Fracture Resistance of 3D-Printed Fixed Partial Dentures: Influence of Connector Size and Materials
Abstract
1. Introduction
- Fracture resistance of FPDs is not influenced by the different 3D-printed material used.
- Fracture resistance of 3D-printed FPDs is not influenced by the connector size of the restoration.
- There is no interaction between material type and connector size that affects the fracture resistance of 3D-printed FPDs.
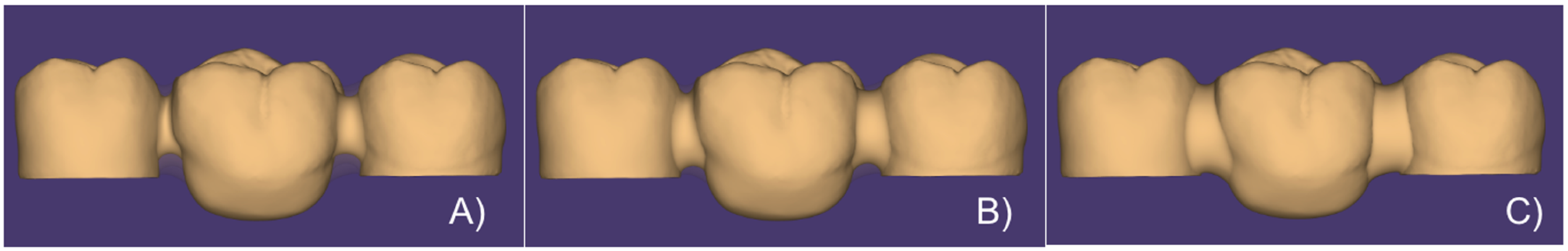
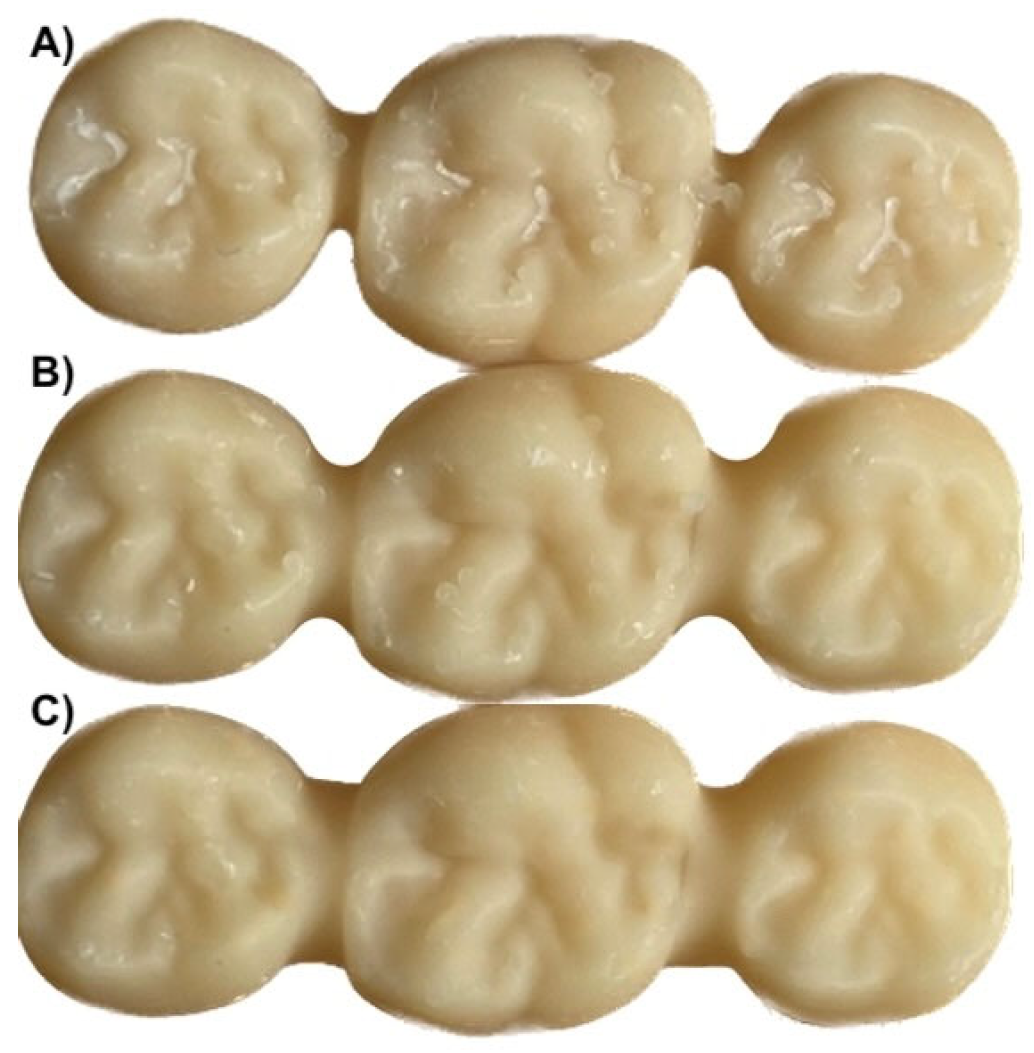
2. Materials and Methods
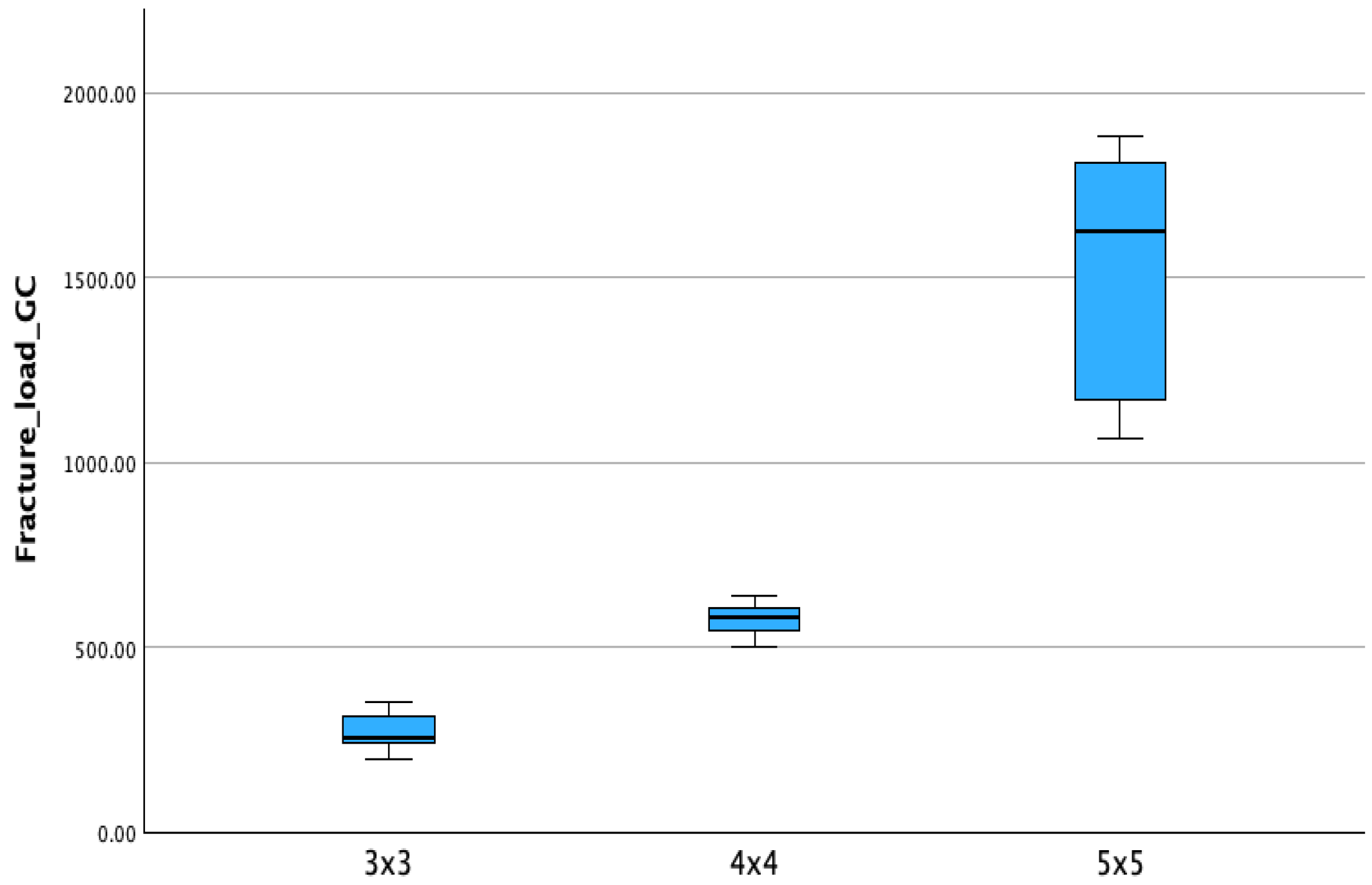
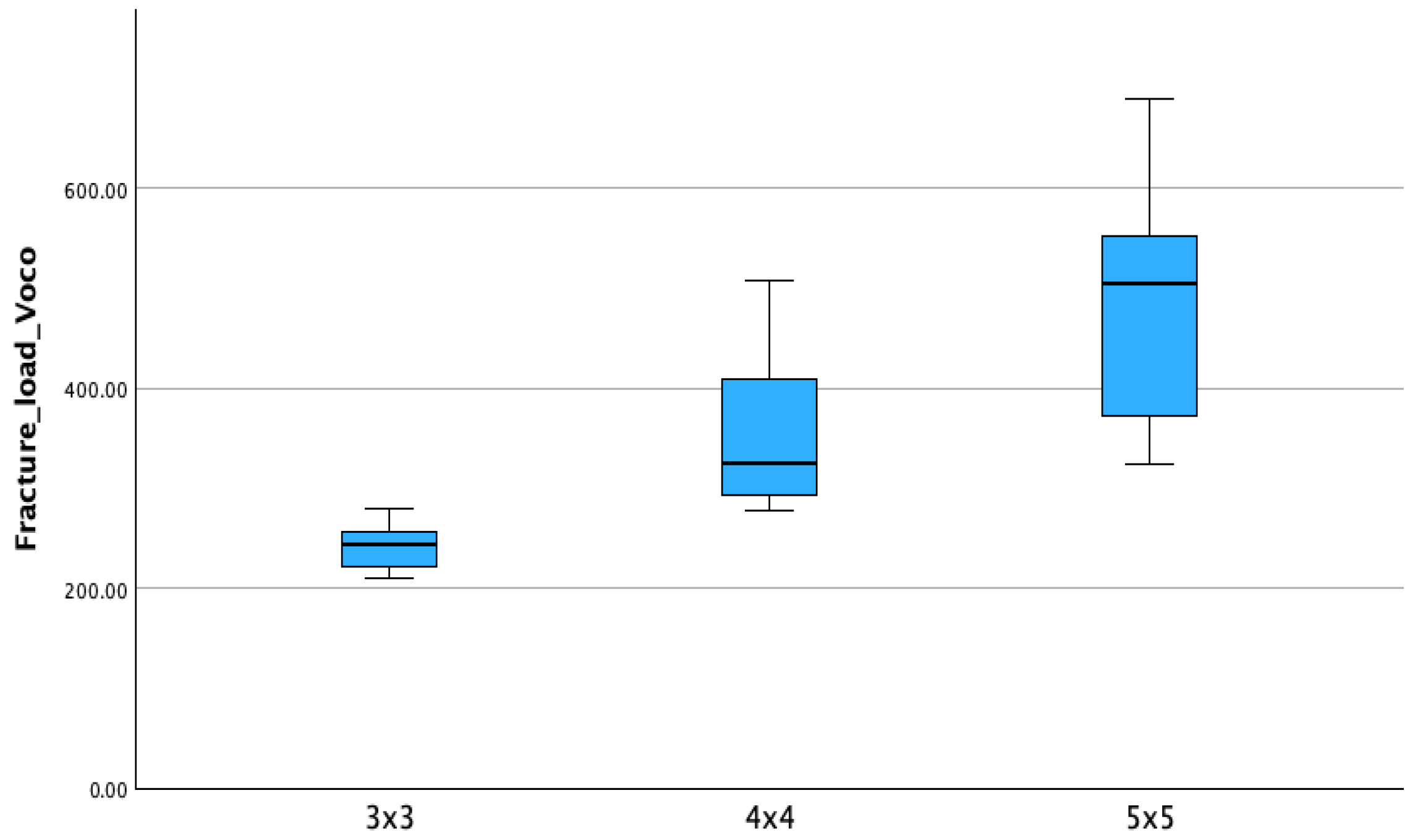
3. Results
4. Discussion
5. Conclusions
- Both material composition and connector size significantly influenced the fracture resistance of 3D-printed posterior fixed partial dentures.
- Temp Print (GC Corp., Tokyo, Japan) resin exhibited superior mechanical performance compared to V-Print c&b temp (Voco GmbH, Cuxhaven, Germany) across all connector dimensions, indicating that resin formulation plays a key role in fracture resistance.
- Increasing the connector size from 3 × 3 mm to 5 × 5 mm led to a substantial improvement in fracture load, with the largest connectors yielding the highest strength values.
- Careful selection of both material and connector design is essential for the clinical success of 3D-printed interim fixed partial dentures, especially in high-load posterior regions.
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Schweiger, J.; Edelhoff, D.; Güth, J.F. 3D Printing in Digital Prosthetic Dentistry: An Overview of Recent Developments in Additive Manufacturing. J. Clin. Med. 2021, 10, 2010. [Google Scholar] [CrossRef]
- Kihara, H.; Sugawara, S.; Yokota, J.; Takafuji, K.; Fukazawa, S.; Tamada, A.; Hatakeyama, W.; Kondo, H. Applications of three-dimensional printers in prosthetic dentistry. J. Oral Sci. 2021, 63, 212–216. [Google Scholar] [CrossRef]
- No-Cortes, J.; Ayres, A.P.; Lima, J.F.; Markarian, R.A.; Attard, N.J.; Cortes, A.R.G. Trueness, 3D Deviation, Time and Cost Comparisons Between Milled and 3D-Printed Resin Single Crowns. Eur. J. Prosthodont. Restor. Dent. 2022, 30, 107–112. [Google Scholar] [PubMed]
- Daher, R.; Ardu, S.; di Bella, E.; Krejci, I.; Duc, O. Efficiency of 3D printed composite resin restorations compared with subtractive materials: Evaluation of fatigue behavior, cost, and time of production. J. Prosthet. Dent. 2024, 131, 943–950. [Google Scholar] [CrossRef]
- Della Bona, A.; Cantelli, V.; Britto, V.T.; Collares, K.F.; Stansbury, J.W. 3D Printing Restorative Materials Using a Stereolithographic Technique: A Systematic Review. Dent. Mater. 2021, 37, 336–350. [Google Scholar] [CrossRef]
- Balestra, D.; Lowther, M.; Goracci, C.; Mandurino, M.; Cortili, S.; Paolone, G.; Louca, C.; Vichi, A. 3D Printed Materials for Permanent Restorations in Indirect Restorative and Prosthetic Dentistry: A Critical Review of the Literature. Materials 2024, 17, 1380. [Google Scholar] [CrossRef]
- Verniani, G.; Casucci, A.; Val, M.; Ruggiero, G.; Manfredini, D.; Ferrari, M.; Ferrari Cagidiaco, E. A Randomized Controlled Clinical Trial on Press, Block Lith ium Disilicate, and 3D Printed Partial Crowns in Posterior Teeth: One-Year Recall. Prosthesis 2024, 6, 887–895. [Google Scholar] [CrossRef]
- Hobbi, P.; Ordueri, T.M.; Öztürk-Bozkurt, F.; Toz-Akalın, T.; Ateş, M.; Özcan, M. 3D-Printed Resin Composite Posterior Fixed Dental Prosthesis: A Prospective Clinical Trial up to 1 Year. Front. Dent. Med. 2024, 5, 1390600. [Google Scholar] [CrossRef]
- Tom, T.; Uthappa, M.A.; Sunny, K.; Begum, F.; Nautiyal, M.C.; Tamore, S. Provisional restorations: An overview of materials used. J. Adv. Clin. Res. Insights 2016, 3, 212–214. [Google Scholar] [CrossRef]
- Vahidi, F. The provisional restoration. Dent. Clin. N. Am. 1987, 31, 363–381. [Google Scholar] [CrossRef]
- Higginbottom, F.L. Quality provisional restorations: A must for successful restorative dentistry. Compend. Contin. Educ. Dent. 1995, 16, 442–447. [Google Scholar] [PubMed]
- Torabi, K.; Farjood, E.; Hamedani, S. Rapid Prototyping Technologies and Their Applications in Prosthodontics: A Review of Literature. J. Dent. 2015, 16, 1–9. [Google Scholar]
- Prause, E.; Malgaj, T.; Kocjan, A.; Beuer, F.; Hey, J.; Jevnikar, P.; Schmidt, F. Mechanical Properties of 3D-Printed and Milled Composite Resins for Definitive Restorations: An In Vitro Comparison of Initial Strength and Fatigue Behavior. J. Esthet. Restor. Dent. 2024, 36, 391–401. [Google Scholar] [CrossRef]
- Martín-Ortega, N.; Sallorenzo, A.; Casajús, J.; Cervera, A.; Revilla-León, M.; Gómez-Polo, M. Fracture Resistance of Additive Manufactured and Milled Implant-Supported Interim Crowns. J. Prosthet. Dent. 2022, 127, 267–274. [Google Scholar] [CrossRef]
- Valenti, C.; Federici, M.I.; Masciotti, F.; Marinucci, L.; Xhimitiku, I.; Cianetti, S.; Pagano, S. Mechanical Properties of 3D Printed Prosthetic Materials Compared with Milled and Conventional Processing: A Systematic Review and Meta-Analysis of In Vitro Studies. J. Prosthet. Dent. 2024, 132, 381–391. [Google Scholar] [CrossRef]
- Casucci, A.; Verniani, G.; Barbieri, A.L.; Ricci, N.M.; Ferrari Cagidiaco, E.; Ferrari, M. Flexural Strength Analysis of Different Complete Denture Resin-Based Materials Obtained by Conventional and Digital Manufacturing. Materials 2023, 16, 6559. [Google Scholar] [CrossRef]
- Zimmermann, M.; Ender, A.; Egli, G.; Özcan, M.; Mehl, A. Fracture Load of CAD/CAM-Fabricated and 3D-Printed Composite Crowns as a Function of Material Thickness. Clin. Oral Investig. 2019, 23, 2777–2784. [Google Scholar] [CrossRef]
- Corbani, K.; Hardan, L.; Skienhe, H.; Özcan, M.; Alharbi, N.; Salameh, Z. Effect of Material Thickness on the Fracture Resistance and Failure Pattern of 3D-Printed Composite Crowns. Int. J. Comput. Dent. 2020, 23, 225–233. [Google Scholar]
- Anusavice, K.J.; Shen, C.; Rawls, H.R. Phillips’ Science of Dental Materials, 12th ed.; Elsevier: Amsterdam, The Netherlands, 2013. [Google Scholar]
- Casucci, A.; Verniani, G.; Haichal, W.S.; Manfredini, D.; Ferrari, M.; Cagidiaco, E.F. Influence of printing angulation on the flexural strength of 3D printed resins: An in vitro study. Appl. Sci. 2024, 14, 10067. [Google Scholar] [CrossRef]
- ISO 4049:2019; Dentistry—Polymer-Based Restorative Materials. ISO: Geneva, Switzerland, 2019.
- Myagmar, G.; Lee, J.H.; Ahn, J.S.; Yeo, I.L.; Yoon, H.I.; Han, J.S. Wear of 3D printed and CAD/CAM milled interim resin materials after chewing simulation. J. Adv. Prosthodont. 2021, 13, 144–151. [Google Scholar] [CrossRef]
- Dimova-Gabrovska, M.; Uzunov, T.; Gusiyska, A.; Shopova, D.; Taneva, I.; Gerdzhikov, I.; Rangelov, S. Exploring Flexural Strength Variation in Polymeric Materials for Provisional Fixed Prosthetic Structures: Comparative Analysis with and without Reinforcement through Laboratory Experimentation and Statistical Evaluation. Appl. Sci. 2024, 14, 3923. [Google Scholar] [CrossRef]
- Gad, M.M.; Fouda, S.M. Factors Affecting Flexural Strength of 3D-Printed Resins: A Systematic Review. J. Prosthodont. 2023, 32, 96–110. [Google Scholar] [CrossRef]
- Singh, A.; Garg, S. Comparative Evaluation of Flexural Strength of Provisional Crown and Bridge Materials-An Invitro Study. J. Clin. Diagn Res. 2016, 10, ZC72–ZC77. [Google Scholar] [CrossRef] [PubMed]
- Shaikh, S.A.; Rai, P.; Aldhuwayhi, S.; Mallineni, S.K.; Lekha, K.; Joseph, A.M.; Kumari, V.V.; Meshramkar, R. Comparative Evaluation of Stress Acting on Abutment, Bone, and Connector of Different Designs of Acid-Etched Resin-Bonded Fixed Partial Dentures: Finite Element Analysis. Front. Bioeng. Biotechnol. 2022, 10, 798988. [Google Scholar] [CrossRef]
- Onodera, K.; Sato, T.; Nomoto, S.; Miho, O.; Yotsuya, M. Effect of Connector Design on Fracture Resistance of Zirconia All-Ceramic Fixed Partial Dentures. Bull. Tokyo Dent. Coll. 2011, 52, 61–67. [Google Scholar] [CrossRef]
- Lakshmi, R.D.; Abraham, A.; Sekar, V.; Hariharan, A. Influence of Connector Dimensions on the Stress Distribution of Monolithic Zirconia and Lithium-Disilicate Inlay Retained Fixed Dental Prostheses–A 3D Finite Element Analysis. Tanta Dent. J. 2015, 12, 56–64. [Google Scholar] [CrossRef]
- De Angelis, F.; D’Arcangelo, C.; Vadini, M. The Effect of Dentin Bonding and Material Thickness on the Flexural Properties of a Lithium-Disilicate Glass-Ceramic. J. Adhes. Dent. 2021, 23, 309–318. [Google Scholar]
- Greuling, A.; Matthies, A.; Eisenburger, M. Fracture Load of 4-Unit Interim Fixed Partial Dentures Using 3D-Printed and Traditionally Manufactured Materials. J. Prosthet. Dent. 2023, 129, 607.e1–607.e8. [Google Scholar] [CrossRef]
- Shah, R.; Patel, K.; Patel, M. Influence of connector design and cross-sectional shape on stress distribution in posterior fixed partial dentures: A 3D FEA and experimental study. J. Indian Prosthodont. Soc. 2014, 14 (Suppl. 1), S151–S158. [Google Scholar]
- Oh, W.S.; Anusavice, K.J. Effect of connector design on the fracture resistance of all-ceramic fixed partial dentures. J. Prosthet. Dent. 2002, 87, 536–542. [Google Scholar] [CrossRef]
- Ikejima, I.; Nomoto, R.; McCabe, J.F. Shear Punch Strength and Flexural Strength of Model Composites with Varying Filler Volume Fraction, Particle Size and Silanation. Dent. Mater. 2003, 19, 206–211. [Google Scholar] [CrossRef]
- Weng, Z.; Zhou, Y.; Lin, W.; Senthil, T.; Wu, L. Structure-Property Relationship of Nano Enhanced Stereolithography Resin for Desktop SLA 3D Printer. Compos. Part A Appl. Sci. Manuf. 2016, 88, 234–242. [Google Scholar] [CrossRef]
- Reymus, M.; Fabritius, R.; Keßler, A.; Hickel, R.; Edelhoff, D.; Stawarczyk, B. Fracture Load of 3D-Printed Fixed Dental Prostheses Compared with Milled and Conventionally Fabricated Ones: The Impact of Resin Material, Build Direction, Post-Curing, and Artificial Aging—An In Vitro Study. Clin. Oral Investig. 2020, 24, 701–710. [Google Scholar] [CrossRef]
- Ibrahim, A.; El Shehawy, D.; El-Naggar, G. Fracture Resistance of Interim Restoration Constructed by 3D Printing Versus CAD/CAM Technique (In Vitro Study). Ain Shams Dent. J. 2020, 23, e14–e20. [Google Scholar]
- Piedra-Cascón, W.; Krishnamurthy, V.R.; Att, W.; Revilla-León, M. 3D Printing Parameters, Supporting Structures, Slicing, and Post-Processing Procedures of Vat-Polymerization Additive Manufacturing Technologies: A Narrative Review. J. Dent. 2021, 109, 103630. [Google Scholar] [CrossRef] [PubMed]
- Fan, Y.; Shu, X.; Leung, K.C.M.; Lo, E.C.M. Associations of general health conditions with masticatory performance and maximum bite force in older adults: A systematic review of cross-sectional studies. J. Dent. 2022, 123, 104186. [Google Scholar] [CrossRef] [PubMed]
- Ferrario, V.F.; Sforza, C.; Zanotti, G.; Tartaglia, G.M. Maximal Bite Forces in Healthy Young Adults as Predicted by Surface Electromyography. J. Dent. 2004, 32, 451–457. [Google Scholar] [CrossRef]
- Denry, I.; Kelly, J.R. State of the art of zirconia for dental applications. Dent. Mater. 2008, 24, 299–307. [Google Scholar] [CrossRef]
- Hong, S.; Park, J.; Lee, J.; Lee, H.; Lee, D. Mechanical properties of cobalt-chromium alloys fabricated by selective laser melting and casting for dental prostheses. Materials 2020, 13, 5414. [Google Scholar] [CrossRef]
- Al-Harbi, F.A.; Kara, H.B.; Barazanchi, A.; McMillan, A.S.; Waddell, J.N. Mechanical properties of 3D-printed provisional restorative materials compared with CAD/CAM and conventional resins. J. Prosthodont. 2016, 25, 618–624. [Google Scholar]
- Hobbi, P.; Ordueri, T.M.; Öztürk-Bozkurt, F.; Toz-Akalın, T.; Ateş, M.M.; Özcan, M. Assessing the performance of 3D-printed resin composite posterior fixed dental prostheses: A 3-year prospective clinical trial. J. Dent. 2025, 160, 105887. [Google Scholar] [CrossRef]
- Haselton, D.R.; Diaz-Arnold, A.M.; Vargas, M.A. Flexural strength of provisional crown and fixed partial denture resins. J. Prosthet. Dent. 2002, 87, 225–228. [Google Scholar] [CrossRef]
- Sharma, S.P.; Jain, A.R.; Balasubramanian, R.; Alavandar, S.; Manoharan, P.S. An in vitro evaluation of flexural strength of two provisional restorative materials: Light polymerised resin and autopolymerised resin. IOSR J. Dent. Med. Sci. 2013, 6, 5–10. [Google Scholar] [CrossRef]
- Rand, A.; Kohorst, P.; Greuling, A.; Borchers, L.; Stiesch, M. Stress Distribution in All-Ceramic Posterior 4-Unit Fixed Dental Prostheses Supported in Different Ways: Finite Element Analysis. Implant Dent. 2016, 25, 485–491. [Google Scholar] [CrossRef] [PubMed]



| Product Name | Manufacturer | Components | Batch | Properties Provided by the Manufacturer |
|---|---|---|---|---|
| Temp PRINT | GC Corp., Tokyo, Japan | Urethane dimethacrylate (UDMA) dimethacrylate component quartz (SiO2) photoinitiator synergist UV-light absorber. | 10004797 | Viscosity 0.5–2.0 Pa s; density 1.1–1.3 g/mm3; flexural strength > 90 MPa; sorption < 40 µg/mm3; solubility < 7.5 µg/mm3; layer thickness 50 µm; light wavelength 385–405 nm. |
| V-Print c&b temp | Voco GmbH, Cuxhaven, Germany | UDMA Bis-EMA TEGDMA 50–100% 25–50% 5–10% 4,4-Isopropylidenediphenol, ethoxylated 2-methylprop-2enoic acid, benzeneacetic acid, alpha. | 6897 | Viscosity 2.80 Pa s; flexural strength 132 MPa (DIN EN ISO 10477); modulus of elasticity 4417 MPa (DIN EN ISO 178); water absorption 17.63 µg/mm3 (DIN EN ISO 10477); water solubility 0.68 µg/mm3 (DIN EN ISO 10477); filler content 26% by weight. |
| Material | Mean (N) ± SD | Sign. |
|---|---|---|
| Temp Print | 792.34 ± 578.36 | A |
| V-Print | 359.74 ± 131.64 | B |
| Connector | Mean (N) ± SD | Sign. |
|---|---|---|
| 3 × 3 | 254.72 ± 40.65 | C |
| 4 × 4 | 464.07 ± 130.00 | B |
| 5 × 5 | 1037.99 ± 589.93 | A |
| Connector | Temp Print (N) ± SD | V-Print (N) ± SD | p-Value |
|---|---|---|---|
| 3 × 3 | 266.09 ± 50.79 A,a | 242.09 ± 21.81 A,a | 0.414 |
| 4 × 4 | 576.82 ± 41.72 B,a | 351.32 ± 75.41 B,b | <0.001 |
| 5 × 5 | 1534.12 ± 320.68 C,a | 486.74 ± 133.43 C,b | <0.001 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Verniani, G.; Ferrari Cagidiaco, E.; Alavi Tabatabaei, S.; Casucci, A. Fracture Resistance of 3D-Printed Fixed Partial Dentures: Influence of Connector Size and Materials. Materials 2025, 18, 3468. https://doi.org/10.3390/ma18153468
Verniani G, Ferrari Cagidiaco E, Alavi Tabatabaei S, Casucci A. Fracture Resistance of 3D-Printed Fixed Partial Dentures: Influence of Connector Size and Materials. Materials. 2025; 18(15):3468. https://doi.org/10.3390/ma18153468
Chicago/Turabian StyleVerniani, Giulia, Edoardo Ferrari Cagidiaco, SeyedReza Alavi Tabatabaei, and Alessio Casucci. 2025. "Fracture Resistance of 3D-Printed Fixed Partial Dentures: Influence of Connector Size and Materials" Materials 18, no. 15: 3468. https://doi.org/10.3390/ma18153468
APA StyleVerniani, G., Ferrari Cagidiaco, E., Alavi Tabatabaei, S., & Casucci, A. (2025). Fracture Resistance of 3D-Printed Fixed Partial Dentures: Influence of Connector Size and Materials. Materials, 18(15), 3468. https://doi.org/10.3390/ma18153468






