Development of American-Lineage Influenza H5N2 Reassortant Vaccine Viruses for Pandemic Preparedness
Abstract
1. Introduction
2. Materials and Methods
2.1. Cells, Viruses, and Medium
2.2. Clone
2.3. Generatation of H5N2 Vaccine Viruses Using Reverse Genetics
2.4. Sequencing
2.5. Antigenicity Analysis
2.6. Trypsin Dependency Test
2.7. Intravenous Pathogenicity Index (IVPI)
2.8. Pathogenicity Tests and Immunization in Ferrets
2.9. Preparation of Standard Antigen and Antiserum
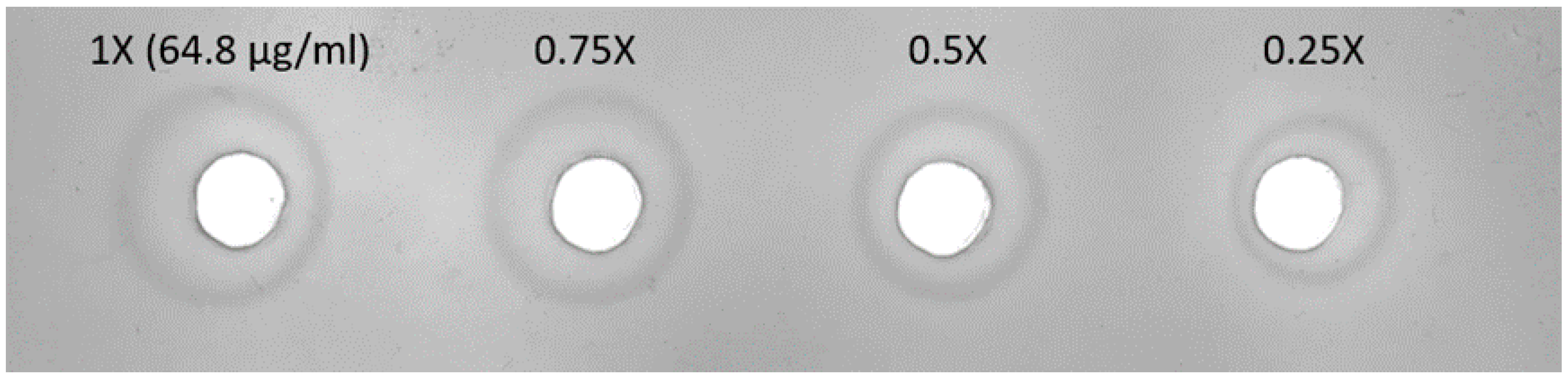
2.10. Radial Immunodiffusion (SRID) Assay
2.11. Ethics Statement
3. Results
3.1. Generation of Influenza Reassortant H5N2 Vaccine Viruses
3.2. Qualification of Candidate Vaccine Viruses
3.3. Genetic Stability and Trypsin Dependency of H5N2 Vaccine Viruses
3.4. Intravenous Pathogenicity Index (IVPI) of H5N2 Vaccine Viruses
3.5. Pathogenicity in Ferrets
3.6. Preparation of Standard Antigen and Antiserum
3.7. Ferret Immunization
4. Discussion
Supplementary Materials
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- Schrauwen, E.J.; Fouchier, R.A. Host adaptation and transmission of influenza A viruses in mammals. Emerg. Microbes Infect. 2014, 3, e9. [Google Scholar] [CrossRef] [PubMed]
- Neumann, G.; Kawaoka, Y. Transmission of influenza A viruses. Virology 2015, 479–480, 234–246. [Google Scholar] [CrossRef] [PubMed]
- Cheng, M.C.; Soda, K.; Lee, M.S.; Lee, S.H.; Sakoda, Y.; Kida, H.; Wang, C.H. Isolation and characterization of potentially pathogenic H5N2 influenza virus from a chicken in Taiwan in 2008. Avian Dis. 2010, 54, 885–893. [Google Scholar] [CrossRef] [PubMed]
- Lee, C.C.; Zhu, H.; Huang, P.Y.; Peng, L.; Chang, Y.C.; Yip, C.H.; Li, Y.T.; Cheung, C.L.; Compans, R.; Yang, C.; et al. Emergence and evolution of avian H5N2 influenza viruses in chickens in Taiwan. J. Virol. 2014, 88, 5677–5686. [Google Scholar] [CrossRef] [PubMed]
- Wu, H.S.; Yang, J.R.; Liu, M.T.; Yang, C.H.; Cheng, M.C.; Chang, F.Y. Influenza A(H5N2) virus antibodies in humans after contact with infected poultry, Taiwan, 2012. Emerg. Infect. Dis. 2014, 20, 857–860. [Google Scholar] [CrossRef] [PubMed]
- Lin, C.Y.; Chia, M.Y.; Chen, P.L.; Yeh, C.T.; Cheng, M.C.; Su, I.J.; Lee, M.S. Assessment of pathogenicity and antigenicity of American lineage influenza H5N2 viruses in Taiwan. Virology 2017, 508, 159–163. [Google Scholar] [CrossRef] [PubMed]
- Harding, A.T.; Heaton, N.S. Efforts to Improve the Seasonal Influenza Vaccine. Vaccines 2018, 6, 19. [Google Scholar] [CrossRef] [PubMed]
- Hegde, N.R. Cell culture-based influenza vaccines: A necessary and indispensable investment for the future. Hum. Vaccines Immunother. 2015, 11, 1223–1234. [Google Scholar] [CrossRef] [PubMed]
- Manini, I.; Trombetta, C.M.; Lazzeri, G.; Pozzi, T.; Rossi, S.; Montomoli, E. Egg-Independent Influenza Vaccines and Vaccine Candidates. Vaccines 2017, 5, 18. [Google Scholar] [CrossRef] [PubMed]
- Perez Rubio, A.; Eiros, J.M. Cell culture-derived flu vaccine: Present and future. Hum. Vaccines Immunother. 2018, 14, 1874–1882. [Google Scholar] [CrossRef] [PubMed]
- Choi, W.S.; Noh, J.Y.; Song, J.Y.; Cheong, H.J.; Wie, S.H.; Lee, J.S.; Lee, J.; Kim, S.W.; Jeong, H.W.; Jung, S.I.; et al. Immunogenicity and safety of a cell culture-derived inactivated quadrivalent influenza vaccine (NBP607-QIV): A randomized, double-blind, multi-center, phase III clinical trial in adults and elderly subjects. Hum. Vaccines Immunother. 2017, 13, 1653–1660. [Google Scholar] [CrossRef] [PubMed]
- Oh, C.E.; Choi, U.Y.; Eun, B.W.; Lee, T.J.; Kim, K.H.; Kim, D.H.; Kim, N.H.; Jo, D.S.; Shin, S.H.; Kim, K.H.; et al. A Randomized, Double-blind, Active-controlled Clinical Trial of a Cell Culture-derived Inactivated Trivalent Influenza Vaccine (NBP607) in Healthy Children 6 Months Through 18 Years of Age. Pediatr. Infect. Dis. J. 2018, 37, 605–611. [Google Scholar] [CrossRef] [PubMed]
- Lee, M.S.; Hu, A.Y. A cell-based backup to speed up pandemic influenza vaccine production. Trends Microbiol. 2012, 20, 103–105. [Google Scholar] [CrossRef] [PubMed]
- Barrett, P.N.; Terpening, S.J.; Snow, D.; Cobb, R.R.; Kistner, O. Vero cell technology for rapid development of inactivated whole virus vaccines for emerging viral diseases. Expert Rev. Vaccines 2017, 16, 883–894. [Google Scholar] [CrossRef] [PubMed]
- Tseng, Y.F.; Hu, A.Y.; Huang, M.L.; Yeh, W.Z.; Weng, T.C.; Chen, Y.S.; Chong, P.; Lee, M.S. Adaptation of high-growth influenza H5N1 vaccine virus in Vero cells: implications for pandemic preparedness. PLoS ONE 2011, 6, e24057. [Google Scholar] [CrossRef] [PubMed]
- Hoffmann, E.; Stech, J.; Guan, Y.; Webster, R.G.; Perez, D.R. Universal primer set for the full-length amplification of all influenza A viruses. Arch. Virol. 2001, 146, 2275–2289. [Google Scholar] [CrossRef] [PubMed]
- Hoffmann, E.; Neumann, G.; Kawaoka, Y.; Hobom, G.; Webster, R.G. A DNA transfection system for generation of influenza A virus from eight plasmids. Proc. Natl. Acad. Sci. USA 2000, 97, 6108–6113. [Google Scholar] [CrossRef]
- Gohrbandt, S.; Veits, J.; Hundt, J.; Bogs, J.; Breithaupt, A.; Teifke, J.P.; Weber, S.; Mettenleiter, T.C.; Stech, J. Amino acids adjacent to the haemagglutinin cleavage site are relevant for virulence of avian influenza viruses of subtype H5. J. Gen. Virol. 2011, 92, 51–59. [Google Scholar] [CrossRef]
- WHO Manual on Animal Influenza Diagnosis and Surveillance. Available online: http://www.who.int/csr/resources/publications/influenza/en/whocdscsrncs20025rev.pdf (accessed on 12 July 2002).
- Li, S.; Liu, C.; Klimov, A.; Subbarao, K.; Perdue, M.L.; Mo, D.; Ji, Y.; Woods, L.; Hietala, S.; Bryant, M. Recombinant influenza A virus vaccines for the pathogenic human A/Hong Kong/97 (H5N1) viruses. J. Infect. Dis. 1999, 179, 1132–1138. [Google Scholar] [CrossRef]
- Shankar, B.P.; Gowda, R.N.S.; Prabhu, B.H.M.; Pattnaik, B.; Nagarajan, S.; Patil, S.S.; Pradhan, H.K. Assessment of Pathogenic Potential of Two Indian H5N1 Highly Pathogenic Avian Influenza Virus Isolates by Intravenous Pathogenicity Index Test. Int. J. Poult. Sci. 2009, 8, 283–290. [Google Scholar] [CrossRef]
- Tseng, Y.F.; Weng, T.C.; Lai, C.C.; Chen, P.L.; Lee, M.S.; Hu, A.Y. A fast and efficient purification platform for cell-based influenza viruses by flow-through chromatography. Vaccine 2018, 36, 3146–3152. [Google Scholar] [CrossRef] [PubMed]
- Harvey, R.; Hamill, M.; Robertson, J.S.; Minor, P.D.; Vodeiko, G.M.; Weir, J.P.; Takahashi, H.; Harada, Y.; Itamura, S.; Bamford, P.; et al. Application of deglycosylation to SDS PAGE analysis improves calibration of influenza antigen standards. Biologicals 2012, 40, 96–99. [Google Scholar] [CrossRef] [PubMed]
- Jing, X.; Soto, J.; Gao, Y.; Phy, K.; Ye, Z. Assessment of viral replication in eggs and HA protein yield of pre-pandemic H5N1 candidate vaccine viruses. Vaccine 2013, 31, 4091–4097. [Google Scholar] [CrossRef] [PubMed]
- Page, M.; Thorpe, R. Purification of IgG Using Caprylic Acid. In The Protein Protocols Handbook, 3rd ed.; Humana Press: New York, NY, USA, 2009; pp. 1753–1754. [Google Scholar]
- Minor, P.D. Assaying the Potency of Influenza Vaccines. Vaccines 2015, 3, 90–104. [Google Scholar] [CrossRef] [PubMed]
- Making a Candidate Vaccine Virus (CVV) for a HPAI (Bird Flu) Virus. Available online: https://www.cdc.gov/flu/avianflu/candidate-vaccine-virus.htm#quality2017 (accessed on 19 May 2017).
- WHO Biosafety Risk Assessment and Guidelines for the Production and Quality Control of Human Influenza Pandemic Vaccines. Available online: https://www.who.int/biologicals/vaccines/INFLUENZA_BIOSAFETY_GL_draft_1_1st_PC_22_Nov_2017_TZ.pdf (accessed on 22 November 2017).
- Wang, W.; Lu, B.; Zhou, H.; Suguitan, A.L., Jr.; Cheng, X.; Subbarao, K.; Kemble, G.; Jin, H. Glycosylation at 158N of the hemagglutinin protein and receptor binding specificity synergistically affect the antigenicity and immunogenicity of a live attenuated H5N1 A/Vietnam/1203/2004 vaccine virus in ferrets. J. Virol. 2010, 84, 6570–6577. [Google Scholar] [CrossRef]
- Abe, Y.; Takashita, E.; Sugawara, K.; Matsuzaki, Y.; Muraki, Y.; Hongo, S. Effect of the addition of oligosaccharides on the biological activities and antigenicity of influenza A/H3N2 virus hemagglutinin. J. Virol. 2004, 78, 9605–9611. [Google Scholar] [CrossRef] [PubMed]
- Sun, X.; Jayaraman, A.; Maniprasad, P.; Raman, R.; Houser, K.V.; Pappas, C.; Zeng, H.; Sasisekharan, R.; Katz, J.M.; Tumpey, T.M. N-linked glycosylation of the hemagglutinin protein influences virulence and antigenicity of the 1918 pandemic and seasonal H1N1 influenza A viruses. J. Virol. 2013, 87, 8756–8766. [Google Scholar] [CrossRef]
- Barman, S.; Adhikary, L.; Chakrabarti, A.K.; Bernas, C.; Kawaoka, Y.; Nayak, D.P. Role of Transmembrane Domain and Cytoplasmic Tail Amino Acid Sequences of Influenza A Virus Neuraminidase in Raft Association and Virus Budding. J. Virol. 2004, 78, 5258–5269. [Google Scholar] [CrossRef]
- Ohkura, T.; Momose, F.; Ichikawa, R.; Takeuchi, K.; Morikawa, Y. Influenza A virus hemagglutinin and neuraminidase mutually accelerate their apical targeting through clustering of lipid rafts. J. Virol. 2014, 88, 10039–10055. [Google Scholar] [CrossRef]
- Zhang, J.; Leser, G.P.; Pekosz, A.; Lamb, R.A. The cytoplasmic tails of the influenza virus spike glycoproteins are required for normal genome packaging. Virology 2000, 269, 325–334. [Google Scholar] [CrossRef]
- Zhang, J.; Pekosz, A.; Lamb, R.A. Influenza virus assembly and lipid raft microdomains: a role for the cytoplasmic tails of the spike glycoproteins. J. Virol. 2000, 74, 4634–4644. [Google Scholar] [CrossRef] [PubMed]
- Nayak, D.P.; Balogun, R.A.; Yamada, H.; Zhou, Z.H.; Barman, S. Influenza virus morphogenesis and budding. Virus Res. 2009, 143, 147–161. [Google Scholar] [CrossRef] [PubMed]
- Engelhardt, O.G.; Edge, C.; Dunleavy, U.; Guilfoyle, K.; Harvey, R.; Major, D.; Newman, R.; Penn, R.; Skeldon, S.; Storey, C.; et al. Comparison of single radial immunodiffusion, SDS-PAGE and HPLC potency assays for inactivated influenza vaccines shows differences in ability to predict immunogenicity of haemagglutinin antigen. Vaccine 2018, 36, 4339–4345. [Google Scholar] [CrossRef] [PubMed]
- Generic Protocol for the Calibration of Seasonal/Pandemic Influenza Antigen Working Reagents by WHO Essential Regulatory Laboratories. Available online: http://www.who.int/biologicals/vaccines/INFLUENZA_Calibration_protocol_DB_CA_DB23_April.pdf (accessed on 23 April 2012).
- Baras, B.; Stittelaar, K.J.; Simon, J.H.; Thoolen, R.J.; Mossman, S.P.; Pistoor, F.H.; van Amerongen, G.; Wettendorff, M.A.; Hanon, E.; Osterhaus, A.D. Cross-protection against lethal H5N1 challenge in ferrets with an adjuvanted pandemic influenza vaccine. PLoS ONE 2008, 3, e1401. [Google Scholar] [CrossRef] [PubMed]
- Baras, B.; Stittelaar, K.J.; Kuiken, T.; Jacob, V.; Bernhard, R.; Giannini, S.; de Waal, L.; van Amerongen, G.; Simon, J.H.; Osterhaus, A.D.; et al. Longevity of the protective immune response induced after vaccination with one or two doses of AS03A-adjuvanted split H5N1 vaccine in ferrets. Vaccine 2011, 29, 2092–2099. [Google Scholar] [CrossRef] [PubMed]
- Sun, X.; Belser, J.A.; Pulit-Penaloza, J.A.; Creager, H.M.; Guo, Z.; Jefferson, S.N.; Liu, F.; York, I.A.; Stevens, J.; Maines, T.R.; et al. Stockpiled pre-pandemic H5N1 influenza virus vaccines with AS03 adjuvant provide cross-protection from H5N2 clade 2.3.4.4 virus challenge in ferrets. Virology 2017, 508, 164–169. [Google Scholar] [CrossRef] [PubMed]
- Cox, N.J.; Trock, S.C.; Burke, S.A. Pandemic preparedness and the Influenza Risk Assessment Tool (IRAT). Curr. Top. Microbiol. Immunol. 2014, 385, 119–136. [Google Scholar] [PubMed]
- Burke, S.A.; Trock, S.C. Use of Influenza Risk Assessment Tool for Prepandemic Preparedness. Emerg. Infect. Dis. 2018, 24, 471–477. [Google Scholar] [CrossRef]
| Strain ID | E7-V15 V3 | R3-V15 V3 |
|---|---|---|
| Source of HA and NA genes | A/CK/CY/A2628/2012 (E7, LPAI) | A/CK/YL/0502/2012 (R3, HPAI) |
| Modified cleavage site | GGA GAA ACA AGA (GETR) | GGA GAA ACA AGA (GETR) |
| Source of internal genes | Vero-15 | Vero-15 |
| HA titre | 4 HAU | <2 HAU |
| Virus titre | 1.78 × 106 TCID50/mL | 3.98 × 105 TCID50/mL |
| Test Items | Result |
|---|---|
| Live virus titre | 3.16 × 107 TCID50/mL (5.44 × 107 PFU/mL) |
| HA titre | 128 HAU |
| Sequence analysis 1 | HA (N155D, T231K, G323R, I381V) NA (N4K) PA (E349G) |
| Antigenic analysis | Similar to parental strain (E7) |
| Sterility test | No bacteria contamination |
| Trypsin-dependency | Trypsin dependent |
| Chicken pathogenicity | IVPI = 0 |
| Ferret pathogenicity | Low pathogenicity (weight loss <5%) |
| Genetic stability of HA cleavage site | Without mutations on the cleavage site after 10 passages |
| Vaccine Strain | E7-V15 C11+ Al(OH)3 | ||||
|---|---|---|---|---|---|
| Ferret no. | 259 (M) | 269 (M) | 265 (F) | 266 (F) | GMT (M/F) |
| YL/120502 (2012)- R3 | <10 | 10 | 320 | 80 | 7/160 |
| CY/A2628 (2012)- E7 | <10 | 10 | 160 | 80 | 7/113 |
© 2019 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Chen, P.-L.; Hu, A.Y.-C.; Lin, C.-Y.; Weng, T.-C.; Lai, C.-C.; Tseng, Y.-F.; Cheng, M.-C.; Chia, M.-Y.; Lin, W.-C.; Yeh, C.-T.; et al. Development of American-Lineage Influenza H5N2 Reassortant Vaccine Viruses for Pandemic Preparedness. Viruses 2019, 11, 543. https://doi.org/10.3390/v11060543
Chen P-L, Hu AY-C, Lin C-Y, Weng T-C, Lai C-C, Tseng Y-F, Cheng M-C, Chia M-Y, Lin W-C, Yeh C-T, et al. Development of American-Lineage Influenza H5N2 Reassortant Vaccine Viruses for Pandemic Preparedness. Viruses. 2019; 11(6):543. https://doi.org/10.3390/v11060543
Chicago/Turabian StyleChen, Po-Ling, Alan Yung-Chih Hu, Chun-Yang Lin, Tsai-Chuan Weng, Chia-Chun Lai, Yu-Fen Tseng, Ming-Chu Cheng, Min-Yuan Chia, Wen-Chin Lin, Chia-Tsui Yeh, and et al. 2019. "Development of American-Lineage Influenza H5N2 Reassortant Vaccine Viruses for Pandemic Preparedness" Viruses 11, no. 6: 543. https://doi.org/10.3390/v11060543
APA StyleChen, P.-L., Hu, A. Y.-C., Lin, C.-Y., Weng, T.-C., Lai, C.-C., Tseng, Y.-F., Cheng, M.-C., Chia, M.-Y., Lin, W.-C., Yeh, C.-T., Su, I.-J., & Lee, M.-S. (2019). Development of American-Lineage Influenza H5N2 Reassortant Vaccine Viruses for Pandemic Preparedness. Viruses, 11(6), 543. https://doi.org/10.3390/v11060543






