Computational and Rational Design of Single-Chain Antibody against Tick-Borne Encephalitis Virus for Modifying Its Specificity
Abstract
:1. Introduction
2. Materials and Methods
2.1. Design of Mutant Antibody Variants with an Optimized Interface
2.2. Predicting the Effect of Antibody Mutations on Binding Affinity Using the mmCSM-AB and mCSM-AB2 Online Services
2.3. Construction of Plasmid DNAs Encoding Single-Chain Antibody Fragments
2.4. Production of Single-Chain Antibodies in E. coli
2.5. Production of D3 Proteins in E. coli
2.6. Affinity Constant Measurement
3. Results
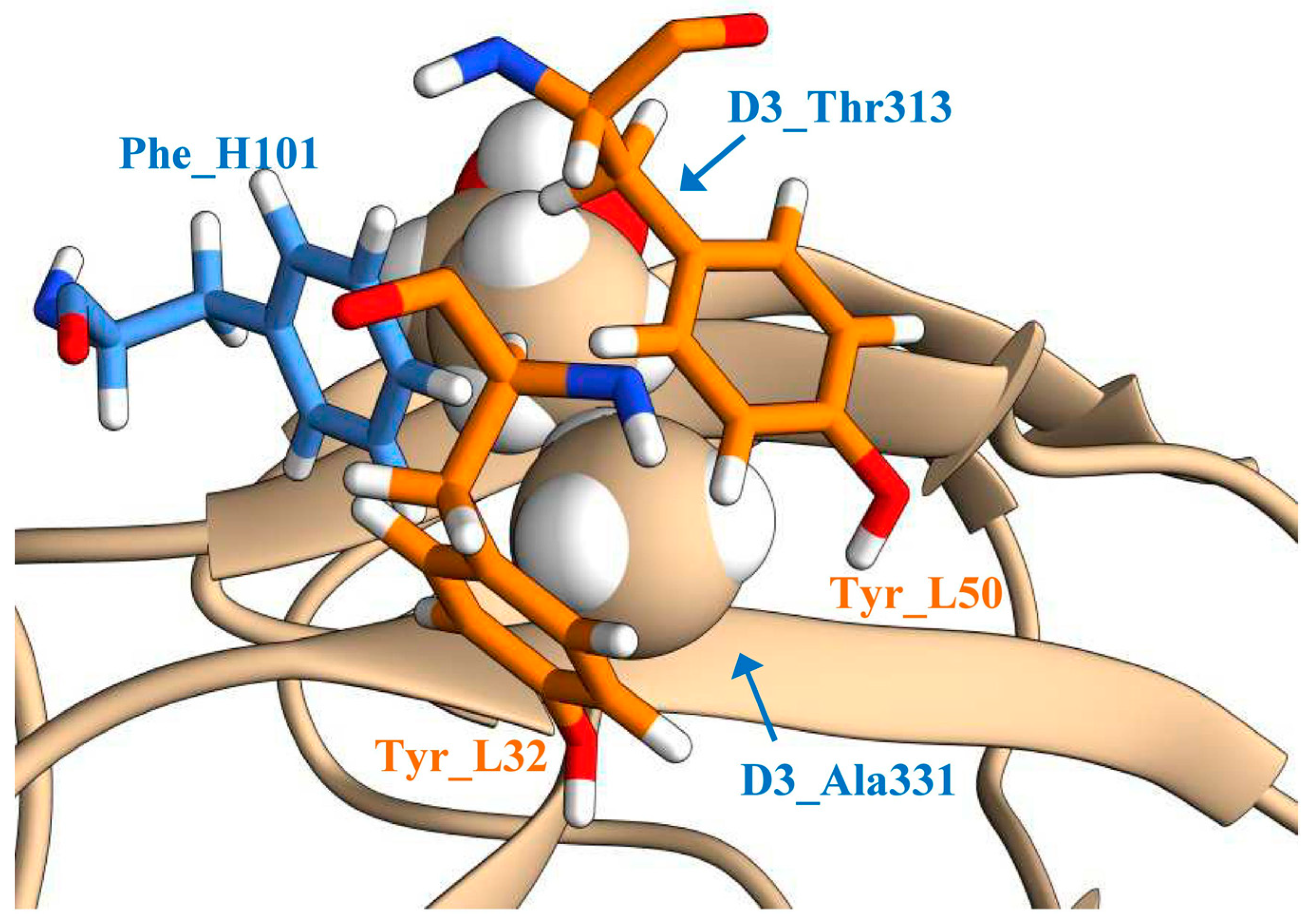
3.1. Optimization of the Geometry of the Antigen−Antibody Interface
3.2. Predicting Favorable Mutations using Machine Learning-Based Methods
4. Discussion
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Ruzek, D.; Avšič Županc, T.; Borde, J.; Chrdle, A.; Eyer, L.; Karganova, G.; Kholodilov, I.; Knap, N.; Kozlovskaya, L.; Matveev, A.; et al. Tick-borne encephalitis in Europe and Russia: Review of pathogenesis, clinical features, therapy, and vaccines. Antivir. Res. 2019, 164, 23–51. [Google Scholar] [CrossRef] [PubMed]
- European Centre for Disease Prevention and Control. Tick-borne encephalitis. In Annual Epidemiological Report for 2019; ECDC: Stockholm, Switzerland, 2021; Available online: https://www.ecdc.europa.eu/en/publications-data/tick-borne-encephalitis-annual-epidemiological-report-2019 (accessed on 24 March 2021).
- Nikitin, A.Y.; Andaev, E.I.; Yatsmenko, E.V.; Trushina Yu, N.; Tolmacheva, M.I.; Verigina, E.V.; Turanov, A.O.; Balakhonov, S.V. Epidemiological Situation on Tick-Borne Viral Encephalitis in the Russian Federation in 2019 and Forecast for 2020. Probl. Part. Danger. Infect. 2020, 1, 33–42. (In Russian) [Google Scholar] [CrossRef] [Green Version]
- Kovalev, S.Y.; Mukhacheva, T.A. Reconsidering the classification of tick-borne encephalitis virus within the Siberian subtype gives new insights into its evolutionary history. Infect. Genet. Evol. 2017, 55, 159–165. [Google Scholar] [CrossRef]
- Dai, X.; Shang, G.; Lu, S.; Yang, J.; Xu, J. A new subtype of eastern tick-borne encephalitis virus discovered in Qinghai-Tibet Plateau, China. Emerg. Microbes Infect. 2018, 7, 74. [Google Scholar] [CrossRef] [PubMed]
- Mansfield, K.L.; Johnson, N.; Phipps, L.P.; Stephenson, J.R.; Fooks, A.R.; Solomon, T. Tick-borne encephalitis virus—A review of an emerging zoonosis. J. Gen. Virol. 2009, 90 Pt 8, 1781–1794. [Google Scholar] [CrossRef]
- Kaiser, R. Tick-borne encephalitis: Clinical findings and prognosis in adults. Wien Med. Wochenschr. 2012, 162, 239–243. [Google Scholar] [CrossRef]
- Kaiser, R. Tick-borne encephalitis. Nervenarzt 2016, 87, 667–680. [Google Scholar] [CrossRef]
- Belikov, S.I.; Kondratov, I.G.; Potapova, U.V.; Leonova, G.N. The relationship between the structure of the tick-borne encephalitis virus strains and their pathogenic properties. PLoS ONE 2014, 9, e94946. [Google Scholar] [CrossRef] [Green Version]
- Tkachev, S.E.; Babkin, I.V.; Chicherina, G.S.; Kozlova, I.V.; Verkhozina, M.M.; Demina, T.V.; Lisak, O.V.; Doroshchenko, E.K.; Dzhioev, Y.P.; Suntsova, O.V.; et al. Genetic diversity and geographical distribution of the Siberian subtype of the tick-borne encephalitis virus. Ticks Tick Borne Dis. 2020, 11, 101327. [Google Scholar] [CrossRef] [PubMed]
- Elsterova, J.; Palus, M.; Sirmarova, J.; Kopecky, J.; Niller, H.H.; Ruzek, D. Tick-borne encephalitis virus neutralization by high dose intravenous immunoglobulin. Ticks Tick Borne Dis. 2017, 8, 253–258. [Google Scholar] [CrossRef]
- Erber, W.; Schmitt, H.J. Self-reported tick-borne encephalitis (TBE) vaccination coverage in Europe: Results from a cross-sectional study. Ticks Tick Borne Dis. 2018, 9, 768–777. [Google Scholar] [CrossRef] [PubMed]
- Baroutsou, V.; Zens, K.D.; Sinniger, P.; Fehr, J.; Lang, P. Analysis of Tick-borne Encephalitis vaccination coverage and compliance in adults in Switzerland, 2018. Vaccine 2020, 38, 7825–7833. [Google Scholar] [CrossRef] [PubMed]
- Andaev, E.I.; Nikitin AYa Yatsmenko, E.V.; Verigina, E.V.; Tolmacheva, M.I.; Ayugin, N.I.; Matveeva, V.A.; Balakhonov, S.V. Trends in Epidemic Process Development of Tick-Borne Encephalitis in the Russian Federation, Laboratory Diagnosis, Prophylaxis and Forecast for 2021. Probl. Part. Danger. Infect. 2021, 1, 6–16. (In Russian) [Google Scholar] [CrossRef]
- Füzik, T.; Formanová, P.; Růžek, D.; Yoshii, K.; Niedrig, M.; Plevka, P. Structure of tick-borne encephalitis virus and its neutralization by a monoclonal antibody. Nat. Commun. 2018, 9, 436. [Google Scholar] [CrossRef] [Green Version]
- Mandl, C.W. Steps of the tick-borne encephalitis virus replication cycle that affect neuropathogenesis. Virus Res. 2005, 111, 161–174. [Google Scholar] [CrossRef]
- Kellman, E.M.; Offerdahl, D.K.; Melik, W.; Bloom, M.E. Viral Determinants of Virulence in Tick-Borne Flaviviruses. Viruses 2018, 10, 329. [Google Scholar] [CrossRef]
- Roehrig, J.T. Antigenic structure of flavivirus proteins. Adv. Virus Res. 2003, 59, 141–175. [Google Scholar]
- Oliphant, T.; Engle, M.; Nybakken, G.E.; Doane, C.; Johnson, S.; Huang, L.; Gorlatov, S.; Mehlhop, E.; Marri, A.; Chung, K.M.; et al. Development of a humanized monoclonal antibody with therapeutic potential against West Nile virus. Nat. Med. 2005, 11, 522–530. [Google Scholar] [CrossRef]
- Sánchez, M.D.; Pierson, T.C.; McAllister, D.; Hanna, S.L.; Puffer, B.A.; Valentine, L.E.; Murtadha, M.M.; Hoxie, J.A.; Doms, R.W. Characterization of neutralizing antibodies to West Nile virus. Virology 2005, 336, 70–82. [Google Scholar] [CrossRef] [Green Version]
- Dai, L.; Wang, Q.; Qi, J.; Shi, Y.; Yan, J.; Gao, G.F. Molecular basis of antibody-mediated neutralization and protection against flavivirus. IUBMB Life 2016, 68, 783–791. [Google Scholar] [CrossRef]
- Baykov, I.K.; Matveev, A.L.; Stronin, O.V.; Ryzhikov, A.B.; Matveev, L.E.; Kasakin, M.F.; Richter, V.A.; Tikunova, N.V. A protective chimeric antibody to tick-borne encephalitis virus. Vaccine 2014, 32, 3589–3594. [Google Scholar] [CrossRef]
- Matveev, A.L.; Kozlova, I.V.; Stronin, O.V.; Khlusevich, Y.A.; Doroshchenko, E.K.; Baykov, I.K.; Lisak, O.V.; Emelyanova, L.A.; Suntsova, O.V.; Matveeva, V.A.; et al. Post-exposure administration of chimeric antibody protects mice against European, Siberian, and Far-Eastern subtypes of tick-borne encephalitis virus. PLoS ONE 2019, 14, e0215075. [Google Scholar] [CrossRef] [PubMed]
- Yang, X.; Qi, J.; Peng, R.; Dai, L.; Gould, E.A.; Gao, G.F.; Tien, P. Molecular Basis of a Protective/Neutralizing Monoclonal Antibody Targeting Envelope Proteins of both Tick-Borne Encephalitis Virus and Louping Ill Virus. J. Virol. 2019, 93, e02132-18. [Google Scholar] [CrossRef] [Green Version]
- Baykov, I.K.; Matveev, A.L.; Emelianova, L.A.; Kaverina, G.B.; Tkachev, S.E.; Tikunova, N.V. The effect of differences in the third domain of the glycoprotein E of tick-borne encephalitis virus of the Far Eastern, Siberian and European subtypes on the binding of recombinant D3 proteins with a chimeric antibody. Vavilov J. Genet. Breed. 2019, 23, 256–261. [Google Scholar] [CrossRef] [Green Version]
- Rey, F.A.; Heinz, F.X.; Mandl, C.; Kunz, C.; Harrison, S.C. The envelope glycoprotein from tick-borne encephalitis virus at 2 A resolution. Nature 1995, 375, 291–298. [Google Scholar] [CrossRef]
- Bates, J.T.; Keefer, C.J.; Utley, T.J.; Correia, B.E.; Schief, W.R.; Crowe, J.E., Jr. Reversion of somatic mutations of the respiratory syncytial virus-specific human monoclonal antibody Fab19 reveal a direct relationship between association rate and neutralizing potency. J. Immunol. 2013, 190, 3732–3739. [Google Scholar] [CrossRef]
- Vivcharuk, V.; Baardsnes, J.; Deprez, C.; Sulea, T.; Jaramillo, M.; Corbeil, C.R.; Mullick, A.; Magoon, J.; Marcil, A.; Durocher, Y.; et al. Assisted Design of Antibody and Protein Therapeutics (ADAPT). PLoS ONE 2017, 12, e0181490. [Google Scholar] [CrossRef] [Green Version]
- Baran, D.; Pszolla, M.G.; Lapidoth, G.D.; Norn, C.; Dym, O.; Unger, T.; Albeck, S.; Tyka, M.D.; Fleishman, S.J. Principles for computational design of binding antibodies. Proc. Natl. Acad. Sci. USA 2017, 114, 10900–10905. [Google Scholar] [CrossRef] [Green Version]
- Fischman, S.; Ofran, Y. Computational design of antibodies. Curr. Opin. Struct. Biol. 2018, 51, 156–162. [Google Scholar] [CrossRef]
- Kuroda, D.; Tsumoto, K. Antibody Affinity Maturation by Computational Design. Methods Mol. Biol. 2018, 1827, 15–34. [Google Scholar]
- Cannon, D.A.; Shan, L.; Du, Q.; Shirinian, L.; Rickert, K.W.; Rosenthal, K.L.; Korade, M., 3rd; van Vlerken-Ysla, L.E.; Buchanan, A.; Vaughan, T.J.; et al. Experimentally guided computational antibody affinity maturation with de novo docking, modelling and rational design. PLoS Comput. Biol. 2019, 15, e1006980. [Google Scholar] [CrossRef] [Green Version]
- Myung, Y.; Pires, D.E.V.; Ascher, D.B. mmCSM-AB: Guiding rational antibody engineering through multiple point mutations. Nucleic Acids Res. 2020, 48, W125–W131. [Google Scholar] [CrossRef] [PubMed]
- Sormanni, P.; Aprile, F.A.; Vendruscolo, M. Third generation antibody discovery methods: In silico rational design. Chem. Soc. Rev. 2018, 47, 9137–9157. [Google Scholar] [CrossRef]
- Kiyoshi, M.; Caaveiro, J.M.; Miura, E.; Nagatoishi, S.; Nakakido, M.; Soga, S.; Shirai, H.; Kawabata, S.; Tsumoto, K. Affinity improvement of a therapeutic antibody by structure-based computational design: Generation of electrostatic interactions in the transition state stabilizes the antibody-antigen complex. PLoS ONE 2014, 9, e87099. [Google Scholar] [CrossRef] [Green Version]
- Clark, L.A.; Boriack-Sjodin, P.A.; Eldredge, J.; Fitch, C.; Friedman, B.; Hanf, K.J.; Jarpe, M.; Liparoto, S.F.; Li, Y.; Lugovskoy, A.; et al. Affinity enhancement of an in vivo matured therapeutic antibody using structure-based computational design. Protein Sci. 2006, 15, 949–960. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Fukunaga, A.; Maeta, S.; Reema, B.; Nakakido, M.; Tsumoto, K. Improvement of antibody affinity by introduction of basic amino acid residues into the framework region. Biochem. Biophys. Rep. 2018, 15, 81–85. [Google Scholar] [CrossRef] [PubMed]
- Chiba, S.; Tanabe, A.; Nakakido, M.; Okuno, Y.; Tsumoto, K.; Ohta, M. Structure-based design and discovery of novel anti-tissue factor antibodies with cooperative double-point mutations, using interaction analysis. Sci. Rep. 2020, 10, 17590. [Google Scholar] [CrossRef] [PubMed]
- Baykov, I.K.; Emelyanova, L.A.; Sokolova, L.M.; Karelina, E.M.; Matveev, A.L.; Babkin, I.V.; Khlusevich, Y.A.; Podgornyy, V.F.; Tikunova, N.V. Analysis of domain specificity of the protective chimeric antibody ch14D5a against glycoprotein E of tick-borne encephalitis virus. Vavilov J. Genet. Breed. 2018, 22, 459–467. [Google Scholar] [CrossRef]
- Baykov, I.K.; Chojnowski, G.; Pachl, P.; Matveev, A.L.; Moor, N.A.; Emelianova, L.A.; Rezacova, P.M.; Lamzin, V.S.; Tikunova, N.V. Structural insights into tick-borne encephalitis virus neutralization and animal protection by a therapeutic antibody. bioRxiv 2021. [Google Scholar] [CrossRef]
- Burakova, L.P.; Kudryavtsev, A.N.; Stepanyuk, G.A.; Baykov, I.K.; Morozova, V.V.; Tikunova, N.V.; Dubova, M.A.; Lyapustin, V.N.; Yakimenko, V.V.; Frank, L.A. Bioluminescent detection probe for tick-borne encephalitis virus immunoassay. Anal. Bioanal. Chem. 2015, 407, 5417–5423. [Google Scholar] [CrossRef]
- Zidane, N.; Dussart, P.; Bremand, L.; Villani, M.E.; Bedouelle, H. Thermodynamic stability of domain III from the envelope protein of flaviviruses and its improvement by molecular design. Protein Eng. Des. Sel. 2013, 26, 389–399. [Google Scholar] [CrossRef] [Green Version]
- Guirakhoo, F.; Heinz, F.X.; Kunz, C. Epitope model of tick-borne encephalitis virus envelope glycoprotein E: Analysis of structural properties, role of carbohydrate side chain, and conformational changes occurring at acidic pH. Virology 1989, 169, 90–99. [Google Scholar] [CrossRef]
- Holzmann, H.; Stiasny, K.; York, H.; Dorner, F.; Kunz, C.; Heinz, F.X. Tick-borne encephalitis virus envelope protein E-specific monoclonal antibodies for the study of low pH-induced conformational changes and immature virions. Arch. Virol. 1995, 140, 213–221. [Google Scholar] [CrossRef]
- Kiermayr, S.; Stiasny, K.; Heinz, F.X. Impact of quaternary organization on the antigenic structure of the tick-borne encephalitis virus envelope glycoprotein E. J. Virol. 2009, 83, 8482–8491. [Google Scholar] [CrossRef] [Green Version]
- Tsekhanovskaya, N.A.; Matveev, L.E.; Rubin, S.G.; Karavanov, A.S.; Pressman, E.K. Epitope analysis of tick-borne encephalitis (TBE) complex viruses using monoclonal antibodies to envelope glycoprotein of TBE virus (persulcatus subtype). Virus Res. 1993, 30, 1–16. [Google Scholar] [CrossRef]
- Agudelo, M.; Palus, M.; Keeffe, J.R.; Bianchini, F.; Svoboda, P.; Salát, J.; Peace, A.; Gazumyan, A.; Cipolla, M.; Kapoor, T.; et al. Broad and potent neutralizing human antibodies to tick-borne flaviviruses protect mice from disease. J. Exp. Med. 2021, 218, e20210236. [Google Scholar] [CrossRef]
- Reid, C.; Rushe, M.; Jarpe, M.; van Vlijmen, H.; Dolinski, B.; Qian, F.; Cachero, T.G.; Cuervo, H.; Yanachkova, M.; Nwankwo, C.; et al. Structure activity relationships of monocyte chemoattractant proteins in complex with a blocking antibody. Protein Eng. Des. Sel. 2006, 19, 317–324. [Google Scholar] [CrossRef] [Green Version]
- Edeling, M.A.; Austin, S.K.; Shrestha, B.; Dowd, K.A.; Mukherjee, S.; Nelson, C.A.; Johnson, S.; Mabila, M.N.; Christian, E.A.; Rucker, J.; et al. Potent dengue virus neutralization by a therapeutic antibody with low monovalent affinity requires bivalent engagement. PLoS Pathog. 2014, 10, e1004072. [Google Scholar] [CrossRef] [Green Version]
- Plevka, P.; Lim, P.Y.; Perera, R.; Cardosa, J.; Suksatu, A.; Kuhn, R.J.; Rossmann, M.G. Neutralizing antibodies can initiate genome release from human enterovirus 71. Proc. Natl. Acad. Sci. USA 2014, 111, 2134–2139. [Google Scholar] [CrossRef] [Green Version]
- Ripoll, D.R.; Khavrutskii, I.; Wallqvist, A.; Chaudhury, S. Modeling the Role of Epitope Arrangement on Antibody Binding Stoichiometry in Flaviviruses. Biophys. J. 2016, 111, 1641–1654. [Google Scholar] [CrossRef] [Green Version]
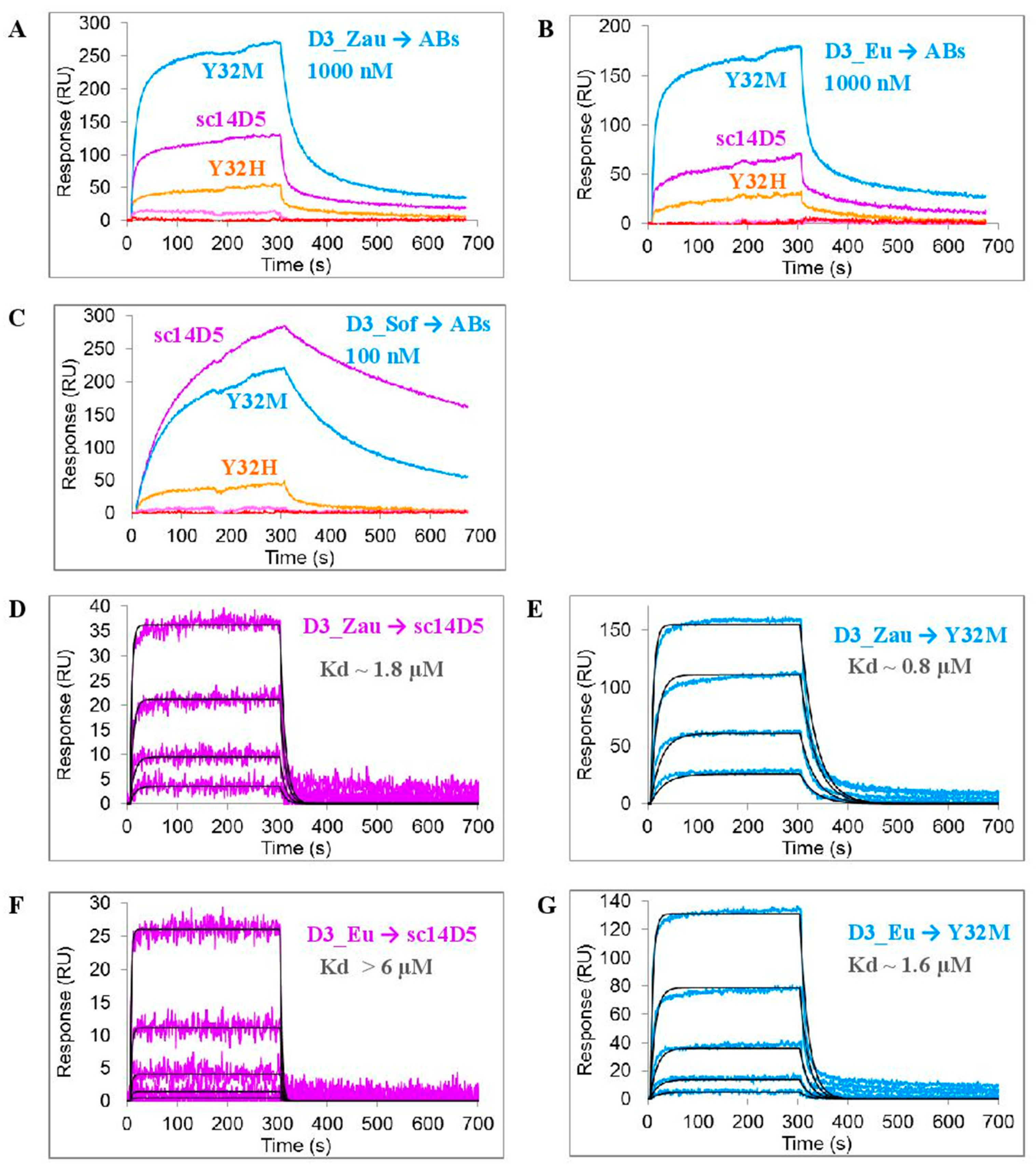
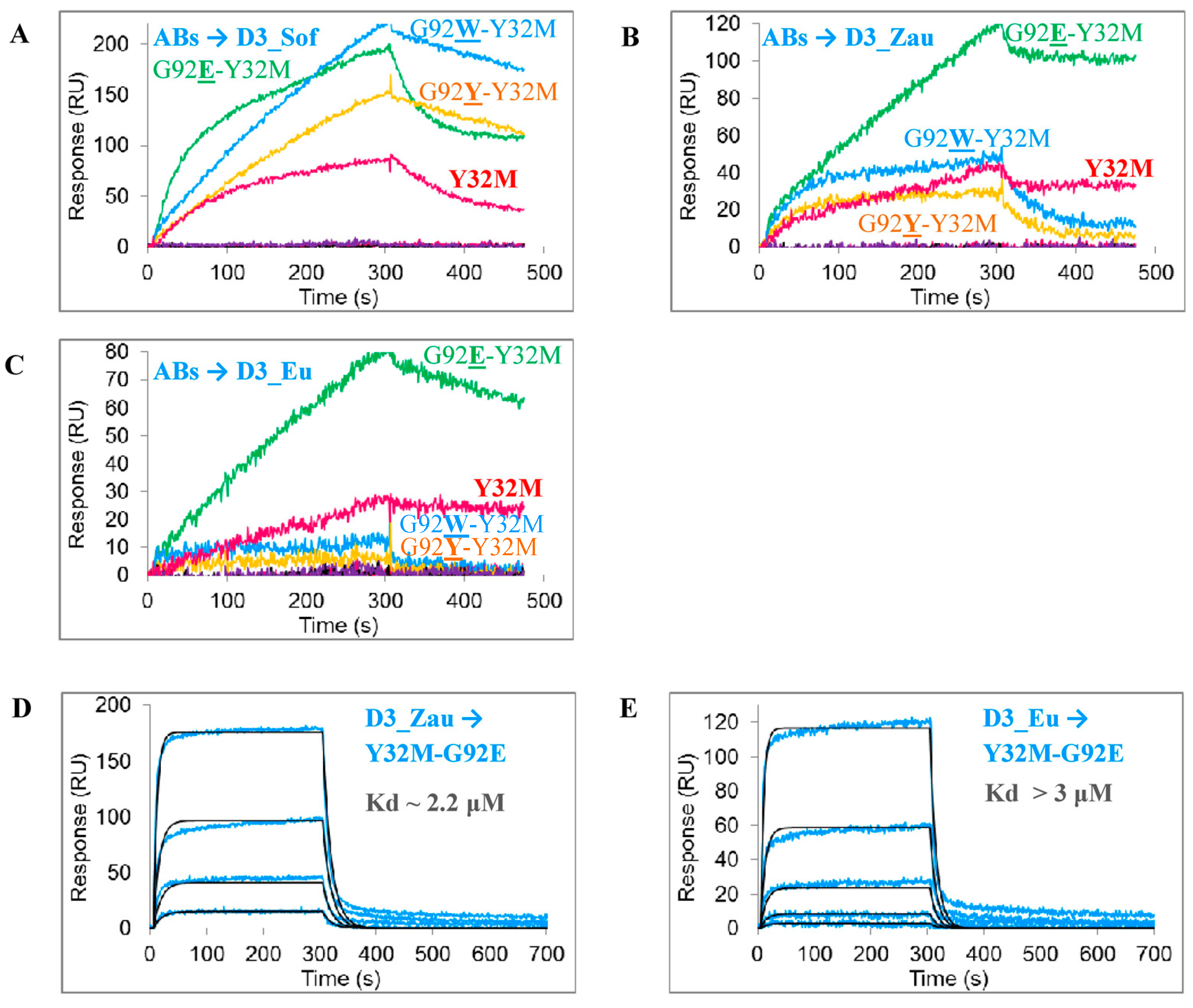
| Group | Name | Mutation 1 | Kd (D3_Sof) ± SD | Kd (D3_Zau) ± SD | Kd (D3_Eu) ± SD |
|---|---|---|---|---|---|
| Parental antibodies | ch14D5 (bivalently-bound) | No mutations | 2.0 ± 0.3 nM | 90 ± 20 nM | 300 ± 50 nM |
| fab_ch14D5 | 44 ± 6 nM | 1.7 ± 0.2 μM | >6 μM | ||
| sc14D5 | 40 ± 5 nM | 1.8 ± 0.2 μM | >6 μM | ||
| Group 1 (optimized interface geometry) | Y32H | L_Y32H | + | 1.7 ± 0.2μM | >2 μM |
| Y32M | L_Y32M | ~120 nM | 0.80 ± 0.11 μM | 1.6 ± 0.2 μM | |
| Y32Q | L_Y32Q | − | − | − | |
| Y50H | L_Y50H | − | − | − | |
| Y50Q | L_Y50Q | − | − | − | |
| F101L | H_F101L | − | − | − | |
| F101M | H_F101M | − | − | − | |
| F101Q | H_F101Q | − | − | − | |
| Group 2 (mmCSM-AB predicted mutations) | Y32M-G91F | L_Y32M + L_G91F | − | − | − |
| Y32M-G91W | L_Y32M + L_G91W | − | − | − | |
| Y32M-G92E | L_Y32M + L_G92E | + | 2.2 ± 0.2 μM | >3μM | |
| Y32M-G92W | L_Y32M + L_G92W | + | + | − | |
| Y32M-G92Y | L_Y32M + L_G92Y | + | + | − | |
| Y32M-G100W | L_Y32M + H_G100W | − | − | − | |
| Y32M-G100Y | L_Y32M + H_G100Y | − | − | − | |
| Y32M-A102W | L_Y32M + H_A102Y | − | − | − |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Baykov, I.K.; Desyukevich, P.Y.; Mikhaylova, E.E.; Kurchenko, O.M.; Tikunova, N.V. Computational and Rational Design of Single-Chain Antibody against Tick-Borne Encephalitis Virus for Modifying Its Specificity. Viruses 2021, 13, 1494. https://doi.org/10.3390/v13081494
Baykov IK, Desyukevich PY, Mikhaylova EE, Kurchenko OM, Tikunova NV. Computational and Rational Design of Single-Chain Antibody against Tick-Borne Encephalitis Virus for Modifying Its Specificity. Viruses. 2021; 13(8):1494. https://doi.org/10.3390/v13081494
Chicago/Turabian StyleBaykov, Ivan K., Pavel Y. Desyukevich, Ekaterina E. Mikhaylova, Olga M. Kurchenko, and Nina V. Tikunova. 2021. "Computational and Rational Design of Single-Chain Antibody against Tick-Borne Encephalitis Virus for Modifying Its Specificity" Viruses 13, no. 8: 1494. https://doi.org/10.3390/v13081494
APA StyleBaykov, I. K., Desyukevich, P. Y., Mikhaylova, E. E., Kurchenko, O. M., & Tikunova, N. V. (2021). Computational and Rational Design of Single-Chain Antibody against Tick-Borne Encephalitis Virus for Modifying Its Specificity. Viruses, 13(8), 1494. https://doi.org/10.3390/v13081494





