Modern Light-Cured Restorative Composites as Luting Agents: The Effect of Preheating on Conversion and Film Thickness
Abstract
1. Introduction
2. Materials and Methods

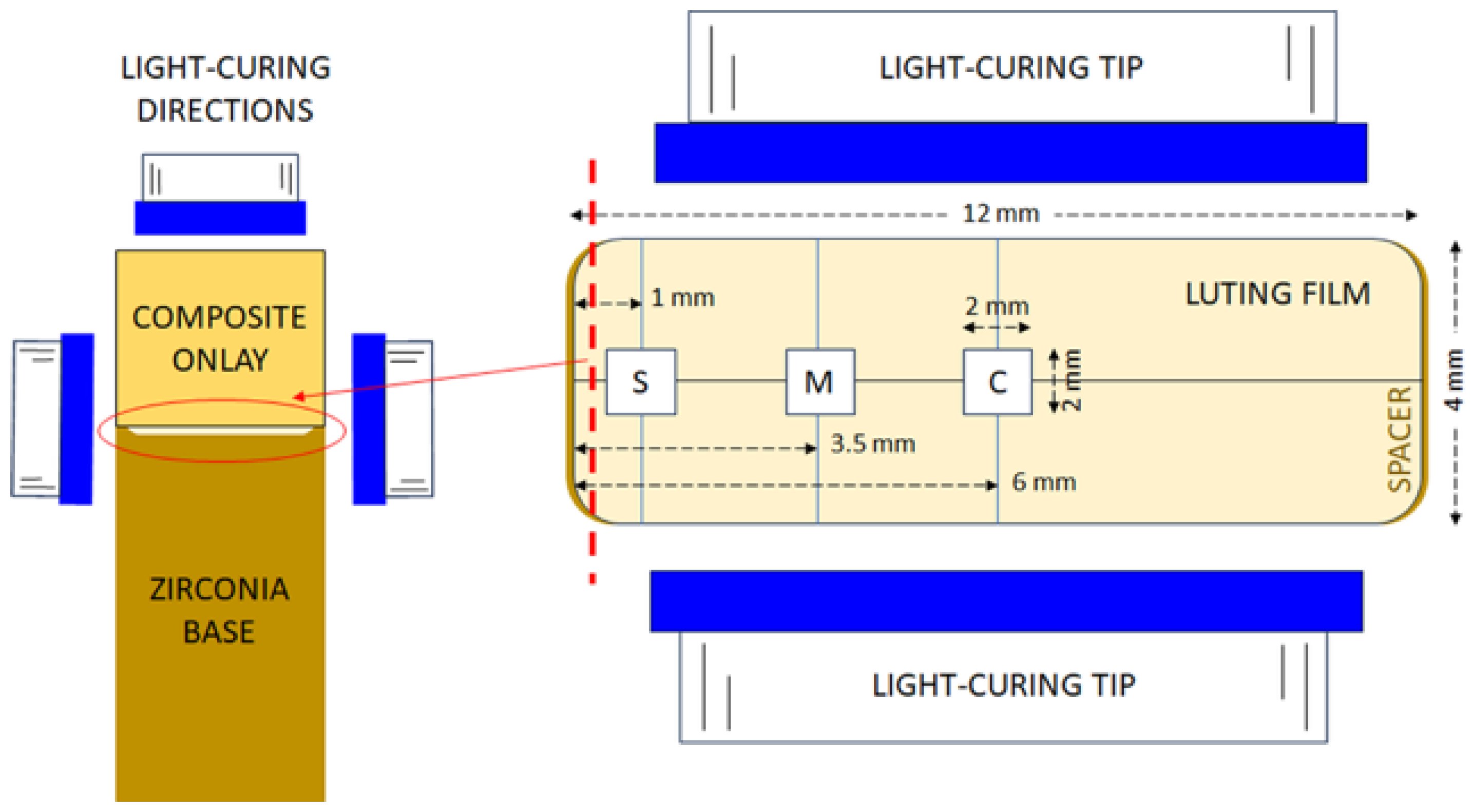
2.1. Curing Capacity
2.1.1. Curing Capacity of Luting Light-Cured Composites Under Onlays at Standard Thickness
2.1.2. Curing Capacity of Luting Light-Cured Composite Under Onlays at Different Thicknesses
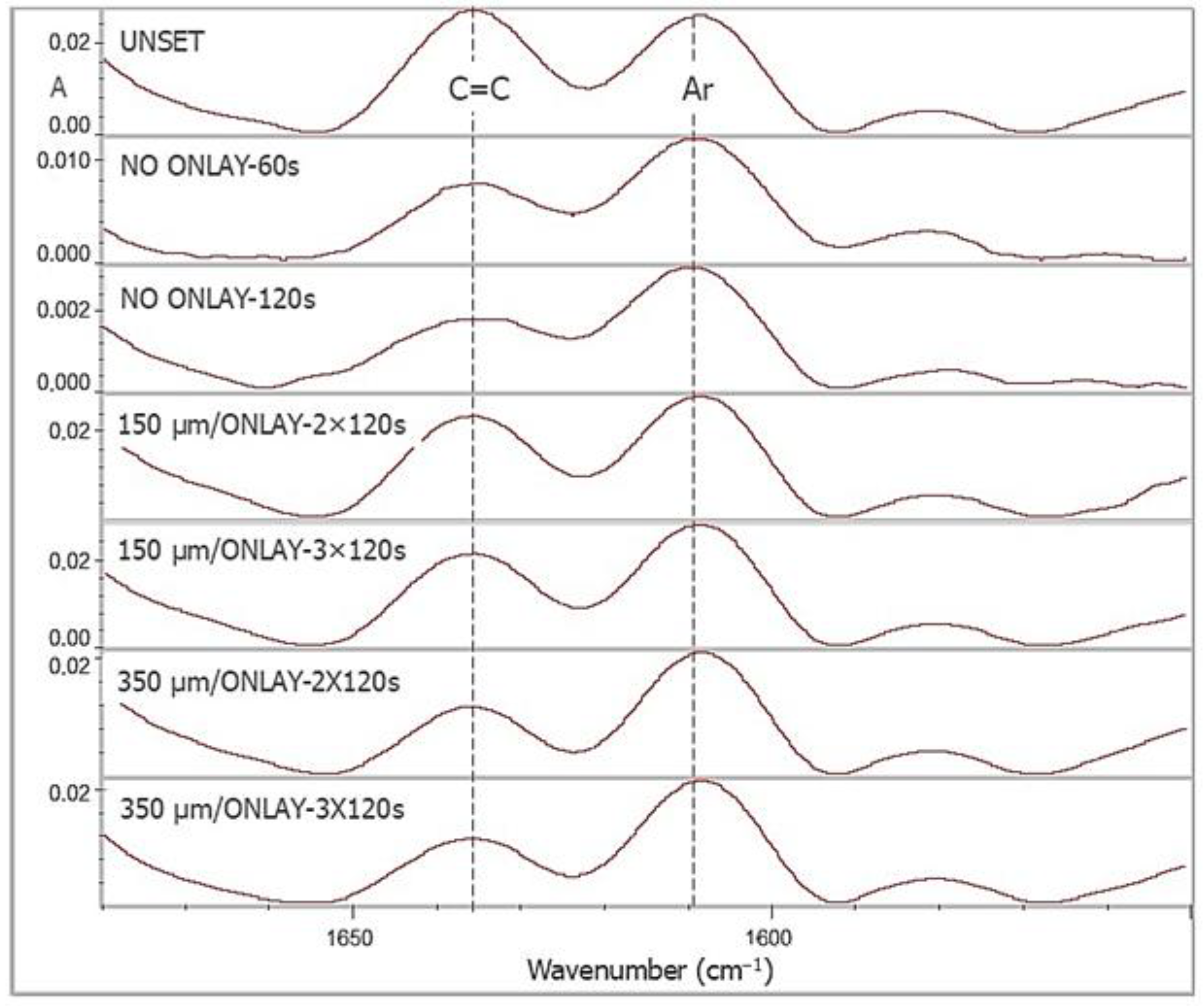
2.1.3. Measurement of the Curing Capacity
2.2. Film Thickness
2.3. Statistical Analysis
3. Results
3.1. Curing Capacity
3.1.1. Curing Capacity of Luting Light-Cured Composites Under Onlays at Standard Thickness
3.1.2. Curing Capacity of Luting Light-Cured Composite Under Onlays at Different Thicknesses
3.2. Film Thickness
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Tribst, J.P.M.; Etoeharnowo, L.; Tadros, M.; Feilzer, A.J.; Werner, A.; Kleverlaan, C.J.; Dal Piva, A.M.O. The influence of pre-heating the restoration and luting agent on the flexural strength of indirect ceramic and composite restorations. Biomater. Investig. Dent. 2023, 10, 2279066. [Google Scholar] [CrossRef] [PubMed]
- Edelhoff, D.; Erdelt, K.-J.; Stawarczyk, B.; Liebermann, A. Pressable lithium disilicate ceramic versus CAD/CAM resin composite restorations in patients with moderate to severe toothwear: Clinical observations up to 13 years. J. Esthet. Restor. Dent. 2023, 35, 116–128. [Google Scholar] [CrossRef] [PubMed]
- Marocho, S.M.S.; Özcan, M.; Amaral, R.; Valandro, L.F.; Bottino, M.A. Effect of seating forces on cement-ceramic adhesion in microtensile bond tests. Clin. Oral Investig. 2013, 17, 325–331. [Google Scholar] [CrossRef] [PubMed]
- Goulart, M.; Borges Veleda, B.; Damin, D.; Bovi Ambrosano, G.M.; Coelho de Souza, F.H.; Erhardt, M.C.G. Preheated composite resin used as a luting agent for indirect restorations: Effects on bond strength and resin-dentin interfaces. Int. J. Esthet. Dent. 2018, 13, 86–97. [Google Scholar]
- Schneider, L.F.J.; Ribeiro, R.B.; Liberato, W.F.; Salgado, V.E.; Moraes, R.R.; Calvacante, L.M. Curing potential and color stability of different resin-based luting materials. Dent. Mater. 2020, 36, e309–e315. [Google Scholar] [CrossRef]
- De Angelis, F.; Vadini, M.; Capogreco, M.; D’Arcangelo, C.; D’Amario, M. Effect of light-sources and thicknesses of composite onlays on micro-hardness of luting composites. Materials 2021, 14, 6849. [Google Scholar] [CrossRef]
- Magalhães, T.; Fidalgo-Pereira, R.; Torres, O.; Carvalho, Ó.; Silva, F.S.; Henriques, B.; Özcan, M.; Souza, J.C.M. Microscopic inspection of the adhesive interface of composite onlays after cementation on low loading: An in vitro study. J. Funct. Biomater. 2023, 14, 148. [Google Scholar] [CrossRef]
- Raposo, C.C.; Nery, L.M.S.; Carvalho, E.M.; Ferreira, P.V.C.; Ardenghi, D.M.; Bauer, J.; Lima, D.M. Effect of preheating on the physicochemical properties and bond strength of composite resins utilized as dental cements: An in vitro study. J. Prosthet. Dent. 2023, 129, 229.e1–229.e7. [Google Scholar] [CrossRef]
- Tomaselli, L.O.; Oliveira, D.C.R.S.; Favarão, J.; Silva, A.F.D.; Pires-de-Souza, F.C.P.; Geraldeli, S.; Sinhoreti, M.A.C. Influence of pre-heating regular resin composites and flowable composites on luting ceramic veneers with different thicknesses. Braz. Dent. J. 2019, 30, 459–466. [Google Scholar] [CrossRef]
- Zhukovsky, L.; Settembrini, L.; Epelboym, D. Tooth-colored inlays: New cementation technique. Gen. Dent. 1997, 45, 290–293. [Google Scholar]
- Porto, B.L.; Barbon, F.J.; Isolan, C.P.; Borges, A.L.; Spazzin, A.O.; Moraes, R.R.; Boscato, N. Effect of ultrasound on preheated resin composites used as ceramic luting agents. Dent. Mater. J. 2022, 41, 451–458. [Google Scholar] [CrossRef]
- Falacho, R.I.; Marques, J.A.; Palma, P.; Roseiro, L.; Caramelo, F.; Ramos, J.C.; Guerra, F.; Blatz, M.B. Luting indirect restorations with resin cements versus composite resins: Effects of preheating and ultrasound energy on film thickness. J. Esthet. Restor. Dent. 2021, 34, 641–649. [Google Scholar] [CrossRef] [PubMed]
- Alvarado, U.M.S.; García, E.D.M.; Guillén, P.A.J.; Arriaga, F.J.C.; Ramírez, R.G.F.; Magdaleno, O.M. Evaluation of the bond strength and marginal seal of indirect restorations of composites bonded with preheating resin. Eur. J. Dent. 2020, 14, 644–650. [Google Scholar] [CrossRef] [PubMed]
- Marcondes, R.L.; Lima, V.P.; Barbon, F.J.; Isolan, C.P.; Carvalho, M.A.; Salvador, M.V.; Lima, A.F.; Moraes, R.R. Viscosity and thermal kinetics of 10 preheated restorative resin composites and effect of ultrasound energy on film thickness. Dent. Mater. 2020, 36, 1356–1364. [Google Scholar] [CrossRef] [PubMed]
- Barbon, F.J.; Isolan, C.P.; Soares, L.D.; Della Bona, A.; da Rosa, W.L.O.; Boscato, N. A systematic review and meta-analysis on using preheated resin composites as luting agents for indirect restorations. Clin. Oral Investig. 2022, 26, 3383–3393. [Google Scholar] [CrossRef]
- Chen, T.A.; Lu, P.Y.; Lin, P.Y.; Chi, C.W.; Cheng, H.Y.; Lai, Y.J.; Wang, F.; Chiang, Y.C. Effects of ceramic thickness, ceramic translucency, and light transmission on light-cured bulk-fill resin composites as luting cement of lithium disilicate based-ceramics. J. Prosthodont. Res. 2024, 68, 255–263. [Google Scholar] [CrossRef]
- Fidalgo-Pereira, R.; Catarino, S.O.; Carvalho, Ó.; Veiga, N.; Torres, O.; Braem, A.; Souza, J.C.M. Light transmittance through resin-matrix composite onlays adhered to resin-matrix cements or flowable composites. J. Mech. Behav. Biomed. Mater. 2024, 151, 106353. [Google Scholar] [CrossRef]
- Daronch, M.; Rueggeberg, F.A.; De Goes, M.F. Monomer conversion of pre-heated composite. J. Dent. Res. 2005, 84, 663–667. [Google Scholar] [CrossRef]
- Yang, J.; Silikas, N.; Watts, D.C. Pre-heating time and exposure duration: Effects on post-irradiation properties of a thermo-viscous resin-composite. Dent. Mater. 2020, 36, 787–793. [Google Scholar] [CrossRef]
- Lohbauer, U.; Zinelis, S.; Rahiotis, C.; Petschelt, A.; Eliades, G. The effect of resin composite pre-heating on monomer conversion and polymerization shrinkage. Dent. Mater. 2009, 25, 514–519. [Google Scholar] [CrossRef]
- Fróes-Salgado, N.R.; Silva, L.M.; Kawano, Y.; Francci, C.; Reis, A.; Loguercio, A.D. Composite pre-heating: Effects on marginal adaptation, degree of conversion and mechanical properties. Dent. Mater. 2010, 26, 908–914. [Google Scholar] [CrossRef]
- ISO 4049; Dentistry-Polymer Based Restorative Materials. 5th ed. International Standardization Organization: Geneva, Switzerland, 2019.
- Pacheco, R.R.; Carvalho, A.O.; André, C.B.; Ayres, A.P.A.; de Sá, R.B.C.; Dias, T.M.; Rueggeberg, F.A.; Giannini, M. Effect of indirect restorative material and thickness on light transmission at different wavelengths. J. Prosthodont. Res. 2019, 63, 232–238. [Google Scholar] [CrossRef] [PubMed]
- Vargas-Corral, F.G.; Vargas-Corral, A.E.; Rodríguez-Valverde, M.A.; Bravo, M.; Rosales-Leal, J.I. Clinical comparison of marginal fit of ceramic inlays between digital and conventional impressions. J. Adv. Prosthodont. 2024, 16, 57–65. [Google Scholar] [CrossRef] [PubMed]
- Zheng, Z.; Wang, H.; Mo, J.; Ling, Z.; Zeng, Y.; Zhang, Y.; Wang, J.; Yan, W. Effect of virtual cement space and restorative materials on the adaptation of CAD-CAM endocrowns. BMC Oral Health 2022, 22, 580. [Google Scholar] [CrossRef] [PubMed]
- Park, S.-H.; Yoo, Y.-J.; Shin, Y.-J.; Cho, B.-H.; Baek, S.-H. Marginal and internal fit of nano-composite CAD/CAM restorations. Restor. Dent. Endod. 2016, 41, 37–43. [Google Scholar] [CrossRef]
- Rocha, M.G.; Oliveira, D.; Felix, C.; Roulet, J.F.; Shinoreti, M.A.C.; Correr, A.B. Beam profiling of dental light curing units using different camera-based systems. Eur. J. Dent. 2022, 16, 64–79. [Google Scholar] [CrossRef]
- do Nascimento Poubel, L.; Zanon, A.E.G.; Almeida, J.C.F.; Rezende, L.V.M.L.; Garcia, F.C.P. Composite resin preheating techniques for cementation of indirect restorations. Int. J. Biomater. 2022, 2022, 5935668. [Google Scholar] [CrossRef]
- Truffier-Boutry, D.; Demoustier-Champagne, S.; Devaux, J.; Biebuyck, J.J.; Mestdagh, M.; Larbanois, P.; Leloup, G. A physico-chemical explanation of the post-polymerization shrinkage in dental resins. Dent. Mater. 2006, 22, 405–412. [Google Scholar] [CrossRef]
- Scotti, N.; Venturello, A.; Borga, F.A.C.; Pasqualini, D.; Paolino, D.S.; Geobaldo, F.; Berutti, E. Post-curing conversion kinetics as functions of the irradiation time and increment thickness. J. Appl. Oral Sci. 2013, 21, 190–195. [Google Scholar] [CrossRef]
- Moad, C.L.; Moad, G. Fundamentals of reversible addition–fragmentation chain transfer (RAFT). Chem. Teach. Int. 2021, 3, 3–17. [Google Scholar] [CrossRef]
- Shah, P.K.; Stansbury, J.W.; Bowman, C.N. Application of an addition-fragmentation chain transfer monomer in di(meth)acrylate network formation to reduce polymerization shrinkage stress. Polym. Chem. 2017, 8, 4339–4351. [Google Scholar] [CrossRef]
- Floyd, C.J.E.; Dickens, S.H. Network structure of Bis-GMA- and UDMA-based resin systems. Dent. Mater. 2006, 22, 1143–1149. [Google Scholar] [CrossRef] [PubMed]
- Ruyter, I.E. Methacrylate-based polymeric dental materials: Conversion and related properties. Summary and review. Acta Odontol. Scand. 1982, 40, 359–376. [Google Scholar] [CrossRef] [PubMed]
- Babaier, R.; Haider, J.; Silikas, N.; Watts, D.C. Effect of CAD/CAM aesthetic material thickness and translucency on the polymerisation of light and dual-cured resin cements. Dent. Mater. 2022, 38, 2073–2083. [Google Scholar] [CrossRef] [PubMed]
- de Kuijper, M.C.F.M.; Ong, Y.; Gerritsen, T.; Cune, M.S.; Gresnigt, M.M.M. Influence of the ceramic translucency on the relative degree of conversion of a direct composite and dual-curing resin cement through lithium disilicate onlays and endocrowns. J. Mech. Behav. Biomed. Mater. 2021, 122, 104662. [Google Scholar] [CrossRef]
- Acquaviva, P.A.; Cerutti, F.; Adami, G.; Gagliani, M.; Ferrari, M.; Gherlone, E.; Cerutti, A. Degree of conversion of three composite materials employed in the adhesive cementation of indirect restorations: A micro-Raman analysis. J. Dent. 2009, 37, 610–615. [Google Scholar] [CrossRef]
- Magne, P.; Alawie, S.; Magne, M.; Carvalho, M.; Milani, T. Comparison of film thickness of restorative composites considered for thermo-modified cementation. J. Esthet. Restor. Dent. 2025, 37, 28–38. [Google Scholar] [CrossRef]
- Magne, P.; Razaghy, M.; Carvalho, M.A.; Soares, L.M. Luting of inlays, onlays, and overlays with preheated restorative composite resin does not prevent seating accuracy. Int. J. Esthet. Dent. 2018, 13, 318–332. [Google Scholar]
- Deb, S.; Di Silvio, L.; Mackler, H.E.; Millar, B.J. Pre-warming of dental composites. Dent. Mater. 2011, 27, e51–e59. [Google Scholar] [CrossRef]
- Coelho, N.F.; Barbon, F.J.; Machado, R.G.; Boscato, N.; Moraes, R.R. Response of composite resins to preheating and the resulting strengthening of luted feldspar ceramic. Dent. Mater. 2019, 35, 1430–1438. [Google Scholar] [CrossRef]
- Zortuk, M.; Bolpaca, P.; Kilic, K.; Ozdemir, E.; Aguloglu, S. Effects of finger pressure applied by dentists during cementation of all-ceramic crowns. Eur. J. Dent. 2010, 4, 383–388. [Google Scholar] [CrossRef]
- Addison, O.; Sodhi, A.; Fleming, G. Seating load parameters impact on dental ceramic reinforcement conferred by cementation with resin-cements. Dent. Mater. 2010, 26, 915–921. [Google Scholar] [CrossRef] [PubMed]
- Loumprinis, N.; Maier, E.; Belli, R.; Petschelt, A.; Eliades, G.; Lohbauer, U. Viscosity and stickiness of dental resin composites at elevated temperatures. Dent. Mater. 2021, 37, 413–422. [Google Scholar] [CrossRef] [PubMed]
- Elbishari, H.; Satterthwaite, J.; Silikas, N. Effect of filler size and temperature on packing stress and viscosity of resin-composites. Int. J. Mol. Sci. 2011, 12, 5330–5338. [Google Scholar] [CrossRef] [PubMed]
- Al-Ahdal, K.; Silikas, N.; Watts, D.C. Rheological properties of resin composites according to variations in composition and temperature. Dent. Mater. 2014, 30, 517–524. [Google Scholar] [CrossRef]
- Dionysopoulos, D.; Tolidis, K.; Gerasimou, P.; Koliniotou-Koumpia, E. Effect of preheating on the film thickness of contemporary composite restorative materials. J. Dent. Sci. 2014, 9, 313–319. [Google Scholar] [CrossRef]
- Quinn, J.; Quinn, G. Material properties and fractography of an indirect dental resin composite. Dent. Mater. 2010, 26, 589–599. [Google Scholar] [CrossRef]
- Molin, M.K.; Karlsson, S.L.; Kristiansen, M.S. Influence of film thickness on joint bend strength of a ceramic/resin composite joint. Dent. Mater. 1996, 12, 245–249. [Google Scholar] [CrossRef]
- Borges, B.C.D.; Vilela, A.R.R.C.; da Silva, C.A., Jr.; Souza, E.J., Jr.; Sinhoreti, M.A.C.; Pinheiro, F.H.S.L.; Braz, R.; Montes, M.A.J.R. Dual-cured etch-and-rinse adhesive systems increase the bond durability of direct coronal dentin restorations. Oper. Dent. 2013, 38, 512–518. [Google Scholar] [CrossRef]
- Melo, A.M.S.; Ribeiro, A.K.C.; Cunha, D.A.; Rodrigues, N.S.; Saboia, V.P.A.; Borges, B.C.D.B.; de Assunção, I.V. Dual-cured adhesive system improves adhesive properties of dentin cavities restored with a bulk-fill resin composite. Braz. J. Oral Sci. 2022, 21, e226262. [Google Scholar] [CrossRef]

| Materials | Composition * | Manufacturer |
|---|---|---|
| INDIRECT ONLAY MATERIAL | ||
| Crea.lign dentine A3 | Resin: Mixture of DUDMA isomers, BGDMA. Filler: Nanosized opalescent ceramic filler (50 w%). | Bredent, Chesterfield, UK |
| DIRECT LIGHT-CURED COMPOSITE RESTORATIVES USED AS LUTING AGENTS | ||
| 3M Filtek Universal A2 (F) | Resin: AUDMA, AFM, DUDMA, DDMA, catalysts, stabilizers, water. Filler: Non-aggregated silica (20 nm), zirconia (4–11 nm), aggregated zirconia/silica clusters, aggregated YbF3 (100 nm), (76.5 w%, 58.4 v% inorganic filler). | 3M, St. PaulMN, USA |
| Clearfil Majestry ES-2 Universal (M) | Resin: BisGMA, hydrophobic aliphatic dimethacrylate, catalysts, stabilizers, pigments. Filler: Silanated Ba-glass filler, pre-polymerized organic filler, (66 w%). | Kuraray Noritake, Okuyama, Japan |
| Tetric EvoCeram A3 (T) | Resin: UDMA, BisGMA, BisEMA, catalysts, stabilizers, pigments. Filler: Ba-glass, mixed oxide, YbF3 and prepolymer additives (82–83 w%, 48.5 w% inorganics, 34 w% prepolymers, mean size of inorganic fillers: 550 nm, range 40 nm–3 μm). | Ivoclar Vivadent Schaan, Lichtenstein |
| VisCalor A2 (V) | Resin: BisGMA, TCDDMA, initiators, stabilizers, pigments. Filler: BaAlB-silicate glass, silica (83 w%). | Voco GmbH, Cuxhaven, Germany |
| DUAL-CURED ADHESIVE RESIN LUTING AGENT | ||
| Variolink Esthetic DC (E) | Resin: UDMA, GDMA, DDMA, AUDMA Filler: YF3, spheroid mixed oxide (60–68 w%, 38 v%, mean size 0.1 μm, range 0.04–0.2 μm). | Ivoclar Vivadent Schaan, Lichtenstein |
| Material | Non-Preheated | Preheated | ||||||
|---|---|---|---|---|---|---|---|---|
| Location | ||||||||
| R | S | M | C | R | S | M | C | |
| F | 50.94 (2.05) a,A,1 | 38.03 (3.85) a,B,1 | 37.03 (2.67) a,B,1 | 41.17 (3.86) a,Β,1 | 60.01 (6.97) a,A,2 | 40.98 (4.55) a,B,1 | 38.9 (2.8) a,B,1 | 40.88 (3.1) a,B,1 |
| M | 48.46 (3.23) a,A,1 | 34.9 (2.95) b,B,1 | 32.53 (0.74) a,B,1 | 35.4 (2.31) b,B,1 | 45.63 (5.64) b,A,1 | 33.57 (1.35) b,B,2 | 35.3 (2.03) b,B,2 | 34.27 (1.55) b,B,1 |
| T | 44.98 (1.73) b,A,1 | 27.44 (4.31) c,B,1 | 33.83 (3.27) a,B,1 | 33.38 (2.31) b,B,1 | 48.91 (8.51) b,A,1 | 35.8 (2.19) b,B,2 | 35.2 (2.88) b,B,1 | 35.7 (2.91) b,B,1 |
| V | 47.14 (5.67) a,A,1 | 32.68 (2.91) b,B,1 | 35.26 (3.54) a,B,1 | 35.47 (2.75) b,B,1 | 50.44 (3.95) b,A,1 | 31.83 (2.02) c,B,1 | 33.67 (2.55) b,B,2 | 34.24 (2.62) b,B,1 |
| Exposure Time | Spacer | |
|---|---|---|
| 150 μm | 350 μm | |
| 2 × 120 s | 32.07 (4.43) a,A | 51.72 (2.03) c,B |
| 3 × 120 s | 38.13 (2.61) b,A | 55.12 (3.14) c,B |
| Controls/preheated | ||
| 60 s | 51.9 (1.15) d | |
| 120 s | 61.18 (2.16) e | |
| Materials | Non-Preheated (μm) | Preheated (μm) | Δ[(H-ΝH)/ΝH] % |
|---|---|---|---|
| F | 423 (11) a,A | 355 (29) b,A | −16.1 |
| M | 261 (23) a,B | 210 (14) b,B | −19.5 |
| T | 202 (12) a,C | 164 (21) b,C | −18.8 |
| V | 237 (13) a,D | 158 (19) b,C | −33.3 |
| Control (Non-preheated) | |||
| E | 104 (11) E | ||
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Dimitriadi, M.; Petropoulou, A.; Papathanasiou, I.; Zinelis, S.; Eliades, G. Modern Light-Cured Restorative Composites as Luting Agents: The Effect of Preheating on Conversion and Film Thickness. Materials 2025, 18, 3721. https://doi.org/10.3390/ma18163721
Dimitriadi M, Petropoulou A, Papathanasiou I, Zinelis S, Eliades G. Modern Light-Cured Restorative Composites as Luting Agents: The Effect of Preheating on Conversion and Film Thickness. Materials. 2025; 18(16):3721. https://doi.org/10.3390/ma18163721
Chicago/Turabian StyleDimitriadi, Maria, Aikaterini Petropoulou, Ioannis Papathanasiou, Spiros Zinelis, and George Eliades. 2025. "Modern Light-Cured Restorative Composites as Luting Agents: The Effect of Preheating on Conversion and Film Thickness" Materials 18, no. 16: 3721. https://doi.org/10.3390/ma18163721
APA StyleDimitriadi, M., Petropoulou, A., Papathanasiou, I., Zinelis, S., & Eliades, G. (2025). Modern Light-Cured Restorative Composites as Luting Agents: The Effect of Preheating on Conversion and Film Thickness. Materials, 18(16), 3721. https://doi.org/10.3390/ma18163721








