Amino Acid at Position 166 of NS2A in Japanese Encephalitis Virus (JEV) Is Associated with In Vitro Growth Characteristics of JEV
Abstract
1. Introduction
2. Materials and Methods
2.1. Cell Culture
2.2. Viruses
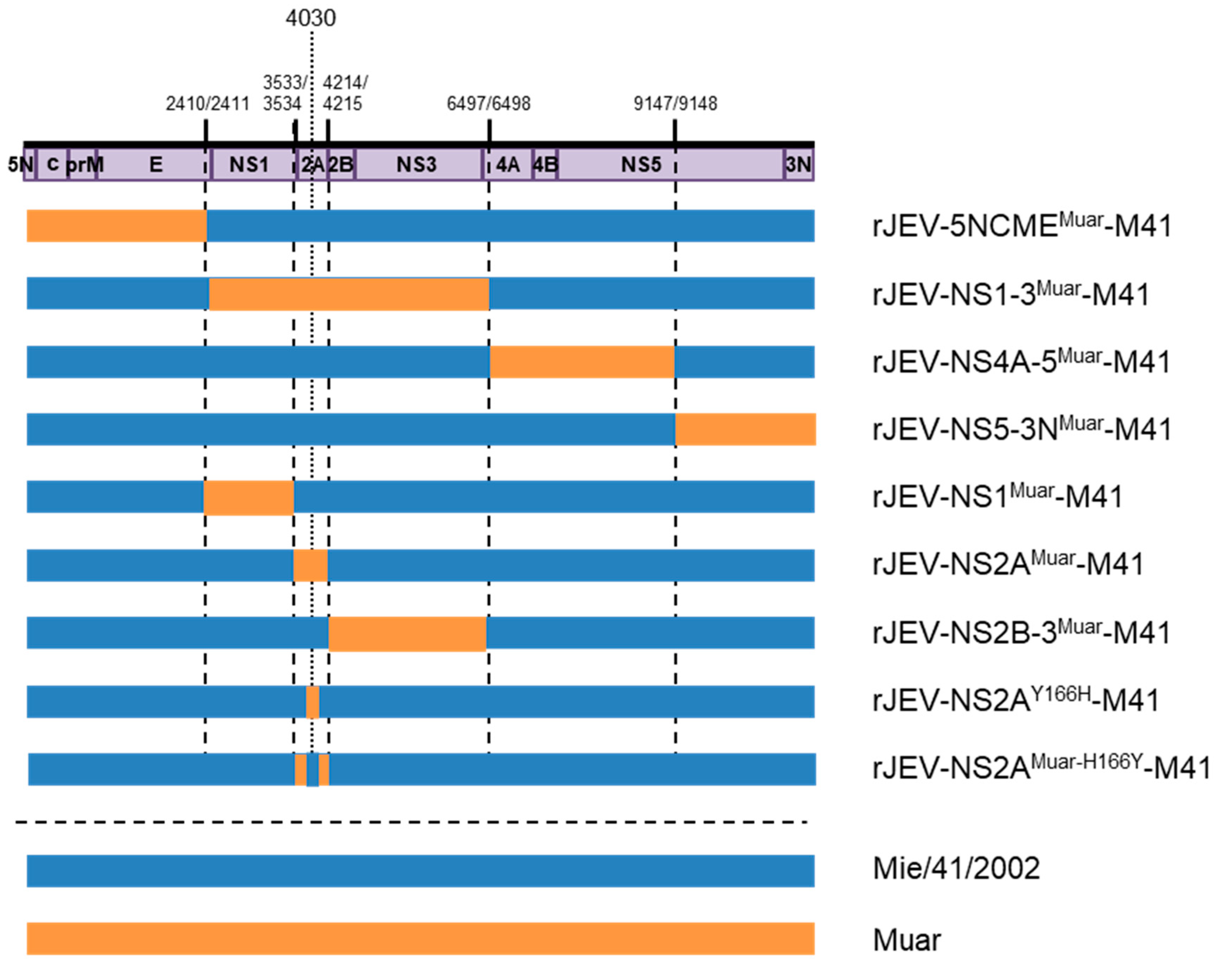
2.3. Recombinant Viruses
2.4. Plaque-Formation Assay and Analysis of Growth Kinetics
2.5. Adaptation of Virus to Mouse Neuroblastoma Cells
2.6. Plaque Cloning (Limiting-Dilution Method)
2.7. Statistical Analysis
3. Results
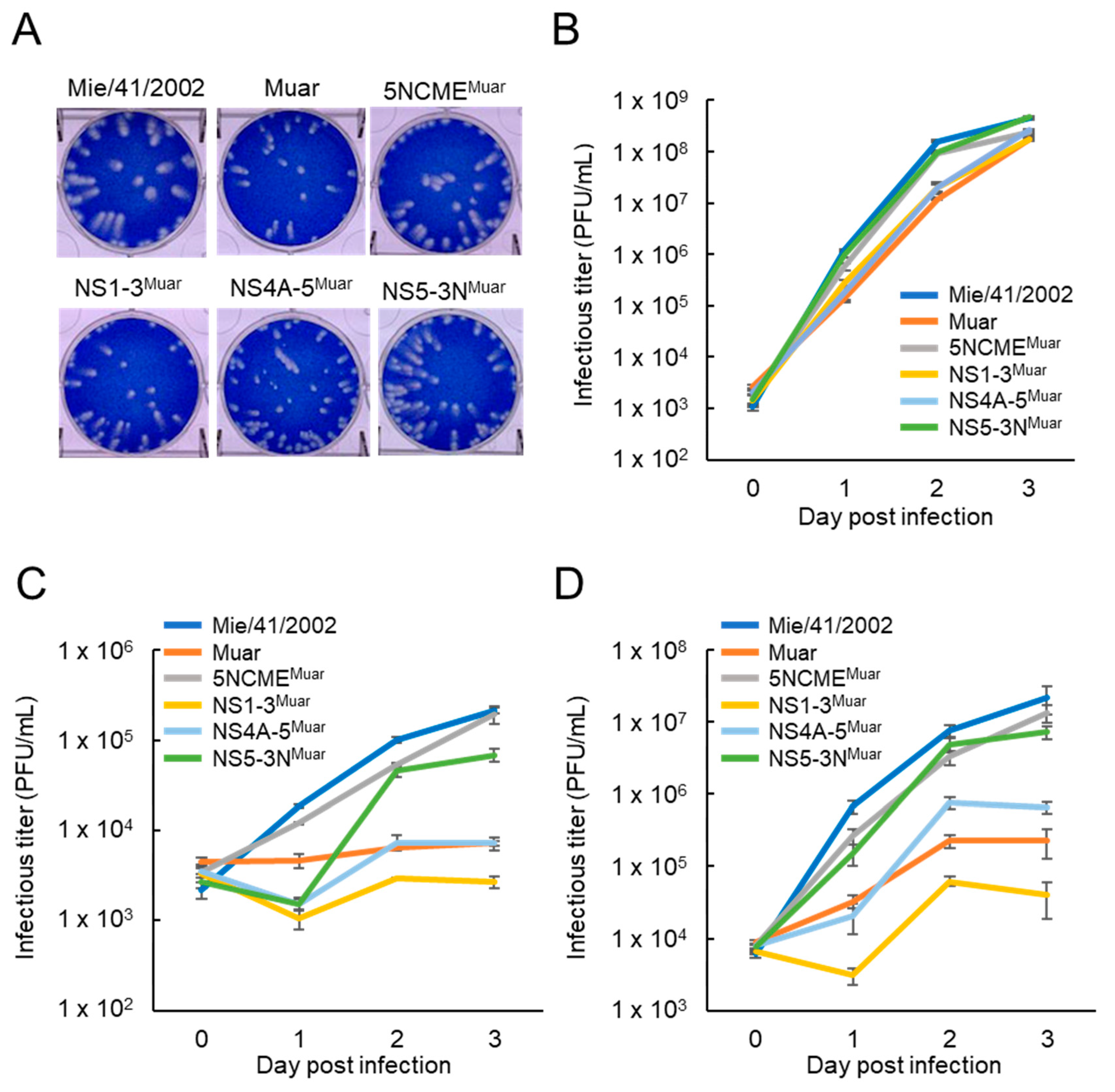
3.1. Growth of GI-GV Intertypic Mutants 5NCMEMuar, NS1-3Muar, NS4A-5Muar, and NS5-3NMuar in Mouse Neuroblastoma Cells
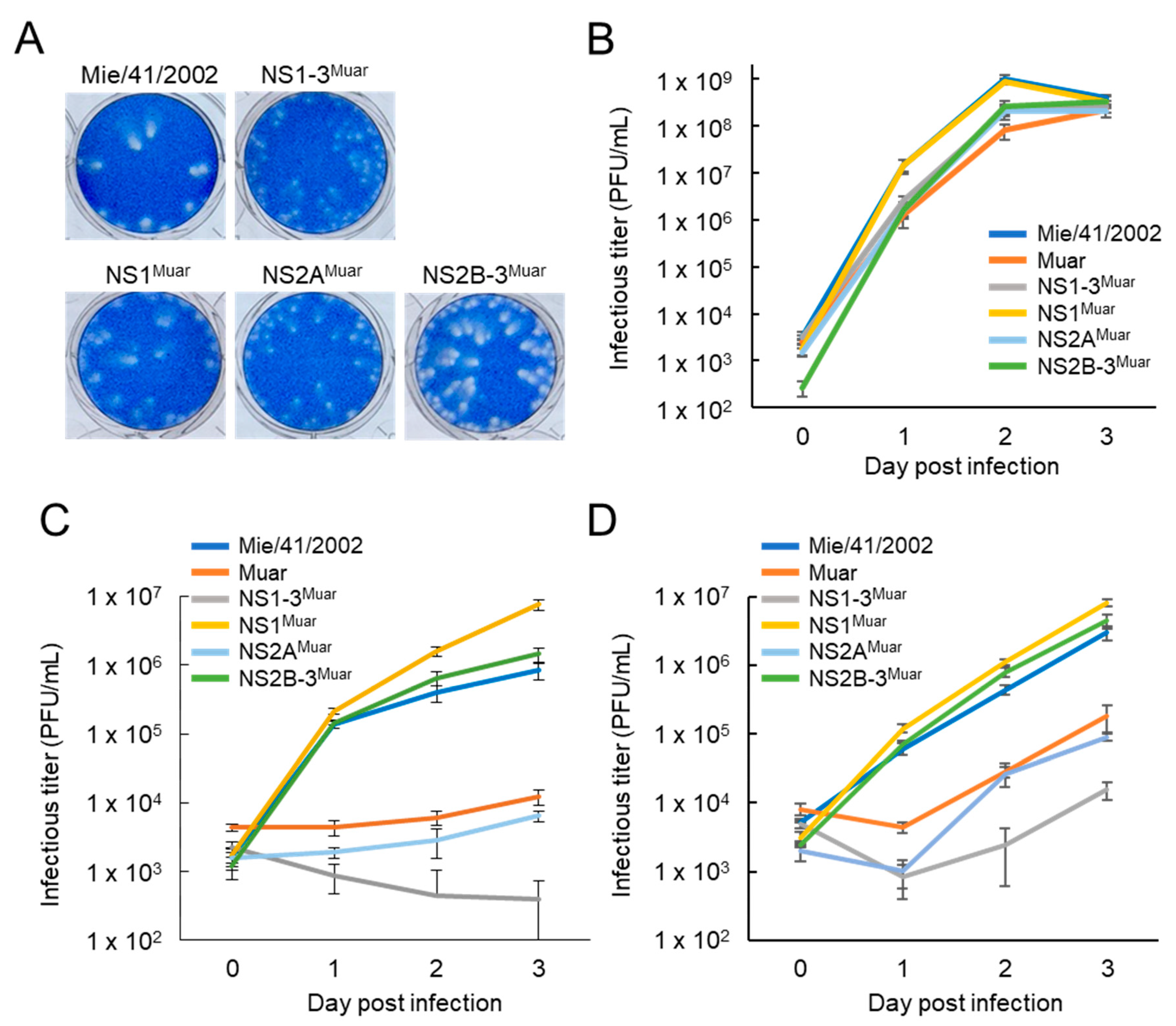
3.2. Growth of GI-GV Intertypic Mutants NS1Muar, NS2AMuar, and NS2B-3Muar in Mouse Neuroblastoma Cells
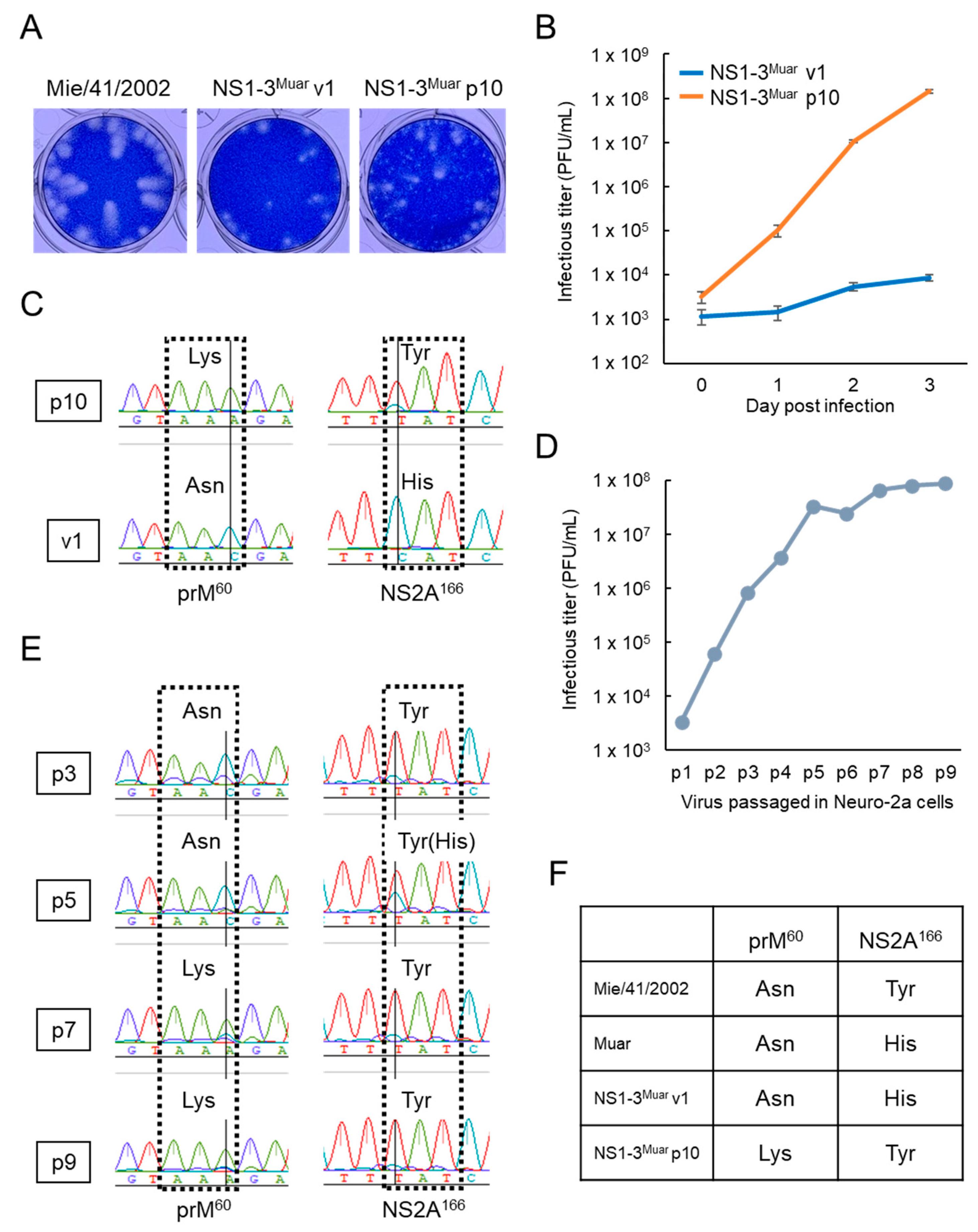
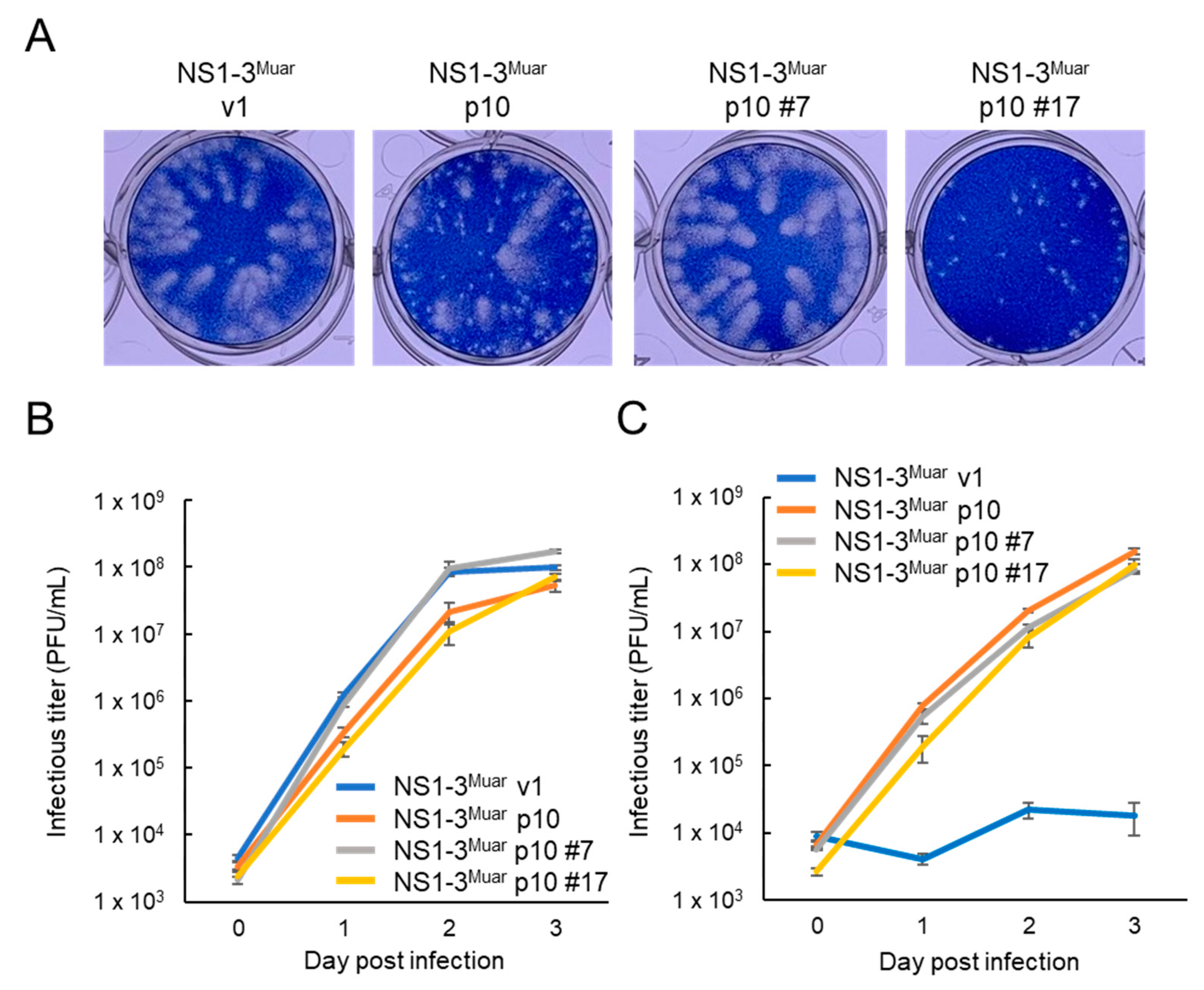
3.3. Adaptation of NS1-3Muar to Mouse Neuroblastoma Neuro-2a Cells
3.4. Characterization of Neuro-2a-Adapted NS1-3Muar p10 Clones
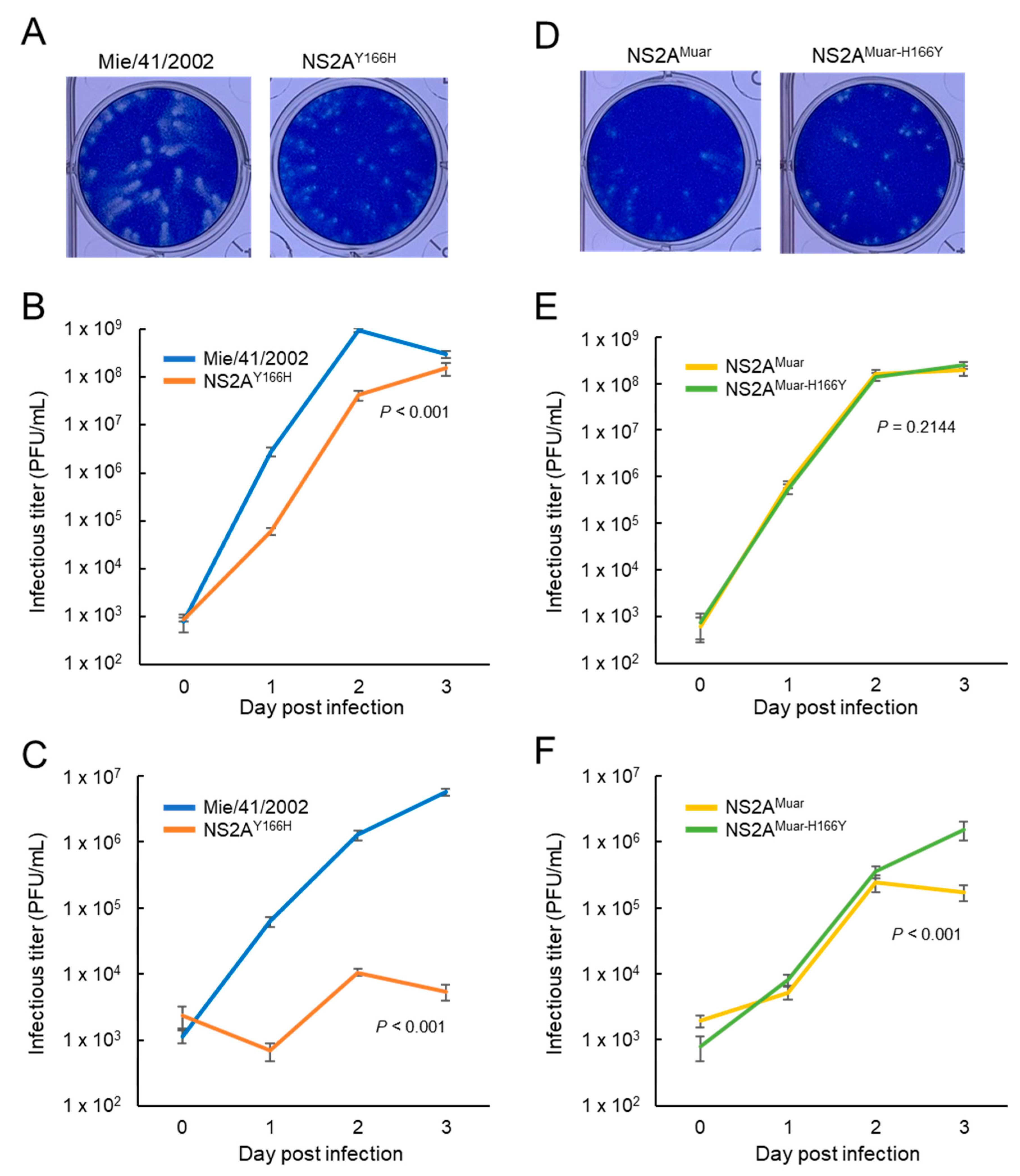
3.5. Growth of Site-Directed Mutants NS2AY166H and NS2AMuar-H166Y in Mouse Neuroblastoma Cells
4. Discussion
Supplementary Materials
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- Tsai, T.F. New initiatives for the control of Japanese encephalitis by vaccination: Minutes of a who/cvi meeting, Bangkok, Thailand, 13–15 October 1998. Vaccine 2000, 18, 1–25. [Google Scholar] [CrossRef]
- Erlanger, T.E.; Weiss, S.; Keiser, J.; Utzinger, J.; Wiedenmayer, K. Past, present, and future of Japanese encephalitis. Emerg Infect. Dis. 2009, 15, 1–7. [Google Scholar] [CrossRef] [PubMed]
- Campbell, G.L.; Hills, S.L.; Fischer, M.; Jacobson, J.A.; Hoke, C.H.; Hombach, J.M.; Marfin, A.A.; Solomon, T.; Tsai, T.F.; Tsu, V.D.; et al. Estimated global incidence of Japanese encephalitis: A systematic review. Bull. World Health Organ. 2011, 89, 766–774. [Google Scholar] [CrossRef]
- Pierson, T.C.; Diamond, M.S. Flaviviruses. In Fields Virology, 6th ed.; Knipe, D.M., Howley, P.M., Eds.; Lippincott Williams & Wilkins: Philadelphia, PA, USA, 2013; pp. 747–794. [Google Scholar]
- Uchil, P.D.; Satchidanandam, V. Phylogenetic analysis of Japanese encephalitis virus: Envelope gene based analysis reveals a fifth genotype, geographic clustering, and multiple introductions of the virus into the Indian subcontinent. Am. J. Trop. Med. Hyg. 2001, 65, 242–251. [Google Scholar] [CrossRef]
- Solomon, T.; Ni, H.; Beasley, D.W.; Ekkelenkamp, M.; Cardosa, M.J.; Barrett, A.D. Origin and evolution of Japanese encephalitis virus in Southeast Asia. J. Virol. 2003, 77, 3091–3098. [Google Scholar] [CrossRef]
- Gao, X.; Liu, H.; Wang, H.; Fu, S.; Guo, Z.; Liang, G. Southernmost Asia is the source of Japanese encephalitis virus (genotype 1) diversity from which the viruses disperse and evolve throughout Asia. PLoS Negl. Trop. Dis. 2013, 7, e2459. [Google Scholar] [CrossRef]
- Schuh, A.J.; Ward, M.J.; Leigh Brown, A.J.; Barrett, A.D. Dynamics of the emergence and establishment of a newly dominant genotype of Japanese encephalitis virus throughout Asia. J. Virol. 2014, 88, 4522–4532. [Google Scholar] [CrossRef]
- Kuwata, R.; Torii, S.; Shimoda, H.; Supriyono, S.; Phichitraslip, T.; Prasertsincharoen, N.; Takemae, H.; Bautista, R.; Ebora, V.; Abella, J.A.C.; et al. Distribution of Japanese encephalitis virus, Japan and Southeast asia, 2016–2018. Emerg. Infect. Dis. 2020, 26, 125–128. [Google Scholar] [CrossRef]
- Li, M.H.; Fu, S.H.; Chen, W.X.; Wang, H.Y.; Guo, Y.H.; Liu, Q.Y.; Li, Y.X.; Luo, H.M.; Da, W.; Duo Ji, D.Z.; et al. Genotype V Japanese encephalitis virus is emerging. PLoS Negl. Trop. Dis. 2011, 5, e1231. [Google Scholar] [CrossRef]
- Takhampunya, R.; Kim, H.C.; Tippayachai, B.; Kengluecha, A.; Klein, T.A.; Lee, W.J.; Grieco, J.; Evans, B.P. Emergence of Japanese encephalitis virus genotype V in the Republic of Korea. Virol. J. 2011, 8, 449. [Google Scholar] [CrossRef] [PubMed]
- Kim, H.; Cha, G.W.; Jeong, Y.E.; Lee, W.G.; Chang, K.S.; Roh, J.Y.; Yang, S.C.; Park, M.Y.; Park, C.; Shin, E.H. Detection of Japanese encephalitis virus genotype V in culex orientalis and culex pipiens (diptera: Culicidae) in Korea. PLoS ONE 2015, 10, e0116547. [Google Scholar] [CrossRef] [PubMed]
- Bae, W.; Kim, J.H.; Kim, J.; Lee, J.; Hwang, E.S. Changes of epidemiological characteristics of Japanese encephalitis viral infection and birds as a potential viral transmitter in Korea. J. Korean Med. Sci. 2018, 33, e70. [Google Scholar] [CrossRef] [PubMed]
- Woo, J.H.; Jeong, Y.E.; Jo, J.E.; Shim, S.M.; Ryou, J.; Kim, K.C.; Lee, W.J.; Lee, J.Y. Genetic characterization of Japanese encephalitis virus genotype 5 isolated from patient, South Korea, 2015. Emerg. Infect. Dis. 2020, 26, 1002–1006. [Google Scholar] [CrossRef]
- Cao, L.; Fu, S.; Gao, X.; Li, M.; Cui, S.; Li, X.; Cao, Y.; Lei, W.; Lu, Z.; He, Y.; et al. Low protective efficacy of the current Japanese encephalitis vaccine against the emerging genotype 5 Japanese encephalitis virus. PLoS Negl. Trop. Dis. 2016, 10, e0004686. [Google Scholar] [CrossRef]
- Tajima, S.; Yagasaki, K.; Kotaki, A.; Tomikawa, T.; Nakayama, E.; Moi, M.L.; Lim, C.K.; Saijo, M.; Kurane, I.; Takasaki, T. In vitro growth, pathogenicity and serological characteristics of the Japanese encephalitis virus genotype V muar strain. J. Gen. Virol. 2015, 96, 2661–2669. [Google Scholar] [CrossRef] [PubMed]
- De Wispelaere, M.; Frenkiel, M.P.; Despres, P. A Japanese encephalitis virus genotype 5 molecular clone is highly neuropathogenic in a mouse model: Implication of the structural proteins region in virulence. J. Virol. 2015, 89, 5862–5875. [Google Scholar] [CrossRef] [PubMed]
- Tajima, S.; Shibasaki, K.I.; Taniguchi, S.; Nakayama, E.; Maeki, T.; Lim, C.K.; Saijo, M. E and prM proteins of genotype V Japanese encephalitis virus are required for its increased virulence in mice. Heliyon 2019, 5, e02882. [Google Scholar] [CrossRef]
- Nerome, R.; Tajima, S.; Takasaki, T.; Yoshida, T.; Kotaki, A.; Lim, C.K.; Ito, M.; Sugiyama, A.; Yamauchi, A.; Yano, T.; et al. Molecular epidemiological analyses of Japanese encephalitis virus isolates from swine in Japan from 2002 to 2004. J. Gen. Virol. 2007, 88, 2762–2768. [Google Scholar] [CrossRef]
- Tajima, S.; Nerome, R.; Nukui, Y.; Kato, F.; Takasaki, T.; Kurane, I. A single mutation in the Japanese encephalitis virus E protein (S123R) increases its growth rate in mouse neuroblastoma cells and its pathogenicity in mice. Virology 2010, 396, 298–304. [Google Scholar] [CrossRef]
- Tajima, S.; Nukui, Y.; Ito, M.; Takasaki, T.; Kurane, I. Nineteen nucleotides in the variable region of 3′ non-translated region are dispensable for the replication of dengue type 1 virus in vitro. Virus Res. 2006, 116, 38–44. [Google Scholar] [CrossRef]
- Chiou, S.S.; Liu, H.; Chuang, C.K.; Lin, C.C.; Chen, W.J. Fitness of Japanese encephalitis virus to neuro-2a cells is determined by interactions of the viral envelope protein with highly sulfated glycosaminoglycans on the cell surface. J. Med. Virol. 2005, 76, 583–592. [Google Scholar] [CrossRef]
- Mackenzie, J.M.; Khromykh, A.A.; Jones, M.K.; Westaway, E.G. Subcellular localization and some biochemical properties of the flavivirus kunjin nonstructural proteins ns2a and ns4a. Virology 1998, 245, 203–215. [Google Scholar] [CrossRef]
- Vossmann, S.; Wieseler, J.; Kerber, R.; Kummerer, B.M. A basic cluster in the N terminus of yellow fever virus NS2A contributes to infectious particle production. J. Virol. 2015, 89, 4951–4965. [Google Scholar] [CrossRef]
- Xie, X.; Zou, J.; Puttikhunt, C.; Yuan, Z.; Shi, P.Y. Two distinct sets of NS2A molecules are responsible for dengue virus rna synthesis and virion assembly. J. Virol. 2015, 89, 1298–1313. [Google Scholar] [CrossRef] [PubMed]
- Xie, X.; Zou, J.; Zhang, X.; Zhou, Y.; Routh, A.L.; Kang, C.; Popov, V.L.; Chen, X.; Wang, Q.Y.; Dong, H.; et al. Dengue NS2A protein orchestrates virus assembly. Cell Host Microbe 2019, 26, 606–622. [Google Scholar] [CrossRef] [PubMed]
- Zhang, X.; Xie, X.; Zou, J.; Xia, H.; Shan, C.; Chen, X.; Shi, P.Y. Genetic and biochemical characterizations of Zika virus NS2A protein. Emerg. Microbes Infect. 2019, 8, 585–602. [Google Scholar] [CrossRef] [PubMed]
- Wu, R.H.; Tsai, M.H.; Chao, D.Y.; Yueh, A. Scanning mutagenesis studies reveal a potential intramolecular interaction within the C-terminal half of dengue virus NS2A involved in viral RNA replication and virus assembly and secretion. J. Virol. 2015, 89, 4281–4295. [Google Scholar] [CrossRef]
- Kummerer, B.M.; Rice, C.M. Mutations in the yellow fever virus nonstructural protein NS2A selectively block production of infectious particles. J. Virol. 2002, 76, 4773–4784. [Google Scholar] [CrossRef]
- Liu, W.J.; Chen, H.B.; Khromykh, A.A. Molecular and functional analyses of Kunjin virus infectious cDNA clones demonstrate the essential roles for NS2A in virus assembly and for a nonconservative residue in NS3 in RNA replication. J. Virol. 2003, 77, 7804–7813. [Google Scholar] [CrossRef]
- Leung, J.Y.; Pijlman, G.P.; Kondratieva, N.; Hyde, J.; Mackenzie, J.M.; Khromykh, A.A. Role of nonstructural protein NS2A in flavivirus assembly. J. Virol. 2008, 82, 4731–4741. [Google Scholar] [CrossRef]
- Munoz-Jordan, J.L.; Sanchez-Burgos, G.G.; Laurent-Rolle, M.; Garcia-Sastre, A. Inhibition of interferon signaling by dengue virus. Proc. Natl. Acad. Sci. USA 2003, 100, 14333–14338. [Google Scholar] [CrossRef] [PubMed]
- Liu, W.J.; Chen, H.B.; Wang, X.J.; Huang, H.; Khromykh, A.A. Analysis of adaptive mutations in Kunjin virus replicon RNA reveals a novel role for the flavivirus nonstructural protein NS2A in inhibition of beta interferon promoter-driven transcription. J. Virol. 2004, 78, 12225–12235. [Google Scholar] [CrossRef] [PubMed]
- Liu, W.J.; Wang, X.J.; Clark, D.C.; Lobigs, M.; Hall, R.A.; Khromykh, A.A. A single amino acid substitution in the West Nile virus nonstructural protein NS2A disables its ability to inhibit alpha/beta interferon induction and attenuates virus virulence in mice. J. Virol. 2006, 80, 2396–2404. [Google Scholar] [CrossRef] [PubMed]
- Tu, Y.C.; Yu, C.Y.; Liang, J.J.; Lin, E.; Liao, C.L.; Lin, Y.L. Blocking double-stranded RNA-activated protein kinase PKR by Japanese encephalitis virus nonstructural protein 2A. J. Virol. 2012, 86, 10347–10358. [Google Scholar] [CrossRef]
- Xia, H.; Luo, H.; Shan, C.; Muruato, A.E.; Nunes, B.T.D.; Medeiros, D.B.A.; Zou, J.; Xie, X.; Giraldo, M.I.; Vasconcelos, P.F.C.; et al. An evolutionary NS1 mutation enhances Zika virus evasion of host interferon induction. Nat. Commun. 2018, 9, 414. [Google Scholar] [CrossRef]
- Melian, E.B.; Edmonds, J.H.; Nagasaki, T.K.; Hinzman, E.; Floden, N.; Khromykh, A.A. West Nile virus NS2A protein facilitates virus-induced apoptosis independently of interferon response. J. Gen. Virol. 2013, 94, 308–313. [Google Scholar] [CrossRef]
- Yoon, K.J.; Song, G.; Qian, X.; Pan, J.; Xu, D.; Rho, H.S.; Kim, N.S.; Habela, C.; Zheng, L.; Jacob, F.; et al. Zika-virus-encoded NS2A disrupts mammalian cortical neurogenesis by degrading adherens junction proteins. Cell Stem Cell 2017, 21, 349–358. [Google Scholar] [CrossRef]
- Wu, R.H.; Tsai, M.H.; Tsai, K.N.; Tian, J.N.; Wu, J.S.; Wu, S.Y.; Chern, J.H.; Chen, C.H.; Yueh, A. Mutagenesis of dengue virus protein NS2A revealed a novel domain responsible for virus-induced cytopathic effect and interactions between NS2A and NS2B transmembrane segments. J. Virol. 2017, 91, e01836-16. [Google Scholar] [CrossRef] [PubMed]
- Fan, W.; Wu, M.; Qian, S.; Zhou, Y.; Chen, H.; Li, X.; Qian, P. TRIM52 inhibits Japanese encephalitis virus replication by degrading the viral NS2A. Sci. Rep. 2016, 6, 33698. [Google Scholar] [CrossRef] [PubMed]
- Firth, A.E.; Atkins, J.F. A conserved predicted pseudoknot in the NS2A-encoding sequence of West Nile and Japanese encephalitis flaviviruses suggests NS1’ may derive from ribosomal frameshifting. Virol. J. 2009, 6, 14. [Google Scholar] [CrossRef] [PubMed]
- Wang, J.; Li, X.; Gu, J.; Fan, Y.; Zhao, P.; Cao, R.; Chen, P. The A66G back mutation in NS2A of JEV SA14-14-2 strain contributes to production of NS1’ protein and the secreted NS1′ can be used for diagnostic biomarker for virulent virus infection. Infect. Genet. Evol. 2015, 36, 116–125. [Google Scholar] [CrossRef] [PubMed]
- Xie, X.; Gayen, S.; Kang, C.; Yuan, Z.; Shi, P.Y. Membrane topology and function of dengue virus NS2A protein. J. Virol. 2013, 87, 4609–4622. [Google Scholar] [CrossRef]
- Takamatsu, Y.; Morita, K.; Hayasaka, D. A single amino acid substitution in the NS2A protein of Japanese encephalitis virus affects virus propagation in vitro but not in vivo. J. Virol. 2015, 89, 6126–6130. [Google Scholar] [CrossRef] [PubMed]
- Zhang, X.; Xie, X.; Xia, H.; Zou, J.; Huang, L.; Popov, V.L.; Chen, X.; Shi, P.Y. Zika virus NS2A-mediated virion assembly. MBio 2019, 10, e02375-19. [Google Scholar] [CrossRef]
- Sood, V.; Sharma, K.B.; Gupta, V.; Saha, D.; Dhapola, P.; Sharma, M.; Sen, U.; Kitajima, S.; Chowdhury, S.; Kalia, M.; et al. ATF3 negatively regulates cellular antiviral signaling and autophagy in the absence of type I interferons. Sci. Rep. 2017, 7, 8789. [Google Scholar] [CrossRef] [PubMed]
| Amino Acid at Position | ||||
|---|---|---|---|---|
| Category or Strain | Clone No. | prM7 | prM60 | NS2A166 |
| Pin-sized-plaque clones | 1 | Gln | Lys | Tyr |
| 2 | Gln | Lys | Tyr | |
| 4 | Gln | Lys | Tyr | |
| 17 * | Gln | Lys | Tyr | |
| 18 | Gln | Asn | His | |
| Native-sized-plaque clones | 6 | Arg | Asn/Lys mix | Tyr |
| 7 * | Arg | Asn | Tyr | |
| 9 | Gln/Arg mix | Lys/Asn mix | Tyr | |
| 12 | Arg | Asn | Tyr | |
| 22 | Arg | Asn | Tyr | |
| NS1-3Muar v1 * | - | Gln | Asn | His |
| NS1-3Muar p10 * | - | Gln | Lys | Tyr |
| Muar | - | Gln | Asn | His |
| Mie/41/2002 | - | Gln | Asn | Tyr |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Tajima, S.; Taniguchi, S.; Nakayama, E.; Maeki, T.; Inagaki, T.; Lim, C.-K.; Saijo, M. Amino Acid at Position 166 of NS2A in Japanese Encephalitis Virus (JEV) Is Associated with In Vitro Growth Characteristics of JEV. Viruses 2020, 12, 709. https://doi.org/10.3390/v12070709
Tajima S, Taniguchi S, Nakayama E, Maeki T, Inagaki T, Lim C-K, Saijo M. Amino Acid at Position 166 of NS2A in Japanese Encephalitis Virus (JEV) Is Associated with In Vitro Growth Characteristics of JEV. Viruses. 2020; 12(7):709. https://doi.org/10.3390/v12070709
Chicago/Turabian StyleTajima, Shigeru, Satoshi Taniguchi, Eri Nakayama, Takahiro Maeki, Takuya Inagaki, Chang-Kweng Lim, and Masayuki Saijo. 2020. "Amino Acid at Position 166 of NS2A in Japanese Encephalitis Virus (JEV) Is Associated with In Vitro Growth Characteristics of JEV" Viruses 12, no. 7: 709. https://doi.org/10.3390/v12070709
APA StyleTajima, S., Taniguchi, S., Nakayama, E., Maeki, T., Inagaki, T., Lim, C.-K., & Saijo, M. (2020). Amino Acid at Position 166 of NS2A in Japanese Encephalitis Virus (JEV) Is Associated with In Vitro Growth Characteristics of JEV. Viruses, 12(7), 709. https://doi.org/10.3390/v12070709





