The Role of Nucleocapsid Protein (NP) in the Immunology of Crimean–Congo Hemorrhagic Fever Virus (CCHFV)
Abstract
1. Introduction
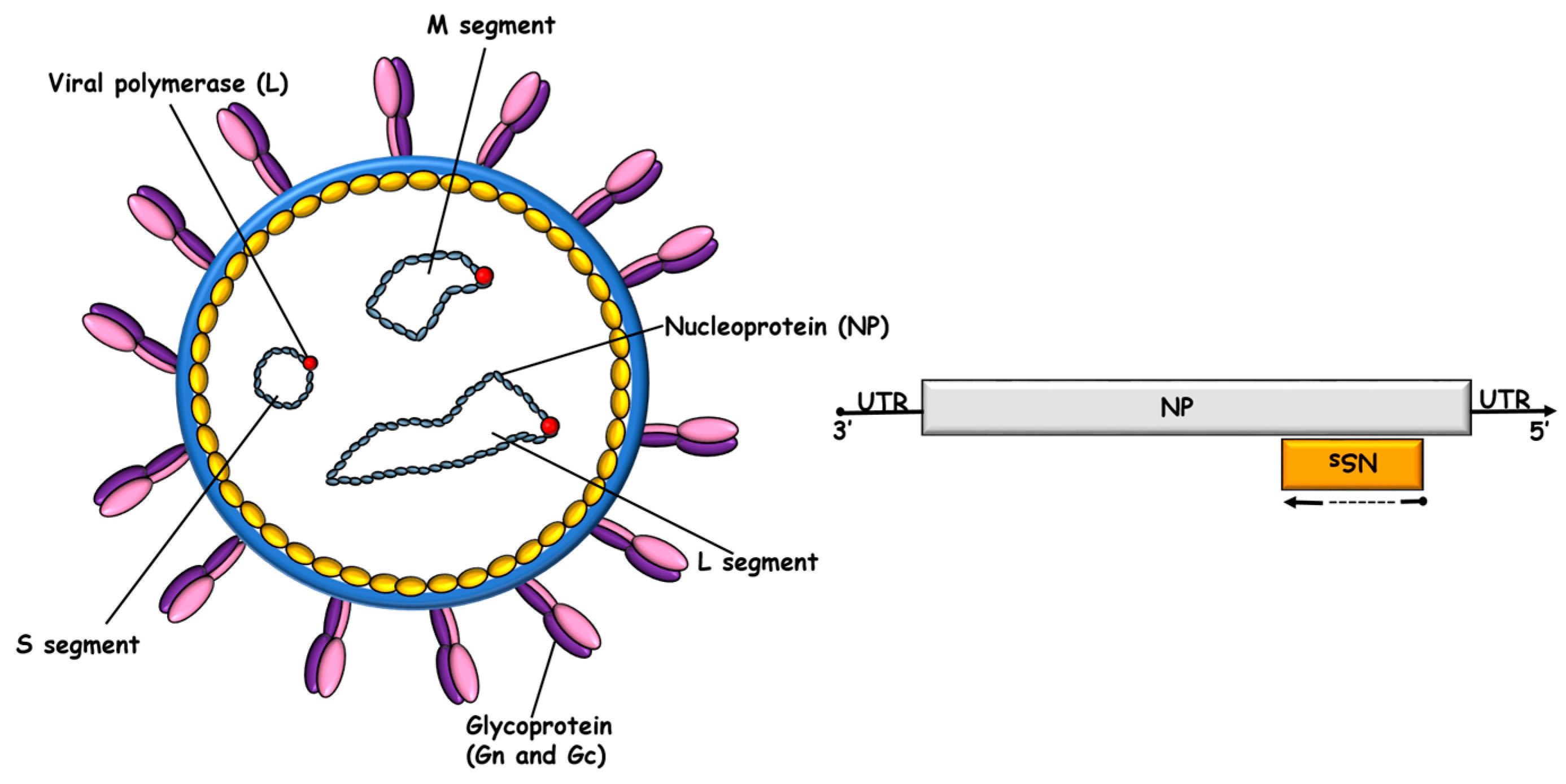
2. CCHFV NP in Viral Biology
3. CCHFV NP in Innate Immunity
4. CCHFV NP in Humoral Immunity
5. CCHFV NP in Cellular Immunity
6. CCHFV NP and Protective Immunological Epitopes
7. CCHFV NP Immunology and Diagnostic Tests
8. CCHFV NP and Vaccines
9. Conclusions
Author Contributions
Funding
Conflicts of Interest
References
- Adams, M.J.; Lefkowitz, E.J.; King, A.M.Q.; Harrach, B.; Harrison, R.L.; Knowles, N.J.; Kropinski, A.M.; Krupovic, M.; Kuhn, J.H.; Mushegian, A.R.; et al. Changes to taxonomy and the International Code of Virus Classification and Nomenclature ratified by the International Committee on Taxonomy of Viruses (2017). Arch. Virol. 2017, 162, 2505–2538. [Google Scholar] [CrossRef]
- Abudurexiti, A.; Adkins, S.; Alioto, D.; Alkhovsky, S.V.; Avsic-Zupanc, T.; Ballinger, M.J.; Bente, D.A.; Beer, M.; Bergeron, E.; Blair, C.D.; et al. Taxonomy of the order Bunyavirales: Update 2019. Arch. Virol. 2019, 164, 1949–1965. [Google Scholar] [CrossRef] [PubMed]
- Alatrash, R.; Herrera, B.B. The Adaptive Immune Response against Bunyavirales. Viruses 2024, 16, 483. [Google Scholar] [CrossRef] [PubMed]
- Zivcec, M.; Scholte, F.E.; Spiropoulou, C.F.; Spengler, J.R.; Bergeron, E. Molecular Insights into Crimean-Congo Hemorrhagic Fever Virus. Viruses 2016, 8, 106. [Google Scholar] [CrossRef] [PubMed]
- Honig, J.E.; Osborne, J.C.; Nichol, S.T. The high genetic variation of viruses of the genus Nairovirus reflects the diversity of their predominant tick hosts. Virology 2004, 318, 10–16. [Google Scholar] [CrossRef] [PubMed]
- Hawman, D.W.; Feldmann, H. Crimean-Congo haemorrhagic fever virus. Nat. Rev. Microbiol. 2023, 21, 463–477. [Google Scholar] [CrossRef]
- Vasmehjani, A.A.; Pouriayevali, M.H.; Shahmahmoodi, S.; Salehi-Vaziri, M. Persistence of IgG and neutralizing antibodies in Crimean-Congo hemorrhagic fever survivors. J. Med. Virol. 2024, 96, e29581. [Google Scholar] [CrossRef]
- Rodriguez, S.E.; Hawman, D.W.; Sorvillo, T.E.; O’Neal, T.J.; Bird, B.H.; Rodriguez, L.L.; Bergeron, E.; Nichol, S.T.; Montgomery, J.M.; Spiropoulou, C.F.; et al. Immunobiology of Crimean-Congo hemorrhagic fever. Antivir. Res. 2022, 199, 105244. [Google Scholar] [CrossRef]
- Celina, S.S.; Cerny, J. Genetic background of adaptation of Crimean-Congo haemorrhagic fever virus to the different tick hosts. PLoS ONE 2024, 19, e0302224. [Google Scholar] [CrossRef]
- Celina, S.S.; Cerny, J.; Samy, A.M. Mapping the potential distribution of the principal vector of Crimean-Congo haemorrhagic fever virus Hyalomma marginatum in the Old World. PLoS Negl. Trop. Dis. 2023, 17, e0010855. [Google Scholar] [CrossRef]
- Hua, B.L.; Scholte, F.E.; Ohlendorf, V.; Kopp, A.; Marklewitz, M.; Drosten, C.; Nichol, S.T.; Spiropoulou, C.; Junglen, S.; Bergeron, E. A single mutation in Crimean-Congo hemorrhagic fever virus discovered in ticks impairs infectivity in human cells. Elife 2020, 9, e50999. [Google Scholar] [CrossRef] [PubMed]
- Bodur, H.; Akinci, E.; Onguru, P.; Uyar, Y.; Basturk, B.; Gozel, M.G.; Kayaaslan, B.U. Evidence of vascular endothelial damage in Crimean-Congo hemorrhagic fever. Int. J. Infect. Dis. 2010, 14, e704–e707. [Google Scholar] [CrossRef] [PubMed]
- Zivcec, M.; Safronetz, D.; Scott, D.; Robertson, S.; Ebihara, H.; Feldmann, H. Lethal Crimean-Congo hemorrhagic fever virus infection in interferon alpha/beta receptor knockout mice is associated with high viral loads, proinflammatory responses, and coagulopathy. J. Infect. Dis. 2013, 207, 1909–1921. [Google Scholar] [CrossRef] [PubMed]
- Frank, M.G.; Weaver, G.; Raabe, V.; State of the Clinical Science Working Group of the National Emerging Pathogens Training; Education Center’s Special Pathogens Research Network. Crimean-Congo Hemorrhagic Fever Virus for Clinicians-Epidemiology, Clinical Manifestations, and Prevention. Emerg. Infect. Dis. 2024, 30, 854–863. [Google Scholar] [CrossRef]
- Tonbak, S.; Aktas, M.; Altay, K.; Azkur, A.K.; Kalkan, A.; Bolat, Y.; Dumanli, N.; Ozdarendeli, A. Crimean-Congo hemorrhagic fever virus: Genetic analysis and tick survey in Turkey. J. Clin. Microbiol. 2006, 44, 4120–4124. [Google Scholar] [CrossRef]
- Negredo, A.; de la Calle-Prieto, F.; Palencia-Herrejon, E.; Mora-Rillo, M.; Astray-Mochales, J.; Sanchez-Seco, M.P.; Bermejo Lopez, E.; Menarguez, J.; Fernandez-Cruz, A.; Sanchez-Artola, B.; et al. Autochthonous Crimean-Congo Hemorrhagic Fever in Spain. N. Engl. J. Med. 2017, 377, 154–161. [Google Scholar] [CrossRef]
- Cuadrado-Matias, R.; Moraga-Fernandez, A.; Peralbo-Moreno, A.; Negredo, A.I.; Sanchez-Seco, M.P.; Ruiz-Fons, F. Crimean-Congo haemorrhagic fever virus in questing non-Hyalomma spp. ticks in Northwest Spain, 2021. Zoonoses Public Health 2024, 71, 578–583. [Google Scholar] [CrossRef]
- World Health Organization. Prioritizing Diseases for Research and Development in Emergency Contexts. 2015. Available online: https://www.who.int/activities/prioritizing-diseases-for-research-and-development-in-emergency-contexts (accessed on 29 July 2024).
- Bente, D.A.; Forrester, N.L.; Watts, D.M.; McAuley, A.J.; Whitehouse, C.A.; Bray, M. Crimean-Congo hemorrhagic fever: History, epidemiology, pathogenesis, clinical syndrome and genetic diversity. Antivir. Res. 2013, 100, 159–189. [Google Scholar] [CrossRef]
- Hawman, D.W.; Feldmann, H. Recent advances in understanding Crimean-Congo hemorrhagic fever virus. F1000Research 2018, 7. [Google Scholar] [CrossRef]
- Papa, A.; Tsergouli, K.; Tsioka, K.; Mirazimi, A. Crimean-Congo Hemorrhagic Fever: Tick-Host-Virus Interactions. Front. Cell Infect. Microbiol. 2017, 7, 213. [Google Scholar] [CrossRef]
- Garrison, A.R.; Smith, D.R.; Golden, J.W. Animal Models for Crimean-Congo Hemorrhagic Fever Human Disease. Viruses 2019, 11, 590. [Google Scholar] [CrossRef]
- Spengler, J.R.; Bergeron, E.; Rollin, P.E. Seroepidemiological Studies of Crimean-Congo Hemorrhagic Fever Virus in Domestic and Wild Animals. PLoS Negl. Trop. Dis. 2016, 10, e0004210. [Google Scholar] [CrossRef] [PubMed]
- Saijo, M.; Moriikawa, S.; Kurane, I. Crimean-Congo hemorrhagic fever. Uirusu 2004, 54, 223–227. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Weber, F.; Mirazimi, A. Interferon and cytokine responses to Crimean Congo hemorrhagic fever virus; an emerging and neglected viral zonoosis. Cytokine Growth Factor. Rev. 2008, 19, 395–404. [Google Scholar] [CrossRef] [PubMed]
- Papa, A. Diagnostic approaches for Crimean-Congo hemorrhagic fever virus. Expert. Rev. Mol. Diagn. 2019, 19, 531–536. [Google Scholar] [CrossRef]
- Dowall, S.D.; Carroll, M.W.; Hewson, R. Development of vaccines against Crimean-Congo haemorrhagic fever virus. Vaccine 2017, 35, 6015–6023. [Google Scholar] [CrossRef]
- Ozdarendeli, A. Crimean-Congo Hemorrhagic Fever Virus: Progress in Vaccine Development. Diagnostics 2023, 13, 2708. [Google Scholar] [CrossRef]
- Tipih, T.; Burt, F.J. Crimean-Congo Hemorrhagic Fever Virus: Advances in Vaccine Development. Biores. Open Access 2020, 9, 137–150. [Google Scholar] [CrossRef]
- Barnwal, B.; Karlberg, H.; Mirazimi, A.; Tan, Y.J. The Non-structural Protein of Crimean-Congo Hemorrhagic Fever Virus Disrupts the Mitochondrial Membrane Potential and Induces Apoptosis. J. Biol. Chem. 2016, 291, 582–592. [Google Scholar] [CrossRef]
- Luo, M.; Terrell, J.R.; McManus, S.A. Nucleocapsid Structure of Negative Strand RNA Virus. Viruses 2020, 12, 835. [Google Scholar] [CrossRef]
- Wang, W.; Liu, X.; Wang, X.; Dong, H.; Ma, C.; Wang, J.; Liu, B.; Mao, Y.; Wang, Y.; Li, T.; et al. Structural and Functional Diversity of Nairovirus-Encoded Nucleoproteins. J. Virol. 2015, 89, 11740–11749. [Google Scholar] [CrossRef] [PubMed]
- Guo, Y.; Wang, W.; Ji, W.; Deng, M.; Sun, Y.; Zhou, H.; Yang, C.; Deng, F.; Wang, H.; Hu, Z.; et al. Crimean-Congo hemorrhagic fever virus nucleoprotein reveals endonuclease activity in bunyaviruses. Proc. Natl. Acad. Sci. USA 2012, 109, 5046–5051. [Google Scholar] [CrossRef] [PubMed]
- Jeeva, S.; Pador, S.; Voss, B.; Ganaie, S.S.; Mir, M.A. Crimean-Congo hemorrhagic fever virus nucleocapsid protein has dual RNA binding modes. PLoS ONE 2017, 12, e0184935. [Google Scholar] [CrossRef] [PubMed]
- Jeeva, S.; Mir, S.; Velasquez, A.; Ragan, J.; Leka, A.; Wu, S.; Sevarany, A.T.; Royster, A.D.; Almeida, N.A.; Chan, F.; et al. Crimean-Congo hemorrhagic fever virus nucleocapsid protein harbors distinct RNA-binding sites in the stalk and head domains. J. Biol. Chem. 2019, 294, 5023–5037. [Google Scholar] [CrossRef] [PubMed]
- Wang, Y.; Dutta, S.; Karlberg, H.; Devignot, S.; Weber, F.; Hao, Q.; Tan, Y.J.; Mirazimi, A.; Kotaka, M. Structure of Crimean-Congo hemorrhagic fever virus nucleoprotein: Superhelical homo-oligomers and the role of caspase-3 cleavage. J. Virol. 2012, 86, 12294–12303. [Google Scholar] [CrossRef] [PubMed]
- Carter, S.D.; Surtees, R.; Walter, C.T.; Ariza, A.; Bergeron, E.; Nichol, S.T.; Hiscox, J.A.; Edwards, T.A.; Barr, J.N. Structure, function, and evolution of the Crimean-Congo hemorrhagic fever virus nucleocapsid protein. J. Virol. 2012, 86, 10914–10923. [Google Scholar] [CrossRef]
- Jeeva, S.; Cheng, E.; Ganaie, S.S.; Mir, M.A. Crimean-Congo Hemorrhagic Fever Virus Nucleocapsid Protein Augments mRNA Translation. J. Virol. 2017, 91, 10–1128. [Google Scholar] [CrossRef]
- Xu, Z.S.; Du, W.T.; Wang, S.Y.; Wang, M.Y.; Yang, Y.N.; Li, Y.H.; Li, Z.Q.; Zhao, L.X.; Yang, Y.; Luo, W.W.; et al. LDLR is an entry receptor for Crimean-Congo hemorrhagic fever virus. Cell Res. 2024, 34, 140–150. [Google Scholar] [CrossRef]
- Monteil, V.M.; Wright, S.C.; Dyczynski, M.; Kellner, M.J.; Appelberg, S.; Platzer, S.W.; Ibrahim, A.; Kwon, H.; Pittarokoilis, I.; Mirandola, M.; et al. Crimean-Congo haemorrhagic fever virus uses LDLR to bind and enter host cells. Nat. Microbiol. 2024, 9, 1499–1512. [Google Scholar] [CrossRef]
- Ritter, M.; Canus, L.; Gautam, A.; Vallet, T.; Zhong, L.; Lalande, A.; Boson, B.; Gandhi, A.; Bodoirat, S.; Burlaud-Gaillard, J.; et al. The low-density lipoprotein receptor and apolipoprotein E associated with CCHFV particles mediate CCHFV entry into cells. Nat. Commun. 2024, 15, 4542. [Google Scholar] [CrossRef]
- Surtees, R.; Dowall, S.D.; Shaw, A.; Armstrong, S.; Hewson, R.; Carroll, M.W.; Mankouri, J.; Edwards, T.A.; Hiscox, J.A.; Barr, J.N. Heat Shock Protein 70 Family Members Interact with Crimean-Congo Hemorrhagic Fever Virus and Hazara Virus Nucleocapsid Proteins and Perform a Functional Role in the Nairovirus Replication Cycle. J. Virol. 2016, 90, 9305–9316. [Google Scholar] [CrossRef] [PubMed]
- Andersson, I.; Simon, M.; Lundkvist, A.; Nilsson, M.; Holmstrom, A.; Elgh, F.; Mirazimi, A. Role of actin filaments in targeting of Crimean Congo hemorrhagic fever virus nucleocapsid protein to perinuclear regions of mammalian cells. J. Med. Virol. 2004, 72, 83–93. [Google Scholar] [CrossRef] [PubMed]
- Macleod, J.M.L.; Marmor, H.; Garcia-Sastre, A.; Frias-Staheli, N. Mapping of the interaction domains of the Crimean-Congo hemorrhagic fever virus nucleocapsid protein. J. Gen. Virol. 2015, 96, 524–537. [Google Scholar] [CrossRef] [PubMed]
- Bergeron, E.; Albarino, C.G.; Khristova, M.L.; Nichol, S.T. Crimean-Congo hemorrhagic fever virus-encoded ovarian tumor protease activity is dispensable for virus RNA polymerase function. J. Virol. 2010, 84, 216–226. [Google Scholar] [CrossRef] [PubMed]
- Hawman, D.W.; Meade-White, K.; Leventhal, S.; Feldmann, F.; Okumura, A.; Smith, B.; Scott, D.; Feldmann, H. Immunocompetent mouse model for Crimean-Congo hemorrhagic fever virus. Elife 2021, 10, e63906. [Google Scholar] [CrossRef]
- Hawman, D.W.; Meade-White, K.; Haddock, E.; Habib, R.; Scott, D.; Thomas, T.; Rosenke, R.; Feldmann, H. Crimean-Congo Hemorrhagic Fever Mouse Model Recapitulating Human Convalescence. J. Virol. 2019, 93, 10–1128. [Google Scholar] [CrossRef]
- Bereczky, S.; Lindegren, G.; Karlberg, H.; Akerstrom, S.; Klingstrom, J.; Mirazimi, A. Crimean-Congo hemorrhagic fever virus infection is lethal for adult type I interferon receptor-knockout mice. J. Gen. Virol. 2010, 91, 1473–1477. [Google Scholar] [CrossRef]
- Bente, D.A.; Alimonti, J.B.; Shieh, W.J.; Camus, G.; Stroher, U.; Zaki, S.; Jones, S.M. Pathogenesis and immune response of Crimean-Congo hemorrhagic fever virus in a STAT-1 knockout mouse model. J. Virol. 2010, 84, 11089–11100. [Google Scholar] [CrossRef]
- Papa, A.; Tsergouli, K.; Caglayik, D.Y.; Bino, S.; Como, N.; Uyar, Y.; Korukluoglu, G. Cytokines as biomarkers of Crimean-Congo hemorrhagic fever. J. Med. Virol. 2016, 88, 21–27. [Google Scholar] [CrossRef]
- Ergonul, O.; Seref, C.; Eren, S.; Celikbas, A.; Baykam, N.; Dokuzoguz, B.; Gonen, M.; Can, F. Cytokine response in crimean-congo hemorrhagic fever virus infection. J. Med. Virol. 2017, 89, 1707–1713. [Google Scholar] [CrossRef]
- Golden, J.W.; Zeng, X.; Cline, C.R.; Smith, J.M.; Daye, S.P.; Carey, B.D.; Blancett, C.D.; Shoemaker, C.J.; Liu, J.; Fitzpatrick, C.J.; et al. The host inflammatory response contributes to disease severity in Crimean-Congo hemorrhagic fever virus infected mice. PLoS Pathog. 2022, 18, e1010485. [Google Scholar] [CrossRef] [PubMed]
- Engin, A.; Arslan, S.; Ozbilum, N.; Bakir, M. Is there any relationship between Toll-like receptor 3 c.1377C/T and -7C/A polymorphisms and susceptibility to Crimean Congo hemorrhagic fever? J. Med. Virol. 2016, 88, 1690–1696. [Google Scholar] [CrossRef]
- Xagorari, A.; Chlichlia, K. Toll-like receptors and viruses: Induction of innate antiviral immune responses. Open Microbiol. J. 2008, 2, 49–59. [Google Scholar] [CrossRef] [PubMed]
- Arslan, S.; Engin, A.; Ozbilum, N.; Bakir, M. Toll-like receptor 7 Gln11Leu, c.4-151A/G, and +1817G/T polymorphisms in Crimean Congo hemorrhagic fever. J. Med. Virol. 2015, 87, 1090–1095. [Google Scholar] [CrossRef] [PubMed]
- Engin, A.; Arslan, S.; Kizildag, S.; Ozturk, H.; Elaldi, N.; Dokmetas, I.; Bakir, M. Toll-like receptor 8 and 9 polymorphisms in Crimean-Congo hemorrhagic fever. Microbes Infect. 2010, 12, 1071–1078. [Google Scholar] [CrossRef] [PubMed]
- Spengler, J.R.; Patel, J.R.; Chakrabarti, A.K.; Zivcec, M.; Garcia-Sastre, A.; Spiropoulou, C.F.; Bergeron, E. RIG-I Mediates an Antiviral Response to Crimean-Congo Hemorrhagic Fever Virus. J. Virol. 2015, 89, 10219–10229. [Google Scholar] [CrossRef]
- Habjan, M.; Andersson, I.; Klingstrom, J.; Schumann, M.; Martin, A.; Zimmermann, P.; Wagner, V.; Pichlmair, A.; Schneider, U.; Muhlberger, E.; et al. Processing of genome 5′ termini as a strategy of negative-strand RNA viruses to avoid RIG-I-dependent interferon induction. PLoS ONE 2008, 3, e2032. [Google Scholar] [CrossRef]
- Andersson, I.; Karlberg, H.; Mousavi-Jazi, M.; Martinez-Sobrido, L.; Weber, F.; Mirazimi, A. Crimean-Congo hemorrhagic fever virus delays activation of the innate immune response. J. Med. Virol. 2008, 80, 1397–1404. [Google Scholar] [CrossRef]
- Fajs, L.; Resman, K.; Avsic-Zupanc, T. Crimean-Congo hemorrhagic fever virus nucleoprotein suppresses IFN-beta-promoter-mediated gene expression. Arch. Virol. 2014, 159, 345–348. [Google Scholar] [CrossRef]
- Scholte, F.E.M.; Zivcec, M.; Dzimianski, J.V.; Deaton, M.K.; Spengler, J.R.; Welch, S.R.; Nichol, S.T.; Pegan, S.D.; Spiropoulou, C.F.; Bergeron, E. Crimean-Congo Hemorrhagic Fever Virus Suppresses Innate Immune Responses via a Ubiquitin and ISG15 Specific Protease. Cell Rep. 2017, 20, 2396–2407. [Google Scholar] [CrossRef]
- Frias-Staheli, N.; Giannakopoulos, N.V.; Kikkert, M.; Taylor, S.L.; Bridgen, A.; Paragas, J.; Richt, J.A.; Rowland, R.R.; Schmaljohn, C.S.; Lenschow, D.J.; et al. Ovarian tumor domain-containing viral proteases evade ubiquitin- and ISG15-dependent innate immune responses. Cell Host Microbe 2007, 2, 404–416. [Google Scholar] [CrossRef] [PubMed]
- Leventhal, S.S.; Wilson, D.; Feldmann, H.; Hawman, D.W. A Look into Bunyavirales Genomes: Functions of Non-Structural (NS) Proteins. Viruses 2021, 13, 314. [Google Scholar] [CrossRef] [PubMed]
- Pavlovic, J.; Schroder, A.; Blank, A.; Pitossi, F.; Staeheli, P. Mx proteins: GTPases involved in the interferon-induced antiviral state. Ciba Found. Symp. 1993, 176, 233–243, discussion 243–237. [Google Scholar] [CrossRef] [PubMed]
- Weber, F.; Haller, O.; Kochs, G. MxA GTPase blocks reporter gene expression of reconstituted Thogoto virus ribonucleoprotein complexes. J. Virol. 2000, 74, 560–563. [Google Scholar] [CrossRef] [PubMed]
- Andersson, I.; Bladh, L.; Mousavi-Jazi, M.; Magnusson, K.E.; Lundkvist, A.; Haller, O.; Mirazimi, A. Human MxA protein inhibits the replication of Crimean-Congo hemorrhagic fever virus. J. Virol. 2004, 78, 4323–4329. [Google Scholar] [CrossRef] [PubMed]
- Karlberg, H.; Tan, Y.J.; Mirazimi, A. Crimean-Congo haemorrhagic fever replication interplays with regulation mechanisms of apoptosis. J. Gen. Virol. 2015, 96, 538–546. [Google Scholar] [CrossRef]
- Muzammil, K.; Rayyani, S.; Abbas Sahib, A.; Gholizadeh, O.; Naji Sameer, H.; Jwad Kazem, T.; Badran Mohammed, H.; Ghafouri Kalajahi, H.; Zainul, R.; Yasamineh, S. Recent Advances in Crimean-Congo Hemorrhagic Fever Virus Detection, Treatment, and Vaccination: Overview of Current Status and Challenges. Biol. Proced. Online 2024, 26, 20. [Google Scholar] [CrossRef]
- Burt, F.J.; Leman, P.A.; Abbott, J.C.; Swanepoel, R. Serodiagnosis of Crimean-Congo haemorrhagic fever. Epidemiol. Infect. 1994, 113, 551–562. [Google Scholar] [CrossRef]
- Shepherd, A.J.; Swanepoel, R.; Leman, P.A. Antibody response in Crimean-Congo hemorrhagic fever. Rev. Infect. Dis. 1989, 11 (Suppl. S4), S801–S806. [Google Scholar] [CrossRef]
- Epstein, S.L.; Kong, W.P.; Misplon, J.A.; Lo, C.Y.; Tumpey, T.M.; Xu, L.; Nabel, G.J. Protection against multiple influenza A subtypes by vaccination with highly conserved nucleoprotein. Vaccine 2005, 23, 5404–5410. [Google Scholar] [CrossRef]
- Wilson, J.A.; Hart, M.K. Protection from Ebola virus mediated by cytotoxic T lymphocytes specific for the viral nucleoprotein. J. Virol. 2001, 75, 2660–2664. [Google Scholar] [CrossRef] [PubMed]
- Clegg, J.C.; Lloyd, G. Vaccinia recombinant expressing Lassa-virus internal nucleocapsid protein protects guineapigs against Lassa fever. Lancet 1987, 2, 186–188. [Google Scholar] [CrossRef] [PubMed]
- Boshra, H.; Lorenzo, G.; Rodriguez, F.; Brun, A. A DNA vaccine encoding ubiquitinated Rift Valley fever virus nucleoprotein provides consistent immunity and protects IFNAR(-/-) mice upon lethal virus challenge. Vaccine 2011, 29, 4469–4475. [Google Scholar] [CrossRef] [PubMed]
- Gott, P.; Zoller, L.; Darai, G.; Bautz, E.K. A major antigenic domain of hantaviruses is located on the aminoproximal site of the viral nucleocapsid protein. Virus Genes 1997, 14, 31–40. [Google Scholar] [CrossRef] [PubMed]
- Saijo, M.; Tang, Q.; Shimayi, B.; Han, L.; Zhang, Y.; Asiguma, M.; Tianshu, D.; Maeda, A.; Kurane, I.; Morikawa, S. Recombinant nucleoprotein-based serological diagnosis of Crimean-Congo hemorrhagic fever virus infections. J. Med. Virol. 2005, 75, 295–299. [Google Scholar] [CrossRef]
- Saijo, M.; Qing, T.; Niikura, M.; Maeda, A.; Ikegami, T.; Prehaud, C.; Kurane, I.; Morikawa, S. Recombinant nucleoprotein-based enzyme-linked immunosorbent assay for detection of immunoglobulin G antibodies to Crimean-Congo hemorrhagic fever virus. J. Clin. Microbiol. 2002, 40, 1587–1591. [Google Scholar] [CrossRef]
- Hawman, D.W.; Ahlen, G.; Appelberg, K.S.; Meade-White, K.; Hanley, P.W.; Scott, D.; Monteil, V.; Devignot, S.; Okumura, A.; Weber, F.; et al. A DNA-based vaccine protects against Crimean-Congo haemorrhagic fever virus disease in a Cynomolgus macaque model. Nat. Microbiol. 2021, 6, 187–195. [Google Scholar] [CrossRef]
- Karaaslan, E.; Cetin, N.S.; Kalkan-Yazici, M.; Hasanoglu, S.; Karakecili, F.; Ozdarendeli, A.; Kalkan, A.; Kilic, A.O.; Doymaz, M.Z. Immune responses in multiple hosts to Nucleocapsid Protein (NP) of Crimean-Congo Hemorrhagic Fever Virus (CCHFV). PLoS Negl. Trop. Dis. 2021, 15, e0009973. [Google Scholar] [CrossRef]
- Kalkan-Yazici, M.; Karaaslan, E.; Cetin, N.S.; Hasanoglu, S.; Guney, F.; Zeybek, U.; Doymaz, M.Z. Cross-Reactive anti-Nucleocapsid Protein Immunity against Crimean-Congo Hemorrhagic Fever Virus and Hazara Virus in Multiple Species. J. Virol. 2021, 95, 10–1128. [Google Scholar] [CrossRef]
- Zivcec, M.; Guerrero, L.I.W.; Albarino, C.G.; Bergeron, E.; Nichol, S.T.; Spiropoulou, C.F. Identification of broadly neutralizing monoclonal antibodies against Crimean-Congo hemorrhagic fever virus. Antivir. Res. 2017, 146, 112–120. [Google Scholar] [CrossRef]
- Bertolotti-Ciarlet, A.; Smith, J.; Strecker, K.; Paragas, J.; Altamura, L.A.; McFalls, J.M.; Frias-Staheli, N.; Garcia-Sastre, A.; Schmaljohn, C.S.; Doms, R.W. Cellular localization and antigenic characterization of crimean-congo hemorrhagic fever virus glycoproteins. J. Virol. 2005, 79, 6152–6161. [Google Scholar] [CrossRef] [PubMed]
- Pierre, C.N.; Adams, L.E.; Higgins, J.S.; Anasti, K.; Goodman, D.; Mielke, D.; Stanfield-Oakley, S.; Powers, J.M.; Li, D.; Rountree, W.; et al. Non-neutralizing SARS-CoV-2 N-terminal domain antibodies protect mice against severe disease using Fc-mediated effector functions. PLoS Pathog. 2024, 20, e1011569. [Google Scholar] [CrossRef] [PubMed]
- Scholte, F.E.M.; Karaaslan, E.; O’Neal, T.J.; Sorvillo, T.E.; Genzer, S.C.; Welch, S.R.; Coleman-McCray, J.D.; Spengler, J.R.; Kainulainen, M.H.; Montgomery, J.M.; et al. Vaccination with the Crimean-Congo hemorrhagic fever virus viral replicon vaccine induces NP-based T-cell activation and antibodies possessing Fc-mediated effector functions. Front. Cell Infect. Microbiol. 2023, 13, 1233148. [Google Scholar] [CrossRef] [PubMed]
- Keshtkar-Jahromi, M.; Kuhn, J.H.; Christova, I.; Bradfute, S.B.; Jahrling, P.B.; Bavari, S. Crimean-Congo hemorrhagic fever: Current and future prospects of vaccines and therapies. Antivir. Res. 2011, 90, 85–92. [Google Scholar] [CrossRef]
- Golden, J.W.; Shoemaker, C.J.; Lindquist, M.E.; Zeng, X.; Daye, S.P.; Williams, J.A.; Liu, J.; Coffin, K.M.; Olschner, S.; Flusin, O.; et al. GP38-targeting monoclonal antibodies protect adult mice against lethal Crimean-Congo hemorrhagic fever virus infection. Sci. Adv. 2019, 5, eaaw9535. [Google Scholar] [CrossRef]
- Garrison, A.R.; Moresco, V.; Zeng, X.; Cline, C.R.; Ward, M.D.; Ricks, K.M.; Olschner, S.P.; Cazares, L.H.; Karaaslan, E.; Fitzpatrick, C.J.; et al. Nucleocapsid protein-specific monoclonal antibodies protect mice against Crimean-Congo hemorrhagic fever virus. Nat. Commun. 2024, 15, 1722. [Google Scholar] [CrossRef]
- Rangunwala, A.; Samudzi, R.R.; Burt, F.J. Detection of IgG antibody against Crimean-Congo haemorrhagic fever virus using ELISA with recombinant nucleoprotein antigens from genetically diverse strains. Epidemiol. Infect. 2014, 142, 2147–2154. [Google Scholar] [CrossRef]
- Kortekaas, J.; Vloet, R.P.; McAuley, A.J.; Shen, X.; Bosch, B.J.; de Vries, L.; Moormann, R.J.; Bente, D.A. Crimean-Congo Hemorrhagic Fever Virus Subunit Vaccines Induce High Levels of Neutralizing Antibodies But No Protection in STAT1 Knockout Mice. Vector Borne Zoonotic Dis. 2015, 15, 759–764. [Google Scholar] [CrossRef]
- Dowall, S.D.; Graham, V.A.; Rayner, E.; Hunter, L.; Watson, R.; Taylor, I.; Rule, A.; Carroll, M.W.; Hewson, R. Protective effects of a Modified Vaccinia Ankara-based vaccine candidate against Crimean-Congo Haemorrhagic Fever virus require both cellular and humoral responses. PLoS ONE 2016, 11, e0156637. [Google Scholar] [CrossRef]
- Dowall, S.D.; Buttigieg, K.R.; Findlay-Wilson, S.J.; Rayner, E.; Pearson, G.; Miloszewska, A.; Graham, V.A.; Carroll, M.W.; Hewson, R. A Crimean-Congo hemorrhagic fever (CCHF) viral vaccine expressing nucleoprotein is immunogenic but fails to confer protection against lethal disease. Hum. Vaccines Immunother. 2016, 12, 519–527. [Google Scholar] [CrossRef]
- Hinkula, J.; Devignot, S.; Akerstrom, S.; Karlberg, H.; Wattrang, E.; Bereczky, S.; Mousavi-Jazi, M.; Risinger, C.; Lindegren, G.; Vernersson, C.; et al. Immunization with DNA Plasmids Coding for Crimean-Congo Hemorrhagic Fever Virus Capsid and Envelope Proteins and/or Virus-Like Particles Induces Protection and Survival in Challenged Mice. J. Virol. 2017, 91, 10–1128. [Google Scholar] [CrossRef] [PubMed]
- Hawman, D.W.; Meade-White, K.; Leventhal, S.; Carmody, A.; Haddock, E.; Hasenkrug, K.; Feldmann, H. T-Cells and Interferon Gamma Are Necessary for Survival Following Crimean-Congo Hemorrhagic Fever Virus Infection in Mice. Microorganisms 2021, 9, 279. [Google Scholar] [CrossRef] [PubMed]
- Santak, M.; Matic, Z. The Role of Nucleoprotein in Immunity to Human Negative-Stranded RNA Viruses-Not Just Another Brick in the Viral Nucleocapsid. Viruses 2022, 14, 521. [Google Scholar] [CrossRef]
- Van Epps, H.L.; Terajima, M.; Mustonen, J.; Arstila, T.P.; Corey, E.A.; Vaheri, A.; Ennis, F.A. Long-lived memory T lymphocyte responses after hantavirus infection. J. Exp. Med. 2002, 196, 579–588. [Google Scholar] [CrossRef] [PubMed]
- Goedhals, D.; Paweska, J.T.; Burt, F.J. Long-lived CD8+ T cell responses following Crimean-Congo haemorrhagic fever virus infection. PLoS Negl. Trop. Dis. 2017, 11, e0006149. [Google Scholar] [CrossRef] [PubMed]
- Kalkan-Yazıcı, M.; Karaaslan, E.; Çetin, N.S.; Doymaz, M.Z. Cellular Immunity to Nucleoproteins (NP) of Crimean-Congo Hemorrhagic Fever Virus (CCHFV) and Hazara Virus (HAZV). Med. Microbiol. Immunulogy 2024, Submitted. [Google Scholar]
- Wei, P.F.; Luo, Y.J.; Li, T.X.; Wang, H.L.; Hu, Z.H.; Zhang, F.C.; Zhang, Y.J.; Deng, F.; Sun, S.R. Serial expression of the truncated fragments of the nucleocapsid protein of CCHFV and identification of the epitope region. Virol. Sin. 2010, 25, 45–51. [Google Scholar] [CrossRef]
- Moming, A.; Tuoken, D.; Yue, X.; Xu, W.; Guo, R.; Liu, D.; Li, Y.; Hu, Z.; Deng, F.; Zhang, Y.; et al. Mapping of B-cell epitopes on the N-terminal and C-terminal segment of nucleocapsid protein from Crimean-Congo hemorrhagic fever virus. PLoS ONE 2018, 13, e0204264. [Google Scholar] [CrossRef]
- Lombe, B.P.; Saito, T.; Miyamoto, H.; Mori-Kajihara, A.; Kajihara, M.; Saijo, M.; Masumu, J.; Hattori, T.; Igarashi, M.; Takada, A. Mapping of Antibody Epitopes on the Crimean-Congo Hemorrhagic Fever Virus Nucleoprotein. Viruses 2022, 14, 544. [Google Scholar] [CrossRef]
- Marriott, A.C.; Polyzoni, T.; Antoniadis, A.; Nuttall, P.A. Detection of human antibodies to Crimean-Congo haemorrhagic fever virus using expressed viral nucleocapsid protein. J. Gen. Virol. 1994, 75 Pt 9, 2157–2161. [Google Scholar] [CrossRef]
- Srinivasan, P.; Kumar, S.P.; Karthikeyan, M.; Jeyakanthan, J.; Jasrai, Y.T.; Pandya, H.A.; Rawal, R.M.; Patel, S.K. Epitope-based immunoinformatics and molecular docking studies of nucleocapsid protein and ovarian tumor domain of crimean-congo hemorrhagic Fever virus. Front. Genet. 2011, 2, 72. [Google Scholar] [CrossRef] [PubMed]
- Burt, F.J.; Samudzi, R.R.; Randall, C.; Pieters, D.; Vermeulen, J.; Knox, C.M. Human defined antigenic region on the nucleoprotein of Crimean-Congo hemorrhagic fever virus identified using truncated proteins and a bioinformatics approach. J. Virol. Methods 2013, 193, 706–712. [Google Scholar] [CrossRef]
- Raabe, V.N. Diagnostic Testing for Crimean-Congo Hemorrhagic Fever. J. Clin. Microbiol. 2020, 58, 10–1128. [Google Scholar] [CrossRef] [PubMed]
- Saijo, M.; Tang, Q.; Shimayi, B.; Han, L.; Zhang, Y.; Asiguma, M.; Tianshu, D.; Maeda, A.; Kurane, I.; Morikawa, S. Antigen-capture enzyme-linked immunosorbent assay for the diagnosis of crimean-congo hemorrhagic fever using a novel monoclonal antibody. J. Med. Virol. 2005, 77, 83–88. [Google Scholar] [CrossRef] [PubMed]
- Swanepoel, R.; Gill, D.E.; Shepherd, A.J.; Leman, P.A.; Mynhardt, J.H.; Harvey, S. The clinical pathology of Crimean-Congo hemorrhagic fever. Rev. Infect. Dis. 1989, 11 (Suppl. S4), S794–S800. [Google Scholar] [CrossRef] [PubMed]
- Emmerich, P.; Mika, A.; von Possel, R.; Rackow, A.; Liu, Y.; Schmitz, H.; Gunther, S.; Sherifi, K.; Halili, B.; Jakupi, X.; et al. Sensitive and specific detection of Crimean-Congo Hemorrhagic Fever Virus (CCHFV)-Specific IgM and IgG antibodies in human sera using recombinant CCHFV nucleoprotein as antigen in mu-capture and IgG immune complex (IC) ELISA tests. PLoS Negl. Trop. Dis. 2018, 12, e0006366. [Google Scholar] [CrossRef]
- Belij-Rammerstorfer, S.; Limon, G.; Maze, E.A.; Hannant, K.; Hughes, E.; Tchakarova, S.R.; Alexandrov, T.; Mmbaga, B.T.; Willett, B.; Booth, G.; et al. Development of anti-Crimean-Congo hemorrhagic fever virus Gc and NP-specific ELISA for detection of antibodies in domestic animal sera. Front. Vet. Sci. 2022, 9, 913046. [Google Scholar] [CrossRef]
- Sas, M.A.; Comtet, L.; Donnet, F.; Mertens, M.; Vatansever, Z.; Tordo, N.; Pourquier, P.; Groschup, M.H. A novel double-antigen sandwich ELISA for the species-independent detection of Crimean-Congo hemorrhagic fever virus-specific antibodies. Antivir. Res. 2018, 151, 24–26. [Google Scholar] [CrossRef]
- Samudzi, R.R.; Leman, P.A.; Paweska, J.T.; Swanepoel, R.; Burt, F.J. Bacterial expression of Crimean-Congo hemorrhagic fever virus nucleoprotein and its evaluation as a diagnostic reagent in an indirect ELISA. J. Virol. Methods 2012, 179, 70–76. [Google Scholar] [CrossRef]
- Shrivastava, N.; Shrivastava, A.; Ninawe, S.M.; Sharma, S.; Kumar, J.S.; Alam, S.I.; Kanani, A.; Sharma, S.K.; Dash, P.K. Development of Multispecies Recombinant Nucleoprotein-Based Indirect ELISA for High-Throughput Screening of Crimean-Congo Hemorrhagic Fever Virus-Specific Antibodies. Front. Microbiol. 2019, 10, 1822. [Google Scholar] [CrossRef]
- Atkinson, R.; Burt, F.; Rybicki, E.P.; Meyers, A.E. Plant-produced Crimean-Congo haemorrhagic fever virus nucleoprotein for use in indirect ELISA. J. Virol. Methods 2016, 236, 170–177. [Google Scholar] [CrossRef] [PubMed]
- Ma, B.; Hang, C.; Zhao, Y.; Wang, S.; Xie, Y. Use of a novel baculovirus vector to express nucleoprotein gene of Crimean-Congo hemorrhagic fever virus in both insect and mammalian cells. Zhonghua Shi Yan He Lin Chuang Bing Du Xue Za Zhi 2002, 16, 249–252. [Google Scholar] [PubMed]
- Gulce-Iz, S.; Elaldi, N.; Can, H.; Sahar, E.A.; Karakavuk, M.; Gul, A.; Kumoglu, G.O.; Doskaya, A.D.; Guruz, A.Y.; Ozdarendeli, A.; et al. Development of a novel recombinant ELISA for the detection of Crimean-Congo hemorrhagic fever virus IgG antibodies. Sci. Rep. 2021, 11, 5936. [Google Scholar] [CrossRef] [PubMed]
- Hoste, A.C.R.; Djadjovski, I.; Jimenez-Clavero, M.A.; Rueda, P.; Barr, J.N.; Sastre, P. Multiplex Assay for Simultaneous Detection of Antibodies against Crimean-Congo Hemorrhagic Fever Virus Nucleocapsid Protein and Glycoproteins in Ruminants. Microbiol. Spectr. 2023, 11, e0260022. [Google Scholar] [CrossRef] [PubMed]
- Lombe, B.P.; Miyamoto, H.; Saito, T.; Yoshida, R.; Manzoor, R.; Kajihara, M.; Shimojima, M.; Fukushi, S.; Morikawa, S.; Yoshikawa, T.; et al. Purification of Crimean-Congo hemorrhagic fever virus nucleoprotein and its utility for serological diagnosis. Sci. Rep. 2021, 11, 2324. [Google Scholar] [CrossRef]
- Cosgun, Y.; Aydemir, A.; Hedef, H.; Oz Kamiloglu, A.; Klemens, O.; Lattwein, E.; Klemens, J.M.; Saschenbrecker, S.; Steinhagen, K.; Korukluoglu, G. Evaluation of Nucleoprotein-Based Enzyme-Linked Immunosorbent Assay for Serodiagnosis of Acute Crimean-Congo Hemorrhagic Fever Virus Infections in a Turkish Population. Vector Borne Zoonotic Dis. 2023, 23, 44–53. [Google Scholar] [CrossRef]
- Alvarez-Rodriguez, B.; Tiede, C.; Hoste, A.C.R.; Surtees, R.A.; Trinh, C.H.; Slack, G.S.; Chamberlain, J.; Hewson, R.; Fresco, A.; Sastre, P.; et al. Characterization and applications of a Crimean-Congo hemorrhagic fever virus nucleoprotein-specific Affimer: Inhibitory effects in viral replication and development of colorimetric diagnostic tests. PLoS Negl. Trop. Dis. 2020, 14, e0008364. [Google Scholar] [CrossRef]
- World Health Organization. WHO Model Lists of Essential Medicines. 2007. Available online: https://www.who.int/groups/expert-committee-on-selection-and-use-of-essential-medicines/essential-medicines-lists (accessed on 29 July 2024).
- Hawman, D.W.; Haddock, E.; Meade-White, K.; Williamson, B.; Hanley, P.W.; Rosenke, K.; Komeno, T.; Furuta, Y.; Gowen, B.B.; Feldmann, H. Favipiravir (T-705) but not ribavirin is effective against two distinct strains of Crimean-Congo hemorrhagic fever virus in mice. Antivir. Res. 2018, 157, 18–26. [Google Scholar] [CrossRef]
- Furuta, Y.; Gowen, B.B.; Takahashi, K.; Shiraki, K.; Smee, D.F.; Barnard, D.L. Favipiravir (T-705), a novel viral RNA polymerase inhibitor. Antivir. Res. 2013, 100, 446–454. [Google Scholar] [CrossRef]
- Tipih, T.; Meade-White, K.; Rao, D.; Bushmaker, T.; Lewis, M.; Shaia, C.; Feldmann, H.; Hawman, D.W. Favipiravir and Ribavirin protect immunocompetent mice from lethal CCHFV infection. Antivir. Res. 2023, 218, 105703. [Google Scholar] [CrossRef]
- Dulger, A.C.; Yakarisik, M.; Uzun, Y.E.; Sahin, A.M. Treatment of Crimean-Congo Haemorrhagic Fever by Favipiravir in a Patient with Novel Coronavirus Co-Infection. Eur. J. Case Rep. Intern. Med. 2020, 7, 002042. [Google Scholar] [CrossRef] [PubMed]
- Buyuktuna, S.A.; Hasbek, M.; Oksuz, C.; Baysal, C.; Oz, M.; Elaldi, N.; Bakir, M. [COVID-19 Co-infection in a patient with Crimean Congo Hemorrhagic Fever: A Case Report]. Mikrobiyol. Bul. 2021, 55, 445–451. [Google Scholar] [CrossRef] [PubMed]
- Liu, K.; Li, L.; Liu, Y.; Wang, X.; Liu, J.; Li, J.; Deng, F.; Zhang, R.; Zhou, Y.; Hu, Z.; et al. Discovery of baloxavir sodium as a novel anti-CCHFV inhibitor: Biological evaluation of in vitro and in vivo. Antivir. Res. 2024, 227, 105890. [Google Scholar] [CrossRef] [PubMed]
- Scholte, F.E.M.; Hua, B.L.; Spengler, J.R.; Dzimianski, J.V.; Coleman-McCray, J.D.; Welch, S.R.; McMullan, L.K.; Nichol, S.T.; Pegan, S.D.; Spiropoulou, C.F.; et al. Stable Occupancy of the Crimean-Congo Hemorrhagic Fever Virus-Encoded Deubiquitinase Blocks Viral Infection. MBio 2019, 10, 10–1128. [Google Scholar] [CrossRef] [PubMed]
- Scholte, F.E.M.; Spengler, J.R.; Welch, S.R.; Harmon, J.R.; Coleman-McCray, J.D.; Davies, K.A.; Pegan, S.D.; Montgomery, J.M.; Spiropoulou, C.F.; Bergeron, E. Evaluation of two inoculation routes of an adenovirus-mediated viral protein inhibitor in a Crimean-Congo hemorrhagic fever mouse model. Virus Res. 2024, 345, 199398. [Google Scholar] [CrossRef] [PubMed]
- World Health Organization. Introduction to Crimean-Congo Haemorrhaigc Fever 2019. 2019. Available online: https://www.who.int/publications/i/item/introduction-to-crimean-congo-haemorrhaigc-fever (accessed on 29 July 2024).
- Tahir Ul Qamar, M.; Ismail, S.; Ahmad, S.; Mirza, M.U.; Abbasi, S.W.; Ashfaq, U.A.; Chen, L.L. Development of a Novel Multi-Epitope Vaccine Against Crimean-Congo Hemorrhagic Fever Virus: An Integrated Reverse Vaccinology, Vaccine Informatics and Biophysics Approach. Front. Immunol. 2021, 12, 669812. [Google Scholar] [CrossRef] [PubMed]
- Alam, R.; Samad, A.; Ahammad, F.; Nur, S.M.; Alsaiari, A.A.; Imon, R.R.; Talukder, M.E.K.; Nain, Z.; Rahman, M.M.; Mohammad, F.; et al. In silico formulation of a next-generation multiepitope vaccine for use as a prophylactic candidate against Crimean-Congo hemorrhagic fever. BMC Med. 2023, 21, 36. [Google Scholar] [CrossRef]
- Mousavi-Jazi, M.; Karlberg, H.; Papa, A.; Christova, I.; Mirazimi, A. Healthy individuals’ immune response to the Bulgarian Crimean-Congo hemorrhagic fever virus vaccine. Vaccine 2012, 30, 6225–6229. [Google Scholar] [CrossRef]
- Canakoglu, N.; Berber, E.; Tonbak, S.; Ertek, M.; Sozdutmaz, I.; Aktas, M.; Kalkan, A.; Ozdarendeli, A. Immunization of knock-out alpha/beta interferon receptor mice against high lethal dose of Crimean-Congo hemorrhagic fever virus with a cell culture based vaccine. PLoS Negl. Trop. Dis. 2015, 9, e0003579. [Google Scholar] [CrossRef]
- Pavel, S.T.I.; Yetiskin, H.; Kalkan, A.; Ozdarendeli, A. Evaluation of the cell culture based and the mouse brain derived inactivated vaccines against Crimean-Congo hemorrhagic fever virus in transiently immune-suppressed (IS) mouse model. PLoS Negl. Trop. Dis. 2020, 14, e0008834. [Google Scholar] [CrossRef]
- Zhang, G.; Wang, P.; Jiang, L.; Wang, S.; Zhang, S.; Li, Y. Evaluation of the immunogenicity of vaccine candidates developed using a baculovirus surface display system for Crimean-Congo hemorrhagic fever virus in mice. Front. Microbiol. 2023, 14, 1107874. [Google Scholar] [CrossRef] [PubMed]
- Zhang, G.; Wang, P.; Jiang, L.; Kong, Y.; Wang, S.; Li, Y.; Zhang, S. Evaluation of the immunogenicity of a Crimean-Congo hemorrhagic fever virus vaccine candidate in mice developed based on a baculovirus Zera nanoparticle delivery system. Front. Vet. Sci. 2023, 10, 1126785. [Google Scholar] [CrossRef] [PubMed]
- Hu, Y.L.; Zhang, L.Q.; Liu, X.Q.; Ye, W.; Zhao, Y.X.; Zhang, L.; Qiang, Z.X.; Zhang, L.X.; Lei, Y.F.; Jiang, D.B.; et al. Construction and evaluation of DNA vaccine encoding Crimean Congo hemorrhagic fever virus nucleocapsid protein, glycoprotein N-terminal and C-terminal fused with LAMP1. Front. Cell Infect. Microbiol. 2023, 13, 1121163. [Google Scholar] [CrossRef] [PubMed]
- Aligholipour Farzani, T.; Hanifehnezhad, A.; Foldes, K.; Ergunay, K.; Yilmaz, E.; Hashim Mohamed Ali, H.; Ozkul, A. Co-Delivery Effect of CD24 on the Immunogenicity and Lethal Challenge Protection of a DNA Vector Expressing Nucleocapsid Protein of Crimean Congo Hemorrhagic Fever Virus. Viruses 2019, 11, 75. [Google Scholar] [CrossRef]
- Hawman, D.W.; Meade-White, K.; Leventhal, S.; Appelberg, S.; Ahlen, G.; Nikouyan, N.; Clancy, C.; Smith, B.; Hanley, P.; Lovaglio, J.; et al. Accelerated DNA vaccine regimen provides protection against Crimean-Congo hemorrhagic fever virus challenge in a macaque model. Mol. Ther. 2023, 31, 387–397. [Google Scholar] [CrossRef] [PubMed]
- Scholte, F.E.M.; Spengler, J.R.; Welch, S.R.; Harmon, J.R.; Coleman-McCray, J.D.; Freitas, B.T.; Kainulainen, M.H.; Pegan, S.D.; Nichol, S.T.; Bergeron, E.; et al. Single-dose replicon particle vaccine provides complete protection against Crimean-Congo hemorrhagic fever virus in mice. Emerg. Microbes Infect. 2019, 8, 575–578. [Google Scholar] [CrossRef]
- Spengler, J.R.; Welch, S.R.; Scholte, F.E.M.; Coleman-McCray, J.D.; Harmon, J.R.; Nichol, S.T.; Bergeron, E.; Spiropoulou, C.F. Heterologous protection against Crimean-Congo hemorrhagic fever in mice after a single dose of replicon particle vaccine. Antivir. Res. 2019, 170, 104573. [Google Scholar] [CrossRef]
- Spengler, J.R.; Welch, S.R.; Scholte, F.E.M.; Rodriguez, S.E.; Harmon, J.R.; Coleman-McCray, J.D.; Nichol, S.T.; Montgomery, J.M.; Bergeron, E.; Spiropoulou, C.F. Viral replicon particles protect IFNAR-/- mice against lethal Crimean-Congo hemorrhagic fever virus challenge three days after vaccination. Antivir. Res. 2021, 191, 105090. [Google Scholar] [CrossRef]
- Sorvillo, T.E.; Karaaslan, E.; Scholte, F.E.M.; Welch, S.R.; Coleman-McCray, J.D.; Genzer, S.C.; Ritter, J.M.; Hayes, H.M.; Jain, S.; Pegan, S.D.; et al. Replicon particle vaccination induces non-neutralizing anti-nucleoprotein antibody-mediated control of Crimean-Congo hemorrhagic fever virus. NPJ Vaccines 2024, 9, 88. [Google Scholar] [CrossRef]
- Zivcec, M.; Safronetz, D.; Scott, D.P.; Robertson, S.; Feldmann, H. Nucleocapsid protein-based vaccine provides protection in mice against lethal Crimean-Congo hemorrhagic fever virus challenge. PLoS Negl. Trop. Dis. 2018, 12, e0006628. [Google Scholar] [CrossRef]
- Aligholipour Farzani, T.; Foldes, K.; Hanifehnezhad, A.; Yener Ilce, B.; Bilge Dagalp, S.; Amirzadeh Khiabani, N.; Ergunay, K.; Alkan, F.; Karaoglu, T.; Bodur, H.; et al. Bovine Herpesvirus Type 4 (BoHV-4) Vector Delivering Nucleocapsid Protein of Crimean-Congo Hemorrhagic Fever Virus Induces Comparable Protective Immunity against Lethal Challenge in IFNα/β/γR−/− Mice Models. Viruses 2019, 11, 237. [Google Scholar] [CrossRef] [PubMed]
- Tipih, T.; Heise, M.; Burt, F.J. Immunogenicity of a DNA-Based Sindbis Replicon Expressing Crimean-Congo Hemorrhagic Fever Virus Nucleoprotein. Vaccines 2021, 9, 1491. [Google Scholar] [CrossRef] [PubMed]
- Leventhal, S.S.; Meade-White, K.; Rao, D.; Haddock, E.; Leung, J.; Scott, D.; Archer, J.; Randall, S.; Erasmus, J.H.; Feldmann, H.; et al. Replicating RNA vaccination elicits an unexpected immune response that efficiently protects mice against lethal Crimean-Congo hemorrhagic fever virus challenge. EBioMedicine. 2022, 82, 104188. [Google Scholar] [CrossRef] [PubMed]
- Leventhal, S.S.; Meade-White, K.; Shaia, C.; Tipih, T.; Lewis, M.; Mihalakakos, E.A.; Hinkley, T.; Khandhar, A.P.; Erasmus, J.H.; Feldmann, H.; et al. Single dose, dual antigen RNA vaccines protect against lethal Crimean-Congo haemorrhagic fever virus infection in mice. EBioMedicine 2024, 101, 105017. [Google Scholar] [CrossRef] [PubMed]
- Hawman, D.W.; Leventhal, S.S.; Meade-White, K.; Khandhar, A.; Murray, J.; Lovaglio, J.; Shaia, C.; Saturday, G.; Hinkley, T.; Erasmus, J.; et al. A replicating RNA vaccine confers protection in a rhesus macaque model of Crimean-Congo hemorrhagic fever. NPJ Vaccines 2024, 9, 86. [Google Scholar] [CrossRef]
- Aligholipour Farzani, T.; Foldes, K.; Ergunay, K.; Gurdal, H.; Bastug, A.; Ozkul, A. Immunological Analysis of a CCHFV mRNA Vaccine Candidate in Mouse Models. Vaccines 2019, 7, 115. [Google Scholar] [CrossRef]
- Appelberg, S.; John, L.; Pardi, N.; Vegvari, A.; Bereczky, S.; Ahlen, G.; Monteil, V.; Abdurahman, S.; Mikaeloff, F.; Beattie, M.; et al. Nucleoside-Modified mRNA Vaccines Protect IFNAR-/- Mice against Crimean-Congo Hemorrhagic Fever Virus Infection. J. Virol. 2022, 96, e0156821. [Google Scholar] [CrossRef]
- Keskin, S.; Sak, R.; Bahadorı, F.; Doymaz, M.Z. Immunological Characterization of PLGA Encapsulated mRNA Expressing Crimean-Congo Haemorrhagic Fever Virus (CCHFV) Nucleocapsid Protein (NP) [Oral Presentation]. In Proceedings of the 17th World Immune Regulation Meeting, Zürich, Switzerland, 6 July 2023. [Google Scholar]

| Strain Name | Types of Antigen | Animal Model | Vaccination Dose and Regime | Antibody Response | T Cell Response | Challenge | Efficacy, % Survival | Ref. | |
|---|---|---|---|---|---|---|---|---|---|
| Inactivated vaccines | Bulgarian V42/81 strain | CCHFV whole antigen Suckling mouse brain-derived | NE | Single or four dose | YES | YES | NE | NE | Mousavi-Jazi et al. (2012) [131] |
| Turkey-Kelkit06 strain | CCHFV whole antigen Cell culture-based (VeroE6) | IFNAR−/− mice | Doses: 5 μg Vaccination: 0, 21, 42 day | YES | YES | Turkey-Kelkit06 strain; 1000 PPFU | 60% | Canakoglu et al. (2015) [132] | |
| Doses: 20 μg or 40 μg Vaccination: 0, 21, 42 day | 80% | ||||||||
| IS-BALB/c mice | Doses: 20 μg Vaccination: 0, 14, 28 day | YES | YES | Turkey-Kelkit06 strain; 100 PPFU | 100% | Pavel et al. (2020) [133] | |||
| Subunit vaccines | Chinese Xinjiang strain HANM18 | NP and Gn Expressed in baculovirus-insect expression system | BALB/c mice | Doses: 107 PFU Vaccination: 0, 14, 28 day | YES | YES | NE | NE | Zhang et al. (2023) [134] |
| NP and Gn Fused with Zera tags Expressed in baculovirus-insect expression system | Doses: 10 μg Vaccination: 0, 14, 28 day | YES | YES | NE | NE | Zhang et al. (2023) [135] | |||
| DNA vaccines | IbAr10200 strain | NP, Gn and Gc | IFNAR−/− mice | Doses: 50 μg Vaccination: 0, 28, 49 day | YES | YES | IbAr 10200 strain; 400 FFU | 100% | Hinkula et al. (2017) [92] |
| IbAr10200 strain | NP, Gn and Gc Fused with LAMP1 | Human MHC (HLA-A11/DR1) transgenic mice | Doses: 70 μg Vaccination: 0, 3, 6 week | YES | YES | 100 TCID50 CCHFV tecVLPS | % survival not measured NP provided protection | Hu et al. (2023) [136] | |
| Ank-2 strain | NP and NP combined with CD24 | For immunological response: BALB/c mice For challenge: IFNAR−/− mice | Doses: Totally 50 μg Vaccination: 0, 14 day | YES | YES | Ank-2 strain; 1000 TCID50 | 100% | Farzani et al. (2019) [137] | |
| Hoti strain | NP and GPC Fused with ubiquitin | Cynomolgus Macaque | Doses: 1 mg each plasmids Vaccination: 3 times, 3 weeks interval | YES | YES | Hoti strain; 100,000 TCID50 | NP+ GPC provided clinical improvements | Hawman et al. (2021) [78] | |
| NP and GPC Fused with ubiquitin | Cynomolgus Macaque | Doses: 1 mg both NP plasmid and GPC plasmid Vaccination: 2 times, 3 weeks interval | YES | YES | Hoti strain; 100,000 TCID50 | Two times vaccination regime provided earlier protection | Hawman et al. (2023) [138] | ||
| Doses: 1 mg NP plasmid or GPC plasmid Vaccination: 3 times, 3 weeks interval | |||||||||
| Virus-like replicon particles (VRP) vaccines | IbAr10200 strain | CCHF tc-VLP components | IFNAR−/−mice | Dose: 106 VLPs Vaccination: 0, 28, 49 day | YES | YES | IbAr10200 strain; 400 FFU | 40% | Hinkula et al. (2017) [92] |
| IbAr10200 strain | CCHF VRP components | IFNAR−/− mice | Doses: 100,000 TCID50 Vaccination: Single dose | YES | NE | IbAr 10200 strain; 100 TCID50 | 100% | Scholte et al. (2019) [139] | |
| Doses: 1000 TCID50 Vaccination: Single dose | 78% | ||||||||
| Doses: 100,000 TCID50 Vaccination: Single dose | NE | NE | Turkey strain and Oman-97 strain; 100 TCID50 | 100% | Spengler et al. (2019) [140] | ||||
| Turkey-2004 strain; 100 TCID50 | Single dose VRP protected against lethal outcome 3 days post- vaccination | Spengler et al. (2021) [141] | |||||||
| Doses: 100,000 TCID50 Vaccination: 3, 7, 14, or 28 day | YES | YES | Longer vaccination periods provided stronger protection | Sorvillo et al. (2024) [142] | |||||
| Viral-vector based vaccines | IbAr10200 strain | NP expressed in modified vaccinia virus Ankara (MVA) | IFNα/β/γR−/− mice | Doses:107 PFU Vaccination: 0, 2 week | YES | YES | IbAr 10200 strain; 200 TCID50 | 0% | Dowall et al. (2016) [91] |
| IbAr10200 strain | NP expressed in Adenovirus type 5 (AdV5) | IFNAR−/− mice | Doses: 1.25 × 107 IFU; day 0 108 IFU; day 28 | YES | NE | IbAr10200 strain; 1000 LD50 | 78% | Zivcec et al. (2018) [143] | |
| Ank-2 strain | NP expressed in Bovine Herpesvirus Type 4 (BoHV-4) | For immunological response: BALB/c mice For challenge: IFNα/β/γR−/− mice | Doses: 100 TCID50 Vaccination: 0, 2 week | YES | YES | Ank-2 strain; 1000 TCID50 | 100% | Farzani et al. (2019) [144] | |
| Self- replicating Alphavirus-based vaccines | SPU 187/90 strain | NP DNA-based Sindbis replicon | NIH-III Heterozygous mice strain | Doses: 100 μg NP Vaccination: 0, 21, 42 day | YES | YES | NE | NE | Tipih et al. (2021) [145] |
| Hoti strain | NP and GPCVenezuelan Equine Encephalitis Virus (VEEV) RNA replicon | IS -C57BL/6 mice | Doses: 2.5 μg NP, 2.5 μg GPC, and 5 μg NP + GPC Vaccination: 0, 4 week | YES | NE | UG3010 strain; 100 TCID50 | 100% NP and NP + GPC | Leventhal et al. (2022) [146] | |
| Doses: 1 μg NP + GPC, two dual RNAs and 0,5 μg repGcFL-NP, bivalent single-RNA Vaccination: Single dose | YES | YES | UG3010 strain; 100 TCID50 | 100% | Leventhal et al. (2024) [147] | ||||
| Rhesus Macaque | Doses: 25 μg NP, 25 μg GPC, and 50 μg NP + GPC Vaccination: 2 times, 6 weeks interval | YES | NE | CMP-CCHFV Hoti strain; 100,000 TCID50 | NP + GPC provided protection | Hawman et al. (2024) [148] | |||
| mRNA vaccines | Ank-2 strain | Naked NP mRNA | For immunological response: C57BL/6 mice For challenge: IFNα/β/γR−/− mice | Doses: 25 μg mRNA Vaccination: 0, 2 week | YES | YES | Ank-2 strain; 1000 TCID50 | Single dose showed 50% protection Double dose showed 100% protection | Farzani et al. (2019) [149] |
| IbAr10200 strain | Nucleoside- modified NP and GcGn mRNAs Formulated within LNP | IFNAR−/− mice | Doses: 10 μg each mRNAs and 20 μg mix Vaccination: 0, 3 week | YES | YES | IbAr10200 strain; 400 FFU | 100% | Appelberg et al. (2022) [150] | |
| Turkey-Kelkit06 strain | Nucleoside- modified NP mRNA Formulated within PLGA | For immunological response: BALB/c mice For challenge: IS-C57BL/6 mice | Doses: 10 μg mRNA; day 0 20-25 μg mRNA; day 14 Vaccination: 0, 2 week | YES | YES | Turkey-Kelkit06 strain; 400 PPFU | 100% | Keskin et al. (2023) [151] |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Pirincal, A.; Doymaz, M.Z. The Role of Nucleocapsid Protein (NP) in the Immunology of Crimean–Congo Hemorrhagic Fever Virus (CCHFV). Viruses 2024, 16, 1547. https://doi.org/10.3390/v16101547
Pirincal A, Doymaz MZ. The Role of Nucleocapsid Protein (NP) in the Immunology of Crimean–Congo Hemorrhagic Fever Virus (CCHFV). Viruses. 2024; 16(10):1547. https://doi.org/10.3390/v16101547
Chicago/Turabian StylePirincal, Aysegul, and Mehmet Z. Doymaz. 2024. "The Role of Nucleocapsid Protein (NP) in the Immunology of Crimean–Congo Hemorrhagic Fever Virus (CCHFV)" Viruses 16, no. 10: 1547. https://doi.org/10.3390/v16101547
APA StylePirincal, A., & Doymaz, M. Z. (2024). The Role of Nucleocapsid Protein (NP) in the Immunology of Crimean–Congo Hemorrhagic Fever Virus (CCHFV). Viruses, 16(10), 1547. https://doi.org/10.3390/v16101547






