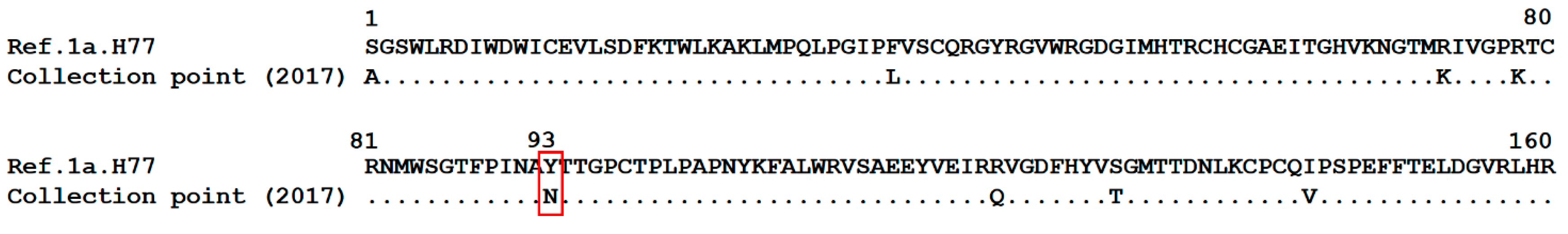
Resistance Mutations A30K and Y93N Associated with Treatment Failure with Sofosbuvir and Daclatasvir for Hepatitis C Virus Infection Non-Responder Patients: Case Reports
Abstract
1. Introduction
2. Materials and Methods
3. Results
3.1. Case Report 1
3.2. Case Report 2
4. Discussion
5. Conclusions
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- WHO. Prevalence of Chronically Infected People with Hepatitis C Virus (HCV) Worldwide. 2018. Available online: http://www.who.int/news-room/fact-sheets/detail/hepatitis-c (accessed on 25 April 2019).
- Lampe, E.; Espirito-Santo, M.P.; Martins, R.M.; Bello, G. Epidemic history of Hepatitis C virus in Brazil. Infect. Genet. Evol. J. Mol. Epidemiol. Evol. Genet. Infect. Dis. 2010, 10, 886–895. [Google Scholar] [CrossRef] [PubMed]
- Ministério da Saúde, Brasil. Protocolo Clínico e Diretrizes Terapêuticas para Hepatite C e Coinfecções. 2015. Available online: http://bvsms.saude.gov.br/bvs/publicacoes/protocolo_clinico_diretrizes_hepatite_co_coinfeccoes.pdf (accessed on 25 April 2019).
- Sarrazin, C. The importance of resistance to direct antiviral drugs in HCV infection in clinical practice. J. Hepatol. 2016, 64, 486–504. [Google Scholar] [CrossRef] [PubMed]
- Fridell, R.A.; Wang, C.; Sun, J.H.; O’Boyle, D.R., II; Nower, P.; Valera, L.; Qiu, D.; Roberts, S.; Huang, X.; Kienzle, B.; et al. Genotypic and phenotypic analysis of variants resistant to hepatitis C virus nonstructural protein 5A replication complex inhibitor BMS-790052 in humans: In vitro and in vivo correlations. Hepatology 2011, 54, 1924–1935. [Google Scholar] [CrossRef] [PubMed]
- Wang, C.; Valera, L.; Jia, L.; Kirk, M.J.; Gao, M.; Fridell, R.A. In vitro activity of daclatasvir on hepatitis C virus genotype 3 NS5A. Antimicrob. Agents Chemother. 2013, 57, 611–613. [Google Scholar] [CrossRef] [PubMed]
- Hernandez, D.; Zhou, N.; Ueland, J.; Monikowski, A.; McPhee, F. Natural prevalence of NS5A polymorphisms in subjects infected with hepatitis C virus genotype 3 and their effects on the antiviral activity of NS5A inhibitors. J. Clin. Virol. 2013, 57, 13–18. [Google Scholar] [CrossRef] [PubMed]
- Lok, A.S.; Gardiner, D.F.; Hezode, C.; Lawitz, E.J.; Bourliere, M.; Everson, G.T.; Marcellin, P.; Rodriguez-Torres, M.; Pol, S.; Serfaty, L.; et al. Randomized trial of daclatasvir and asunaprevir with or without PegIFN/RBV for hepatitis C virus genotype 1 null responders. J. Hepatol. 2014, 60, 490–499. [Google Scholar] [CrossRef]
- Malta, F.; Gaspareto, K.V.; Lisboa-Neto, G.; Carrilho, F.J.; Mendes-Correa, M.C.; Pinho, J.R.R. Prevalence of naturally occurring NS5A resistance-associated substitutions in patients infected with hepatitis C virus subtype 1a, 1b, and 3a, co-infected or not with HIV in Brazil. BMC Infect. Dis. 2017, 17, 716. [Google Scholar] [CrossRef]
- Costa, V.D.; Brandao-Mello, C.E.; Nunes, E.P.; Dos Santos Silva, P.G.C.; de Souza Rodrigues, L.; Lampe, E.; do Amaral Mello, F.C. Treatment of chronic HCV infection with DAAs in Rio de Janeiro/Brazil: SVR rates and baseline resistance analyses in NS5A and NS5B genes. PLoS ONE 2019, 14, e0216327. [Google Scholar] [CrossRef]
- Coppola, N.; Minichini, C.; Starace, M.; Sagnelli, C.; Sagnelli, E. Clinical impact of the hepatitis C virus mutations in the era of directly acting antivirals. J. Med. Virol. 2016, 88, 1659–1671. [Google Scholar] [CrossRef]
- Wyles, D.L.; Luetkemeyer, A.F. Understanding Hepatitis C Virus Drug Resistance: Clinical Implications for Current and Future Regimens. Top. Antivir. Med. 2017, 25, 103–109. [Google Scholar]
- Kuiken, C.; Yusim, K.; Boykin, L.; Richardson, R. The Los Alamos hepatitis C sequence database. Bioinformatics 2005, 21, 379–384. [Google Scholar] [CrossRef] [PubMed]
- Kumar, S.; Stecher, G.; Tamura, K. MEGA7: Molecular Evolutionary Genetics Analysis Version 7.0 for Bigger Datasets. Mol. Biol. Evol. 2016, 33, 1870–1874. [Google Scholar] [CrossRef] [PubMed]
- Li, D.K.; Chung, R.T. Overview of Direct-Acting Antiviral Drugs and Drug Resistance of Hepatitis C Virus. Methods Mol. Biol. 2019, 1911, 3–32. [Google Scholar] [CrossRef] [PubMed]
- Cheinquer, H.; Sette, H., Jr.; Wolff, F.H.; de Araujo, A.; Coelho-Borges, S.; Soares, S.R.P.; Barros, M.F.A. Treatment of Chronic HCV Infection with the New Direct Acting Antivirals (DAA): First Report of a Real World Experience in Southern Brazil. Ann. Hepatol. 2017, 16, 727–733. [Google Scholar] [CrossRef] [PubMed]
- Buti, M.; Esteban, R. Management of direct antiviral agent failures. Clin. Mol. Hepatol. 2016, 22, 432–438. [Google Scholar] [CrossRef]
- Nelson, D.R.; Cooper, J.N.; Lalezari, J.P.; Lawitz, E.; Pockros, P.J.; Gitlin, N.; Freilich, B.F.; Younes, Z.H.; Harlan, W.; Ghalib, R.; et al. All-oral 12-week treatment with daclatasvir plus sofosbuvir in patients with hepatitis C virus genotype 3 infection: ALLY-3 phase III study. Hepatology 2015, 61, 1127–1135. [Google Scholar] [CrossRef]
- Poordad, F.; Schiff, E.R.; Vierling, J.M.; Landis, C.; Fontana, R.J.; Yang, R.; McPhee, F.; Hughes, E.A.; Noviello, S.; Swenson, E.S. Daclatasvir with sofosbuvir and ribavirin for hepatitis C virus infection with advanced cirrhosis or post-liver transplantation recurrence. Hepatology 2016, 63, 1493–1505. [Google Scholar] [CrossRef]
- Lahser, F.; Galloway, A.; Hwang, P.; Palcza, J.; Brunhofer, J.; Wahl, J.; Robertson, M.; Barr, E.; Black, T.; Asante-Appiah, E.; et al. Interim analysis of a 3-year follow-up study of NS5A and NS3 resistance-associated substitutions after treatment with grazoprevir-containing regimens in participants with chronic HCV infection. Antivir. Ther. 2018, 23, 593–603. [Google Scholar] [CrossRef]
- Liu, R.; Curry, S.; McMonagle, P.; Yeh, W.W.; Ludmerer, S.W.; Jumes, P.A.; Marshall, W.L.; Kong, S.; Ingravallo, P.; Black, S.; et al. Susceptibilities of genotype 1a, 1b, and 3 hepatitis C virus variants to the NS5A inhibitor elbasvir. Antimicrob. Agents Chemother. 2015, 59, 6922–6929. [Google Scholar] [CrossRef]
- Lawitz, E.J.; Dvory-Sobol, H.; Doehle, B.P.; Worth, A.S.; McNally, J.; Brainard, D.M.; Link, J.O.; Miller, M.D.; Mo, H. Clinical Resistance to Velpatasvir (GS-5816), a Novel Pan-Genotypic Inhibitor of the Hepatitis C Virus NS5A Protein. Antimicrob. Agents Chemother. 2016, 60, 5368–5378. [Google Scholar] [CrossRef]
- Kwo, P.Y.; Poordad, F.; Asatryan, A.; Wang, S.; Wyles, D.L.; Hassanein, T.; Felizarta, F.; Sulkowski, M.S.; Gane, E.; Maliakkal, B.; et al. Glecaprevir and pibrentasvir yield high response rates in patients with HCV genotype 1-6 without cirrhosis. J. Hepatol. 2017, 67, 263–271. [Google Scholar] [CrossRef] [PubMed]

© 2019 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Costa, V.D.; Pellegrini, P.; Rotman, V.; Pittella, A.M.; Nunes, E.P.; Lago, B.V.; Lampe, E.; Mello, F.C.A. Resistance Mutations A30K and Y93N Associated with Treatment Failure with Sofosbuvir and Daclatasvir for Hepatitis C Virus Infection Non-Responder Patients: Case Reports. Viruses 2019, 11, 1004. https://doi.org/10.3390/v11111004
Costa VD, Pellegrini P, Rotman V, Pittella AM, Nunes EP, Lago BV, Lampe E, Mello FCA. Resistance Mutations A30K and Y93N Associated with Treatment Failure with Sofosbuvir and Daclatasvir for Hepatitis C Virus Infection Non-Responder Patients: Case Reports. Viruses. 2019; 11(11):1004. https://doi.org/10.3390/v11111004
Chicago/Turabian StyleCosta, Vanessa D., Patricia Pellegrini, Vivian Rotman, Ana Maria Pittella, Estevão P. Nunes, Barbara V. Lago, Elisabeth Lampe, and Francisco C. A. Mello. 2019. "Resistance Mutations A30K and Y93N Associated with Treatment Failure with Sofosbuvir and Daclatasvir for Hepatitis C Virus Infection Non-Responder Patients: Case Reports" Viruses 11, no. 11: 1004. https://doi.org/10.3390/v11111004
APA StyleCosta, V. D., Pellegrini, P., Rotman, V., Pittella, A. M., Nunes, E. P., Lago, B. V., Lampe, E., & Mello, F. C. A. (2019). Resistance Mutations A30K and Y93N Associated with Treatment Failure with Sofosbuvir and Daclatasvir for Hepatitis C Virus Infection Non-Responder Patients: Case Reports. Viruses, 11(11), 1004. https://doi.org/10.3390/v11111004




