Fracture Toughness, Work of Fracture and Hardness of 3D-Printed Denture Base Resins
Abstract
1. Introduction
2. Materials and Methods
2.1. Materials
2.1.1. Sampling
2.1.2. Sample Fabrication
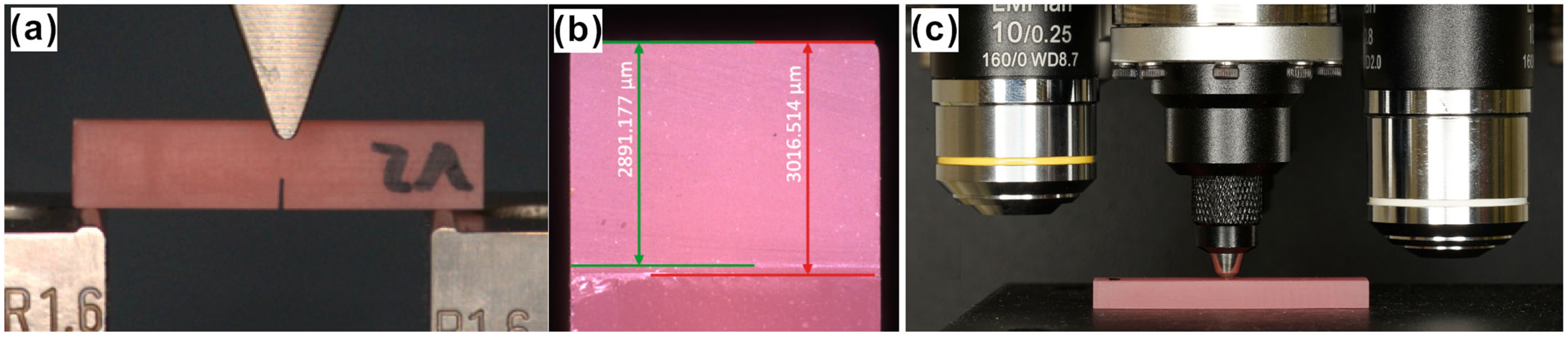
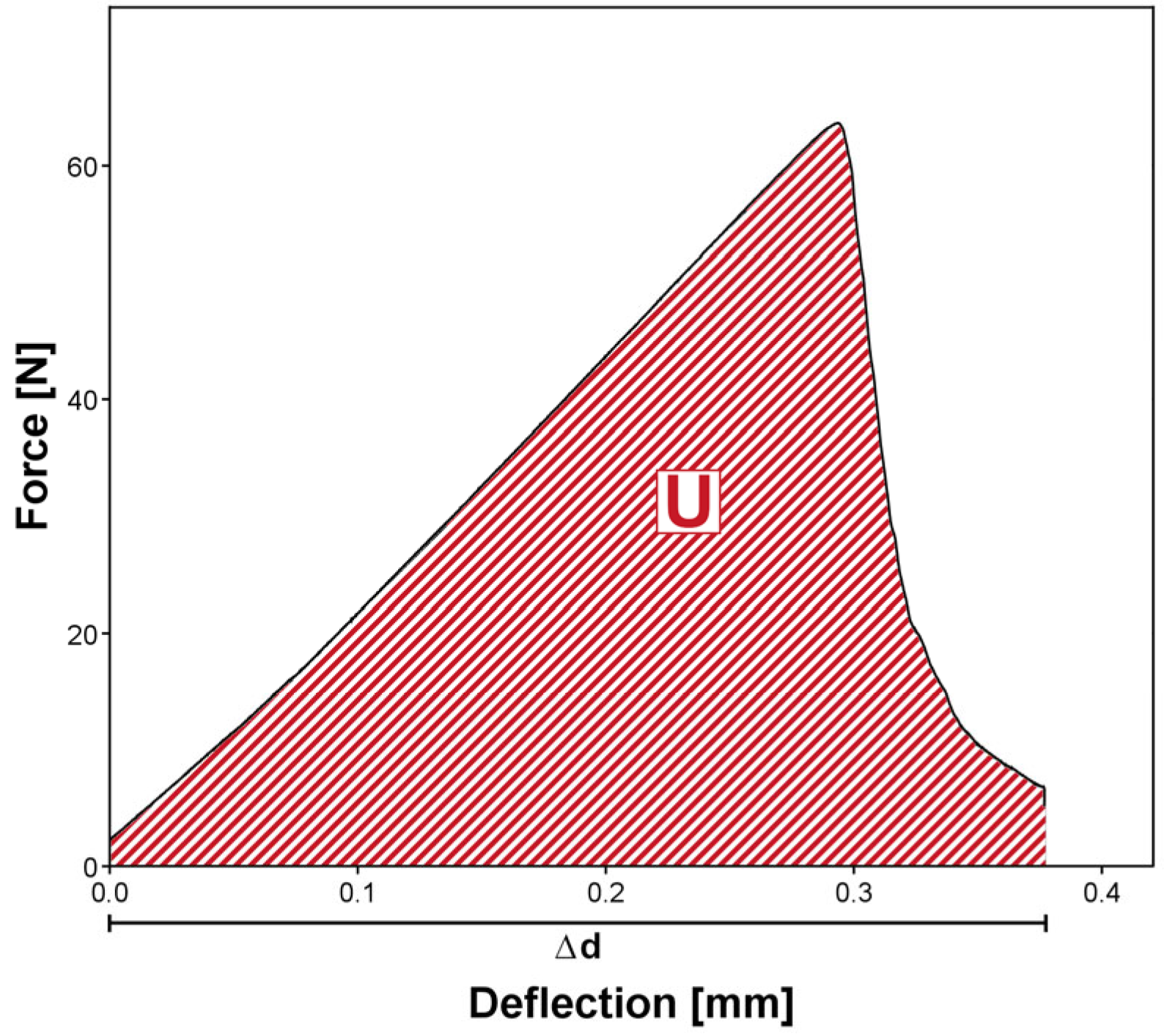
2.2. Fracture Toughness and Work of Fracture Testing
2.3. Vickers Hardness Measurement
2.4. Statistical Analysis
3. Results
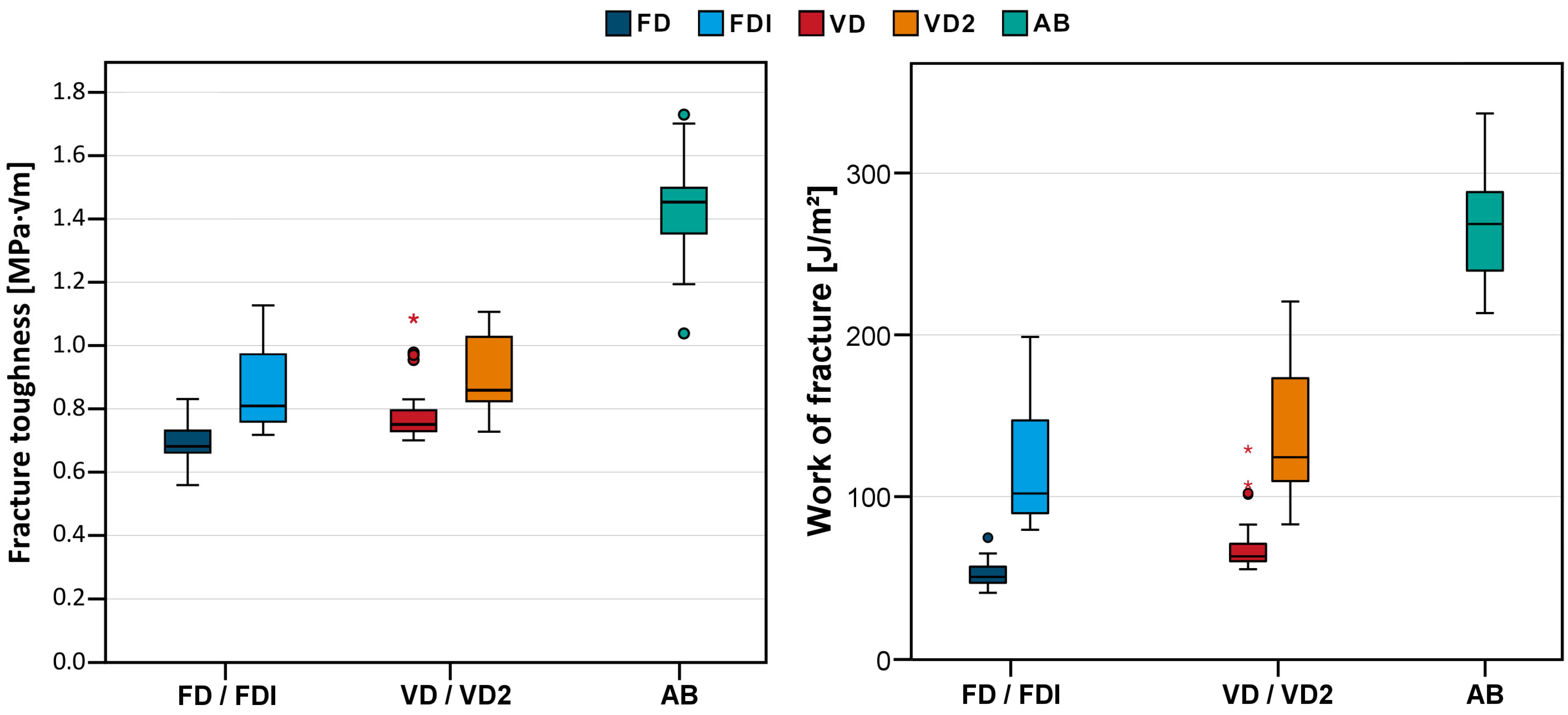
3.1. Fracture Toughness and Work of Fracture
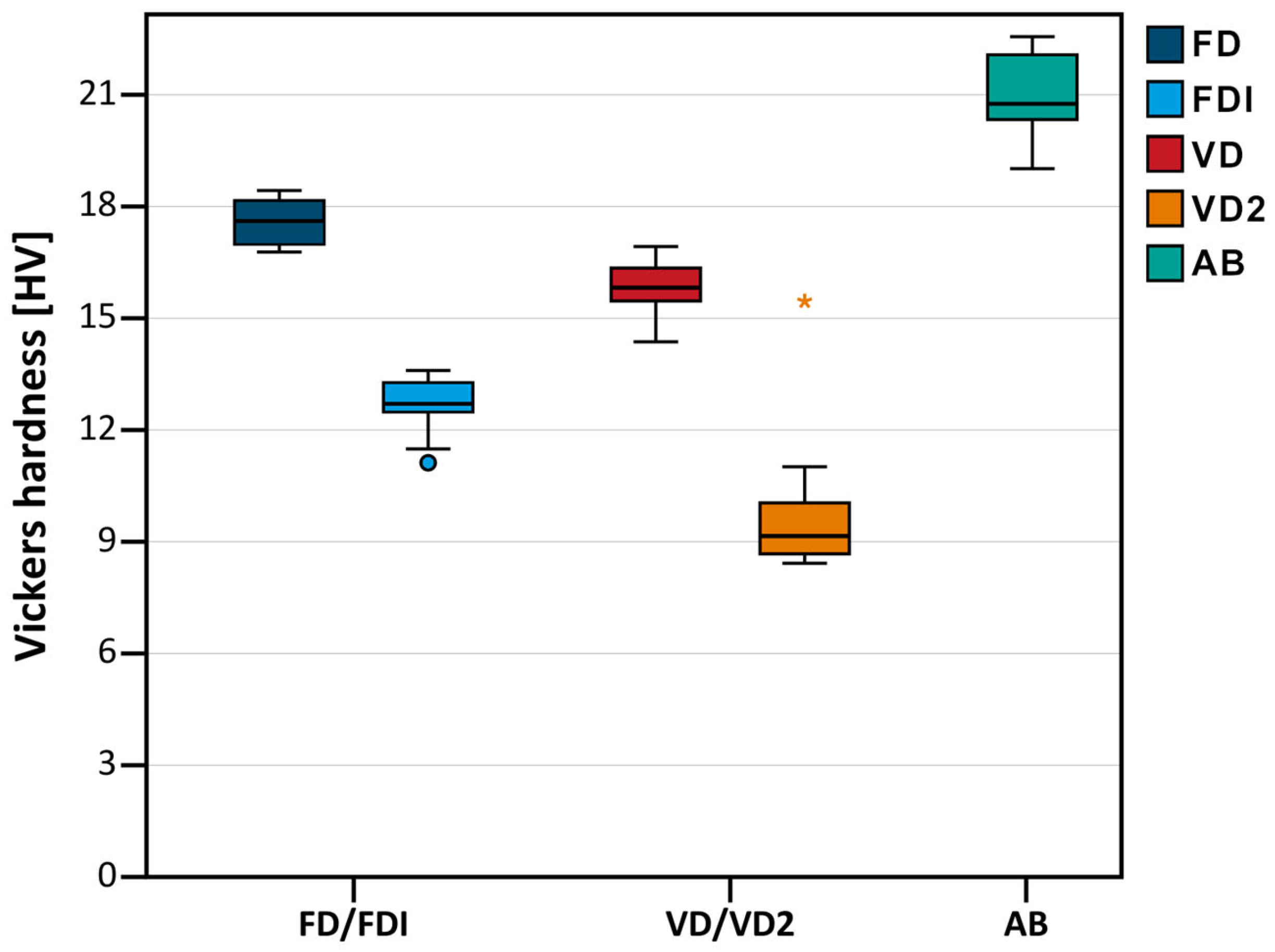
3.2. Vickers Hardness
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Abbreviations
| FD | Freeprint denture (DETAX) |
| FDI | Freeprint denture impact (DETAX) |
| VD | V-Print dentbase (Voco) |
| VD2 | V-Print dentbase 2.0 (Voco) |
| AB | Aesthetic Blue (Candulor) |
| CAD/CAM | Computer aided design/computer aided manufacturing |
| SD | Standard deviation |
| FT | Fracture toughness |
| WOF | Work of fracture |
| HV | Vickers hardness |
| DC | Degree of conversion |
| IBOMA | isobornyl methacrylate |
| TEGDMA | Triethylenglykoldimethacrylat |
References
- Yan, L.; Xie, B.; Li, Y.; Liu, Z.; Huang, Y.; He, B.; Qiu, Y.; Luo, L.; Yan, F.; Chen, F. Global burden of oral disorders with projections over the next 30 years. J. Periodontol. 2025, 1–13. [Google Scholar] [CrossRef]
- Feng, Y.; Feng, Z.; Li, J.; Chen, J.; Yu, H.; Jiang, X.; Zhou, Y.; Zhang, Y.; Huang, C.; Fu, B.; et al. Expert consensus on digital restoration of complete dentures. Int. J. Oral Sci. 2025, 17, 58. [Google Scholar] [CrossRef] [PubMed]
- Casucci, A.; Cagidiaco, E.F.; Verniani, G.; Ferrari, M.; Borracchini, A. Digital vs. conventional removable complete dentures: A retrospective study on clinical effectiveness and cost-efficiency in edentulous patients: Clinical effectiveness and cost-efficiency analysis of digital dentures. J. Dent. 2025, 153, 105505. [Google Scholar] [CrossRef] [PubMed]
- Vincze, Z.E.; Nagy, L.; Kelemen, K.; Cavalcante, B.G.N.; Gede, N.; Hegyi, P.; Banyai, D.; Koles, L.; Marton, K. Milling has superior mechanical properties to other fabrication methods for PMMA denture bases: A systematic review and network meta-analysis. Dent. Mater. 2025, 41, 366–382. [Google Scholar] [CrossRef] [PubMed]
- Arora, O.; Ahmed, N.; Nallaswamy, D.; Ganapathy, D.; Srinivasan, M. Denture base materials: An in vitro evaluation of the mechanical and color properties. J. Dent. 2024, 145, 104993. [Google Scholar] [CrossRef]
- Goodacre, B.J.; Goodacre, C.J. Additive Manufacturing for Complete Denture Fabrication: A Narrative Review. J. Prosthodont. 2022, 31, 47–51. [Google Scholar] [CrossRef]
- Lo Russo, L.; Zhurakivska, K.; Guida, L.; Chochlidakis, K.; Troiano, G.; Ercoli, C. Comparative cost-analysis for removable complete dentures fabricated with conventional, partial, and complete digital workflows. J. Prosthet. Dent. 2024, 131, 689–696. [Google Scholar] [CrossRef]
- Zahel, A.; Roehler, A.; Kaucher-Fernandez, P.; Spintzyk, S.; Rupp, F.; Engel, E. Conventionally and digitally fabricated removable complete dentures: Manufacturing accuracy, fracture resistance and repairability. Dent. Mater. 2024, 40, 1635–1642. [Google Scholar] [CrossRef]
- Handermann, R.; Zehender, N.; Rues, S.; Kobayashi, H.; Rammelsberg, P.; Schwindling, F.S. Load-bearing capacity of 3D-printed incisor partial-coverage crowns made from zirconia and composite. J. Prosthodont. Res. 2024, 68, 532–539. [Google Scholar] [CrossRef]
- Yudaev, P.; Chuev, V.; Klyukin, B.; Kuskov, A.; Mezhuev, Y.; Chistyakov, E. Polymeric Dental Nanomaterials: Antimicrobial Action. Polymers 2022, 14, 864. [Google Scholar] [CrossRef]
- Xiong, C.R.; Xiao, J.H.; Li, Z.Y.; Zhao, G.; Xiao, W.L. Knowledge graph network-driven process reasoning for laser metal additive manufacturing based on relation mining. Appl. Intell. 2024, 54, 11472–11483. [Google Scholar] [CrossRef]
- Xiao, J.H.; Lan, B.W.; Jiang, C.R.; Terzi, S.; Zheng, C.; Eynard, B.; Anwer, N.; Huang, H.L. Graph attention-based knowledge reasoning for mechanical performance prediction of L-PBF printing parts. Int. J. Adv. Manuf. Technol. 2025, 138, 4175–4195. [Google Scholar] [CrossRef]
- ISO/DIS 20795-1:2007; Dentistry—Base Polymers—Part 1: Denture Base Polymers. DIN German Institute for Standardization: Berlin, Germany, 2007.
- Geiger, V.; Mayinger, F.; Hoffmann, M.; Reymus, M.; Stawarczyk, B. Fracture toughness, work of fracture, flexural strength and elastic modulus of 3D-printed denture base resins in two measurement environments after artificial aging. J. Mech. Behav. Biomed. Mater. 2024, 150, 106234. [Google Scholar] [CrossRef] [PubMed]
- Malik, A. Flexural Strength, Fracture Toughness, and Denture Tooth Adhesion of Computer Aided Milled and Printed Denture Bases. Master’s Thesis, The Ohio State University, Columbus, OH, USA, 2019. [Google Scholar]
- Perea-Lowery, L.; Gibreel, M.; Vallittu, P.K.; Lassila, L.V. 3D-Printed vs. Heat-Polymerizing and Autopolymerizing Denture Base Acrylic Resins. Materials 2021, 14, 5781. [Google Scholar] [CrossRef] [PubMed]
- Prpic, V.; Schauperl, Z.; Catic, A.; Dulcic, N.; Cimic, S. Comparison of Mechanical Properties of 3D-Printed, CAD/CAM, and Conventional Denture Base Materials. J. Prosthodont. 2020, 29, 524–528. [Google Scholar] [CrossRef] [PubMed]
- Alifui-Segbaya, F.; Bowman, J.; White, A.R.; George, R.; Fidan, I. Characterization of the Double Bond Conversion of Acrylic Resins for 3D Printing of Dental Prostheses. Compend. Contin. Educ. Dent. 2019, 40, e7–e11. [Google Scholar]
- Calheiros, F.C.; Daronch, M.; Rueggeberg, F.A.; Braga, R.R. Degree of conversion and mechanical properties of a BisGMA:TEGDMA composite as a function of the applied radiant exposure. J. Biomed. Mater. Res. B Appl. Biomater. 2008, 84, 503–509. [Google Scholar] [CrossRef]
- Reymus, M.; Lumkemann, N.; Stawarczyk, B. 3D-printed material for temporary restorations: Impact of print layer thickness and post-curing method on degree of conversion. Int. J. Comput. Dent. 2019, 22, 231–237. [Google Scholar]
- Pacquet, W.; Benoit, A.; Hatege-Kimana, C.; Wulfman, C. Mechanical Properties of CAD/CAM Denture Base Resins. Int. J. Prosthodont. 2019, 32, 104–106. [Google Scholar] [CrossRef]
- Gad, M.M.; Fouda, S.M.; Abualsaud, R.; Alshahrani, F.A.; Al-Thobity, A.M.; Khan, S.Q.; Akhtar, S.; Ateeq, I.S.; Helal, M.A.; Al-Harbi, F.A. Strength and Surface Properties of a 3D-Printed Denture Base Polymer. J. Prosthodont. 2022, 31, 412–418. [Google Scholar] [CrossRef]
- Kim, D.; Shim, J.S.; Lee, D.; Shin, S.H.; Nam, N.E.; Park, K.H.; Shim, J.S.; Kim, J.E. Effects of Post-Curing Time on the Mechanical and Color Properties of Three-Dimensional Printed Crown and Bridge Materials. Polymers 2020, 12, 2762. [Google Scholar] [CrossRef]
- Aati, S.; Akram, Z.; Shrestha, B.; Patel, J.; Shih, B.; Shearston, K.; Ngo, H.; Fawzy, A. Effect of post-curing light exposure time on the physico-mechanical properties and cytotoxicity of 3D-printed denture base material. Dent. Mater. 2022, 38, 57–67. [Google Scholar] [CrossRef]
- Greil, V.; Mayinger, F.; Reymus, M.; Stawarczyk, B. Water sorption, water solubility, degree of conversion, elastic indentation modulus, edge chipping resistance and flexural strength of 3D-printed denture base resins. J. Mech. Behav. Biomed. Mater. 2023, 137, 105565. [Google Scholar] [CrossRef]
- Lovell, L.G.; Newman, S.M.; Bowman, C.N. The effects of light intensity, temperature, and comonomer composition on the polymerization behavior of dimethacrylate dental resins. J. Dent. Res. 1999, 78, 1469–1476. [Google Scholar] [CrossRef] [PubMed]
- Vallittu, P.K.; Ruyter, I.E.; Buykuilmaz, S. Effect of polymerization temperature and time on the residual monomer content of denture base polymers. Eur. J. Oral Sci. 1998, 106, 588–593. [Google Scholar] [CrossRef] [PubMed]
- Alsandi, Q.; Ikeda, M.; Arisaka, Y.; Nikaido, T.; Tsuchida, Y.; Sadr, A.; Yui, N.; Tagami, J. Evaluation of Mechanical and Physical Properties of Light and Heat Polymerized UDMA for DLP 3D Printer. Sensors 2021, 21, 3331. [Google Scholar] [CrossRef] [PubMed]
- Mayer, J.; Reymus, M.; Wiedenmann, F.; Edelhoff, D.; Hickel, R.; Stawarczyk, B. Temporary 3D printed fixed dental prosthesis materials: Impact of post printing cleaning methods on degree of conversion as well as surface and mechanical properties. Int. J. Prosthodont. 2021, 34, 784–795. [Google Scholar] [CrossRef]
- Fouda, S.; Ji, W.; Gad, M.M.; AlGhamdi, M.A.; Rohr, N. Flexural Strength and Surface Properties of 3D-Printed Denture Base Resins-Effect of Build Angle, Layer Thickness and Aging. Materials 2025, 18, 913. [Google Scholar] [CrossRef]
- Es-Said, O.S.; Noorani, J.F.R.; Mendelson, M.; Marloth, R. Effect of Layer Orientation on MechanicalProperties of Rapid Prototyped Samples. Mater. Manuf. Process. 2000, 15, 107–122. [Google Scholar] [CrossRef]
- Freeprint Denture; Safety Data Sheet, DETAX Gmbh. 2024. Available online: https://www.detax.com/de/dental/produkt/dx-denture (accessed on 11 August 2025).
- Freeprint Denture Impact; Safety Data Sheet, DETAX Gmbh. 2024. Available online: https://www.detax.com/dental/product/dx-denture-impact (accessed on 11 August 2025).
- V-Print Dentbase; Safety Data Sheet, VOCO GmbH 2024. Available online: https://www.voco.dental/en/digital/material/3d-printing-material/v-print-dentbase.aspx (accessed on 11 August 2025).
- Martins, A.R.M.; Machado-Santos, L.; Grassia, R.C.F., Jr.; Vitti, R.P.; Sinhoreti, M.A.C.; Brandt, W.C. Physical and Mechanical Properties of Resins Blends Containing a Monomethacrylate with Low-polymerization Shrinkage. Eur. J. Dent. 2021, 15, 96–100. [Google Scholar] [CrossRef]
- Martins, A.R.M.; Silva, I.D.; Machado-Santos, L.; Vitti, R.P.; Sinhoreti, M.A.C.; Brandt, W.C. Isobornyl methacrylate as diluent co-monomer on physical-mechanical properties of dental resin composites. J. Appl. Polym. Sci. 2021, 138, 50498. [Google Scholar] [CrossRef]
- Pereira, R.P.; de Oliveira, D.; Rocha, M.G.; Correr-Sobrinho, L.; Roulet, J.F.; Sinhoreti, M.A.C. Physicochemical properties of flowable composites using isobornyl methacrylate as diluent monomer. J. Appl. Oral Sci. 2024, 32, e20240172. [Google Scholar] [CrossRef]
- Gonçalves, F.; Kawano, Y.; Pfeifer, C.; Stansbury, J.W.; Braga, R.R. Influence of BisGMA, TEGDMA, and BisEMA contents on viscosity, conversion, and flexural strength of experimental resins and composites. Eur. J. Oral Sci. 2009, 117, 442–446. [Google Scholar] [CrossRef]
- Majeed, H.F.; Hamad, T.I.; Bairam, L.R. Enhancing 3D-printed denture base resins: A review of material innovations. Sci. Prog. 2024, 107, 368504241263484. [Google Scholar] [CrossRef]
- Mosaddad, S.A.; Khorasani, E.; Schimmel, M.; Santos, A.T.; Pieralli, S.; Cakmak, G.; Molinero-Mourelle, P. Do resin-modified 3D-printed complete dentures show improved mechanical, physical, surface, and biological properties? A systematic review and meta-analysis. J. Dent. 2025, 161, 105983. [Google Scholar] [CrossRef]


| Name | Abbreviation | Manufacturer | Technique |
|---|---|---|---|
| FREEPRINT® DENTURE | FD | DETAX GmbH, Ettlingen, Germany | 3D-Printing |
| FREEPRINT® DENTURE IMPACT | FDI | ||
| V-Print® dentbase | VD | VOCO GmbH, Cuxhaven, Germany | |
| V-Print® dentbase 2.0 | VD2 | ||
| AESTHETIC BLUE® | AB | CANDULOR AG, Opfikon, Switzerland | Casting |
| Material | Fracture Toughness [MPa∙√m] | Work of Fracture [J/m2] | Vickers Hardness [HV0.3] | |||
|---|---|---|---|---|---|---|
| Mean Value | SD | Mean Value | SD | Mean Value | SD | |
| FD | 0.69 A | 0.06 | 52 A | 8 | 17.6 A | 0.7 |
| FDI | 0.85 B | 0.12 | 117 B | 35 | 12.6 B | 0.8 |
| VD | 0.78 C | 0.08 | 69 C | 16 | 15.8 A | 0.8 |
| VD2 | 0.91 B | 0.11 | 140 B | 39 | 10.0 C | 2.2 |
| AB | 1.46 D | 0.12 | 257 D | 30 | 20.9 D | 1.1 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Hetzler, S.; Rehm, S.; Räther, S.; Rues, S.; Zenthöfer, A.; Rammelsberg, P.; Schwindling, F.S. Fracture Toughness, Work of Fracture and Hardness of 3D-Printed Denture Base Resins. Materials 2025, 18, 4338. https://doi.org/10.3390/ma18184338
Hetzler S, Rehm S, Räther S, Rues S, Zenthöfer A, Rammelsberg P, Schwindling FS. Fracture Toughness, Work of Fracture and Hardness of 3D-Printed Denture Base Resins. Materials. 2025; 18(18):4338. https://doi.org/10.3390/ma18184338
Chicago/Turabian StyleHetzler, Sebastian, Sebastian Rehm, Sven Räther, Stefan Rues, Andreas Zenthöfer, Peter Rammelsberg, and Franz Sebastian Schwindling. 2025. "Fracture Toughness, Work of Fracture and Hardness of 3D-Printed Denture Base Resins" Materials 18, no. 18: 4338. https://doi.org/10.3390/ma18184338
APA StyleHetzler, S., Rehm, S., Räther, S., Rues, S., Zenthöfer, A., Rammelsberg, P., & Schwindling, F. S. (2025). Fracture Toughness, Work of Fracture and Hardness of 3D-Printed Denture Base Resins. Materials, 18(18), 4338. https://doi.org/10.3390/ma18184338







