Stress Distribution within the Peri-Implant Bone for Different Implant Materials Obtained by Digital Image Correlation
Abstract
1. Introduction
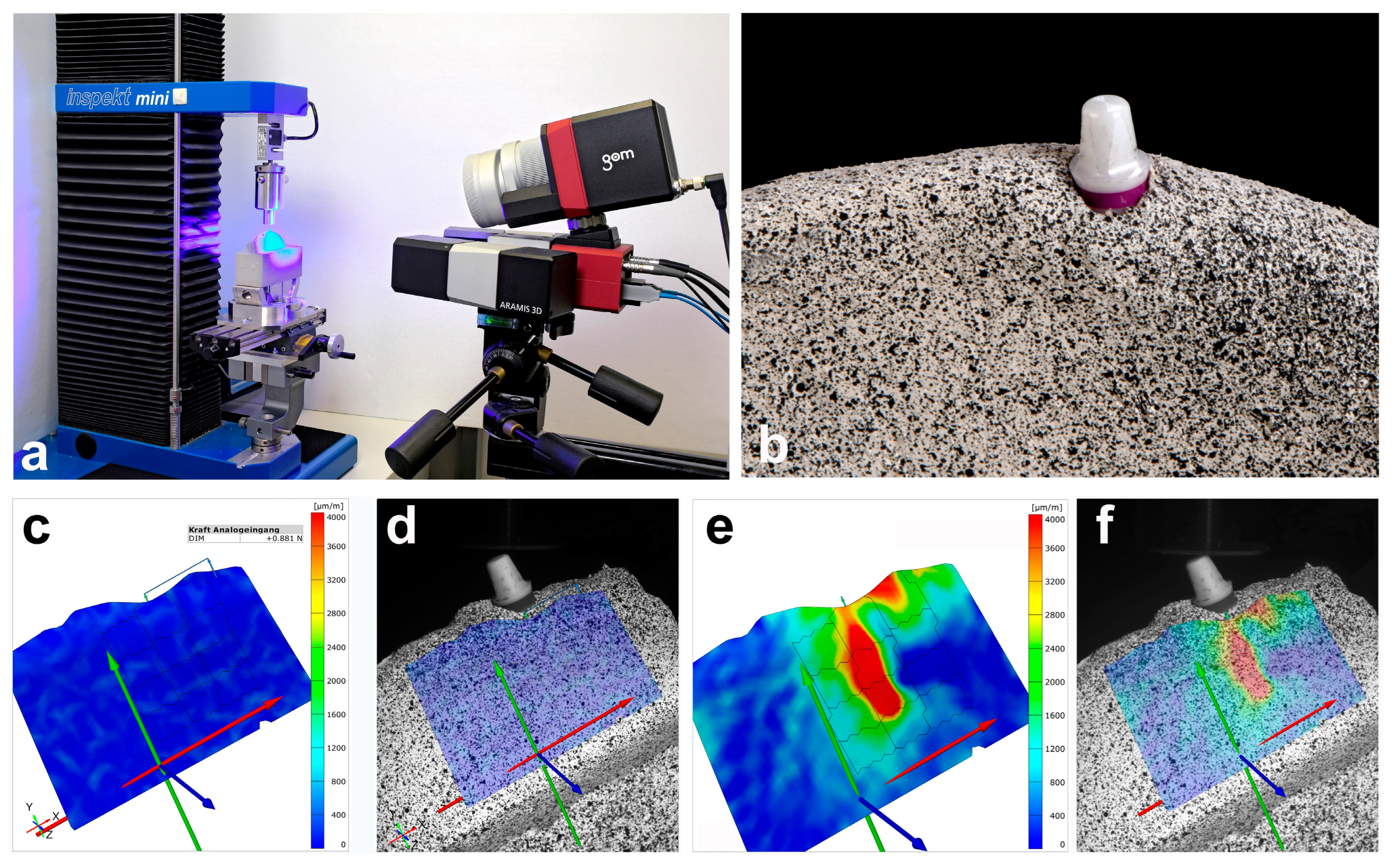
2. Materials and Methods
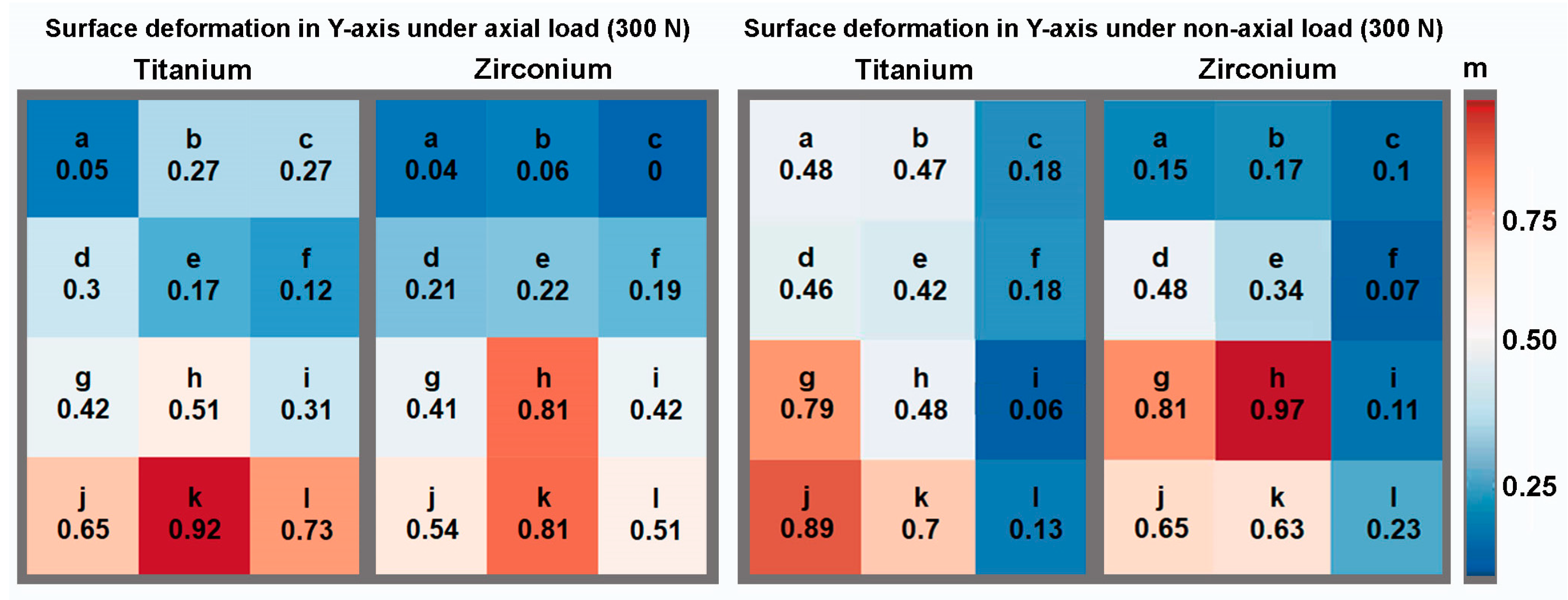
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Branemark, P.I.; Adell, R.; Breine, U.; Hansson, B.O.; Lindstrom, J.; Ohlsson, A. Intra-osseous anchorage of dental prostheses. I. Experimental studies. Scand. J. Plast. Reconstr. Surg. 1969, 3, 81–100. [Google Scholar] [CrossRef] [PubMed]
- Assif, D.; Marshak, B.; Horowitz, A. Analysis of load transfer and stress distribution by an implant-supported fixed partial denture. J. Prosthet. Dent. 1996, 75, 285–291. [Google Scholar] [CrossRef] [PubMed]
- Frost, H.M. Wolff’s Law and bone’s structural adaptations to mechanical usage: An overview for clinicians. Angle Orthod. 1994, 64, 175–188. [Google Scholar] [CrossRef] [PubMed]
- Wiskott, H.W.; Belser, U.C. Lack of integration of smooth titanium surfaces: A working hypothesis based on strains generated in the surrounding bone. Clin. Oral Implants Res. 1999, 10, 429–444. [Google Scholar] [CrossRef] [PubMed]
- Frost, H.M. A 2003 update of bone physiology and Wolff’s Law for clinicians. Angle Orthod. 2004, 74, 3–15. [Google Scholar] [CrossRef] [PubMed]
- Cehreli, M.C.; Iplikcioglu, H.; Bilir, O.G. The influence of the location of load transfer on strains around implants supporting four unit cement-retained fixed prostheses: In vitro evaluation of axial versus off-set loading. J. Oral Rehabil. 2002, 29, 394–400. [Google Scholar] [CrossRef]
- Lee, J.H.; Frias, V.; Lee, K.W.; Wright, R.F. Effect of implant size and shape on implant success rates: A literature review. J. Prosthet. Dent. 2005, 94, 377–381. [Google Scholar] [CrossRef]
- Nishioka, R.S.; Nishioka, L.N.; Abreu, C.W.; de Vasconcellos, L.G.; Balducci, I. Machined and plastic copings in three-element prostheses with different types of implant-abutment joints: A strain gauge comparative analysis. J. Appl. Oral Sci. 2010, 18, 225–230. [Google Scholar] [CrossRef]
- de Vasconcellos, L.G.; Nishioka, R.S.; de Vasconcellos, L.M.; Balducci, I.; Kojima, A.N. Microstrain around dental implants supporting fixed partial prostheses under axial and non-axial loading conditions, in vitro strain gauge analysis. J. Craniofacial Surg. 2013, 24, e546–e551. [Google Scholar] [CrossRef]
- Kheiralla, L.S.; Younis, J.F. Peri-implant biomechanical responses to standard, short-wide, and mini implants supporting single crowns under axial and off-axial loading (an in vitro study). J. Oral Implantol. 2014, 40, 42–52. [Google Scholar] [CrossRef]
- Fabris, D.; Moura, J.P.A.; Fredel, M.C.; Souza, J.C.M.; Silva, F.S.; Henriques, B. Biomechanical analyses of one-piece dental implants composed of titanium, zirconia, PEEK, CFR-PEEK, or GFR-PEEK: Stresses, strains, and bone remodeling prediction by the finite element method. J. Biomed. Mater. Res. B Appl. Biomater. 2022, 110, 79–88. [Google Scholar] [CrossRef] [PubMed]
- Osman, R.B.; Swain, M.V. A Critical Review of Dental Implant Materials with an Emphasis on Titanium versus Zirconia. Materials 2015, 8, 932–958. [Google Scholar] [CrossRef] [PubMed]
- Khaohoen, A.; Sornsuwan, T.; Chaijareenont, P.; Poovarodom, P.; Rungsiyakull, C.; Rungsiyakull, P. Biomaterials and Clinical Application of Dental Implants in Relation to Bone Density-A Narrative Review. J. Clin. Med. 2023, 12, 6924. [Google Scholar] [CrossRef] [PubMed]
- Albrektsson, T.; Jacobsson, M. Bone-metal interface in osseointegration. J. Prosthet. Dent. 1987, 57, 597–607. [Google Scholar] [CrossRef] [PubMed]
- Palmquist, A.; Omar, O.M.; Esposito, M.; Lausmaa, J.; Thomsen, P. Titanium oral implants: Surface characteristics, interface biology and clinical outcome. J. R. Soc. Interface 2010, 7 (Suppl. S5), S515–S527. [Google Scholar] [CrossRef]
- Hoque, M.E.; Showva, N.N.; Ahmed, M.; Rashid, A.B.; Sadique, S.E.; El-Bialy, T.; Xu, H. Titanium and titanium alloys in dentistry: Current trends, recent developments, and future prospects. Heliyon 2022, 8, e11300. [Google Scholar] [CrossRef]
- Binon, P.P. Implants and components: Entering the new millennium. Int. J. Oral Maxillofac. Implants 2000, 15, 76–94. [Google Scholar] [PubMed]
- Jung, R.E.; Sailer, I.; Hammerle, C.H.; Attin, T.; Schmidlin, P. In vitro color changes of soft tissues caused by restorative materials. Int. J. Periodontics Restor. Dent. 2007, 27, 251–257. [Google Scholar]
- Sevimay, M.; Turhan, F.; Kilicarslan, M.A.; Eskitascioglu, G. Three-dimensional finite element analysis of the effect of different bone quality on stress distribution in an implant-supported crown. J. Prosthet. Dent. 2005, 93, 227–234. [Google Scholar] [CrossRef]
- Manzano, G.; Herrero, L.R.; Montero, J. Comparison of clinical performance of zirconia implants and titanium implants in animal models: A systematic review. Int. J. Oral Maxillofac. Implants 2014, 29, 311–320. [Google Scholar] [CrossRef]
- Wenz, H.J.; Bartsch, J.; Wolfart, S.; Kern, M. Osseointegration and clinical success of zirconia dental implants: A systematic review. Int. J. Prosthodont. 2008, 21, 27–36. [Google Scholar] [PubMed]
- Roehling, S.; Astasov-Frauenhoffer, M.; Hauser-Gerspach, I.; Braissant, O.; Woelfler, H.; Waltimo, T.; Kniha, H.; Gahlert, M. In Vitro Biofilm Formation on Titanium and Zirconia Implant Surfaces. J. Periodontol. 2017, 88, 298–307. [Google Scholar] [CrossRef] [PubMed]
- Happe, A.; Schulte-Mattler, V.; Strassert, C.; Naumann, M.; Stimmelmayr, M.; Zoller, J.E.; Rothamel, D. In vitro color changes of soft tissues caused by dyed fluorescent zirconia and nondyed, nonfluorescent zirconia in thin mucosa. Int. J. Periodontics Restor. Dent. 2013, 33, e1–e8. [Google Scholar] [CrossRef] [PubMed]
- Kohal, R.J.; Knauf, M.; Larsson, B.; Sahlin, H.; Butz, F. One-piece zirconia oral implants: One-year results from a prospective cohort study. 1. Single tooth replacement. J. Clin. Periodontol. 2012, 39, 590–597. [Google Scholar] [CrossRef] [PubMed]
- Jung, R.E.; Grohmann, P.; Sailer, I.; Steinhart, Y.N.; Feher, A.; Hammerle, C.; Strub, J.R.; Kohal, R. Evaluation of a one-piece ceramic implant used for single-tooth replacement and three-unit fixed partial dentures: A prospective cohort clinical trial. Clin. Oral Implants Res. 2016, 27, 751–761. [Google Scholar] [CrossRef] [PubMed]
- Kohal, R.J.; Finke, H.C.; Klaus, G. Stability of prototype two-piece zirconia and titanium implants after artificial aging: An in vitro pilot study. Clin. Implant Dent. Relat. Res. 2009, 11, 323–329. [Google Scholar] [CrossRef] [PubMed]
- Sannino, G.; Gloria, F.; Ottria, L.; Barlattani, A. Influence of finish line in the distribution of stress trough an all ceramic implant-supported crown.: A 3D Finite Element Analysis. Oral Implantol. 2009, 2, 14–27. [Google Scholar]
- Lopez, C.A.V.; Vasco, M.A.A.; Ruales, E.; Bedoya, K.A.; Benfatti, C.M.; Bezzon, O.L.; Deliberador, T.M. Three-Dimensional Finite Element Analysis of Stress Distribution in Zirconia and Titanium Dental Implants. J. Oral Implantol. 2018, 44, 409–415. [Google Scholar] [CrossRef] [PubMed]
- Brenner, S.C. The Mathematical Theory of Finite Element Methods, 3rd ed.; Springer: New York, NY, USA, 2008; p. 96. [Google Scholar]
- Matta, R.E.; Riegger, K.; Trägler, H.; Adler, W.; Eitner, S.; Wichmann, M.; Motel, C. Establishment of a New Biomechanical Measurement Method for Surface Deformation of Bone by Force Application via Dental Implants—A Pilot Study. Appl. Sci. 2021, 11, 7568. [Google Scholar] [CrossRef]
- Bakalarz, M.M.; Tworzewski, P.P. Application of Digital Image Correlation to Evaluate Strain, Stiffness and Ductility of Full-Scale LVL Beams Strengthened by CFRP. Materials 2023, 16, 1309. [Google Scholar] [CrossRef]
- Goellner, M.; Berthold, C.; Holst, S.; Wichmann, M.; Schmitt, J. Correlations between photogrammetric measurements of tooth mobility and the Periotest method. Acta Odontol. Scand. 2012, 70, 27–35. [Google Scholar] [CrossRef] [PubMed]
- Lezaja, M.; Veljovic, D.; Manojlovic, D.; Milosevic, M.; Mitrovic, N.; Janackovic, D.; Miletic, V. Bond strength of restorative materials to hydroxyapatite inserts and dimensional changes of insert-containing restorations during polymerization. Dent. Mater. 2015, 31, 171–181. [Google Scholar] [CrossRef] [PubMed]
- Miletic, V.; Peric, D.; Milosevic, M.; Manojlovic, D.; Mitrovic, N. Local deformation fields and marginal integrity of sculptable bulk-fill, low-shrinkage and conventional composites. Dent. Mater. 2016, 32, 1441–1451. [Google Scholar] [CrossRef] [PubMed]
- Haseeb, S.A.; Vinaya, K.C.; Vijaykumar, N.; Sree Durga, B.A.; Kumar, A.S.; Sruthi, M.K. Finite element evaluation to compare stress pattern in bone surrounding implant with carbon fiber-reinforced poly-ether-ether-ketone and commercially pure titanium implants. Natl. J. Maxillofac. Surg. 2022, 13, 243–247. [Google Scholar] [CrossRef] [PubMed]
- Wight, C.M.; Schemitsch, E.H. In vitro testing for hip head-neck taper tribocorrosion: A review of experimental methods. Proc. Inst. Mech. Eng. Part H 2022, 236, 9544119221074582. [Google Scholar] [CrossRef]
- Masoomi, F.; Mahboub, F. Stress distribution pattern in all-on-four maxillary restorations supported by porous tantalum and solid titanium implants using three-dimensional finite element analysis. Eur. J. Transl. Myol. 2024, 34. [Google Scholar] [CrossRef] [PubMed]
- Tribst, J.P.M.; Dal Piva, A.M.O.; Ozcan, M.; Borges, A.L.S.; Bottino, M.A. Influence of Ceramic Materials on Biomechanical Behavior of Implant Supported Fixed Prosthesis with Hybrid Abutment. Eur. J. Prosthodont. Restor. Dent. 2019, 27, 76–82. [Google Scholar] [CrossRef] [PubMed]
- Boldt, J.; Knapp, W.; Proff, P.; Rottner, K.; Richter, E.J. Measurement of tooth and implant mobility under physiological loading conditions. Ann. Anat. 2012, 194, 185–189. [Google Scholar] [CrossRef] [PubMed]
- Pilliar, R.M.; Lee, J.M.; Maniatopoulos, C. Observations on the effect of movement on bone ingrowth into porous-surfaced implants. Clin. Orthop. Relat. Res. 1986, 208, 108–113. [Google Scholar] [CrossRef]
- Brunski, J.B. Biomechanical factors affecting the bone-dental implant interface. Clin. Mater. 1992, 10, 153–201. [Google Scholar] [CrossRef]
- Kao, H.C.; Gung, Y.W.; Chung, T.F.; Hsu, M.L. The influence of abutment angulation on micromotion level for immediately loaded dental implants: A 3-D finite element analysis. Int. J. Oral Maxillofac. Implants 2008, 23, 623–630. [Google Scholar] [PubMed]
- Sakka, S.; Baroudi, K.; Nassani, M.Z. Factors associated with early and late failure of dental implants. J. Investig. Clin. Dent. 2012, 3, 258–261. [Google Scholar] [CrossRef] [PubMed]
- Duyck, J.; Vandamme, K. The effect of loading on peri-implant bone: A critical review of the literature. J. Oral Rehabil. 2014, 41, 783–794. [Google Scholar] [CrossRef] [PubMed]
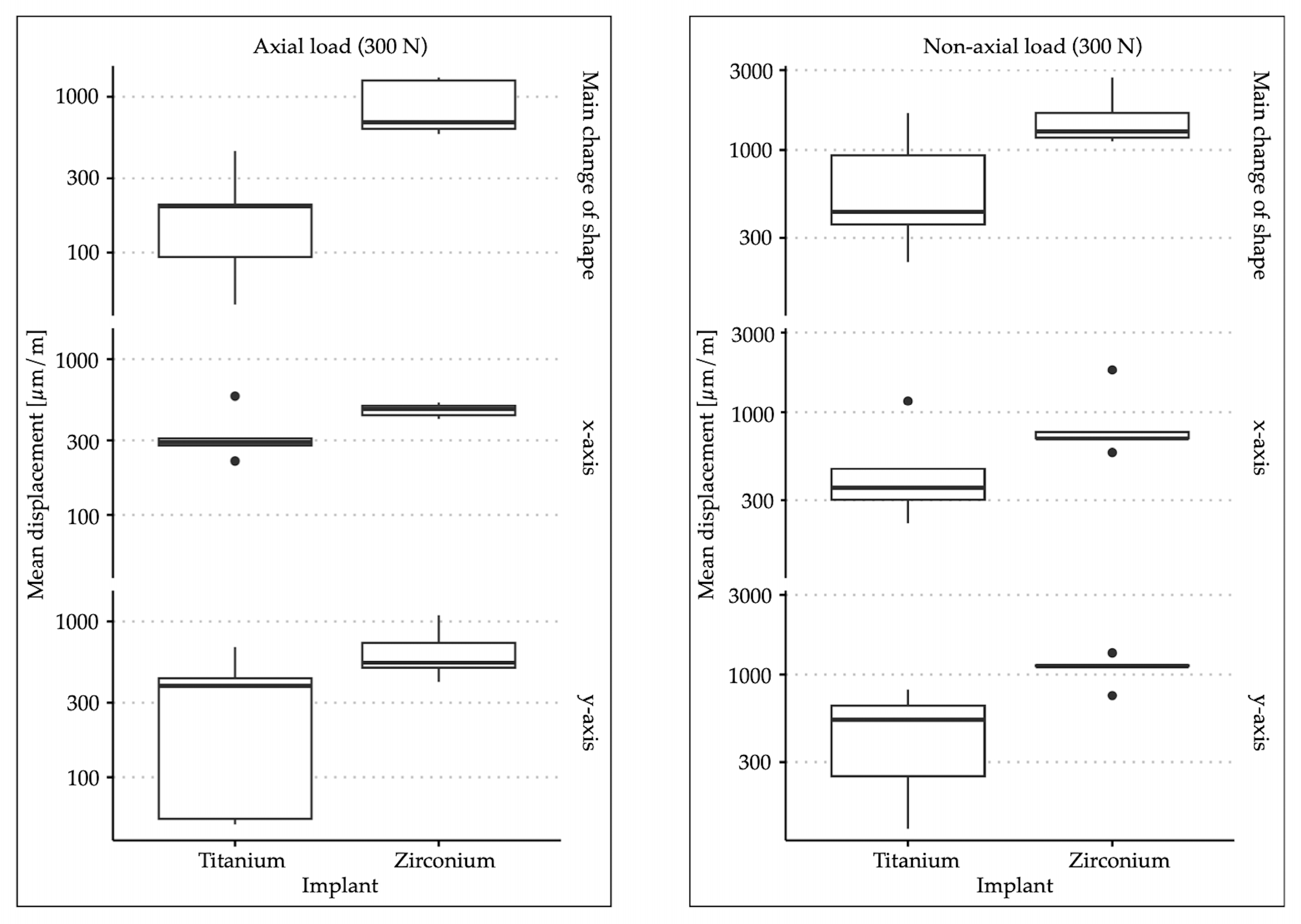
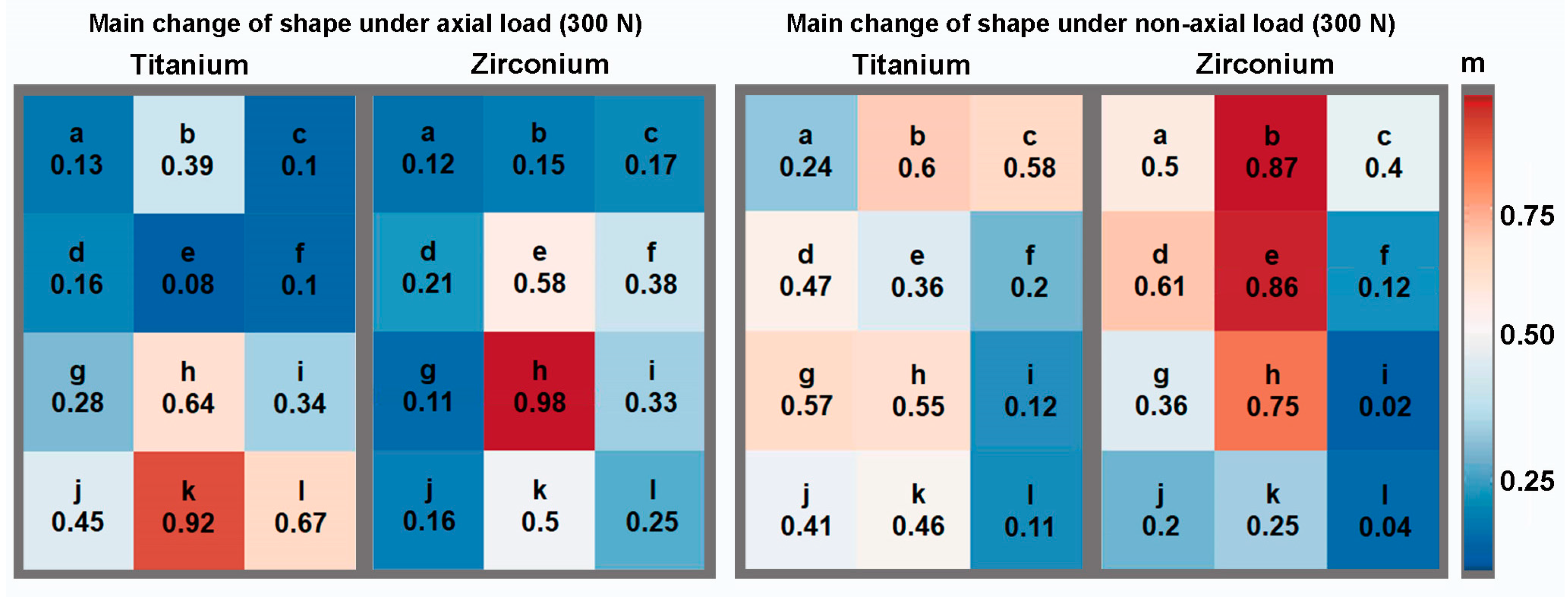
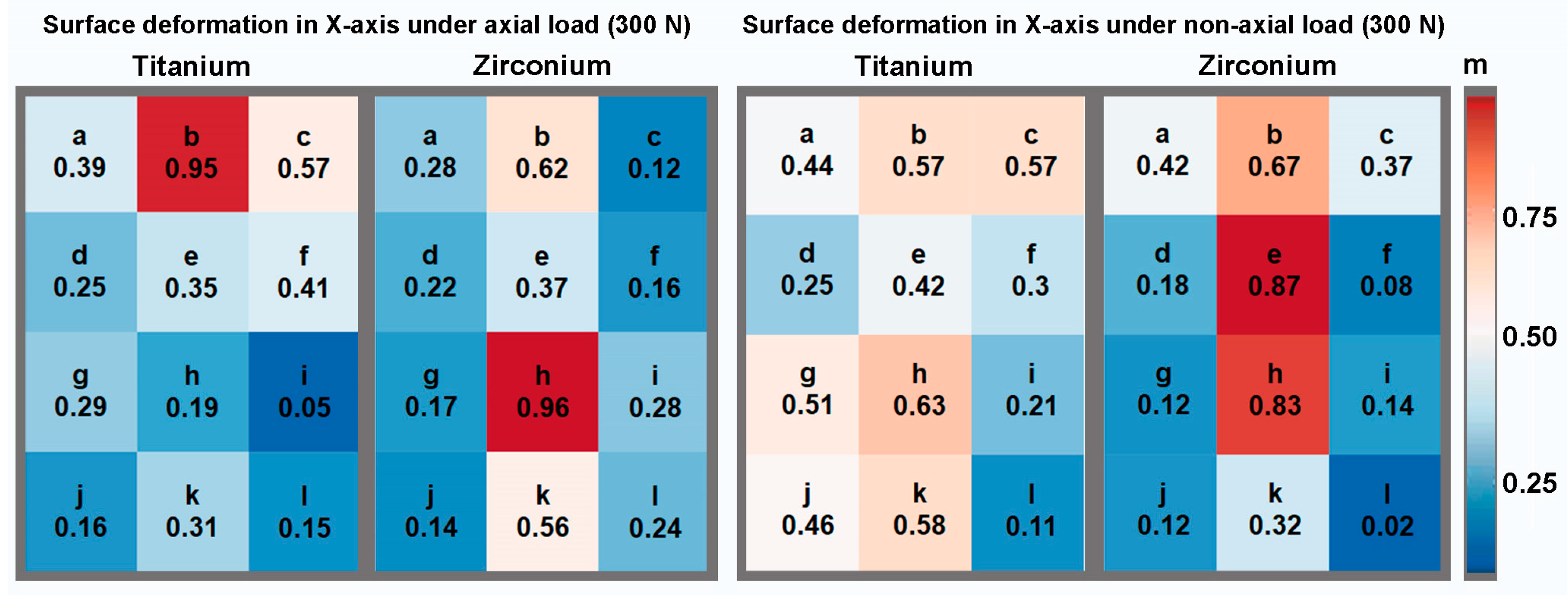
| Material | Angulation | Main Change in Shape | Change in Shape in X-axis | Change in Shape in Y-axis | |||
|---|---|---|---|---|---|---|---|
| Mean | SD | Mean | SD | Mean | SD | ||
| Titanium | 0° | 198.38 | 155.57 | 336.02 | 139.62 | 320.9 | 270.41 |
| 30° | 720.77 | 594.95 | 501.09 | 383.49 | 475.05 | 287.1 | |
| Zirconium | 0° | 898.95 | 373.53 | 471.83 | 47.25 | 654.69 | 271.02 |
| 30° | 1601.46 | 661.08 | 906.31 | 499.68 | 1095.38 | 216.24 | |
| Angulation | Dimension | p-Value |
|---|---|---|
| 0° | main change in shape | 0.009 |
| X-axis | 0.1172 | |
| Y-axis | 0.0758 | |
| 30° | main change in shape | 0.0472 |
| X-axis | 0.0758 | |
| Y-axis | 0.0163 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Matta, R.E.; Berger, L.; Loehlein, M.; Leven, L.; Taxis, J.; Wichmann, M.; Motel, C. Stress Distribution within the Peri-Implant Bone for Different Implant Materials Obtained by Digital Image Correlation. Materials 2024, 17, 2161. https://doi.org/10.3390/ma17092161
Matta RE, Berger L, Loehlein M, Leven L, Taxis J, Wichmann M, Motel C. Stress Distribution within the Peri-Implant Bone for Different Implant Materials Obtained by Digital Image Correlation. Materials. 2024; 17(9):2161. https://doi.org/10.3390/ma17092161
Chicago/Turabian StyleMatta, Ragai Edward, Lara Berger, Moritz Loehlein, Linus Leven, Juergen Taxis, Manfred Wichmann, and Constantin Motel. 2024. "Stress Distribution within the Peri-Implant Bone for Different Implant Materials Obtained by Digital Image Correlation" Materials 17, no. 9: 2161. https://doi.org/10.3390/ma17092161
APA StyleMatta, R. E., Berger, L., Loehlein, M., Leven, L., Taxis, J., Wichmann, M., & Motel, C. (2024). Stress Distribution within the Peri-Implant Bone for Different Implant Materials Obtained by Digital Image Correlation. Materials, 17(9), 2161. https://doi.org/10.3390/ma17092161







