Case of Poliomyelitis Caused by Significantly Diverged Derivative of the Poliovirus Type 3 Vaccine Sabin Strain Circulating in the Orphanage
Abstract
1. Introduction
2. Materials and Methods
2.1. The Acute Flaccid Paralysis Case
2.2. Virological Methods
2.3. Serological Methods
2.4. Genome Sequencing
2.5. Bioinformatics Methods
2.6. GenBank Deposition
3. Results
3.1. A Case of VAPP in a Small Cluster of VDPV Excretors
3.2. Characterization of the Viral Isolates
3.3. Epidemiological Measures Carried Out in the Orphanage
4. Discussion
4.1. Genetic Features of Isolated Viruses
4.2. Epidemiological Assessment of the Situation
4.3. Implications for the Development of Vaccination Strategy for the Polio Eradication Program
4.4. Importance for Surveillance of Poliovirus Circulation
Supplementary Materials
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- Sutter, R.W.; Kew, O.M.; Cochi, S.L.; Aylward, R.B. Poliovirus vaccine—Live. In Vaccines, 7th ed.; Plotkin, S.A., Orenstein, W.A., Offit, P.A., Edwards, K.M., Eds.; Elsevier: Philadelphia, PA, USA; Amsterdam, The Netherlands, 2018; pp. 866–916. [Google Scholar]
- World Health Organization (WHO). Transmission of wild poliovirus type 2—Apparent global interruption. Wkly. Epidemiol. Rec. 2001, 76, 95–97. [Google Scholar]
- World Health Organization (WHO). Report from the Twentieth Meeting of the Global Commission for Certification of Poliomyelitis Eradication. In Proceedings of the Twentieth Meeting of the GCC, Geneva, Switzerland, 17–18 October 2019; Available online: http://polioeradication.org/wp-content/uploads/2016/07/20th-meeting-of-the-Global-Commission-for-the-Certification-of-Eradication-of-Poliomyelitis-17-18-October-2019.pdf (accessed on 5 August 2020).
- Centers for Disease Control and Prevention (CDC). Certification of poliomyelitis eradication—The Americas, 1994. MMWR Morb. Mortal. Wkly. Rep. 1994, 43, 720–722. [Google Scholar]
- Centers for Disease Control and Prevention (CDC). Certification of poliomyelitis eradication—The Western Pacific region, October 2000. MMWR Morb. Mortal. Wkly. Rep. 2001, 50, 1–3. [Google Scholar]
- Centers for Disease Control and Prevention (CDC). Certification of poliomyelitis eradication—European Region, June 2002. MMWR Morb. Mortal. Wkly. Rep. 2002, 51, 572–574. [Google Scholar]
- Bahl, S.; Kumar, R.; Menabde, N.; Thapa, A.; McFarland, J.; Swezy, V.; Tangermann, R.H.; Jafari, H.S.; Elsner, L.; Wassilak, S.G.F.; et al. Polio-free certification and lessons learned—South-East Asia. MMWR Morb. Mortal. Wkly. Rep. 2014, 63, 941–946. [Google Scholar]
- Sutter, R.W.; Cáceres, V.M.; Mas Lago, P. The role of routine polio immunization in the post-certification era. Bull. World Health Organ. 2004, 82, 31–39. [Google Scholar]
- Ivanova, O.E.; Eremeeva, T.P.; Morozova, N.S.; Shakaryan, A.K.; Korotkova, E.A.; Kozlovskaya, L.I.; Baykova, O.Y.; Krasota, A.Y.; Gmyl, A.P. Vaccine-associated paralytic poliomyelitis in the Russian Federation in 1998–2014. Int. J. Infect. Dis. 2018, 76, 64–69. [Google Scholar] [CrossRef]
- Burns, C.C.; Diop, O.M.; Sutter, R.W.; Kew, O.M. Vaccine-Derived Polioviruses. J. Infect. Dis. 2014, 210 (Suppl. 1), S283–S293. [Google Scholar] [CrossRef]
- World Health Organization (WHO). Global Polio Eradication Initiative 2020. Circulating Vaccine-Derived Poliovirus. Available online: http://polioeradication.org/wp-content/uploads/2020/06/weekly-polio-analyses-cVDPV-20200602.pdf (accessed on 8 June 2020).
- Jorba, J.; Diop, O.M.; Iber, J.; Henderson, E.; Zhao, K.; Quddus, A.; Sutter, R.; Vertefeuille, J.F.; Wenger, J.; Wassilak, S.G.F.; et al. Update on Vaccine-Derived Poliovirus Outbreaks—Worldwide, January 2018–June 2019. MMWR Morb. Mortal. Wkly. Rep. 2019, 68, 1024–1028. [Google Scholar] [CrossRef]
- Hampton, L.M.; Farrell, M.; Ramirez-Gonzalez, A.; Menning, L.; Shendale, S.; Lewis, I.; Rubin, J.; Garon, J.; Harris, J.; Hyde, T.; et al. Cessation of trivalent oral poliovirus vaccine and introduction of inactivated poliovirus vaccine: Worldwide, 2016. MMWR Morb. Mortal. Wkly. Rep. 2016, 65, 934–938. [Google Scholar] [CrossRef]
- World Health Organization (WHO). Standard Operating Procedures for Responding to a Poliovirus Event or Outbreak; WHO: Geneva, Switzerland, 2019; Available online: http://polioeradication.org/wp-content/uploads/2016/07/sop-polio-outbreak-response-version-20193101.pdf (accessed on 5 August 2020).
- Diop, O.M.; Asghar, H.; Gavrilin, E.; Moeletsi, N.G.; Benito, G.R.; Paladin, F.; Pattamadilok, S.; Zhang, Y.; Goel, A.; Quddus, A. Virologic monitoring of poliovirus type 2 after oral poliovirus vaccine type 2 withdrawal in April 2016—Worldwide, 2016–2017. MMWR Morb. Mortal. Wkly. Rep. 2017, 66, 538–542. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Garon, J.; Sutter, R.W.; Orenstein, W. High population immunity reduces poliovirus community transmission. Lancet Infect. Dis. 2017, 17, 1009–1011. [Google Scholar] [CrossRef]
- Jorba, J.; Diop, O.M.; Iber, J.; Henderson, E.; Zhao, K.; Sutter, R.W.; Wassilak, S.G.F.; Burns, C.C. Update on Vaccine-Derived Polioviruses—Worldwide, January 2017–June 2018. MMWR Morb. Mortal. Wkly. Rep. 2018, 67, 1189–1194. [Google Scholar] [CrossRef] [PubMed]
- Kalkowska, D.A.; Pallansch, M.A.; Thompson, K.M. Updated modelling of the prevalence of immunodeficiency-associated long-term vaccine-derived poliovirus (iVDPV) excreters. Epidemiol. Infect. 2019, 147, e295. [Google Scholar] [CrossRef]
- Roivainen, M.; Blomqvist, S.; Al-Hello, H.; Paananen, A.; Delpeyroux, F.; Kuusi, M.; Hovi, T. Highly divergent neurovirulent vaccine-derived polioviruses of all three serotypes are recurrently detected in Finnish sewage. Euro. Surveill. 2010, 15, 19566. [Google Scholar] [CrossRef]
- Al-Hello, H.; Jorba, J.; Blomqvist, S.; Raud, R.; Kew, O.; Roivainen, M. Highly divergent type 2 and 3 vaccine-derived polioviruses isolated from sewage in Tallinn, Estonia. J. Virol. 2013, 87, 13076–13080. [Google Scholar] [CrossRef][Green Version]
- World Health Organization (WHO). Guidelines for Implementing Poliovirus Surveillance among Patients with Primary Immunodeficiency Disorders (PIDs); WHO: Geneva, Switzerland, 2019; Available online: https://www.who.int/immunization/sage/meetings/2019/april/2_Guidelines_Implementing_PID_Suveillance.pdf?ua=1 (accessed on 5 August 2020).
- Alexander, J.P.; Ehresmann, K.; Seward, J.; Wax, G.; Harriman, K.; Fuller, S.; Cebelinski, E.A.; Chen, Q.; Jorba, J.; Kew, O.M.; et al. Transmission of imported vaccine-derived poliovirus in an undervaccinated community in Minnesota. J. Infect. Dis. 2009, 199, 391–397. [Google Scholar] [CrossRef]
- Avellon, A.; Cabrerizo, M.; de Miguel, T.; Pérez-Breña, P.; Tenorio, A.; Pérez, J.L.; Martínez de Aragón, M.V.; Trallero, G. Paralysis case and contact spread of recombinant vaccine-derived poliovirus, Spain. Emerg. Infect. Dis. 2008, 14, 1807–1809. [Google Scholar] [CrossRef]
- Federal Centre for Hygiene and Epidemiology of the Service for Surveillance on Consumer Rights Protection and Human Wellbeing (Rospotrebnadzor). Prevention of Poliomyelitis; Sanitary rules 3.1.2951-11; Federal Centre for Hygiene and Epidemiology of the Service for Surveillance on Consumer Rights Protection and Human Wellbeing (Rospotrebnadzor): Moscow, Russia, 2011. [Google Scholar]
- World Health Organization (WHO). Manual for Virological Investigation of Poliomyelitis; WHO/EPI/GEN/97.1: Geneva, Switzerland, 1997; Available online: http://whqlibdoc.who.int/hq/1997/WHO_EPI_GEN_97.01.pdf (accessed on 5 August 2020).
- World Health Organization (WHO). Manual for the Virological Investigation of Polio, 4th ed.; WHO: Geneva, Switzerland, 2004; Available online: http://whqlibdoc.who.int/hq/2004/WHO_IVB_04.10.pdf (accessed on 5 August 2020).
- van der Avoort, H.G.A.M.; Hull, B.P.; Hovi, T.; Pallansch, M.A.; Kew, O.M.; Crainic, R.; Wood, D.J.; Mulders, M.N.; van Loon, A.M. A comparative study of five methods of intratypic differentiation of polioviruses. J. Clin. Microbiol. 1995, 33, 2562–2566. [Google Scholar] [CrossRef]
- Kilpatrick, D.R.; Yang, C.F.; Ching, K.; Vincent, A.; Iber, J.; Campagnoli, R.; Mandelbaum, M.; De, L.; Yang, S.-J.; Nix, A.; et al. Rapid group-, serotype-, and vaccine strain-specific identification of poliovirus isolates by real-time reverse transcription-PCR using degenerate primers and probes containing deoxyinosine residues. J. Clin. Microbiol. 2009, 47, 1939–1941. [Google Scholar] [CrossRef]
- Tamura, K.; Stecher, G.; Peterson, D.; Filipski, A.; Kumar, S. MEGA6: Molecular Evolutionary Genetics Analysis version 6.0. Mol. Biol. Evol. 2013, 30, 2725–2729. [Google Scholar] [CrossRef] [PubMed]
- World Health Organization (WHO). Report of the Second Meeting of the Technical Consultation Group for Global Eradication of Poliomyelitis; WHO/EPI/GEN/98/04: Geneva, Switzerland, 1998; Available online: http://apps.who.int/iris/bitstream/10665/63994/1/WHO_EPI_GEN_98.04.pdf (accessed on 5 August 2020).
- Leschinskaya, E.V.; Latysheva, I.N. The Clinic, Diagnosis and Treatment of Acute Poliomyelitis. Guidelines; Institute of Poliomyelitis and Viral Encephalitis them, M.P. Chumakov Russian Academy of Medical Sciences: Moscow, Russia, 1998. [Google Scholar]
- World Health Organization (WHO). Classification and Reporting of Vaccine-Derived Polioviruses (VDPV); GPEI Guidelines; WHO: Geneva, Switzerland, 2016; Available online: http://polioeradication.org/wp-content/uploads/2016/09/Reporting-and-Classification-of-VDPVs_Aug2016_EN.pdf (accessed on 5 August 2020).
- Martín, J.; Dunn, G.; Hull, R.; Patel, V.; Minor, P.D. Evolution of the Sabin strain of type 3 poliovirus in an immunodeficient patient during the entire 637-day period of virus excretion. J. Virol. 2000, 74, 3001–3010. [Google Scholar] [CrossRef] [PubMed]
- Minor, P.D. The molecular biology of poliovaccines. J. Gen. Virol. 1992, 73, 3065–3077. [Google Scholar] [CrossRef] [PubMed]
- Rezapkin, G.V.; Douthitt, M.; Dragunsky, E.; Chumakov, K.M. Reevaluation of nucleotide sequences of wild-type and attenuated poliovirusesof type 3. Virus Res. 1999, 65, 111–119. [Google Scholar] [CrossRef]
- Minor, P.D.; Dunn, G.; Evans, D.M.; Magrath, D.I.; John, A.; Howlett, J.; Phillips, A.; Westrop, G.; Wareham, K.; Almond, J.W. The temperature sensitivity of the Sabin type 3 vaccine strain of poliovirus: Molecular and structural effects of a mutation in the capsid protein VP3. J. Gen. Virol. 1989, 70, 1117–1123. [Google Scholar] [CrossRef]
- Yakovenko, M.L.; Cherkasova, E.A.; Rezapkin, G.V.; Ivanova, O.E.; Ivanov, A.P.; Eremeeva, T.P.; Baykova, O.Y.; Chumakov, K.M.; Agol, V.I. Antigenic evolution of vaccine-derived polioviruses: Changes in individual epitopes and relative stability of the overall immunological properties. J. Virol. 2006, 80, 2641–2653. [Google Scholar] [CrossRef]
- Belnap, D.M.; McDermott, B.M., Jr.; Filman, D.; Cheng, N.; Trus, B.L.; Zuccola, H.J.; Racaniello, V.R.; Hogle, J.M.; Steven, A.C. Three-dimensional structure of poliovirus receptor bound to poliovirus. Proc. Natl. Acad. Sci. USA 2000, 97, 73–78. [Google Scholar] [CrossRef]
- Pilipenko, E.V.; Blinov, V.M.; Romanova, L.I.; Sinyakov, A.N.; Maslova SVAgol, V.I. Conserved structural domains in the 5′-untranslated region of picornaviral genomes: An analysis of the segment controlling translation and neurovirulence. Virology 1989, 168, 201–209. [Google Scholar] [CrossRef]
- Han, J.Q.; Townsend, H.L.; Jha, B.K.; Paranjape, J.M.; Silverman, R.H.; Barton, D.J. A phylogenetically conserved RNA structure in the poliovirus open reading frame inhibits the antiviral endoribonuclease RNase L. J. Virol. 2007, 81, 5561–5572. [Google Scholar] [CrossRef]
- Burrill, C.P.; Westesson, O.; Schulte, M.B.; Strings, V.R.; Segal, M.; Andino, R.J. Global RNA structure analysis of poliovirus identifies a conserved RNA structure involved in viral replication and infectivity. Virology 2013, 87, 11670–11683. [Google Scholar] [CrossRef]
- Korotkova, E.; Laassri, M.; Zagorodnyaya, T.; Petrovskaya, S.; Rodionova, E.; Cherkasova, E.; Gmyl, A.; Ivanova, O.E.; Eremeeva, T.; Lipskaya, G.Y.; et al. Pressure for Pattern-Specific Intertypic Recombination between Sabin Polioviruses: Evolutionary Implications. Viruses 2017, 9, 353. [Google Scholar] [CrossRef] [PubMed]
- WHO Global Polio Eradication Initiative. Available online: http://polioeradication.org/polio-today/polio-now/ (accessed on 5 August 2020).
- Kew, O.M.; Sutter, R.W.; de Gourville, E.M.; Dowdle, W.R.; Pallansch, M.A. Vaccine-derived polioviruses and the endgame strategy for global polio eradication. Annu. Rev. Microbiol. 2005, 59, 587–635. [Google Scholar] [CrossRef]
- Platt, L.R.; Estivariz, C.F.; Sutter, R.W. Vaccine-associated paralytic poliomyelitis: Are view of the epidemiology and estimation of the global burden. J. Infect. Dis. 2014, 210, 380–389. [Google Scholar] [CrossRef] [PubMed]
- Korotkova, E.A.; Gmyl, A.P.; Yakovenko, M.L.; Ivanova, O.E.; Eremeeva, T.P.; Kozlovskaya, L.I.; Shakaryan, A.K.; Lipskaya, G.Y.; Parshina, I.L.; Loginovskikh, N.V.; et al. A Cluster of Paralytic Poliomyelitis Cases Due to Transmission of Slightly Diverged Sabin 2 Vaccine Poliovirus. J. Virol. 2016, 90, 5978–5988. [Google Scholar] [CrossRef] [PubMed]
- Westrop, G.D.; Wareham, K.A.; Evans, D.M.; Dunn, G.; Minor, P.D.; Magrath, D.I.; Taffs, F.; Marsden, S.; Skinner, M.A.; Schild, G.C. Genetic basis of attenuation of the Sabin type 3 oral poliovirus vaccine. J. Virol. 1989, 63, 1338–1344. [Google Scholar] [CrossRef] [PubMed]
- Cuervo, N.S.; Guillot, S.; Romanenkova, N.; Combiescu, M.; Aubert-Combiescu, A.; Seghier, M.; Caro, V.; Crainic, R.; Delpeyroux, F. Genomic features of intertypic recombinant Sabin poliovirus strains excreted by primary vaccinees. J. Virol. 2001, 75, 5740–5751. [Google Scholar] [CrossRef]
- Guillot, S.; Caro, V.; Cuervo, N.; Korotkova, E.; Combiescu, M.; Persu, A.; Aubert-Combiescu, A.; Delpeyroux, F.; Crainic, R. Natural genetic exchanges between vaccine and wild poliovirus strains in humans. J. Virol. 2000, 74, 8434–8443. [Google Scholar] [CrossRef]
- Ministry of Health of the Russian Federation. On Approval of the National Calendar of Preventive Vaccinations and the Calendar of Preventive Vaccinations according to Epidemic Indications; Order of March 21, 2014 N 125н; Ministry of Health of the Russian Federation: Moscow, Russia, 2014. [Google Scholar]
- World Health Organization (WHO). Meeting of the Strategic Advisory Group of Experts on immunization, April 2017—Conclusions and recommendations. Wkly. Epidemiol. Rec. 2017, 9, 301–320. [Google Scholar]
- Korotkova, E.A.; Park, R.; Cherkasova, E.A.; Lipskaya, G.Y.; Chumakov, K.M.; Feldman, E.V.; Kew, O.M.; Agol, V.I. Retrospective Analysis of a Local Cessation of Vaccination Against Poliomyelitis: A Possible Scenario for the Future. J. Virol. 2003, 77, 12460–12465. [Google Scholar] [CrossRef]
- Sanders, B.P.; de Los Rios Oakes, I.; van Hoek, V.; Bockstal, V.; Kamphuis, T.; Uil, T.G.; Song, Y.; Cooper, G.; Crawt, L.E.; Martín, J.; et al. Cold-Adapted Viral Attenuation (CAVA): Highly Temperature Sensitive Polioviruses as Novel Vaccine Strains for a Next Generation Inactivated Poliovirus Vaccine. PLoS Pathog. 2016, 12, e1005483. [Google Scholar] [CrossRef]
- Fox, H.; Knowlson, S.; Minor, P.D.; Macadam, A.J. Genetically Thermo-Stabilised, Immunogenic Poliovirus Empty Capsids; a Strategy for Non-replicating Vaccines. PLoS Pathog. 2017, 13, e1006117. [Google Scholar] [CrossRef] [PubMed]
- Van Damme, P.; De Coster, I.; Bandyopadhyay, A.; Revets, H.; Withanage, K.; De Smedt, P.; Suykens, L.; Oberste, M.S.; Weldon, W.C.; Costa-Clemens, S.A.; et al. The safety and immunogenicity of two novel live attenuated monovalent (serotype2) oral poliovirus vaccines in healthy adults: A double-blind, single-centre phase 1 study. Lancet 2019, 394, 148–158. [Google Scholar] [CrossRef]
- Konopka-Anstadt, J.L.; Campagnoli, R.; Vincent, A.; Shaw, J.; Wei, L.; Wynn, N.T.; Smithee, S.E.; Bujaki, E.; Yeh, M.T.; Laassri, M.; et al. Development of a new oral poliovirus vaccine for the eradication end game using codon deoptimization. NPJ Vaccines 2020, 5, 26. [Google Scholar] [CrossRef]
- Li, L.; Ivanova, O.; Driss, N.; Tiongco-Recto, M.; da Silva, R.; Shahmahmoodi, S.; Sazzad, H.M.S.; Mach, O.; Kahn, A.-L.; Sutter, R.W. Poliovirus excretion among persons with primary immune deficiency disorders: Summary of a seven-country study series. J. Infect. Dis. 2014, 210 (Suppl. 1), 368–372. [Google Scholar] [CrossRef] [PubMed]
- Aghamohammadi, A.; Abolhassani, H.; Kutukculer, N.; Wassilak, S.G.; Pallansch, M.A.; Kluglein, S.; Quinn, J.; Sutter, R.W.; Wang, X.; Sanal, O.; et al. Patients with Primary Immunodeficiencies Are a Reservoir of Poliovirus and a Risk to Polio Eradication. Front. Immunol. 2017, 8, 685. [Google Scholar] [CrossRef]
- Guo, J.; Bolivar-Wagers, S.; Srinivas, N.; Holubar, M.; Maldonado, Y. Immunodeficiency-related Vaccine-Derived Poliovirus (iVDPV) Cases: A Systematic Review and Implications for Polio Eradication. Vaccine 2015, 33, 1235–1242. [Google Scholar] [CrossRef]
- Ivanova, O.E.; Yarmolskaya, M.S.; Eremeeva, T.P.; Babkina, G.M.; Baykova, O.Y.; Akhmadishina, L.V.; Krasota, A.Y.; Kozlovskaya, L.I.; Lukashev, A.N. Environmental surveillance for poliovirus and other enteroviruses: Long-term experience in Moscow, Russian Federation, 2004–2017. Viruses 2019, 11, 424. [Google Scholar] [CrossRef]
| The Contacts (Age in Months at the Time of the Acute Flaccid Paralysis (AFP) Case Detection) | Number of IPV (+OPV) Doses before the First Serological Examination | Antibody Titer (7–8 October 2014) against Poliovirus Serotype: | Number of IPV Doses between Two Serological Examinations | Antibody Titer (24 November 2014) against Poliovirus Serotype: | ||||
|---|---|---|---|---|---|---|---|---|
| 1 | 2 | 3 | 1 | 2 | 3 | |||
| C-4 (23) | 2 (+3) | 1:64 | 1:256 | 1:32 | 0 | ND *** | ND | ND |
| C-5 (41) | 2 (+3) | <1:8 | 1:128 | <1:8 | 0 | <1:8 | 1:256 | <1:8 |
| C-6 * (31) | 2 (+3) | 1:512 | 1:512 | 1:1024 | 0 | 1:256 | 1:256 | 1:512 |
| C-7 (31) | 3 (+2) | 1:512 | 1:512 | 1:512 | 0 | 1:512 | 1:256 | 1:256 |
| C-8 (33) | 3 (+2) | 1:32 | 1:128 | 1:256 | 0 | 1:64 | 1:128 | 1:128 |
| C-9 (41) | 3 (+2) | 1:64 | 1:64 | 1:16 | 0 | 1:64 | 1:64 | 1:8 |
| C-10 (36) | 4 (+1) | 1:512 | 1:512 | 1:128 | 0 | 1:256 | 1:512 | 1:256 |
| C-11 (12) | 2 (+1) | 1:32 | 1:64 | 1:16 | 0 | 1:16 | 1:64 | 1:16 |
| C-12 (13) | 2 (+1) | 1:64 | 1:64 | 1:512 | 1 | 1:512 | 1:512 | 1:512 |
| C-13 (30) | 6 | 1:64 | 1:256 | >1:1024 | 0 | 1:64 | 1:128 | 1:256 |
| C-14 (25) | 6 | 1:128 | 1:128 | 1:128 | 0 | 1:64 | 1:128 | 1:64 |
| C-15 (44) | 5 | >1:1024 | 1:512 | 1:512 | 0 | >1:1024 | 1:512 | 1:512 |
| C-16 * (25) | 5 | 1:512 | 1:512 | 1:256 | 0 | 1:128 | 1:256 | 1:128 |
| C-17 (31) | 5 | 1:64 | 1:32 | 1:512 | 0 | 1:32 | 1:64 | 1:256 |
| C-18 (41) | 5 | 1:64 | 1:128 | 1:256 | 0 | 1:64 | 1:256 | 1:128 |
| C-19 (47) | 5 | 1:32 | 1:256 | 1:64 | 0 | 1:64 | 1:256 | 1:64 |
| C-20 (20) | 5 | 1:64 | 1:128 | 1:64 | 0 | 1:64 | 1:128 | 1:64 |
| C-21 (33) | 5 | 1:32 | 1:128 | 1:16 | 0 | 1:16 | 1:64 | <1:8 |
| C-22 (24) | 4 | >1:1024 | 1:1024 | 1:256 | 0 | 1:512 | 1:256 | 1:128 |
| C-23 (21) | 4 | 1:64 | 1:128 | 1:256 | 0 | 1:256 | 1:64 | 1:256 |
| C-2 ** (22) | 4 | 1:64 | 1:128 | 1:256 | 0 | 1:16 | 1:16 | 1:128 |
| C-1 ** (20) | 4 | <1:8 | <1:8 | 1:64 | 1 | 1:64 | 1:16 | 1:64 |
| C-24 (21) | 3 | 1:1024 | 1:256 | 1:512 | 0 | 1:256 | 1:256 | 1:128 |
| C-25 (11) | 3 | 1:256 | 1:512 | 1:256 | 0 | 1:32 | 1:128 | 1:64 |
| C-26 * (23) | 3 | 1:256 | 1:256 | 1:512 | 0 | 1:128 | 1:256 | 1:128 |
| C-27 (52) | 2 | 1:512 | 1:1024 | 1:512 | 1 | 1:128 | 1:256 | 1:512 |
| C-28 (9) | 2 | 1:256 | 1:256 | 1:128 | 1 | 1:256 | 1:256 | 1:64 |
| C-29 (10) | 2 | 1:64 | 1:256 | 1:128 | 1 | 1:64 | 1:256 | 1:512 |
| C-30 (43) | 2 | 1:32 | 1:256 | 1:256 | 1 | 1:16 | 1:128 | 1:512 |
| C-31 (11) | 2 | 1:16 | 1:32 | 1:256 | 1 | 1:128 | 1:128 | 1:256 |
| C-32 (9) | 2 | 1:32 | 1:128 | 1:64 | 1 | 1:256 | 1:512 | 1:256 |
| C-33 (9) | 2 | <1:8 | 1:16 | 1:256 | 1 | 1:8 | 1:32 | 1:256 |
| C-34 (14) | 2 | <1:8 | <1:8 | 1:128 | 1 | 1:64 | 1:32 | 1:256 |
| C-35 * (5) | 1 | 1:512 | 1:512 | 1:128 | 1 | 1:256 | 1:256 | 1:16 |
| C-36 (1) | 1 | 1:64 | 1:128 | 1:64 | 1 | 1:512 | 1:512 | 1:256 |
| C-37 (24) | 1 | 1:32 | 1:16 | 1:8 | 1 | 1:128 | 1:128 | 1:32 |
| C-38 (3) | 1 | 1:8 | 1:64 | 1:32 | 1 | 1:256 | 1:256 | 1:256 |
| C-39 (38) | 1 | 1:8 | 1:64 | 1:16 | 1 | 1:128 | 1:64 | 1:8 |
| C-40 (13) | 1 | <1:8 | 1:8 | 1:128 | 1 | 1:64 | 1:64 | 1:512 |
| C-41 (1) | 1 | <1:8 | 1:32 | <1:8 | 1 | 1:128 | 1:64 | 1:128 |
| C-42 (4) | 1 | <1:8 | 1:8 | <1:8 | 2 | 1:64 | 1:128 | 1:32 |
| C-43 (4) | 1 | <1:8 | <1:8 | <1:8 | 1 | 1:64 | 1:64 | 1:64 |
| C-44 (23) | 1 | <1:8 | 1:8 | 1:256 | 0 | ND | ND | ND |
| C-45 (1) | 1 | <1:8 | <1:8 | <1:8 | 0 | ND | ND | ND |
| C-46 (0) | 0 | <1:8 | <1:8 | <1:8 | 2 | 1:16 | 1:16 | <1:8 |
| C-47 (35) | 0 | <1:8 | <1:8 | <1:8 | 2 | 1:8 | <1:8 | 1:8 |
| C-48 (13) | 0 | <1:8 | <1:8 | <1:8 | 2 | <1:8 | <1:8 | 1:8 |
| C-49 (2) | 0 | <1:8 | <1:8 | <1:8 | 2 | <1:8 | <1:8 | <1:8 |
| C-50 (6) | 0 | <1:8 | <1:8 | <1:8 | 2 | <1:8 | <1:8 | <1:8 |
| C-51 (7) | 0 | <1:8 | <1:8 | <1:8 | 2 | <1:8 | <1:8 | <1:8 |
| C-52 (8) | 0 | <1:8 | <1:8 | <1:8 | 2 | <1:8 | <1:8 | <1:8 |
| C-53 (16) | 0 | <1:8 | <1:8 | <1:8 | 2 | <1:8 | <1:8 | <1:8 |
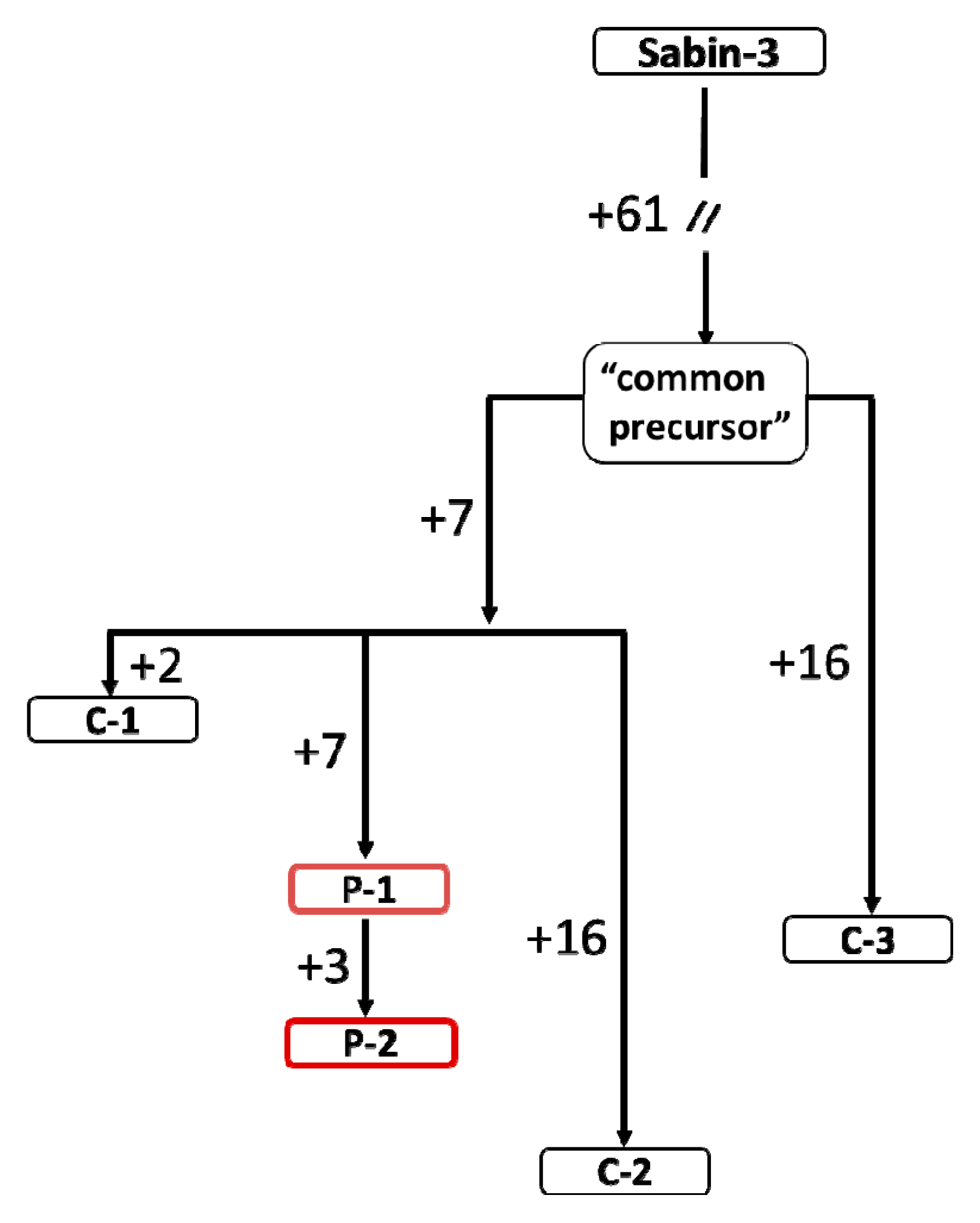
| Isolate Genome | Number of Mutations Per Genome | Approximated Age, Months * |
|---|---|---|
| “Common ancestor” | 61 | 7.7 |
| P-1 | 75 | 9.5 |
| P-2 | 78 | 9.8 |
| C-1 | 70 | 8.8 |
| C-2 | 84 | 10.6 |
| C-3 | 77 | 9.7 |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Korotkova, E.A.; Prostova, M.A.; Gmyl, A.P.; Kozlovskaya, L.I.; Eremeeva, T.P.; Baikova, O.Y.; Krasota, A.Y.; Morozova, N.S.; Ivanova, O.E. Case of Poliomyelitis Caused by Significantly Diverged Derivative of the Poliovirus Type 3 Vaccine Sabin Strain Circulating in the Orphanage. Viruses 2020, 12, 970. https://doi.org/10.3390/v12090970
Korotkova EA, Prostova MA, Gmyl AP, Kozlovskaya LI, Eremeeva TP, Baikova OY, Krasota AY, Morozova NS, Ivanova OE. Case of Poliomyelitis Caused by Significantly Diverged Derivative of the Poliovirus Type 3 Vaccine Sabin Strain Circulating in the Orphanage. Viruses. 2020; 12(9):970. https://doi.org/10.3390/v12090970
Chicago/Turabian StyleKorotkova, Ekaterina A., Maria A. Prostova, Anatoly P. Gmyl, Liubov I. Kozlovskaya, Tatiana P. Eremeeva, Olga Y. Baikova, Alexandr Y. Krasota, Nadezhda S. Morozova, and Olga E. Ivanova. 2020. "Case of Poliomyelitis Caused by Significantly Diverged Derivative of the Poliovirus Type 3 Vaccine Sabin Strain Circulating in the Orphanage" Viruses 12, no. 9: 970. https://doi.org/10.3390/v12090970
APA StyleKorotkova, E. A., Prostova, M. A., Gmyl, A. P., Kozlovskaya, L. I., Eremeeva, T. P., Baikova, O. Y., Krasota, A. Y., Morozova, N. S., & Ivanova, O. E. (2020). Case of Poliomyelitis Caused by Significantly Diverged Derivative of the Poliovirus Type 3 Vaccine Sabin Strain Circulating in the Orphanage. Viruses, 12(9), 970. https://doi.org/10.3390/v12090970





