The Influence of PBF-LB/M Part Forming Angle and Support Structure Parameters on the Distortion of Oral Stent
Abstract
1. Introduction
2. Methods
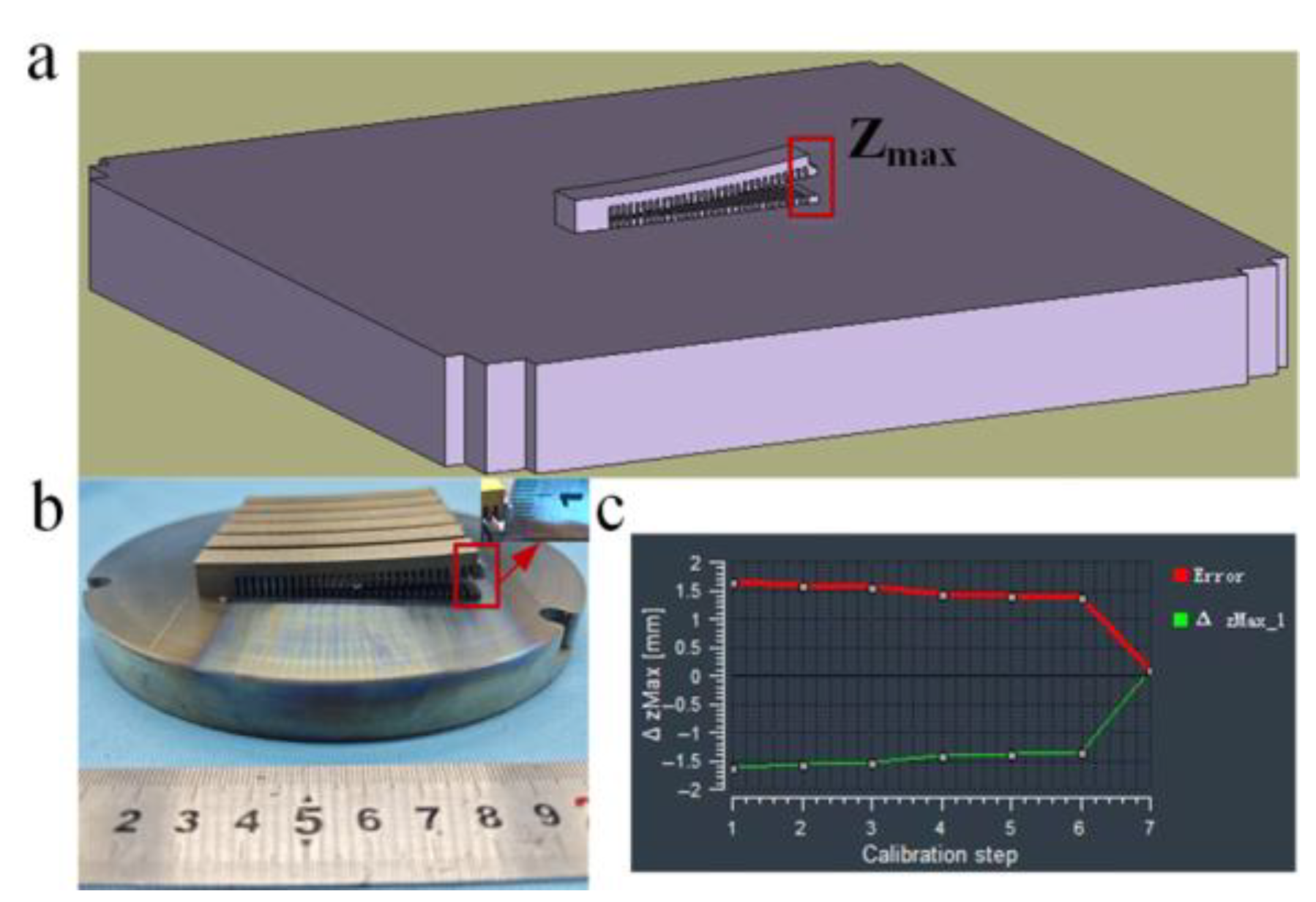
2.1. Experimental Equipment
- (1)
- A φ180 mm build envelope capable of producing 25 scaffolds per job, equipped with dual lasers;
- (2)
- Maximum scaffold dimensions of 60 mm with build height ≥60 mm;
- (3)
- Bidirectional powder spreading, enhancing production efficiency;
- (4)
- Top-fed powder delivery integrated with a recycling system, improving efficiency while enabling automated production line compatibility;
- (5)
- Optimized gas flow with a main flow zone removing spatter and smoke, and an upper flow zone protecting optical paths while suppressing plume recirculation;
- (6)
- Powder recycling system incorporating cyclonic separation and slag discharge mechanisms to increase powder reuse rate.
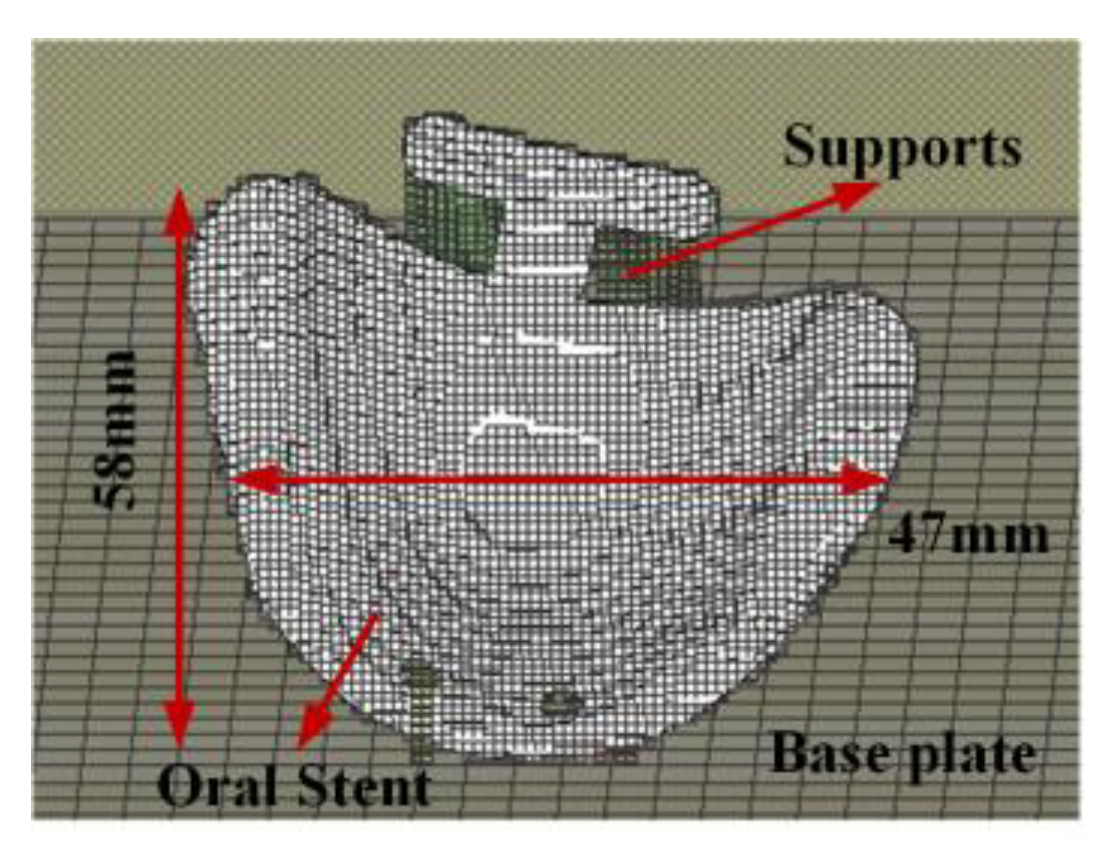
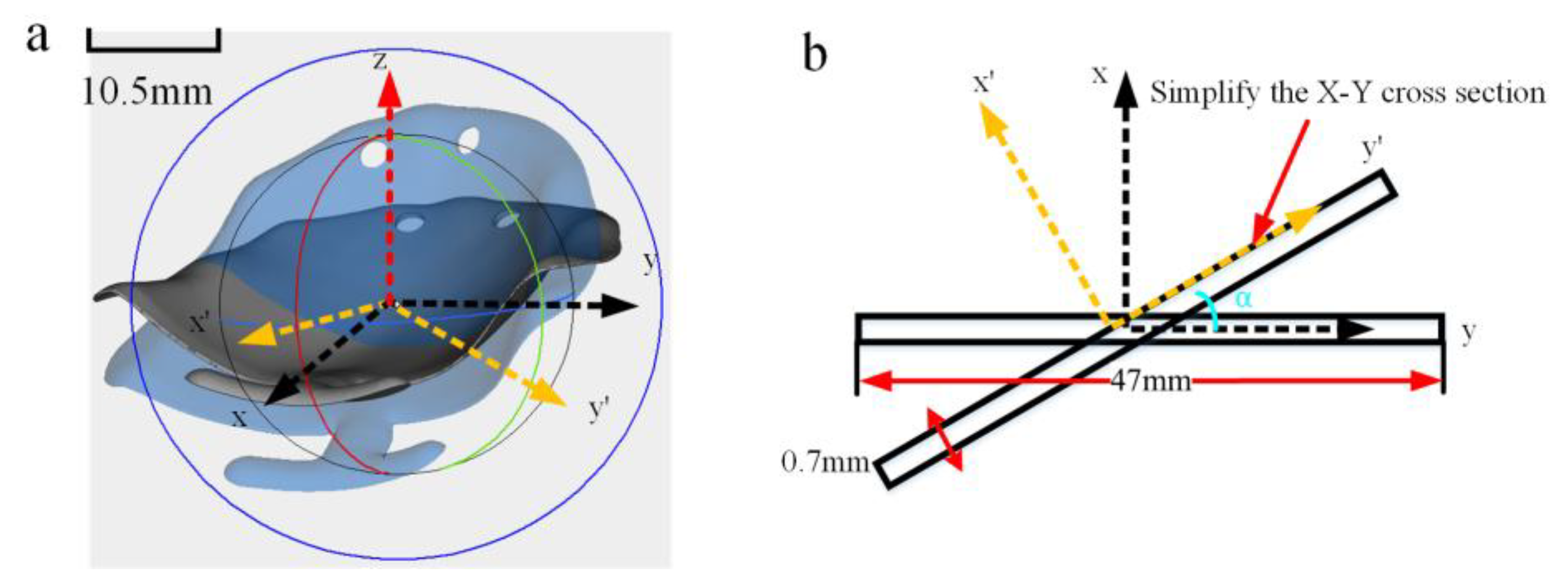
2.2. Simulation Model
2.2.1. Inherent Strain Theory
2.2.2. Simulation Model Setup
- (1)
- Mechanical assumption: The simulation is treated as a linear elastic static problem, with the material considered isotropic at the macroscopic scale;
- (2)
- Thermal assumption: The complex transient thermo-mechanical coupling process is simplified into an equivalent and calibratable “inherent strain” parameter, which comprehensively reflects the main effects of thermally induced plastic strain;
- (3)
- Geometric assumption: The part, supports, and substrate are all treated as continuous bodies, ignoring the microstructural details of the powder layer.
3. Results
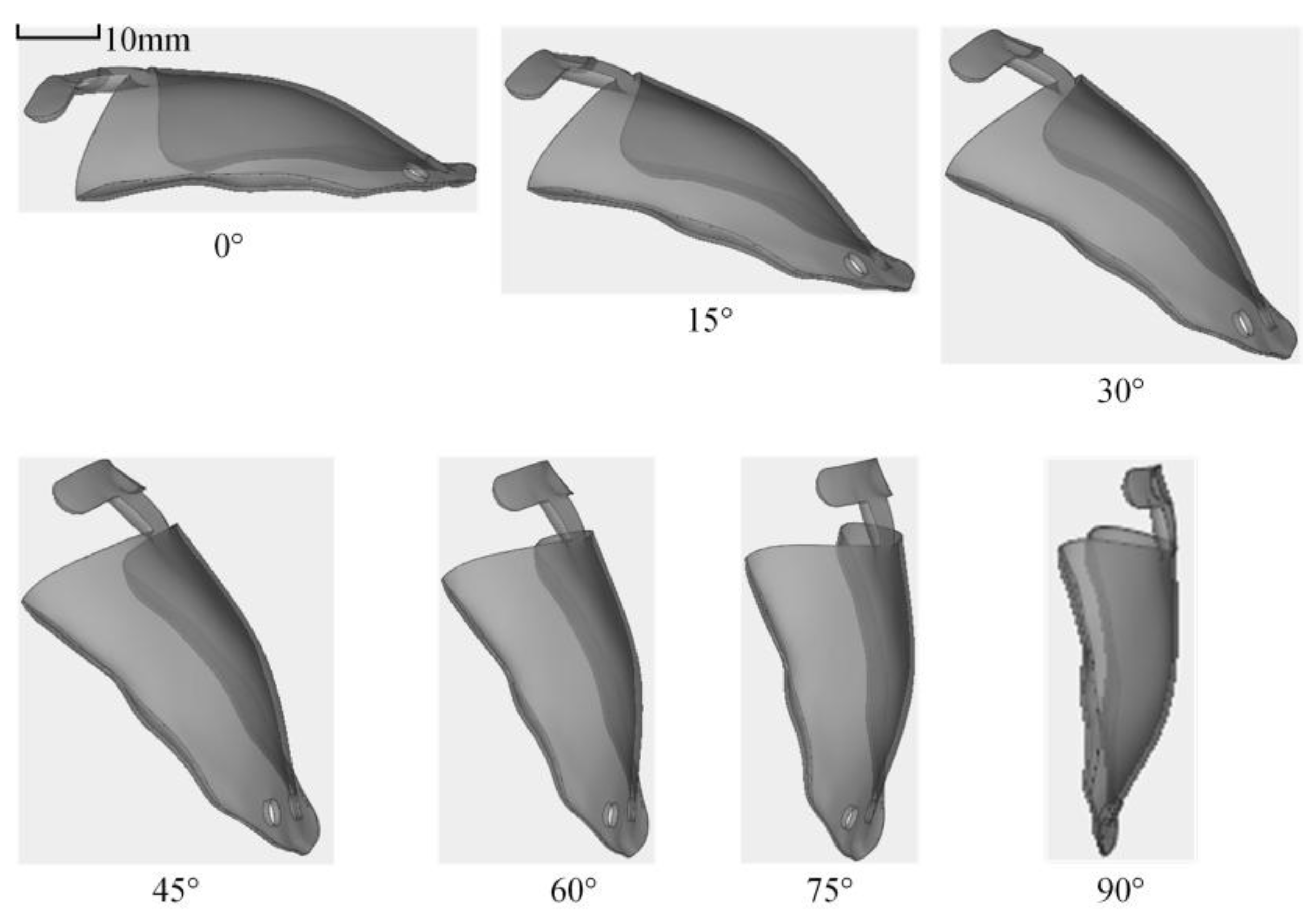
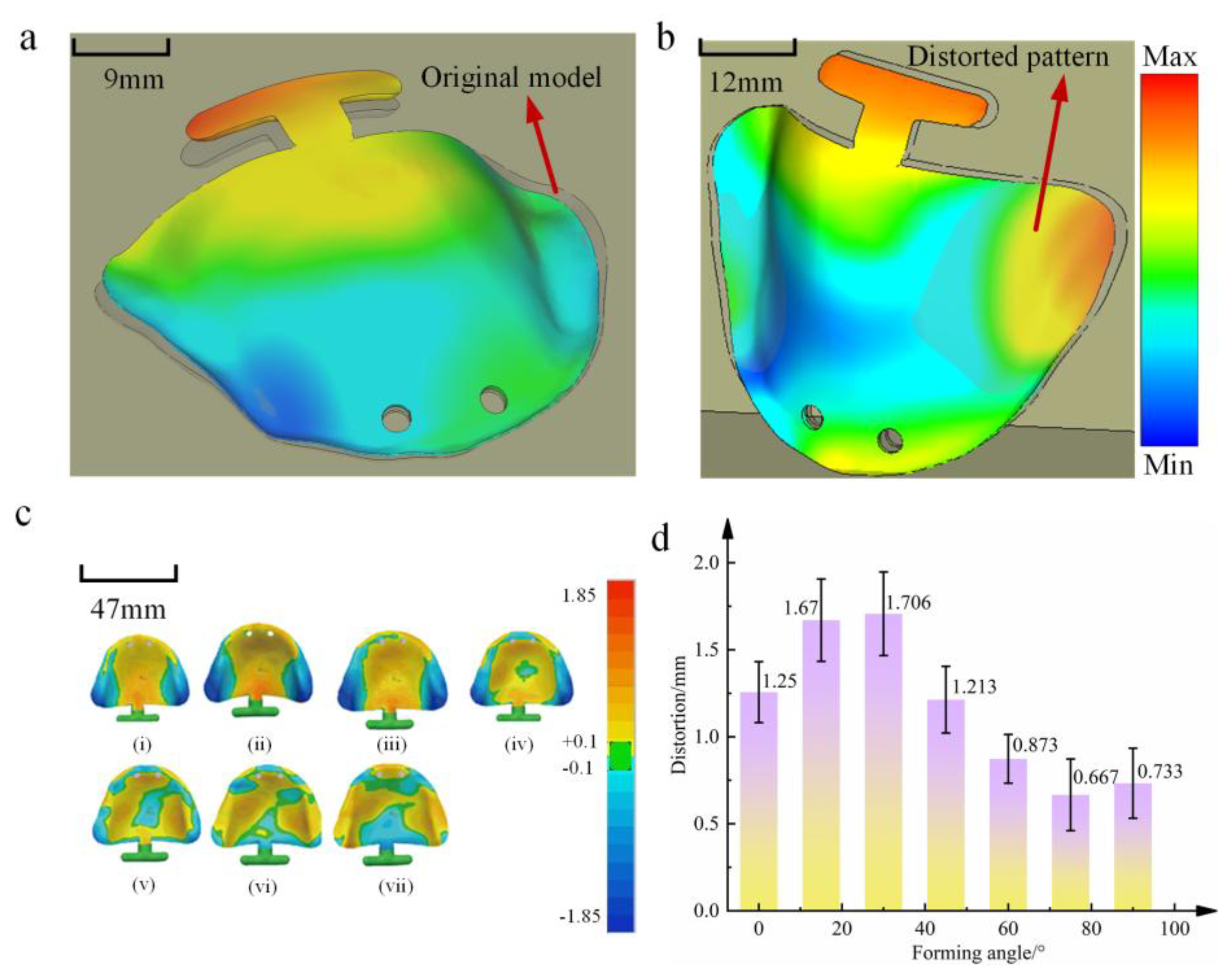
3.1. The Influence of Part Forming Angle on the Distortion of Oral Stents
3.1.1. Summary of Distortion Behavior in Oral Stent Based on Part Forming Angle
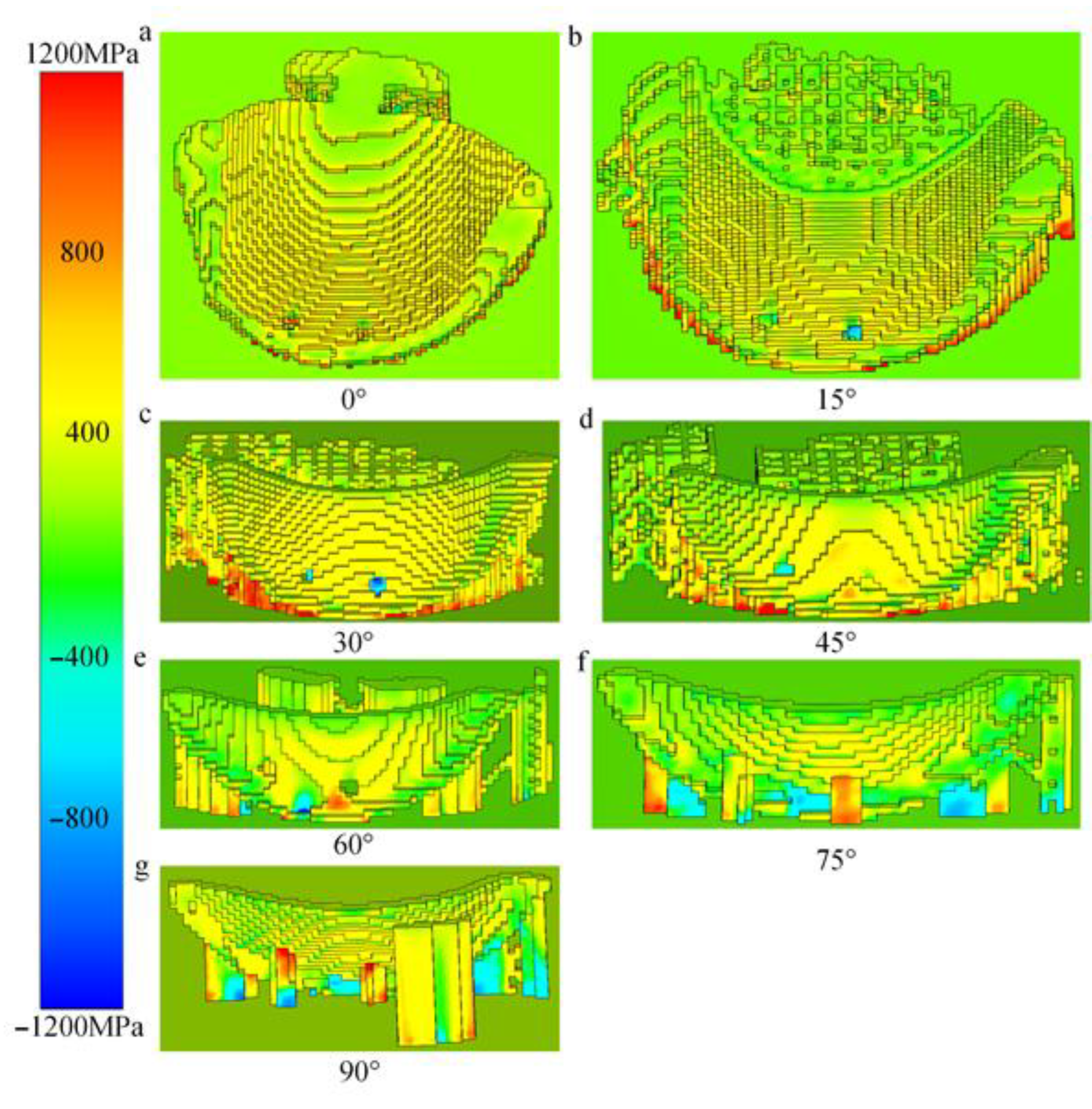
3.1.2. Analysis of Distortion Mechanisms in Oral Stents Based on Part Forming Angle
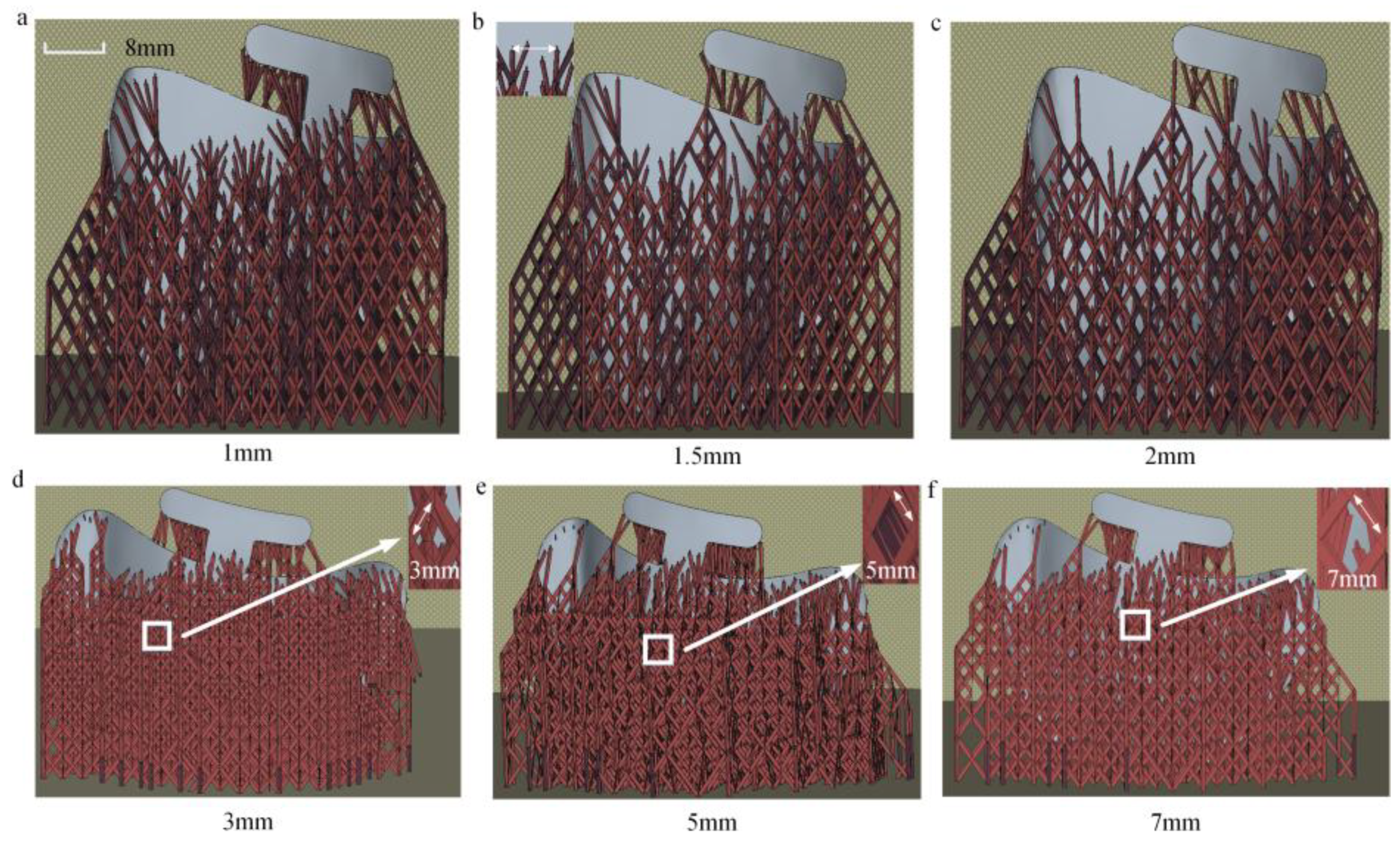
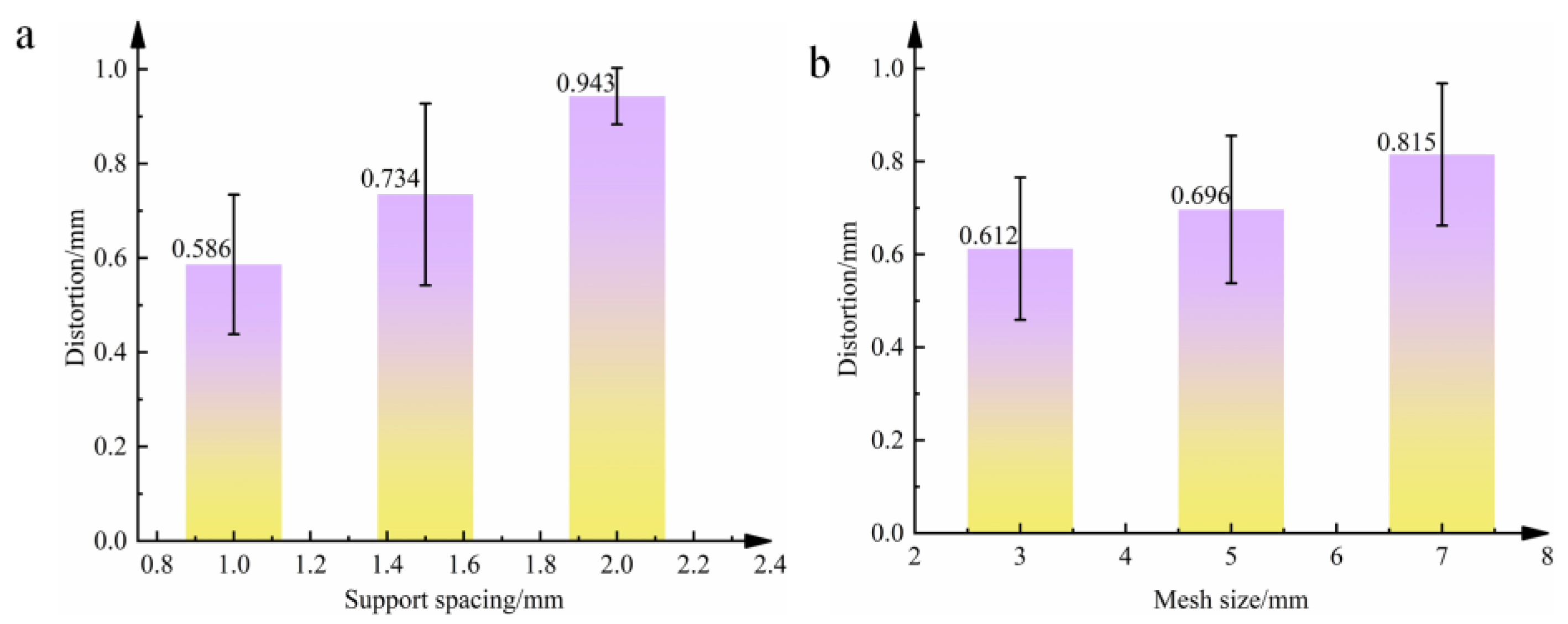
3.2. Influence of Support Structure Parameters on Distortion of Oral Stents
3.2.1. Summary of Distortion Behavior in Oral Stents Based on Support Structure Parameters
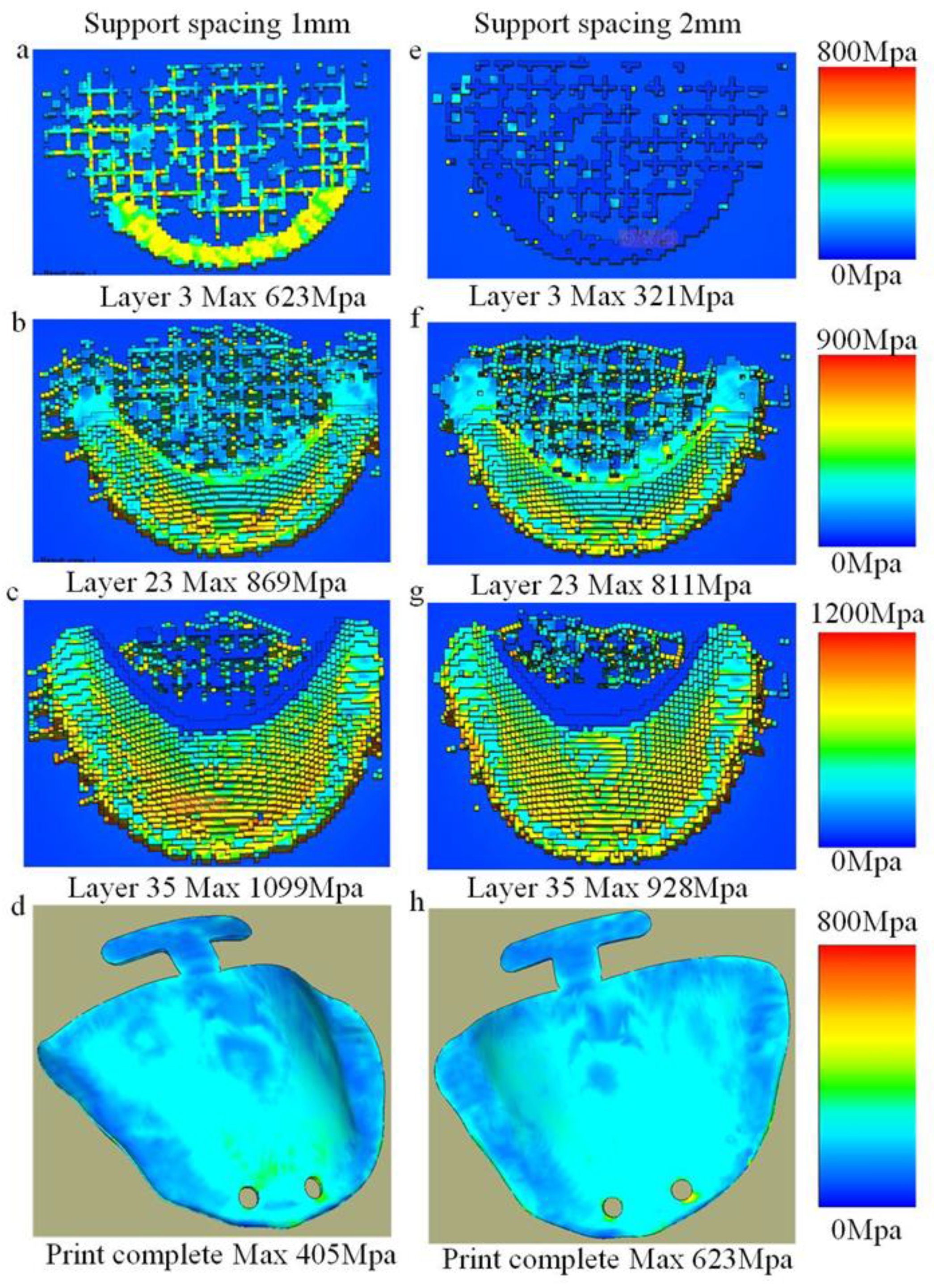
3.2.2. Analysis of Distortion Mechanisms in Oral Stents Based on Support Structure Parameters
4. Conclusions
- Effect of forming angle: As the forming angle increases from 0° to 90°, the maximum distortion magnitude of oral stents exhibits an initial increase followed by a decrease and subsequent increase. The peak distortion occurs at 30° (0.895 mm), while the minimum distortion is observed at 75° (0.615 mm).
- Distortion pattern by forming angle: When the forming angle is below 45°, distortion predominantly manifests as mid-section warping of the oral stent. Beyond 45°, the distortion pattern notably shifts to peripheral warping.
- The maximum distortion of oral stents demonstrates a direct proportional relationship with support spacing. Specifically, peak distortion (0.895 mm) occurs at 2 mm spacing. Similarly, distortion magnitude increases proportionally with support mesh size, reaching maximum distortion (0.881 mm) at 7 mm mesh dimensions.
- 4.
- The distortion variation induced by forming angle alterations primarily stems from thermal stress accumulation during printing, exhibiting direct proportionality to both the printed cross-sectional area and printing height. Notably, printing height constitutes the primary contributing factor to distortion at forming angles below 30°, whereas the printed cross-sectional area becomes the dominant influence beyond 30°.
- 5.
- Support spacing and mesh size mitigate distortion through enhanced structural rigidity and improved load transfer efficiency. This effect demonstrates an inversely proportional relationship with both parameters, indicating that diminished spacing and smaller mesh dimensions yield progressively more pronounced distortion reduction.
Author Contributions
Funding
Data Availability Statement
Conflicts of Interest
References
- Ahmed, N. Direct Metal Fabrication in Rapid Prototyping: A Review. J. Manuf. Process. 2019, 42, 167–191. [Google Scholar] [CrossRef]
- Korkmaz, M.E.; Gupta, M.K.; Waqar, S.; Kuntoğlu, M.; Krolczyk, G.M.; Maruda, R.W.; Pimenov, D.Y. A Short Review on Thermal Treatments of Titanium & Nickel Based Alloys Processed by Selective Laser Melting. J. Mater. Res. Technol. 2022, 16, 1090–1101. [Google Scholar] [CrossRef]
- Bian, P.; Jammal, A.; Xu, K.; Ye, F.; Zhao, N.; Song, Y. A Review of the Evolution of Residual Stresses in Additive Manufacturing during Selective Laser Melting Technology. Materials 2025, 18, 1707. [Google Scholar] [CrossRef]
- Liu, T.-S.; Chen, P.; Qiu, F.; Yang, H.-Y.; Jin, N.T.Y.; Chew, Y.; Wang, D.; Li, R.; Jiang, Q.-C.; Tan, C. Review on Laser Directed Energy Deposited Aluminum Alloys. Int. J. Extrem. Manuf. 2024, 6, 22004. [Google Scholar] [CrossRef]
- Javidrad, H.R.; Javidrad, F. Review of State-of-the-Art Research on the Design and Manufacturing of Support Structures for Powder-Bed Fusion Additive Manufacturing. Prog. Addit. Manuf. 2023, 8, 1517–1542. [Google Scholar] [CrossRef]
- Lawrence, J.E.; Lawrence, M.P.; Fezzaa, K.; Clark, S.J.; Crane, N.B. High-Speed X-Ray Imaging of Droplet-Powder Interaction in Binder Jet Additive Manufacturing. Addit. Manuf. 2024, 89, 104269. [Google Scholar] [CrossRef]
- Ebrahimi, F.; Xu, H.; Fuenmayor, E.; Major, I. Material Compatibility and Processing Challenges in Droplet Deposition Modelling Additive Manufacturing: A Study on Pharmaceutical Excipients Polyvinylpyrrolidone/vinyl Acetate (PVP/VA) and Polycaprolactone (PCL). Eur. J. Pharm. Sci. 2024, 200, 106850. [Google Scholar] [CrossRef]
- Yang, Y.; Jiang, R.; Han, C.; Chen, J.; Li, H.; Wang, Y.; Tang, J.; Zhou, H.; Hu, W.; Zheng, B.; et al. Frontiers in Laser Additive Manufacturing Technology. Addit. Manuf. Front. 2024, 3, 200160. [Google Scholar] [CrossRef]
- Lee, S.; Ng, J.; Cher, S.; Villalon, J.; Chan, T. Evaluation of Different Dental Materials in the Fabrication of Oral Positioning Stents for Head and Neck Radiotherapy. J. Med. Imaging Radiat. Sci. 2023, 54, S5. [Google Scholar] [CrossRef]
- Ong, J.E.X. How to Restore Lower Complete Edentulism with Implant-Supported Overdentures: An Evidence-Based Clinical Management. Br. Dent. J. 2024, 237, 773–777. [Google Scholar] [CrossRef]
- Elshazly, T.M.; Bourauel, C.; Aldesoki, M.; Ghoneima, A.; Abuzayda, M.; Talaat, W.; Talaat, S.; Keilig, L. Computer-Aided Finite Element Model for Biomechanical Analysis of Orthodontic Aligners. Clin. Oral Investig. 2023, 27, 115–124. [Google Scholar] [CrossRef]
- Mundee, T.; Jongwannasiri, C.; Fuangrod, T. Design of 3D-Printed Universal Oral Stent for Tongue Immobilization in Head and Neck Radiotherapy. Biomed. Phys. Eng. Express 2022, 9, 15011. [Google Scholar] [CrossRef]
- Nematollahi, M.; Saghaian, S.E.; Safaei, K.; Bayati, P.; Bassani, P.; Biffi, C.; Tuissi, A.; Karaca, H.; Elahinia, M. Building Orientation-Structure-Property in Laser Powder Bed Fusion of NiTi Shape Memory Alloy. J. Alloys Compd. 2021, 873, 159791. [Google Scholar] [CrossRef]
- Ni, C.; Shi, Y.; Zhang, W.; Wang, W.; Liu, C. Effects of Laying Angles on Stainless Steel Fabricated by Selective Laser Melting. Mater. Sci. Technol. 2024, 40, 821–828. [Google Scholar] [CrossRef]
- Zhou, Y.; Ning, F. Build Orientation Effect on Geometric Performance of Curved-Surface 316L Stainless Steel Parts Fabricated by Selective Laser Melting. J. Manuf. Sci. Eng. 2020, 142, 121002. [Google Scholar] [CrossRef]
- Cao, Q.; Zhang, J.; Chang, S.; Fuh, J.Y.H.; Wang, H. The Effect of Support Structures on Maraging Steel MS1 Parts Fabricated by Selective Laser Melting at Different Building Angles. Rapid Prototyp. J. 2020, 26, 1465–1476. [Google Scholar] [CrossRef]
- Wang, D.; Yang, Y.; Liu, R.; Xiao, D.; Sun, J. Study on the Designing Rules and Processability of Porous Structure Based on Selective Laser Melting (SLM). J. Mater. Process. Technol. 2013, 213, 1734–1742. [Google Scholar] [CrossRef]
- Zhang, G.; Yang, Y.; Zhang, Z.; Song, C.; Wang, A.; Yu, J. Optimization of Support Structure for Laser selective melting forming Parts. Chin. J. Lasers 2016, 43, 59–66. [Google Scholar]
- Zhang, H. Research on Support Design of Selected Laser Melting Forming Part. Master’s Thesis, Zhejiang University of Technology, Hangzhou, China, 2018. [Google Scholar]
- Wu, S. Structural Lightweight Design and Support Addition Based on Selective Laser Melting Technology. Master’s Thesis, Jiangsu University of Science and Technology, Zhenjiang, China, 2020. [Google Scholar]
- Dimopoulos, A.; Salimi, M.; Gan, T.-H.; Chatzakos, P. Support Structures Optimisation for High-Quality Metal Additive Manufacturing with Laser Powder Bed Fusion: A Numerical Simulation Study. Materials 2023, 16, 7164. [Google Scholar] [CrossRef]
- Khobzi, A.; Mehr, F.F.; Cockcroft, S.; Maijer, D.; Sing, S.L.; Yeong, W.Y. The Role of Block-Type Support Structure Design on the Thermal Field and Deformation in Components Fabricated by Laser Powder Bed Fusion. Addit. Manuf. 2022, 51, 102644. [Google Scholar] [CrossRef]
- Sulaiman, M.R.; Yusof, F. Effect of Support Structure Design Toward Residual Stress of Part Build using Selective Laser Melting: Auswirkung Des Stützstrukturdesigns Auf Die Restspannung Des Bauteilaufbaus Unter Verwendung Des Selektiven Laserstrahlschmelzens. Mater. Werkst. 2023, 54, 1138–1147. [Google Scholar] [CrossRef]
- Yang, E.; Leary, M.; Lozanovski, B.; Downing, D.; Mazur, M.; Sarker, A.; Khorasani, A.; Jones, A.; Maconachie, T.; Bateman, S.; et al. Effect of Geometry on the Mechanical Properties of Ti-6Al-4V Gyroid Structures Fabricated Via SLM: A Numerical Study. Mater. Des. 2019, 184, 108165. [Google Scholar] [CrossRef]
- Tian, Y.; He, J.; Ren, H.; Zha, X.; Lin, K.; Zhou, M.; Xiong, Y. Effect of Process and Geometric Parameters on Residual Distortion of Ti-6Al-4V Body-Centered Cubic Lattice Structures in Laser Powder Bed Fusion. Addit. Manuf. Front. 2024, 3, 200170. [Google Scholar] [CrossRef]
- Zhao, Y.; Kan, X.; Chu, X.; Sun, H.; Zhao, Z.; Sun, J.; Wang, H. Twinning behavior in deformation of SLM 316L stainless steel. Mater. Res. Express 2022, 9, 96502. [Google Scholar] [CrossRef]
- Morgan, D.; Agba, E.; Hill, C. Support Structure Development and Initial Results for Metal Powder Bed Fusion Additive Manufacturing. Procedia Manuf. 2017, 10, 819–830. [Google Scholar] [CrossRef]
- Zhang, J.; Cao, Q.; Lu, W. A review on design and removal of support structures in metal additive manufacturing. Mater. Today Proc. 2022, 70, 407–411. [Google Scholar] [CrossRef]
- Bobbio, L.D.; Qin, S.; Dunbar, A.; Michaleris, P.; Beese, A.M. Characterization of the strength of support structures used in powder bed fusion additive manufacturing of Ti-6Al-4V. Addit. Manuf. 2017, 14, 60–68. [Google Scholar] [CrossRef]
- Jalali, M.; Mohammadi, K.; Movahhedy, M.R.; Karimi, F.; Sadrnezhaad, S.K.; Chernyshikhin, S.V.; Shishkovsky, I.V. SLM Additive Manufacturing of NiTi Porous Implants: A Review of Constitutive Models, Finite Element Simulations, Manufacturing, Heat Treatment, Mechanical, and Biomedical Studies. Met. Mater. Int. 2023, 29, 2458–2491. [Google Scholar] [CrossRef]
- Cao, Q.; Shi, Z.; Bai, Y.; Zhang, J. A novel method to improve the removability of cone support structures in selective laser melting of 316L stainless steel. J. Alloys Compd. 2021, 854, 157133. [Google Scholar] [CrossRef]
- Xiao, Y.; Zhang, C.; Cai, J. Comparative study on internal quality of titanium and titanium alloy denture scaffolds with different processes. China Med. Device Inf. 2022, 28, 26–28. [Google Scholar]
- Rakesh, C.S.; Priyanka, N.; Jayaganthan, R.; Vasa, N.J. Effect of build atmosphere on the mechanical properties of AlSi10Mg produced by selective laser melting. Mater. Today Proc. 2018, 5, 17231–17238. [Google Scholar] [CrossRef]
- Lin, H. Process Simulation and Technology Research of Laser Selective Melting Forming Overhang Structure. Master’s Thesis, Nanjing University of Aeronautics and Astronautics, Nanjing, China, 2018. [Google Scholar]
- Yan, P.; Bai, J.; Yuan, Z.; Wang, S.; Ma, R.; Zheng, J. Constitutive Equation and Hot Deformation Behavior of SLM-GH3536 Alloy. J. Mater. Eng. Perform. 2023, 32, 4567–4578. [Google Scholar] [CrossRef]
- Agyapong, J.; Czekanski, A.; Yiadom, S.B. Microstructural evolution and high strain rate deformation response of SLM-printed CoCrFeMnNi after annealing and deep-cryogenic treatment. Mater. Charact. 2024, 218, 114506. [Google Scholar] [CrossRef]
- Li, W.; Meng, L.; Wang, S.; Zhang, H.; Niu, X.; Lu, H. Plastic deformation behavior and strengthening mechanism of SLM 316L reinforced by micro-TiC particles. Mater. Sci. Eng. 2023, 884, 145557. [Google Scholar] [CrossRef]
- Seitz, G.; Bantle, P.; Biegler, M.; Elsner, B.A.M.; Rethmeier, M. An Inherent Strain Method using Progressive Element Activation for Fast Distortion Calculation in Directed Energy Deposition. Metals 2024, 14, 1338. [Google Scholar] [CrossRef]
- Mahmood, M.A.; Khraisheh, M.; Popescu, A.C.; Liou, F. Processing Windows for Al-357 by LPBF Process: A Novel Framework Integrating FEM Simulation and Machine Learning with Empirical Testing. Rapid Prototyp. J. 2024, 30, 1846–1858. [Google Scholar] [CrossRef]
- Wiegold, T.; Klinge, S. Numerical simulation of cyclic deformation behavior of SLM-manufactured aluminum alloys. Comput. Mater. Sci. 2021, 189, 110213. [Google Scholar] [CrossRef]
- Kale, A.B.; Alluri, S. The deformation and fracture behavior of 316L SS fabricated by SLM under mini V-bending test. Int. J. Mech. Sci. 2021, 196, 106292. [Google Scholar] [CrossRef]
- Zhang, X.; Wang, J.; Kang, J. The dynamic arch bending mechanism of flat bridge structure of AlSi10Mg during SLM process. Mater. Des. 2020, 188, 108469. [Google Scholar] [CrossRef]
- Li, L.; Pan, T.; Zhang, X.; Chen, Y.; Cui, W.; Yan, L.; Liou, F. Deformations and stresses prediction of cantilever structures fabricated by selective laser melting process. Rapid Prototyp. J. 2021, 27, 453–464. [Google Scholar] [CrossRef]
- Uddin, S.Z. Laser Powder Bed Fusion and in Situ Process Monitoring of Tall Thin-Walled Structures. Doctoral Dissertation, Carnegie Mellon University, Pittsburgh, PA, USA, 2022. [Google Scholar]
- Tangestani, R.; Chakraborty, A.; Sabiston, T.; Yuan, L.; Martin, E. Buckling Mechanism Simulation for Thin-Wall Components made by Laser Powder Bed Fusion. Key Eng. Mater. 2023, 964, 1–6. [Google Scholar] [CrossRef]
- Shu, D. Mechanical Properties of Engineering Materials, 2nd ed.; Mechanical Industry Press: New York, NY, USA, 2007. [Google Scholar]
- Wang, T.; Zhang, J.; Zhou, Y. Calculation on Bending Stiffness of RC Short Beam Strengthened by CFRP. Adv. Civ. Eng. 2020, 2020, 1–13. [Google Scholar] [CrossRef]
- Jabaraj, D.J.; Jaafar, M.S. Theoretical Calculation of Bending Stiffness of Alveolar Wall. J. Membr. Biol. 2013, 246, 981–984. [Google Scholar] [CrossRef]

| Process Parameters | Value |
|---|---|
| Laser power/W | 160 |
| Interlayer corner/° | 67 |
| Scanning speed/mm/s | 1250 |
| Scanning spacing/mm | 0.1 |
| Layer thickness/um | 30 |
| Items | Supporting Generated Critical Angle (°) | Support Spacing (mm) | Support Mesh Size (mm2) |
|---|---|---|---|
| 1 | 75 | 1.0 | 3 |
| 2 | 75 | 1.5 | 5 |
| 3 | 75 | 2.0 | 7 |
| Parameters | Value |
|---|---|
| Specific heat c (J·Kg−1·°C−1) | Temperature dependent |
| Thermal conductivity h (W·m−1·°C−1) | Temperature dependent |
| Coefficient of thermal expansion λ (°C−1) | Temperature dependent |
| Ambient temperature (°C) | 20 |
| Bulk density ρTA15 (g/cm3) | 4.450 |
| Radiation emissivity Ɛ | 0.36 |
| Poisson’s ratio μ | 0.32 |
| Absorptivity Ae | 0.7 |
| T (°C) | Specific Heat (J·kg−1·°C−1) | Thermal Conductivity (W·m−1·°C−1) | Coefficient of Thermal Expansion (°C−1) |
|---|---|---|---|
| 100 | 545 | 8.8 | 8.9 |
| 200 | 587 | 10.2 | 9.0 |
| 300 | 628 | 10.9 | 9.2 |
| 400 | 670 | 12.2 | 9.7 |
| 500 | 712 | 13.8 | 10.0 |
| 600 | 755 | 15.1 | 10.4 |
| 700 | 838 | 16.8 | 10.9 |
| 800 | 880 | 18.0 | 10.9 |
| 900 | 922 | 19.7 | 10.9 |
| Forming Angle (°) | I (m4) |
|---|---|
| 0 | 2.42 × 10−8 |
| 15 | 2.25 × 10−8 |
| 30 | 1.8154 × 10−8 |
| 45 | 1.2105 × 10−8 |
| 60 | 0.605 × 10−8 |
| 75 | 0.1475 × 10−8 |
| 90 | 5.373 × 10−12 |
| Forming Angle (°) | Released Stress/MPa |
|---|---|
| 0 | 1416 |
| 15 | 1655 |
| 30 | 2625 |
| 45 | 1065 |
| 60 | 936 |
| 75 | 730 |
| 90 | 820 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Liu, Y.; Xie, D.; Liu, Y.; Tian, Z.; Shangguan, S.; Liao, J.; Hua, Z. The Influence of PBF-LB/M Part Forming Angle and Support Structure Parameters on the Distortion of Oral Stent. Materials 2025, 18, 4588. https://doi.org/10.3390/ma18194588
Liu Y, Xie D, Liu Y, Tian Z, Shangguan S, Liao J, Hua Z. The Influence of PBF-LB/M Part Forming Angle and Support Structure Parameters on the Distortion of Oral Stent. Materials. 2025; 18(19):4588. https://doi.org/10.3390/ma18194588
Chicago/Turabian StyleLiu, Yang, Deqiao Xie, Yihan Liu, Zongjun Tian, Shimao Shangguan, Jinbiao Liao, and Zhizhong Hua. 2025. "The Influence of PBF-LB/M Part Forming Angle and Support Structure Parameters on the Distortion of Oral Stent" Materials 18, no. 19: 4588. https://doi.org/10.3390/ma18194588
APA StyleLiu, Y., Xie, D., Liu, Y., Tian, Z., Shangguan, S., Liao, J., & Hua, Z. (2025). The Influence of PBF-LB/M Part Forming Angle and Support Structure Parameters on the Distortion of Oral Stent. Materials, 18(19), 4588. https://doi.org/10.3390/ma18194588








