A Hierarchical Framework for Assessing Transmission Causality of Respiratory Viruses
Abstract
:1. Introduction
2. From Bacteriology to Virology
3. Hill’s Criteria
4. Gwaltney and Hendley Postulates
5. The Genomics Era
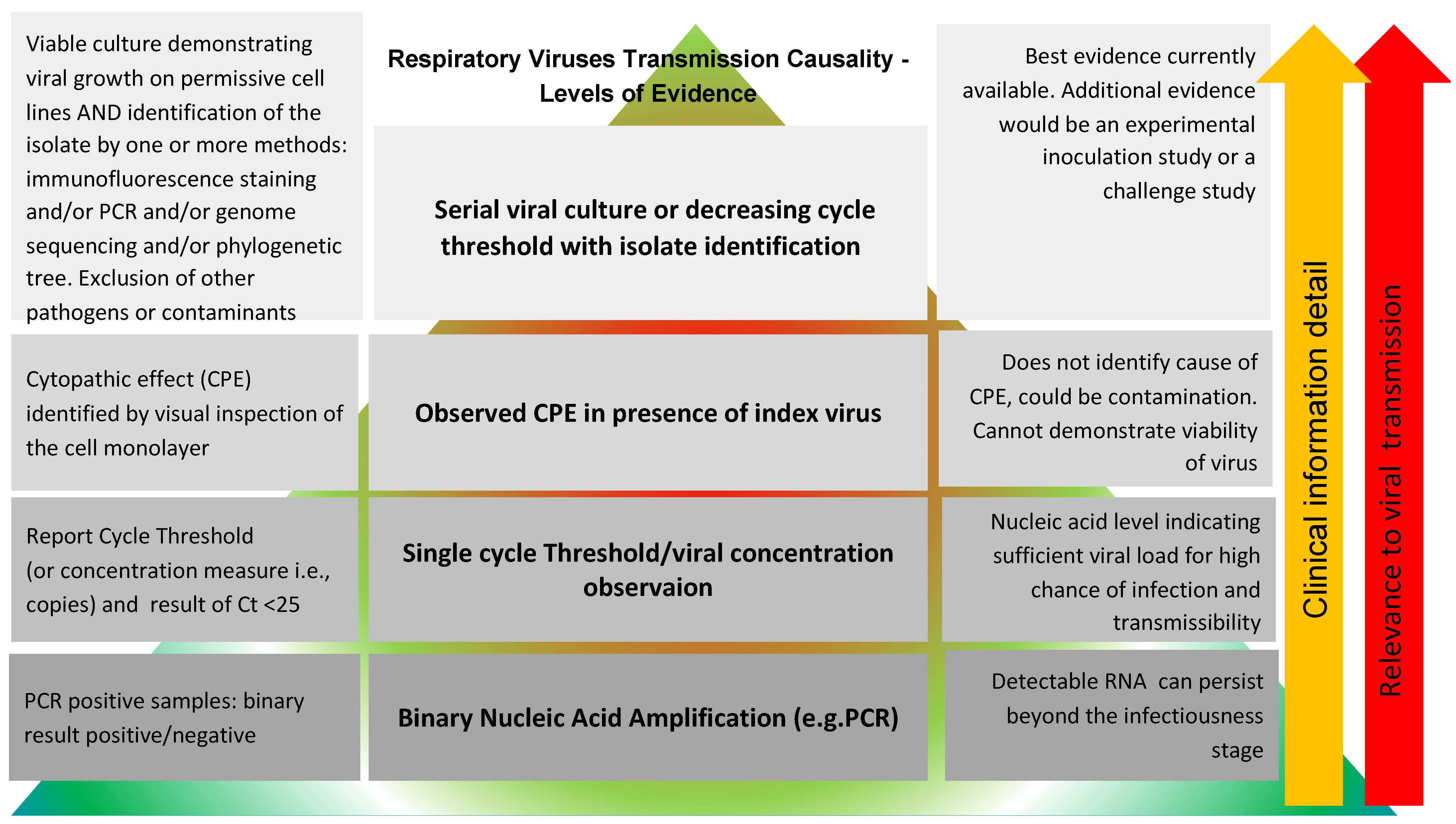
6. A Proposed Framework for Assessing Transmission Causality of Respiratory Viruses
- Level 1: Binary PCR or nucleic acid antigen result in the absence of clinical data.
- Level 2: Single Quantitative PCR result.
- Level 3: Cytopathic Effects (CPE).
- Level 4: Serial Viral Culture or validated viral load surrogate and genome sequencing.
7. Discussion
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Huebner, R.J. Criteria for etiologic association of prevalent viruses with prevalent diseases; the virologist’s dilemma. Ann. N. Y. Acad. Sci. 1957, 67, 430–438. [Google Scholar] [CrossRef] [PubMed]
- Dotto, L.; Kinalski, M.D.A.; Machado, P.S.; Pereira, G.K.R.; Sarkis-Onofre, R.; dos Santos, M.B.F. The mass production of systematic reviews about COVID-19: An analysis of PROSPERO records. J. Evid. Based Med. 2021, 14, 56–64. [Google Scholar] [CrossRef] [PubMed]
- Jung, R.G.; Di Santo, P.; Clifford, C.; Prosperi-Porta, G.; Skanes, S.; Hung, A.; Parlow, S.; Visintini, S.; Ramirez, F.D.; Simard, T.; et al. Methodological quality of COVID-19 clinical research. Nat. Commun. 2021, 12, 943. [Google Scholar] [CrossRef] [PubMed]
- Quinn, T.J.; Burton, J.K.; Carter, B.; Cooper, N.; Dwan, K.; Field, R.; Freeman, S.C.; Geue, C.; Hsieh, P.-H.; McGill, K.; et al. Following the science? Comparison of methodological and reporting quality of covid-19 and other research from the first wave of the pandemic. BMC Med. 2021, 19, 46. [Google Scholar] [CrossRef]
- Yang, S.; Li, A.; Eshaghpour, A.; Ivanisevic, S.; Salopek, A.; Eikelboom, J.; Crowther, M. Quality of early evidence on the pathogenesis, diagnosis, prognosis and treatment of COVID-19. BMJ Evid. Based Med. 2020, 26, 302–306. [Google Scholar] [CrossRef]
- Savvides, C.; Siegel, R. Asymptomatic and presymptomatic transmission of SARS-CoV-2: A systematic review. medRxiv 2020. [Google Scholar] [CrossRef]
- Zdravkovic, M.; Berger-Estilita, J.; Zdravkovic, B.; Berger, D. Scientific quality of COVID-19 and SARS CoV-2 publications in the highest impact medical journals during the early phase of the pandemic: A case control study. PLoS ONE 2020, 15, e0241826. [Google Scholar] [CrossRef]
- Fomenko, A.; Weibel, S.; Moezi, H.; Menger, K.; Schmucker, C.; Metzendorf, M.; Motschall, E.; Falcone, V.; Huzly, D.; Panning, M.; et al. Assessing severe acute respiratory syndrome coronavirus 2 infectivity by reverse-transcription polymerase chain reaction: A systematic review and meta-analysis. Rev. Med. Virol. 2022, e2342. [Google Scholar] [CrossRef]
- Heneghan, C.; Spencer, E.A.; Brassey, J.; Plüddemann, A.; Onakpoya, I.J.; Evans, D.H.; Conly, J.M.; Jefferson, T. SARS-CoV-2 and the role of orofecal transmission: A systematic review. F1000Research 2021, 10, 231. [Google Scholar] [CrossRef]
- Heneghan, C.; Spencer, E.A.; Brassey, J.; Plüddemann, A.; Onakpoya, I.J.; Evans, D.H.; Conly, J.M. SARS-CoV-2 and the role of airborne transmission: A systematic review. F1000Research 2021, 10, 232. [Google Scholar] [CrossRef]
- Onakpoya, I.J.; Heneghan, C.J.; Spencer, E.A.; Brassey, J.; Plüddemann, A.; Evans, D.H.; Conly, J.M.; Jefferson, T. SARS-CoV-2 and the role of fomite transmission: A systematic review. F1000Research 2021, 10, 233. [Google Scholar] [CrossRef] [PubMed]
- Onakpoya, I.J.; Heneghan, C.J.; Spencer, E.A.; Brassey, J.; Plüddemann, A.; Evans, D.H.; Conly, J.M.; Jefferson, T. SARS-CoV-2 and the Role of Close Contact in Transmission: A Systematic Review. F1000Research 2021, 10, 280. [Google Scholar] [CrossRef]
- Plüddemann, A.; Spencer, E.A.; Heneghan, C.; Brassey, J.; Onakpoya, I.J.; Rosca, E.C.; Evans, D.H.; Conly, J.M.; Jefferson, T. SARS-CoV-2 and the role of vertical transmission from infected pregnant women to their fetuses: Systematic review. medRxiv 2021. [Google Scholar] [CrossRef]
- Parascandola, J. Background to Robert Koch’s Lecture at the International Congress in Berlin, 1890; Springer: Berlin/Heidelberg, Germany, 1989. [Google Scholar]
- Halliday, S. Death and miasma in Victorian London: An obstinate belief. BMJ 2001, 323, 1469–1471. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Rivers, T.M. Viruses and Koch’s Postulates. J. Bacteriol. 1937, 33, 1–12. [Google Scholar] [CrossRef] [Green Version]
- Evans, A.S. Causation and disease: Effect of technology on postulates of causation. Yale J. Biol. Med. 1991, 64, 513–528. [Google Scholar]
- Hill, A.B. The Environment and Disease: Association or Causation? Proc. R. Soc. Med. 1965, 58, 295–300. [Google Scholar] [CrossRef] [Green Version]
- Gwaltney, J.M.; Hendley, J.O. Rhinovirus transmission: One if by air, two if by hand. Trans. Am. Clin. Climatol. Assoc. 1978, 89, 194–200. [Google Scholar]
- Leitner, T.; Escanilla, D.; Franzén, C.; Uhlén, M.; Albert, J. Accurate reconstruction of a known HIV-1 transmission history by phylogenetic tree analysis. Proc. Natl. Acad. Sci. USA 1996, 93, 10864–10869. [Google Scholar] [CrossRef] [Green Version]
- Fredericks, D.N.; Relman, D.A. Sequence-based identification of microbial pathogens: A reconsideration of Koch’s postulates. Clin. Microbiol. Rev. 1996, 9, 18–33. [Google Scholar] [CrossRef]
- Lipkin, W.I. The changing face of pathogen discovery and surveillance. Nat. Rev. Microbiol. 2013, 11, 133–144. [Google Scholar] [CrossRef] [PubMed]
- Byrd, A.L.; Segre, J.A. Adapting Koch’s postulates. Science 2016, 351, 224–226. [Google Scholar] [CrossRef]
- Jefferson, T.; Spencer, E.A.; Brassey, J.; Heneghan, C. Viral cultures for COVID-19 infectious potential assessment—A systematic review. Clin. Infect. Dis. 2020, 73, e3884–e3899. [Google Scholar] [CrossRef]
- Oxford Centre for Evidence Based Medicine Levels of Evidence Working Group. The Oxford Levels of Evidence 2. Oxford Centre for Evidence-Based Medicine. Available online: https://www.cebm.ox.ac.uk/resources/levels-of-evidence/ocebm-levels-of-evidence (accessed on 2 January 2022).
- Cevik, M.; Tate, M.; Lloyd, O.; Maraolo, A.E.; Schafers, J.; Ho, A. SARS-CoV-2, SARS-CoV, and MERS-CoV viral load dynamics, duration of viral shedding, and infectiousness: A systematic review and meta-analysis. Lancet Microbe 2021, 2, e13–e22. [Google Scholar] [CrossRef]
- Sepulcri, C.; Dentone, C.; Mikulska, M.; Bruzzone, B.; Lai, A.; Fenoglio, D.; Bozzano, F.; Bergna, A.; Parodi, A.; Altosole, T.; et al. The longest persistence of viable SARS-CoV-2 with recurrence of viremia and relapsing symptomatic COVID-19 in an immunocompromised patient—A case study. medRxiv 2021. [Google Scholar] [CrossRef] [PubMed]
- Rajakumar, I.A.-O.; Isaac, D.L.; Fine, N.M.; Clarke, B.; Ward, L.P.; Malott, R.J.; Pabbaraju, K.; Gill, K.; Berenger, B.M.; Lin, Y.-C.; et al. Extensive environmental contamination and prolonged severe acute respiratory coronavirus-2 (SARS CoV-2) viability in immunosuppressed recent heart transplant recipients with clinical and virologic benefit with remdesivir. Infect. Control. Hosp. Epidemiol. 2022, 43, 817–819. [Google Scholar] [CrossRef] [PubMed]
- Lednicky, J.A.; Shankar, S.N.; ElBadry, M.A.; Gibson, J.C.; Alam, M.; Stephenson, C.J.; Eiguren-Fernandez, A.; Morris, J.G.; Mavian, C.N.; Salemi, M.; et al. Collection of SARS-CoV-2 Virus from the Air of a Clinic within a University Student Health Care Center and Analyses of the Viral Genomic Sequence. Aerosol Air Qual. Res. 2020, 20, 1167–1171. [Google Scholar] [CrossRef]
- Cuypers, L.; Bode, J.; Beuselinck, K.; Laenen, L.; Dewaele, K.; Janssen, R.; Capron, A.; Lafort, Y.; Paridaens, H.; Bearzatto, B.; et al. Nationwide Harmonization Effort for Semi-Quantitative Reporting of SARS-CoV-2 PCR Test Results in Belgium. Viruses 2022, 14, 1294. [Google Scholar] [CrossRef]
- Kirby, J.E.; Cheng, A.; Cleveland, M.H.; Degli-Angeli, E.; DeMarco, C.T.; Faron, M.; Gallagher, T.L.; Garlick, R.K.; Goecker, E.; Coombs, R.W.; et al. A Multi-Institutional Study Benchmarking Cycle Threshold Values for Major Clinical SARS-CoV-2 RT-PCR Assays. medRxiv 2022. [Google Scholar] [CrossRef]
- Killingley, B.; Mann, A.J.; Kalinova, M.; Boyers, A.; Goonawardane, N.; Zhou, J.; Lindsell, K.; Hare, S.S.; Brown, J.; Frise, R.; et al. Safety, tolerability and viral kinetics during SARS-CoV-2 human challenge. Nat. Portf. 2022, 28, 1031–1041. [Google Scholar] [CrossRef]
- Bradburne, A.F.; Bynoe, M.L.; Tyrrell, D.A. Effects of a “new” human respiratory virus in volunteers. Br. Med. J. 1967, 3, 767–769. [Google Scholar] [CrossRef] [PubMed] [Green Version]
|
|
|
|
|
|
|
|
|
|
|
|
| Postulate Number One Microbial growth at the proposed anatomic site of origin. |
| Postulate Number Two Microbes present in secretions or tissues shed from the site of origin. |
| Postulate Number Three Microbes contaminate and survive in or on environmental substance or object. |
| Postulate Number Four Contaminated substance or object reaches portal of entry of new host. |
| Postulate Number Five Interruption of transmission by hypothesized route reduces incidence of natural infection. |
|
|
|
|
|
|
|
|
|
|
|
|
| Review | Primary Studies | PCR Result (% of Studies) | Ct (% of Studies) | Ct < 25 (% of Studies) | Attempted Viral Culture (% of Studies) | CPE (% of Studies) | Genome Sequencing (% of Studies) | Serial Viral Culture Positive (% of Studies) |
|---|---|---|---|---|---|---|---|---|
| Airborne Transmission [10] | 127 | 53 (79.1%) | 51 (40.2%) | 5 (3.9%) | 26 (20.4%) | 5 (3.7%) 1 | 6 (4.7%) | 3 (2.3%) 2 |
| Fomite Transmission [11] | 63 | 51 (81.0%) | 13 (20.6%) | 3 (4.8%) | 11 (17.5%) | 0 | 0 | 0 |
| Orofecal Transmission [9] | 77 | 46 (59.7%) | 22 (28.6%) | 7 (9.1%) | 6 (7.8%) | 1 (1.3%) 3 | 1 (1.3%) | 0 3 |
| Close Contact Transmission [12] | 258 | 163 (73.7%) | 26 (10.1%) | 6 (2.3%) | 4 (1.6%) | 2 (0.6%) | 18 (5.8%) | 2 (1.2%) |
| Vertical Transmission [13] | 66 | 66 (100%) | 9 (13.6%) | 2 (3.0%) | 0 | 0 | 1 (1.5%) | 0 |
| (% of primary studies) | 591 | 379 (64.1%) | 121 (20.5%) | 23 (3.9%) | 48 (8.1%) | 9 (1.5%) | 26 (4.4%) | 5 (0.85%) |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Jefferson, T.; Heneghan, C.J.; Spencer, E.; Brassey, J.; Plüddemann, A.; Onakpoya, I.; Evans, D.; Conly, J. A Hierarchical Framework for Assessing Transmission Causality of Respiratory Viruses. Viruses 2022, 14, 1605. https://doi.org/10.3390/v14081605
Jefferson T, Heneghan CJ, Spencer E, Brassey J, Plüddemann A, Onakpoya I, Evans D, Conly J. A Hierarchical Framework for Assessing Transmission Causality of Respiratory Viruses. Viruses. 2022; 14(8):1605. https://doi.org/10.3390/v14081605
Chicago/Turabian StyleJefferson, Tom, Carl J. Heneghan, Elizabeth Spencer, Jon Brassey, Annette Plüddemann, Igho Onakpoya, David Evans, and John Conly. 2022. "A Hierarchical Framework for Assessing Transmission Causality of Respiratory Viruses" Viruses 14, no. 8: 1605. https://doi.org/10.3390/v14081605
APA StyleJefferson, T., Heneghan, C. J., Spencer, E., Brassey, J., Plüddemann, A., Onakpoya, I., Evans, D., & Conly, J. (2022). A Hierarchical Framework for Assessing Transmission Causality of Respiratory Viruses. Viruses, 14(8), 1605. https://doi.org/10.3390/v14081605






