Systematic Review of the Quality of Stereolithographic Three-Dimensionally Printed Materials for Provisional Dental Restorations
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Design and Protocol Registration
2.2. Eligibility Criteria
2.3. Literature Search Strategy
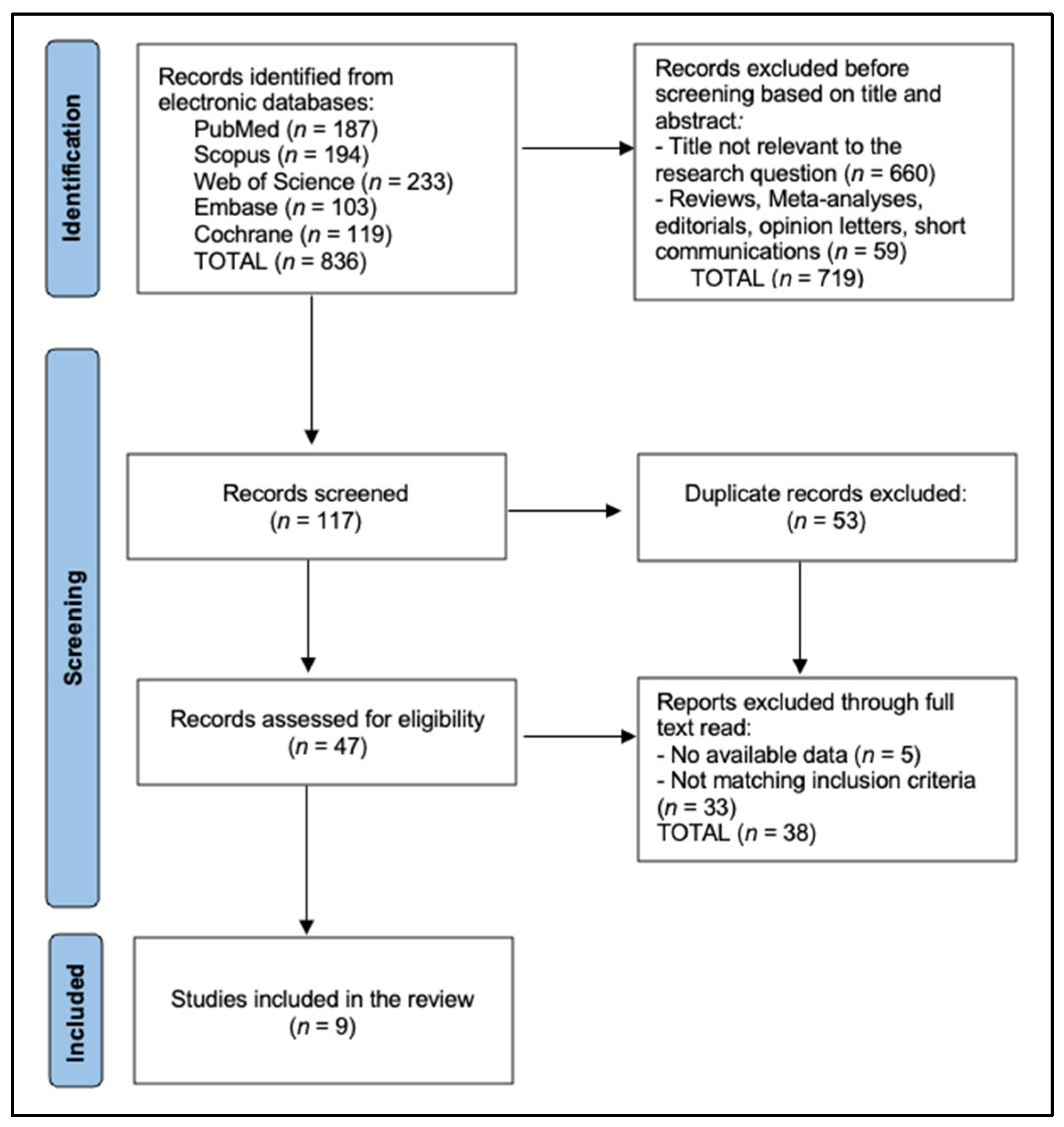
2.4. Study Selection and Data Extraction
3. Results
4. Discussion
4.1. Assessment of Findings and Additional Literature
4.2. Study Limitations
5. Conclusions
Author Contributions
Funding
Data Availability Statement
Conflicts of Interest
References
- Urkande, N.K.; Mankar, N.; Nikhade, P.P.; Chandak, M. Understanding the Complexities of Cast Post Retention: A Comprehensive Review of Influential Factors. Cureus 2023, 15, e51258. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Regish, K.M.; Sharma, D.; Prithviraj, D.R. Techniques of fabrication of provisional restoration: An overview. Int. J. Dent. 2011, 2011, 134659. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Juntavee, N.; Juntavee, A.; Srisontisuk, S. Color Appearance of Various Provisional Restorative Materials for Rehabilitation Upon Aging. Eur. J. Dent. 2023, 17, 1263–1274. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Ribera, O.K.; Mendes, J.M.; Mendes, J.; Barreiros, P.; Aroso, C.; Silva, A.S. Influence of Popular Beverages on the Fracture Resistance of Implant-Supported Bis-Acrylic Resin Provisional Crowns: An In Vitro Study. Polymers 2023, 15, 3411. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Pituru, S.M.; Greabu, M.; Totan, A.; Imre, M.; Pantea, M.; Spinu, T.; Tancu, A.M.C.; Popoviciu, N.O.; Stanescu, I.I.; Ionescu, E. A Review on the Biocompatibility of PMMA-Based Dental Materials for Interim Prosthetic Restorations with a Glimpse into their Modern Manufacturing Techniques. Materials 2020, 13, 2894. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Yeslam, H.E.; Freifrau von Maltzahn, N.; Nassar, H.M. Revolutionizing CAD/CAM-based restorative dental processes and materials with artificial intelligence: A concise narrative review. PeerJ 2024, 12, e17793. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Sajjad, A. Computer-assisted design/computer-assisted manufacturing systems: A revolution in restorative dentistry. J. Indian Prosthodont. Soc. 2016, 16, 96–99. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Hegedus, T.; Kreuter, P.; Kismarczi-Antalffy, A.A.; Demeter, T.; Banyai, D.; Vegh, A.; Geczi, Z.; Hermann, P.; Payer, M.; Zsembery, A.; et al. User Experience and Sustainability of 3D Printing in Dentistry. Int. J. Environ. Res. Public Health 2022, 19, 1921. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Lakkala, P.; Munnangi, S.R.; Bandari, S.; Repka, M. Additive manufacturing technologies with emphasis on stereolithography 3D printing in pharmaceutical and medical applications: A review. Int. J. Pharm. X 2023, 5, 100159. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Curti, C.; Kirby, D.J.; Russell, C.A. Stereolithography Apparatus Evolution: Enhancing Throughput and Efficiency of Pharmaceutical Formulation Development. Pharmaceutics 2021, 13, 616. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Quan, H.; Zhang, T.; Xu, H.; Luo, S.; Nie, J.; Zhu, X. Photo-curing 3D printing technique and its challenges. Bioact. Mater. 2020, 5, 110–115, Erratum in: Bioact. Mater. 2020, 6, 1789–1790. https://doi.org/10.1016/j.bioactmat.2020.11.009. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Astudillo-Rubio, D.; Delgado-Gaete, A.; Bellot-Arcís, C.; Montiel-Company, J.M.; Pascual-Moscardó, A.; Almerich-Silla, J.M. Mechanical properties of provisional dental materials: A systematic review and meta-analysis. PLoS ONE 2018, 13, e0193162, Erratum in PLoS ONE 2018, 13, e0196264.. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Alzahrani, S.J.; Hajjaj, M.S.; Azhari, A.A.; Ahmed, W.M.; Yeslam, H.E.; Carvalho, R.M. Mechanical Properties of Three-Dimensional Printed Provisional Resin Materials for Crown and Fixed Dental Prosthesis: A Systematic Review. Bioengineering 2023, 10, 663. [Google Scholar] [CrossRef]
- Saini, R.S.; Gurumurthy, V.; Quadri, S.A.; Bavabeedu, S.S.; Abdelaziz, K.M.; Okshah, A.; Alshadidi, A.A.F.; Yessayan, L.; Mosaddad, S.A.; Heboyan, A. The flexural strength of 3D-printed provisional restorations fabricated with different resins: A systematic review and meta-analysis. BMC Oral Health 2024, 24, 66. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Iftekar, S.F.; Aabid, A.; Amir, A.; Baig, M. Advancements and Limitations in 3D Printing Materials and Technologies: A Critical Review. Polymers 2023, 15, 2519. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Lassila, L.; Mangoush, E.; He, J.; Vallittu, P.K.; Garoushi, S. Effect of Post-Printing Conditions on the Mechanical and Optical Properties of 3D-Printed Dental Resin. Polymers 2024, 16, 1713. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Uzcategui, A.C.; Muralidharan, A.; Ferguson, V.L.; Bryant, S.J.; McLeod, R.R. Understanding and Improving Mechanical Properties in 3D printed Parts Using a Dual-Cure Acrylate-Based Resin for Stereolithography. Adv. Eng. Mater. 2018, 20, 1800876. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Della Bona, A.; Cantelli, V.; Britto, V.T.; Collares, K.F.; Stansbury, J.W. 3D printing restorative materials using a stereolithographic technique: A systematic review. Dent. Mater. 2021, 37, 336–350. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Parakaw, T.; Ruangsawasdi, N.; Dararat, P.; Phruksaniyom, C.; Srihirun, S.; Petchmedyai, P. Biocompatibility and biofilm formation on conventional and CAD/CAM provisional implant restorations. BMC Oral Health 2023, 23, 718. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Giti, R.; Dabiri, S.; Motamedifar, M.; Derafshi, R. Surface roughness, plaque accumulation, and cytotoxicity of provisional restorative materials fabricated by different methods. PLoS ONE 2021, 16, e0249551. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Engel, A.S.; Kranz, H.T.; Schneider, M.; Tietze, J.P.; Piwowarcyk, A.; Kuzius, T.; Arnold, W.; Naumova, E.A. Biofilm formation on different dental restorative materials in the oral cavity. BMC Oral Health 2020, 20, 162. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Unkovskiy, A.; Schmidt, F.; Beuer, F.; Li, P.; Spintzyk, S.; Kraemer Fernandez, P. Stereolithography vs. Direct Light Processing for Rapid Manufacturing of Complete Denture Bases: An In Vitro Accuracy Analysis. J. Clin. Med. 2021, 10, 1070. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Souza, A.L.C.; de Cruvinel Filho, J.L.O.; da Rocha, S.S. Flexural strength and Vickers hardness of milled and 3D-printed resins for provisional dental restorations. Braz. J. Oral Sci. 2023, 22, e238439. Available online: https://periodicos.sbu.unicamp.br/ojs/index.php/bjos/article/view/8668439 (accessed on 5 November 2024). [CrossRef]
- Won-Tak, C.; Jae-Won, C. Comparison analysis of fracture load and flexural strength of provisional restorative resins fabricated by different methods. J. Korean Acad. Prosthodont. 2019, 57, 225. [Google Scholar] [CrossRef]
- Simoneti, D.M.; Pereira-Cenci, T.; dos Santos, M.B.F. Comparison of material properties and biofilm formation in interim single crowns obtained by 3D printing and conventional methods. J. Prosthet. Dent. 2020, 127, 168–172. [Google Scholar] [CrossRef] [PubMed]
- Wadhwani, V.; Sivaswamy, V.; Rajaraman, V. Surface roughness and marginal adaptation of stereolithography versus digital light processing three-dimensional printed resins: An in-vitro study. J. Indian Prosthodont. Soc. 2022, 22, 377–381. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Nagata, K.; Muromachi, K.; Kouzai, Y.; Inaba, K.; Inoue, E.; Fuchigami, K.; Nihei, T.; Atsumi, M.; Kimoto, K.; Kawana, H. Fit accuracy of resin crown on a dental model fabricated using fused deposition modeling 3D printing and a polylactic acid filament. J. Prosthodont. Res. 2023, 67, 144–149. [Google Scholar] [CrossRef] [PubMed]
- Albahri, R.; Yoon, H.I.; Lee, J.D.; Yoon, S.; Lee, S.J. Shear bond strength of provisional repair materials bonded to 3D printed resin. J. Dent. Sci. 2021, 16, 261–267. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- de Castro, E.F.; Nima, G.; Rueggeberg, F.A.; Giannini, M. Effect of build orientation in accuracy, flexural modulus, flexural strength, and microhardness of 3D-Printed resins for provisional restorations. J. Mech. Behav. Biomed. Mater. 2022, 136, 105479. [Google Scholar] [CrossRef] [PubMed]
- Park, S.M.; Park, J.M.; Kim, S.K.; Heo, S.J.; Koak, J.Y. Flexural Strength of 3D-Printing Resin Materials for Provisional Fixed Dental Prostheses. Materials 2020, 13, 3970. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Sampaio, C.S.; Niemann, K.D.; Schweitzer, D.D.; Hirata, R.; Atria, P.J. Microcomputed tomography evaluation of cement film thickness of veneers and crowns made with conventional and 3D printed provisional materials. J. Esthet. Restor. Dent. 2020, 33, 487–495. [Google Scholar] [CrossRef]
- Gad, M.M.; Fouda, S.M. Factors affecting flexural strength of 3D-printed resins: A systematic review. J. Prosthodont. 2023, 32, 96–110. [Google Scholar] [CrossRef] [PubMed]
- de Gois Moreira, F.G.; da Silva, N.R.; Bezerra, M.G.P.G.; da Silva, S.E.G.; Butler, S.; Souza, K.B.; de Assunção ESouza, R.O. Influence of 3D printing system, postpolymerization and aging protocols on resin flexural strength and dimensional stability for printing occlusal splints, models and temporary restorations. Clin. Oral Investig. 2024, 28, 604. [Google Scholar] [CrossRef] [PubMed]
- Atwal, N.; Bhatnagar, D. Evaluating and Comparing Flexure Strength of Dental Models Printed Using Fused Deposition Modelling, Digital Light Processing, and Stereolithography Apparatus Printers. Cureus 2024, 16, e54312. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Sokola, P.; Ptáček, P.; Bafti, A.; Panžić, I.; Mandić, V.; Blahut, J.; Kalina, M. Comprehensive Study of Stereolithography and Digital Light Processing Printing of Zirconia Photosensitive Suspensions. Ceramics 2024, 7, 1616–1638. [Google Scholar] [CrossRef]
- Meissner, H.; Vacquier, M.; Kresse-Walczak, K.; Boening, K. Mechanical, optical and surface properties of 3D-printed and conventionally processed polyamide 12. Dent. Med. Probl. 2024, 61, 729–738. [Google Scholar] [CrossRef] [PubMed]
- Paradowska-Stolarz, A.; Wieckiewicz, M.; Kozakiewicz, M.; Jurczyszyn, K. Mechanical Properties, Fractal Dimension, and Texture Analysis of Selected 3D-Printed Resins Used in Dentistry That Underwent the Compression Test. Polymers 2023, 15, 1772. [Google Scholar] [CrossRef]
- Wajda, M.; Lis, J.; Kawala, B. Evaluating the accuracy of one-piece and three-piece 3D-printed indirect bonding transfer trays: An in vitro study. Dent. Med. Probl. 2024, 61, 901–908. [Google Scholar] [CrossRef] [PubMed]
- Etajuri, E.A.; Suliman, E.; Mahmood, W.A.A.; Ibrahim, N.; Buzayan, M.; Mohd, N.R. Deviation of dental implants placed using a novel 3D-printed surgical guide: An in vitro study. Dent. Med. Probl. 2020, 57, 359–362. [Google Scholar] [CrossRef] [PubMed]
| Database | Search Equation |
|---|---|
| PubMed | (“stereolithography”[Mesh] OR “stereolithography”[tiab] OR “SLA”[tiab] OR “3D printing”[tiab] OR “additive manufacturing”[tiab]) AND (“provisional dental restorations”[tiab] OR “temporary crowns”[tiab] OR “crowns”[tiab]) AND (“mechanical properties”[tiab] OR “flexural strength”[tiab] OR “hardness”[tiab]) |
| Scopus | TITLE-ABS-KEY(“stereolithography” OR “SLA” OR “3D printing” OR “additive manufacturing”) AND TITLE-ABS-KEY(“provisional dental restorations” OR “temporary crowns” OR “crowns”) AND TITLE-ABS-KEY(“mechanical properties” OR “flexural strength” OR “hardness”) |
| Web of Science | TS = (“stereolithography” OR “SLA” OR “3D printing” OR “additive manufacturing”) AND TS = (“provisional dental restorations” OR “temporary crowns” OR “crowns”) AND TS = (“mechanical properties” OR “flexural strength” OR “hardness”) |
| Embase | (’stereolithography’/exp OR stereolithography:ti,ab OR SLA:ti,ab OR ’3D printing’:ti,ab OR ’additive manufacturing’:ti,ab) AND (’provisional dental restorations’:ti,ab OR ’temporary crowns’:ti,ab OR crowns:ti,ab) AND (’mechanical properties’:ti,ab OR ’flexural strength’:ti,ab OR hardness:ti,ab) |
| Cochrane | (“stereolithography” OR “SLA” OR “3D printing” OR “additive manufacturing”) in Title, Abstract, and Keywords AND (“provisional dental restorations” OR “temporary crowns” OR “crowns”) in Title, Abstract, and Keywords AND (“mechanical properties” OR “flexural strength” OR “hardness”) in Title, Abstract, and Keywords |
| Study ID | Authors | Year | Country | Study Design | Materials Tested | Fabrication Methods | Sample Size | Mechanical Properties Assessed |
|---|---|---|---|---|---|---|---|---|
| 1 | Souza et al. [23] | 2023 | Brazil | In vitro | Evolux PMMA (milled resin), Cosmos Temp (SLA resin), Structur 2 SC (bis-acrylic resin, control) | Milling, SLA 3D printing, conventional | n = 12 (flexural strength), n = 9 (hardness) | Flexural strength, Vickers hardness |
| 2 | Cho and Choi [24] | 2019 | South Korea | In vitro | S3Z (SLA resin), D3Z and D3P (DLP resins), MIL (milled resin), CON (conventional self-cured resin) | SLA and DLP 3D printing, milling, conventional | n = 8 (fracture strength), n = 10 (flexural strength) | Fracture strength, flexural strength |
| 3 | Simoneti et al. [25] | 2020 | Brazil | In vitro | Acrylic resin, Bis-acryl resin, SLS resin, SLA resin | Conventional techniques, SLS and SLA 3D printing | n = 10 (flexural strength), n = 5 (hardness), n = 10 (surface roughness), n = 6 (biofilm formation) | Flexural strength, Vickers microhardness, surface roughness, biofilm formation |
| 4 | Wadhwani et al. [26] | 2022 | India | In vitro | SLA resin (Formlabs), DLP resin (Sprintray) | SLA and DLP 3D printing | n = 16 (8 per group) | Surface roughness, marginal adaptation |
| 5 | Nagata et al. [27] | 2023 | Japan | In vitro | PLA models (FDM), Resin models (SLA), Plaster models | FDM 3D printing, SLA 3D printing, Conventional casting | n = 5 per group | Marginal fit |
| 6 | Albahri et al. [28] | 2021 | USA/South Korea | In vitro | SLA resin repaired with PMMA, Bis-acrylic composite, Bis-GMA composite | SLA 3D printing, repair materials application | n = 15 per group | Shear bond strength |
| 7 | De Castro et al. [29] | 2022 | Brazil | In vitro | PMMA CAD/CAM (Control), Cosmos-SLA, Cosmos-DLP, PriZma-Bioprov, Nanolab | Milling (control), 3D printing (SLA, DLP) | n = 20 (bars), n = 10 (discs) | Accuracy, flexural modulus, flexural strength, microhardness |
| 8 | Park et al. [30] | 2020 | South Korea | In vitro | CV (Self-curing PMMA), SM (milled PMMA), DLP resin, SLA resin, FDM resin (PLA) | Conventional, milling, 3D printing (DLP, SLA, FDM) | n = 15 per group | Flexural strength |
| 9 | Sampaio et al. [31] | 2020 | Chile | In vitro | Acrylic resin, Bis-acrylic resin, PMMA CAD/CAM, 3D-printed resin | Conventional, CAD/CAM, 3D printing (SLA) | n = 6 per group (veneers), n = 6 per group (crowns) | Cement film thickness (via micro-CT) |
| Study ID | Authors | Materials Tested | Flexural Strength (Mean ± SD or Median, Units), MPa | Statistical Findings |
|---|---|---|---|---|
| 1 | Souza et al. [23] | Evolux PMMA (milled resin) | 111.76 | Significantly higher than Cosmos Temp and Structur 2 SC (p < 0.05) |
| Structur 2 SC (bis-acrylic resin) | 87.34 | Intermediate value | ||
| Cosmos Temp (SLA resin) | 56.83 | Significantly lower than Evolux PMMA and Structur 2 SC (p < 0.05) | ||
| 2 | Cho and Choi [24] | S3Z (SLA resin) | 116.08 ± 14.46 | Significantly higher than CON (p < 0.05) |
| D3Z (DLP resin) | 46.83 ± 3.44 | Significantly lower than CON (p < 0.05) | ||
| D3P (DLP resin) | 146.37 ± 7.52 | Significantly higher than CON (p < 0.05) | ||
| MIL (milled resin) | 168.57 ± 2.06 | Highest among all groups | ||
| CON (conventional self-cured resin) | 89.54 ± 6.99 | Reference group | ||
| 3 | Simoneti et al. [25] | Acrylic resin | 69.2 ± 8.8 | Intermediate value |
| Bis-acryl resin | 75.0 ± 8.2 | Intermediate value | ||
| SLA resin | 48.9 ± 1.2 | Lowest among groups (significantly lower) | ||
| SLS resin | 77.3 ± 3.1 | Highest among groups in this study | ||
| 7 | De Castro et al. [29] | Cosmos-SLA (3D-printed resin) | FS after 24h: 96.4 ± 6.5 (0°), 103.9 ± 3.2 (45°), 109.7 ± 5.1 (90°) | After 1 year, FS of 90°, Cosmos-SLA (120.5 ± 4.3 MPa) higher than Control; build orientation influenced FS |
| Cosmos-DLP (3D-printed resin) | FS decreased after 1 year; e.g., 88.4 ± 3.9 (0°) after 24 h to 73.1 ± 2.7 after 1 year | Build orientation influenced FS | ||
| PriZma-Bioprov (3D-printed resin) | FS after 1 year similar to Control; e.g., 102.3 ± 5.7 (90°) after 1 year | After 1 year, FS similar to control | ||
| Nanolab (3D-printed resin) | FS decreased after 1 year; e.g., 84.5 ± 4.0 (0°) after 24 h to 77.2 ± 3.5 after 1 year | FS lower than control | ||
| Control (PMMA CAD/CAM material) | FS after 24 h: 131.9 ± 4.8; After 1 year: 126.7 ± 3.9 | Control had highest FS at both time points | ||
| 8 | Park et al. [30] | CV (conventional self-curing PMMA) | Median 543 N (IQR 429–701 N) | Significantly lower than DLP and SLA groups (p < 0.001) |
| SM (milled PMMA) | Median 1232 N (IQR 1193–1258 N) | No significant difference compared to DLP (p = 0.481) | ||
| DLP (3D-printed resin) | Median 1189 N (IQR 1110–1283 N) | No significant difference compared to SM (p = 0.481) | ||
| SLA (3D-printed resin) | Median 1323 N (IQR 1245–1377 N) | Significantly higher than other groups (p < 0.001) | ||
| FDM (3D-printed resin) | No fracture observed (specimens only dented) | Not included in statistical analysis |
| Study ID | Authors | Materials Tested | Vickers Hardness (Mean ± SD, VHN) | Statistical Findings |
|---|---|---|---|---|
| 1 | Souza et al. [23] | Structur 2 SC (bis-acrylic resin) | 33.37 VHN | No significant difference compared to Evolux PMMA (p > 0.05) |
| Evolux PMMA (milled resin) | 29.11 VHN | No significant difference compared to Structur 2 SC (p > 0.05) | ||
| Cosmos Temp (SLA resin) | 10.90 VHN | Significantly lower than both Structur 2 SC and Evolux PMMA (p < 0.05) | ||
| 3 | Simoneti et al. [25] | Acrylic resin | 14.2 ± 2.6 kgf/mm2 | Highest hardness among groups |
| Bis-acryl resin | 10.7 ± 2.2 kgf/mm2 | Intermediate value | ||
| SLA resin | 8.4 ± 0.2 kgf/mm2 | Lowest among groups (significantly lower) | ||
| SLS resin | 10.3 ± 1.0 kgf/mm2 | Intermediate value | ||
| 7 | De Castro et al. [29] | Nanolab (3D-printed resin) | 31.8 ± 0.9 KHN (0° orientation) | Higher KHN than Control and other 3DRs |
| PriZma-Bioprov (3D-printed resin) | 25.2 ± 0.5 KHN (0° orientation) | Higher KHN than Cosmos-DLP and Cosmos-SLA | ||
| Cosmos-DLP (3D-printed resin) | 9.8 ± 0.4 KHN (0° orientation) | Lower KHN than Control and PriZma | ||
| Cosmos-SLA (3D-printed resin) | 8.1 ± 0.3 KHN (0° orientation) | Lowest KHN among 3DRs | ||
| Control (PMMA CAD/CAM material) | 23.1 ± 0.7 KHN | Lower KHN than Nanolab, higher than Cosmos-SLA and Cosmos-DLP |
| Study ID | Author | Properties Assessed | Results | Key Findings |
|---|---|---|---|---|
| 2 | Cho and Choi [24] | Fracture strength | S3Z (SLA resin): 987.50 ± 74.37 N; D3Z: 1020.99 ± 139.13 N; D3P: 1069.15 ± 153.23 N; MIL: 748.49 ± 135.61 N; CON: 678.48 ± 152.16 N | Additive manufacturing resins had comparable or higher fracture strength compared to milling and conventional methods |
| 3 | Simoneti et al. [25] | Elastic moduli | SLA resin: 513.3 ± 29.7 MPa; SLS resin: 452.4 ± 35.8 MPa; acrylic resin: 859.4 ± 46.3 MPa; bis-acryl resin: 997.3 ± 108.5 MPa | SLA and SLS resins had lower elastic moduli compared to conventional materials |
| Surface roughness (after polishing) | SLA resin: 0.7 ± 0.1 μm; bis-acryl resin: 0.7 ± 0.1 μm; acrylic resin: 0.9 ± 0.2 μm; SLS resin: 1.2 ± 0.3 μm | SLA resin had the lowest surface roughness, comparable to bis-acryl resin | ||
| Biofilm formation | Biofilm mass (OD570): SLA resin: 0.28 ± 0.03; SLS resin: 0.27 ± 0.03; acrylic resin: 0.29 ± 0.02; bis-acryl resin: 0.28 ± 0.03 | No significant differences among materials (p = 0.949) | ||
| 4 | Wadhwani et al. [26] | Surface roughness | SLA resin: Ra = 1.236 ± 0.136 μm; DLP resin: Ra = 1.932 ± 0.258 μm | SLA group had significantly lower surface roughness than DLP group (p < 0.05) |
| Marginal adaptation | SLA resin: marginal gap = 54.60 ± 14.22 μm; DLP resin: marginal gap = 84.58 ± 16.42 μm | SLA group showed significantly better marginal adaptation compared to DLP group (p < 0.005) | ||
| 5 | Nagata et al. [27] | Marginal fit | SLA models: mean gap = 50.4 ± 7.2 μm; plaster models: mean gap = 47.6 ± 6.8 μm; FDM models: mean gap = 68.9 ± 9.1 μm | No significant difference between SLA and plaster models except at one point; FDM models had larger gaps |
| 6 | Albahri et al. [28] | Shear bond strength | Group A (control): 253 ± 10 N; Group B (PMMA): 167 ± 29 N; Group C (bis-acryl composite): 174 ± 25 N; Group D (bis-GMA composite): 196 ± 37 N | Repaired SLA specimens had significantly lower shear bond strength than control (p < 0.001) |
| 7 | De Castro et al. [29] | Accuracy | Length percent error: Cosmos-SLA (90°): 0.02%; thickness percent error: Cosmos-SLA (90°): 0.12%; width percent error: Cosmos-SLA (90°): 0.08% | 90° orientation resulted in best overall accuracy for most 3DRs; Cosmos-SLA accuracy comparable to milled PMMA |
| Flexural modulus (FM) | Cosmos-SLA: FM after 24 h: 2.1 ± 0.1 GPa; after 1 year: 2.3 ± 0.1 GPa | FM of all 3DRs was lower than control (Control FM after 24 h: 3.6 ± 0.1 GPa) | ||
| SEM and EDS Analyses | Nanolab resin had irregular filler particles (~2–14 μm); Cosmos-SLA had few nanometric spherical particles | Nanolab presented irregular fillers affecting properties | ||
| 8 | Park et al. [30] | Fracture patterns | CV group: fractures occurred at connector area; SLA group: fractures at pontic area with small fragments; DLP group: fractures into several pieces | DLP and SLA materials provided adequate flexural strength; FDM specimens did not fracture but dented |
| Surface evaluation (FESEM) | DLP specimens showed stepped layers; SLA specimens had well-filled layers; FDM specimens had visible layer lines | Manufacturing method affects SLA surface characteristics | ||
| 9 | Sampaio et al. [31] | Cement film thickness | Veneers: bis-acrylic resin: 0.09 ± 0.04 mm; acrylic resin: 0.14 ± 0.03 mm; PMMA CAD/CAM: 0.18 ± 0.03 mm; 3D-printed resin: 0.32 ± 0.03 mm | SLA 3D-printed resin showed highest cement film thickness; veneers had smaller thickness than crowns |
| Crowns: PMMA CAD/CAM: 0.24 ± 0.04 mm; bis-acrylic resin: 0.28 ± 0.08 mm; acrylic resin: 0.34 ± 0.06 mm; 3D-printed resin: 0.62 ± 0.08 mm | SLA 3D-printed resin had significantly higher cement film thickness compared to other materials |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Danila, A.I.; Breban-Schwarzkopf, D.; Daescu, E.; Olariu, I.; Dinu, S. Systematic Review of the Quality of Stereolithographic Three-Dimensionally Printed Materials for Provisional Dental Restorations. Materials 2025, 18, 721. https://doi.org/10.3390/ma18030721
Danila AI, Breban-Schwarzkopf D, Daescu E, Olariu I, Dinu S. Systematic Review of the Quality of Stereolithographic Three-Dimensionally Printed Materials for Provisional Dental Restorations. Materials. 2025; 18(3):721. https://doi.org/10.3390/ma18030721
Chicago/Turabian StyleDanila, Alexandra Ioana, Daniel Breban-Schwarzkopf, Ecaterina Daescu, Iustin Olariu, and Stefania Dinu. 2025. "Systematic Review of the Quality of Stereolithographic Three-Dimensionally Printed Materials for Provisional Dental Restorations" Materials 18, no. 3: 721. https://doi.org/10.3390/ma18030721
APA StyleDanila, A. I., Breban-Schwarzkopf, D., Daescu, E., Olariu, I., & Dinu, S. (2025). Systematic Review of the Quality of Stereolithographic Three-Dimensionally Printed Materials for Provisional Dental Restorations. Materials, 18(3), 721. https://doi.org/10.3390/ma18030721







