Development and Characterization of a Sin Nombre Virus Transmission Model in Peromyscus maniculatus
Abstract
1. Introduction
2. Materials and Methods
2.1. Ethics Statement
2.2. Animals and Infections
2.3. Viral Stock Preparation
2.4. Transmission Experiments
2.5. Blood, Swab, and Tissue Collection
2.6. Detection of Viral RNA
2.7. Determination of Seroconversion by ELISA
2.8. Induction of Heat Shock Responses
2.9. Detection of Heat Shock Protein mRNA Expression
2.10. Castration of Male Deer Mice
2.11. Testosterone ELISA
2.12. Implantation of Osmotic Pumps
2.13. Statistical Analysis
3. Results
3.1. Refinement of SNV Infection in Deer Mice
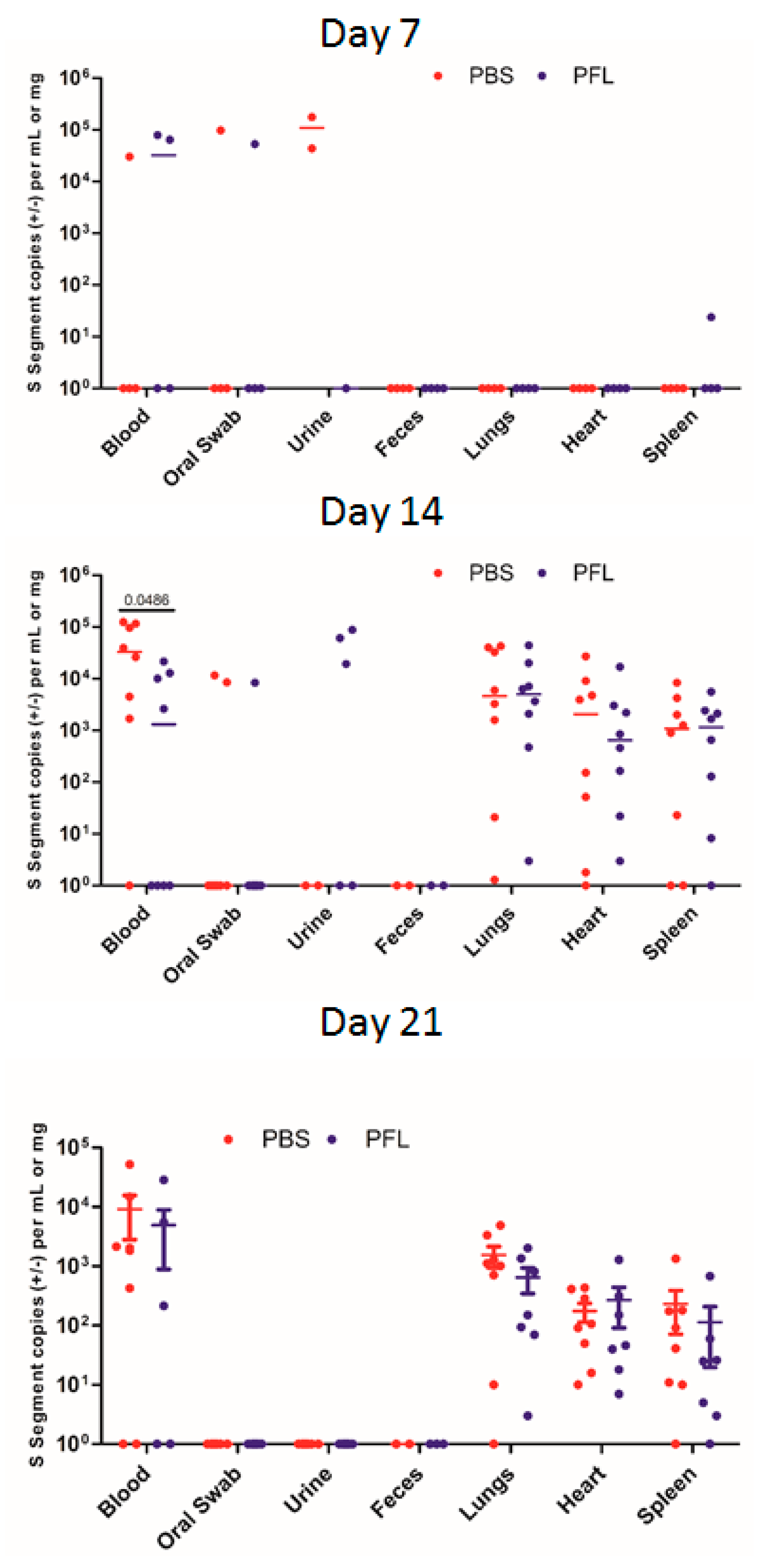
3.2. Direct Intra-Cage Transmission of SNV
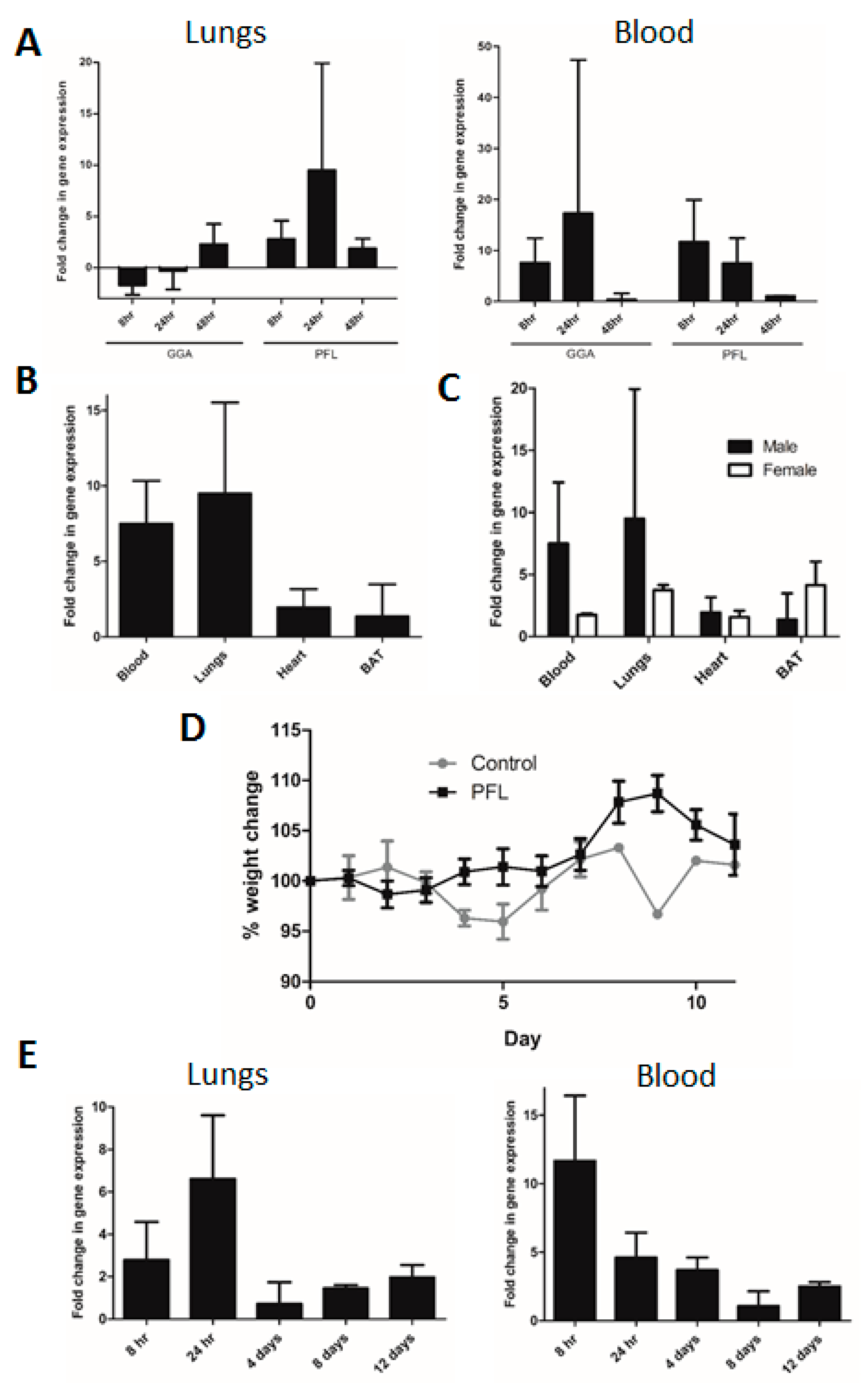
3.3. Induction of Heat Shock Responses
3.4. Transmission Rates in Male and Female Deer Mice
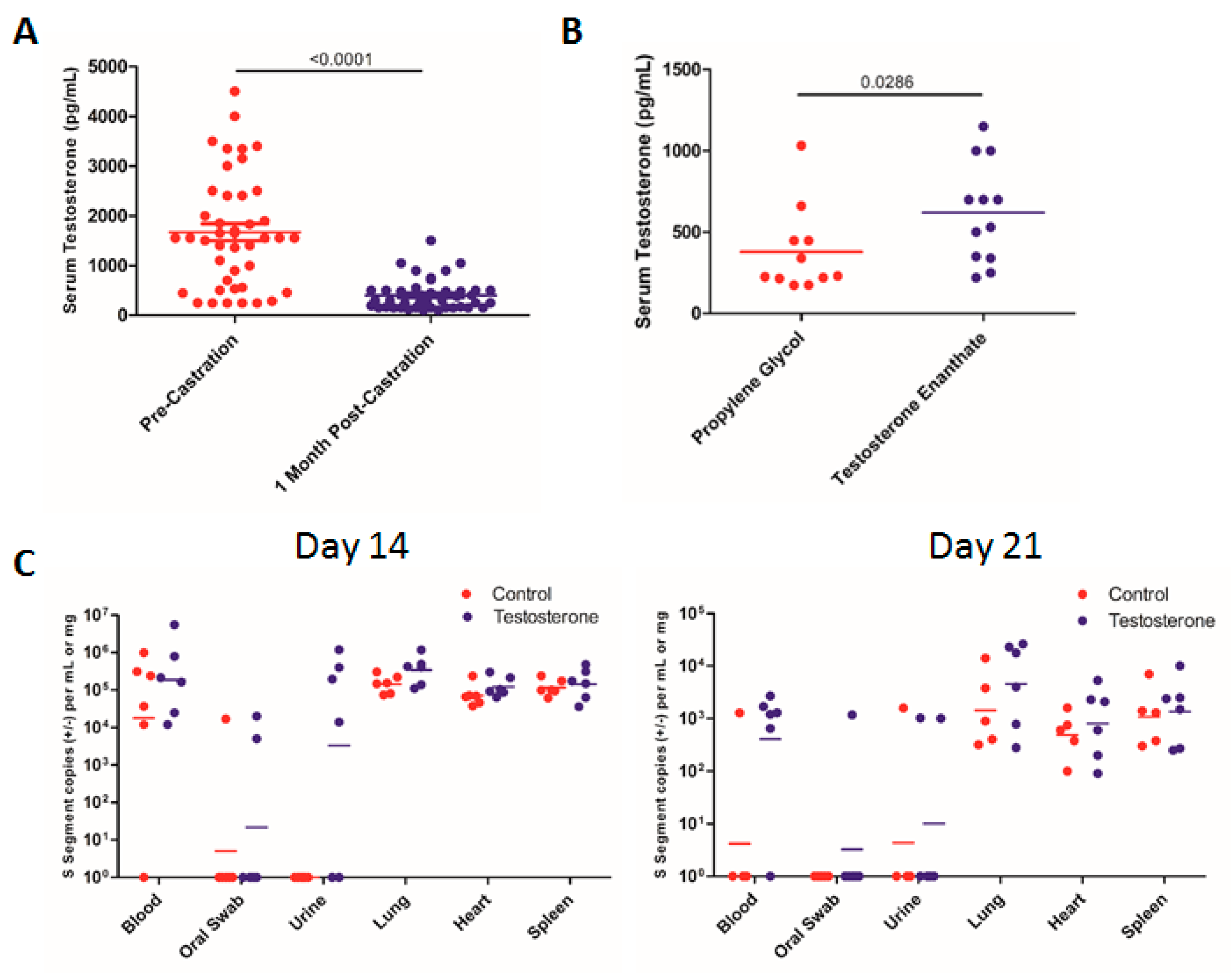
3.5. Effect of Testosterone on SNV Infection
4. Discussion
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- Muranyi, W.; Bahr, U.; Zeier, M.; van der Woude, F.J. Hantavirus Infection. J. Am. Soc. Nephrol. 2005, 16, 3669–3679. [Google Scholar] [CrossRef] [PubMed]
- Lee, H.W.; Lee, P.W.; Johnson, K.M. Isolation of the Etiologic Agent of Korean Hemorrhagic Fever. J. Infect. Dis. 1978, 137, 298–308. [Google Scholar] [CrossRef] [PubMed]
- Hjelle, B.; Jenison, S.; Torrez-Martinez, N.; Yamada, T.; Nolte, K.; Zumwalt, R.; MacInnes, K.; Myers, G. A Novel Hantavirus Associated with an Outbreak of Fatal Respiratory Disease in the Southwestern United States: Evolutionary Relationships to Known Hantaviruses. J. Virol. 1994, 68, 592–596. [Google Scholar] [PubMed]
- De St Maurice, A.; Ervin, E.; Schumacher, M.; Yaglom, H.; VinHatton, E.; Melman, S.; Komatsu, K.; House, J.; Peterson, D.; Buttke, D.; et al. Exposure Characteristics of Hantavirus Pulmonary Syndrome Patients, United States, 1993–2015. Emerg. Infect. Dis. 2017, 23, 733–739. [Google Scholar] [CrossRef] [PubMed]
- Drebot, M.A.; Jones, S.; Grolla, A.; Safronetz, D.; Strong, J.E.; Kobinger, G.; Lindsay, R.L. Hantavirus Pulmonary Syndrome in Canada: An Overview of Clinical Features, Diagnostics, Epidemiology and Prevention. Can. Commun. Dis. Rep. 2015, 41, 124–131. [Google Scholar] [CrossRef] [PubMed]
- Schmaljohn, C.S. Vaccines for Hantaviruses: Progress and Issues. Expert Rev. Vaccines 2012, 11, 511–513. [Google Scholar] [CrossRef] [PubMed]
- Jonsson, C.B.; Figueiredo, L.T.; Vapalahti, O. A Global Perspective on Hantavirus Ecology, Epidemiology, and Disease. Clin. Microbiol. Rev. 2010, 23, 412–441. [Google Scholar] [CrossRef] [PubMed]
- Safronetz, D.; Prescott, J.; Feldmann, F.; Haddock, E.; Rosenke, R.; Okumura, A.; Brining, D.; Dahlstrom, E.; Porcella, S.F.; Ebihara, H.; et al. Pathophysiology of Hantavirus Pulmonary Syndrome in Rhesus Macaques. Proc. Natl. Acad. Sci. USA 2014, 111, 7114–7119. [Google Scholar] [CrossRef] [PubMed]
- Lundkvist, A.; Cheng, Y.; Sjolander, K.B.; Niklasson, B.; Vaheri, A.; Plyusnin, A. Cell Culture Adaptation of Puumala Hantavirus Changes the Infectivity for its Natural Reservoir, Clethrionomys Glareolus, and Leads to Accumulation of Mutants with Altered Genomic RNA S Segment. J. Virol. 1997, 71, 9515–9523. [Google Scholar] [PubMed]
- Nemirov, K.; Lundkvist, A.; Vaheri, A.; Plyusnin, A. Adaptation of Puumala Hantavirus to Cell Culture is Associated with Point Mutations in the Coding Region of the L Segment and in the Noncoding Regions of the S Segment. J. Virol. 2003, 77, 8793–8800. [Google Scholar] [CrossRef] [PubMed]
- Botten, J.; Mirowsky, K.; Ye, C.; Gottlieb, K.; Saavedra, M.; Ponce, L.; Hjelle, B. Shedding and Intracage Transmission of Sin Nombre Hantavirus in the Deer Mouse (Peromyscus Maniculatus) Model. J. Virol. 2002, 76, 7587–7594. [Google Scholar] [CrossRef] [PubMed]
- Bagamian, K.H.; Towner, J.S.; Kuenzi, A.J.; Douglass, R.J.; Rollin, P.E.; Waller, L.A.; Mills, J.N. Transmission Ecology of Sin Nombre Hantavirus in Naturally Infected North American Deermouse Populations in Outdoor Enclosures. PLoS ONE 2012, 7, e47731. [Google Scholar] [CrossRef] [PubMed]
- Botten, J.; Mirowsky, K.; Kusewitt, D.; Ye, C.; Gottlieb, K.; Prescott, J.; Hjelle, B. Persistent Sin Nombre Virus Infection in the Deer Mouse (Peromyscus Maniculatus) Model: Sites of Replication and Strand-Specific Expression. J. Virol. 2003, 77, 1540–1550. [Google Scholar] [CrossRef] [PubMed]
- Hutchinson, K.L.; Rollin, P.E.; Shieh, W.J.; Zaki, S.; Greer, P.W.; Peters, C.J. Transmission of Black Creek Canal Virus between Cotton Rats. J. Med. Virol. 2000, 60, 70–76. [Google Scholar] [CrossRef]
- Padula, P.; Figueroa, R.; Navarrete, M.; Pizarro, E.; Cadiz, R.; Bellomo, C.; Jofre, C.; Zaror, L.; Rodriguez, E.; Murua, R. Transmission Study of Andes Hantavirus Infection in Wild Sigmodontine Rodents. J. Virol. 2004, 78, 11972–11979. [Google Scholar] [CrossRef] [PubMed]
- Kariwa, H.; Fujiki, M.; Yoshimatsu, K.; Arikawa, J.; Takashima, I.; Hashimoto, N. Urine-Associated Horizontal Transmission of Seoul Virus among Rats. Arch. Virol. 1998, 143, 365–374. [Google Scholar] [CrossRef] [PubMed]
- Yanagihara, R.; Amyx, H.L.; Gajdusek, D.C. Experimental Infection with Puumala Virus, the Etiologic Agent of Nephropathia Epidemica, in Bank Voles (Clethrionomys Glareolus). J. Virol. 1985, 55, 34–38. [Google Scholar]
- Kallio, E.R.; Klingström, J.; Gustafsson, E.; Manni, T.; Vaheri, A.; Henttonen, H.; Vapalahti, O.; Lundkvist, Å. Prolonged Survival of Puumala Hantavirus Outside the Host: Evidence for Indirect Transmission Via the Environment. J. Gen. Virol. 2006, 87, 2127–2134. [Google Scholar] [CrossRef]
- Lee, H.W.; Lee, P.W.; Baek, L.J.; Song, C.K.; Seong, I.W. Intraspecific Transmission of Hantaan Virus, Etiologic Agent of Korean Hemorrhagic Fever, in the Rodent Apodemus Agrarius. Am. J. Trop. Med. Hyg. 1981, 30, 1106–1112. [Google Scholar] [CrossRef]
- Botten, J.; Mirowsky, K.; Kusewitt, D.; Bharadwaj, M.; Yee, J.; Ricci, R.; Feddersen, R.M.; Hjelle, B. Experimental Infection Model for Sin Nombre Hantavirus in the Deer Mouse (Peromyscus Maniculatus). Proc. Natl. Acad. Sci. USA 2000, 97, 10578–10583. [Google Scholar] [CrossRef]
- Botten, J.; Ricci, R.; Hjelle, B. Establishment of a Deer Mouse (Peromyscus Maniculatus Rufinus) Breeding Colony from Wild-Caught Founders: Comparison of Reproductive Performance of Wild-Caught and Laboratory-Reared Pairs. Comp. Med. 2001, 51, 314–318. [Google Scholar]
- Valkenburg, K.C.; Amend, S.R.; Pienta, K.J. Murine prostate micro-dissection and surgical castration. J. Vis. Exp. 2016, 111, 53984. [Google Scholar] [CrossRef]
- Matz, J.M.; Blake, M.J.; Tatelman, H.M.; Lavoi, K.P.; Holbrook, N.J. Characterization and Regulation of Cold-Induced Heat Shock Protein Expression in Mouse Brown Adipose Tissue. Am. J. Physiol. 1995, 269, R38–R47. [Google Scholar] [CrossRef]
- Matz, J.M.; LaVoi, K.P.; Moen, R.J.; Blake, M.J. Cold-Induced Heat Shock Protein Expression in Rat Aorta and Brown Adipose Tissue. Physiol. Behav. 1996, 60, 1369–1374. [Google Scholar] [CrossRef]
- Santoro, M.G.; Amici, C.; Rossi, A. Role of Heat Shock Proteins in Viral Infection. In Prokaryotic and Eukaryotic Heat Shock Proteins in Infectious Disease; Springer: Dordrecht, The Netherlands, 2009; pp. 51–84. [Google Scholar]
- Yu, L.; Ye, L.; Zhao, R.; Liu, Y.F.; Yang, S.J. HSP70 Induced by Hantavirus Infection Interacts with Viral Nucleocapsid Protein and its Overexpression Suppresses Virus Infection in Vero E6 Cells. Am. J. Transl. Res. 2009, 1, 367–380. [Google Scholar]
- Wang, X.; Yuan, B.; Dong, W.; Yang, B.; Yang, Y.; Lin, X.; Gong, G. Induction of Heat-Shock Protein 70 Expression by Geranylgeranylacetone shows Cytoprotective Effects in Cardiomyocytes of Mice Under Humid Heat Stress. PLoS ONE 2014, 9, e93536. [Google Scholar] [CrossRef]
- Tokuriki, S.; Igarashi, A.; Okuno, T.; Ohta, G.; Naiki, H.; Ohshima, Y. Treatment with Geranylgeranylacetone Induces Heat Shock Protein 70 and Attenuates Neonatal Hyperoxic Lung Injury in a Model of Bronchopulmonary Dysplasia. Lung 2017, 195, 469–476. [Google Scholar] [CrossRef]
- Hehir, M.P.; Morrison, J.J. Paeoniflorin, a Novel heat-shock Protein Inducing Compound, and Human Myometrial Contractility in Vitro. J. Obstet. Gynaecol. Res. 2016, 42, 302–306. [Google Scholar] [CrossRef]
- Fan, Y.; Qian, C.; Liu, B.; Wang, C.; Liu, H.; Pan, X.; Teng, P.; Hu, L.; Zhang, G.; Han, Y.; et al. Induction of Suppressor of Cytokine Signaling 3 Via HSF-1-HSP70-TLR4 Axis Attenuates Neuroinflammation and Ameliorates Postoperative Pain. Brain Behav. Immun. 2018, 68, 111–122. [Google Scholar] [CrossRef]
- Zhu, S.H.; Liu, B.Q.; Hao, M.J.; Fan, Y.X.; Qian, C.; Teng, P.; Zhou, X.W.; Hu, L.; Liu, W.T.; Yuan, Z.L.; et al. Paeoniflorin Suppressed High Glucose-Induced Retinal Microglia MMP-9 Expression and Inflammatory Response Via Inhibition of TLR4/NF-kappaB Pathway through Upregulation of SOCS3 in Diabetic Retinopathy. Inflammation 2017, 40, 1475–1486. [Google Scholar] [CrossRef]
- Bennet, S.G.; Webb, J.P., Jr.; Madon, M.B.; Childs, J.E.; Ksiazek, T.G.; Torrez-Martinez, N.; Hjelle, B. Hantavirus (Bunyaviridae) Infections in Rodents from Orange and San Diego Counties, California. Am. J. Trop. Med. Hyg. 1999, 60, 75–84. [Google Scholar] [CrossRef]
- Mills, J.N.; Ksiazek, T.G.; Ellis, B.A.; Rollin, P.E.; Nichol, S.T.; Yates, T.L.; Gannon, W.L.; Levy, C.E.; Engelthaler, D.M.; Davis, T.; et al. Patterns of Association with Host and Habitat: Antibody Reactive with Sin Nombre Virus in Small Mammals in the Major Biotic Communities of the Southwestern United States. Am. J. Trop. Med. Hyg. 1997, 56, 273–284. [Google Scholar] [CrossRef]
- Glass, G.E.; Childs, J.E.; Korch, G.W.; LeDuc, J.W. Association of Intraspecific Wounding with Hantaviral Infection in Wild Rats (Rattus Norvegicus). Epidemiol. Infect. 1988, 101, 459–472. [Google Scholar] [CrossRef]
- Easterbrook, J.D.; Kaplan, J.B.; Glass, G.E.; Pletnikov, M.V.; Klein, S.L. Elevated Testosterone and Reduced 5-HIAA Concentrations are Associated with Wounding and Hantavirus Infection in Male Norway Rats. Horm. Behav. 2007, 52, 474–481. [Google Scholar] [CrossRef]
- Hannah, M.F.; Bajic, V.B.; Klein, S.L. Sex Differences in the Recognition of and Innate Antiviral Responses to Seoul Virus in Norway Rats. Brain Behav. Immun. 2008, 22, 503–516. [Google Scholar] [CrossRef]
- Easterbrook, J.D.; Klein, S.L. Corticosteroids Modulate Seoul Virus Infection, Regulatory T-Cell Responses and Matrix Metalloprotease 9 Expression in Male, but Not Female, Norway Rats. J. Gen. Virol. 2008, 89, 2723–2730. [Google Scholar] [CrossRef]
- Fish, E.N. The X-Files in Immunity: Sex-Based Differences Predispose Immune Responses. Nat. Rev. Immunol. 2008, 8, 737–744. [Google Scholar] [CrossRef]
- Easterbrook, J.D.; Klein, S.L. Immunological Mechanisms Mediating Hantavirus Persistence in Rodent Reservoirs. PLoS Pathog. 2008, 4, e1000172. [Google Scholar] [CrossRef]
- Hardestam, J.; Karlsson, M.; Falk, K.I.; Olsson, G.; Klingström, J.; Lundkvist, Å. Puumala hantavirus excretion kinetics in bank voles (Myodes glareolus). Emerging infectious diseases. Emerg. Infect. Dis. 2008, 14, 1209. [Google Scholar] [CrossRef]
- Voutilainen, L.; Sironen, T.; Tonteri, E.; Bäck, A.T.; Razzauti, M.; Karlsson, M.; Wahlström, M.; Niemimaa, J.; Henttonen, H.; Lundkvist, Å. Life-Long Shedding of Puumala Hantavirus in Wild Bank Voles (Myodes Glareolus). J. Gen. Virol. 2015, 96, 1238–1247. [Google Scholar] [CrossRef]
- Forbes, K.M.; Sironen, T.; Plyusnin, A. Hantavirus Maintenance and Transmission in Reservoir Host Populations. Curr. Opin. Virol. 2018, 28, 1–6. [Google Scholar] [CrossRef]
- Safronetz, D.; Drebot, M.A.; Artsob, H.; Cote, T.; Makowski, K.; Lindsay, L.R. Sin Nombre Virus Shedding Patterns in Naturally Infected Deer Mice (Peromyscus Maniculatus) in Relation to Duration of Infection. Vector Borne Zoonotic Dis. 2008, 8, 97–100. [Google Scholar] [CrossRef]
- Milhano, N.; Korslund, L.; Evander, M.; Ahlm, C.; Vainio, K.; Dudman, S.G.; Andreassen, A. Circulation and Diagnostics of Puumala Virus in Norway: Nephropatia Epidemica Incidence and Rodent Population Dynamics. APMIS 2017, 125, 732–742. [Google Scholar] [CrossRef]
- Prist, P.R.; Uriarte, M.; Fernandes, K.; Metzger, J.P. Climate Change and Sugarcane Expansion Increase Hantavirus Infection Risk. PLoS Negl. Trop. Dis. 2017, 11, e0005705. [Google Scholar] [CrossRef]
- Khalil, H.; Hornfeldt, B.; Evander, M.; Magnusson, M.; Olsson, G.; Ecke, F. Dynamics and Drivers of Hantavirus Prevalence in Rodent Populations. Vector Borne Zoonotic Dis. 2014, 14, 537–551. [Google Scholar] [CrossRef]
- Luis, A.D.; Douglass, R.J.; Mills, J.N.; Bjornstad, O.N. Environmental Fluctuations Lead to Predictability in Sin Nombre Hantavirus Outbreaks. Ecology 2015, 96, 1691–1701. [Google Scholar] [CrossRef]
- Hjelle, B.; Glass, G.E. Outbreak of Hantavirus Infection in the Four Corners Region of the United States in the Wake of the 1997–1998 El Nino-Southern Oscillation. J. Infect. Dis. 2000, 181, 1569–1573. [Google Scholar] [CrossRef]
- Clement, J.; Vercauteren, J.; Verstraeten, W.W.; Ducoffre, G.; Barrios, J.M.; Vandamme, A.M.; Maes, P.; Van Ranst, M. Relating Increasing Hantavirus Incidences to the Changing Climate: The Mast Connection. Int. J. Health. Geogr. 2009, 8, 1. [Google Scholar] [CrossRef]

| Group | Exposed, Naïve Mice | Transmission Events * | % of Naïve Infected | Risk Ratio (95% CI) | P Value (Fisher’s Exact Test) |
|---|---|---|---|---|---|
| Direct Transmission | 33 | 8 | 24 | 1.320 (1.088–1.601) | 0.0051 |
| Indirect Transmission | 30 | 0 | 0 |
| Group | Exposed, Naïve Mice | Transmission Events * | % of Naïve Infected | Risk Ratio (95% CI) | P Value (Fisher’s Exact Test) |
|---|---|---|---|---|---|
| Direct Transmission | 33 | 8 | 24 | 1.355 (0.9489–1.878) | 0.1311 |
| PFL Treated ψ | 37 | 16 | 43 |
| Group | Male | Female |
|---|---|---|
| Control | 2/13 | 6/20 |
| PFL-Treated | 9/18 | 7/19 |
| Total | 11/31 | 13/39 |
| Group | Exposed, Naïve Mice | Transmission Events * | % of Naïve Infected | Risk Ratio (95% CI) | P Value (Fisher’s Exact Test) |
|---|---|---|---|---|---|
| Propylene Glycol | 30 | 10 | 33 | 1.074 (0.7339–1.572) | 0.7892 |
| Testosterone | 29 | 11 | 38 |
© 2019 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Warner, B.M.; Stein, D.R.; Griffin, B.D.; Tierney, K.; Leung, A.; Sloan, A.; Kobasa, D.; Poliquin, G.; Kobinger, G.P.; Safronetz, D. Development and Characterization of a Sin Nombre Virus Transmission Model in Peromyscus maniculatus. Viruses 2019, 11, 183. https://doi.org/10.3390/v11020183
Warner BM, Stein DR, Griffin BD, Tierney K, Leung A, Sloan A, Kobasa D, Poliquin G, Kobinger GP, Safronetz D. Development and Characterization of a Sin Nombre Virus Transmission Model in Peromyscus maniculatus. Viruses. 2019; 11(2):183. https://doi.org/10.3390/v11020183
Chicago/Turabian StyleWarner, Bryce M., Derek R. Stein, Bryan D. Griffin, Kevin Tierney, Anders Leung, Angela Sloan, Darwyn Kobasa, Guillaume Poliquin, Gary P. Kobinger, and David Safronetz. 2019. "Development and Characterization of a Sin Nombre Virus Transmission Model in Peromyscus maniculatus" Viruses 11, no. 2: 183. https://doi.org/10.3390/v11020183
APA StyleWarner, B. M., Stein, D. R., Griffin, B. D., Tierney, K., Leung, A., Sloan, A., Kobasa, D., Poliquin, G., Kobinger, G. P., & Safronetz, D. (2019). Development and Characterization of a Sin Nombre Virus Transmission Model in Peromyscus maniculatus. Viruses, 11(2), 183. https://doi.org/10.3390/v11020183





