The Lived Experience of Chronic Hepatitis B: A Broader View of Its Impacts and Why We Need a Cure
Abstract
1. Introduction
- To clarify the rationale for finding a cure (e.g., “Why does a cure matter?”);
- To understand if proposed treatment interventions would be useful (e.g., “Is the cure that I am proposing going to be practical in the real world?”);
- To avoid any unintentional harm to the affected community (e.g., by exacerbating stigma);
- To maintain a trusting and respectful relationship between the scientific community and affected communities.
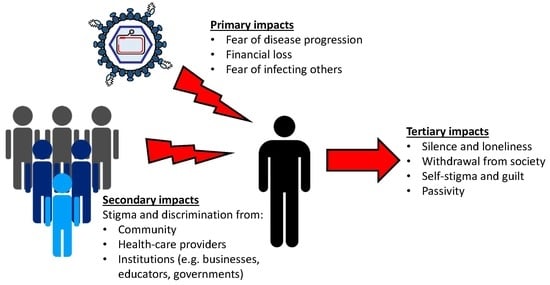
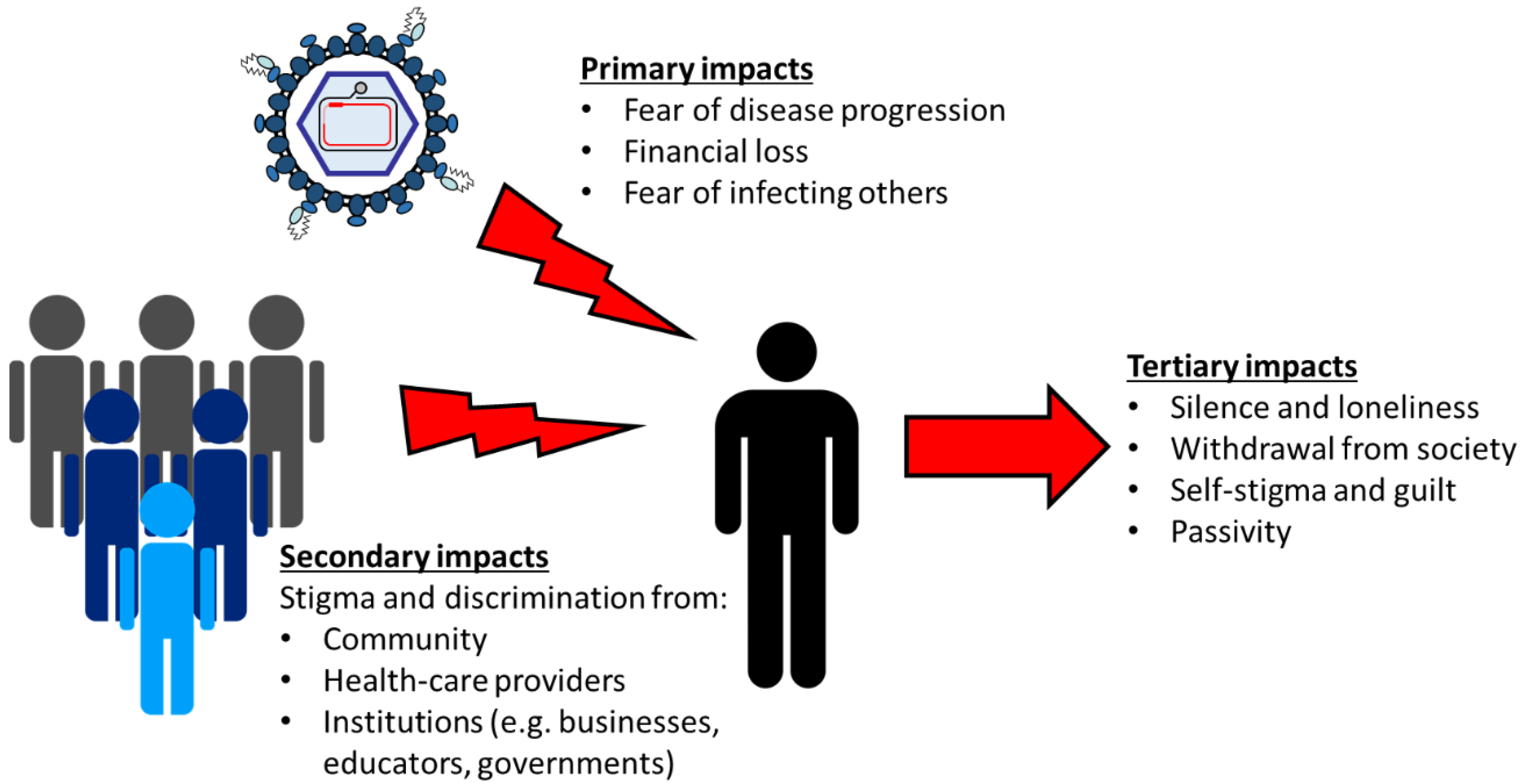
2. The Lived Experience of Chronic Hepatitis B
- Primary impacts: the direct psychosocial impacts on the person living with CHB caused by the disease;
- Secondary impacts: the impact on the affected person caused by the response from society (e.g., family members, healthcare providers, and community and government institutions);
- Tertiary impacts: the harms associated with an affected person’s response to societal stigma and discrimination.
2.1. Primary Impacts
2.1.1. Fear of Liver Cancer and Cirrhosis
2.1.2. Financial Loss and Instability
2.1.3. Fear of Infecting Others
2.2. Secondary Impacts
2.2.1. Stigma and Discrimination by Community
- HBV can be spread by sharing food or eating with someone;
- HBV can be transmitted through simple physical contact;
- HBV is only transmitted through promiscuous sex or illicit drug use;
- HBV is caused by dirty conditions;
- HBV is a genetic disease; or
- HBV always leads to death.
2.2.2. Stigma and Discrimination by Healthcare Providers
2.2.3. Stigma and Discrimination by Institutions
2.3. Tertiary Impacts
2.3.1. Silence and Loneliness
2.3.2. Withdrawal from the Majority (or Mainstream) Society
2.3.3. Guilt and Self-Stigma
2.3.4. Passivity
3. The Impact and Development of a Cure for CHB
4. Limitations of Our Review
5. Conclusions
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
Appendix A. Why Should the Patient Perspective Be Heard?
Appendix A.1. To Fully Answer the Question “Why Does a Cure Matter?”
Appendix A.2. To Inform Researchers What a Useful Cure Looks Like
Appendix A.3. To Limit Harm
Appendix A.4. To Maintain a Trusting Relationship with the General Public
Appendix B. Actions that Researchers Can Take
Appendix B.1. Acknowledge Lived Experiences
Appendix B.2. Use Appropriate Terminology
Appendix B.3. Partner with Affected Communities
Appendix B.4. Educate Society
Appendix B.5. Develop a Cure
References
- WHO. Global Hepatitis Report 2017; World Health Organization: Geneva, Switzerland, 2017. [Google Scholar]
- Polaris Observatory, C. Global prevalence, treatment, and prevention of hepatitis b virus infection in 2016: A modelling study. Lancet Gastroenterol. Hepatol. 2018, 3, 383–403. [Google Scholar]
- Schweitzer, A.; Horn, J.; Mikolajczyk, R.T.; Krause, G.; Ott, J.J. Estimations of worldwide prevalence of chronic hepatitis b virus infection: A systematic review of data published between 1965 and 2013. Lancet 2015, 386, 1546–1555. [Google Scholar] [CrossRef]
- Lemoine, M.; Nayagam, S.; Thursz, M. Viral hepatitis in resource-limited countries and access to antiviral therapies: Current and future challenges. Future Virol. 2013, 8, 371–380. [Google Scholar] [CrossRef] [PubMed]
- Zhu, D.; Guo, N.; Wang, J.; Nicholas, S.; Wang, Z.; Zhang, G.; Shi, L.; Wangen, K.R. Socioeconomic inequality in hepatitis b vaccination of rural adults in china. Hum. Vaccin Immunother. 2018, 14, 464–470. [Google Scholar] [CrossRef] [PubMed]
- Morisco, F.; Stroffolini, T.; Lombardo, F.L.; Guarino, M.; Camera, S.; Cossiga, V.; Donnarumma, L.; Loperto, I.; Caporaso, N. Prevalence of and risk factors for hbv infection in a metropolitan southern italian area: Evidence for the effectiveness of universal hepatitis b vaccination. Dig. Liver Dis. 2017, 49, 1257–1261. [Google Scholar] [CrossRef] [PubMed]
- Childs, L.; Adrien, P.; Minta, A.A.; Francois, J.; Phaimyr Jn Charles, N.; Blot, V.; Rey-Benito, G.; Vanden Eng, J.L.; Tohme, R.A. Prevalence of chronic hepatitis b virus infection among children in haiti, 2017. Am. J. Trop. Med. Hyg. 2019, 101, 214–219. [Google Scholar] [CrossRef] [PubMed]
- Coles, T.; Simpson, P.; Saulo, D.; Kaldor, J.; Richards, A.; Levy, M.; Wake, C.; Siddall, D.A.; Harrod, M.E.; Kariminia, A.; et al. Trends in hepatitis b prevalence and associated risk factors among indigenous and non-indigenous prison entrants in australia, 2004 to 2013. Aust. N. Z. J. Public Health 2019, 43, 236–240. [Google Scholar] [CrossRef]
- Stuver, S.O.; Boschi-Pinto, C.; Trichopoulos, D. Infection with hepatitis b and c viruses, social class and cancer. Iarc. Sci. Publ. 1997, 319–324. [Google Scholar]
- Arends, P.; Sonneveld, M.J.; Zoutendijk, R.; Carey, I.; Brown, A.; Fasano, M.; Mutimer, D.; Deterding, K.; Reijnders, J.G.; Oo, Y.; et al. Entecavir treatment does not eliminate the risk of hepatocellular carcinoma in chronic hepatitis b: Limited role for risk scores in caucasians. Gut 2015, 64, 1289–1295. [Google Scholar] [CrossRef]
- Smith, S.; Harmanci, H.; Hutin, Y.; Hess, S.; Bulterys, M.; Peck, R.; Rewari, B.; Mozalevskis, A.; Shibeshi, M.; Mumba, M.; et al. Global progress on the elimination of viral hepatitis as a major public health threat: An analysis of who member state responses 2017. Jhep. Rep. 2019, 1, 81–89. [Google Scholar] [CrossRef]
- Jorgensen, C.; Chen, S.; Carnes, C.A.; Block, J.; Chen, D.; Caballero, J.; Moraras, K.; Cohen, C. “Know hepatitis B”: A multilingual communications campaign promoting testing for hepatitis b among asian americans and pacific islanders. Public Health Rep. 2016, 131 (Suppl. 2), 35–40. [Google Scholar] [CrossRef] [PubMed]
- Cohen, C.; Caballero, J.; Martin, M.; Weerasinghe, I.; Ninde, M.; Block, J. Eradication of hepatitis b: A nationwide community coalition approach to improving vaccination, screening, and linkage to care. J. Community Health 2013, 38, 799–804. [Google Scholar] [CrossRef] [PubMed]
- Harris, A.M.; Link-Gelles, R.; Kim, K.; Chandrasekar, E.; Wang, S.; Bannister, N.; Pong, P.; Chak, E.; Chen, M.S., Jr.; Bowlus, C.; et al. Community-based services to improve testing and linkage to care among non-u.S.-born persons with chronic hepatitis b virus infection - three U.S. Programs, october 2014-september 2017. Mmwr. Morb. Mortal Wkly. Rep. 2018, 67, 541–546. [Google Scholar] [CrossRef] [PubMed]
- Richmond, J.A.; Sasadeusz, J.; Temple-Smith, M. The role of primary health care in hepatitis b testing and management: A case study. J. Community Health 2018, 43, 38–47. [Google Scholar] [CrossRef] [PubMed]
- O’Kelly, M.; Byrne, D.; Naughten, E.; Bergin, C.; Williams, C. Opt-out testing for blood-borne viruses in primary care: A multicentre, prospective study. Br. J. Gen. Pr. 2016, 66, e392–e396. [Google Scholar] [CrossRef][Green Version]
- Chak, E.; Taefi, A.; Li, C.S.; Chen, M.S., Jr.; Harris, A.M.; MacDonald, S.; Bowlus, C. Electronic medical alerts increase screening for chronic hepatitis b: A randomized, double-blind, controlled trial. Cancer Epidemiol Biomark. Prev. 2018, 27, 1352–1357. [Google Scholar] [CrossRef]
- Weir, R.C.; Toyoji, M.; McKee, M.; Li, V.; Wang, C.C. Assessing the impact of electronic health record interventions on hepatitis b screening and vaccination. J. Health Care Poor Underserved 2018, 29, 1587–1605. [Google Scholar] [CrossRef]
- Chandrasekar, E.; Kaur, R.; Song, S.; Kim, K.E. A comparison of effectiveness of hepatitis b screening and linkage to care among foreign-born populations in clinical and nonclinical settings. J. Multidiscip Healthc. 2015, 8, 1–9. [Google Scholar] [CrossRef]
- Alter, H.; Block, T.; Brown, N.; Brownstein, A.; Brosgart, C.; Chang, K.M.; Chen, P.J.; Chisari, F.V.; Cohen, C.; El-Serag, H.; et al. A research agenda for curing chronic hepatitis b virus infection. Hepatology 2018, 67, 1127–1131. [Google Scholar] [CrossRef]
- Block, T.M.; Alter, H.; Brown, N.; Brownstein, A.; Brosgart, C.; Chang, K.M.; Chen, P.J.; Cohen, C.; El-Serag, H.; Feld, J.; et al. Research priorities for the discovery of a cure for chronic hepatitis b: Report of a workshop. Antivir. Res. 2018, 150, 93–100. [Google Scholar] [CrossRef]
- Revill, P.A.; Chisari, F.V.; Block, J.M.; Dandri, M.; Gehring, A.J.; Guo, H.; Hu, J.; Kramvis, A.; Lampertico, P.; Janssen, H.L.A.; et al. A global scientific strategy to cure hepatitis b. Lancet Gastroenterol. Hepatol. 2019, 4, 545–558. [Google Scholar] [CrossRef]
- Vedio, A.; Liu, E.Z.H.; Lee, A.C.K.; Salway, S. Improving access to health care for chronic hepatitis b among migrant chinese populations: A systematic mixed methods review of barriers and enablers. J. Viral Hepat. 2017, 24, 526–540. [Google Scholar] [CrossRef] [PubMed]
- Lee, A.C.K.; Vedio, A.; Liu, E.Z.H.; Horsley, J.; Jesurasa, A.; Salway, S. Determinants of uptake of hepatitis b testing and healthcare access by migrant chinese in the england: A qualitative study. Bmc. Public Health 2017, 17, 747. [Google Scholar] [CrossRef] [PubMed]
- Fang, D.M.; Stewart, S.L. Social-cultural, traditional beliefs, and health system barriers of hepatitis b screening among hmong americans: A case study. Cancer 2018, 124 (Suppl. 7), 1576–1582. [Google Scholar] [CrossRef]
- Tanaka, M.; Strong, C.; Lee, S.; Juon, H.S. Influence of information sources on hepatitis b screening behavior and relevant psychosocial factors among asian immigrants. J. Immigr. Minor. Health 2013, 15, 779–787. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Sriphanlop, P.; Jandorf, L.; Kairouz, C.; Thelemaque, L.; Shankar, H.; Perumalswami, P. Factors related to hepatitis b screening among africans in new york city. Am. J. Health Behav 2014, 38, 745–754. [Google Scholar] [CrossRef] [PubMed]
- Wallace, J.; Pitts, M.; Liu, C.; Lin, V.; Hajarizadeh, B.; Richmond, J.; Locarnini, S. More than a virus: A qualitative study of the social implications of hepatitis b infection in china. Int. J. Equity Health 2017, 16, 137. [Google Scholar] [CrossRef]
- Chabrol, F.; Noah Noah, D.; Tchoumi, E.P.; Vidal, L.; Kuaban, C.; Carrieri, M.P.; Boyer, S.; Group, E.V. Screening, diagnosis and care cascade for viral hepatitis b and c in yaounde, cameroon: A qualitative study of patients and health providers coping with uncertainty and unbearable costs. Bmj Open 2019, 9, e025415. [Google Scholar] [CrossRef]
- Carabez, R.M.; Swanner, J.A.; Yoo, G.J.; Ho, M. Knowledge and fears among asian americans chronically infected with hepatitis b. J. Cancer Educ. 2014, 29, 522–528. [Google Scholar] [CrossRef]
- Richmond, J.; Smith, E.; Wallace, J.; Duncan, D.; Lucke, J. Hepatitis b testing and diagnosis experiences of patients and primary care professionals in australia. Aust. Fam. Phys. 2017, 46, 513–519. [Google Scholar]
- Taheri Ezbarami, Z.; Hassani, P.; Zagheri Tafreshi, M.; Alavi Majd, H. A qualitative study on individual experiences of chronic hepatitis b patients. Nurs. Open 2017, 4, 310–318. [Google Scholar] [CrossRef] [PubMed]
- Valizadeh, L.; Zamanzadeh, V.; Negarandeh, R.; Zamani, F.; Hamidia, A.; Zabihi, A. Psychological reactions among patients with chronic hepatitis b: A qualitative study. J. Caring Sci. 2016, 5, 57–66. [Google Scholar] [CrossRef] [PubMed]
- Alizadeh, A.H.; Ranjbar, M.; Yadollahzadeh, M. Patient concerns regarding chronic hepatitis b and c infection. East. Mediterr. Health J. 2008, 14, 1142–1147. [Google Scholar] [PubMed]
- Ng, C.J.; Low, W.Y.; Wong, L.P.; Sudin, M.R.; Mohamed, R. Uncovering the experiences and needs of patients with chronic hepatitis b infection at diagnosis: A qualitative study. Asia Pac. J. Public Health 2013, 25, 32–40. [Google Scholar] [CrossRef] [PubMed]
- Hajarizadeh, B.; Richmond, J.; Ngo, N.; Lucke, J.; Wallace, J. Hepatitis b-related concerns and anxieties among people with chronic hepatitis b in australia. Hepat. Mon. 2016, 16, e35566. [Google Scholar] [CrossRef] [PubMed]
- Hajarizadeh, B.; Wallace, J.; Richmond, J.; Ngo, N.; Enright, C. Hepatitis b knowledge and associated factors among people with chronic hepatitis b. Aust N. Z. J. Public Health 2015, 39, 563–568. [Google Scholar] [CrossRef]
- Mohamed, R.; Ng, C.J.; Tong, W.T.; Abidin, S.Z.; Wong, L.P.; Low, W.Y. Knowledge, attitudes and practices among people with chronic hepatitis b attending a hepatology clinic in malaysia: A cross sectional study. Bmc Public Health 2012, 12, 601. [Google Scholar] [CrossRef]
- Yamagiwa, Y.; Masaki, N. Factors improving the utility of antiviral therapy for chronic hepatitis b: A nationwide multicenter study in japan. Hepatol. Res. 2018, 48, 1069–1080. [Google Scholar] [CrossRef]
- Sublette, V.A.; Smith, S.K.; George, J.; McCaffery, K.; Douglas, M.W. The hepatitis c treatment experience: Patients’ perceptions of the facilitators of and barriers to uptake, adherence and completion. Psychol. Health 2015, 30, 987–1004. [Google Scholar] [CrossRef]
- Levy, A.R.; Kowdley, K.V.; Iloeje, U.; Tafesse, E.; Mukherjee, J.; Gish, R.; Bzowej, N.; Briggs, A.H. The impact of chronic hepatitis b on quality of life: A multinational study of utilities from infected and uninfected persons. Value Health 2008, 11, 527–538. [Google Scholar] [CrossRef]
- Evon, D.M.; Lin, H.S.; Khalili, M.; Fontana, R.J.; Yim, C.; Wahed, A.S.; Fried, M.W.; Hoofnagle, J.H.; Hepatitis, B.R.N. Patient-reported outcomes in a large north american cohort living with chronic hepatitis b virus: A cross-sectional analysis. Aliment. Pharm. 2020, 51, 457–468. [Google Scholar] [CrossRef] [PubMed]
- Bondini, S.; Kallman, J.; Dan, A.; Younoszai, Z.; Ramsey, L.; Nader, F.; Younossi, Z.M. Health-related quality of life in patients with chronic hepatitis b. Liver Int. 2007, 27, 1119–1125. [Google Scholar] [CrossRef] [PubMed]
- Ong, S.C.; Mak, B.; Aung, M.O.; Li, S.C.; Lim, S.G. Health-related quality of life in chronic hepatitis b patients. Hepatology 2008, 47, 1108–1117. [Google Scholar] [CrossRef] [PubMed]
- Fotos, N.V.; Elefsiniotis, I.; Patelarou, A.; Giakoumidakis, K.; Patelarou, E.; Kouros, A.; Brokalaki, H. Psychological disorders and quality of life among patients with chronic viral hepatitis: A single-center cross-sectional study with pair-matched healthy controls. Gastroenterol. Nurs. 2018, 41, 206–218. [Google Scholar] [CrossRef] [PubMed]
- Vu, T.T.M.; Le, T.V.; Dang, A.K.; Nguyen, L.H.; Nguyen, B.C.; Tran, B.X.; Latkin, C.A.; Ho, C.S.H.; Ho, R.C.M. Socioeconomic vulnerability to depressive symptoms in patients with chronic hepatitis b. Int. J. Env. Res. Public Health 2019, 16, 255. [Google Scholar] [CrossRef] [PubMed]
- Atesci, F.C.; Cetin, B.C.; Oguzhanoglu, N.K.; Karadag, F.; Turgut, H. Psychiatric disorders and functioning in hepatitis b virus carriers. Psychosomatics 2005, 46, 142–147. [Google Scholar] [CrossRef]
- Lu, J.; Xu, A.; Wang, J.; Zhang, L.; Song, L.; Li, R.; Zhang, S.; Zhuang, G.; Lu, M. Direct economic burden of hepatitis b virus related diseases: Evidence from shandong, china. Bmc Health Serv. Res. 2013, 13, 37. [Google Scholar] [CrossRef]
- Zhiqiang, G.; Zhaohui, D.; Qinhuan, W.; Dexian, C.; Yunyun, F.; Hongtao, L.; Iloeje, U.H. Cost of chronic hepatitis b infection in china. J. Clin. Gastroenterol. 2004, 38, S175–S178. [Google Scholar] [CrossRef]
- Lai, C.L.; Shouval, D.; Lok, A.S.; Chang, T.T.; Cheinquer, H.; Goodman, Z.; DeHertogh, D.; Wilber, R.; Zink, R.C.; Cross, A.; et al. Entecavir versus lamivudine for patients with hbeag-negative chronic hepatitis b. N. Engl. J. Med. 2006, 354, 1011–1020. [Google Scholar] [CrossRef]
- Lai, C.L.; Rosmawati, M.; Lao, J.; Van Vlierberghe, H.; Anderson, F.H.; Thomas, N.; Dehertogh, D. Entecavir is superior to lamivudine in reducing hepatitis b virus DNA in patients with chronic hepatitis b infection. Gastroenterology 2002, 123, 1831–1838. [Google Scholar] [CrossRef]
- Buti, M.; Brosa, M.; Casado, M.A.; Rueda, M.; Esteban, R. Modeling the cost-effectiveness of different oral antiviral therapies in patients with chronic hepatitis b. J. Hepatol. 2009, 51, 640–646. [Google Scholar] [CrossRef] [PubMed]
- Wu, H.; Yim, C.; Chan, A.; Ho, M.; Heathcote, J. Sociocultural factors that potentially affect the institution of prevention and treatment strategies for prevention of hepatitis b in chinese canadians. Can. J. Gastroenterol. 2009, 23, 31–36. [Google Scholar] [CrossRef] [PubMed]
- Adjei, C.A.; Stutterheim, S.E.; Naab, F.; Ruiter, R.A.C. Barriers to chronic hepatitis b treatment and care in ghana: A qualitative study with people with hepatitis b and healthcare providers. PLoS ONE 2019, 14, e0225830. [Google Scholar] [CrossRef] [PubMed]
- Spiegel, B.M.; Bolus, R.; Han, S.; Tong, M.; Esrailian, E.; Talley, J.; Tran, T.; Smith, J.; Karsan, H.A.; Durazo, F.; et al. Development and validation of a disease-targeted quality of life instrument in chronic hepatitis b: The hepatitis b quality of life instrument, version 1.0. Hepatology 2007, 46, 113–121. [Google Scholar] [CrossRef] [PubMed]
- Guirgis, M.; Nusair, F.; Bu, Y.M.; Yan, K.; Zekry, A.T. Barriers faced by migrants in accessing healthcare for viral hepatitis infection. Intern. Med. J. 2012, 42, 491–496. [Google Scholar] [CrossRef]
- Valizadeh, L.; Zamanzadeh, V.; Bayani, M.; Zabihi, A. The social stigma experience in patients with hepatitis b infection: A qualitative study. Gastroenterol. Nurs. 2017, 40, 143–150. [Google Scholar] [CrossRef] [PubMed]
- Smith-Palmer, J.; Cerri, K.; Sbarigia, U.; Chan, E.K.H.; Pollock, R.F.; Valentine, W.J.; Bonroy, K. Impact of stigma on people living with chronic hepatitis b. Patient Relat. Outcome Meas. 2020, 11, 95–107. [Google Scholar] [CrossRef]
- Mokaya, J.; McNaughton, A.L.; Burbridge, L.; Maponga, T.; O’Hara, G.; Andersson, M.; Seeley, J.; Matthews, P.C. A blind spot? Confronting the stigma of hepatitis b virus (hbv) infection - a systematic review. Wellcome Open Res. 2018, 3, 29. [Google Scholar] [CrossRef]
- Lee, H.; Fawcett, J.; Kim, D.; Yang, J.H. Correlates of hepatitis b virus-related stigmatization experienced by asians: A scoping review of literature. Asia Pac. J. Oncol. Nurs. 2016, 3, 324–334. [Google Scholar] [CrossRef]
- Cotler, S.J.; Cotler, S.; Xie, H.; Luc, B.J.; Layden, T.J.; Wong, S.S. Characterizing hepatitis b stigma in chinese immigrants. J. Viral Hepat. 2012, 19, 147–152. [Google Scholar] [CrossRef]
- Li, D.; Tang, T.; Patterson, M.; Ho, M.; Heathcote, J.; Shah, H. The impact of hepatitis b knowledge and stigma on screening in canadian chinese persons. Can. J. Gastroenterol. 2012, 26, 597–602. [Google Scholar] [CrossRef] [PubMed]
- Philbin, M.M.; Erby, L.A.; Lee, S.; Juon, H.S. Hepatitis b and liver cancer among three asian american sub-groups: A focus group inquiry. J. Immigr. Minor. Health 2012, 14, 858–868. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Wang, W.L.; Wang, C.J.; Tseng, H.F. Comparing knowledge, health beliefs, and self-efficacy toward hepatitis b prevention among university students with different hepatitis b virus infectious statuses. J. Nurs. Res. 2009, 17, 10–19. [Google Scholar] [CrossRef] [PubMed]
- Yu, L.; Wang, J.; Zhu, D.; Leng, A.; Wangen, K.R. Hepatitis b-related knowledge and vaccination in association with discrimination against hepatitis b in rural china. Hum. Vaccin. Immunother 2016, 12, 70–76. [Google Scholar] [CrossRef]
- Lin, X.; Robinson, N.J.; Thursz, M.; Rosenberg, D.M.; Weild, A.; Pimenta, J.M.; Hall, A.J. Chronic hepatitis b virus infection in the asia-pacific region and africa: Review of disease progression. J. Gastroenterol. Hepatol. 2005, 20, 833–843. [Google Scholar] [CrossRef]
- Dahl, T.F.; Cowie, B.C.; Biggs, B.A.; Leder, K.; MacLachlan, J.H.; Marshall, C. Health literacy in patients with chronic hepatitis b attending a tertiary hospital in melbourne: A questionnaire based survey. Bmc Infect. Dis 2014, 14, 537. [Google Scholar] [CrossRef]
- Yoo, G.J.; Fang, T.; Zola, J.; Dariotis, W.M. Destigmatizing hepatitis b in the asian american community: Lessons learned from the san francisco hep b free campaign. J. Cancer Educ. 2012, 27, 138–144. [Google Scholar] [CrossRef]
- Le, T.V.; Vu, T.T.M.; Mai, H.T.; Nguyen, L.H.; Truong, N.T.; Hoang, C.L.; Nguyen, S.H.; Nguyen, C.T.; Nguyen, B.C.; Tran, T.H.; et al. Social determinants of stigma and discrimination in vietnamese patients with chronic hepatitis B. Int. J. Env. Res. Public Health 2019, 16, 398. [Google Scholar] [CrossRef]
- Huang, J.; Guan, M.L.; Balch, J.; Wu, E.; Rao, H.; Lin, A.; Wei, L.; Lok, A.S. Survey of hepatitis b knowledge and stigma among chronically infected patients and uninfected persons in beijing, china. Liver Int. 2016, 36, 1595–1603. [Google Scholar] [CrossRef]
- Leng, A.; Li, Y.; Wangen, K.R.; Nicholas, S.; Maitland, E.; Wang, J. Hepatitis b discrimination in everyday life by rural migrant workers in beijing. Hum. Vaccin. Immunother. 2016, 12, 1164–1171. [Google Scholar] [CrossRef]
- Yu, L.; Liu, H.; Zheng, J.; Liu, R.; Wangen, K.R.; Wang, J. Present situation and influencing factors of discrimination against hepatitis b patients and carriers among rural adults in three eastern provinces in china. Zhonghua Yu Fang Yi Xue Za Zhi 2015, 49, 771–776. [Google Scholar] [PubMed]
- Eguchi, H.; Wada, K. Knowledge of hbv and hcv and individuals’ attitudes toward hbv- and hcv-infected colleagues: A national cross-sectional study among a working population in japan. PLoS ONE 2013, 8, e76921. [Google Scholar] [CrossRef]
- Cohen, C.; Evans, A.A.; Huang, P.; London, W.T.; Block, J.M.; Chen, G. Hepatitis b knowledge among key stakeholders in haimen city, china: Implications for addressing chronic hbv infection. Hepatol. Med. Policy 2016, 1, 4. [Google Scholar] [CrossRef]
- Maxwell, A.E.; Stewart, S.L.; Glenn, B.A.; Wong, W.K.; Yasui, Y.; Chang, L.C.; Taylor, V.M.; Nguyen, T.T.; Chen, M.S.; Bastani, R. Theoretically informed correlates of hepatitis b knowledge among four asian groups: The health behavior framework. Asian Pac. J. Cancer Prev. 2012, 13, 1687–1692. [Google Scholar] [CrossRef]
- Freeland, C.; Bodor, S.; Perera, U.; Cohen, C. Barriers to hepatitis b screening and prevention for african immigrant populations in the united states: A qualitative study. Viruses 2020, 12, 305. [Google Scholar] [CrossRef] [PubMed]
- Adjei, C.A.; Naab, F.; Donkor, E.S. Beyond the diagnosis: A qualitative exploration of the experiences of persons with hepatitis b in the accra metropolis, ghana. Bmj Open 2017, 7, e017665. [Google Scholar] [CrossRef] [PubMed]
- Han, B.; Yuan, Q.; Shi, Y.; Wei, L.; Hou, J.; Shang, J.; Han, Y.; Jin, C.; Chan, P.L.; Zhuang, H.; et al. The experience of discrimination of individuals living with chronic hepatitis b in four provinces of china. PLoS ONE 2018, 13, e0195455. [Google Scholar] [CrossRef]
- Chao, J.; Chang, E.T.; So, S.K. Hepatitis b and liver cancer knowledge and practices among healthcare and public health professionals in china: A cross-sectional study. Bmc Public Health 2010, 10, 98. [Google Scholar] [CrossRef]
- Wada, K.; Smith, D.R.; Ishimaru, T. Reluctance to care for patients with hiv or hepatitis b / c in japan. BMC Pregnancy Childbirth 2016, 16, 31. [Google Scholar] [CrossRef]
- Hoofnagle, J.H.; Shafritz, D.A.; Popper, H. Chronic type b hepatitis and the "healthy" hbsag carrier state. Hepatology 1987, 7, 758–763. [Google Scholar] [CrossRef]
- Van Gemert, C.; Howell, J.; Wang, J.; Stoove, M.; Cowie, B.; Allard, N.; Enright, C.; Dunn, E.; Towell, V.; Hellard, M. Knowledge and practices of chronic hepatitis B virus testing by general practitioners in victoria, australia, 2014–2015. Aust. Fam. Phys. 2017, 46, 683–689. [Google Scholar]
- Lai, C.J.; Nguyen, T.T.; Hwang, J.; Stewart, S.L.; Kwan, A.; McPhee, S.J. Provider knowledge and practice regarding hepatitis b screening in chinese-speaking patients. J. Cancer Educ. 2007, 22, 37–41. [Google Scholar] [CrossRef] [PubMed]
- Robotin, M.; Patton, Y.; George, J. Getting it right: The impact of a continuing medical education program on hepatitis b knowledge of australian primary care providers. Int. J. Gen. Med. 2013, 6, 115–122. [Google Scholar] [CrossRef] [PubMed]
- Mukhtar, N.A.; Kathpalia, P.; Hilton, J.F.; Lau, G.; Yu, A.; Grumbach, K.; Nguyen, T.T.; Chan, D.; Khalili, M. Provider, patient, and practice factors shape hepatitis b prevention and management by primary care providers. J. Clin. Gastroenterol. 2017, 51, 626–631. [Google Scholar] [CrossRef]
- Papatheodoridis, G.V.; Sypsa, V.; Dalekos, G.; Yurdaydin, C.; van Boemmel, F.; Buti, M.; Goulis, J.; Calleja, J.L.; Chi, H.; Manolakopoulos, S.; et al. Eight-year survival in chronic hepatitis b patients under long-term entecavir or tenofovir therapy is similar to the general population. J. Hepatol. 2018, 68, 1129–1136. [Google Scholar] [CrossRef]
- Su, T.H.; Hu, T.H.; Chen, C.Y.; Huang, Y.H.; Chuang, W.L.; Lin, C.C.; Wang, C.C.; Su, W.W.; Chen, M.Y.; Peng, C.Y.; et al. Four-year entecavir therapy reduces hepatocellular carcinoma, cirrhotic events and mortality in chronic hepatitis b patients. Liver Int. 2016, 36, 1755–1764. [Google Scholar] [CrossRef]
- Yang, T.; Wu, M.C. Discrimination against hepatitis b carriers in china. Lancet 2011, 378, 1059. [Google Scholar] [CrossRef]
- Government, U.A.E. Health conditions for uae residence visa. Available online: https://u.ae/en/information-and-services/health-and-fitness/health-conditions-for-uae-residence-visa (accessed on 19 March 2020).
- Cornberg, M.; Lok, A.S.; Terrault, N.A.; Zoulim, F.; Faculty, E.-A.H.T.E.C. Guidance for design and endpoints of clinical trials in chronic hepatitis b - report from the 2019 easl-aasld hbv treatment endpoints conference. Hepatology 2019, 72, 539–557. [Google Scholar] [CrossRef]
- Block, T.M.; Locarnini, S.; McMahon, B.J.; Rehermann, B.; Peters, M.G. Use of current and new endpoints in the evaluation of experimental hepatitis b therapeutics. Clin. Infect. Dis. 2017, 64, 1283–1288. [Google Scholar] [CrossRef]
- Liang, T.J.; Block, T.M.; McMahon, B.J.; Ghany, M.G.; Urban, S.; Guo, J.T.; Locarnini, S.; Zoulim, F.; Chang, K.M.; Lok, A.S. Present and future therapies of hepatitis b: From discovery to cure. Hepatology 2015, 62, 1893–1908. [Google Scholar] [CrossRef]
- Levrero, M.; Testoni, B.; Zoulim, F. Hbv cure: Why, how, when? Curr. Opin. Virol. 2016, 18, 135–143. [Google Scholar] [CrossRef] [PubMed]
- Gane, E.J. Future anti-hbv strategies. Liver Int. 2017, 37 (Suppl. 1), 40–44. [Google Scholar] [CrossRef] [PubMed]
- Mugisha, J.; Mokaya, J.; Bukenya, D.; Ssembajja, F.; Mayambala, D.; Newton, R.; Matthews, P.C.; Seeley, J. A study of knowledge, experience, and beliefs about hepatitis b virus (hbv) infection in south western uganda. Front. Public Health 2019, 7, 304. [Google Scholar] [CrossRef] [PubMed]
- Funk, C.; Hefferon, M.; Kennedy, B.; Johnson, C. Trust and Mistrust in Americans’ Views of Scientific Experts. Pew Research Center. Available online: https://www.pewresearch.org/science/2019/08/02/trust-and-mistrust-in-americans-views-of-scientific-experts (accessed on 21 March 2020).
- MORI, I. Trust: The Truth; Ipsos MORI: London, UK, 2019. [Google Scholar]
- Younossi, Z.M.; Stepanova, M.; Younossi, I.; Papatheodoridis, G.; Janssen, H.L.A.; Agarwal, K.; Nguyen, M.H.; Gane, E.; Tsai, N.; Nader, F. Patient-reported outcomes in patients chronic viral hepatitis without cirrhosis: The impact of hepatitis b and c viral replication. Liver Int. 2019, 39, 1837–1844. [Google Scholar] [CrossRef] [PubMed]
- Karacaer, Z.; Cakir, B.; Erdem, H.; Ugurlu, K.; Durmus, G.; Ince, N.K.; Ozturk, C.; Hasbun, R.; Batirel, A.; Yilmaz, E.M.; et al. Quality of life and related factors among chronic hepatitis b-infected patients: A multi-center study, turkey. Health Qual. Life Outcomes 2016, 14, 153. [Google Scholar] [CrossRef] [PubMed]
- Xue, X.; Cai, S.; Ou, H.; Zheng, C.; Wu, X. Health-related quality of life in patients with chronic hepatitis b during antiviral treatment and off-treatment. Patient Prefer. Adherence 2017, 11, 85–93. [Google Scholar] [CrossRef]
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Tu, T.; Block, J.M.; Wang, S.; Cohen, C.; Douglas, M.W. The Lived Experience of Chronic Hepatitis B: A Broader View of Its Impacts and Why We Need a Cure. Viruses 2020, 12, 515. https://doi.org/10.3390/v12050515
Tu T, Block JM, Wang S, Cohen C, Douglas MW. The Lived Experience of Chronic Hepatitis B: A Broader View of Its Impacts and Why We Need a Cure. Viruses. 2020; 12(5):515. https://doi.org/10.3390/v12050515
Chicago/Turabian StyleTu, Thomas, Joan M. Block, Su Wang, Chari Cohen, and Mark W. Douglas. 2020. "The Lived Experience of Chronic Hepatitis B: A Broader View of Its Impacts and Why We Need a Cure" Viruses 12, no. 5: 515. https://doi.org/10.3390/v12050515
APA StyleTu, T., Block, J. M., Wang, S., Cohen, C., & Douglas, M. W. (2020). The Lived Experience of Chronic Hepatitis B: A Broader View of Its Impacts and Why We Need a Cure. Viruses, 12(5), 515. https://doi.org/10.3390/v12050515