Human West Nile Virus Lineage 2 Infection: Epidemiological, Clinical, and Virological Findings
Abstract
1. Introduction
2. Materials and Methods
2.1. Sample and Data Collection
2.2. Entomological Surveillance
2.3. Laboratory Methods
2.4. Statistical Analysis
2.5. Ethics Statement
3. Results
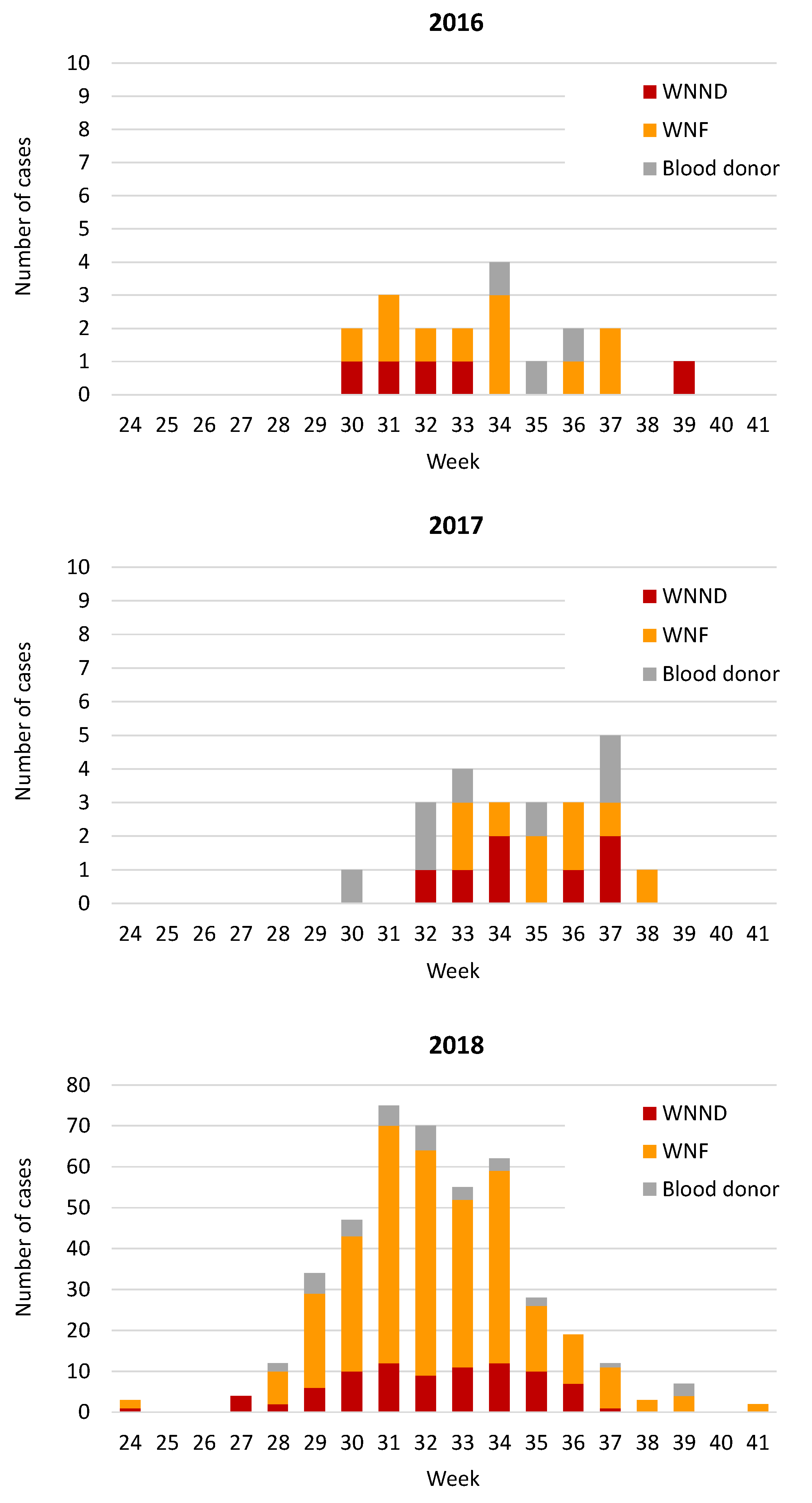
3.1. Demographic and Epidemiological Analyses of Human Cases of WNV Infection
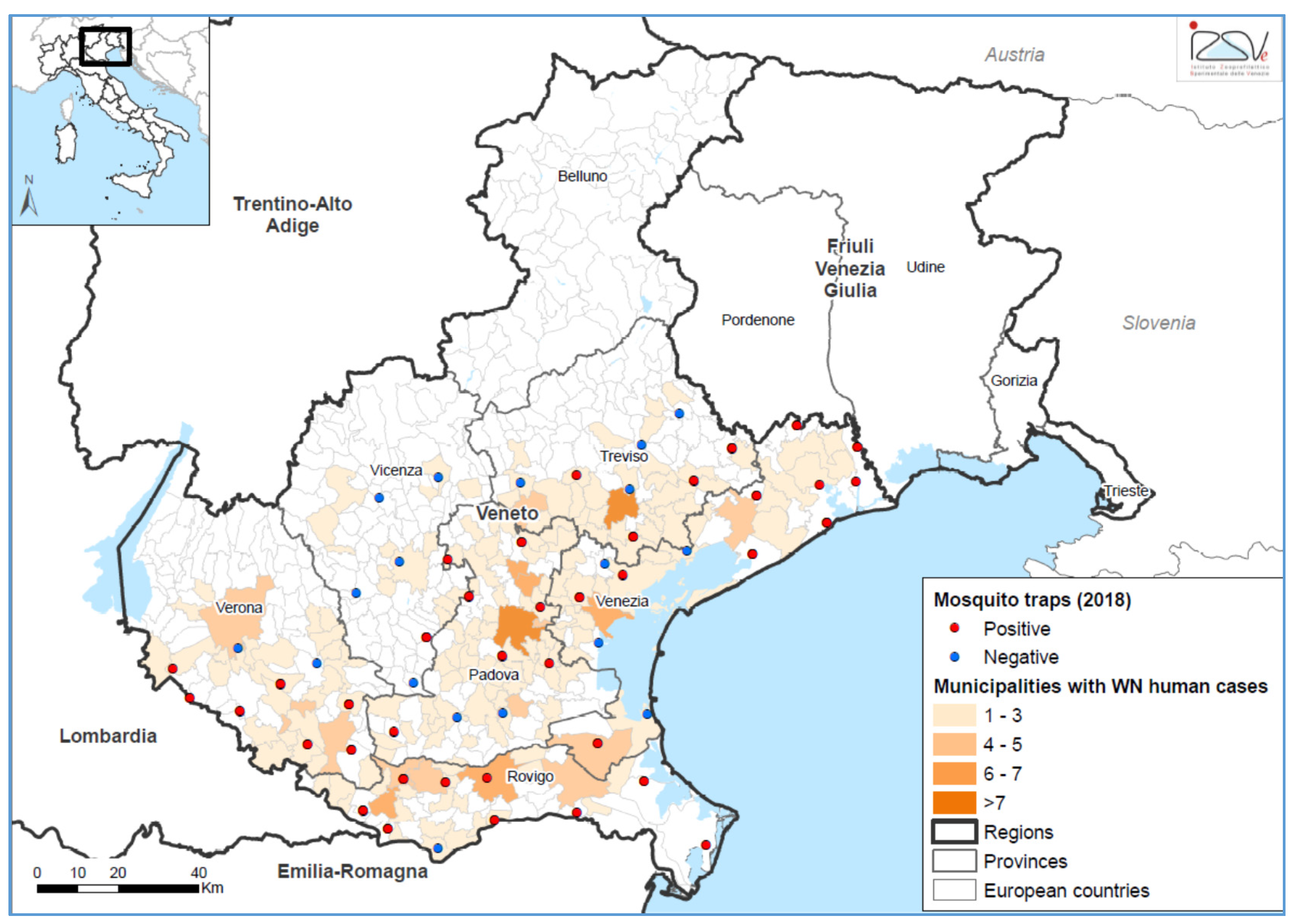
3.2. Entomological Surveillance
3.3. Clinical Findings
3.4. Virological Findings
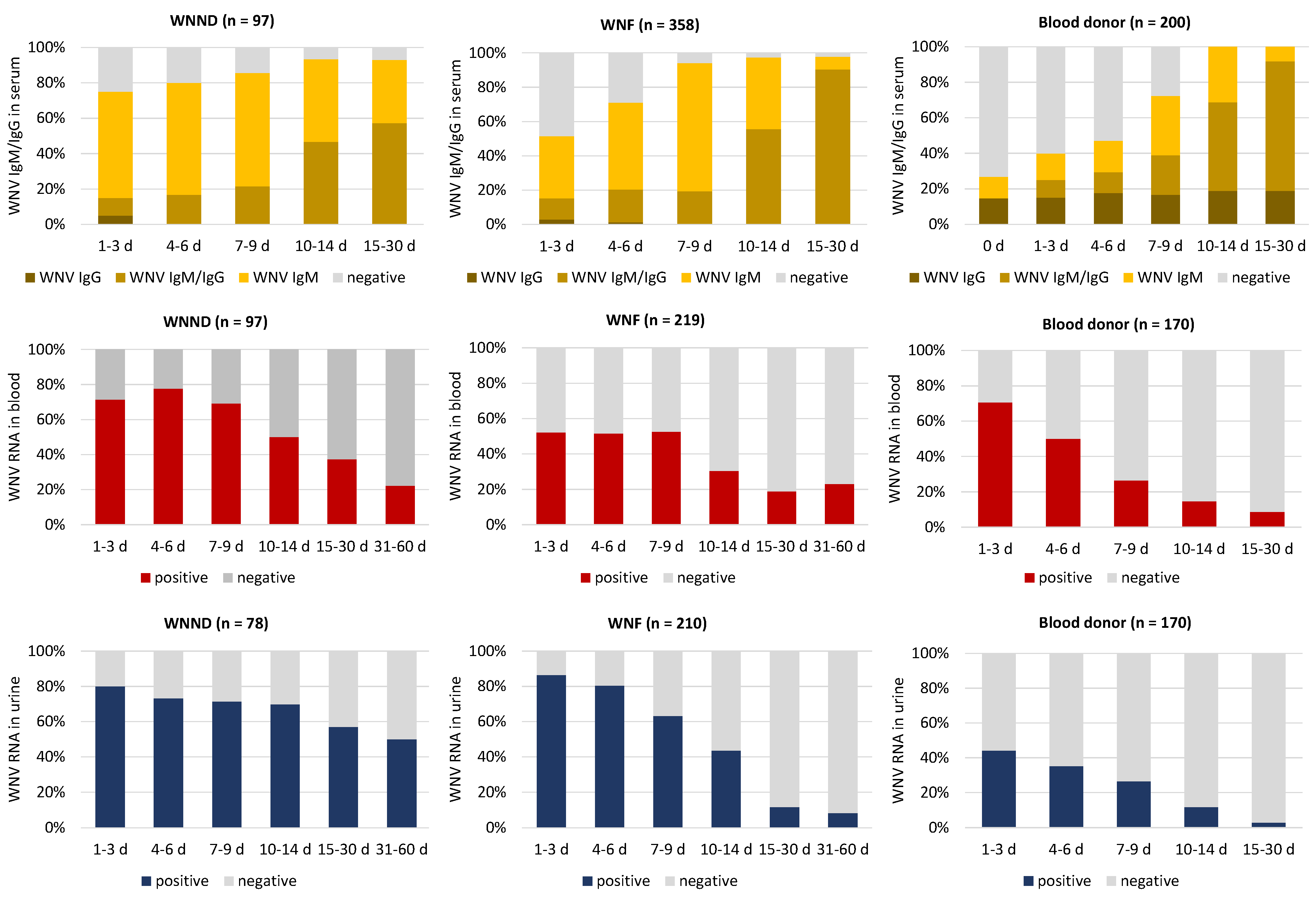
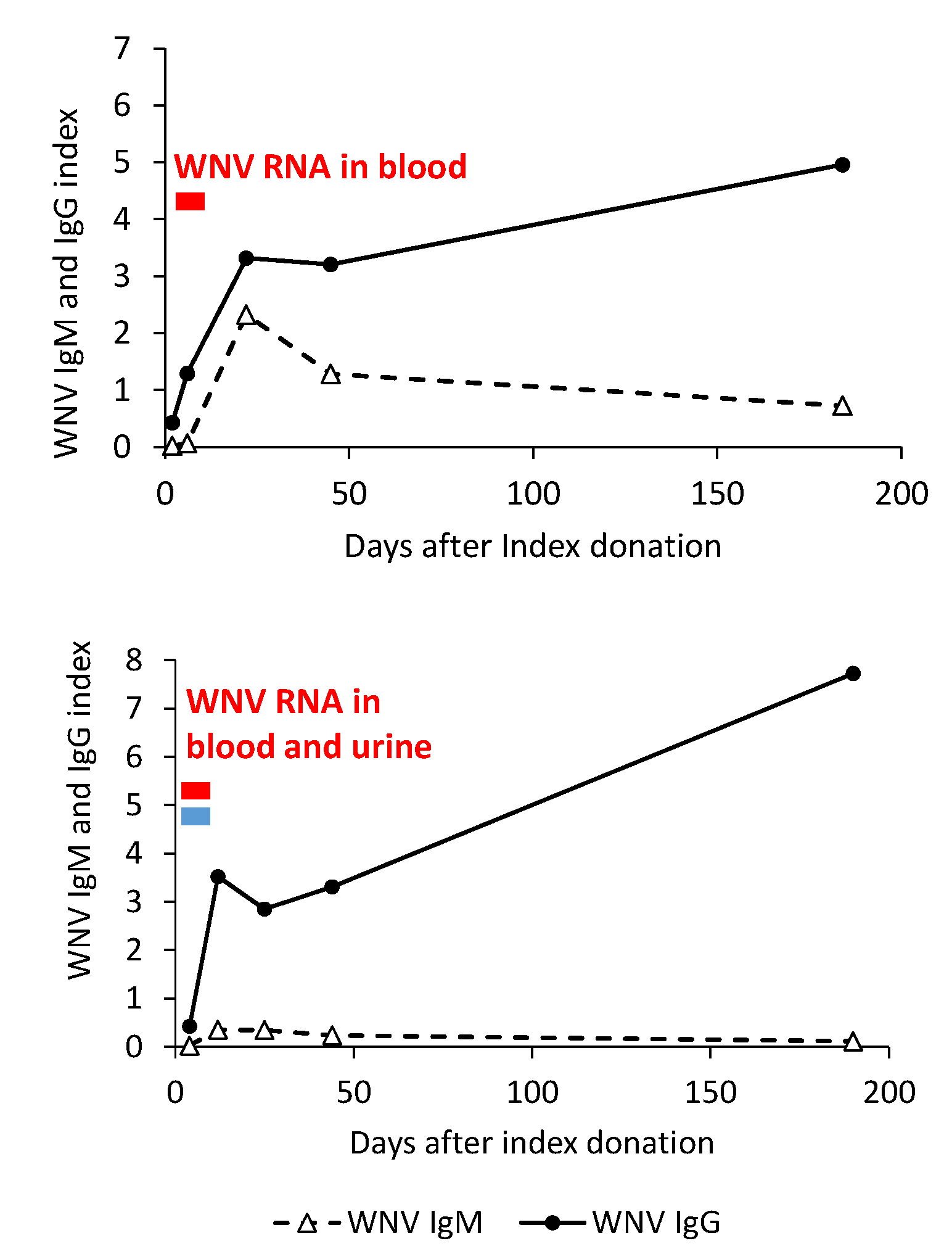
3.4.1. WNV Antibody Dynamics
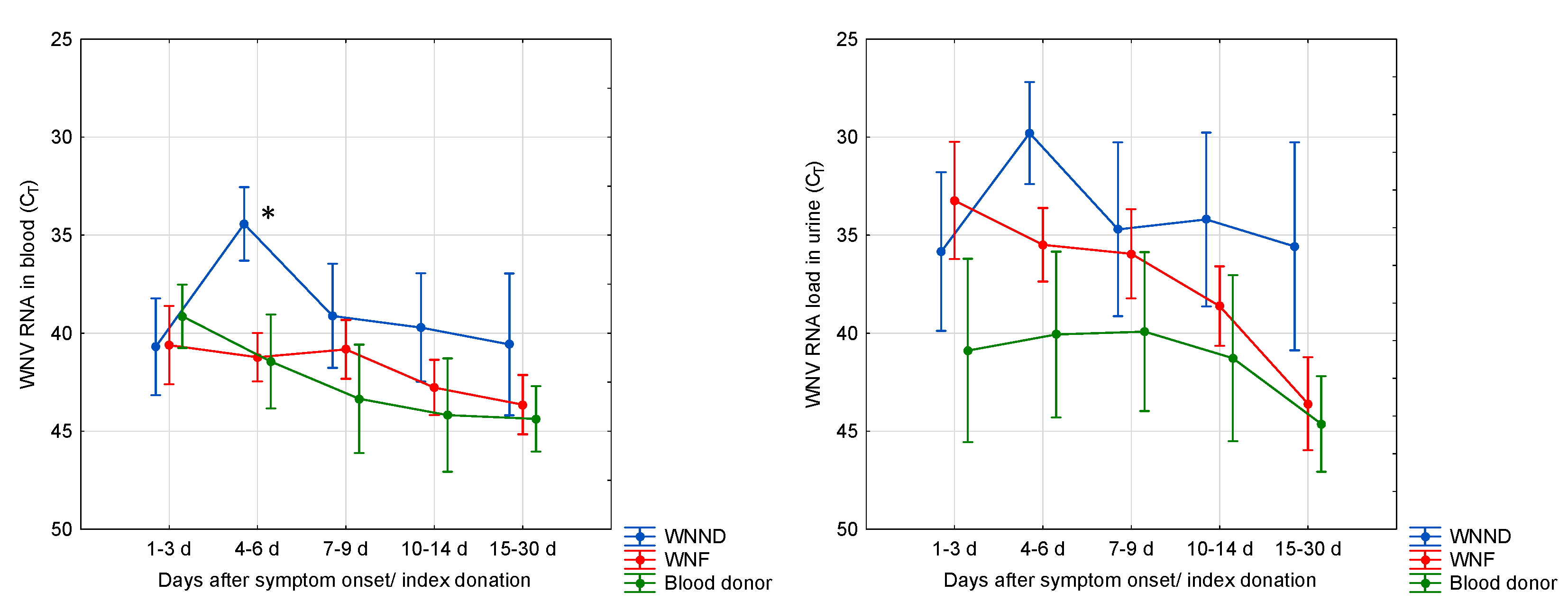
3.4.2. WNV RNA Kinetics in Blood and Urine
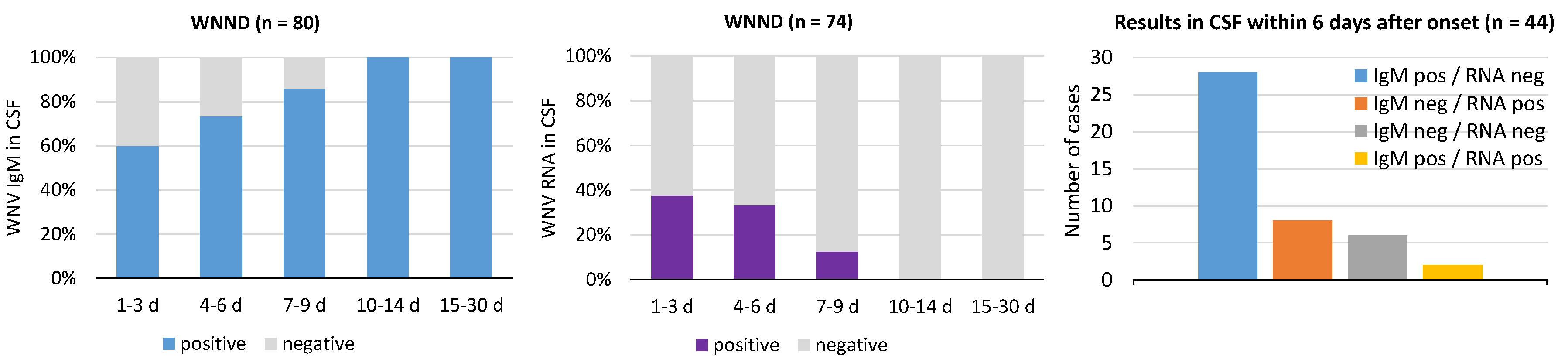
3.4.3. WNV RNA and IgM in Cerebrospinal Fluid (CSF)
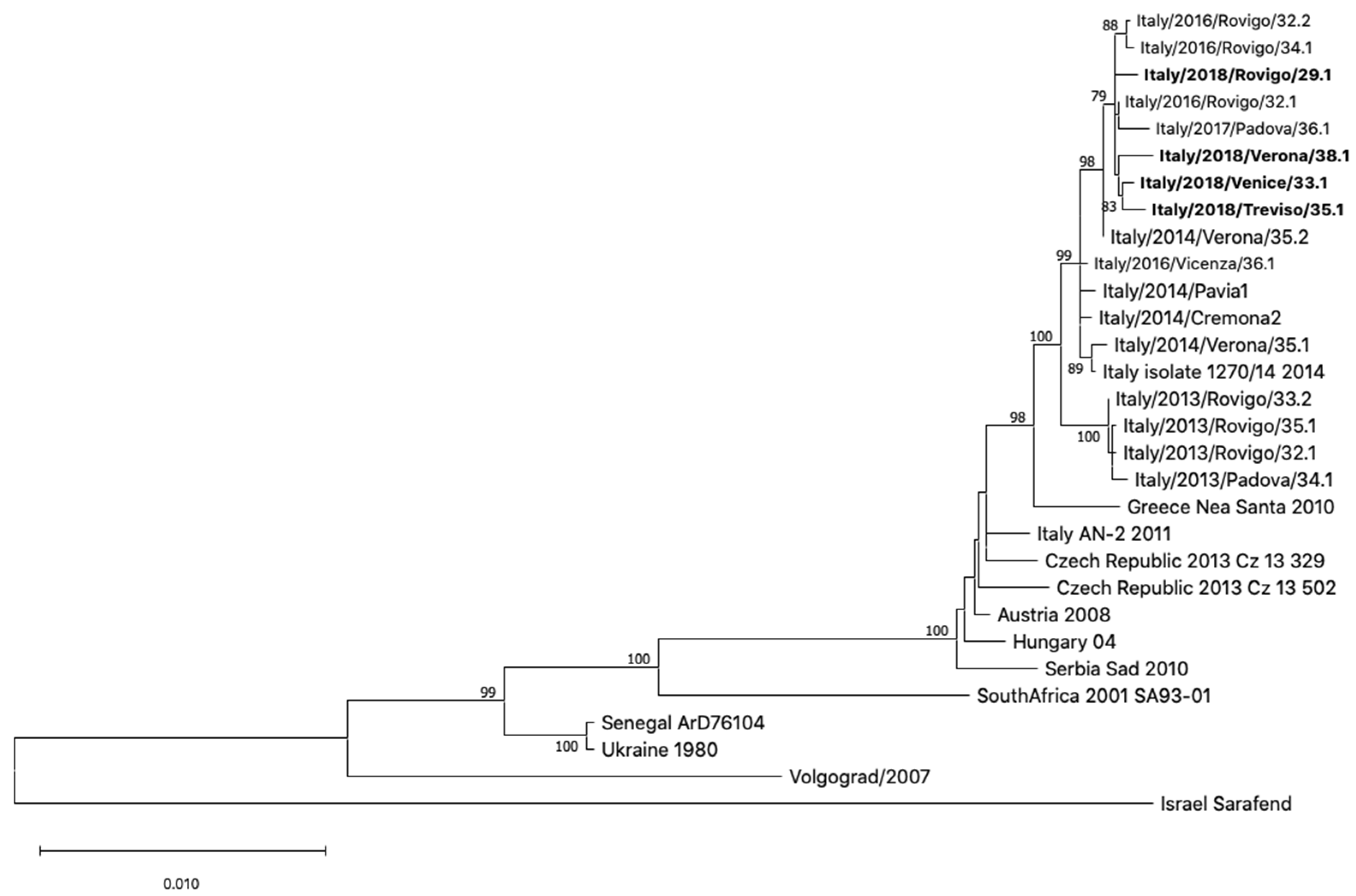
3.5. Phylogenetic Analysis of WNV Genome Sequences
4. Discussion
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- Barzon, L. Ongoing and emerging arbovirus threats in Europe. J. Clin. Virol. 2018, 107, 38–47. [Google Scholar] [CrossRef] [PubMed]
- Sejvar, J.J. The long-term outcomes of human West Nile virus infection. Clin. Infect. Dis. 2007, 44, 1617–1624. [Google Scholar] [CrossRef] [PubMed]
- Rizzoli, A.; Jimenez-Clavero, M.A.; Barzon, L.; Cordioli, P.; Figuerola, J.; Koraka, P.; Martina, B.; Moreno, A.; Nowotny, N.; Pardigon, N.; et al. The challenge of West Nile virus in Europe: Knowledge gaps and research priorities. Euro. Surveill. 2015, 20, 21135. [Google Scholar] [CrossRef] [PubMed]
- Bakonyi, T.; Ivanics, E.; Erdélyi, K.; Ferenczi, E.; Weissenböck, H.; Nowotny, N. Lineage 1 and 2 strains of encephalitic West Nile virus, central Europe. Emerg. Infect. Dis. 2006, 12, 618–623. [Google Scholar] [CrossRef] [PubMed]
- Danis, K.; Papa, A.; Theocharopoulos, G.; Dougas, G.; Athanasiou, M.; Detsis, M.; Baka, A.; Lytras, T.; Mellou, K.; Bonovas, S.; et al. Outbreak of West Nile virus infection in Greece, 2010. Emerg. Infect. Dis. 2011, 17, 1868–1872. [Google Scholar] [CrossRef] [PubMed]
- Barzon, L.; Pacenti, M.; Franchin, E.; Lavezzo, E.; Masi, G.; Squarzon, L.; Pagni, S.; Toppo, S.; Russo, F.; Cattai, M.; et al. Whole genome sequencing and phylogenetic analysis of West Nile virus lineage 1 and lineage 2 from human cases of infection, Italy, August 2013. Euro. Surveill. 2013, 18, 20591. [Google Scholar] [CrossRef] [PubMed]
- Barzon, L.; Pacenti, M.; Franchin, E.; Squarzon, L.; Lavezzo, E.; Cattai, M.; Cusinato, R.; Palù, G. The complex epidemiological scenario of West Nile virus in Italy. Int. J. Environ. Res. Public Health 2013, 10, 4669–4689. [Google Scholar] [CrossRef]
- Barzon, L.; Papa, A.; Lavezzo, E.; Franchin, E.; Pacenti, M.; Sinigaglia, A.; Masi, G.; Trevisan, M.; Squarzon, L.; Toppo, S.; et al. Phylogenetic characterization of Central/Southern European lineage 2 West Nile virus: Analysis of human outbreaks in Italy and Greece, 2013–2014. Clin. Microbiol. Infect. 2015, 21. [Google Scholar] [CrossRef]
- Ravagnan, S.; Montarsi, F.; Cazzin, S.; Porcellato, E.; Russo, F.; Palei, M.; Monne, I.; Savini, G.; Marangon, S.; Barzon, L.; et al. First report outside Eastern Europe of West Nile virus lineage 2 related to the Volgograd 2007 strain, northeastern Italy, 2014. Parasit. Vectors. 2015, 8, 418. [Google Scholar] [CrossRef][Green Version]
- Weissenböck, H.; Bakonyi, T.; Rossi, G.; Mani, P.; Nowotny, N. Usutu virus, Italy, 1996. Emerg. Infect. Dis. 2013, 19, 274–277. [Google Scholar] [CrossRef]
- Mancini, G.; Montarsi, F.; Calzolari, M.; Capelli, G.; Dottori, M.; Ravagnan, S.; Lelli, D.; Chiari, M.; Santilli, A.; Quaglia, M.; et al. Mosquito species involved in the circulation of West Nile and Usutu viruses in Italy. Vet. Ital. 2017, 53, 97–110. [Google Scholar] [CrossRef] [PubMed]
- Pacenti, M.; Sinigaglia, A.; Martello, T.; De Rui, M.E.; Franchin, E.; Pagni, S.; Peta, E.; Riccetti, S.; Milani, A.; Montarsi, F.; et al. Clinical and virological findings in patients with Usutu virus infection, northern Italy, 2018. Euro. Surveill. 2019, 24, 1900180. [Google Scholar] [CrossRef] [PubMed]
- Italian Ministry of Health. Piano nazionale integrato di sorveglianza e risposta ai virus West Nile e Usutu-2018. In National Surveillance and Response Integrated Plan for West Nile and Usutu Viruses-2018; Ministry of Health: Rome, Italy, 2018. Available online: http://www.trovanorme.salute.gov.it/norme/renderNormsanPdf?anno=2018&codLeg=65084&parte=1%20&serie=null (accessed on 30 January 2020).
- Barzon, L.; Squarzon, L.; Cattai, M.; Franchin, E.; Pagni, S.; Cusinato, R.; Palu, G. West Nile virus infection in Veneto region, Italy, 2008-2009. Euro. Surveill. 2009, 14, 19289. [Google Scholar] [CrossRef] [PubMed]
- Gobbi, F.; Capelli, G.; Angheben, A.; Giobbia, M.; Conforto, M.; Franzetti, M.; Cattelan, A.M.; Raise, E.; Rovere, P.; Mulatti, P.; et al. Human and entomological surveillance of West Nile fever, dengue and chikungunya in Veneto Region, Italy, 2010–2012. BMC Infect. Dis. 2014, 14, 60. [Google Scholar] [CrossRef] [PubMed]
- Haussig, J.M.; Young, J.J.; Gossner, C.M.; Mezei, E.; Bella, A.; Sirbu, A.; Pervanidou, D.; Drakulovic, M.B.; Sudre, B. Early start of the West Nile fever transmission season 2018 in Europe. Euro. Surveill. 2018, 23, 1800428. [Google Scholar] [CrossRef] [PubMed]
- Nagy, A.; Mezei, E.; Nagy, O.; Bakonyi, T.; Csonka, N.; Kaposi, M.; Koroknai, A.; Szomor, K.; Rigó, Z.; Molnár, Z.; et al. Extraordinary increase in West Nile virus cases and first confirmed human Usutu virus infection in Hungary, 2018. Euro. Surveill. 2019, 24, 1900038. [Google Scholar] [CrossRef]
- Riccardo, F.; Monaco, F.; Bella, A.; Savini, G.; Russo, F.; Cagarelli, R.; Dottori, M.; Rizzo, C.; Venturi, G.; Di Luca, M.; et al. An early start of West Nile virus seasonal transmission: The added value of One Heath surveillance in detecting early circulation and triggering timely response in Italy, June to July 2018. Euro. Surveill. 2018, 23, 1800427. [Google Scholar] [CrossRef]
- European Centre for Disease Prevention and Control. West Nile virus infection. In ECDC. Annual Epidemiological Report for 2018; ECDC: Stockholm, Sweden, 2019; Available online: https://www.ecdc.europa.eu/sites/default/files/documents/west-nile-fever-annual-epidemiological-report-2018.pdf (accessed on 30 January 2020).
- Istituto Superiore di Sanità. Febbre West Nile. Dati Epidemiologici [West Nile Fever. Epidemiological Data]. Istituto Superiore di Sanità. Available online: https://www.epicentro.iss.it/westnile/epidemiologia-italia (accessed on 30 January 2020).
- Barzon, L.; Pacenti, M.; Franchin, E.; Pagni, S.; Martello, T.; Cattai, M.; Cusinato, R.; Palù, G. Excretion of West Nile virus in urine during acute infection. J. Infect. Dis. 2013, 208, 1086–1092. [Google Scholar] [CrossRef]
- Scaramozzino, N.; Crance, J.M.; Jouan, A.; DeBriel, D.A.; Stoll, F.; Garin, D. Comparison of flavivirus universal primer pairs and development of a rapid, highly sensitive heminested reverse transcription-PCR assay for detection of flaviviruses targeted to a conserved region of the NS5 gene sequences. J. Clin. Microbiol. 2001, 39, 1922–1927. [Google Scholar] [CrossRef]
- Sinigaglia, A.; Pacenti, M.; Martello, T.; Pagni, S.; Franchin, E.; Barzon, L. West Nile virus infection in individuals with pre-existing Usutu virus immunity, Northern Italy, 2018. Euro. Surveill. 2019, 24. [Google Scholar] [CrossRef]
- Jean, C.M.; Honarmand, S.; Louie, J.K.; Glaser, C.A. Risk factors for West Nile virus neuroinvasive disease, California, 2005. Emerg. Infect. Dis. 2007, 13, 1918–1920. [Google Scholar] [CrossRef] [PubMed]
- Pezzotti, P.; Piovesan, C.; Barzon, L.; Cusinato, R.; Cattai, M.; Pacenti, M.; Piazza, A.; Franchin, E.; Pagni, S.; Bressan, S.; et al. Prevalence of IgM and IgG antibodies to West Nile virus among blood donors in an affected area of north-eastern Italy, summer 2009. Euro. Surveill. 2011, 16, 19814. [Google Scholar] [CrossRef] [PubMed]
- Ingersoll, M.A. Sex differences shape the response to infectious diseases. PLoS Pathog. 2017, 13, e1006688. [Google Scholar] [CrossRef] [PubMed]
- Ghosh, S.; Klein, R.S. Sex drives dimorphic immune responses to viral infections. J. Immunol. 2017, 198, 1782–1790. [Google Scholar] [CrossRef]
- McDonald, E.; Martin, S.W.; Landry, K.; Gould, C.V.; Lehman, J.; Fischer, M.; Lindsey, N.P. West Nile virus and other domestic nationally notifiable arboviral diseases-United States, 2018. MMWR Morb. Mortal. Wkly. Rep. 2019, 68, 673–678. [Google Scholar] [CrossRef]
- Brown, J.A.; Factor, D.L.; Tkachenko, N.; Templeton, S.M.; Crall, N.D.; Pape, W.J.; Bauer, M.J.; Ambruso, D.R.; Dickey, W.D.; Marfin, A.A. West Nile viremic blood donors and risk factors for subsequent West Nile fever. Vector Borne Zoonotic. Dis. 2007, 7, 479–488. [Google Scholar] [CrossRef]
- Zehender, G.; Veo, C.; Ebranati, E.; Carta, V.; Rovida, F.; Percivalle, E.; Moreno, A.; Lelli, D.; Calzolari, M.; Lavazza, A.; et al. Reconstructing the recent West Nile virus lineage 2 epidemic in Europe and Italy using discrete and continuous phylogeography. PLoS ONE 2017, 12, e0179679. [Google Scholar] [CrossRef]
- Chaintoutis, S.C.; Papa, A.; Pervanidou, D.; Dovas, C.I. Evolutionary dynamics of lineage 2 West Nile virus in Europe, 2004-2018: Phylogeny, selection pressure and phylogeography. Mol. Phylogenet. Evol. 2019, 141, 106617. [Google Scholar] [CrossRef]
- Veo, C.; Della Ventura, C.; Moreno, A.; Rovida, F.; Percivalle, E.; Canziani, S.; Torri, D.; Calzolari, M.; Baldanti, F.; Galli, M.; et al. Evolutionary dynamics of the lineage 2 West Nile virus that caused the largest European epidemic: Italy 2011–2018. Viruses 2019, 11, 814. [Google Scholar] [CrossRef]
- Camp, J.V.; Nowotny, N. The knowns and unknowns of West Nile virus in Europe: What did we learn from the 2018 outbreak? Expert Rev. Anti. Infect. Ther. 2020, 18, 145–154. [Google Scholar] [CrossRef]
- Marini, G.; Calzolari, M.; Angelini, P.; Bellini, R.; Bellini, S.; Bolzoni, L.; Torri, D.; Defilippo, F.; Dorigatti, I.; Nikolay, B.; et al. A quantitative comparison of West Nile virus incidence from 2013 to 2018 in Emilia-Romagna, Italy. PLoS Negl. Trop. Dis. 2020, 14, e0007953. [Google Scholar] [CrossRef] [PubMed]

| Characteristic | Clinical Condition | ||
|---|---|---|---|
| WNND (n = 86) | WNF (n = 307) | Blood Donor (n = 34) | |
| Age, years | |||
| Median (IQR) | 75 (60–81) a | 56 (41–70) a | 51 (44–57) |
| Sex, no. (%) | |||
| Male | 56 (65) b | 172 (56) b | 27 (0.035) c |
| Female | 30 (35) | 135 (44) | 7 (0.017) c |
| Clinical syndrome, no. (%) | |||
| Encephalitis | 34 (44) | 0 | 0 |
| Meningitis | 31 (40) | 0 | 0 |
| Meningoencephalitis | 9 (12) | 0 | 0 |
| Acute flaccid paralysis | 2 (3) | 0 | 0 |
| Guillain Barré syndrome | 1 (1) | 0 | 0 |
| Symptoms, no. (%) | |||
| Days since onset of symptoms or index blood donation, median (IQR) | 6 (1–12) | 9 (1–20) | 4 (2–6) |
| Fever | 84 (97) | 264 (86) | 9 (26) |
| Median temperature, °C | 39.0 (up to 41) | 38.5 (up to 40.5) | 38 (up to 39) |
| Arthralgia | 20 (23) | 141 (46) | 7 (21) |
| Myalgia | 21 (24) | 130 (43) | 12 (35) |
| Headache | 41 (47) | 138 (45) | 12 (35) |
| Asthenia | 53 (61) | 184 (60) | 14 (41) |
| Lymphadenopathy | 4 (4) | 34 (11) | 2 (6) |
| Itching | 0 | 9 (9) | 4 (12) |
| Rash | 22 (26) | 138 (45) | 8 (24) |
| Gastrointestinal symptoms | 0 | 17 (6) | 4 (12) |
| Asymptomatic | 0 | 0 | 10 (29) |
| Outcome | |||
| Death, no. (%) | 19 (22) | 0 | 0 |
| Male | 10 (53) | - | - |
| Female | 9 (47) | - | - |
| Age, median years (range) | 81 (58–91) | - | - |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Pacenti, M.; Sinigaglia, A.; Franchin, E.; Pagni, S.; Lavezzo, E.; Montarsi, F.; Capelli, G.; Barzon, L. Human West Nile Virus Lineage 2 Infection: Epidemiological, Clinical, and Virological Findings. Viruses 2020, 12, 458. https://doi.org/10.3390/v12040458
Pacenti M, Sinigaglia A, Franchin E, Pagni S, Lavezzo E, Montarsi F, Capelli G, Barzon L. Human West Nile Virus Lineage 2 Infection: Epidemiological, Clinical, and Virological Findings. Viruses. 2020; 12(4):458. https://doi.org/10.3390/v12040458
Chicago/Turabian StylePacenti, Monia, Alessandro Sinigaglia, Elisa Franchin, Silvana Pagni, Enrico Lavezzo, Fabrizio Montarsi, Gioia Capelli, and Luisa Barzon. 2020. "Human West Nile Virus Lineage 2 Infection: Epidemiological, Clinical, and Virological Findings" Viruses 12, no. 4: 458. https://doi.org/10.3390/v12040458
APA StylePacenti, M., Sinigaglia, A., Franchin, E., Pagni, S., Lavezzo, E., Montarsi, F., Capelli, G., & Barzon, L. (2020). Human West Nile Virus Lineage 2 Infection: Epidemiological, Clinical, and Virological Findings. Viruses, 12(4), 458. https://doi.org/10.3390/v12040458








