Evaluation of Stability, Inactivation, and Disinfection Effectiveness of Mpox Virus
Abstract
1. Introduction
2. Materials and Methods
2.1. Cells and Virus
2.2. Virus Culture and Titration
2.3. Temperature and Freeze–Thaw Cycle Stability
2.4. Heat Inactivation
2.5. BPL Inactivation
2.6. Validation of the Inactivation
2.7. Virucidal Activity of Disinfectants
2.8. Statistical Analysis
3. Results
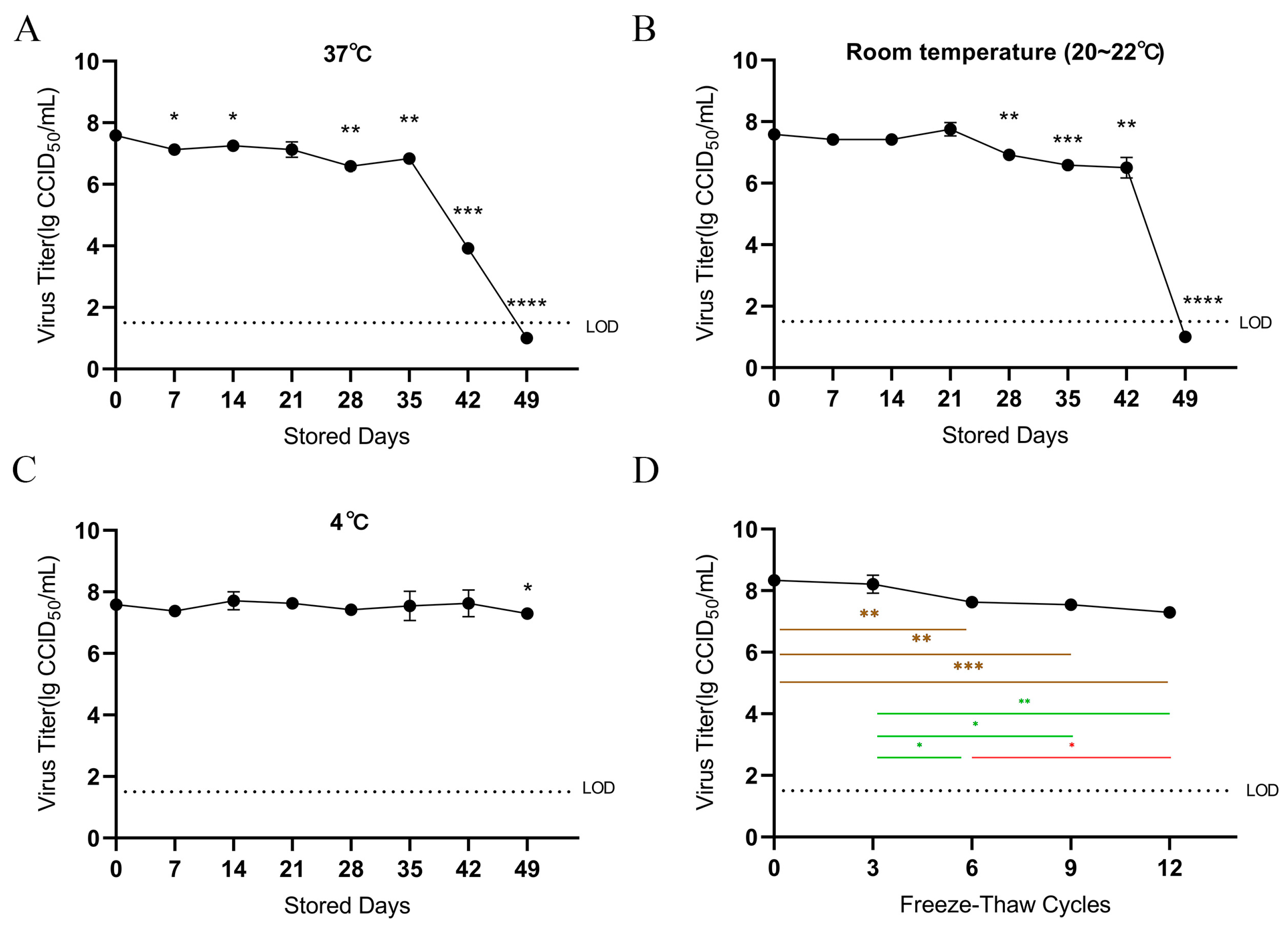
3.1. Temperature Stability
3.2. Freeze–Thaw Cycle Stability
3.3. Heat Inactivation
3.4. BPL Inactivation Method
3.5. Virucidal Activity of Disinfectants
4. Discussion
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Ladnyj, I.D.; Ziegler, P.; Kima, E. A human infection caused by monkeypox virus in Basankusu Territory, Democratic Republic of the Congo. Bull. World Health Organ. 1972, 46, 593–597. [Google Scholar] [PubMed]
- Foster, S.O.; Brink, E.W.; Hutchins, D.L.; Pifer, J.M.; Lourie, B.; Moser, C.R.; Cummings, E.C.; Kuteyi, O.E.; Eke, R.E.; Titus, J.B.; et al. Human monkeypox. Bull. World Health Organ. 1972, 46, 569–576. [Google Scholar] [PubMed]
- Breman, J.G.; Kalisa, R.; Steniowski, M.V.; Zanotto, E.; Gromyko, A.I.; Arita, I. Human monkeypox, 1970–1979. Bull. World Health Organ. 1980, 58, 165–182. [Google Scholar] [PubMed]
- Realegeno, S.; Puschnik, A.S.; Kumar, A.; Goldsmith, C.; Burgado, J.; Sambhara, S.; Olson, V.A.; Carroll, D.; Damon, I.; Hirata, T.; et al. Monkeypox Virus Host Factor Screen Using Haploid Cells Identifies Essential Role of GARP Complex in Extracellular Virus Formation. J. Virol. 2017, 91, e00011-17. [Google Scholar] [CrossRef] [PubMed]
- Likos, A.M.; Sammons, S.A.; Olson, V.A.; Frace, A.M.; Li, Y.; Olsen-Rasmussen, M.; Davidson, W.; Galloway, R.; Khristova, M.L.; Reynolds, M.G.; et al. A tale of two clades: Monkeypox viruses. J. Gen. Virol. 2005, 86, 2661–2672. [Google Scholar] [CrossRef] [PubMed]
- Xiang, Y.; White, A. Monkeypox virus emerges from the shadow of its more infamous cousin: Family biology matters. Emerg. Microbes Infect. 2022, 11, 1768–1777. [Google Scholar] [CrossRef]
- Srivastava, S.; Kumar, S.; Jain, S.; Mohanty, A.; Thapa, N.; Poudel, P.; Bhusal, K.; Al-Qaim, Z.H.; Barboza, J.J.; Padhi, B.K.; et al. The Global Monkeypox (Mpox) Outbreak: A Comprehensive Review. Vaccines 2023, 11, 1093. [Google Scholar] [CrossRef] [PubMed]
- World Health Organization. 2022–23 Mpox (Monkeypox) Outbreak: Global Trends. Available online: https://worldhealthorg.shinyapps.io/mpx_global/ (accessed on 6 August 2023).
- WHO. Virtual Press Conference on COVID-19 and Other Global Health Issues Transcript 11 May 2023. Available online: https://www.who.int/publications/m/item/virtual-press-conference-on-covid-19-and-other-global-health-issues-transcript---11-may-2023 (accessed on 2 December 2023).
- World Health Organization. Multi-Country Outbreak of Mpox. Available online: https://www.who.int/publications/m/item/multi-country-outbreak-of-mpox--external-situation-report--22---11-may-2023 (accessed on 2 December 2023).
- Adler, H.; Gould, S.; Hine, P.; Snell, L.B.; Wong, W.; Houlihan, C.F.; Osborne, J.C.; Rampling, T.; Beadsworth, M.B.; Duncan, C.J.; et al. Clinical features and management of human monkeypox: A retrospective observational study in the UK. Lancet Infect. Dis. 2022, 22, 1153–1162. [Google Scholar] [CrossRef]
- Meister, T.L.; Brüggemann, Y.; Todt, D.; Tao, R.; Müller, L.; Steinmann, J.; Steinmann, J.; Timm, J.; Drexler, I.; Steinmann, E. Stability and inactivation of monkeypox virus on inanimate surfaces. J. Infect. Dis. 2023, 228, 1227–1230. [Google Scholar] [CrossRef]
- Kampf, G. Efficacy of biocidal agents and disinfectants against the monkeypox virus and other orthopoxviruses. J. Hosp. Infect. 2022, 127, 101–110. [Google Scholar] [CrossRef]
- Kärber, G. Beitrag zur kollektiven Behandlung pharmakologischer Reihenversuche. Naunyn Schmiedebergs Arch. Exp. Pathol. Pharmakol. 1931, 162, 480–483. [Google Scholar] [CrossRef]
- Spearman, C. The method of ‘right and wrong cases’ (‘constant stimuli’) without Gauss’s formulae. Br. J. Psychol. 1908, 2, 227–242. [Google Scholar] [CrossRef]
- World Health Organization. Mpox (monkeypox). Available online: https://www.who.int/news-room/fact-sheets/detail/monkeypox (accessed on 18 April 2023).
- Liu, B.; Panda, D.; Mendez-Rios, J.D.; Ganesan, S.; Wyatt, L.S.; Moss, B. Identification of Poxvirus Genome Uncoating and DNA Replication Factors with Mutually Redundant Roles. J. Virol. 2018, 92, e02152-17. [Google Scholar] [CrossRef]
- Liu, B.; Forman, M.; Valsamakis, A. Optimization and evaluation of a novel real-time RT-PCR test for detection of parechovirus in cerebrospinal fluid. J. Virol. Methods 2019, 272, 113690. [Google Scholar] [CrossRef]
- Liu, B.; Yang, J.X.; Yan, L.; Zhuang, H.; Li, T. Novel HBV recombinants between genotypes B and C in 3′-terminal reverse transcriptase (RT) sequences are associated with enhanced viral DNA load, higher RT point mutation rates and place of birth among Chinese patients. Infect. Genet. Evol. 2018, 57, 26–35. [Google Scholar] [CrossRef] [PubMed]
- Peng, Y.; Liu, B.; Hou, J.; Sun, J.; Hao, R.; Xiang, K.; Yan, L.; Zhang, J.; Zhuang, H.; Li, T. Naturally occurring deletions/insertions in HBV core promoter tend to decrease in hepatitis B e antigen-positive chronic hepatitis B patients during antiviral therapy. Antivir. Ther. 2015, 20, 623–632. [Google Scholar] [CrossRef] [PubMed]
- Wißmann, J.E.; Kirchhoff, L.; Brüggemann, Y.; Todt, D.; Steinmann, J.; Steinmann, E. Persistence of Pathogens on Inanimate Surfaces: A Narrative Review. Microorganisms 2021, 9, 343. [Google Scholar] [CrossRef] [PubMed]
- Kampf, G. Efficacy of heat against the vaccinia virus, variola virus and monkeypox virus. J. Hosp. Infect. 2022, 127, 131–132. [Google Scholar] [CrossRef]
- Butcher, W.; Ulaeto, D. Contact inactivation of orthopoxviruses by household disinfectants. J. Appl. Microbiol. 2005, 99, 279–284. [Google Scholar] [CrossRef] [PubMed]
- Wood, J.P.; Choi, Y.W.; Wendling, M.Q.; Rogers, J.V.; Chappie, D.J. Environmental persistence of vaccinia virus on materials. Lett. Appl. Microbiol. 2013, 57, 399–404. [Google Scholar] [CrossRef]
- Maccallum, F.O.; McDonald, J.R. Survival of variola virus in raw cotton. Bull. World Health Organ. 1957, 16, 247–254. [Google Scholar]
- Maccallum, F.O.; McDonald, J.R. Effect of temperatures of up to 45 degrees C on survival of variola virus in human material in relation to laboratory diagnosis. Bull. World Health Organ. 1957, 16, 441–443. [Google Scholar] [PubMed]
- Essbauer, S.; Meyer, H.; Porsch-Ozcürümez, M.; Pfeffer, M. Long-lasting stability of vaccinia virus (orthopoxvirus) in food and environmental samples. Zoonoses Public Health 2007, 54, 118–124. [Google Scholar] [CrossRef] [PubMed]
- Morgan, C.N.; Whitehill, F.; Doty, J.B.; Schulte, J.; Matheny, A.; Stringer, J.; Delaney, L.J.; Esparza, R.; Rao, A.K.; McCollum, A.M. Environmental Persistence of Monkeypox Virus on Surfaces in Household of Person with Travel-Associated Infection, Dallas, Texas, USA, 2021. Emerg. Infect. Dis. 2022, 28, 1982–1989. [Google Scholar] [CrossRef]
- Chin, A.W.H.; Chu, J.T.S.; Perera, M.R.A.; Hui, K.P.Y.; Yen, H.L.; Chan, M.C.W.; Peiris, M.; Poon, L.L.M. Stability of SARS-CoV-2 in different environmental conditions. Lancet Microbe 2020, 1, e10. [Google Scholar] [CrossRef] [PubMed]
- Dai, M.; Li, H.; Yan, N.; Huang, J.; Zhao, L.; Xu, S.; Wu, J.; Jiang, S.; Pan, C.; Liao, M. Long-term Survival of SARS-CoV-2 on Salmon as a Source for International Transmission. J. Infect. Dis. 2021, 223, 537–539. [Google Scholar] [CrossRef]
- Quéromès, G.; Frobert, E.; Bouscambert-Duchamp, M.; Oblette, A.; Valette, M.; Billaud, G.; Escuret, V.; Lina, B.; Morfin, F.; Gaymard, A. Rapid and reliable inactivation protocols for the diagnostics of emerging viruses: The example of SARS-CoV-2 and monkeypox virus. J. Med. Virol. 2023, 95, e28126. [Google Scholar] [CrossRef]
- Batéjat, C.; Grassin, Q.; Feher, M.; Hoinard, D.; Vanhomwegen, J.; Manuguerra, J.C.; Leclercq, I. Heat inactivation of monkeypox virus. J. Biosaf. Biosecur. 2022, 4, 121–123. [Google Scholar] [CrossRef]
- Kozlovskaya, L.I.; Piniaeva, A.N.; Ignatyev, G.M.; Gordeychuk, I.V.; Volok, V.P.; Rogova, Y.V.; Shishova, A.A.; Kovpak, A.A.; Ivin, Y.Y.; Antonova, L.P.; et al. Long-term humoral immunogenicity, safety and protective efficacy of inactivated vaccine against COVID-19 (CoviVac) in preclinical studies. Emerg. Microbes Infect. 2021, 10, 1790–1806. [Google Scholar] [CrossRef]
- Abdoli, A.; Aalizadeh, R.; Aminianfar, H.; Kianmehr, Z.; Teimoori, A.; Azimi, E.; Emamipour, N.; Eghtedardoost, M.; Siavashi, V.; Jamshidi, H.; et al. Safety and potency of BIV1-CovIran inactivated vaccine candidate for SARS-CoV-2: A preclinical study. Rev. Med. Virol. 2022, 32, e2305. [Google Scholar] [CrossRef]
- Wang, H.; Zhang, Y.; Huang, B.; Deng, W.; Quan, Y.; Wang, W.; Xu, W.; Zhao, Y.; Li, N.; Zhang, J.; et al. Development of an Inactivated Vaccine Candidate, BBIBP-CorV, with Potent Protection against SARS-CoV-2. Cell 2020, 182, 713–721.e9. [Google Scholar] [CrossRef] [PubMed]
- Xia, S.; Duan, K.; Zhang, Y.; Zeng, X.; Zhao, D.; Zhang, H.; Xie, Z.; Li, X.; Peng, C.; Zhang, W.; et al. Safety and Immunogenicity of an Inactivated COVID-19 Vaccine, WIBP-CorV, in Healthy Children: Interim Analysis of a Randomized, Double-Blind, Controlled, Phase 1/2 Trial. Front. Immunol. 2022, 13, 898151. [Google Scholar] [CrossRef] [PubMed]
- Hoffman, R.K.; Warshowsky, B. Betapropiolactone vapor as a disinfectant. Appl. Microbiol. 1958, 6, 358–362. [Google Scholar] [CrossRef] [PubMed]
- Chowdhury, P.; Topno, R.; Khan, S.A.; Mahanta, J. Comparison of β-Propiolactone and Formalin Inactivation on Antigenicity and Immune Response of West Nile Virus. Adv. Virol. 2015, 2015, 616898. [Google Scholar] [CrossRef] [PubMed]
- Xia, S.; Duan, K.; Zhang, Y.; Zhao, D.; Zhang, H.; Xie, Z.; Li, X.; Peng, C.; Zhang, Y.; Zhang, W.; et al. Effect of an Inactivated Vaccine Against SARS-CoV-2 on Safety and Immunogenicity Outcomes: Interim Analysis of 2 Randomized Clinical Trials. JAMA 2020, 324, 951–960. [Google Scholar] [CrossRef]
- Ivanov, A.P.; Klebleeva, T.D.; Rogova, Y.V.; Ivanova, O.E. Development of inactivated cultural yellow fever vaccine. Vopr. Virusol. 2020, 65, 212–217. [Google Scholar] [CrossRef] [PubMed]
- NF EN 14476+A2. Chemical Disinfectants and Antiseptics—Quantitative Suspension Test for the Evaluation of Virucidal Activity in the Medical Area—Test Method and Requirements (Phase 2/Step 1). Available online: https://www.une.org/encuentra-tu-norma/busca-tu-norma/norma?c=N0064335. (accessed on 2 December 2023).
- World Health Organization. Who Guidelines on Viral Inactivation and Removal Procedures Intended to Assure the Viral Safety of Human Blood Plasma products, Annex 4, TRS No 924. Available online: https://www.who.int/publications/m/item/WHO-TRS924-Annex4 (accessed on 2 December 2023).
- Kampf, G.; Steinmann, J.; Rabenau, H. Suitability of vaccinia virus and bovine viral diarrhea virus (BVDV) for determining activities of three commonly-used alcohol-based hand rubs against enveloped viruses. BMC Infect. Dis. 2007, 7, 5. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Steinmann, J.; Paulmann, D.; Becker, B.; Bischoff, B.; Steinmann, E.; Steinmann, J. Comparison of virucidal activity of alcohol-based hand sanitizers versus antimicrobial hand soaps in vitro and in vivo. J. Hosp. Infect. 2012, 82, 277–280. [Google Scholar] [CrossRef]
- Kampf, G.; Rudolf, M.; Labadie, J.C.; Barrett, S.P. Spectrum of antimicrobial activity and user acceptability of the hand disinfectant agent Sterillium Gel. J. Hosp. Infect. 2002, 52, 141–147. [Google Scholar] [CrossRef]
- Siddharta, A.; Pfaender, S.; Vielle, N.J.; Dijkman, R.; Friesland, M.; Becker, B.; Yang, J.; Engelmann, M.; Todt, D.; Windisch, M.P.; et al. Virucidal Activity of World Health Organization-Recommended Formulations Against Enveloped Viruses, Including Zika, Ebola, and Emerging Coronaviruses. J. Infect. Dis. 2017, 215, 902–906. [Google Scholar] [CrossRef]
- Meister, T.L.; Tao, R.; Brüggemann, Y.; Todt, D.; Steinmann, J.; Timm, J.; Drexler, I.; Steinmann, E. Efficient Inactivation of Monkeypox Virus by World Health Organization–Recommended Hand Rub Formulations and Alcohols. Emerg. Infect. Dis. 2023, 29, 189–192. [Google Scholar] [CrossRef] [PubMed]
- Peiró-Mestres, A.; Fuertes, I.; Camprubí-Ferrer, D.; Marcos, M.; Vilella, A.; Navarro, M.; Rodriguez-Elena, L.; Riera, J.; Català, A.; Martínez, M.J.; et al. Frequent detection of monkeypox virus DNA in saliva, semen, and other clinical samples from 12 patients, Barcelona, Spain, May to June 2022. Eurosurveillance 2022, 27, 2200503. [Google Scholar] [CrossRef] [PubMed]
- Cassir, N.; Cardona, F.; Tissot-Dupont, H.; Bruel, C.; Doudier, B.; Lahouel, S.; Bendamardji, K.; Boschi, C.; Aherfi, S.; Edouard, S.; et al. Observational Cohort Study of Evolving Epidemiologic, Clinical, and Virologic Features of Monkeypox in Southern France. Emerg. Infect. Dis. 2022, 28, 2409–2415. [Google Scholar] [CrossRef] [PubMed]
- Yinda, C.K.; Morris, D.H.; Fischer, R.J.; Gallogly, S.; Weishampel, Z.A.; Port, J.R.; Bushmaker, T.; Schulz, J.E.; Bibby, K.; van Doremalen, N.; et al. Stability of Monkeypox Virus in Body Fluids and Wastewater. Emerg. Infect. Dis. 2023, 29, 2065–2072. [Google Scholar] [CrossRef]
| Temp | Time | Virus Titer (lg CCID50/mL; Mean ± SD) | CPE (1/2/3 Passage) | Inactivated (Y/N) | |
|---|---|---|---|---|---|
| Pre-Heating | After-Heating | ||||
| (A) | |||||
| 56 °C | 5 min | 7.13 | 5.97 ± 0.28 | +/+/+ | N |
| 10 min | 3.64 ± 0.9 | +/+/+ | N | ||
| 20 min | 1.88 ± 0 | −/+/+ | N | ||
| 30 min | ND | −/+/+ | N | ||
| 40 min | ND | −/−/− | Y | ||
| 50 min | ND | −/−/− | Y | ||
| (B) | |||||
| 70 °C | 2 min | 7.13 | 6.38 ± 0.05 | +/+/+ | N |
| 5 min | ND | −/−/+ | N | ||
| 10 min | ND | −/−/− | Y | ||
| 15 min | ND | −/−/− | Y | ||
| 20 min | ND | −/−/− | Y | ||
| 30 min | ND | −/−/− | Y | ||
| (C) | |||||
| 95 °C | 2 min | 7.13 | 1.63 ± 0 | −/+/+ | N |
| 5 min | ND | −/−/− | Y | ||
| 10 min | ND | −/−/− | Y | ||
| 15 min | ND | −/−/− | Y | ||
| 20 min | ND | −/−/− | Y | ||
| 30 min | ND | −/−/− | Y | ||
| BPL:Virus | Time (h) | CPE (1/2/3 Passage) | Inactivated (Y/N) |
|---|---|---|---|
| 1:1000 | 24 | −/−/− | Y |
| 1:2000 | −/+/+ | N |
| Chemicals | Concentration (v/v) | Time (min) | Virus Control Titer (Undisinfected; lg CCID50/mL) | Virus Titer (Disinfected; lg CCID50/mL) | Reduction Factor (lg) |
|---|---|---|---|---|---|
| MCP | 5% | 1 | 5.75 | ND | ≥4.25 |
| 5 | ND | ≥4.25 | |||
| 2% | 1 | ND | ≥4.25 | ||
| 5 | ND | ≥4.25 | |||
| Ethanol | 75% | 1 | ND | ≥4.25 | |
| 5 | ND | ≥4.25 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Li, Y.; Lv, S.; Zeng, Y.; Chen, Z.; Xia, F.; Zhang, H.; Dan, D.; Hu, C.; Tang, Y.; Yang, Q.; et al. Evaluation of Stability, Inactivation, and Disinfection Effectiveness of Mpox Virus. Viruses 2024, 16, 104. https://doi.org/10.3390/v16010104
Li Y, Lv S, Zeng Y, Chen Z, Xia F, Zhang H, Dan D, Hu C, Tang Y, Yang Q, et al. Evaluation of Stability, Inactivation, and Disinfection Effectiveness of Mpox Virus. Viruses. 2024; 16(1):104. https://doi.org/10.3390/v16010104
Chicago/Turabian StyleLi, Yuwei, Shiyun Lv, Yan Zeng, Zhuo Chen, Fei Xia, Hao Zhang, Demiao Dan, Chunxia Hu, Yi Tang, Qiao Yang, and et al. 2024. "Evaluation of Stability, Inactivation, and Disinfection Effectiveness of Mpox Virus" Viruses 16, no. 1: 104. https://doi.org/10.3390/v16010104
APA StyleLi, Y., Lv, S., Zeng, Y., Chen, Z., Xia, F., Zhang, H., Dan, D., Hu, C., Tang, Y., Yang, Q., Ji, Y., Lu, J., & Wang, Z. (2024). Evaluation of Stability, Inactivation, and Disinfection Effectiveness of Mpox Virus. Viruses, 16(1), 104. https://doi.org/10.3390/v16010104






