Cytomegalovirus Diseases of the Gastrointestinal Tract
Abstract
:1. Introduction
2. Materials and Methods
2.1. Patient
2.2. Data Collection
2.3. Definition of Immune Status
2.4. Statistical Analysis
2.5. Ethics
3. Results
3.1. Demographics and General Condition at Diagnosis
3.2. Underlying Diseases
3.3. Clinical Presentation and Diagnostic Work-Up
3.4. Treatment and Outcome
3.5. Prognostic Factors of In-Hospital Mortality and Survival Analysis
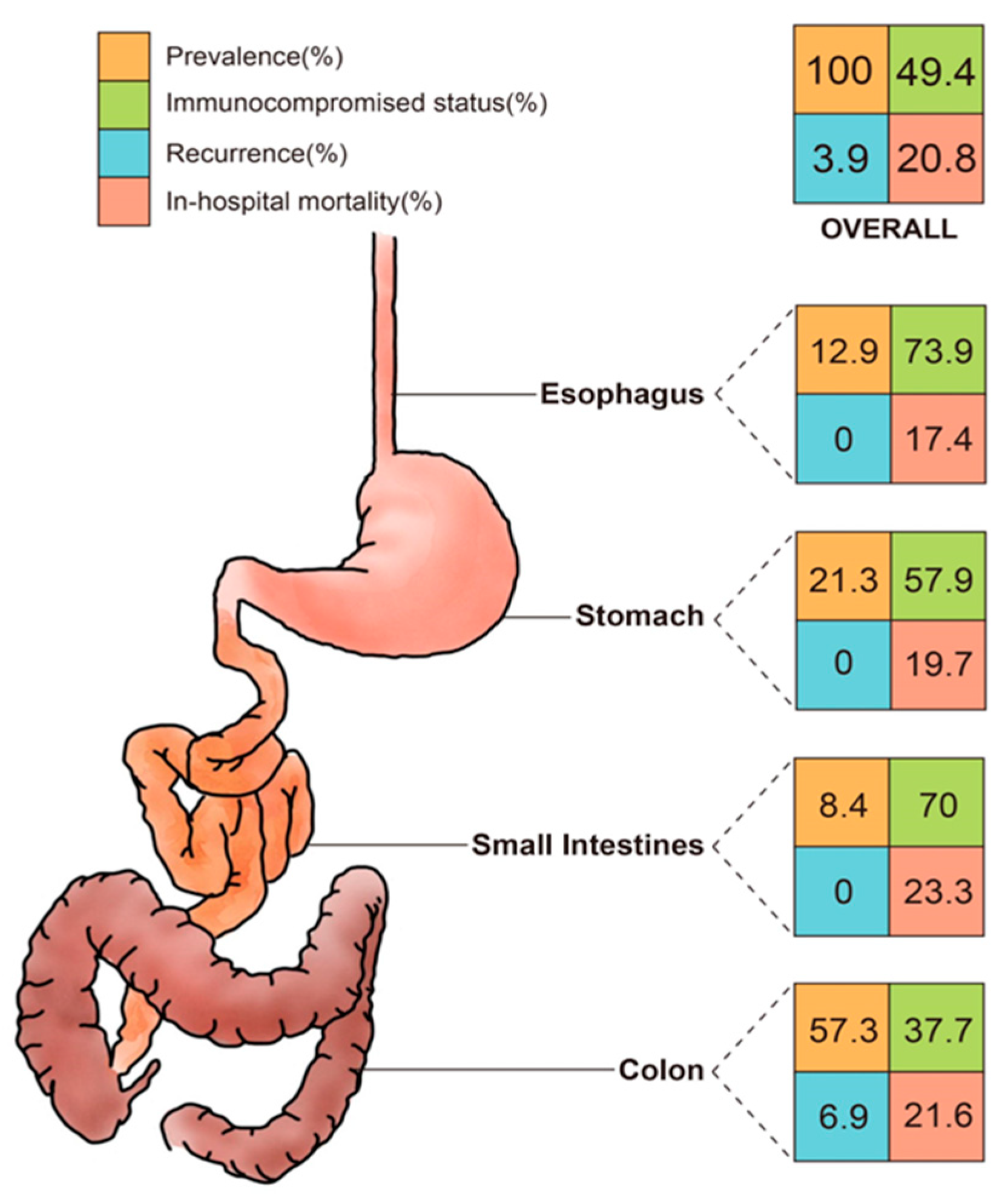
3.6. Impact of Different Locations, Treatment Courses, and Immune Status on In-Hospital Mortality
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Fakhreddine, A.Y.; Frenette, C.T.; Konijeti, G.G. A practical review of cytomegalovirus in gastroenterology and hepatology. Gastroenterol. Res. Pract. 2019, 2019, 6156581. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- You, D.M.; Johnson, M.D. Cytomegalovirus infection and the gastrointestinal tract. Curr. Gastroenterol. Rep. 2012, 14, 334–342. [Google Scholar] [CrossRef] [PubMed]
- Rafailidis, P.I.; Mourtzoukou, E.G.; Varbobitis, I.C.; Falagas, M.E. Severe cytomegalovirus infection in apparently immunocompetent patients: A systematic review. Virol. J. 2008, 5, 47. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Ljungman, P.; Boeckh, M.; Hirsch, H.H.; Josephson, F.; Lundgren, J.; Nichols, G.; Pikis, A.; Razonable, R.R.; Miller, V.; Griffiths, P.D. Definitions of cytomegalovirus infection and disease in transplant patients for use in clinical trials. Clin. Infect. Dis. 2016, 64, 87–91. [Google Scholar] [CrossRef] [Green Version]
- Ross, S.A.; Novak, Z.; Pati, S.; Boppana, S.B. Overview of the diagnosis of cytomegalovirus infection. Infect. Disord.-Drug Targets 2011, 11, 466–474. [Google Scholar] [CrossRef]
- Liao, X.; Reed, S.L.; Lin, G.Y. Immunostaining detection of cytomegalovirus in gastrointestinal biopsies: Clinicopathological correlation at a large academic health system. Gastroenterol. Res. 2016, 9, 92–98. [Google Scholar] [CrossRef] [Green Version]
- Wetwittayakhlang, P.; Rujeerapaiboon, N.; Wetwittayakhlung, P.; Sripongpun, P.; Pruphetkaew, N.; Jandee, S.; Chamroonkul, N.; Piratvisuth, T. Clinical features, endoscopic findings, and predictive factors for mortality in tissue-invasive gastrointestinal cytomegalovirus disease between immunocompetent and immunocompromised patients. Gastroenterol. Res. Pract. 2021, 2021, 8886525. [Google Scholar] [CrossRef]
- Yeh, P.-J.; Chiu, C.-T.; Lai, M.-W.; Wu, R.-C.; Kuo, C.-J.; Hsu, J.-T.; Su, M.-Y.; Le, P.-H. Cytomegalovirus gastritis: Clinicopathological profile. Dig. Liver Dis. 2021, 53, 722–728. [Google Scholar] [CrossRef]
- Chaemsupaphan, T.; Limsrivilai, J.; Thongdee, C.; Sudcharoen, A.; Pongpaibul, A.; Pausawasdi, N.; Charatcharoenwitthaya, P. Patient characteristics, clinical manifestations, prognosis, and factors associated with gastrointestinal cytomegalovirus infection in immunocompetent patients. BMC Gastroenterol. 2020, 20, 22. [Google Scholar] [CrossRef] [Green Version]
- Azer, S.A.; Limaiem, F. Cytomegalovirus Colitis; StatPearls Publishing: Treasure Island, FL, USA, 2021. [Google Scholar]
- Clos-Parals, A.; Rodríguez-Martínez, P.; Cañete, F.; Mañosa, M.; Ruiz-Cerulla, A.; Paúles, M.J.; Llaó, J.; Gordillo, J.; Fumagalli, C.; Garcia-Planella, E.; et al. Prognostic value of the burden of cytomegalovirus colonic reactivation evaluated by immunohistochemical staining in patients with active ulcerative colitis. J. Crohn’s Colitis 2019, 13, 385–388. [Google Scholar] [CrossRef]
- Lin, W.-R.; Su, M.-Y.; Hsu, C.-M.; Ho, Y.-P.; Ngan, K.-W.; Chiu, C.-T.; Chen, P.-C. Clinical and endoscopic features for alimentary tract cytomegalovirus disease: Report of 20 cases with gastrointestinal cytomegalovirus disease. Chang Gung Med. J. 2005, 28, 476–484. [Google Scholar] [PubMed]
- Ko, J.-H.; Peck, K.R.; Lee, W.J.; Huh, K.; Yoo, J.R.; Kim, K.-M.; Cho, S.Y.; Ha, Y.E.; Kang, C.-I.; Chung, D.R.; et al. Risk factors for cytomegalovirus gastrointestinal diseases in adult patients with cancer. Eur. J. Clin. Microbiol. 2014, 33, 1847–1853. [Google Scholar] [CrossRef]
- Yeh, P.-J.; Chiu, C.-T.; Lai, M.-W.; Wu, R.-C.; Chen, C.-M.; Kuo, C.-J.; Hsu, J.-T.; Su, M.-Y.; Lin, W.-P.; Chen, T.-H.; et al. Clinical manifestations, risk factors, and prognostic factors of cytomegalovirus enteritis. Gut Pathog. 2021, 13, 53. [Google Scholar] [CrossRef]
- Le, P.-H.; Lin, W.-R.; Kuo, C.-J.; Wu, R.-C.; Hsu, J.-T.; Su, M.-Y.; Lin, C.-J.; Chiu, C.-T. Clinical characteristics of cytomegalovirus colitis: A 15-year experience from a tertiary reference center. Ther. Clin. Risk Manag. 2018, 13, 1585–1593. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Marques, S.; Carmo, J.; Pinto, D.; Bispo, M.; Ramos, S.; Chagas, C. Cytomegalovirus disease of the upper gastrointestinal tract: A 10-year retrospective study. GE Port. J. Gastroenterol. 2017, 24, 262–268. [Google Scholar] [CrossRef]
- Yoon, J.; Lee, J.; Kim, D.S.; Lee, J.W.; Hong, S.W.; Hwang, H.W.; Hwang, S.W.; Park, S.H.; Yang, D.-H.; Ye, B.D.; et al. Endoscopic features and clinical outcomes of cytomegalovirus gastroenterocolitis in immunocompetent patients. Sci. Rep. 2021, 11, 6284. [Google Scholar] [CrossRef] [PubMed]
- Bernard, S.; Germi, R.; Lupo, J.; Laverrière, M.H.; Masse, V.; Morand, P.; Gavazzi, G. Symptomatic cytomegalovirus gastrointestinal infection with positive quantitative real-time PCR findings in apparently immunocompetent patients: A case series. Clin. Microbiol. Infect. 2015, 21, 1121.e1–1121.e7. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Le, P.-H.; Kuo, C.-J.; Wu, R.-C.; Hsu, J.-T.; Su, M.-Y.; Lin, C.-J.; Chiu, C.-T. Pancolitis associated with higher mortality risk of cytomegalovirus colitis in patients without inflammatory bowel disease. Ther. Clin. Risk Manag. 2018, 14, 1445–1451. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Lee, J.S.; Yun, J.; Ham, S.; Park, H.; Lee, H.; Kim, J.; Byeon, J.-S.; Jung, H.-Y.; Kim, N.; Kim, D.H. Machine learning approach for differentiating cytomegalovirus esophagitis from herpes simplex virus esophagitis. Sci. Rep. 2021, 11, 3672. [Google Scholar] [CrossRef] [PubMed]
- Gravito-Soares, E.; Almeida, N. Cytomegalovirus disease of the upper gastrointestinal tract: An emerging infection in immunocompetent hosts. GE-Port. J. Gastroenterol. 2017, 24, 259–261. [Google Scholar] [CrossRef] [PubMed]
- Reddy, N.; Wilcox, C.M. Diagnosis & management of cytomegalovirus infections in the GI tract. Expert Rev. Gastroenterol. Hepatol. 2007, 1, 287–294. [Google Scholar] [CrossRef] [PubMed]
- McCoy, M.H.; Post, K.; Sen, J.D.; Chang, H.Y.; Zhao, Z.; Fan, R.; Chen, S.; Leland, D.; Cheng, L.; Lin, J. qPCR increases sensitivity to detect cytomegalovirus in formalin-fixed, paraffin-embedded tissue of gastrointestinal biopsies. Hum. Pathol. 2014, 45, 48–53. [Google Scholar] [CrossRef] [PubMed]
- Suárez-Lledó, M.; Marcos, M.; Cuatrecasas, M.; Bombi, J.A.; Fernández-Avilés, F.; Magnano, L.; Martínez-Cibrián, N.; Llobet, N.; Rosiñol, L.; Gutiérrez-García, G.; et al. Quantitative PCR is faster, more objective, and more reliable than immunohistochemistry for the diagnosis of cytomegalovirus gastrointestinal disease in allogeneic stem cell transplantation. Biol. Blood Marrow Transplant. 2019, 25, 2281–2286. [Google Scholar] [CrossRef] [PubMed]
- Vincent, J.-L.; Dubois, M.-J.; Navickis, R.J.; Wilkes, M.M. Hypoalbuminemia in acute illness: Is there a rationale for intervention? A meta-analysis of cohort studies and controlled trials. Ann. Surg. 2003, 237, 319–334. [Google Scholar] [CrossRef] [PubMed]
- Jellinge, M.E.; Henriksen, D.P.; Hallas, P.; Brabrand, M. Hypoalbuminemia is a strong predictor of 30-day all-cause mortality in acutely admitted medical patients: A prospective, observational, cohort study. PLoS ONE 2014, 9, e105983. [Google Scholar] [CrossRef]
- Wiedermann, C. Hypoalbuminemia as surrogate and culprit of infections. Int. J. Mol. Sci. 2021, 22, 4496. [Google Scholar] [CrossRef]
- Segal, J.B.; Moliterno, A.R. Platelet counts differ by sex, ethnicity, and age in the United States. Ann. Epidemiol. 2006, 16, 123–130. [Google Scholar] [CrossRef]
- Ichiche, M.; Fontaine, C.; Lacor, P. Severe thrombocytopenia secondary to cytomegalovirus infection in an immunocompetent adult. Eur. J. Intern. Med. 2003, 14, 56–59. [Google Scholar] [CrossRef]
- Andrews, P.A.; Emery, V.; Newstead, C. Summary of the British Transplantation Society guidelines for the prevention and management of CMV disease after solid organ transplantation. Transplantation 2011, 92, 1181–1187. [Google Scholar] [CrossRef]
- Razonable, R.R.; Humar, A. Cytomegalovirus in solid organ transplant recipients—Guidelines of the American Society of Transplantation Infectious Diseases Community of Practice. Clin. Transplant. 2019, 33, e13512. [Google Scholar] [CrossRef]
- O’Hara, K.M.; Pontrelli, G.; Kunstel, K.L. An introduction to gastrointestinal tract CMV disease. J. Am. Acad. Physician Assist. 2017, 30, 48–52. [Google Scholar] [CrossRef] [PubMed]


| Characteristics | ES (n = 46) | ST (n = 76) | SI (n = 30) | CO (n = 204) | All (n = 356) |
|---|---|---|---|---|---|
| Sex (M/F) | 36 (78.3%) | 45 (59.2%) | 20 (66.7%) | 122 (59.8%) | 223 (62.6%) |
| Age, year (mean ± SD) | 59.7 ± 18.1 | 59.1 ± 17.8 | 50 ± 21 | 61.9 ± 18.3 | 60 ± 18.6 |
| General condition | |||||
| OPD/IPD | 11 (23.9%) | 30 (39.5%) | 3 (10%) | 38 (18.6%) | 82 (23%) |
| Shock | 8 (17.4%) | 9 (11.8%) | 10 (33.3%) | 47 (23%) | 74 (20.8%) |
| Intubation | 6 (13%) | 7 (9.2%) | 8 (26.7%) | 46 (22.5%) | 67 (18.8%) |
| ICU | 7 (15.2%) | 13 (17.1%) | 10 (33.3%) | 58 (28.4%) | 88 (24.7%) |
| Underlying disease | |||||
| Immunocompromised | 34 (73.9%) | 44 (57.9%) | 21 (70%) | 77 (37.7%) | 176 (49.4%) |
| DM | 9 (19.6%) | 23 (30.3%) | 3 (10%) | 66 (32.4%) | 101 (28.4%) |
| HTN | 20 (43.5%) | 38 (50%) | 10 (33.3%) | 94 (46.1%) | 162 (45.5%) |
| Old CVA | 4 (8.7%) | 4 (5.3%) | 2 (6.7%) | 31 (15.2%) | 41 (11.5%) |
| COPD | 4 (8.7%) | 2 (2.6%) | 2 (6.7%) | 10 (4.9%) | 18 (5.1%) |
| CAD | 5 (10.9%) | 5 (6.6%) | 3 (10%) | 32 (15.7%) | 45 (12.6%) |
| LC | 2 (4.3%) | 6 (7.9%) | 0 (0%) | 8 (3.9%) | 16 (4.5%) |
| ESRD | 4 (8.7%) | 8 (10.5%) | 6 (20%) | 25 (12.3%) | 43 (12.1%) |
| AKI | 6 (13%) | 8 (10.5%) | 7 (23.3%) | 48 (23.5%) | 69 (19.4%) |
| CD | 0 (0%) | 0 (0%) | 3 (10%) | 8 (3.9%) | 11 (3.1%) |
| UC | 1 (2.2%) | 1 (1.3%) | 1 (3.3%) | 31 (15.2%) | 34 (9.6%) |
| HIV | 8 (17.4%) | 5 (6.6%) | 2 (6.7%) | 18 (8.8%) | 33 (9.3%) |
| Malignancy | 20 (43.5%) | 29 (38.2%) | 11 (36.7%) | 38 (18.6%) | 98 (27.5%) |
| Transplant | 3 (6.5%) | 5 (6.6%) | 5 (16.7%) | 7 (3.4%) | 20 (5.6%) |
| Chemotherapy | 15 (32.6%) | 23 (30.3%) | 5 (16.7%) | 18 (8.8%) | 61 (17.1%) |
| Radiotherapy | 16 (34.8%) | 14 (18.4%) | 5 (16.7%) | 11 (5.4%) | 46 (12.9%) |
| Steroid | 23 (50%) | 36 (47.4%) | 13 (43.3%) | 65 (31.9%) | 137 (38.5%) |
| Immunosuppressant | 6 (13%) | 11 (14.7%) | 10 (33.3%) | 17 (8.3%) | 44 (12.4%) |
| Laboratory data (mean ± SD) | |||||
| WBC | 6471.4 ± 4592.8 | 7743.9 ± 4697.1 | 7742.9 ± 3840.2 | 8176.2 ± 4179.1 | 7837 ± 4329.9 |
| Segment | 76.2 ± 13.9 | 70.7 ± 15.8 | 71.3 ± 18.5 | 73.9 ± 13.8 | 73.3 ± 14.7 |
| Lymphocyte | 12.6 ± 10.3 | 18 ± 14.5 | 16.1 ± 14.1 | 16.7 ± 12 | 16.4 ± 12.6 |
| Hemoglobin | 10.3 ± 1.7 | 10.2 ± 2 | 9.2 ± 2.8 | 10.4 ± 2.6 | 10.2 ± 2.5 |
| Platelet | 186.2 ± 91.8 | 197.3 ± 111.9 | 198.4 ± 110.6 | 235.8 ± 128.7 | 218.5 ± 121.1 |
| Bilirubin | 0.7 ± 0.5 | 1.8 ± 7.6 | 0.9 ± 1 | 1.3 ± 2.8 | 1.3 ± 4.1 |
| Creatinine | 1.4 ± 1.6 | 1.8 ± 3.7 | 2.1 ± 2.1 | 1.8 ± 2.2 | 1.8 ± 2.5 |
| Albumin | 2.7 ± 0.7 | 3.1 ± 0.7 | 2.8 ± 0.6 | 3 ± 3.8 | 2.9 ± 2.9 |
| CRP | 57.7 ± 61.7 | 61.1 ± 74.6 | 76.9 ± 76.5 | 62.6 ± 71.3 | 63.3 ± 71.3 |
| CMV status | |||||
| CMV IgM | 3 (21.4%) | 7 (20%) | 4 (26.7%) | 14 (15.7%) | 28 (18.3%) |
| CMV IgG | 13 (92.9%) | 29 (96.7%) | 15 (100%) | 83 (97.6%) | 140 (97.2%) |
| CMV antigenemia | 8 (66.7%) | 13 (48.1%) | 4 (36.4%) | 43 (58.1%) | 68 (54.8%) |
| CMV viremia | 4 (57.1%) | 6 (33.3%) | 8 (72.7%) | 57 (81.4%) | 75 (70.8%) |
| Clinical presentation | |||||
| Fever | 17 (37%) | 20 (26.3%) | 12 (40%) | 69 (33.8%) | 118 (33.1%) |
| Abdominal pain | 20 (43.5%) | 30 (39.5%) | 15 (50%) | 47 (23%) | 112 (31.5%) |
| GI bleeding | 14 (30.4%) | 26 (34.2%) | 21 (70%) | 102 (50%) | 163 (45.8%) |
| Endoscopic feature | |||||
| Polypoid mass | 6 (13%) | 5 (6.6%) | 6 (20%) | 24 (11.8%) | 41 (11.5%) |
| Inflammation | 1 (2.2%) | 6 (7.9%) | 4 (13.3%) | 23 (11.3%) | 34 (9.6%) |
| Ulcer | 42 (91.3%) | 66 (86.8%) | 23 (76.7%) | 171 (83.8%) | 302 (84.8%) |
| Treatment | |||||
| Operation | 0 (0%) | 2 (2.6%) | 6 (20%) | 17 (8.3%) | 25 (7%) |
| IV ± PO | 27 (58.7%) | 40 (52.6%) | 18 (60%) | 127 (62.3%) | 212 (59.6%) |
| IV + PO (Combo) | 6 (13%) | 10 (13.2%) | 6 (20%) | 34 (16.7%) | 56 (15.7%) |
| IV (exclusive) | 8 (17.4%) | 12 (15.8%) | 10 (33.3%) | 55 (27%) | 85 (23.9%) |
| PO (exclusive) | 13 (28.3%) | 17 (22.4%) | 2 (6.7%) | 37 (18.1%) | 69 (19.4%) |
| Course/Outcome (mean ± SD) | |||||
| Time-to-diagnosis | 15.8 ± 13.1 | 17.8 ± 20.1 | 19.7 ± 16.3 | 21.5 ± 21.1 | 19.8 ± 19.7 |
| Admission duration | 33.4 ± 27.2 | 41.9 ± 34.5 | 32 ± 18 | 44.2 ± 34.5 | 41.2 ± 32.6 |
| Follow up duration | 922.1 ± 1504.8 | 1532.6 ± 5139.1 | 637.6 ± 1049.7 | 768.8 ± 1199.3 | 939.8 ± 2615.1 |
| Perforation | 0 (0%) | 1 (1.3%) | 2 (6.7%) | 8 (3.9%) | 11 (3.1%) |
| Recurrence | 0 (0%) | 0 (0%) | 0 (0%) | 14 (6.9%) | 14 (3.9%) |
| In-hospital mortality | 8 (17.4%) | 15 (19.7%) | 7 (23.3%) | 44 (21.6%) | 74 (20.8%) |
| Overall mortality | 23 (50%) | 31 (40.8%) | 13 (43.3%) | 77 (37.7%) | 144 (40.4%) |
| Characteristics | Univariable Analysis | Multivariable Analysis | ||||
|---|---|---|---|---|---|---|
| OR | 95% CI | p-Value | OR | 95% CI | p-Value | |
| Sex (M/F) | 0.844 | 0.5–1.425 | 0.525 | |||
| Age, year | 1.023 | 1.007–1.039 | 0.004 * | 1.042 | 1.005–1.081 | 0.026 * |
| General condition | ||||||
| OPD source | 0.034 | 0.005–0.249 | 0.001 * | <0.001 | - | 0.999 |
| Shock | 6.622 | 3.737–11.732 | <0.001 * | 1.754 | 0.571–5.39 | 0.326 |
| Intubation | 4.926 | 2.76–8.792 | <0.001 * | 1.247 | 0.289–5.388 | 0.768 |
| ICU | 7.305 | 4.168–12.803 | <0.001 * | 2.078 | 0.536–8.053 | 0.290 |
| Underlying disease | ||||||
| Immunocompromised | 1.921 | 1.136–3.247 | 0.015 * | 9.927 | 1.575–62.545 | 0.015 * |
| DM | 0.843 | 0.471–1.507 | 0.564 | |||
| HTN | 1.440 | 0.862–2.407 | 0.164 | |||
| Old CVA | 1.467 | 0.697–3.087 | 0.313 | |||
| COPD | 0.752 | 0.212–2.67 | 0.66 | |||
| CAD | 2.407 | 1.227–4.721 | 0.011 * | 2.040 | 0.511–8.136 | 0.313 |
| LC | 0.532 | 0.118–2.393 | 0.411 | |||
| ESRD | 1.010 | 0.461–2.212 | 0.98 | |||
| AKI | 3.283 | 1.846–5.838 | <0.001 * | 1.799 | 0.564–5.737 | 0.321 |
| CD | <0.001 | - | - | |||
| UC | 0.217 | 0.051–0.927 | 0.039 | 2.677 | 0.178–40.367 | 0.477 |
| HIV | 0.355 | 0.105–1.197 | 0.095 | |||
| Malignancy | 2.313 | 1.352–3.958 | 0.002 * | 2.692 | 0.335–21.653 | 0.352 |
| Transplant | 0.951 | 0.308–2.933 | 0.93 | |||
| Chemotherapy | 1.974 | 1.066–3.655 | 0.03 * | 0.601 | 0.088–4.12 | 0.604 |
| Radiotherapy | 2.602 | 1.339–5.055 | 0.005 * | 2.157 | 0.309–15.038 | 0.438 |
| Steroid | 2.407 | 1.431–4.05 | 0.001 * | 0.866 | 0.232–3.238 | 0.831 |
| Immunosuppressant | 0.689 | 0.294–1.615 | 0.392 | |||
| Laboratory data | ||||||
| WBC | 1.000 | 1.000–1.000 | 0.006 * | 1.000 | 1.000–1.000 | 0.075 |
| Segment | 1.067 | 1.041–1.094 | <0.001 * | 0.957 | 0.858–1.068 | 0.435 |
| Lymphocyte | 0.920 | 0.889–0.951 | <0.001 * | 0.951 | 0.843–1.072 | 0.411 |
| Hemoglobin | 0.783 | 0.683–0.898 | <0.001 * | 0.938 | 0.714–1.232 | 0.644 |
| Platelet | 0.992 | 0.989–0.995 | <0.001 * | 0.993 | 0.986–0.999 | 0.027 * |
| Bilirubin | 1.058 | 0.975–1.148 | 0.173 | |||
| Creatinine | 1.055 | 0.961–1.158 | 0.264 | |||
| Albumin | 0.233 | 0.134–0.405 | <0.001 * | 0.346 | 0.119–1.001 | 0.050 * |
| CRP | 1.010 | 1.006–1.014 | <0.001 * | 1.003 | 0.996–1.009 | 0.433 |
| Clinical presentation | ||||||
| Fever | 2.152 | 1.275–3.631 | 0.004 * | 1.848 | 0.603–5.664 | 0.283 |
| Abdominal pain | 0.903 | 0.517–1.577 | 0.719 | |||
| GI bleeding | 4.663 | 2.626–8.28 | <0.001 * | 6.067 | 1.611–22.84 | 0.008 * |
| Endoscopic feature | ||||||
| Polypoid mass | 0.271 | 0.081–0.905 | 0.034 * | 0.325 | 0.025–4.202 | 0.390 |
| Inflammation | 0.632 | 0.236–1.694 | 0.362 | |||
| Ulcer | 2.902 | 1.113–7.567 | 0.029 * | 1.631 | 0.268–9.933 | 0.596 |
| Treatment | ||||||
| Operation | 2.781 | 1.194–6.477 | 0.018 * | 0.951 | 0.165–5.463 | 0.955 |
| IV ± PO | 1.328 | 0.78–2.263 | 0.296 | |||
| IV + PO (Combo) | 0.183 | 0.055–0.602 | 0.005 * | 0.031 | 0.002–0.589 | 0.021 * |
| IV (exclusive) | 4.164 | 2.404–7.212 | <0.001 * | 1.009 | 0.324–3.142 | 0.988 |
| PO (exclusive) | 0.591 | 0.286–1.22 | 0.155 | |||
| Course/Outcome | ||||||
| Time-to-diagnosis | 1.032 | 1.016–1.048 | <0.001 * | 1.023 | 1.003–1.044 | 0.025 * |
| Perforation | 0.843 | 0.178–3.986 | 0.829 | |||
| Immunocompetent (n = 180) | Immunocompromised (n = 176) | |||||
|---|---|---|---|---|---|---|
| Survival | Death | p-Value | Survival | Death | p-Value | |
| Any treatment (IV or PO) | 81 (53.3%) | 18 (64.3%) | 0.282 | 83 (63.8%) | 30 (65.2%) | 0.868 |
| No treatment (IV or PO) | 71 (46.7%) | 10 (35.7%) | 47 (36.2%) | 16 (34.8%) | ||
| IV + PO (Combo) (+) | 25 (16.4%) | 0 (0%) | 0.016 * | 28 (21.5%) | 3 (6.5%) | 0.022 * |
| IV + PO (Combo) (−) | 127 (83.6%) | 28 (100%) | 102 (78.5%) | 43 (93.5%) | ||
| IV (exclusive) (+) | 24 (15.8%) | 14 (50%) | <0.001 * | 26 (20%) | 21 (45.7%) | 0.001 * |
| IV (exclusive) (−) | 128 (84.2%) | 14 (50%) | 104 (80%) | 25 (54.3%) | ||
| PO (exclusive) (+) | 31 (20.4%) | 4 (14.3%) | 0.453 | 28 (21.5%) | 6 (13%) | 0.21 |
| PO (exclusive) (−) | 121 (79.6%) | 24 (85.7%) | 102 (78.5%) | 40 (87%) | ||
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Yeh, P.-J.; Wu, R.-C.; Chiu, C.-T.; Lai, M.-W.; Chen, C.-M.; Pan, Y.-B.; Su, M.-Y.; Kuo, C.-J.; Lin, W.-R.; Le, P.-H. Cytomegalovirus Diseases of the Gastrointestinal Tract. Viruses 2022, 14, 352. https://doi.org/10.3390/v14020352
Yeh P-J, Wu R-C, Chiu C-T, Lai M-W, Chen C-M, Pan Y-B, Su M-Y, Kuo C-J, Lin W-R, Le P-H. Cytomegalovirus Diseases of the Gastrointestinal Tract. Viruses. 2022; 14(2):352. https://doi.org/10.3390/v14020352
Chicago/Turabian StyleYeh, Pai-Jui, Ren-Chin Wu, Cheng-Tang Chiu, Ming-Wei Lai, Chien-Ming Chen, Yu-Bin Pan, Ming-Yao Su, Chia-Jung Kuo, Wey-Ran Lin, and Puo-Hsien Le. 2022. "Cytomegalovirus Diseases of the Gastrointestinal Tract" Viruses 14, no. 2: 352. https://doi.org/10.3390/v14020352
APA StyleYeh, P.-J., Wu, R.-C., Chiu, C.-T., Lai, M.-W., Chen, C.-M., Pan, Y.-B., Su, M.-Y., Kuo, C.-J., Lin, W.-R., & Le, P.-H. (2022). Cytomegalovirus Diseases of the Gastrointestinal Tract. Viruses, 14(2), 352. https://doi.org/10.3390/v14020352






