Sociodemographic and Clinical Factors for Microcephaly Secondary to Teratogenic Infections in Brazil: An Ecological Study
Abstract
1. Introduction
2. Material and Methods
2.1. Ethical Considerations
2.2. Type of Study
2.3. Data Base
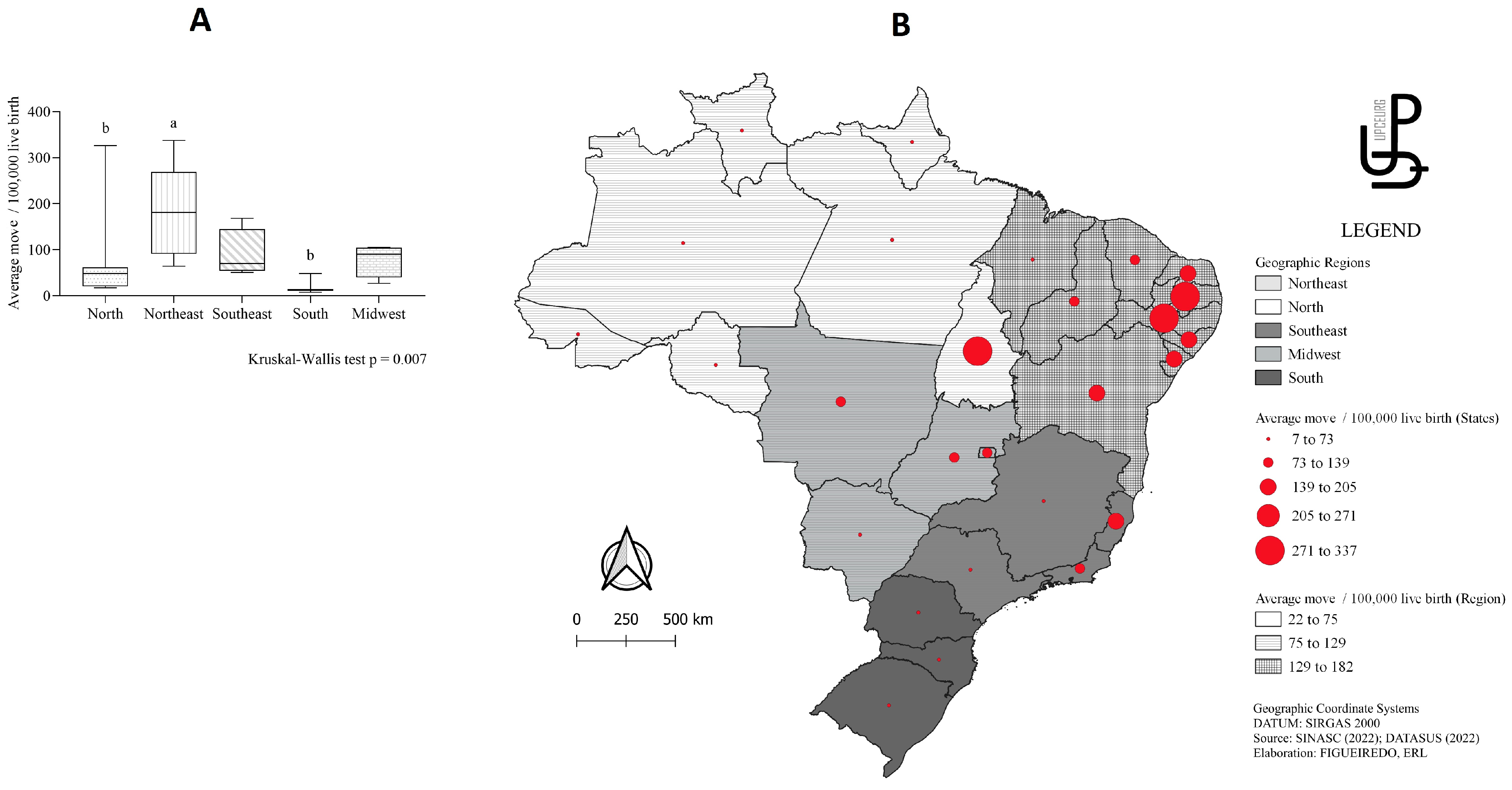
2.4. Description and Characterization of the Area
2.5. Population and Study Period
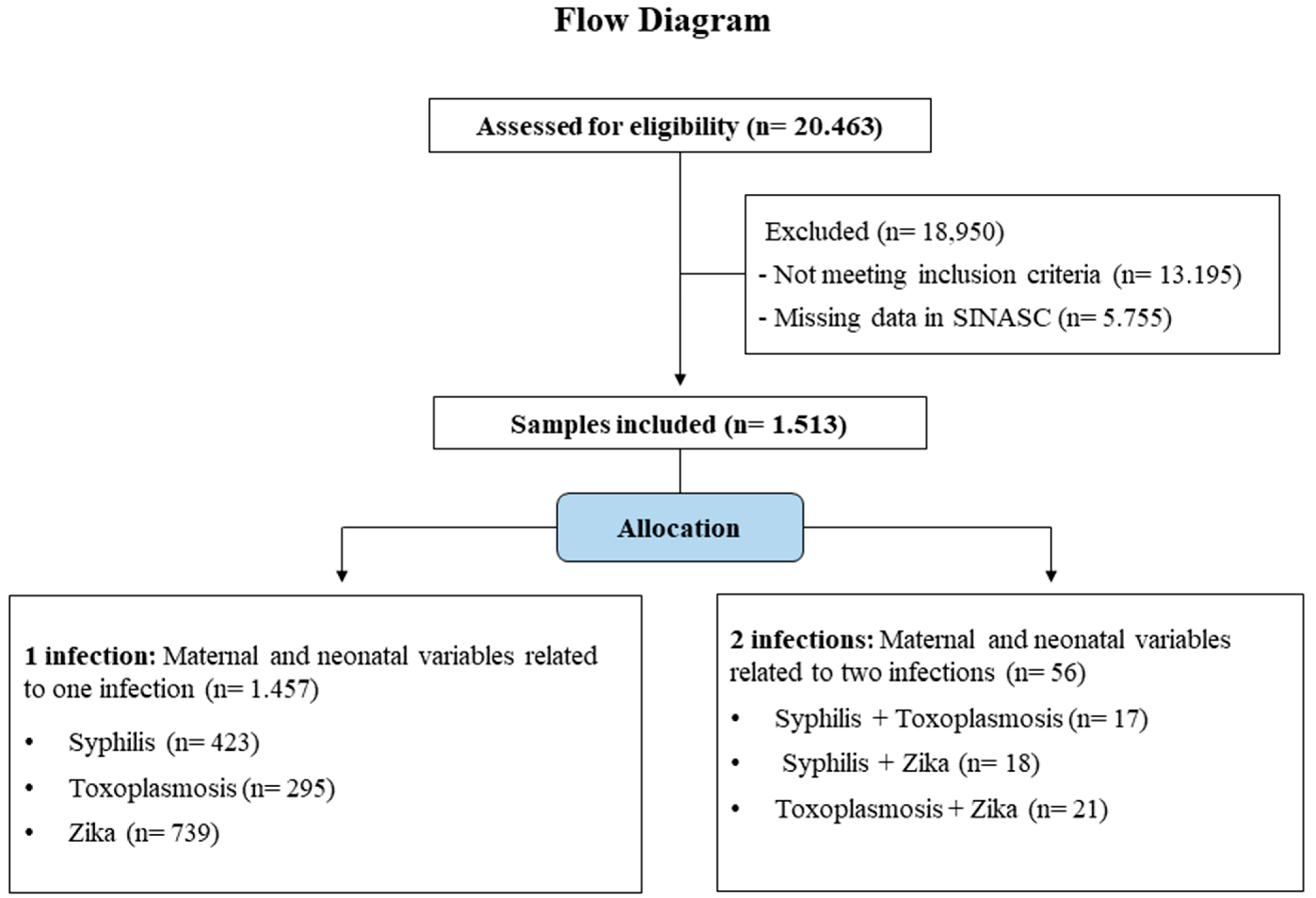
2.6. Allocation of the Selected Samples
2.7. Variables
2.8. Statistical Analysis
3. Results
3.1. Neonatal and Maternal Sociodemographic Factors
3.2. Maternal Clinical Factors
3.3. Clinical Factors in Newborns
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Pires, L.; Freita, L.; Almeida, L.; Cunha, L.; Teixeira, L.; Corrêa, M.; Fortes, C.P.D.D. Microcefalia: Semiologia e abordagem diagnóstica. Resid. Pediatr. 2019, 9, 70–79. [Google Scholar] [CrossRef]
- Faheem, M.; Naseer, M.I.; Rasool, M.; Chaudhary, A.G.; Kumosani, T.A.; Ilyas, A.M.; Pushparaj, P.N.; Ahmed, F.; Algahtani, H.A.; Al-Qahtani, M.H.; et al. Molecular genetics of human primary microcephaly: An overview. BMC Med. Genom. 2015, 8, S4. [Google Scholar] [CrossRef]
- Ministério da Saúde. Protocolo de Vigilância e Resposta à Ocorrência de Microcefalia e/ou Alterações do Sistema Nervoso Central (SNC). 2015. Available online: https://pesquisa.bvsalud.org/portal/resource/pt/lil-786728 (accessed on 10 November 2022).
- Ministério da Saúde. Protocolo de Atenção à Saúde e Resposta à Ocorrência de Microcefalia Relacionada à Infecção Pelo Vírus Zika. 2016. Available online: https://bvsms.saude.gov.br/bvs/publicacoes/protocolo_resposta_microcefalia_relacionada_infeccao_virus_zika.pdf (accessed on 10 November 2022).
- Quintans, M.D.S.; Bueno, A.C.; Cardoso, C.A.A. Microcephaly caused by or associated with congenital infections in the last 20 years in Brazil: A systematic review. Rev. Inst. Med. Trop. São Paulo 2022, 64, e7. [Google Scholar] [CrossRef] [PubMed]
- Neu, N.; Duchon, J.; Zachariah, P. TORCH Infections. Clin. Perinatol. 2015, 42, 77–103. [Google Scholar] [CrossRef] [PubMed]
- Patterson, J.; Sammon, M.; Garg, M. Dengue, Zika and Chikungunya: Emerging Arboviruses in the New World. West. J. Emerg. Med. 2016, 17, 671–679. [Google Scholar] [CrossRef]
- World Health Organization (WHO). Screening, Assessment and Management of Neonates and Infants with Complications Associated with Zika Virus Exposure in Utero. 2016. Available online: https://apps.who.int/iris/handle/10665/204475 (accessed on 10 November 2022).
- Ostrander, B.; Bale, J.F. Congenital and perinatal infections. Handb. Clin. Neurol. 2019, 162, 133–153. [Google Scholar]
- Bahia Oliveira, L.M.G.; Liborio Neto, A.O.; Dudus, M.M. Microcephaly due to congenital toxoplasmosis in times of Zika virus epidemic in Brazil. Sci. Medica 2018, 28, 12. [Google Scholar]
- Donadono, V.; Saccone, G.; Maruotti, G.M.; Berghella, V.; Migliorini, S.; Esposito, G.; Sirico, A.; Tagliaferri, S.; Ward, A.; Mazzarelli, L.L.; et al. Incidence of toxoplasmosis in pregnancy in Campania: A population-based study on screening, treatment, and outcome. Eur. J. Obstet. Gynecol. Reprod. Biol. 2019, 240, 316–321. [Google Scholar] [CrossRef]
- Donadono, V.; Saccone, G.; Sarno, L.; Esposito, G.; Mazzarelli, L.L.; Sirico, A.; Guida, M.; Martinelli, P.; Zullo, F.; Maruotti, G.M. Association between lymphadenopathy after toxoplasmosis seroconversion in pregnancy and risk of congenital infection. Eur. J. Clin. Microbiol. Infect. Dis. 2021, 41, 45–51. [Google Scholar] [CrossRef]
- Venancio, F.A.; Quilião, M.E.; Moura, D.d.A.; de Azevedo, M.V.; Metzker, S.d.A.; Mareto, L.K.; de Medeiros, M.J.; Santos-Pinto, C.D.B.; de Oliveira, E.F. Congenital anomalies during the 2015–2018 Zika virus epidemic: A population-based cross-sectional study. BMC Public Health 2022, 22, 2069. [Google Scholar] [CrossRef] [PubMed]
- Bezerra, M.L.D.M.B.; Fernandes, F.E.C.V.; de Oliveira Nunes, J.P.; Baltar, S.L.S.M.D.A.; Randau, K.P. Congenital Syphilis as a Measure of Maternal and Child Healthcare, Brazil. Emerg. Infect. Dis. 2019, 25, 1469–1476. [Google Scholar] [CrossRef]
- Bale, J.F. Fetal Infections and Brain Development. Clin. Perinatol. 2009, 36, 639–653. [Google Scholar] [CrossRef] [PubMed]
- de Magalhães-Barbosa, M.C.; Prata-Barbosa, A.; Robaina, J.R.; Raymundo, C.E.; Lima-Setta, F.; da Cunha, A.J.L.A. Trends of the microcephaly and Zika virus outbreak in Brazil, January–July 2016. Travel Med. Infect. Dis. 2016, 14, 458–463. [Google Scholar] [CrossRef] [PubMed]
- Nunes, M.L.; Carlini, C.R.; Marinowic, D.; Kalil Neto, F.; Fiori, H.H.; Scotta, M.C.; Zanella, P.L.A.; Soder, R.B.; da Costa, J.C. Microcephaly and Zika virus: A clinical and epidemiological analysis of the current outbreak in Brazil. J. Pediatr. 2016, 92, 230–240. [Google Scholar] [CrossRef]
- Duarte, G.; Miranda, A.E.; Bermudez, X.P.D.; Saraceni, V.; Martinez-Espinosa, F.E. Brazilian Protocol for Sexually Transmitted Infections 2020: Zika virus infection. Rev. Soc. Bras. Med. Trop. 2021, 54, e2020609. [Google Scholar] [CrossRef] [PubMed]
- Duarte, G.; Moron, A.F.; Timerman, A.; Fernandes, C.E.; Neto, C.M.; Filho, G.L.d.A.; Junior, H.W.; Santo, H.F.B.D.E.; Steibel, J.A.P.; Filho, J.B.; et al. Zika Virus Infection in Pregnant Women and Microcephaly. Rev. Bras. Ginecol. Obstet. 2017, 39, 235–248. [Google Scholar] [CrossRef]
- Musso, D.; Roche, C.; Robin, E.; Nhan, T.; Teissier, A.; Cao-Lormeau, V.-M. Potential Sexual Transmission of Zika Virus. Emerg. Infect. Dis. 2015, 21, 359–361. [Google Scholar] [CrossRef]
- Macnamara, F.N. Zika virus: A report on three cases of human infection during an epidemic of jaundice in Nigeria. Trans. R. Soc. Trop. Med. Hyg. 1954, 48, 139–145. [Google Scholar] [CrossRef]
- Liu, Z.-Y.; Shi, W.-F.; Qin, C.-F. The evolution of Zika virus from Asia to the Americas. Nat. Rev. Genet. 2019, 17, 131–139. [Google Scholar] [CrossRef]
- Cabral, C.M.; Nóbrega, M.E.B.D.; Leite, P.L.; Souza, M.S.F.D.; Teixeira, D.C.P.; Cavalcante, T.F.; de Souza Lima, R.G.; de Azevedo Tavares, L.M.S.; de Souza, P.B.; Saad, E. Clinical-epidemiological description of live births with microcephaly in the state of Sergipe, Brazil, 2015. Epidemiol. Serv. Saúde 2017, 26, 245–254. [Google Scholar] [CrossRef]
- de França, G.V.A.; Pedi, V.D.; de Oliveira Garcia, M.H.; do Carmo, G.M.I.; Leal, M.B.; Garcia, L.P. Congenital syndrome associated with Zika virus infection among live births in Brazil: A description of the distribution of reported and confirmed cases in 2015–2016. Epidemiol. Serv. Saúde 2018, 27, e2017473. [Google Scholar]
- Brasil. Ministério da Saúde. Conselho Nacional de Saúde. Resolução nº 510, de 7 de Abril de 2016. Available online: http://bvsms.saude.gov.br/bvs/saudelegis/cns/2016/res0510_07_04_2016.html (accessed on 15 November 2022).
- Departamento de Informática do Sistema Único de Saúde (DATASUS). SINASC. Live Births—Since 1994 DATASUS. 2022. Available online: https://datasus.saude.gov.br/nascidos-vivos-desde-1994/ (accessed on 15 November 2022).
- Departamento de Informática do Sistema Único de Saúde (DATASUS). OpenDataSUS—SINASC. 2022. Available online: https://opendatasus.saude.gov.br/dataset/sistema-de-informacao-sobre-nascidos-vivos-sinasc (accessed on 15 November 2022).
- Ministério da Saúde. Manual de Procedimentos do Sistema de Informações Sobre Nascidos Vivos. 2001. Available online: https://bvsms.saude.gov.br/bvs/publicacoes/sis_mortalidade.pdf (accessed on 15 November 2022).
- Instituto Brasileiro de Geografia e Estatística. Cidades e Estados do Brasil. 2021. Available online: https://cidades.ibge.gov.br (accessed on 15 November 2022).
- Stamm, L.V.; Noda, A. Elimination of Mother-To-Child Transmission of Syphilis in the Americas—A Goal That Must Not Slip Away. Sex. Transm. Dis. 2017, 44, 12–13. [Google Scholar] [CrossRef] [PubMed]
- Fitchett, E.J.A.; Seale, A.C.; Vergnano, S.; Sharland, M.; Heath, P.T.; Saha, S.K.; Agarwal, R.; Ayede, A.I.; Bhutta, Z.A.; Black, R.; et al. Strengthening the Reporting of Observational Studies in Epidemiology for Newborn Infection (STROBE-NI): An extension of the STROBE statement for neonatal infection research. Lancet Infect. Dis. 2016, 16, e202–e213. [Google Scholar] [CrossRef] [PubMed]
- Vissoci, J.R.N.; Rocha, T.; Da Silva, N.C.; Queiroz, R.C.D.S.; Thomaz, E.B.A.F.; Amaral, P.V.M.; Lein, A.; Branco, M.D.R.F.C.; Aquino, J.; Rodrigues, Z.M.R.; et al. Zika virus infection and microcephaly: Evidence regarding geospatial associations. PLoS Neglect. Trop. Dis. 2018, 12, e0006392. [Google Scholar] [CrossRef]
- Freitas, P.D.S.S.; Soares, G.B.; Mocelin, H.J.S.; Lacerda, L.C.X.; do Prado, T.N.; Sales, C.M.M.; Perez, F.; de Azevedo Bussinger, E.C.; Maciel, E.L.N. Congenital Zika syndrome: Sociodemographic profile of mothersSíndrome congénito por el virus del Zika: Perfil sociodemográfico de las madres. Rev. Panam. Salud Publica Pan Am. J. Public Health 2019, 43, e24. [Google Scholar]
- Diniz, D.; Brito, L. UMA EPIDEMIA SEM FIM: Zika e Mulheres. In Políticas Etnográficas no Campo da Moral [Internet]; Universidade Federal do Rio Grande do Sul (UFRGS): Porto Alegre, Brazil, 2019. [Google Scholar]
- Staurengo-Ferrari, L.; da Silva Sanfelice, R.A.; de Souza, J.B.; Assolini, J.P.; dos Santos, D.P.; Cataneo, A.H.D.; Bordignon, J.; Conchon-Costa, I.; da Costa, I.N.; Fernandes, G.S.A. Impact of Toxoplasma Gondii Infection on TM3 Leydig Cells: Alterations in Testosterone and Cytokines Levels. Acta Tropica 2021, 220, 105938. [Google Scholar] [CrossRef]
- Kaňková, Š.; Šulc, J.; Nouzová, K.; Fajfrlík, K.; Frynta, D.; Flegr, J. Women infected with parasite Toxoplasma have more sons. Naturwissenschaften 2007, 94, 122–127. [Google Scholar] [CrossRef] [PubMed]
- Wang, J.-N.; Ling, F. Zika Virus Infection and Microcephaly: Evidence for a Causal Link. Int. J. Environ. Res. Public Health 2016, 13, 1031. [Google Scholar] [CrossRef]
- de Fatima Pessoa Militão de Albuquerque, M.; de Souza, W.V.; Araújo, T.V.B.; Braga, M.C.; de Barros Miranda-Filho, D.; de Alencar Ximenes, R.A.; de Melo Filho, D.A.; de Brito, C.A.A.; Valongueiro, S.; de Melo, A.P.L.; et al. The microcephaly epidemic and Zika virus: Building knowledge in epidemiology. Cad. Saude Publica 2018, 34, e00069018. [Google Scholar]
- de Oliveira, W.K.; de França, G.V.A.; Carmo, E.H.; Duncan, B.B.; de Souza, K.R.; Schmidt, M.I. Infection-related microcephaly after the 2015 and 2016 Zika virus outbreaks in Brazil: A surveillance-based analysis. Lancet 2017, 390, 861–870. [Google Scholar] [CrossRef]
- Hurt, K.; Kodym, P.; Stejskal, D.; Zikan, M.; Mojhova, M.; Rakovic, J. Toxoplasmosis impact on prematurity and low birth weight. PLoS ONE 2022, 17, e0262593. [Google Scholar] [CrossRef] [PubMed]
- Carvalho-Sauer, R.; Costa, M.D.C.N.; Barreto, F.R.; Teixeira, M.G. Congenital Zika Syndrome: Prevalence of low birth weight and associated factors. Bahia, 2015–2017. Int. J. Infect. Dis. 2019, 82, 44–50. [Google Scholar] [CrossRef]
- Chibueze, E.C.; Tirado, V.; Lopes, K.D.S.; Balogun, O.O.; Takemoto, Y.; Swa, T.; Dagvadorj, A.; Nagata, C.; Morisaki, N.; Menendez, C.; et al. Zika virus infection in pregnancy: A systematic review of disease course and complications. Reprod. Health 2017, 14, 28. [Google Scholar] [CrossRef]
- França, G.V.A.; Schuler-Faccini, L.; Oliveira, W.K.; Henriques, C.M.P.; Carmo, E.H.; Pedi, V.D.; Nunes, M.L.; De Castro, M.C.; Serruya, S.; Silveira, M.F.; et al. Congenital Zika virus syndrome in Brazil: A case series of the first 1501 livebirths with complete investigation. Lancet 2016, 388, 891–897. [Google Scholar] [CrossRef]
- Howick, J.; Kelly, P.; Kelly, M. Establishing a causal link between social relationships and health using the Bradford Hill Guidelines. SSM—Popul. Health 2019, 8, 100402. [Google Scholar] [CrossRef] [PubMed]
- Silva, A.A.; Barbieri, M.A.; Alves, M.T.; Carvalho, C.A.; Batista, R.F.; Ribeiro, M.R.; Lamy-Filho, F.; Lamy, Z.C.; Cardoso, V.C.; Cavalli, R.C.; et al. Prevalence and Risk Factors for Microcephaly at Birth in Brazil in 2010. Pediatrics 2018, 141, e20170589. [Google Scholar] [CrossRef]
- Gallo, L.G.; Martinez-Cajas, J.; Peixoto, H.M.; Pereira, A.C.E.D.S.; Carter, J.E.; McKeown, S.; Schaub, B.; Ventura, C.V.; De França, G.V.A.; Pomar, L.; et al. Another piece of the Zika puzzle: Assessing the associated factors to microcephaly in a systematic review and meta-analysis. BMC Public Health 2020, 20, 827. [Google Scholar] [CrossRef] [PubMed]
- Melo, N.D.L.; de Sousa, D.F.; Laporta, G.Z. Microcephaly and Associated Risk Factors in Newborns: A Systematic Review and Meta-Analysis Study. Trop. Med. Infect. Dis. 2022, 7, 261. [Google Scholar] [CrossRef] [PubMed]
- Auger, N.; Quach, C.; Healy-Profitós, J.; Lowe, A.-M.; Arbour, L. Congenital microcephaly in Quebec: Baseline prevalence, risk factors and outcomes in a large cohort of neonates. Arch. Dis. Child.—Fetal Neonatal Ed. 2017, 103, F167–F172. [Google Scholar] [CrossRef]
- Liu, S.; Pan, Y.; Auger, N.; Sun, W.; Dai, L.; Li, S.; Xie, S.; Wen, S.W.; Chen, D. Small head circumference at birth: An 8-year retrospective cohort study in China. BMJ Paediatr. Open 2019, 3, e000470. [Google Scholar] [CrossRef]
| Syphilis (n = 423) | Toxoplasmosis (n = 295) | Zika Vírus (n = 739) | χ2 or Fisher’s Exact Test | p-Value | |
|---|---|---|---|---|---|
| Race/Ethnicity Maternal | |||||
| White | 64 (19.8%) a | 74 (31.4%) | 127 (30.3%) b | 1.165 º | <0.050 * |
| Black | 49 (15.1%) a | 20 (8.5%) | 20 (4.8%) b | ||
| Yellow | 1 (0.3%) | 2 (0.8%) | 3 (0.7%) | ||
| Brown | 208 (64.2%) | 138 (58.5%) | 268 (64%) | ||
| Indigenous | 2 (0.6%) | 2 (0.8%) | 1 (0.2%) | ||
| Sex of the neonate | |||||
| Male | 173 (41.2%) | 111 (37.9%) a | 348 (47.9%) b | 10.206 # | 0.006 * |
| Female | 247 (41.2%) | 182 (62.1%) a | 379 (52.1%) b | ||
| Year of birth | |||||
| 2015 | 53 (12.6%) a | 36 (12.3%) a | 214 (29%) b | 131.829 # | <0.001 * |
| 2016 | 127 (30.2%) | 75 (25.6%) a | 279 (37.8%) b | ||
| 2017 | 59 (14%) | 48 (16.4%) | 92 (12.5%) | ||
| 2018 | 59 (14%) a | 38 (13%) | 63 (8.5%) b | ||
| 2019 | 50 (11.9%) a | 40 (13.7%) a | 40 (5.4%) b | ||
| 2020 | 37 (8.8%) | 36 (12.3%) a | 31 (4.2%) b | ||
| 2021 | 35 (8.3%) a | 20 (6.8%) | 19 (2.6%) b | ||
| Classification of the live birth | |||||
| Preterm birth (<37 weeks) | 100 (24.5%) | 82 (29.1%) a | 134 (20%) b | 5.017 º | 0.025 * |
| Term birth (37 to <42 weeks) | 307 (75.2%) | 199 (70.6%) a | 529 (79%) b | ||
| Post term birth (≥42 weeks) | 1 (0.2%) | 1 (0.4%) | 7 (1%) |
| 1 Infection (n= 1457 ) | 2 Infections (n = 56 ) | χ2 or Fisher’s Exact Test | p-Value | |
|---|---|---|---|---|
| Race/Ethnicity | 0.923 º | 0.337 | ||
| White | 265 (27.1%) | 9 (20.5%) | ||
| Black | 89 (9.1%) | 4 (9.1%) | ||
| Yellow | 6 (0.6%) | 0 (0%) | ||
| Brown | 614 (62.7%) | 31 (70.5%) | ||
| Indigenous | 5 (0.5%) | 0 (0%) | ||
| Sex of the neonate | 0.409 # | 0.261 | ||
| Male | 632 (43.9%) | 27 (48.2%) | ||
| Female | 808 (56.1%) | 29 (51.8%) | ||
| Year of birth | 5.472 º | 0.019 * | ||
| 2015 | 303 (20.9%) a | 5 (9.1%) b | ||
| 2016 | 481 (33.1%) | 17 (30.9%) | ||
| 2017 | 199 (13.7%) | 10 (18.2%) | ||
| 2018 | 160 (11%) | 9 (16.4%) | ||
| 2019 | 130 (9%) | 1 (1.8%) | ||
| 2020 | 104 (7.2%) | 7 (12.7%) | ||
| 2021 | 74 (5.1%) | 6 (10.9%) | ||
| Classification of the live birth | 0.387 # | 0.412 | ||
| Preterm birth (<37 weeks) | 316 (23.2%) | 12 (25%) | ||
| Term birth (37 to <42 weeks) | 1035 (76.1%) | 36 (75%) | ||
| Post term birth (≥42 weeks) | 9 (0.7%) | 0 (0%) |
| Syphilis (n = 419) | Toxoplasmosis (n = 275) | Zika Vírus (n = 727) | χ2, Fisher’s Exact Test or H Value | p-Value | |
|---|---|---|---|---|---|
| Mother’s Age § | 25 (11) a | 26 (11) a | 28 (10) b | 2316 ¢ | <0.001 * |
| Type of pregnancy | |||||
| Single | 393 (96.1%) | 279 (98.2%) | 655 (97.5%) | ||
| Double | 16 (3.9%) | 5 (1.8%) | 16 (2.4%) | 1009 º | 0.315 |
| Triple | 0 (0%) | 0 (0%) | 0 (0%) | ||
| Gestational fever | |||||
| Yes | 48 (14.7%) a | 35 (14.9%) a | 264 (48.8%) b | 148.04 # | <0.001 * |
| No | 279 (85.3%) a | 200 (85.1%) a | 277 (51.2%) b | ||
| Exanthema | |||||
| Yes, in the 1st quarter | 23 (7.2%) a | 23 (10%) a | 239 (41.4%) b | ||
| Yes, no 2nd quarter | 12 (3.8%) a | 9 (3.9%) a | 105 (18.2%)b | ||
| Yes, no 3rd trimester | 7 (2.2%) a | 5 (2.2%) a | 51 (8.8%) b | 354.9 # | <0.001 * |
| Yes, but no gestational date or period | 10 (3.1%) | 4 (1.7%) | 22 (3.8%) | ||
| Exanthema absent | 267 (83.7%) a | 188 (82.1%) a | 160 (27.7%) b | ||
| Pruritus | |||||
| Yes | 25 (5.9%) a | 17 (5.8%) a | 177 (24%) b | 93.436 # | <0.001 * |
| No | 398 (94.1%) a | 278 (94.2%) a | 562 (76%) b | ||
| Conjunctivitis | |||||
| Yes | 8 (1.9%) a | 1 (0.3%) a | 41 (5.5%) b | 21.531 # | <0.001 * |
| No | 415 (98.1%) a | 294 (99.7%) a | 698 (94.5%) b | ||
| Joint pain | |||||
| Yes | 20 (4.7%) a | 5 (1.7%) a | 135 (18.3%) b | 83.082 # | <0.001 * |
| No | 403 (95.3%) a | 290 (98.3%) a | 604 (81.7%) b | ||
| Muscular pain | |||||
| Yes | 24 (5.7%) a | 5 (1.7%) b | 105 (14.2%) c | 48.39 # | <0.001 * |
| No | 399 (94.3%) a | 290 (98.7%) b | 634 (85.8%) c | ||
| Edema | |||||
| Yes | 6 (1.4%) a | 2 (0.7%) a | 22 (3%) b | 6739 # | 0.034 * |
| No | 417 (98.6%) a | 293 (99.3%) a | 717 (97%) b | ||
| Headache | |||||
| Yes | 29 (6.9%) a | 22 (7.5%) a | 128 (17.3%) b | 35.34 # | <0.001 * |
| No | 394 (93.1%) a | 273 (92.5%) a | 611 (82.7%) b | ||
| Ganglion hypertrophy | |||||
| Yes | 1 (0.2%) a | 1 (0.3%) a | 10 (1.4%) b | 4579 º | 0.032 * |
| No | 422 (99.8%) a | 294 (99.7%) a | 729 (98.6%) b | ||
| Neural damage | |||||
| Yes | 3 (0.7%) | 0 (0%) | 4 (0.5%) | 0.051 º | 0.821 |
| No | 420 (99.3%) | 295 (100%) | 735 (99.5%) |
| 1 Infection (n = 1457) | 2 Infections (n = 67) | χ2, Fisher’s Exact Test or Mann–Whitney U | p-Value | |
|---|---|---|---|---|
| Mother’s Age ¬ | 27 (10) a | 23 (9) b | 28.34000 | 0.012 * |
| Type of Pregnancy | ||||
| Single | 1327 (97.2%) | 47 (97.9%) | 0.096 º | 0.757 |
| Double | 37 (2.7%) | 1 (2.1%) | ||
| Triple | 1 (0.1%) | 0 (0%) | ||
| Gestational fever | ||||
| Yes | 374 (31.5%) | 13 (26.0%) | 0.664 # | 0.415 |
| No | 756 (68.5%) | 37 (74%) | ||
| Exanthema | ||||
| Yes, in the 1st quarter | 285 (25.3%) | 11 (22.9%) | ||
| Yes, no 2nd quarter | 126 (11.2%) | 6 (12.5%) | 0.614 # | 0.958 |
| Yes, no 3rd trimester | 63 (5.6%) | 2 (4.2%) | ||
| Yes, but no gestational date or period | 36 (3.2%) | 1 (2.1%) | ||
| Exanthema absent | 615 (54.7%) | 28 (58.3%) | ||
| Pruritus | ||||
| Yes | 219 (15%) | 6 (10.7%) | 0.794 # | 0.373 |
| No | 1238 (85%) | 50 (89.3%) | ||
| Conjunctivitis | ||||
| Yes | 50 (3.4%) | 2 (3.6%) | 0.003 º | 0.955 |
| No | 1407 (96.6%) | 54 (96.4%) | ||
| Joint pain | ||||
| Yes | 160 (11%) | 7 (12.5%) | 0.127 # | 0.722 |
| No | 1297 (89%) | 49 (87.5%) | ||
| Muscular pain | ||||
| Yes | 134 (9.2%) | 3 (5.4%) | 0.966# | 0.326 |
| No | 1323 (90.8%) | 53 (94.6%) | ||
| Edema | ||||
| Yes | 30 (2.1%) | 1 (1.8%) | 0.020 º | 0.887 |
| No | 1427 (97.9%) | 55 (98.2%) | ||
| Headache | ||||
| Yes | 179 (12.3%) | 7 (12.5%) | 0.002 # | 0.962 |
| No | 1278 (87.8%) | 49 (87.5%) | ||
| Ganglion hypertrophy | ||||
| Yes | 12 (0.8%) | 0 (0%) | 0.465 º | 0.495 |
| No | 1445 (99.2%) | 56 (100%) | ||
| Neural damage | ||||
| Yes | 7 (0.5%) | 0 (0%) | 0.270 º | 0.603 |
| No | 1450 (99.5%) | 56 (100%) |
| Syphilis (n = 419) | Toxoplasmosis (n = 275) | Zika Vírus (n = 727) | χ2, Fisher’s Exact Test or H Value | p-Value | |
|---|---|---|---|---|---|
| Newborn weight § | 2347.5 (636) | 2435 (760) | 2660 (728) | 3197 ¢ | <0.001 * |
| Cephalic Perimeter § | 30.50 (2) | 30.40 (3) | 30.00 (4) | 1611 ¢ | 0.491 * |
| Neurological Disability | |||||
| Yes | 5 (1.2%) | 4 (1.4%) | 13 (1.8%) | 0.661 # | 0.718 |
| No | 418 (98.8%) | 291 (99.6%) | 726 (98.2%) | ||
| Visual Impairment | |||||
| Yes | 2 (0.5%) | 3 (1.0%) | 5 (0.7%) | 0.093 º | 0.761 |
| No | 421 (99.5%) | 292 (99.5%) | 734 (99.3%) | ||
| Hearing Impairment | |||||
| Yes | 7 (1.7%) | 7 (2.4%) | 15 (2%) | 0.471 # | 0.790 |
| No | 416 (98.3%) | 288 (97.6%) | 724 (98%) | ||
| Detection Type | |||||
| Intrauterine (during pregnancy) | 68 (17.3%) | 68 (25.6%) | 191 (43.5%) | 71.08 # | <0.001 * |
| Postpartum | 325 (82.7%) | 198 (74.4%) | 248 (56.5%) | ||
| Magnetic resonance imaging results | |||||
| Normal result | 2 (11.1%) | 0 (0%) | 2 (10.5%) | ||
| Altered result, suggestive of infection | 12 (66.7%) | 0 (0%) a | 16 (84.2%) b | 20.5 # | 0.002 * |
| Altered result, with other changes | 3 (16.7%) | 3 (100%) a | 0 (0%) b | ||
| Indeterminate result | 1 (5.6%) | 0 (0%) | 1 (5.3%) | ||
| Ultrasonography Transfontanela Result | |||||
| Normal result | 36 (41.9%) a | 50 (83.3%) b | 123 (76.9%) b | ||
| Altered result, suggestive of congenital infection | 40 (46.5%) a | 7 (11.7%) b | 25 (15.6%) b | 41.95 # | <0.001 * |
| Altered result, with other changes | 8 (9.3%) | 2 (3.3%) | 9 (5.6%) | ||
| Indeterminate result | 2 (2.3%) | 1 (1.7%) | 3 (1.9%) | ||
| CT scan result | |||||
| Normal result | 46 (23.1%) a | 55 (62.5%) b | 136 (53.3%) b | ||
| Altered result, suggestive of congenital infection | 142 (71.4%) a | 26 (29.5%) b | 84 (32.9%) b | 82.86 # | <0.001 * |
| Altered result, with other changes | 9 (4.5%) a | 7 (8%) | 30 (11.8%) b | ||
| Indeterminate result | 2 (1%) | 0 (0%) | 5 (2%) | ||
| Ultrasonography result | |||||
| Normal result | 34 (40%) a | 34 (72.3%) b | 48 (56.5%) | ||
| Altered result, suggestive of infection | 32 (37.6%) a | 6 (12.8%) b | 16 (18.8%) | 17.774 # | 0.007 * |
| Altered result, with other changes | 9 (10.6%) | 2 (4.3%) | 10 (11.8%) | ||
| Indeterminate result | 10 (11.8%) | 5 (10.6%) | 11 (12.9%) |
| 1 Infection (n = 1457) | 2 Infections (n = 56) | χ2, Fisher’s Exact Test or Mann–Whitney U | p-Value | |
|---|---|---|---|---|
| Newborn weight ¬ | 2520 (726) | 2655 (870) | 286.443.500 | 0.251 |
| Cephalic diameter ¬ | 30.00 (3) | 30.50 (4) | 27.105 | 0.109 |
| Neurological Disability | ||||
| Yes | 22 (1.5%) | 2 (3.6%) | 1467 º | 0.226 |
| No | 1435 (98.5%) | 54 (96.4%) | ||
| Visual Impairment | ||||
| Yes | 29 (2%) | 2 (3.6%) | 0.671 º | 0.413 |
| No | 1428 (98%) | 54 (96.4%) | ||
| Hearing Impairment | ||||
| Yes | 10 (0.7%) | 0 (0%) | 0.387 º | 0.534 |
| No | 1447 (%) | 56 (100%) | ||
| Detection Type | ||||
| Intrauterine (during pregnancy) | 327 (29.8%) | 18 (39.1%) | 1831 # | 0.176 |
| Postpartum | 771 (70.2%) | 28 (60.9%) | ||
| Magnetic resonance imaging results | ||||
| Normal result | 4 (10%) | 1 (100%) | ||
| Altered result, suggestive of infection | 28 (70%) | 0 (0%) | 7380 # | 0.061 |
| Altered result, with other changes | 6 (15%) | 0 (0%) | ||
| Indeterminate result | 2 (5%) | 0 (0%) | ||
| Ultrasonography | ||||
| Normal result | 116 (53.5%) | 7 (58.3%) | ||
| Altered result, suggestive of congenital infection | 54 (24.9%) | 3 (25%) | 0.200 # | 0.978 |
| Altered result, with other changes | 21 (9.7%) | 1 (8.3%) | ||
| Indeterminate result | 26 (12%) | 1 (8.3%) | ||
| Ultrasonography Transfontanela Result | ||||
| Normal result | 209 (68.3%) | 10 (71.4%) | ||
| Altered result, suggestive of congenital infection | 72 (23.5%) | 3 (21.4%) | 0.338 # | 0.953 |
| Altered result, with other changes | 19 (6.2%) | 1 (7.1%) | ||
| Indeterminate result | 6 (2%) | 0 (0%) | ||
| CT scan result | ||||
| Normal result | 237 (43.7%) | 11 (44%) | ||
| Altered result, suggestive of congenital infection | 252 (46.5%) | 11 (44%) | 0.697 # | 0.874 |
| Altered result, with other changes | 46 (8.5%) | 3 (12%) | ||
| Indeterminate result | 7 (1.3%) | 0 (0%) |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Ferreira, A.P.; Santana, D.S.; Figueiredo, E.R.L.; Simões, M.C.; de Morais, D.F.; Tavares, V.B.; de Sousa, J.G.; Silva, M.J.A.; de Campos Gomes, F.; de Melo Neto, J.S. Sociodemographic and Clinical Factors for Microcephaly Secondary to Teratogenic Infections in Brazil: An Ecological Study. Viruses 2023, 15, 1675. https://doi.org/10.3390/v15081675
Ferreira AP, Santana DS, Figueiredo ERL, Simões MC, de Morais DF, Tavares VB, de Sousa JG, Silva MJA, de Campos Gomes F, de Melo Neto JS. Sociodemographic and Clinical Factors for Microcephaly Secondary to Teratogenic Infections in Brazil: An Ecological Study. Viruses. 2023; 15(8):1675. https://doi.org/10.3390/v15081675
Chicago/Turabian StyleFerreira, Arlison Pereira, Davi Silva Santana, Eric Renato Lima Figueiredo, Marcelo Coelho Simões, Dionei Freitas de Morais, Victória Brioso Tavares, Juliana Gonçalves de Sousa, Marcos Jessé Abrahão Silva, Fabiana de Campos Gomes, and João Simão de Melo Neto. 2023. "Sociodemographic and Clinical Factors for Microcephaly Secondary to Teratogenic Infections in Brazil: An Ecological Study" Viruses 15, no. 8: 1675. https://doi.org/10.3390/v15081675
APA StyleFerreira, A. P., Santana, D. S., Figueiredo, E. R. L., Simões, M. C., de Morais, D. F., Tavares, V. B., de Sousa, J. G., Silva, M. J. A., de Campos Gomes, F., & de Melo Neto, J. S. (2023). Sociodemographic and Clinical Factors for Microcephaly Secondary to Teratogenic Infections in Brazil: An Ecological Study. Viruses, 15(8), 1675. https://doi.org/10.3390/v15081675







