High Incidence of Respiratory Syncytial Virus in Children with Community-Acquired Pneumonia from a City in the Brazilian Pre-Amazon Region
Abstract
1. Introduction
2. Materials and Methods
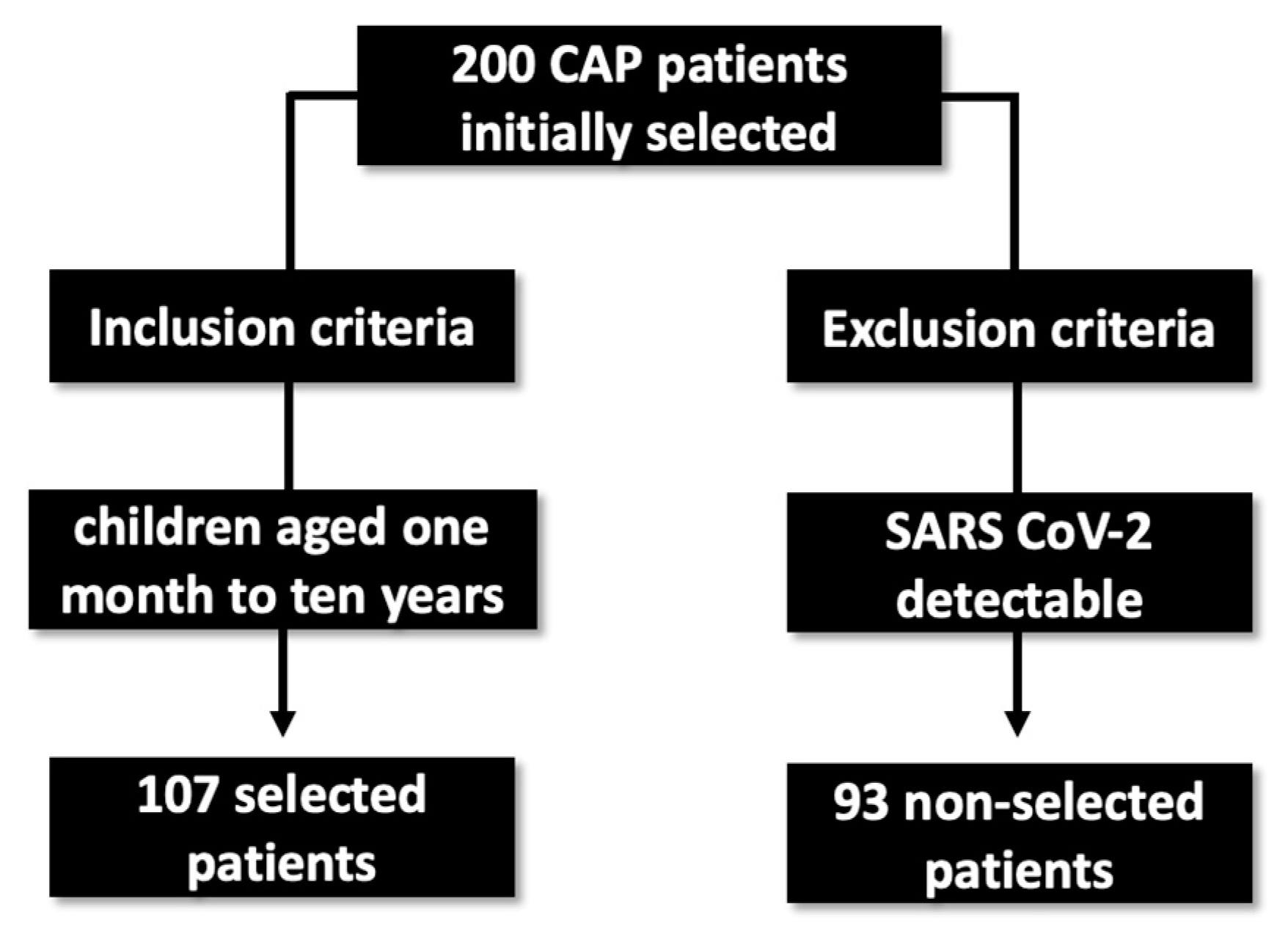
2.1. Study Population
2.2. Ethical Approval and Consent to Participate
2.3. Data Collection
2.4. Biological Samples
2.5. Nucleic Acid Extraction
2.6. Molecular Analysis
2.7. Statistical Analysis
3. Results
3.1. Clinical and Epidemiological Data
3.2. Viral Detection
3.3. Clinical Profile of Children with RSV
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Bruce, C.S.; Hoare, C.; Mukherjee, A.; Paul, S.P. Managing acute respiratory tract infections in children. Br. J. Nurs. 2017, 26, 602–609. [Google Scholar] [CrossRef]
- GBD 2016 Lower Respiratory Infections Collaborators. Estimates of the global, regional, and national morbidity, mortality, and aetiologies of lower respiratory infections in 195 countries, 1990–2016: A systematic analysis for the Global Burden of Disease Study 2016. Lancet Infect. Dis. 2018, 18, 1191–1210. [Google Scholar] [CrossRef] [PubMed]
- Collaborators GBDCoD. Global, regional, and national age-sex-specific mortality for 282 causes of death in 195 countries and territories, 1980–2017: A systematic analysis for the Global Burden of Disease Study 2017; GBD 2017 Causes of Death Collaborators. Lancet 2018, 392, 1736–1788. [Google Scholar] [CrossRef] [PubMed]
- Rudan, I.; O’brien, K.L.; Nair, H.; Liu, L.; Theodoratou, E.; Qazi, S.; Lukšić, I.; Walker, C.L.F.; Black, R.E.; Campbell, H. Epidemiology and etiology of childhood pneumonia in 2010: Estimates of incidence, severe morbidity, mortality, underlying risk factors and causative pathogens for 192 countries. J. Glob. Health 2013, 3, 010401. [Google Scholar] [PubMed]
- DeAntonio, R.; Yarzabal, J.-P.; Cruz, J.P.; Schmidt, J.E.; Kleijnen, J. Epidemiology of community-acquired pneumonia and implications for vaccination of children living in developing and newly industrialized countries: A systematic literature review. Hum. Vaccines Immunother. 2016, 12, 2422–2440. [Google Scholar] [CrossRef] [PubMed]
- Sonego, M.; Pellegrin, M.C.; Becker, G.; Lazzerini, M. Risk Factors for Mortality from Acute Lower Respiratory Infections (ALRI) in Children under Five Years of Age in Low and Middle-Income Countries: A Systematic Review and Meta-Analysis of Observational Studies. PLoS ONE 2015, 10, e0116380. [Google Scholar] [CrossRef]
- Huang, H.-S.; Tsai, C.-L.; Chang, J.; Hsu, T.-C.; Lin, S.; Lee, C.-C. Multiplex PCR system for the rapid diagnosis of respiratory virus infection: Systematic review and meta-analysis. Clin. Microbiol. Infect. 2017, 24, 1055–1063. [Google Scholar] [CrossRef]
- Wang, L.; Cheng, G. Sequence analysis of the emerging SARS-CoV-2 variant Omicron in South Africa. J. Med. Virol. 2021, 94, 1728–1733. [Google Scholar] [CrossRef] [PubMed]
- Ferreira, H.L.D.S.; Costa, K.L.P.; Cariolano, M.D.S.; Oliveira, G.S.; Felipe, K.K.P.; Silva, E.S.A.; Alves, M.S.; Maramaldo, C.E.C.; De Sousa, E.M.; Rego, J.S.; et al. High incidence of rhinovirus infection in children with community-acquired pneumonia from a city in the Brazilian pre-Amazon region. J. Med. Virol. 2019, 91, 1751–1758. [Google Scholar] [CrossRef]
- Corrêa, R.D.A.; Costa, A.N.; Lundgren, F.; Michelin, L.; Figueiredo, M.R.; Holanda, M.; Gomes, M.; Teixeira, P.J.Z.; Martins, R.; Silva, R.; et al. 2018 recommendations for the management of community acquired pneumonia. J. Bras. Pneumol. 2018, 44, 405–423. [Google Scholar] [CrossRef]
- Li, Y.; Reeves, R.M.; Wang, X.; Bassat, Q.; Brooks, W.A.; Cohen, C.; Moore, D.P.; Nunes, M.; Rath, B.; Campbell, H.; et al. Global patterns in monthly activity of influenza virus, respiratory syncytial virus, parainfluenza virus, and metapneumovirus: A systematic analysis. Lancet Glob. Health 2019, 7, e1031–e1045. [Google Scholar] [CrossRef]
- Negro, R.W.D.; Zanasi, A.; Turco, P.; Povero, M. Acute cough in Italian children: Parents’ beliefs, approach to treatment, and the family impact. Multidiscip. Respir. Med. 2019, 14, 16. [Google Scholar] [CrossRef]
- Martins, S.; De Moura, M.C.; Neves, A.M.; Trindade, J.C. Cough in paediatrics. Rev. Port. Pneumol. 2008, 14, 517–526. [Google Scholar] [CrossRef] [PubMed]
- Li, X.; Li, J.; Meng, L.; Zhu, W.; Liu, X.; Yang, M.; Yu, D.; Niu, L.; Shen, X. Viral etiologies and epidemiology of patients with acute respiratory infections based on sentinel hospitals in Gansu Province, Northwest China, 2011–2015. J. Med. Virol. 2018, 90, 828–835. [Google Scholar] [CrossRef] [PubMed]
- Bont, L.; Checchia, P.A.; Fauroux, B.; Figueras-Aloy, J.; Manzoni, P.; Paes, B.; Simões, E.A.F.; Carbonell-Estrany, X. Defining the Epidemiology and Burden of Severe Respiratory Syncytial Virus Infection Among Infants and Children in Western Countries. Infect. Dis. Ther. 2016, 5, 271–298. [Google Scholar] [CrossRef]
- Cattoir, L.; Vankeerberghen, A.; Boel, A.; Van Vaerenbergh, K.; De Beenhouwer, H. Epidemiology of RSV and hMPV in Belgium: A 10-year follow-up. Acta Clin. Belg. 2018, 74, 229–235. [Google Scholar] [CrossRef] [PubMed]
- Gentile, A.; Lucion, M.F.; Juárez, M.D.V.; Castellano, V.; Bakir, J.; Pacchiotti, A.; Areso, M.S.; Viegas, M.; Goya, S.; Mistchenko, A. Respiratory syncytial virus in preterm infants: 19 years of active epidemiological surveillance in a children’s hospital. Arch. Argent. Pediatr. 2020, 118, 386–392. [Google Scholar] [CrossRef]
- Zurita-Cruz, J.N.; Gutierrez-Gonzalez, A.; Manuel-Apolinar, L.; Fernández-Gárate, J.E.; Arellano-Flores, M.L.; Gonzalez, R.A.C.; Vázquez-Rosales, G.; Sanchez-Armas, R.; Cisneros-González, N. Hospitalizations for viral respiratory infections in children under 2 years of age: Epidemiology and in-hospital complications. BMC Pediatr. 2020, 20, 285. [Google Scholar] [CrossRef]
- Yan, X.; Li, Y.; Tang, Y.; Xie, Z.; Gao, H.; Yang, X.; Liu, L.; Duan, Z. Clinical characteristics and viral load of respiratory syncytial virus and human metapneumovirus in children hospitaled for acute lower respiratory tract infection. J. Med. Virol. 2017, 89, 589–597. [Google Scholar] [CrossRef] [PubMed]
- Britton, P.N.; Hu, N.; Saravanos, G.; Shrapnel, J.; Davis, J.; Snelling, T.; Dalby-Payne, J.; Kesson, A.M.; Wood, N.; Macartney, K.; et al. COVID-19 public health measures and respiratory syncytial virus. Lancet Child Adolesc. Health 2020, 4, e42–e43. [Google Scholar] [CrossRef]
- Oz-Alcalay, L.; Ashkenazi, S.; Glatman-Freedman, A.; Weisman-Demri, S.; Lowenthal, A.; Livni, G. Hospitalization for Respiratory Syncytial Virus Bronchiolitis in the Palivizumab Prophylaxis Era: Need for Reconsideration of Preventive Timing and Eligibility. Isr. Med. Assoc. J. IMAJ 2019, 21, 110–115. [Google Scholar]
- Pierangeli, A.; Scagnolari, C.; Antonelli, G. Respiratory syncytial virus. Minerva Pediatr. 2018, 70, 553–565. [Google Scholar] [CrossRef] [PubMed]
- Ozdemir, S.A.; Soysal, B.; Calkavur, S.; Yıldırım, T.G.; Kıymet, E.; Kalkanlı, O.; Çolak, R.; Devrim, I. Is respiratory syncytial virus infection more dangerous than COVID 19 in the neonatal period? J. Matern. Neonatal Med. 2020, 35, 4398–4403. [Google Scholar] [CrossRef] [PubMed]
- Robbie, G.J.; Criste, R.; Dall’acqua, W.F.; Jensen, K.; Patel, N.K.; Losonsky, G.A.; Griffin, M.P. A novel investigational Fc-modified humanized monoclonal antibody, motavizumab-YTE, has an extended half-life in healthy adults. Antimicrob. Agents Chemother. 2013, 57, 6147–6153. [Google Scholar] [CrossRef]
- Passos, S.D.; Maziero, F.F.; Antoniassi, D.Q.; Souza, L.T.D.; Felix, A.F.; Dotta, E.; Orensztejn, M.E.; Marchi, E.; Gazeta, R.E. Acute Respiratory Diseases in Brazilian Children: Are Caregivers Able to Detect Early Warning Signs? Rev. Paul Pediatr. 2018, 36, 7. [Google Scholar] [CrossRef] [PubMed]
- Choi, E.; Ha, K.-S.; Song, D.J.; Lee, J.H.; Lee, K.C. Clinical and laboratory profiles of hospitalized children with acute respiratory virus infection. Korean J. Pediatr. 2018, 61, 180–186. [Google Scholar] [CrossRef]
- Chen, J.; Hu, P.; Zhou, T.; Zheng, T.; Zhou, L.; Jiang, C.; Pei, X. Epidemiology and clinical characteristics of acute respiratory tract infections among hospitalized infants and young children in Chengdu, West China, 2009–2014. BMC Pediatr. 2018, 18, 216. [Google Scholar] [CrossRef]
- Lopes, G.P.; Amorim, P.S.; de Melo, B.D.O.; Maramaldo, C.E.C.; Bomfim, M.R.Q.; Neto, L.G.L.; Alves, M.S.; Silva, F.B.; Soeiro-Pereira, P.V.; Falcai, A. Identification and seasonality of rhinovirus and respiratory syncytial virus in asthmatic children in tropical climate. Biosci. Rep. 2020, 40, BSR20200634. [Google Scholar] [CrossRef]
- Morley, C.; Grimwood, K.; Maloney, S.; Ware, R.S. Meteorological factors and respiratory syncytial virus seasonality in subtropical Australia. Epidemiol. Infect. 2018, 146, 757–762. [Google Scholar] [CrossRef]
- Chi, H.; Chung, C.-H.; Lin, Y.-J.; Lin, C.-H. Seasonal peaks and risk factors of respiratory syncytial virus infections related hospitalization of preterm infants in Taiwan. PLoS ONE 2018, 13, e0197410. [Google Scholar] [CrossRef]
- Janet, S.; Broad, J.; Snape, M.D. Respiratory syncytial virus seasonality and its implications on prevention strategies. Hum. Vaccines Immunother. 2018, 14, 234–244. [Google Scholar] [CrossRef] [PubMed]
- Obando-Pacheco, P.; Justicia-Grande, A.J.; Rivero-Calle, I.; Rodríguez-Tenreiro, C.; Sly, P.; Ramilo, O.; Mejías, A.; Baraldi, E.; Papadopoulos, N.G.; Nair, H.; et al. Respiratory Syncytial Virus Seasonality: A Global Overview. J. Infect. Dis. 2018, 217, 1356–1364. [Google Scholar] [CrossRef] [PubMed]
- Coppée, R.; Chenane, H.R.; Bridier-Nahmias, A.; Tcherakian, C.; Catherinot, E.; Collin, G.; Lebourgeois, S.; Visseaux, B.; Descamps, D.; Vasse, M.; et al. Temporal dynamics of RSV shedding and genetic diversity in adults during the COVID-19 pandemic in a French hospital, early 2021. Virus Res. 2023, 323, 198950. [Google Scholar] [CrossRef] [PubMed]
- Leli, C.; Di Matteo, L.; Gotta, F.; Vay, D.; Piceghello, A.; Cornaglia, E.; Cavallo, V.; Busso, S.; Carrabba, L.; Mazzeo, R.; et al. Prevalence of respiratory viruses by Multiplex PCR: A four-and-a-half year retrospective study in an Italian general hospital. Infez Med. 2021, 29, 94–101. [Google Scholar] [PubMed]
- Le Glass, E.; Hoang, V.T.; Boschi, C.; Ninove, L.; Zandotti, C.; Boutin, A.; Bremond, V.; Dubourg, G.; Ranque, S.; Lagier, J.-C.; et al. Incidence and Outcome of Coinfections with SARS-CoV-2 and Rhinovirus. Viruses 2021, 13, 2528. [Google Scholar] [CrossRef]
- Krammer, F.; Smith, G.J.D.; Fouchier, R.A.M.; Peiris, M.; Kedzierska, K.; Doherty, P.C.; Palese, P.; Shaw, M.L.; Treanor, J.; Webster, R.G.; et al. Influenza. Nat. Rev. Dis. Prim. 2018, 4, 3. [Google Scholar] [CrossRef] [PubMed]
- Barrezueta, L.B.; Zamorano, M.G.; López-Casillas, P.; Brezmes-Raposo, M.; Fernández, I.S.; Vázquez, M.D.L.A.P. Influence of the COVID-19 pandemic on the epidemiology of acute bronchiolitis. Enferm. Infecc. Microbiol. Clin. 2022; 1–4, in press. [Google Scholar] [CrossRef] [PubMed]
- Ma, J.E.; Ma, Q.F.; Wang, W.; Gentile, A.; Lucion, M.F.; Juarez, M.D.V.; Zeng, Y.; Cui, X.; Wang, G.; Liu, S.; et al. Analysis of Common Respiratory Infected Pathogens in 3100 Children after the Coronavirus Disease 2019 Pandemic. Curr. Med. Sci. 2022, 42, 1094–1098. [Google Scholar] [CrossRef]
- Simões, E.A.F.; Bont, L.; Manzoni, P.; Fauroux, B.; Paes, B.; Figueras-Aloy, J.; Checchia, P.A.; Carbonell-Estrany, X. Past, Present and Future Approaches to the Prevention and Treatment of Respiratory Syncytial Virus Infection in Children. Infect. Dis. Ther. 2018, 7, 87–120. [Google Scholar] [CrossRef]
- Jackson, D.J.; Makrinioti, H.; Rana, B.M.J.; Shamji, B.W.H.; Trujillo-Torralbo, M.-B.; Footitt, J.; Del-Rosario, J.; Telcian, A.G.; Nikonova, A.; Zhu, J.; et al. IL-33–Dependent Type 2 Inflammation during Rhinovirus-induced Asthma Exacerbations In Vivo. Am. J. Respir. Crit. Care Med. 2014, 190, 1373–1382. [Google Scholar] [CrossRef]
- Alvarez, A.E.; Marson, F.A.L.; Bertuzzo, C.S.; Arns, C.W.; Ribeiro, J.D. Características epidemiológicas e genéticas associadas à gravidade da bronquiolite viral aguda pelo vírus sincicial respiratório. J. Pediatr. 2013, 89, 531–543. [Google Scholar] [CrossRef] [PubMed]
- Blanken, M.O.; Rovers, M.M.; Molenaar, J.M.; Winkler-Seinstra, P.L.; Meijer, A.; Kimpen, J.L.; Bont, L. Respiratory Syncytial Virus and Recurrent Wheeze in Healthy Preterm Infants. N. Engl. J. Med. 2013, 368, 1791–1799. [Google Scholar] [CrossRef] [PubMed]
- Brasil—Ministério da Saúde. Palivizumabe para a Prevenção da Infecção pelo Vírus Sincicial Respiratório. Relatório de Recomendação da Comissão Nacional de Incorporação de Tecnologias no SUS (CONITEC) 2012. Available online: http://conitec.gov.br/images/Incorporados/Palivizumabe-VirusSincicial-final.pdf (accessed on 3 March 2022).
- Brasil—Ministério da Saúde. Protocolo de Uso do Palivizumabe para a Prevenção da Infecção pelo Vírus Sincicial Respiratório. 2018. Available online: https://www.in.gov.br/web/guest/materia/-/asset_publisher/Kujrw0TZC2Mb/content/id/44708464/ (accessed on 3 March 2022).
- Ministério da Saúde. Estabelecer a Sazona-Lidade do Vírus Sincicial Respiratório no Brasil e Oferecer Esclarecimentos Referentes ao Protocolo de Uso do Palivizumabe; Nota Técnica Conjunta No 05/2015; de 09 de Fevereiro de 2015; Ministério da Saúde: Brasilia, Brazil, 2015.
| Variables | CAP (n = 107) | Severe CAP (n = 14) | Non-Severe CAP (n = 93) | p * |
|---|---|---|---|---|
| Age (>24 months) | 80 (74.8%) | 10 (71.4%) | 70 (75.3%) | 0.999 |
| Male gender | 53 (49.5%) | 7 (50.0%) | 46 (49.5%) | 0.999 |
| Cough | 74 (69.1%) | 14 (100.0%) | 60 (64.5%) | 0.004 * |
| Fever | 68 (63.5%) | 11 (78.6%) | 57 (61.3%) | 0.249 |
| Tiredness | 51 (47.6%) | 10 (71.4%) | 41 (44.1%) | 0.083 |
| Expectoration | 48 (44.8%) | 9 (64.3%) | 39 (41.9%) | 0.758 |
| Snoring | 37 (34.6%) | 9 (64.3%) | 28 (30.1%) | 0.017 * |
| Dyspnea | 49 (45.8%) | 9 (64.3%) | 40 (43.0%) | 0.159 |
| Tachypnea | 35 (32.7%) | 7 (50.0%) | 28 (30.1%) | 0.219 |
| Runny nose | 30 (28.0%) | 5 (35.7%) | 25 (26.9%) | 0.529 |
| Vomiting | 31 (29.0%) | 4 (28.6%) | 27 (29.0%) | 0.999 |
| Nasal obstruction | 7 (6.5%) | 4 (28.6%) | 3 (3.2%) | 0.005 * |
| Diarrhea | 7 (6.5%) | 3 (21.4%) | 4 (4.3%) | 0.046 * |
| Wheezing | 28 (26.2%) | 2 (14.3%) | 26 (28.0%) | 0.347 |
| Cyanosis | 7 (6.5%) | 2 (14.3%) | 5 (5.4%) | 0.227 |
| Abdominal pain | 6 (5.6%) | 2 (14.3%) | 4 (4.3%) | 0.175 |
| Congenital heart disease | 8 (7.5%) | 1 (7.1%) | 7 (7.5%) | 0.999 |
| Hematological diseases | 1 (0.9%) | 1 (7.1%) | 0 (0.0%) | 0.13 |
| Prematurity | 12 (11.2%) | 0 (0.0%) | 12 (12.9%) | 0.359 |
| Neurological diseases | 1 (0.9%) | 1 (7.1%) | 0 (0.0%) | 0.13 |
| Chronic kidney disease | 3 (2.8%) | 0 (0.0%) | 3 (3.2%) | 0.999 |
| Chronic liver disease | 4 (3.7%) | 0 (0.0%) | 4 (4.3%) | 0.999 |
| Asthma | 1 (0.9%) | 0 (0.0%) | 1 (1.1%) | 0.999 |
| Visceral leishmaniasis | 4 (3.7%) | 1 (7.1%) | 3 (3.2%) | 0.434 |
| Pulmonary tuberculosis | 2 (1.9%) | 0 (0.0%) | 2 (2.1%) | 0.999 |
| HIV infection | 1 (0.9%) | 0 (0.0%) | 1 (1.1%) | 0.999 |
| Mesenteric cyst | 1 (0.9%) | 0 (0.0%) | 1 (1.1%) | 0.999 |
| Absence of comorbidity | 62 (57.9%) | 10 (71.4%) | 52 (55.9%) | 0.386 |
| Virus Positivity | CAP, n = 107 | Severe CAP, n = 14 | Non-Severe IRA, n = 93 | p * |
|---|---|---|---|---|
| RSV | 70 (65.4) | 13 (92.8%) | 57 (61.2%) | 0.031 |
| HVSR A | 2 (1.9%) | 0 (0.0%) | 2 (2.1%) | 1 |
| HVSR B | 68 (63.5%) | 13 (92.8%) | 55 (59.1%) | 0.016 |
| Rhinovirus | 4 (3.7%) | 1 (7.1%) | 3 (3.2%) | 0.434 |
| FluA | ND | ND | ND | -- |
| FluB | ND | ND | ND | -- |
| HADV | ND | ND | ND | -- |
| HMPV | ND | ND | ND | -- |
| HCoV 229E | 7 (6.5%) | 3 (21.4%) | 4 (4.3%) | 0.046 |
| HCoV NL63 | ND | ND | ND | -- |
| HCoV OC43 | ND | ND | ND | -- |
| HCoV HKU1 | ND | ND | ND | -- |
| HPIV 1 | ND | ND | ND | -- |
| HPIV 2 | ND | ND | ND | -- |
| HPIV 3 | ND | ND | ND | -- |
| Coinfections | 7 (6.5%) | 3 (21.4%) | 4 (4.3%) | 0.046 |
| No virus detected | 33 (30.8%) | 0 (0.0%) | 33 (35.5%) | 1.000 |
| Variables | Total CAP (n = 107) | VSR Detected (n = 66) | VSR Not Detected (n = 41) | p * |
|---|---|---|---|---|
| Young age, % | 80 (74.7%) | 55 (83.3%) | 25 (60.9%) | 0.012 * |
| Cough | 74 (69.1%) | 55 (83.3%) | 19 (46.3%) | <0.0001 * |
| Fever | 68 (63.5%) | 49 (74.2%) | 19 (46.3%) | 0.006 * |
| Tiredness | 51 (47.6%) | 39 (59.1%) | 12 (29.3%) | 0.003 * |
| Expectoration | 48 (44.8%) | 38 (57.6%) | 10 (24.4%) | <0.001 * |
| Snoring | 37 (34.6%) | 37 (56.1%) | 0 (0.0%) | <0.0001 * |
| Dyspnea | 49 (45.8%) | 28 (42.4%) | 21 (51.2%) | 0.427 |
| Tachypnoea | 35 (32.7%) | 27 (40.9%) | 8 (19.5%) | 0.033 * |
| Runny nose | 30 (28.0%) | 21 (31.8%) | 9 (21.9%) | 0.376 |
| Vomiting | 31 (29.0%) | 26 (39.4%) | 5 (12.2%) | 0.003 * |
| Nasal obstruction | 7 (6.5%) | 6 (9.1%) | 1 (2.4%) | 0.246 |
| Diarrhea | 7 (6.5%) | 7 (10.6%) | 0 (0.0%) | 0.042 * |
| Wheezing | 28 (26.2%) | 20 (30.3%) | 8 (19.5%) | 0.262 |
| Cyanosis | 7 (6.5%) | 4 (6.1%) | 3 (7.3%) | >0.999 |
| Abdominal pain | 6 (5.6%) | 3 (4.5%) | 3 (7.3%) | 0.673 |
| Congenital heart disease | 12 (11.2%) | 7 (10.6%) | 5 (12.2%) | >0.999 |
| Hematological diseases | 13 (12.1%) | 10 (15.1%) | 3 (7.3%) | 0.362 |
| Prematurity | 12 (11.2%) | 12 (18.2%) | 0 (0.0%) | 0.003 * |
| Neurological diseases | 8 (7.5%) | 1 (1.5%) | 7 (17.1%) | 0.004 * |
| Cough | 2 (1.9%) | 0 (0.0%) | 2 (4.9%) | 0.144 |
| Fever | 12 (11.2%) | 7 (10.6%) | 5 (12.2%) | >0.999 |
| Tiredness | 1 (0.9%) | 0 (0.0%) | 1 (2.4%) | 0.383 |
| Chronic kidney disease | 3 (2.8%) | 1 (1.5%) | 2 (4.9%) | 0.556 |
| Chronic liver disease | 4 (3.7%) | 0 (0.0%) | 3 (7.3%) | 0.144 |
| Asthma | 1 (0.9%) | 0 (0.0%) | 1 (2.4%) | 0.383 |
| Visceral leishmaniasis | 4 (3.7%) | 1 (1.5%) | 3 (7.3%) | 0.156 |
| Pulmonary tuberculosis | 2 (1.9%) | 0 (0.0%) | 2 (4.9%) | 0.144 |
| Mesenteric cyst | 1 (0.9%) | 0 (0.0%) | 1 (2.4%) | 0.383 |
| Absence of comorbidity | 62 (57.9%) | 51 (77.2%) | 11 (26.9%) | <0.0001 * |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Fontes, V.; Ferreira, H.; Ribeiro, M.; Pinheiro, A.; Maramaldo, C.; Pereira, E.; Batista, L.; Júnior, A.; Lobato, L.; Silva, F.; et al. High Incidence of Respiratory Syncytial Virus in Children with Community-Acquired Pneumonia from a City in the Brazilian Pre-Amazon Region. Viruses 2023, 15, 1306. https://doi.org/10.3390/v15061306
Fontes V, Ferreira H, Ribeiro M, Pinheiro A, Maramaldo C, Pereira E, Batista L, Júnior A, Lobato L, Silva F, et al. High Incidence of Respiratory Syncytial Virus in Children with Community-Acquired Pneumonia from a City in the Brazilian Pre-Amazon Region. Viruses. 2023; 15(6):1306. https://doi.org/10.3390/v15061306
Chicago/Turabian StyleFontes, Valéria, Hivylla Ferreira, Marilene Ribeiro, Aruanã Pinheiro, Carlos Maramaldo, Eduardo Pereira, Luís Batista, Antonio Júnior, Luis Lobato, Fabiano Silva, and et al. 2023. "High Incidence of Respiratory Syncytial Virus in Children with Community-Acquired Pneumonia from a City in the Brazilian Pre-Amazon Region" Viruses 15, no. 6: 1306. https://doi.org/10.3390/v15061306
APA StyleFontes, V., Ferreira, H., Ribeiro, M., Pinheiro, A., Maramaldo, C., Pereira, E., Batista, L., Júnior, A., Lobato, L., Silva, F., Sousa, L., Lima, W., Lima, C., Soczek, S., Carvalho, R., Santos, M., Fernandes, E., Sousa, E., & Neto, L. (2023). High Incidence of Respiratory Syncytial Virus in Children with Community-Acquired Pneumonia from a City in the Brazilian Pre-Amazon Region. Viruses, 15(6), 1306. https://doi.org/10.3390/v15061306









