Orthohantavirus Isolated in Reservoir Host Cells Displays Minimal Genetic Changes and Retains Wild-Type Infection Properties
Abstract
1. Introduction
2. Materials and Methods
2.1. Establishment of the Permanent Mygla.REC.B Cell Line
2.2. Virus Isolation and Propagation
2.3. Next-Generation Sequencing
2.4. Phylogenetic Analysis
2.5. Detection of Infected Cells in Cell Culture
2.6. Detection of Antiviral Responses in Cell Culture
2.7. Protein Content Analysis in Virus Preparations
2.8. Experimental Infections
2.9. Virus Quantification
2.10. Histological and Immunohistological Examinations
2.11. PUUV-Specific Immunoglobulin Analysis
2.12. Ethics Statement
3. Results
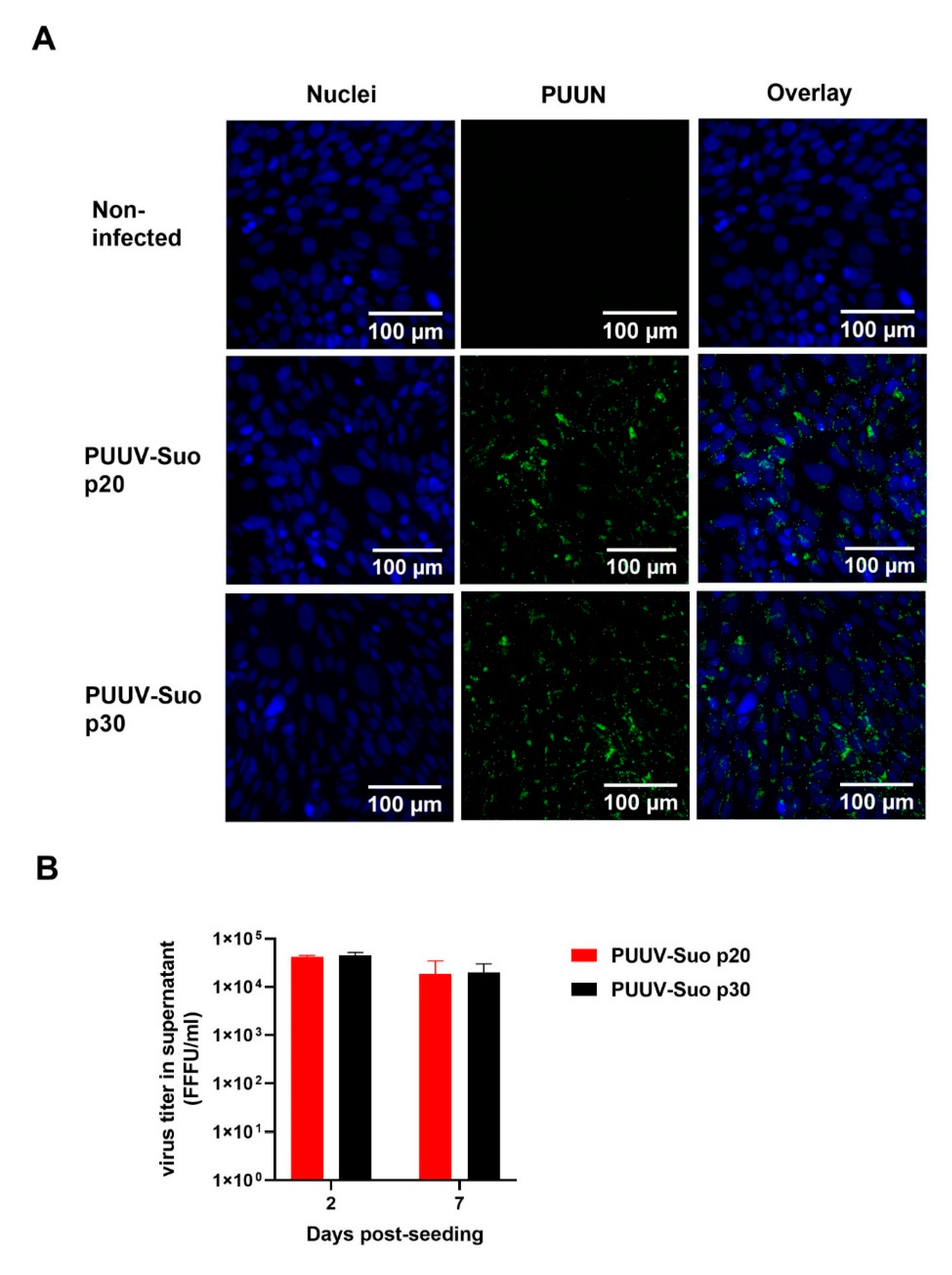
3.1. Isolation of PUUV-Suo in Epithelial Bank Vole Cells
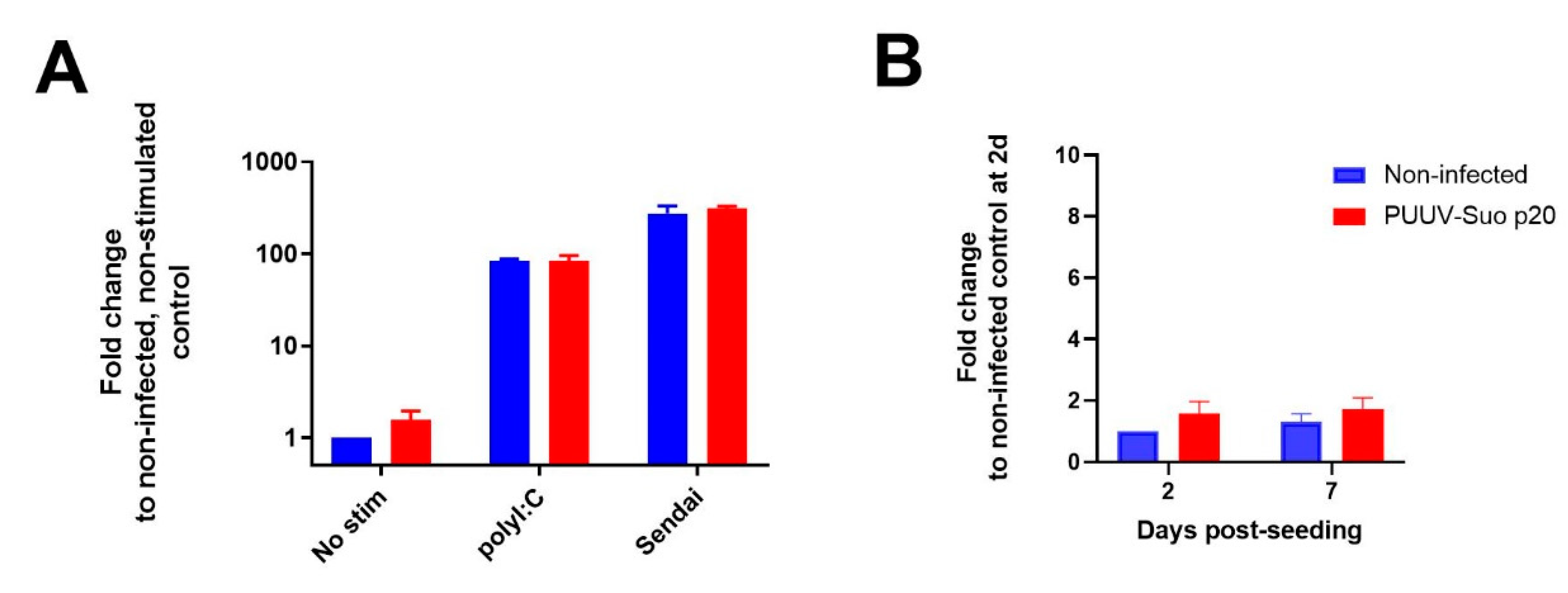
3.2. Replication of PUUV-Suo in Mygla.REC.B Cells Evades Antiviral Responses
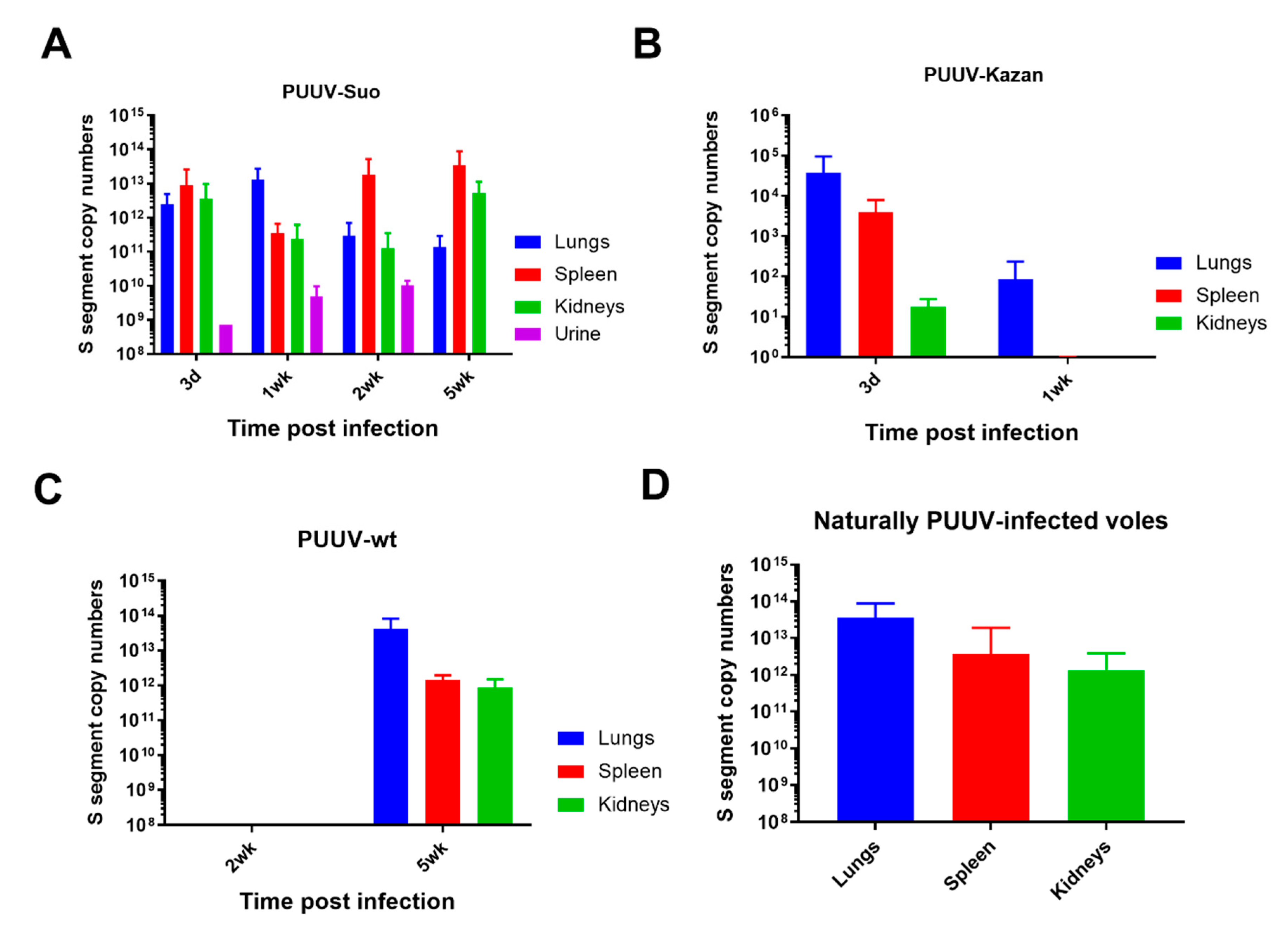
3.3. Experimental PUUV-Suo Infection Resembles Natural Infection in Bank Voles
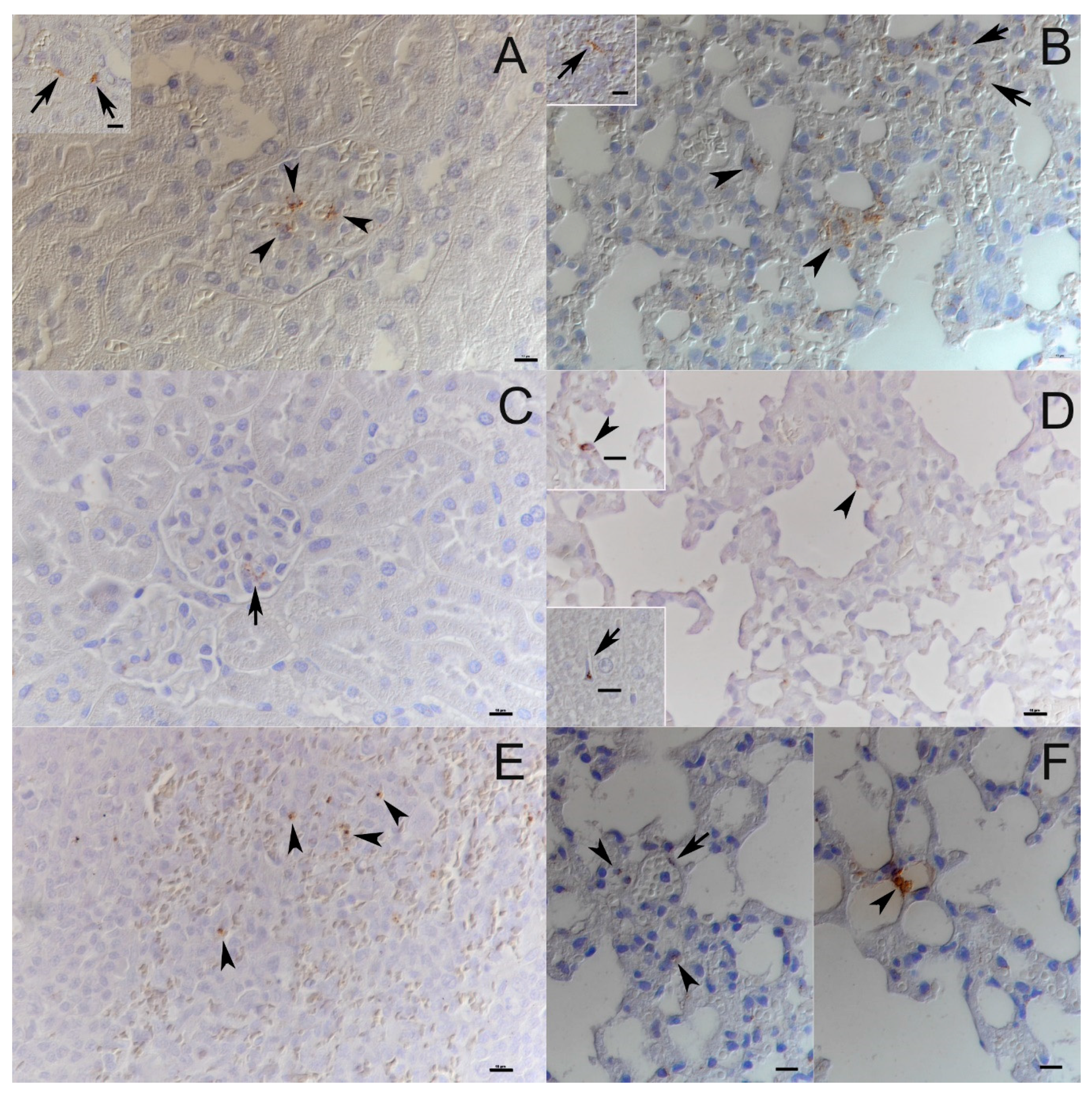
3.4. PUUV-Suo Host Cell Range Resembles Natural Infections
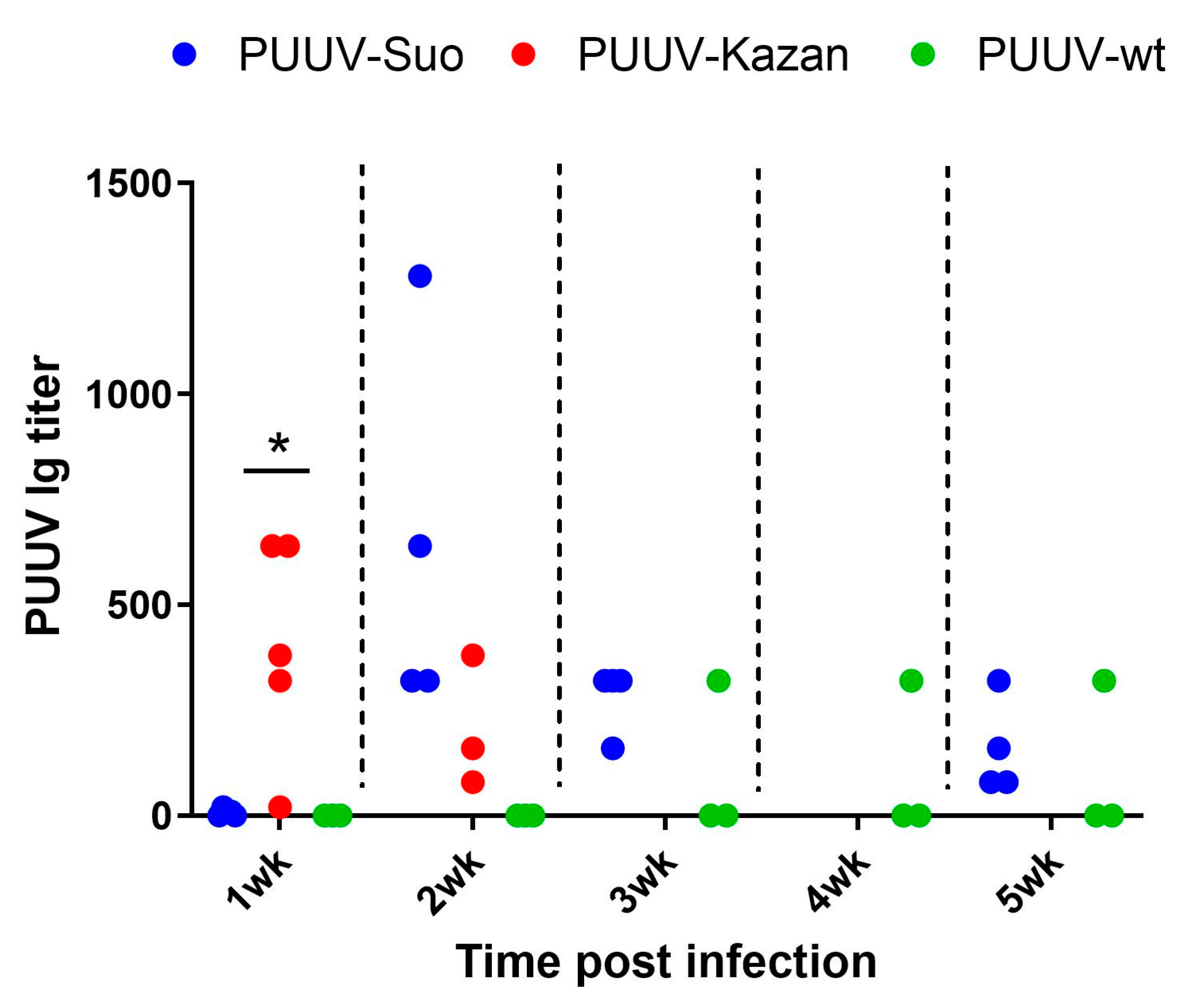
3.5. Delayed PUUV-Specific Immunoglobulin (Ig) Responses in Experimental Bank Vole Infections
4. Discussion
Supplementary Materials
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- Plowright, R.K.; Parrish, C.R.; McCallum, H.; Hudson, P.J.; Ko, A.I.; Graham, A.L.; Lloyd-Smith, J.O. Pathways to zoonotic spillover. Nat. Rev. Microbiol. 2017, 15, 502–510. [Google Scholar] [CrossRef] [PubMed]
- Han, B.A.; Park, A.W.; Jolles, A.E.; Altizer, S. Infectious disease transmission and behavioural allometry in wild mammals. J. Anim. Ecol. 2015, 84, 637–646. [Google Scholar] [CrossRef] [PubMed]
- Viana, M.; Mancy, R.; Biek, R.; Cleaveland, S.; Cross, P.C.; Lloyd-Smith, J.O.; Haydon, D.T. Assembling evidence for identifying reservoirs of infection. Trends Ecol. Evol. 2014, 29, 270–279. [Google Scholar] [CrossRef] [PubMed]
- Altizer, S.; Bartel, R.; Han, B.A. Animal migration and infectious disease risk. Science 2011, 331, 296–302. [Google Scholar] [CrossRef]
- Plowright, R.K.; Field, H.E.; Smith, C.; Divljan, A.; Palmer, C.; Tabor, G.; Daszak, P.; Foley, J.E. Reproduction and nutritional stress are risk factors for hendra virus infection in little red flying foxes (Pteropus scapulatus). Proc. Biol. Sci. 2008, 275, 861–869. [Google Scholar] [CrossRef]
- Forbes, K.M.; Sironen, T.; Plyusnin, A. Hantavirus maintenance and transmission in reservoir host populations. Curr. Opin. Virol. 2018, 28, 1–6. [Google Scholar] [CrossRef]
- Jonsson, C.B.; Figueiredo, L.T.; Vapalahti, O. A global perspective on hantavirus ecology, epidemiology, and disease. Clin. Microbiol. Rev. 2010, 23, 412–441. [Google Scholar] [CrossRef]
- Vapalahti, O.; Mustonen, J.; Lundkvist, A.; Henttonen, H.; Plyusnin, A.; Vaheri, A. Hantavirus infections in europe. Lancet Infect. Dis. 2003, 3, 653–661. [Google Scholar] [CrossRef]
- Madrières, S.; Castel, G.; Murri, S.; Vulin, J.; Marianneau, P.; Charbonnel, N. The Needs for Developing Experiments on Reservoirs in Hantavirus Research: Accomplishments, Challenges and Promises for the Future. Viruses 2019, 11, 664. [Google Scholar] [CrossRef]
- Botten, J.; Mirowsky, K.; Kusewitt, D.; Bharadwaj, M.; Yee, J.; Ricci, R.; Feddersen, R.M.; Hjelle, B. Experimental infection model for sin nombre hantavirus in the deer mouse (Peromyscus maniculatus). Proc. Natl. Acad. Sci. USA 2000, 97, 10578–10583. [Google Scholar] [CrossRef]
- Yanagihara, R.; Amyx, H.L.; Gajdusek, D.C. Experimental infection with puumala virus, the etiologic agent of nephropathia epidemica, in bank voles (Clethrionomys glareolus). J. Virol. 1985, 55, 34–38. [Google Scholar] [CrossRef]
- Klingstrom, J.; Plyusnin, A.; Vaheri, A.; Lundkvist, A. Wild-type puumala hantavirus infection induces cytokines, c-reactive protein, creatinine, and nitric oxide in cynomolgus macaques. J. Virol. 2002, 76, 444–449. [Google Scholar] [CrossRef] [PubMed]
- Prescott, J.; Feldmann, H.; Safronetz, D. Amending koch’s postulates for viral disease: When “growth in pure culture” leads to a loss of virulence. Antivir. Res. 2017, 137, 1–5. [Google Scholar] [CrossRef]
- Lundkvist, A.; Cheng, Y.; Sjolander, K.B.; Niklasson, B.; Vaheri, A.; Plyusnin, A. Cell culture adaptation of puumala hantavirus changes the infectivity for its natural reservoir, clethrionomys glareolus, and leads to accumulation of mutants with altered genomic rna s segment. J. Virol. 1997, 71, 9515–9523. [Google Scholar] [CrossRef] [PubMed]
- Safronetz, D.; Prescott, J.; Feldmann, F.; Haddock, E.; Rosenke, R.; Okumura, A.; Brining, D.; Dahlstrom, E.; Porcella, S.F.; Ebihara, H.; et al. Pathophysiology of hantavirus pulmonary syndrome in rhesus macaques. Proc. Natl. Acad. Sci. USA 2014, 111, 7114–7119. [Google Scholar] [CrossRef] [PubMed]
- Eckerle, I.; Ehlen, L.; Kallies, R.; Wollny, R.; Corman, V.M.; Cottontail, V.M.; Tschapka, M.; Oppong, S.; Drosten, C.; Muller, M.A. Bat airway epithelial cells: A novel tool for the study of zoonotic viruses. PLoS ONE 2014, 9, e84679. [Google Scholar] [CrossRef]
- Bolger, A.M.; Lohse, M.; Usadel, B. Trimmomatic: A flexible trimmer for illumina sequence data. Bioinformatics 2014, 30, 2114–2120. [Google Scholar] [CrossRef]
- Li, H.; Handsaker, B.; Wysoker, A.; Fennell, T.; Ruan, J.; Homer, N.; Marth, G.; Abecasis, G.; Durbin, R. The sequence alignment/map format and samtools. Bioinformatics 2009, 25, 2078–2079. [Google Scholar] [CrossRef]
- Edgar, R.C. Muscle: A multiple sequence alignment method with reduced time and space complexity. BMC Bioinform. 2004, 5, 113. [Google Scholar] [CrossRef]
- Darriba, D.; Taboada, G.L.; Doallo, R.; Posada, D. Jmodeltest 2: More models, new heuristics and parallel computing. Nat. Methods 2012, 9, 772. [Google Scholar] [CrossRef]
- Ronquist, F.; Teslenko, M.; van der Mark, P.; Ayres, D.L.; Darling, A.; Hohna, S.; Larget, B.; Liu, L.; Suchard, M.A.; Huelsenbeck, J.P. Mrbayes 3.2: Efficient bayesian phylogenetic inference and model choice across a large model space. Syst. Biol. 2012, 61, 539–542. [Google Scholar] [PubMed]
- Haller, O.; Kochs, G. Human mxa protein: An interferon-induced dynamin-like gtpase with broad antiviral activity. J. Interferon. Cytokine Res. 2011, 31, 79–87. [Google Scholar] [CrossRef] [PubMed]
- Stoltz, M.; Sundstrom, K.B.; Hidmark, A.; Tolf, C.; Vene, S.; Ahlm, C.; Lindberg, A.M.; Lundkvist, A.; Klingstrom, J. A model system for in vitro studies of bank vole borne viruses. PLoS ONE 2011, 6, e28992. [Google Scholar] [CrossRef] [PubMed]
- Schmittgen, T.D.; Livak, K.J. Analyzing real-time pcr data by the comparative c(t) method. Nat. Protoc. 2008, 3, 1101–1108. [Google Scholar] [CrossRef] [PubMed]
- Hepojoki, J.; Strandin, T.; Vaheri, A.; Lankinen, H. Interactions and oligomerization of hantavirus glycoproteins. J. Virol. 2010, 84, 227–242. [Google Scholar] [CrossRef] [PubMed]
- Niskanen, S.; Jääskeläinen, A.; Vapalahti, O.; Sironen, T. Evaluation of Real-Time RT-PCR for Diagnostic Use in Detection of Puumala Virus. Viruses 2019, 11, 661. [Google Scholar] [CrossRef] [PubMed]
- Korzyukov, Y.; Hetzel, U.; Kipar, A.; Vapalahti, O.; Hepojoki, J. Generation of anti-boa immunoglobulin antibodies for serodiagnostic applications, and their use to detect anti-reptarenavirus antibodies in boa constrictor. PLoS ONE 2016, 11, e0158417. [Google Scholar] [CrossRef]
- Hepojoki, S.; Hepojoki, J.; Hedman, K.; Vapalahti, O.; Vaheri, A. Rapid homogeneous immunoassay based on time-resolved forster resonance energy transfer for serodiagnosis of acute hantavirus infection. J. Clin. Microbiol. 2015, 53, 636–640. [Google Scholar] [CrossRef][Green Version]
- Kallio-Kokko, H.; Laakkonen, J.; Rizzoli, A.; Tagliapietra, V.; Cattadori, I.; Perkins, S.E.; Hudson, P.J.; Cristofolini, A.; Versini, W.; Vapalahti, O.; et al. Hantavirus and arenavirus antibody prevalence in rodents and humans in trentino, northern italy. Epidemiol. Infect. 2006, 134, 830–836. [Google Scholar] [CrossRef]
- Razzauti, M.; Plyusnina, A.; Henttonen, H.; Plyusnin, A. Microevolution of puumala hantavirus during a complete population cycle of its host, the bank vole (Myodes glareolus). PLoS ONE 2013, 8, e64447. [Google Scholar] [CrossRef]
- Plyusnina, A.; Razzauti, M.; Sironen, T.; Niemimaa, J.; Vapalahti, O.; Vaheri, A.; Henttonen, H.; Plyusnin, A. Analysis of complete puumala virus genome, finland. Emerg. Infect. Dis. 2012, 18, 2070–2072. [Google Scholar] [CrossRef] [PubMed]
- Emeny, J.M.; Morgan, M.J. Regulation of the interferon system: Evidence that vero cells have a genetic defect in interferon production. J. Gen. Virol. 1979, 43, 247–252. [Google Scholar] [CrossRef] [PubMed]
- Nemirov, K.; Lundkvist, A.; Vaheri, A.; Plyusnin, A. Adaptation of puumala hantavirus to cell culture is associated with point mutations in the coding region of the l segment and in the noncoding regions of the s segment. J. Virol. 2003, 77, 8793–8800. [Google Scholar] [CrossRef]
- Voutilainen, L.; Sironen, T.; Tonteri, E.; Back, A.T.; Razzauti, M.; Karlsson, M.; Wahlstrom, M.; Niemimaa, J.; Henttonen, H.; Lundkvist, A. Life-long shedding of puumala hantavirus in wild bank voles (Myodes glareolus). J. Gen. Virol. 2015, 96, 1238–1247. [Google Scholar] [CrossRef] [PubMed]
- Green, W.; Feddersen, R.; Yousef, O.; Behr, M.; Smith, K.; Nestler, J.; Jenison, S.; Yamada, T.; Hjelle, B. Tissue distribution of hantavirus antigen in naturally infected humans and deer mice. J. Infect. Dis. 1998, 177, 1696–1700. [Google Scholar] [CrossRef]
- Lee, H.W.; Lee, P.W.; Baek, L.J.; Song, C.K.; Seong, I.W. Intraspecific transmission of hantaan virus, etiologic agent of korean hemorrhagic fever, in the rodent apodemus agrarius. Am. J. Trop. Med. Hyg. 1981, 30, 1106–1112. [Google Scholar] [CrossRef]
- Kariwa, H.; Kimura, M.; Yoshizumi, S.; Arikawa, J.; Yoshimatsu, K.; Takashima, I.; Hashimoto, N. Modes of seoul virus infections: Persistency in newborn rats and transiency in adult rats. Arch. Virol. 1996, 141, 2327–2338. [Google Scholar] [CrossRef]
- Botten, J.; Mirowsky, K.; Kusewitt, D.; Ye, C.; Gottlieb, K.; Prescott, J.; Hjelle, B. Persistent sin nombre virus infection in the deer mouse (Peromyscus maniculatus) model: Sites of replication and strand-specific expression. J. Virol. 2003, 77, 1540–1550. [Google Scholar] [CrossRef]
| Segment | Nucleotide Position in Anti-Genomic Orientation | Nucleotide in Original Virus | Nucleotide in Isolate | Amino Acid in Original Virus | Amino Acid in Isolate | Codon Position |
|---|---|---|---|---|---|---|
| L | 66 | A | G | no change | 3rd | |
| 411 | G | A | Methionine | Isoleucine | 3rd | |
| 5700 | A | G | Isoleucine | Methionine | 3rd | |
| 5942 | C | U | Alanine | Valine | 2nd | |
| M | 89 | U | C | no change | 1st | |
| 3544 | U | C | non-coding | |||
| S | 136 | G | U | Valine | Leucine | 1st |
| 1625 | C | U | non-coding | |||
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Strandin, T.; Smura, T.; Ahola, P.; Aaltonen, K.; Sironen, T.; Hepojoki, J.; Eckerle, I.; Ulrich, R.G.; Vapalahti, O.; Kipar, A.; et al. Orthohantavirus Isolated in Reservoir Host Cells Displays Minimal Genetic Changes and Retains Wild-Type Infection Properties. Viruses 2020, 12, 457. https://doi.org/10.3390/v12040457
Strandin T, Smura T, Ahola P, Aaltonen K, Sironen T, Hepojoki J, Eckerle I, Ulrich RG, Vapalahti O, Kipar A, et al. Orthohantavirus Isolated in Reservoir Host Cells Displays Minimal Genetic Changes and Retains Wild-Type Infection Properties. Viruses. 2020; 12(4):457. https://doi.org/10.3390/v12040457
Chicago/Turabian StyleStrandin, Tomas, Teemu Smura, Paula Ahola, Kirsi Aaltonen, Tarja Sironen, Jussi Hepojoki, Isabella Eckerle, Rainer G. Ulrich, Olli Vapalahti, Anja Kipar, and et al. 2020. "Orthohantavirus Isolated in Reservoir Host Cells Displays Minimal Genetic Changes and Retains Wild-Type Infection Properties" Viruses 12, no. 4: 457. https://doi.org/10.3390/v12040457
APA StyleStrandin, T., Smura, T., Ahola, P., Aaltonen, K., Sironen, T., Hepojoki, J., Eckerle, I., Ulrich, R. G., Vapalahti, O., Kipar, A., & Forbes, K. M. (2020). Orthohantavirus Isolated in Reservoir Host Cells Displays Minimal Genetic Changes and Retains Wild-Type Infection Properties. Viruses, 12(4), 457. https://doi.org/10.3390/v12040457






