Host Cellular Receptors for the Peste des Petits Ruminant Virus
Abstract
1. Introduction
2. PPRV Genome Organization
3. PPRV Host Cellular Receptors
3.1. Signaling Lymphocyte Activation Molecule (SLAM/CD150)
3.2. Nectin-4/PVRL4
3.3. CD46
3.4. Other Putative Receptors
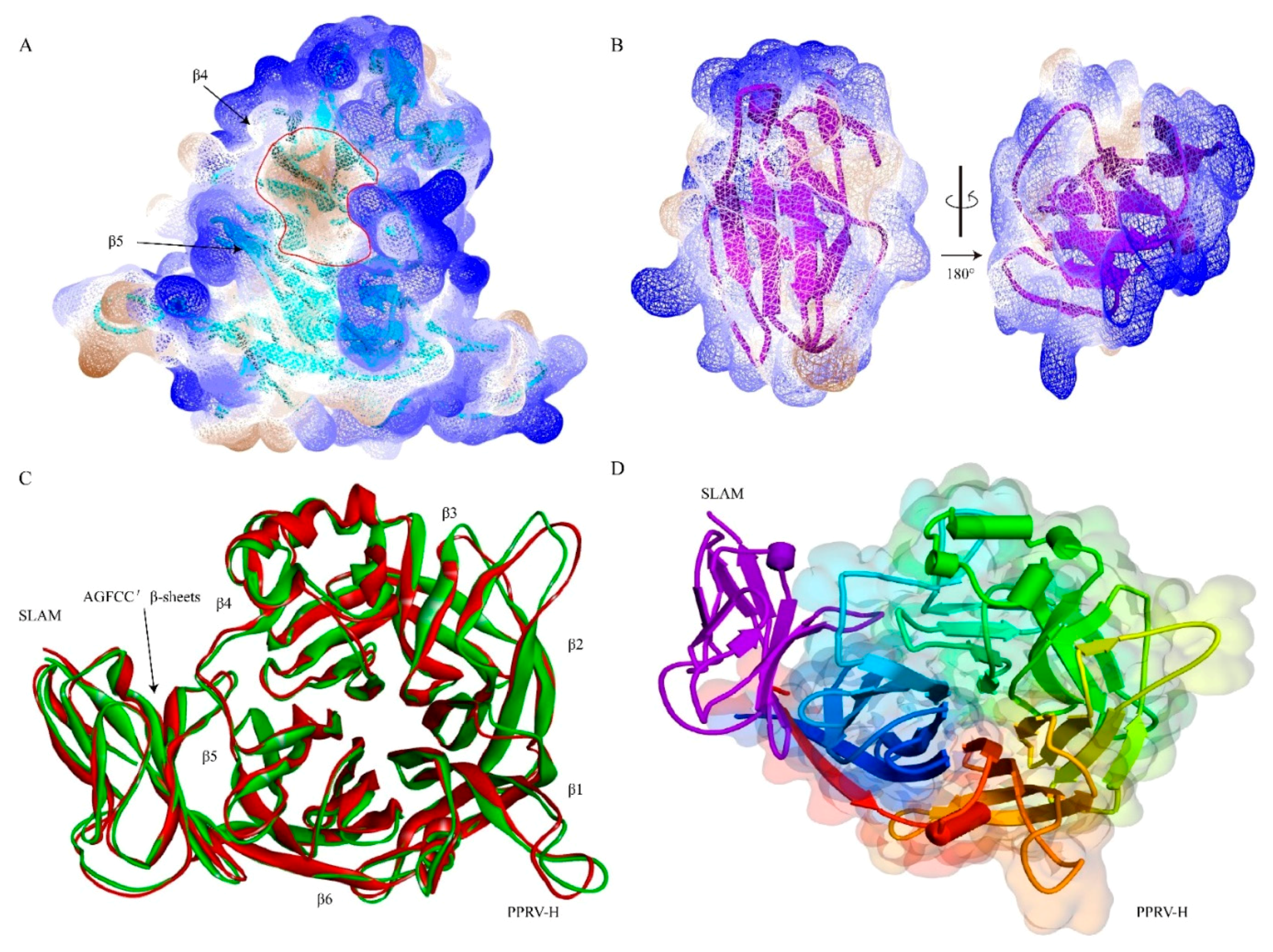
4. Receptor Binding Domain (Ligand) on PPRV H Protein
5. The Potential Role of Virus-Receptor Interaction in Host Range Restriction
6. The Impact of Virus-Receptor Interactions on the Immune Response against PPRV
6.1. Innate Immune Response
6.2. Adaptive Immune Response
6.3. Inhibitory Impact of Viral Protein-SLAM Interactions on the Immune Response
7. Conclusions
Funding
Conflicts of Interest
References
- OIE. Geographical Distribution of PPR. Available online: http://www.oie.int/en/animal-health-in-the-world/ppr-portal/distribution/ (accessed on 17 May 2018).
- Nanda, Y.P.; Chatterjee, A.; Purohit, A.K.; Diallo, A.; Innui, K.; Sharma, R.N.; Libeau, G.; Thevasagayam, J.A.; Bruning, A.; Kitching, R.P.; et al. The isolation of peste des petits ruminants virus from northern India. Vet. Microbiol. 1996, 51, 207–216. [Google Scholar] [CrossRef]
- Truong, T.; Boshra, H.; Embury-Hyatt, C.; Nfon, C.; Gerdts, V.; Tikoo, S.; Babiuk, L.A.; Kara, P.; Chetty, T.; Mather, A.; et al. Peste des petits ruminants virus tissue tropism and pathogenesis in sheep and goats following experimental infection. PLoS ONE 2014, 9, e87145. [Google Scholar] [CrossRef] [PubMed]
- Parida, S.; Muniraju, M.; Altan, E.; Baazizi, R.; Raj, G.D.; Mahapatra, M. Emergence of PPR and its threat to Europe. Small Rumin. Res. 2016, 142, 16–21. [Google Scholar] [CrossRef] [PubMed]
- Khan, H.A.; Siddique, M.; Abubakar, M.; Ashraf, M. The detection of antibody against peste des petits ruminants virus in sheep, goats, cattle and buffaloes. Trop. Anim. Health Prod. 2008, 40, 521–527. [Google Scholar] [CrossRef] [PubMed]
- Pope, R.A.; Parida, S.; Bailey, D.; Brownlie, J.; Barrett, T.; Banyard, A.C. Early events following experimental infection with Peste-Des-Petits ruminants virus suggest immune cell targeting. PLoS ONE 2013, 8, e55830. [Google Scholar] [CrossRef] [PubMed]
- Scott, G.R. Rinderpest and peste des petits ruminants. In Virus Diseases of Food Animals. A World Geography of Epidemiology and Control; Gibbs, E.P.J., Ed.; Academic Press: Cambridge, MA, USA, 1981; Volume 11, pp. 401–432. [Google Scholar]
- Kahn, C.M. Peste Des Petits Ruminants. In The Merck Veterinary Manual, 9th ed.; Merck and Co.Inc.: Whitehouse Station, NJ, USA, 2008. [Google Scholar]
- Barrett, T.; Amarel-Doel, C.; Kitching, R.P.; Gusev, A. Use of the polymerase chain reaction in differentiating rinderpest field virus and vaccine virus in the same animals. Rev. Sci. Tech. 1993, 12, 865–872. [Google Scholar] [CrossRef] [PubMed]
- Bailey, D.; Banyard, A.; Dash, P.; Ozkul, A.; Barrett, T. Full genome sequence of peste des petits ruminants virus, a member of the Morbillivirus genus. Virus Res. 2005, 110, 119–124. [Google Scholar] [CrossRef]
- Durojaiye, O.A.; Taylor, W.P.; Smale, C. The ultrastructure of peste des petits ruminants virus. Zent. Fur Vet. Reihe B. J. Vet. Med. Ser. B 1985, 32, 460–465. [Google Scholar] [CrossRef]
- Gibbs, E.P.; Taylor, W.P.; Lawman, M.J.; Bryant, J. Classification of peste des petits ruminants virus as the fourth member of the genus Morbillivirus. Intervirology 1979, 11, 268–274. [Google Scholar] [CrossRef]
- Diallo, A. Morbillivirus group: Genome organisation and proteins. Vet. Microbiol. 1990, 23, 155–163. [Google Scholar] [CrossRef]
- Crowley, J.C.; Dowling, P.C.; Menonna, J.; Silverman, J.I.; Schuback, D.; Cook, S.D.; Blumberg, B.M. Sequence variability and function of measles virus 3′ and 5′ ends and intercistronic regions. Virology 1988, 164, 498–506. [Google Scholar] [CrossRef]
- Diallo, A.; Barrett, T.; Barbron, M.; Meyer, G.; Lefevre, P.C. Cloning of the nucleocapsid protein gene of peste-des-petits-ruminants virus: Relationship to other morbilliviruses. J. Gen. Virol. 1994, 75, 233–237. [Google Scholar] [CrossRef] [PubMed]
- Haas, L.; Baron, M.D.; Liess, B.; Barrett, T. Editing of morbillivirus P gene transcripts in infected animals. Vet. Microbiol. 1995, 44, 299–306. [Google Scholar] [CrossRef]
- Sidhu, M.S.; Husar, W.; Cook, S.D.; Dowling, P.C.; Udem, S.A. Canine distemper terminal and intergenic non-protein coding nucleotide sequences: Completion of the entire CDV genome sequence. Virology 1993, 193, 66–72. [Google Scholar] [CrossRef] [PubMed]
- Lamb, R.A.; Kolakofsky, D. Paramyxoviridae: The viruses and their replication. In Fields Virology, 4th ed.; Fields, B.N., Knipe, D.N., Howley, P.M., Eds.; Lippincott Williams and Wilkins: Philadelphia, PA, USA, 2001; pp. 1305–1340. [Google Scholar]
- Dhar, P.; Sreenivasa, B.P.; Barrett, T.; Corteyn, M.; Singh, R.P.; Bandyopadhyay, S.K. Recent epidemiology of peste des petits ruminants virus (PPRV). Vet. Microbiol. 2002, 88, 153–159. [Google Scholar] [CrossRef]
- Birch, J.; Juleff, N.; Heaton, M.P.; Kalbfleisch, T.; Kijas, J.; Bailey, D. Characterization of ovine Nectin-4, a novel peste des petits ruminants virus receptor. J. Virol. 2013, 87, 4756–4761. [Google Scholar] [CrossRef] [PubMed]
- Pawar, R.M.; Raj, G.D.; Kumar, T.M.A.S.; Raja, A.; Balachandran, C. Effect of siRNA mediated suppression of signaling lymphocyte activation molecule on replication of peste des petits ruminants virus in vitro. Virus Res. 2008, 136, 118–123. [Google Scholar] [CrossRef]
- Dorig, R.E.; Marcil, A.; Chopra, A.; Richardson, C.D. The human CD46 molecule is a receptor for measles virus (Edmonston strain). Cell 1993, 75, 295–305. [Google Scholar] [CrossRef]
- Yang, B.; Qi, X.; Guo, H.; Jia, P.; Chen, S.; Chen, Z.; Wang, T.; Wang, J.; Xue, Q. Peste des Petits Ruminants Virus Enters Caprine Endometrial Epithelial Cells via the Caveolae-Mediated Endocytosis Pathway; Frontiers: Lausanne, Switzerland, 2018; Volume 9, p. 210. [Google Scholar]
- Tatsuo, H.; Ono, N.; Yanagi, Y. Morbilliviruses use signaling lymphocyte activation molecules (CD150) as cellular receptors. J. Virol. 2001, 75, 5842–5850. [Google Scholar] [CrossRef]
- Tatsuo, H.; Ono, N.; Tanaka, K.; Yanagi, Y. SLAM (CDw150) is a cellular receptor for measles virus. Nature 2000, 406, 893–897. [Google Scholar] [CrossRef]
- Pawar, R.M.; Dhinakar Raj, G.; Balachandran, C. Relationship between the level of signaling lymphocyte activation molecule mRNA and replication of Peste-des-petits-ruminants virus in peripheral blood mononuclear cells of host animals. Acta Virol. 2008, 52, 231–236. [Google Scholar] [PubMed]
- Sarkar, J.; Balamurugan, V.; Sen, A.; Saravanan, P.; Sahay, B.; Rajak, K.K.; Rasool, T.J.; Bhanuprakash, V.; Singh, R.K. Sequence analysis of morbillivirus CD150 receptor-Signaling Lymphocyte Activation Molecule (SLAM) of different animal species. Virus Genes 2009, 39, 335–341. [Google Scholar] [CrossRef] [PubMed]
- Ohishi, K.; Ando, A.; Suzuki, R.; Takishita, K.; Kawato, M.; Katsumata, E.; Ohtsu, D.; Okutsu, K.; Tokutake, K.; Miyahara, H.; et al. Host–virus specificity of morbilliviruses predicted by structural modeling of the marine mammal SLAM, a receptor. Comp. Immunol. Microbiol. Infect. Dis. 2010, 33, 227–241. [Google Scholar] [CrossRef] [PubMed]
- Veillette, A.; Latour, S. The SLAM family of immune-cell receptors. Curr. Opin. Immunol. 2003, 15, 277–285. [Google Scholar] [CrossRef]
- Vincent, S.; Spehner, D.; Manie, S.; Delorme, R.; Drillien, R.; Gerlier, D. Inefficient measles virus budding in murine L.CD46 fibroblasts. Virology 1999, 265, 185–195. [Google Scholar] [CrossRef] [PubMed]
- Schwartzberg, P.L.; Mueller, K.L.; Qi, H.; Cannons, J.L. SLAM receptors and SAP influence lymphocyte interactions, development and function. Nat. Rev. Immunol. 2009, 9, 39. [Google Scholar] [CrossRef] [PubMed]
- Cocks, B.G.; Chang, C.C.; Carballido, J.M.; Yssel, H.; de Vries, J.E.; Aversa, G. A novel receptor involved in T-cell activation. Nature 1995, 376, 260–263. [Google Scholar] [CrossRef] [PubMed]
- Tangye, S.G.; Phillips, J.H.; Lanier, L.L. The CD2-subset of the Ig superfamily of cell surface molecules: Receptor-ligand pairs expressed by NK cells and other immune cells. Semin. Immunol. 2000, 12, 149–157. [Google Scholar] [CrossRef] [PubMed]
- Ono, N.; Tatsuo, H.; Tanaka, K.; Minagawa, H.; Yanagi, Y. V domain of human SLAM (CDw150) is essential for its function as a measles virus receptor. J. Virol. 2001, 75, 1594–1600. [Google Scholar] [CrossRef] [PubMed]
- Ohno, S.; Seki, F.; Ono, N.; Yanagi, Y. Histidine at position 61 and its adjacent amino acid residues are critical for the ability of SLAM (CD150) to act as a cellular receptor for measles virus. J. Gen. Virol. 2003, 84, 2381–2388. [Google Scholar] [CrossRef] [PubMed]
- Castro, A.G.; Hauser, T.M.; Cocks, B.G.; Abrams, J.; Zurawski, S.; Churakova, T.; Zonin, F.; Robinson, D.; Tangye, S.G.; Aversa, G.; et al. Molecular and functional characterization of mouse signaling lymphocytic activation molecule (SLAM): Differential expression and responsiveness in Th1 and Th2 cells. J. Immunol. 1999, 163, 5860–5870. [Google Scholar] [PubMed]
- Ono, N.; Tatsuo, H.; Hidaka, Y.; Aoki, T.; Minagawa, H.; Yanagi, Y. Measles viruses on throat swabs from measles patients use signaling lymphocytic activation molecule (CDw150) but not CD46 as a cellular receptor. J. Virol. 2001, 75, 4399–4401. [Google Scholar] [CrossRef] [PubMed]
- Yanagi, Y.; Takeda, M.; Ohno, S.; Hashiguchi, T. Measles virus receptors. Curr. Top. Microbiol. Immunol. 2009, 329, 13–30. [Google Scholar] [PubMed]
- Lu, G.; Gao, G.F.; Yan, J. The receptors and entry of measles virus: A review. Sheng Wu Gong Cheng Xue Bao 2013, 29, 1–9. [Google Scholar] [PubMed]
- Navaratnarajah, C.K.; Vongpunsawad, S.; Oezguen, N.; Stehle, T.; Braun, W.; Hashiguchi, T.; Maenaka, K.; Yanagi, Y.; Cattaneo, R. Dynamic interaction of the measles virus hemagglutinin with its receptor signaling lymphocytic activation molecule (SLAM, CD150). J. Biol. Chem. 2008, 283, 11763–11771. [Google Scholar] [CrossRef] [PubMed]
- De Vries, R.D.; McQuaid, S.; van Amerongen, G.; Yuksel, S.; Verburgh, R.J.; Osterhaus, A.D.; Duprex, W.P.; de Swart, R.L. Measles immune suppression: Lessons from the macaque model. PLoS Pathog. 2012, 8, e1002885. [Google Scholar] [CrossRef] [PubMed]
- Laksono, B.M.; Grosserichter-Wagener, C.; de Vries, R.D.; Langeveld, S.A.G.; Brem, M.D.; van Dongen, J.J.M.; Katsikis, P.D.; Koopmans, M.P.G.; van Zelm, M.C.; de Swart, R.L. In Vitro Measles Virus Infection of Human Lymphocyte Subsets Demonstrates High Susceptibility and Permissiveness of both Naive and Memory B Cells. J. Virol. 2018, 92. [Google Scholar] [CrossRef] [PubMed]
- Condack, C.; Grivel, J.C.; Devaux, P.; Margolis, L.; Cattaneo, R. Measles virus vaccine attenuation: Suboptimal infection of lymphatic tissue and tropism alteration. J. Infect. Dis. 2007, 196, 541–549. [Google Scholar] [CrossRef]
- Rojas, J.M.; Moreno, H.; Valcarcel, F.; Pena, L.; Sevilla, N.; Martin, V. Vaccination with recombinant adenoviruses expressing the peste des petits ruminants virus F or H proteins overcomes viral immunosuppression and induces protective immunity against PPRV challenge in sheep. PLoS ONE 2014, 9, e101226. [Google Scholar] [CrossRef]
- Herbert, R.; Baron, J.; Batten, C.; Baron, M.; Taylor, G. Recombinant adenovirus expressing the haemagglutinin of Peste des petits ruminants virus (PPRV) protects goats against challenge with pathogenic virus; a DIVA vaccine for PPR. Vet. Res. 2014, 45, 24. [Google Scholar] [CrossRef]
- Manjunath, S.; Kumar, G.R.; Mishra, B.P.; Mishra, B.; Sahoo, A.P.; Joshi, C.G.; Tiwari, A.K.; Rajak, K.K.; Janga, S.C. Genomic analysis of host—Peste des petits ruminants vaccine viral transcriptome uncovers transcription factors modulating immune regulatory pathways. Vet. Res. 2015, 46, 15. [Google Scholar] [CrossRef] [PubMed]
- Mondal, B.; Sreenivasa, B.P.; Dhar, P.; Singh, R.P.; Bandyopadhyay, S.K. Apoptosis induced by peste des petits ruminants virus in goat peripheral blood mononuclear cells. Virus Res. 2001, 73, 113–119. [Google Scholar] [CrossRef]
- Kul, O.; Kabakci, N.; Atmaca, H.T.; Ozkul, A. Natural peste des petits ruminants virus infection: Novel pathologic findings resembling other morbillivirus infections. Vet Pathol. 2007, 44, 479–486. [Google Scholar] [CrossRef] [PubMed]
- Griffin, D.E. Measles virus. In Fields Virology, 5th ed.; Knipe, D.M., Howley, P.M., Griffin, D.E., Lamb, R.A., Martin, M.A., Roizman, B., Straus, S.E., Eds.; Lippincott Williams & Wilkins: Philadelphia, PA, USA, 2007; pp. 1551–1585. [Google Scholar]
- Muhlebach, M.D.; Mateo, M.; Sinn, P.L.; Prufer, S.; Uhlig, K.M.; Leonard, V.H.; Navaratnarajah, C.K.; Frenzke, M.; Wong, X.X.; Sawatsky, B.; et al. Adherens junction protein nectin-4 is the epithelial receptor for measles virus. Nature 2011, 480, 530–533. [Google Scholar] [CrossRef] [PubMed]
- Noyce, R.S.; Bondre, D.G.; Ha, M.N.; Lin, L.T.; Sisson, G.; Tsao, M.S.; Richardson, C.D. Tumor cell marker PVRL4 (nectin 4) is an epithelial cell receptor for measles virus. PLoS Pathog. 2011, 7, e1002240. [Google Scholar] [CrossRef] [PubMed]
- Delpeut, S.; Noyce, R.S.; Richardson, C.D. The tumor-associated marker, PVRL4 (nectin-4), is the epithelial receptor for morbilliviruses. Viruses 2014, 6, 2268–2286. [Google Scholar] [CrossRef] [PubMed]
- Delpeut, S.; Noyce, R.S.; Richardson, C.D. The V domain of dog PVRL4 (nectin-4) mediates canine distemper virus entry and virus cell-to-cell spread. Virology 2014, 454, 109–117. [Google Scholar] [CrossRef] [PubMed]
- Takai, Y.; Miyoshi, J.; Ikeda, W.; Ogita, H. Nectins and nectin-like molecules: Roles in contact inhibition of cell movement and proliferation. Nat. Rev. Mol. Cell Biol. 2008, 9, 603–615. [Google Scholar] [CrossRef] [PubMed]
- Fabre, S.; Reymond, N.; Cocchi, F.; Menotti, L.; Dubreuil, P.; Campadelli-Fiume, G.; Lopez, M. Prominent role of the Ig-like V domain in trans-interactions of nectins. Nectin3 and nectin 4 bind to the predicted C-C′-C″-D beta-strands of the nectin1 V domain. J. Biol. Chem. 2002, 277, 27006–27013. [Google Scholar] [CrossRef] [PubMed]
- Takai, Y.; Ikeda, W.; Ogita, H.; Rikitake, Y. The immunoglobulin-like cell adhesion molecule nectin and its associated protein afadin. Annu. Rev. Cell Dev. Biol. 2008, 24, 309–342. [Google Scholar] [CrossRef]
- Satoh-Horikawa, K.; Nakanishi, H.; Takahashi, K.; Miyahara, M.; Nishimura, M.; Tachibana, K.; Mizoguchi, A.; Takai, Y. Nectin-3, a new member of immunoglobulin-like cell adhesion molecules that shows homophilic and heterophilic cell-cell adhesion activities. J. Biol. Chem. 2000, 275, 10291–10299. [Google Scholar] [CrossRef] [PubMed]
- Mendelsohn, C.L.; Wimmer, E.; Racaniello, V.R. Cellular receptor for poliovirus: Molecular cloning, nucleotide sequence, and expression of a new member of the immunoglobulin superfamily. Cell 1989, 56, 855–865. [Google Scholar] [CrossRef]
- Takahashi, K.; Nakanishi, H.; Miyahara, M.; Mandai, K.; Satoh, K.; Satoh, A.; Nishioka, H.; Aoki, J.; Nomoto, A.; Mizoguchi, A.; et al. Nectin/PRR: An immunoglobulin-like cell adhesion molecule recruited to cadherin-based adherens junctions through interaction with Afadin, a PDZ domain-containing protein. J. Cell Biol. 1999, 145, 539–549. [Google Scholar] [CrossRef] [PubMed]
- Reymond, N.; Fabre, S.; Lecocq, E.; Adelaide, J.; Dubreuil, P.; Lopez, M. Nectin4/PRR4, a new afadin-associated member of the nectin family that trans-interacts with nectin1/PRR1 through V domain interaction. J. Biol. Chem. 2001, 276, 43205–43215. [Google Scholar] [CrossRef] [PubMed]
- Pratakpiriya, W.; Seki, F.; Otsuki, N.; Sakai, K.; Fukuhara, H.; Katamoto, H.; Hirai, T.; Maenaka, K.; Techangamsuwan, S.; Lan, N.T.; et al. Nectin4 is an epithelial cell receptor for canine distemper virus and involved in neurovirulence. J. Virol. 2012, 86, 10207–10210. [Google Scholar] [CrossRef] [PubMed]
- Pratakpiriya, W.; Ping Teh, A.P.; Radtanakatikanon, A.; Pirarat, N.; Thi Lan, N.; Takeda, M.; Techangamsuwan, S.; Yamaguchi, R. Expression of canine distemper virus receptor nectin-4 in the central nervous system of dogs. Sci. Rep. 2017, 7, 349. [Google Scholar] [CrossRef] [PubMed]
- Alves, L.; Khosravi, M.; Avila, M.; Ader-Ebert, N.; Bringolf, F.; Zurbriggen, A.; Vandevelde, M.; Plattet, P. SLAM- and Nectin-4-Independent Noncytolytic Spread of Canine Distemper Virus in Astrocytes. J. Virol. 2015, 89, 5724–5733. [Google Scholar] [CrossRef] [PubMed]
- Fakri, F.; Elarkam, A.; Daouam, S.; Tadlaoui, K.; Fassi-Fihri, O.; Richardson, C.D.; Elharrak, M. VeroNectin-4 is a highly sensitive cell line that can be used for the isolation and titration of Peste des Petits Ruminants virus. J. Virol. Methods 2016, 228, 135–139. [Google Scholar] [CrossRef]
- Ogita, H.; Rikitake, Y.; Miyoshi, J.; Takai, Y. Cell adhesion molecules nectins and associating proteins: Implications for physiology and pathology. Proc. Jpn. Acad. Ser. B Phys. Biol. Sci. 2010, 86, 621–629. [Google Scholar] [CrossRef]
- Abdullah, H.; Brankin, B.; Brady, C.; Cosby, S.L. Wild-type measles virus infection upregulates poliovirus receptor-related 4 and causes apoptosis in brain endothelial cells by induction of tumor necrosis factor-related apoptosis-inducing ligand. J. Neuropathol. Exp Neurol. 2013, 72, 681–696. [Google Scholar] [CrossRef]
- Leonard, V.H.; Sinn, P.L.; Hodge, G.; Miest, T.; Devaux, P.; Oezguen, N.; Braun, W.; McCray, P.B., Jr.; McChesney, M.B.; Cattaneo, R. Measles virus blind to its epithelial cell receptor remains virulent in rhesus monkeys but cannot cross the airway epithelium and is not shed. J. Clin. Investig. 2008, 118, 2448–2458. [Google Scholar] [CrossRef] [PubMed]
- Ludlow, M.; Rennick, L.J.; Sarlang, S.; Skibinski, G.; McQuaid, S.; Moore, T.; de Swart, R.L.; Duprex, W.P. Wild-type measles virus infection of primary epithelial cells occurs via the basolateral surface without syncytium formation or release of infectious virus. J. Gen. Virol. 2010, 91, 971–979. [Google Scholar] [CrossRef] [PubMed]
- Naniche, D.; Varior-Krishnan, G.; Cervoni, F.; Wild, T.F.; Rossi, B.; Rabourdin-Combe, C.; Gerlier, D. Human membrane cofactor protein (CD46) acts as a cellular receptor for measles virus. J. Virol. 1993, 67, 6025–6032. [Google Scholar] [PubMed]
- Buchholz, C.J.; Schneider, U.; Devaux, P.; Gerlier, D.; Cattaneo, R. Cell entry by measles virus: Long hybrid receptors uncouple binding from membrane fusion. J. Virol. 1996, 70, 3716–3723. [Google Scholar] [PubMed]
- Buchholz, C.J.; Koller, D.; Devaux, P.; Mumenthaler, C.; Schneider-Schaulies, J.; Braun, W.; Gerlier, D.; Cattaneo, R. Mapping of the primary binding site of measles virus to its receptor CD46. J. Biol. Chem. 1997, 272, 22072–22079. [Google Scholar] [CrossRef] [PubMed]
- Galbraith, S.E.; Tiwari, A.; Baron, M.D.; Lund, B.T.; Barrett, T.; Cosby, S.L. Morbillivirus downregulation of CD46. J. Virol. 1998, 72, 10292–10297. [Google Scholar] [PubMed]
- Naniche, D.; Wild, T.F.; Rabourdin-Combe, C.; Gerlier, D. Measles virus haemagglutinin induces down-regulation of gp57/67, a molecule involved in virus binding. J. Gen. Virol. 1993, 74, 1073–1079. [Google Scholar] [CrossRef]
- Singethan, K.; Topfstedt, E.; Schubert, S.; Duprex, W.P.; Rima, B.K.; Schneider-Schaulies, J. CD9-dependent regulation of Canine distemper virus-induced cell-cell fusion segregates with the extracellular domain of the haemagglutinin. J. Gen. Virol. 2006, 87, 1635–1642. [Google Scholar] [CrossRef]
- Marie, J.C.; Astier, A.L.; Rivailler, P.; Rabourdin-Combe, C.; Wild, T.F.; Horvat, B. Linking innate and acquired immunity: Divergent role of CD46 cytoplasmic domains in T cell–induced inflammation. Nature Immunol. 2002, 3, 659. [Google Scholar] [CrossRef]
- Kemper, C.; Chan, A.C.; Green, J.M.; Brett, K.A.; Murphy, K.M.; Atkinson, J.P. Activation of human CD4+ cells with CD3 and CD46 induces a T-regulatory cell 1 phenotype. Nature 2003, 421, 388. [Google Scholar] [CrossRef]
- Katayama, Y.; Hirano, A.; Wong, T.C. Human Receptor for Measles Virus (CD46) Enhances Nitric Oxide Production and Restricts Virus Replication in Mouse Macrophages by Modulating Production of Alpha/Beta Interferon. J. Virol. 2000, 74, 1252–1257. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Casasnovas, J.M.; Larvie, M.; Stehle, T. Crystal structure of two CD46 domains reveals an extended measles virus-binding surface. EMBO J. 1999, 18, 2911–2922. [Google Scholar] [CrossRef] [PubMed]
- Christiansen, D.; Deleage, G.; Gerlier, D. Evidence for distinct complement regulatory and measles virus binding sites on CD46 SCR2. Eur. J. Immunol. 2000, 30, 3457–3462. [Google Scholar] [CrossRef]
- Hsu, E.C.; Dörig, R.E.; Sarangi, F.; Marcil, A.; Iorio, C.; Richardson, C.D. Artificial mutations and natural variations in the CD46 molecules from human and monkey cells define regions important for measles virus binding. J. Virol. 1997, 71, 6144–6154. [Google Scholar] [PubMed]
- Hsu, E.C.; Sabatinos, S.; Hoedemaeker, F.J.; Rose, D.R.; Richardson, C.D. Use of site-specific mutagenesis and monoclonal antibodies to map regions of CD46 that interact with measles virus H protein. Virology 1999, 258, 314–326. [Google Scholar] [CrossRef] [PubMed]
- Manoharan, S.; Jayakumar, R.; Govindarajan, R.; Koteeswaran, A. Haemagglutination as a confirmatory test for Peste des petits ruminants diagnosis. Small Rumin. Res. 2005, 59, 75–78. [Google Scholar] [CrossRef]
- Sato, Y.; Watanabe, S.; Fukuda, Y.; Hashiguchi, T.; Yanagi, Y.; Ohno, S. Cell-to-Cell Measles Virus Spread between Human Neurons Is Dependent on Hemagglutinin and Hyperfusogenic Fusion Protein. J. Virol. 2018, 92. [Google Scholar] [CrossRef]
- Toplu, N.; Oguzoglu, T.C.; Albayrak, H. Dual infection of fetal and neonatal small ruminants with border disease virus and peste des petits ruminants virus (PPRV): Neuronal tropism of PPRV as a novel finding. J. Comp. Pathol. 2012, 146, 289–297. [Google Scholar] [CrossRef]
- De Witte, L.; de Vries, R.D.; van der Vlist, M.; Yuksel, S.; Litjens, M.; de Swart, R.L.; Geijtenbeek, T.B. DC-SIGN and CD150 have distinct roles in transmission of measles virus from dendritic cells to T-lymphocytes. PLoS Pathog. 2008, 4, e1000049. [Google Scholar] [CrossRef] [PubMed]
- Fujita, K.; Miura, R.; Yoneda, M.; Shimizu, F.; Sato, H.; Muto, Y.; Endo, Y.; Tsukiyama-Kohara, K.; Kai, C. Host range and receptor utilization of canine distemper virus analyzed by recombinant viruses: Involvement of heparin-like molecule in CDV infection. Virology 2007, 359, 324–335. [Google Scholar] [CrossRef]
- Terao-Muto, Y.; Yoneda, M.; Seki, T.; Watanabe, A.; Tsukiyama-Kohara, K.; Fujita, K.; Kai, C. Heparin-like glycosaminoglycans prevent the infection of measles virus in SLAM-negative cell lines. Antivir. Res. 2008, 80, 370–376. [Google Scholar] [CrossRef] [PubMed]
- Baron, M.D. Wild-type Rinderpest virus uses SLAM (CD150) as its receptor. J. Gen. Virol. 2005, 86, 1753–1757. [Google Scholar] [CrossRef] [PubMed]
- Melia, M.M.; Earle, J.P.; Abdullah, H.; Reaney, K.; Tangy, F.; Cosby, S.L. Use of SLAM and PVRL4 and identification of pro-HB-EGF as cell entry receptors for wild type phocine distemper virus. PLoS ONE 2014, 9, e106281. [Google Scholar] [CrossRef] [PubMed]
- Vongpunsawad, S.; Oezgun, N.; Braun, W.; Cattaneo, R. Selectively receptor-blind measles viruses: Identification of residues necessary for SLAM- or CD46-induced fusion and their localization on a new hemagglutinin structural model. J. Virol. 2004, 78, 302–313. [Google Scholar] [CrossRef] [PubMed]
- Hashiguchi, T.; Kajikawa, M.; Maita, N.; Takeda, M.; Kuroki, K.; Sasaki, K.; Kohda, D.; Yanagi, Y.; Maenaka, K. Crystal structure of measles virus hemagglutinin provides insight into effective vaccines. Proc. Natl. Acad. Sci. USA 2007, 104, 19535–19540. [Google Scholar] [CrossRef] [PubMed]
- Munir, M.; Zohari, S.; Berg, M. Molecular Biology and Pathogenesis of Peste des Petits Ruminants Virus. In Springer Briefs in Animal Sciences; Springer: Berlin/Heidelberg, Germany, 2013. [Google Scholar] [CrossRef]
- Santiago, C.; Celma, M.L.; Stehle, T.; Casasnovas, J.M. Structure of the measles virus hemagglutinin bound to the CD46 receptor. Nat. Struct. Mol. Biol. 2010, 17, 124–129. [Google Scholar] [CrossRef] [PubMed]
- Hashiguchi, T.; Ose, T.; Kubota, M.; Maita, N.; Kamishikiryo, J.; Maenaka, K.; Yanagi, Y. Structure of the measles virus hemagglutinin bound to its cellular receptor SLAM. Nat. Struct. Mol. Biol. 2011, 18, 135–141. [Google Scholar] [CrossRef] [PubMed]
- Liang, Z.; Yuan, R.; Chen, L.; Zhu, X.; Dou, Y. Molecular Evolution and Characterization of Hemagglutinin (H) in Peste des Petits Ruminants Virus. PLoS ONE 2016, 11, e0152587. [Google Scholar] [CrossRef] [PubMed]
- Langedijk, J.P.; Daus, F.J.; van Oirschot, J.T. Sequence and structure alignment of Paramyxoviridae attachment proteins and discovery of enzymatic activity for a morbillivirus hemagglutinin. J. Virol. 1997, 71, 6155–6167. [Google Scholar] [PubMed]
- Scheid, A.; Choppin, P.W. Identification of biological activities of paramyxovirus glycoproteins. Activation of cell fusion, hemolysis, and infectivity of proteolytic cleavage of an inactive precursor protein of Sendai virus. Virology 1974, 57, 475–490. [Google Scholar] [CrossRef]
- Morrison, T.; Ward, L.J.; Semerjian, A. Intracellular processing of the Newcastle disease virus fusion glycoprotein. J. Virol. 1985, 53, 851–857. [Google Scholar] [PubMed]
- Paal, T.; Brindley, M.A.; St Clair, C.; Prussia, A.; Gaus, D.; Krumm, S.A.; Snyder, J.P.; Plemper, R.K. Probing the spatial organization of measles virus fusion complexes. J. Virol. 2009, 83, 10480–10493. [Google Scholar] [CrossRef] [PubMed]
- Rahaman, A.; Srinivasan, N.; Shamala, N.; Shaila, M.S. The fusion core complex of the peste des petits ruminants virus is a six-helix bundle assembly. Biochemistry 2003, 42, 922–931. [Google Scholar] [CrossRef] [PubMed]
- Yin, H.S.; Wen, X.; Paterson, R.G.; Lamb, R.A.; Jardetzky, T.S. Structure of the parainfluenza virus 5 F protein in its metastable, prefusion conformation. Nature 2006, 439, 38–44. [Google Scholar] [CrossRef] [PubMed]
- Muhlebach, M.D.; Leonard, V.H.; Cattaneo, R. The measles virus fusion protein transmembrane region modulates availability of an active glycoprotein complex and fusion efficiency. J. Virol. 2008, 82, 11437–11445. [Google Scholar] [CrossRef] [PubMed]
- Lee, J.K.; Prussia, A.; Snyder, J.P.; Plemper, R.K. Reversible inhibition of the fusion activity of measles virus F protein by an engineered intersubunit disulfide bridge. J. Virol. 2007, 81, 8821–8826. [Google Scholar] [CrossRef] [PubMed]
- Seth, S.; Shaila, M.S. The fusion protein of Peste des petits ruminants virus mediates biological fusion in the absence of hemagglutinin-neuraminidase protein. Virology 2001, 289, 86–94. [Google Scholar] [CrossRef]
- Plemper, R.K.; Brindley, M.A.; Iorio, R.M. Structural and mechanistic studies of measles virus illuminate paramyxovirus entry. PLoS Pathog. 2011, 7, e1002058. [Google Scholar] [CrossRef]
- Schneider-Schaulies, S.; ter Meulen, V. Measles virus and immunomodulation: Molecular bases and perspectives. Expert Rev. Mol. Med. 2002, 4, 1–18. [Google Scholar] [CrossRef]
- Yanagi, Y.; Takeda, M.; Ohno, S. Measles virus: Cellular receptors, tropism and pathogenesis. J. Gen. Virol. 2006, 87, 2767–2779. [Google Scholar] [CrossRef]
- Meng, X.; Deng, R.; Zhu, X.; Zhang, Z. Quantitative investigation of the direct interaction between Hemagglutinin and fusion proteins of Peste des petits ruminant virus using surface Plasmon resonance. Virol. J. 2018, 15, 21. [Google Scholar] [CrossRef] [PubMed]
- Xu, F.; Tanaka, S.; Watanabe, H.; Shimane, Y.; Iwasawa, M.; Ohishi, K.; Maruyama, T. Computational Analysis of the Interaction Energies between Amino Acid Residues of the Measles Virus Hemagglutinin and Its Receptors. Viruses 2018, 10, 236. [Google Scholar] [CrossRef] [PubMed]
- Wohlsein, P.; Singh, R.P. Peste des petits ruminants in unusual hosts: Epidemiology, disease, and impact on eradication. In Peste Des Petits Ruminants Virus; Munir, M., Ed.; Springer: Berlin, Germany, 2015; pp. 95–118. [Google Scholar]
- Beineke, A.; Baumgartner, W.; Wohlsein, P. Cross-species transmission of canine distemper virus-an update. One Health 2015, 1, 49–59. [Google Scholar] [CrossRef] [PubMed]
- Sakai, K.; Yoshikawa, T.; Seki, F.; Fukushi, S.; Tahara, M.; Nagata, N.; Ami, Y.; Mizutani, T.; Kurane, I.; Yamaguchi, R.; et al. Canine distemper virus associated with a lethal outbreak in monkeys can readily adapt to use human receptors. J. Virol. 2013, 87, 7170–7175. [Google Scholar] [CrossRef] [PubMed]
- Sakai, K.; Nagata, N.; Ami, Y.; Seki, F.; Suzaki, Y.; Iwata-Yoshikawa, N.; Suzuki, T.; Fukushi, S.; Mizutani, T.; Yoshikawa, T.; et al. Lethal canine distemper virus outbreak in cynomolgus monkeys in Japan in 2008. J. Virol. 2013, 87, 1105–1114. [Google Scholar] [CrossRef] [PubMed]
- Auwaerter, P.G.; Rota, P.A.; Elkins, W.R.; Adams, R.J.; DeLozier, T.; Shi, Y.; Bellini, W.J.; Murphy, B.R.; Griffin, D.E. Measles virus infection in rhesus macaques: Altered immune responses and comparison of the virulence of six different virus strains. J. Infect. Dis. 1999, 180, 950–958. [Google Scholar] [CrossRef] [PubMed]
- Bankamp, B.; Hodge, G.; McChesney, M.B.; Bellini, W.J.; Rota, P.A. Genetic changes that affect the virulence of measles virus in a rhesus macaque model. Virology 2008, 373, 39–50. [Google Scholar] [CrossRef] [PubMed]
- De Swart, R.L. Measles studies in the macaque model. Curr. Top. Microbiol. Immunol. 2009, 330, 55–72. [Google Scholar] [PubMed]
- Kobune, F.; Takahashi, H.; Terao, K.; Ohkawa, T.; Ami, Y.; Suzaki, Y.; Nagata, N.; Sakata, H.; Yamanouchi, K.; Kai, C. Nonhuman primate models of measles. Lab. Anim. Sci. 1996, 46, 315–320. [Google Scholar]
- McChesney, M.B.; Fujinami, R.S.; Lerche, N.W.; Marx, P.A.; Oldstone, M.B. Virus-induced immunosuppression: Infection of peripheral blood mononuclear cells and suppression of immunoglobulin synthesis during natural measles virus infection of rhesus monkeys. J. Infect. Dis. 1989, 159, 757–760. [Google Scholar] [CrossRef]
- McChesney, M.B.; Miller, C.J.; Rota, P.A.; Zhu, Y.D.; Antipa, L.; Lerche, N.W.; Ahmed, R.; Bellini, W.J. Experimental measles. I. Pathogenesis in the normal and the immunized host. Virology 1997, 233, 74–84. [Google Scholar] [CrossRef] [PubMed]
- Janeway, C.A., Jr.; Medzhitov, R. Innate immune recognition. Annu. Rev. Immunol. 2002, 20, 197–216. [Google Scholar] [CrossRef] [PubMed]
- West, N.P.; Pyne, D.B.; Renshaw, G.; Cripps, A.W. Antimicrobial peptides and proteins, exercise and innate mucosal immunity. Fems Immunol. Med. Microbiol. 2006, 48, 293–304. [Google Scholar] [CrossRef] [PubMed]
- OIE. Peste Des Petits Ruminants. Available online: http://www.oie.int/en/animal-health-in-the-world/official-disease-status/peste-des-petits-ruminants/ (accessed on 23 July 2018).
- Randall, R.E.; Goodbourn, S. Interferons and viruses: An interplay between induction, signalling, antiviral responses and virus countermeasures. J. Gen. Virol. 2008, 89, 1–47. [Google Scholar] [CrossRef] [PubMed]
- Platanias, L.C. Mechanisms of type-I- and type-II-interferon-mediated signalling. Nat. Rev. Immunol. 2005, 5, 375–386. [Google Scholar] [CrossRef] [PubMed]
- Van Riel, D.; Leijten, L.M.; van der Eerden, M.; Hoogsteden, H.C.; Boven, L.A.; Lambrecht, B.N.; Osterhaus, A.D.; Kuiken, T. Highly pathogenic avian influenza virus H5N1 infects alveolar macrophages without virus production or excessive TNF-alpha induction. PLoS Pathog. 2011, 7, e1002099. [Google Scholar] [CrossRef] [PubMed]
- Bieback, K.; Lien, E.; Klagge, I.M.; Avota, E.; Schneider-Schaulies, J.; Duprex, W.P.; Wagner, H.; Kirschning, C.J.; Ter Meulen, V.; Schneider-Schaulies, S. Hemagglutinin protein of wild-type measles virus activates toll-like receptor 2 signaling. J. Virol. 2002, 76, 8729–8736. [Google Scholar] [CrossRef] [PubMed]
- Atmaca, H.T.; Kul, O. Examination of epithelial tissue cytokine response to natural peste des petits ruminants virus (PPRV) infection in sheep and goats by immunohistochemistry. Histol. Histopathol. 2012, 27, 69–78. [Google Scholar] [CrossRef]
- Baron, J.; Bin-Tarif, A.; Herbert, R.; Frost, L.; Taylor, G.; Baron, M.D. Early changes in cytokine expression in peste des petits ruminants disease. Vet. Res. 2014, 45, 22. [Google Scholar] [CrossRef] [PubMed]
- Koyama, S.; Ishii, K.J.; Coban, C.; Akira, S. Innate immune response to viral infection. Cytokine 2008, 43, 336–341. [Google Scholar] [CrossRef] [PubMed]
- Yang, B.; Qi, X.; Chen, Z.; Chen, S.; Xue, Q.; Jia, P.; Wang, T.; Wang, J. Binding and entry of peste des petits ruminants virus into caprine endometrial epithelial cells profoundly affect early cellular gene expression. Vet. Res. 2018, 49, 8. [Google Scholar] [CrossRef] [PubMed]
- Andrejeva, J.; Childs, K.S.; Young, D.F.; Carlos, T.S.; Stock, N.; Goodbourn, S.; Randall, R.E. The V proteins of paramyxoviruses bind the IFN-inducible RNA helicase, mda-5, and inhibit its activation of the IFN-beta promoter. Proc. Natl. Acad. Sci. USA 2004, 101, 17264–17269. [Google Scholar] [CrossRef] [PubMed]
- Childs, K.; Stock, N.; Ross, C.; Andrejeva, J.; Hilton, L.; Skinner, M.; Randall, R.; Goodbourn, S. mda-5, but not RIG-I, is a common target for paramyxovirus V proteins. Virology 2007, 359, 190–200. [Google Scholar] [CrossRef] [PubMed]
- Caignard, G.; Guerbois, M.; Labernardiere, J.L.; Jacob, Y.; Jones, L.M.; Wild, F.; Tangy, F.; Vidalain, P.O. Measles virus V protein blocks Jak1-mediated phosphorylation of STAT1 to escape IFN-alpha/beta signaling. Virology 2007, 368, 351–362. [Google Scholar] [CrossRef] [PubMed]
- Devaux, P.; von Messling, V.; Songsungthong, W.; Springfeld, C.; Cattaneo, R. Tyrosine 110 in the measles virus phosphoprotein is required to block STAT1 phosphorylation. Virology 2007, 360, 72–83. [Google Scholar] [CrossRef] [PubMed]
- Ma, X.; Yang, X.; Nian, X.; Zhang, Z.; Dou, Y.; Zhang, X.; Luo, X.; Su, J.; Zhu, Q.; Cai, X. Identification of amino-acid residues in the V protein of peste des petits ruminants essential for interference and suppression of STAT-mediated interferon signaling. Virology 2015, 483, 54–63. [Google Scholar] [CrossRef] [PubMed]
- Chinnakannan, S.K.; Nanda, S.K.; Baron, M.D. Morbillivirus v proteins exhibit multiple mechanisms to block type 1 and type 2 interferon signalling pathways. PLoS ONE 2013, 8, e57063. [Google Scholar] [CrossRef] [PubMed]
- Abbas, A.K.; Lichtman, A.H. Cellular and Molecular Immunology, 5th ed.; Saunders: Philadelphia, PA, USA, 2003; p. 562. [Google Scholar]
- Naik, S.; Renukaradhya, G.J.; Rajasekhar, M.; Shaila, M.S. Immunogenic and protective properties of haemagglutinin protein (H) of rinderpest virus expressed by a recombinant baculovirus. Vaccine 1997, 15, 603–607. [Google Scholar] [CrossRef]
- Naik, S.; Shaila, M. Characterization of Membrane-bound and Membrane Anchor-less Forms of Hemagglutinin Glycoprotein of Rinderpest Virus Expressed by Baculovirus Recombinants. Virus Genes 1997, 14, 95–104. [Google Scholar] [CrossRef] [PubMed]
- Sinnathamby, G.; Nayak, R.; Shaila, M.S. Mapping of T-helper epitopes of Rinderpest virus hemagglutinin protein. Viral Immunol. 2001, 14, 83–92. [Google Scholar] [CrossRef] [PubMed]
- Diallo, A.; Minet, C.; Le Goff, C.; Berhe, G.; Albina, E.; Libeau, G.; Barrett, T. The threat of peste des petits ruminants: Progress in vaccine development for disease control. Vaccine 2007, 25, 5591–5597. [Google Scholar] [CrossRef] [PubMed]
- Rojas, J.M.; Rodriguez-Martin, D.; Avia, M.; Martin, V.; Sevilla, N. Peste des Petits Ruminants Virus Fusion and Hemagglutinin Proteins Trigger Antibody-Dependent Cell-Mediated Cytotoxicity in Infected Cells. Front. Immunol. 2018, 9, 3172. [Google Scholar] [CrossRef] [PubMed]
- Mitra-Kaushik, S.; Nayak, R.; Shaila, M.S. Identification of a cytotoxic T-cell epitope on the recombinant nucleocapsid proteins of Rinderpest and Peste des petits ruminants viruses presented as assembled nucleocapsids. Virology 2001, 279, 210–220. [Google Scholar] [CrossRef] [PubMed]
- Jones, L.; Giavedoni, L.; Saliki, J.T.; Brown, C.; Mebus, C.; Yilma, T. Protection of goats against peste des petits ruminants with a vaccinia virus double recombinant expressing the F and H genes of rinderpest virus. Vaccine 1993, 11, 961–964. [Google Scholar] [CrossRef]
- Romero, C.H.; Barrett, T.; Chamberlain, R.W.; Kitching, R.P.; Fleming, M.; Black, D.N. Recombinant Capripoxvirus Expressing the Hemagglutinin Protein Gene of Rinderpest Virus: Protection of Cattle against Rinderpest and Lumpy Skin Disease Viruses. Virology 1994, 204, 425–429. [Google Scholar] [CrossRef] [PubMed]
- Hu, Q.; Chen, W.; Huang, K.; Baron, M.D.; Bu, Z. Rescue of recombinant peste des petits ruminants virus: Creation of a GFP-expressing virus and application in rapid virus neutralization test. Vet. Res. 2012, 43, 48. [Google Scholar] [CrossRef] [PubMed]
- Muniraju, M.; Mahapatra, M.; Buczkowski, H.; Batten, C.; Banyard, A.C.; Parida, S. Rescue of a vaccine strain of peste des petits ruminants virus: In vivo evaluation and comparison with standard vaccine. Vaccine 2015, 33, 465–471. [Google Scholar] [CrossRef] [PubMed]
- Niyokwishimira, A.; Dou, Y.; Qian, B.; Meera, P.; Zhang, Z. Reverse Genetics for Peste des Petits Ruminants Virus: Current Status and Lessons to Learn from Other Non-segmented Negative-Sense RNA Viruses. Virol. Sin. 2018, 33, 472–483. [Google Scholar] [CrossRef] [PubMed]
- Choi, K.-S.; Nah, J.-J.; Ko, Y.-J.; Kang, S.-Y.; Joo, Y. Localization of antigenic sites at the amino-terminus of rinderpest virus N protein using deleted N mutants and monoclonal antibody. J. Vet. Sci. 2003, 4, 167–173. [Google Scholar] [CrossRef]
- Renukaradhya, G.J.; Sinnathamby, G.; Seth, S.; Rajasekhar, M.; Shaila, M.S. Mapping of B-cell epitopic sites and delineation of functional domains on the hemagglutinin-neuraminidase protein of peste des petits ruminants virus. Virus Res. 2002, 90. [Google Scholar] [CrossRef]
- Beckford, A.P.; Kaschula, R.O.; Stephen, C. Factors associated with fatal cases of measles. A retrospective autopsy study. South Afr. Med. J. Suid. Afrik. Tydskr. Vir Geneeskd. 1985, 68, 858–863. [Google Scholar]
- Griffin, D.E. Measles virus-induced suppression of immune responses. Immunol. Rev. 2010, 236, 176–189. [Google Scholar] [CrossRef] [PubMed]
- Schneider-Schaulies, S.; Niewiesk, S.; Schneider-Schaulies, J.; ter Meulen, V. Measles virus induced immunosuppression: Targets and effector mechanisms. Curr. Mol. Med. 2001, 1, 163–181. [Google Scholar] [CrossRef] [PubMed]
- Schlender, J.; Schnorr, J.J.; Spielhoffer, P.; Cathomen, T.; Cattaneo, R.; Billeter, M.A.; ter Meulen, V.; Schneider-Schaulies, S. Interaction of measles virus glycoproteins with the surface of uninfected peripheral blood lymphocytes induces immunosuppression in vitro. Proc. Natl. Acad. Sci. USA 1996, 93, 13194–13199. [Google Scholar] [CrossRef] [PubMed]
- Heaney, J.; Barrett, T.; Cosby, S.L. Inhibition of in vitro leukocyte proliferation by morbilliviruses. J. Virol. 2002, 76, 3579–3584. [Google Scholar] [CrossRef]
- Yoneda, M.; Miura, R.; Barrett, T.; Tsukiyama-Kohara, K.; Kai, C. Rinderpest virus phosphoprotein gene is a major determinant of species-specific pathogenicity. J. Virol. 2004, 78, 6676–6681. [Google Scholar] [CrossRef] [PubMed]
- Yoneda, M.; Bandyopadhyay, S.K.; Shiotani, M.; Fujita, K.; Nuntaprasert, A.; Miura, R.; Baron, M.D.; Barrett, T.; Kai, C. Rinderpest virus H protein: Role in determining host range in rabbits. J. Gen. Virol. 2002, 83, 1457–1463. [Google Scholar] [CrossRef]
- Yokota, S.; Saito, H.; Kubota, T.; Yokosawa, N.; Amano, K.; Fujii, N. Measles virus suppresses interferon-alpha signaling pathway: Suppression of Jak1 phosphorylation and association of viral accessory proteins, C and V, with interferon-alpha receptor complex. Virology 2003, 306, 135–146. [Google Scholar] [CrossRef]
- Ravanel, K.; Castelle, C.; Defrance, T.; Wild, T.F.; Charron, D.; Lotteau, V.; Rabourdin-Combe, C. Measles virus nucleocapsid protein binds to FcgammaRII and inhibits human B cell antibody production. J. Exp. Med. 1997, 186, 269–278. [Google Scholar] [CrossRef]
- Avota, E.; Gassert, E.; Schneider-Schaulies, S. Measles virus-induced immunosuppression: From effectors to mechanisms. Med. Microbiol. Immunol. 2010, 199, 227–237. [Google Scholar] [CrossRef]
- Niewiesk, S.; Schneider-Schaulies, J.; Ohnimus, H.; Jassoy, C.; Schneider-Schaulies, S.; Diamond, L.; Logan, J.S.; ter Meulen, V. CD46 expression does not overcome the intracellular block of measles virus replication in transgenic rats. J. Virol. 1997, 71, 7969–7973. [Google Scholar] [PubMed]
- Nizamani, Z.; Servan de Almeida, R.; Albina, E.; Parveen, F.; Libeau, G. In vitro study of lymphotropic and immunomodulatory properties of the peste des petits ruminants virus (PPRV). J. Anim. Plant Sci. 2014, 24, 1380–1387. [Google Scholar]
- De Swart, R.L.; Ludlow, M.; de Witte, L.; Yanagi, Y.; van Amerongen, G.; McQuaid, S.; Yuksel, S.; Geijtenbeek, T.B.; Duprex, W.P.; Osterhaus, A.D. Predominant infection of CD150+ lymphocytes and dendritic cells during measles virus infection of macaques. PLoS Pathog. 2007, 3, e178. [Google Scholar] [CrossRef] [PubMed]
- Welstead, G.G.; Hsu, E.C.; Iorio, C.; Bolotin, S.; Richardson, C.D. Mechanism of CD150 (SLAM) down regulation from the host cell surface by measles virus hemagglutinin protein. J. Virol. 2004, 78, 9666–9674. [Google Scholar] [CrossRef] [PubMed]
- Erlenhoefer, C.; Wurzer, W.J.; Loffler, S.; Schneider-Schaulies, S.; ter Meulen, V.; Schneider-Schaulies, J. CD150 (SLAM) is a receptor for measles virus but is not involved in viral contact-mediated proliferation inhibition. J. Virol. 2001, 75, 4499–4505. [Google Scholar] [CrossRef] [PubMed]
- Romanets-Korbut, O.; Kovalevska, L.M.; Seya, T.; Sidorenko, S.P.; Horvat, B. Measles virus hemagglutinin triggers intracellular signaling in CD150-expressing dendritic cells and inhibits immune response. Cell. Mol. Immunol. 2016, 13, 828–838. [Google Scholar] [CrossRef] [PubMed]
- Sanz Bernardo, B.; Goodbourn, S.; Baron, M.D. Control of the induction of type I interferon by Peste des petits ruminants virus. PLoS ONE 2017, 12, e0177300. [Google Scholar] [CrossRef]
- Hahm, B.; Cho, J.H.; Oldstone, M.B. Measles virus-dendritic cell interaction via SLAM inhibits innate immunity: Selective signaling through TLR4 but not other TLRs mediates suppression of IL-12 synthesis. Virology 2007, 358, 251–257. [Google Scholar] [CrossRef]
- Caignard, G.; Bourai, M.; Jacob, Y.; Tangy, F.; Vidalain, P.O. Inhibition of IFN-alpha/beta signaling by two discrete peptides within measles virus V protein that specifically bind STAT1 and STAT2. Virology 2009, 383, 112–120. [Google Scholar] [CrossRef]
- Boxer, E.L.; Nanda, S.K.; Baron, M.D. The rinderpest virus non-structural C protein blocks the induction of type 1 interferon. Virology 2009, 385, 134–142. [Google Scholar] [CrossRef]
© 2019 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Prajapati, M.; Alfred, N.; Dou, Y.; Yin, X.; Prajapati, R.; Li, Y.; Zhang, Z. Host Cellular Receptors for the Peste des Petits Ruminant Virus. Viruses 2019, 11, 729. https://doi.org/10.3390/v11080729
Prajapati M, Alfred N, Dou Y, Yin X, Prajapati R, Li Y, Zhang Z. Host Cellular Receptors for the Peste des Petits Ruminant Virus. Viruses. 2019; 11(8):729. https://doi.org/10.3390/v11080729
Chicago/Turabian StylePrajapati, Meera, Niyokwishimira Alfred, Yongxi Dou, Xiangping Yin, Raju Prajapati, Yanmin Li, and Zhidong Zhang. 2019. "Host Cellular Receptors for the Peste des Petits Ruminant Virus" Viruses 11, no. 8: 729. https://doi.org/10.3390/v11080729
APA StylePrajapati, M., Alfred, N., Dou, Y., Yin, X., Prajapati, R., Li, Y., & Zhang, Z. (2019). Host Cellular Receptors for the Peste des Petits Ruminant Virus. Viruses, 11(8), 729. https://doi.org/10.3390/v11080729





