Indicators of the Psychosocial and Physiological Effects of Forest Therapy: A Systematic Review
Abstract
1. Introduction
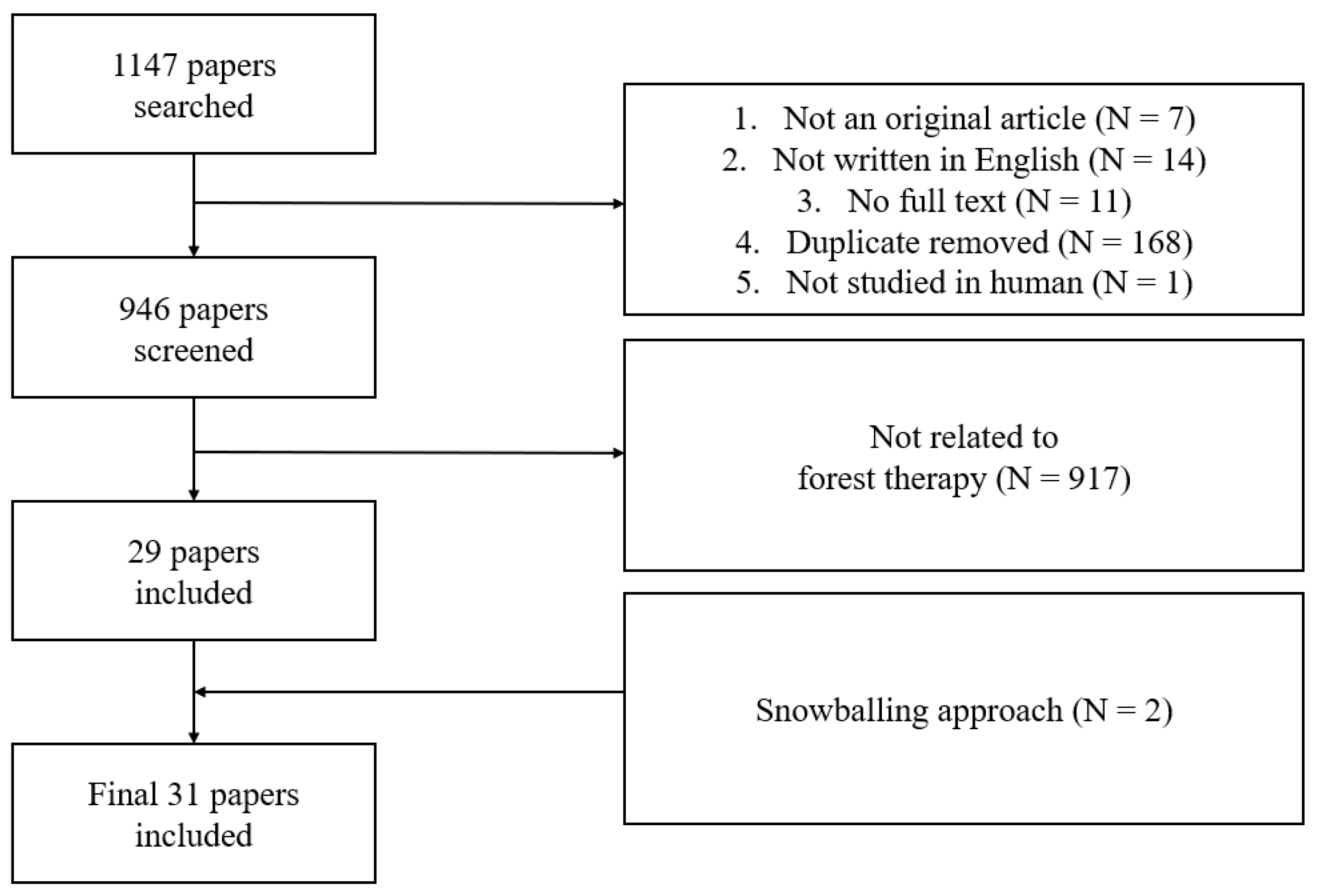
2. Methods
2.1. Literature Search
2.2. Selection Criteria
2.3. Data Extraction
2.4. Data Cleaning
2.4.1. Study Characteristics
2.4.2. Natural Therapeutic Elements
2.4.3. Characteristics of Forest-Therapy Programs
2.4.4. Psychological and Physiological Health Outcomes
Psychological Health Outcome and Measure
Physiological Health Outcome and Measure
2.5. Data Analysis
3. Results
3.1. Characteristics of the Included Studies
3.2. Natural Therapeutic Elements
3.3. Types of Forest-Therapy Programs
3.4. Effect of Forest Therapy on Mental Health
3.5. Indicators of Physical Health
3.6. Cross-Tabulation of Psychological and Physiological Health Outcomes
3.7. Cross-Tabulation of Psychological and Physiological Outcomes of Forest-Therapy Session Content
4. Discussion
4.1. Natural Therapeutic Elements
4.2. Characteristics of Forest-Therapy Programs
4.3. Health Outcomes
4.3.1. Health Outcomes and Measures
4.3.2. Health Outcomes and Natural Therapeutic Elements
4.3.3. Health Outcomes and Forest-Therapy Sessions
4.4. Limitations
4.5. Strengths and Message
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Data Availability Statement
Conflicts of Interest
Abbreviations
| Abbreviation | Explanation |
| MBI-GS | Maslach Burnout Inventory–General Survey |
| REQ | Recovery Experience Questionnaire |
| SMBQ | Shirom–Melamed Burnout Questionnaire |
| korean_CASS-S | Conners–Wells’ Adolescent Self-Report Scale (Short Form) |
| HADS | Hospital anxiety and depression scale |
| POMS | Profile of Mood States |
| STAI | The State–Trait Anxiety Inventory |
| STAI-S | The State–Trait Anxiety Inventory to measure state |
| POMS | Profile of Mood States |
| PSQ | Perceived Stress Questionnaire |
| BDI | Beck Depression Inventory |
| CDI | Korean version of the Children’s Depression Inventory |
| GeriatricDS | The Geriatric Depression Scale |
| HAM-D17 | Hamilton Depression Rating Scale |
| KPDS-K6 | Kessler Psychological Distress Scale |
| Perception_env | Perception environment |
| CIS | Checklist Individual Strength questionnaire |
| VAS-F | Visual analogue scale to evaluate fatigue severity |
| BRUMS | The Brunel Mood State Inventory |
| PANAS | The Positive and Negative Affect Schedule |
| ROS | The Restorative Outcome Scale |
| SemanticDT | Semantic differential techniques to assess subjective feelings of “comfortable” and “soothed” |
| SVS | Subjective Vitality Scale |
| ZIPERS | Zuckerman Inventory of Personal Reaction Scale |
| sf-36 | The Short Form Health Survey 36 |
| SF-8 | Short version of Health-Related Quality of Life |
| RSE | Rosenberg Self-Esteem Scale |
| SCQ | Social Communication Questionnaire |
| HPLP2 | Health-Promoting Lifestyle Profile II |
| q_healthcon | Single-sentence question: “How do you feel about your overall health condition?” |
| Q_Symptom | Self-reported symptoms and medicines used by the group |
| ESS | Epworth sleepiness scale |
| insomniaSI | Insomnia severity index |
| PSQI | Pittsburgh Sleep Questionnaire Index (PSQI) |
| SSS | Stanford sleepiness scale |
| STOP-Bang | Assessment tool used to help diagnose obstructive sleep apnea (STOP-BANG—snoring, tired, observed, pressure, body mass index, age, neck size, gender) |
| PLMi | Periodic limb movement index |
| ODI | Oxygen desaturation index |
| AHI | Apnea Hypopnea Index |
| Peer_relation | The peer relationship instrument |
| RCS | The Relationship Change Scale |
| SASS | Social Adaptation Self-evaluation Scale |
| KPDS-K6 | Kessler Psychological Distress Scale K6 |
| PSS-Korean | Perceived Stress Scale, Korean |
| SRI-MF | Stress Response Inventory-Modified Form |
| Stress-CT | Stress-coping techniques |
| Tool_hemodialysis | Tool developed for hemodialysis patients by Kim (physiological stress, psychological stress) |
| WSRI | Worker’s Stress Response Inventory |
References
- World Health Organization. Mental Health: Strengthening Our Response; World Health Organization: Geneva, Switzerland, 2018. [Google Scholar]
- Vogt, T.; Pope, C.; Mullooly, J.; Hollis, J. Mental health status as a predictor of morbidity and mortality: A 15-year follow-up of members of a health maintenance organization. Am. J. Public Health 1994, 84, 227–231. [Google Scholar] [CrossRef] [PubMed]
- Littrell, J. The mind-body connection: Not just a theory anymore. Soc. Work. Health Care 2008, 46, 17–37. [Google Scholar] [CrossRef] [PubMed]
- McCaffrey, R.; Frock, T.L.; Garguilo, H. Understanding chronic pain and the mind-body connection. Holist. Nurs. Pract. 2003, 17, 281–289. [Google Scholar] [CrossRef] [PubMed]
- Kim, K.W. Theoretical study of characteristics of therapeutic elements and application to forest therapy. J. Korean Soc. People Plants Environ. 2006, 9, 111–123. [Google Scholar]
- Park, S.; Kim, S.; Kim, G.; Choi, Y.; Kim, E.; Paek, D. Evidence-based status of forest healing program in South Korea. Int. J. Environ. Res. Public Health 2021, 18, 10368. [Google Scholar] [CrossRef] [PubMed]
- Kim, G. A study on conceptual method for forest trail planning. J. Korean Inst. Forest Recreat 2009, 13, 11–24. [Google Scholar] [CrossRef]
- Bratman, G.N.; Anderson, C.B.; Berman, M.G.; Cochran, B.; De Vries, S.; Flanders, J.; Folke, C.; Frumkin, H.; Gross, J.J.; Hartig, T. Nature and mental health: An ecosystem service perspective. Sci. Adv. 2019, 5, eaax0903. [Google Scholar] [CrossRef]
- Rajoo, K.S.; Karam, D.S.; Abdullah, M.Z. The physiological and psychosocial effects of forest therapy: A systematic review. Urban For. Urban Green. 2020, 54, 126744. [Google Scholar] [CrossRef]
- Ochiai, H.; Ikei, H.; Song, C.; Kobayashi, M.; Miura, T.; Kagawa, T.; Li, Q.; Kumeda, S.; Imai, M.; Miyazaki, Y. Physiological and psychological effects of a forest therapy program on middle-aged females. Int. J. Environ. Res. Public Health 2015, 12, 15222–15232. [Google Scholar] [CrossRef]
- Lee, J.; Tsunetsugu, Y.; Takayama, N.; Park, B.-J.; Li, Q.; Song, C.; Komatsu, M.; Ikei, H.; Tyrväinen, L.; Kagawa, T. Influence of forest therapy on cardiovascular relaxation in young adults. Evid.-Based Complement. Altern. Med. 2014, 2014, 834360. [Google Scholar] [CrossRef]
- Li, Q.; Kobayashi, M.; Kumeda, S.; Ochiai, T.; Miura, T.; Kagawa, T.; Imai, M.; Wang, Z.; Otsuka, T.; Kawada, T. Effects of forest bathing on cardiovascular and metabolic parameters in middle-aged males. Evid.-Based Complement. Altern. Med. 2016, 2016, 2587381. [Google Scholar] [CrossRef] [PubMed]
- Sung, J.; Woo, J.-M.; Kim, W.; Lim, S.-K.; Chung, E.-J. The effect of cognitive behavior therapy-based “forest therapy” program on blood pressure, salivary cortisol level, and quality of life in elderly hypertensive patients. Clin. Exp. Hypertens. 2012, 34, 1–7. [Google Scholar] [CrossRef] [PubMed]
- Song, C.; Ikei, H.; Miyazaki, Y. Sustained effects of a forest therapy program on the blood pressure of office workers. Urban For. Urban Green. 2017, 27, 246–252. [Google Scholar] [CrossRef]
- Mao, G.X.; Cao, Y.B.; Lan, X.G.; He, Z.H.; Chen, Z.M.; Wang, Y.Z.; Hu, X.-L.; Lv, Y.D.; Wang, G.-F.; Yan, J. Therapeutic effect of forest bathing on human hypertension in the elderly. J. Cardiol. 2012, 60, 495–502. [Google Scholar] [CrossRef]
- Kim, H.; Kim, J.; Ju, H.J.; Jang, B.J.; Wang, T.K.; Kim, Y.I. Effect of forest therapy for menopausal women with insomnia. Int. J. Environ. Res. Public Health 2020, 17, 6548. [Google Scholar] [CrossRef]
- Chae, Y.; Lee, S.; Jo, Y.; Kang, S.; Park, S.; Kang, H. The Effects of Forest Therapy on Immune Function. International Journal of Environmental Research and Public Health 2021, 18, 8440. [Google Scholar] [CrossRef]
- Lyu, B.; Zeng, C.; Xie, S.; Li, D.; Lin, W.; Li, N.; Jiang, M.; Liu, S.; Chen, Q. Benefits of a three-day bamboo forest therapy session on the psychophysiology and immune system responses of male college students. Int. J. Environ. Res. Public Health 2019, 16, 4991. [Google Scholar] [CrossRef]
- Lee, I.; Choi, H.; Bang, K.S.; Kim, S.; Song, M.; Lee, B. Effects of Forest Therapy on Depressive Symptoms among Adults: A Systematic Review. Int. J. Environ. Res. Public Health 2017, 14, 321. [Google Scholar] [CrossRef]
- Zhao, J.; An, Y. Behavioural intention of forest therapy tourism in China: Based on health belief model and the theory of planned behaviour. Curr. Issues Tour. 2021, 24, 3425–3432. [Google Scholar] [CrossRef]
- Kang, B.; Kim, T.; Kim, M.J.; Lee, K.H.; Choi, S.; Lee, D.H.; Kim, H.R.; Jun, B.; Park, S.Y.; Lee, S.J. Relief of chronic posterior neck pain depending on the type of forest therapy: Comparison of the therapeutic effect of forest bathing alone versus forest bathing with exercise. Ann. Rehabil. Med. 2015, 39, 957–963. [Google Scholar] [CrossRef]
- Zeng, C.; Lyu, B.; Deng, S.; Yu, Y.; Li, N.; Lin, W.; Li, D.; Chen, Q. Benefits of a Three-Day Bamboo Forest Therapy Session on the Physiological Responses of University Students. Int. J. Environ. Res. Public Health 2020, 17, 3238. [Google Scholar] [CrossRef]
- Bielinis, E.; Jaroszewska, A.; Łukowski, A.; Takayama, N. The Effects of a Forest Therapy Programme on Mental Hospital Patients with Affective and Psychotic Disorders. Int. J. Environ. Res. Public Health 2020, 17, 118. [Google Scholar] [CrossRef]
- Bach Pagès, A.; Peñuelas, J.; Clarà, J.; Llusià, J.; Campillo i López, F.; Maneja, R. How Should Forests Be Characterized in Regard to Human Health? Evidence from Existing Literature. Int. J. Environ. Res. Public Health 2020, 17, 1027. [Google Scholar] [CrossRef]
- Hansen, M.M.; Jones, R.; Tocchini, K. Shinrin-Yoku (Forest Bathing) and Nature Therapy: A State-of-the-Art Review. Int. J. Environ. Res. Public Health 2017, 14, 851. [Google Scholar] [CrossRef]
- Bang, K.S.; Lee, I.; Kim, S.; Lim, C.S.; Joh, H.K.; Park, B.J.; Song, M.K. The Effects of a Campus Forest-Walking Program on Undergraduate and Graduate Students’ Physical and Psychological Health. Int. J. Environ. Res. Public Health 2017, 14, 728. [Google Scholar] [CrossRef]
- Bielinis, E.; Takayama, N.; Boiko, S.; Omelan, A.; Bielinis, L. The effect of winter forest bathing on psychological relaxation of young Polish adults. Urban For. Urban Green. 2018, 29, 276–283. [Google Scholar] [CrossRef]
- Chun, M.H.; Chang, M.C.; Lee, S.J. The effects of forest therapy on depression and anxiety in patients with chronic stroke. Int. J. Neurosci. 2017, 127, 199–203. [Google Scholar] [CrossRef]
- Bielinis, E.; Janeczko, E.; Takayama, N.; Zawadzka, A.; Słupska, A.; Piętka, S.; Lipponen, M.; Bielinis, L. The effects of viewing a winter forest landscape with the ground and trees covered in snow on the psychological relaxation of young Finnish adults: A pilot study. PLoS ONE 2021, 16, e0244799. [Google Scholar] [CrossRef]
- Dolling, A.; Nilsson, H.; Lundell, Y. Stress recovery in forest or handicraft environments—An intervention study. Urban For. Urban Green. 2017, 27, 162–172. [Google Scholar] [CrossRef]
- Duncan, M.J.; Clarke, N.D.; Birch, S.L.; Tallis, J.; Hankey, J.; Bryant, E.; Eyre, E.L. The effect of green exercise on blood pressure, heart rate and mood state in primary school children. Int. J. Environ. Res. Public Health 2014, 11, 3678–3688. [Google Scholar] [CrossRef]
- Furuyashiki, A.; Tabuchi, K.; Norikoshi, K.; Kobayashi, T.; Oriyama, S. A comparative study of the physiological and psychological effects of forest bathing (Shinrin-yoku) on working age people with and without depressive tendencies. Environ. Health Prev. Med. 2019, 24, 1–11. [Google Scholar] [CrossRef] [PubMed]
- Gabrielsen, L.E.; Harper, N.J.; Fernee, C.R. What are constructive anxiety levels in wilderness therapy? An exploratory pilot study. Complement. Ther. Clin. Pract. 2019, 37, 51–57. [Google Scholar] [CrossRef] [PubMed]
- Lee, M.M.; Park, B.J. Effects of forest healing program on depression, stress and cortisol changes of cancer patients. J. People Plants Environ. 2020, 23, 245–254. [Google Scholar] [CrossRef]
- Hong, J.; Park, S.; An, M. Are Forest healing programs useful in promoting children’s emotional welfare? The Interpersonal relationships of children in foster care. Urban For. Urban Green. 2021, 59, 127034. [Google Scholar] [CrossRef]
- Lim, Y.-S.; Kim, J.; Khil, T.; Yi, J.; Kim, D.-J. Effects of the Forest Healing Program on Depression, Cognition, and the Autonomic Nervous System in the Elderly with Cognitive Decline. J. People Plants Environ. 2021, 24, 107–117. [Google Scholar] [CrossRef]
- Shin, W.S.; Shin, C.S.; Yeoun, P.S. The influence of forest therapy camp on depression in alcoholics. Environ. Health Prev. Med. 2012, 17, 73–76. [Google Scholar] [CrossRef]
- Song, C.; Ikei, H.; Kobayashi, M.; Miura, T.; Taue, M.; Kagawa, T.; Li, Q.; Kumeda, S.; Imai, M.; Miyazaki, Y. Effect of forest walking on autonomic nervous system activity in middle-aged hypertensive individuals: A pilot study. Int. J. Environ. Res. Public Health 2015, 12, 2687–2699. [Google Scholar] [CrossRef]
- Hassan, A.; Tao, J.; Li, G.; Jiang, M.; Aii, L.; Zhihui, J.; Zongfang, L.; Qibing, C. Effects of Walking in Bamboo Forest and City Environments on Brainwave Activity in Young Adults. Evid. Based Complement. Alternat. Med. 2018, 2018, 9653857. [Google Scholar] [CrossRef]
- Horiuchi, M.; Endo, J.; Akatsuka, S.; Hasegawa, T.; Yamamoto, E.; Uno, T.; Kikuchi, S. An effective strategy to reduce blood pressure after forest walking in middle-aged and aged people. J. Phys. Ther. Sci. 2015, 27, 3711–3716. [Google Scholar] [CrossRef]
- Jung, W.H.; Woo, J.M.; Ryu, J.S. Effect of a forest therapy program and the forest environment on female workers’ stress. Urban For. Urban Green. 2015, 14, 274–281. [Google Scholar] [CrossRef]
- Kang, H.; Chae, Y. Effects of Integrated Indirect Forest Experience on Emotion, Fatigue, Stress and Immune Function in Hemodialysis Patients. Int. J. Environ. Res. Public Health 2021, 18, 1701. [Google Scholar] [CrossRef]
- Kim, H.; Lee, Y.W.; Ju, H.J.; Jang, B.J.; Kim, Y.I. An Exploratory Study on the Effects of Forest Therapy on Sleep Quality in Patients with Gastrointestinal Tract Cancers. Int. J. Environ. Res. Public Health 2019, 16, 2449. [Google Scholar] [CrossRef]
- Lee, J.; Park, B.J.; Tsunetsugu, Y.; Ohira, T.; Kagawa, T.; Miyazaki, Y. Effect of forest bathing on physiological and psychological responses in young Japanese male subjects. Public Health 2011, 125, 93–100. [Google Scholar] [CrossRef]
- Lee, K.J.; Hur, J.; Yang, K.S.; Lee, M.K.; Lee, S.J. Acute Biophysical Responses and Psychological Effects of Different Types of Forests in Patients with Metabolic Syndrome. Environ. Behav. 2018, 50, 298–323. [Google Scholar] [CrossRef]
- Kim, J.; Sin, C.; Kim, D.; Kim, Y.; Lee, H. The stress-reducing effects of forest healing activities in maladjusted military force members. J. People Plants Environ. 2020, 23, 377–385. [Google Scholar] [CrossRef]
- Han, J.-W.; Choi, H.; Jeon, Y.-H.; Yoon, C.-H.; Woo, J.-M.; Kim, W. The effects of forest therapy on coping with chronic widespread pain: Physiological and psychological differences between participants in a forest therapy program and a control group. Int. J. Environ. Res. Public Health 2016, 13, 255. [Google Scholar] [CrossRef]
- Mao, G.X.; Lan, X.G.; Cao, Y.B.; Chen, Z.M.; He, Z.H.; Lv, Y.D.; Wang, Y.Z.; Hu, X.L.; Yan, J. Effects of short-term forest bathing on human health in a broad-leaved evergreen forest in Zhejiang Province, China. Biomed. Environ. Sci. 2012, 25, 317–324. [Google Scholar]
- Bang, K.-S.; Kim, S.; Song, M.K.; Kang, K.I.; Jeong, Y. The Effects of a Health Promotion Program Using Urban Forests and Nursing Student Mentors on the Perceived and Psychological Health of Elementary School Children in Vulnerable Populations. Int. J. Environ. Res. Public Health 2018, 15, 1977. [Google Scholar] [CrossRef]
- Kaplan, S. The restorative benefits of nature: Toward an integrative framework. J. Environ. Psychol. 1995, 15, 169–182. [Google Scholar] [CrossRef]
- Ulrich, R.S.; Simons, R.F.; Losito, B.D.; Fiorito, E.; Miles, M.A.; Zelson, M. Stress recovery during exposure to natural and urban environments. J. Environ. Psychol. 1991, 11, 201–230. [Google Scholar] [CrossRef]
- Appleton, J. The Experience of Landscape; Wiley Chichester: Chichester, UK, 1996. [Google Scholar]
- Ideno, Y.; Hayashi, K.; Abe, Y.; Ueda, K.; Iso, H.; Noda, M.; Lee, J.-S.; Suzuki, S. Blood pressure-lowering effect of Shinrin-yoku (Forest bathing): A systematic review and meta-analysis. BMC Complement. Altern. Med. 2017, 17, 409. [Google Scholar] [CrossRef] [PubMed]
- Corazon, S.S.; Sidenius, U.; Poulsen, D.V.; Gramkow, M.C.; Stigsdotter, U.K. Psycho-physiological stress recovery in outdoor nature-based interventions: A systematic review of the past eight years of research. Int. J. Environ. Res. Public Health 2019, 16, 1711. [Google Scholar] [CrossRef] [PubMed]
- Djernis, D.; Lerstrup, I.; Poulsen, D.; Stigsdotter, U.; Dahlgaard, J.; O’Toole, M. A Systematic Review and Meta-Analysis of Nature-Based Mindfulness: Effects of Moving Mindfulness Training into an Outdoor Natural Setting. Int. J. Environ. Res. Public Health 2019, 16, 3202. [Google Scholar] [CrossRef] [PubMed]
- Son, J.W.; Ha, S.Y.; Kim, J.J. A Study on Visitor Characteristics for Trail Program Development. J. Korean For. Soc. 2012, 101, 469–479. [Google Scholar]
- Oh, J.J.; Song, M.S.; Kim, S.M. Development and Validation of Korean Sleep Scale A. J. Korean Acad. Nurs. 1998, 28, 563–572. [Google Scholar] [CrossRef]
- Marino, M.; Li, Y.; Rueschman, M.N.; Winkelman, J.W.; Ellenbogen, J.; Solet, J.M.; Dulin, H.; Berkman, L.F.; Buxton, O.M. Measuring sleep: Accuracy, sensitivity, and specificity of wrist actigraphy compared to polysomnography. Sleep 2013, 36, 1747–1755. [Google Scholar] [CrossRef]
- Hellhammer, D.H.; Wüst, S.; Kudielka, B.M. Salivary cortisol as a biomarker in stress research. Psychoneuroendocrinology 2009, 34, 163–171. [Google Scholar] [CrossRef]
- Mohr, E.; Langbein, J.; Nürnberg, G. Heart rate variability: A noninvasive approach to measure stress in calves and cows. Physiol. Behav. 2002, 75, 251–259. [Google Scholar] [CrossRef]
- Temple, R.O.; Stern, R.A.; Latham, J.; Ruffolo, J.S.; Arruda, J.E.; Tremont, G. Assessment of mood state in dementia by use of the Visual Analog Mood Scales (VAMS). Am. J. Geriatr. Psychiatry 2004, 12, 527–530. [Google Scholar] [CrossRef]
- Ghassemzadeh, H.; Mojtabai, R.; Karamghadiri, N.; Ebrahimkhani, N. Psychometric properties of a Persian-language version of the Beck Depression Inventory-Second edition: BDI-II-PERSIAN. Depress. Anxiety 2005, 21, 185–192. [Google Scholar] [CrossRef]
- Stier-Jarmer, M.; Throner, V.; Kirschneck, M.; Immich, G.; Frisch, D.; Schuh, A. The psychological and physical effects of forests on human health: A systematic review of systematic reviews and meta-analyses. Int. J. Environ. Res. Public Health 2021, 18, 1770. [Google Scholar] [CrossRef]
- Saxena, S.; Van Ommeren, M.; Tang, K.; Armstrong, T. Mental health benefits of physical activity. J. Ment. Health 2005, 14, 445–451. [Google Scholar] [CrossRef]
- Farmer, M.E.; Locke, B.Z.; Mościcki, E.K.; Dannenberg, A.L.; Larson, D.B.; Radloff, L.S. Physical activity and depressive symptoms: The NHANES I Epidemiologic Follow-up Study. Am. J. Epidemiol. 1988, 128, 1340–1351. [Google Scholar] [CrossRef]
- Camacho, T.C.; Roberts, R.E.; Lazarus, N.B.; Kaplan, G.A.; Cohen, R.D. Physical activity and depression: Evidence from the Alameda County Study. Am. J. Epidemiol. 1991, 134, 220–231. [Google Scholar] [CrossRef]
- Mutrie, N. The relationship between physical activity and clinically defined depression. In Physical Activity and Psychological Well-Being; Routledge: London, UK, 2003; pp. 58–72. [Google Scholar]
- Lee, C.; Russell, A. Effects of physical activity on emotional well-being among older Australian women: Cross-sectional and longitudinal analyses. J. Psychosom. Res. 2003, 54, 155–160. [Google Scholar] [CrossRef]
- Sato, S.; Miao, T.; Oyama-Higa, M. Studies on five senses treatment. In Knowledge-Based Systems in Biomedicine and Computational Life Science; Springer: Berlin/Heidelberg, Germany, 2013; pp. 155–175. [Google Scholar]
- Chiesa, A.; Serretti, A. Mindfulness-based stress reduction for stress management in healthy people: A review and meta-analysis. J. Altern. Complement. Med. 2009, 15, 593–600. [Google Scholar] [CrossRef]
- Pascoe, M.C.; Thompson, D.R.; Ski, C.F. Meditation and endocrine health and wellbeing. Trends Endocrinol. Metab. 2020, 31, 469–477. [Google Scholar] [CrossRef]
| Natural Therapeutic Element | Number of Articles | Percentage |
|---|---|---|
| PM10 * (mg/m3) | 1 | 3.23 |
| Atmospheric pressure | 1 | 3.23 |
| Phytoncide (ng/m3) | 1 | 3.23 |
| Light (lx) | 3 | 9.68 |
| Negative ion (m−3) | 2 | 6.45 |
| Wind speed (m/s) | 5 | 16.13 |
| Sound (dB) | 5 | 16.13 |
| Weather | 8 | 25.81 |
| Weather—sunny | 4 | 12.9 |
| Weather—cloudy | 3 | 9.68 |
| Weather—fair | 2 | 6.45 |
| Vegetation | 26 | 83.87 |
| Mixed | 1 | 3.23 |
| Narrow-leaved forests | 13 | 41.94 |
| Broad-leaved forests | 23 | 74.19 |
| Characteristic of Program | Composition | Number of Articles * | Number of Session Lengths or Stay-Over Program |
|---|---|---|---|
| Session content | Walk | 22 | - |
| Session length | 10–20 min | 5 | 11 |
| 21–30 min | 1 | 2 | |
| 31–40 min | 1 | 2 | |
| 41–60 min | 0 | 1 | |
| 61–90 min | 5 | 12 | |
| 91–120 min | 1 | 9 | |
| Stay-over program | Day program | 4 | 16 |
| Stay-over program—1 day | 6 | 4 | |
| Session content | Physical activities | 15 | |
| Session length | 61–90 min | 3 | 11 |
| Session content | Meditation | 10 | |
| Session length | 10–20 min | 1 | 11 |
| 31–40 min | 2 | 3 | |
| Session content | Viewing | 9 | |
| Stay-over program | A day program | 1 | 16 |
| Stay-over program—2 days | 1 | 1 | |
| Stay-over program—3 days | 1 | 2 | |
| Session content | Five senses stimuli | 7 | |
| Session length | 10–20 min | 1 | 11 |
| 61–90 min | 1 | 10 | |
| Stay-over program | a-day program | 2 | 2 |
| Stay-over program—5 days | 1 | 2 | |
| Session content | Olfactory stimuli | 2 | |
| Session content | Others | 4 | |
| Session length | 41–60 min | 1 | 1 |
| 61–90 min | 2 | 11 | |
| 121–min | 1 | 2 | |
| Stay-over program | Day program | 1 | 16 |
| Stay-over program—2 days | 2 | 2 |
| Mental Health Target | Mental Tool | No. of Tools Used | No. of Significant Effects |
|---|---|---|---|
| ADHD | 1 | 0 | |
| Korean CASS-S | 1 | 0 | |
| Anxiety | 8 | 4 | |
| HADS | 2 | 1 | |
| POMS (Anxiety) | 1 | 1 | |
| STAI | 3 | 2 | |
| STAI-S | 2 | 0 | |
| Depression | 11 | 9 | |
| BDI | 5 | 5 | |
| CDI | 1 | 1 | |
| GeriatricDS | 1 | 1 | |
| HADS | 2 | 1 | |
| HAM-D17 | 1 | 1 | |
| KPDS-K6 | 1 | 0 | |
| Psychological status | 11 | 7 | |
| PANAS | 2 | 0 | |
| Perception_env | 1 | 1 | |
| ROS | 2 | 1 | |
| RSE | 1 | 1 | |
| SemanticDT | 2 | 2 | |
| SVS | 2 | 1 | |
| ZIPERS | 1 | 1 | |
| Self-reported health status | 7 | 4 | |
| CIS | 1 | 1 | |
| HPLP2 | 1 | 0 | |
| Q_healthcon | 1 | 0 | |
| Q_Symptom | 1 | 1 | |
| sf-36 | 1 | 1 | |
| SF-8 | 1 | 0 | |
| VAS-F | 1 | 1 | |
| Sentiment | 18 | 13 | |
| BRUMS | 1 | 1 | |
| POMS | 15 | 10 | |
| POMS-JAPAN | 1 | 1 | |
| PSQ | 1 | 1 | |
| Sleep | 25 | 8 | |
| Subjective assessment tool | ESS | 2 | 1 |
| InsomniaSI | 2 | 0 | |
| PSQI | 2 | 0 | |
| SSS | 2 | 1 | |
| STOP-Bang | 2 | 0 | |
| Objective assessment tool | Oxygen desaturation index (ODI) | 1 | 0 |
| PLMi | 1 | 1 | |
| REM sleep latency | 1 | 1 | |
| REM sleep latency | 1 | 0 | |
| Sleep architecture (N1–N3) | 1 | 0 | |
| Sleep efficiency | 3 | 2 | |
| Total time of sleep | 3 | 0 | |
| Wake after sleep onset | 2 | 2 | |
| Apnea hypopnea index (AHI) | 2 | 0 | |
| Social relationships | 4 | 2 | |
| Peer_relation | 1 | 0 | |
| RCS | 1 | 1 | |
| SASS | 1 | 1 | |
| SCQ | 1 | 0 | |
| Stress | 23 | 17 | |
| Subjective assessment tool | KPDS-K6 | 1 | 0 |
| PSS-Korean | 1 | 1 | |
| SRI-MF | 1 | 1 | |
| Stress-CT | 1 | 1 | |
| Tool_hemodialysis | 1 | 0 | |
| WSRI | 1 | 1 | |
| Objective assessment tool | Biological antioxidant potentials (BAPs) | 1 | 1 |
| Cortisol | 7 | 5 | |
| Heart rate variability (HRV) | 3 | 3 | |
| Malondialdehyde | 1 | 1 | |
| Reactive oxygen metabolite (d-ROM) | 1 | 0 | |
| Salivary amylase | 1 | 0 | |
| Job stress | MBI-GS | 1 | 1 |
| REQ | 1 | 1 | |
| SMBQ | 1 | 1 | |
| Total | 108 | 64 |
| Health Outcome Domain (No. of Articles) | Measure Target | Measure | No. of Measures | No. of Significant Effects |
|---|---|---|---|---|
| Cardiovascular system (18) | Blood pressure | Blood pressure | 11 | 6 |
| Sympathetic-to-parasympathetic system | Heart rate | 7 | 4 | |
| Heart rate variability | 7 | 4 | ||
| Cardiovascular disease risk factor | Blood Marker | |||
| Endothelin-1 (ET-1) | 1 | 1 | ||
| Homocysteine (Hcy) | 1 | 1 | ||
| Renin | 1 | 1 | ||
| Angiotensinogen (AGT) | 1 | 1 | ||
| Triglyceride | 1 | 0 | ||
| Cholesterol | 3 | 0 | ||
| Plasma ET-1(vasoconstrictor) | 1 | 0 | ||
| Platelet activation | 1 | 0 | ||
| T-SOD (superoxide dismutase) | 1 | 0 | ||
| MDA(lipid peroxidation in the serum) | 1 | 1 | ||
| Immune system (6) | Cytokine production | Blood Marker | ||
| Interleukin 6 | 3 | 2 | ||
| C-reactive protein (CRP) | 1 | 0 | ||
| Tumor necrosis factor (TNF-a) | 2 | 1 | ||
| Immunity | NK cell | 4 | 2 | |
| Total T cell | 1 | 0 | ||
| Total B cell | 1 | 1 | ||
| T helper lymphocyte | 1 | 0 | ||
| T Suppressor lymphocyte | 1 | 0 | ||
| CD4/CD8 | 1 | 0 | ||
| Endocrine system (1) | Hormonal change | Blood marker—adiponectin | 1 | 1 |
| Urine Marker | ||||
| Noradrenaline | 1 | 1 | ||
| Dopamine | 1 | 0 | ||
| Adrenaline | 1 | 0 | ||
| Behavioral (3) | Physical Activity | Activity Level | ||
| Physical activity | 1 | 0 | ||
| Energy expenditure | 1 | 1 | ||
| Pedometer | 1 | 1 | ||
| Nervous system (2) | Cognitive health | Brain waves (EEG) | 2 | 2 |
| Musculoskeletal (4) | Chronic pain | Health Status (self-reported) | ||
| Self-reported symptoms | 1 | 1 | ||
| Visual analog scale (VAS) | 2 | 1 | ||
| EuroQol 5D-3L VAS (EQ VAS) | 1 | 0 | ||
| Physical Pain and Activity | ||||
| Neck disability index (NDI) | 1 | 0 | ||
| EQ index | 2 | 1 | ||
| McGill pain questionnaire (MPQ) | 1 | 0 | ||
| Trigger points (TRPs) in the posterior neck region | 1 | 1 | ||
| Cervical range of motion (C-ROM) | 1 | 0 | ||
| Body Composition | Body composition | |||
| BMI | 1 | 0 | ||
| Percent of body fat | 1 | 1 | ||
| Skeletal muscle mass | 1 | 0 | ||
| Amount of muscle | 1 | 0 | ||
| Other (1) | Other | Peripheral oxygen saturation * | 1 | 1 |
| No. of Articles about Session Content | Physical Activities | Sense Activities | Meditation | Others | ||||
|---|---|---|---|---|---|---|---|---|
| Walking | Physical Activities | Viewing | Olfactory | Five Senses | ||||
| 22 | 15 | 9 | 2 | 7 | 10 | 5 | ||
| No. of articles about mental health (effect/total) | 20 | 13 | 8 | 2 | 7 | 10 | 4 | |
| ADHD | 0/1 | 0/1 | 0/1 | 0/0 | 0/0 | 0/1 | 0/0 | 0/1 |
| Anxiety | 4/8 | 3/5 | 2/5 | 1/2 | 0/1 | 2/2 | 2/3 | 0/1 |
| Depression | 8/10 | 7/8 | 5/6 | 1/1 | 0/1 | 5/5 | 4/6 | 2/2 |
| Psychological improvement | 6/7 | 3/4 | 2/2 | 3/4 | 0/0 | 2/2 | 1/1 | 1/1 |
| Self-report | 2/5 | 1/4 | 1/2 | 1/1 | 0/0 | 1/2 | 1/2 | 0/1 |
| Sentiment | 9/14 | 7/11 | 2/4 | 3/7 | 0/0 | 1/1 | 3/3 | 0/0 |
| Sleep | 2/3 | 1/2 | 2/3 | 0/1 | 1/1 | 1/1 | 2/3 | 0/0 |
| Social | 2/4 | 1/3 | 1/3 | 1/2 | 0/0 | 0/1 | 0/1 | 1/2 |
| Stress | 10/13 | 8/10 | 7/8 | 2/4 | 1/1 | 5/5 | 6/7 | 1/1 |
| No. of articles about physical health (effect/total) | 20 | 12 | 6 | 2 | 6 | 9 | 3 | |
| Cardiovascular system | 17/18 | 14/15 | 6/6 | 4/4 | 0/0 | 4/4 | 4/4 | 2/2 |
| Immune system | 3/6 | 3/5 | 1/3 | 0/0 | 0/0 | 0/2 | 1/3 | 1/1 |
| Endocrine system | 6/9 | 5/7 | 4/6 | 1/3 | 1/1 | 3/3 | 4/5 | 1/1 |
| Behavioral | 3/6 | 2/5 | 2/5 | 0/2 | 1/1 | 1/2 | 2/4 | 0/0 |
| Nervous system | 0/2 | 0/2 | 0/1 | 0/0 | 0/0 | 0/1 | 0/0 | 0/0 |
| Respiratory | 0/1 | 0/1 | 0/0 | 0/1 | 0/0 | 0/0 | 0/0 | 0/0 |
| Musculoskeletal | 3/4 | 3/4 | 2/3 | 0/1 | 0/0 | 0/0 | 1/2 | 1/1 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Chun, H.-r.; Choi, Y.-Y.; Cho, I.; Nam, H.-k.; Kim, G.; Park, S.; Cho, S.-i. Indicators of the Psychosocial and Physiological Effects of Forest Therapy: A Systematic Review. Forests 2023, 14, 1407. https://doi.org/10.3390/f14071407
Chun H-r, Choi Y-Y, Cho I, Nam H-k, Kim G, Park S, Cho S-i. Indicators of the Psychosocial and Physiological Effects of Forest Therapy: A Systematic Review. Forests. 2023; 14(7):1407. https://doi.org/10.3390/f14071407
Chicago/Turabian StyleChun, Hae-ryoung, Yoon-Young Choi, Inhyung Cho, Hee-kyoung Nam, Geonwoo Kim, Sujin Park, and Sung-il Cho. 2023. "Indicators of the Psychosocial and Physiological Effects of Forest Therapy: A Systematic Review" Forests 14, no. 7: 1407. https://doi.org/10.3390/f14071407
APA StyleChun, H.-r., Choi, Y.-Y., Cho, I., Nam, H.-k., Kim, G., Park, S., & Cho, S.-i. (2023). Indicators of the Psychosocial and Physiological Effects of Forest Therapy: A Systematic Review. Forests, 14(7), 1407. https://doi.org/10.3390/f14071407







