of Iran. Heliyon 2024, 10, e23414. [Google Scholar] [CrossRef]
- Moming, A.; Shen, S.; Fang, Y.; Zhang, J.; Zhang, Y.; Tang, S.; Li, T.; Hu, Z.; Wang, H.; Zhang, Y.; et al. Evidence of human exposure to Tamdy virus, Northwest China. Emerg. Infect. Dis. 2021, 27, 3166. [Google Scholar] [CrossRef] [PubMed]
- Chen, S.; Saqib, M.; Khan, H.S.; Bai, Y.; Ashfaq, U.A.; Mansoor, M.K.; Moming, A.; Liu, J.; Zhou, M.; Niazi, S.K.; et al. Risk of infection with arboviruses in a healthy population in Pakistan based on seroprevalence. Virol. Sin. 2024, 39, 369–377. [Google Scholar] [CrossRef]
- Defaye, B.; Moutailler, S.; Pasqualini, V.; Quilichini, Y. Distribution of Tick-Borne Pathogens in Domestic Animals and Their Ticks in the Countries of the Mediterranean Basin between 2000 and 2021: A Systematic Review. Microorganisms 2022, 10, 1236. [Google Scholar] [CrossRef] [PubMed]
- Yu, K.M.; Park, S.J. Tick-borne viruses: Epidemiology, pathogenesis, and animal models. One Health 2024, 19, 100903. [Google Scholar] [CrossRef]
- Afzal, M.F.; Naqvi, S.Q.; Sultan, M.A.; Hanif, A. Chikungunya fever among children presenting with nonspecific febrile illness during an epidemic of dengue fever in Lahore, Pakistan. Merit Res. J. Med. Med. Sci. 2015, 3, 69–73. [Google Scholar]
- Atwan, Z.; Alhilfi, R.; Mousa, A.K.; Rawaf, S.; Torre, J.D.L.; Hashim, A.R.; Sharquie, I.K.; Khaleel, H.; Tabche, C. Alarming update on incidence of Crimean-Congo hemorrhagic fever in Iraq in 2023. IJID Reg. 2024, 10, 75–79. [Google Scholar] [CrossRef]
- Ali, I.; Dasti, J.I. Chikungunya virus; an emerging arbovirus in Pakistan. J. Pak. Med. Assoc. 2018, 68, 252–257. [Google Scholar]
- Rehman, A.; Conraths, F.J.; Sauter-Louis, C.; Krücken, J.; Nijhof, A.M. Epidemiology of tick-borne pathogens in the semi-arid and the arid agro-ecological zones of Punjab province, Pakistan. Transbound. Emerg. Dis. 2019, 66, 526–536. [Google Scholar] [CrossRef] [PubMed]
- Rodriguez, J. One Health Ethics and the Ethics of Zoonoses: A Silent Call for Global Action. Vet. Sci. 2024, 11, 394. [Google Scholar] [CrossRef] [PubMed]
- Dagostin, F.; Tagliapietra, V.; Marini, G.; Cataldo, C.; Bellenghi, M.; Pizzarelli, S.; Cammarano, R.R.; Wint, W.; Alexander, N.S.; Neteler, M.; et al. Ecological and environmental factors affecting the risk of tick-borne encephalitis in Europe, 2017 to 2021. Eurosurveillance 2023, 28, 2300121. [Google Scholar] [CrossRef]
- Kraemer, M.U.G.; Reiner, R.C.; Brady, O.J.; Messina, J.P.; Gilbert, M.; Pigott, D.M.; Yi, D.; Johnson, K.; Earl, L.; Marczak, L.B.; et al. Past and future spread of the arbovirus vectors Aedes albopictus and Aedes albopictus. Nat. Microbiol. 2019, 4, 854–863. [Google Scholar] [CrossRef]
- Kolimenakis, A.; Heinz, S.; Wilson, M.L.; Winkler, V.; Yakob, L.; Michaelakis, A.; Papachristos, D.; Richardson, C.; Horstick, O. The role of urbanisation in the spread of Aedes mosquitoes and the diseases they transmit—A systematic review. PLoS Neglected Trop. Dis. 2021, 15, e0009631. [Google Scholar] [CrossRef] [PubMed]
- Lizzi, K.M.; Qualls, W.A.; Brown, S.C.; Beier, J.C. Expanding Integrated Vector Management to promote healthy environments. Trends Parasitol. 2014, 30, 394–400. [Google Scholar] [CrossRef]
- Belay, E.D.; Kile, J.C.; Hall, A.J.; Barton-Behravesh, C.; Parsons, M.B.; Salyer, S.; Walke, H. Zoonotic Disease Programs for Enhancing Global Health Security. Emerg. Infect. Dis. 2017, 23, S65–S70. [Google Scholar] [CrossRef]
- Yasmeen, N.; Jabbar, A.; Shah, T.; Fang, L.-X.; Aslam, B.; Naseeb, I.; Shakeel, F.; Ahmad, H.I.; Baloch, Z.; Liu, Y. One Health Paradigm to Confront Zoonotic Health Threats: A Pakistan Prospective. Front. Microbiol. 2022, 12, 719334. [Google Scholar] [CrossRef] [PubMed]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Ammar, M.; Moaaz, M.; Yue, C.; Fang, Y.; Zhang, Y.; Shen, S.; Deng, F. Emerging Arboviral Diseases in Pakistan: Epidemiology and Public Health Implications. Viruses 2025, 17, 232. https://doi.org/10.3390/v17020232
Ammar M, Moaaz M, Yue C, Fang Y, Zhang Y, Shen S, Deng F. Emerging Arboviral Diseases in Pakistan: Epidemiology and Public Health Implications. Viruses. 2025; 17(2):232. https://doi.org/10.3390/v17020232
Chicago/Turabian StyleAmmar, Muhammad, Muhammad Moaaz, Chaoxiong Yue, Yaohui Fang, Yanfang Zhang, Shu Shen, and Fei Deng. 2025. "Emerging Arboviral Diseases in Pakistan: Epidemiology and Public Health Implications" Viruses 17, no. 2: 232. https://doi.org/10.3390/v17020232
APA StyleAmmar, M., Moaaz, M., Yue, C., Fang, Y., Zhang, Y., Shen, S., & Deng, F. (2025). Emerging Arboviral Diseases in Pakistan: Epidemiology and Public Health Implications. Viruses, 17(2), 232. https://doi.org/10.3390/v17020232






