Comparison of Dental Zirconium Oxide Ceramics Produced Using Additive and Removal Technology for Prosthodontics and Restorative Dentistry—Strength and Surface Tests: An In Vitro Study
Abstract
:1. Introduction
2. Materials and Methods
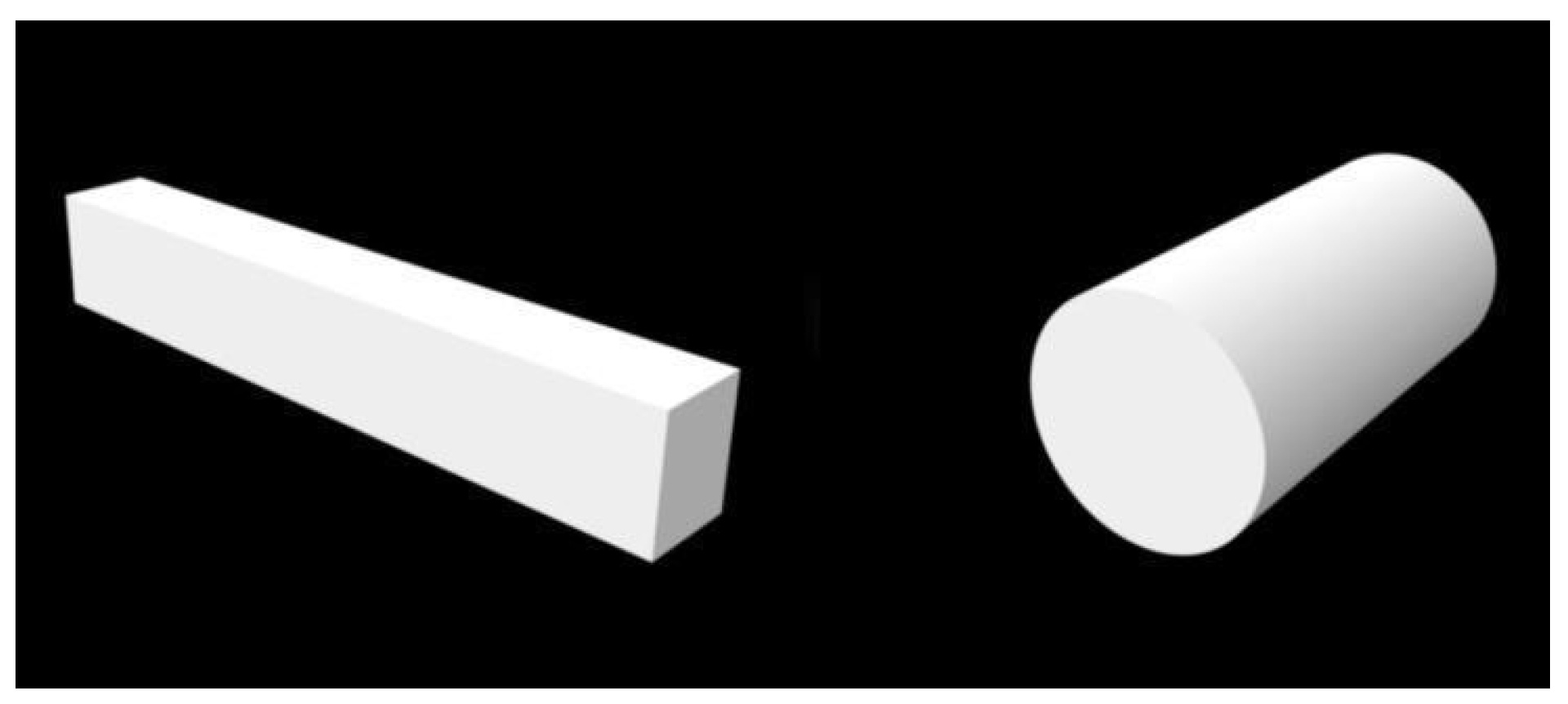
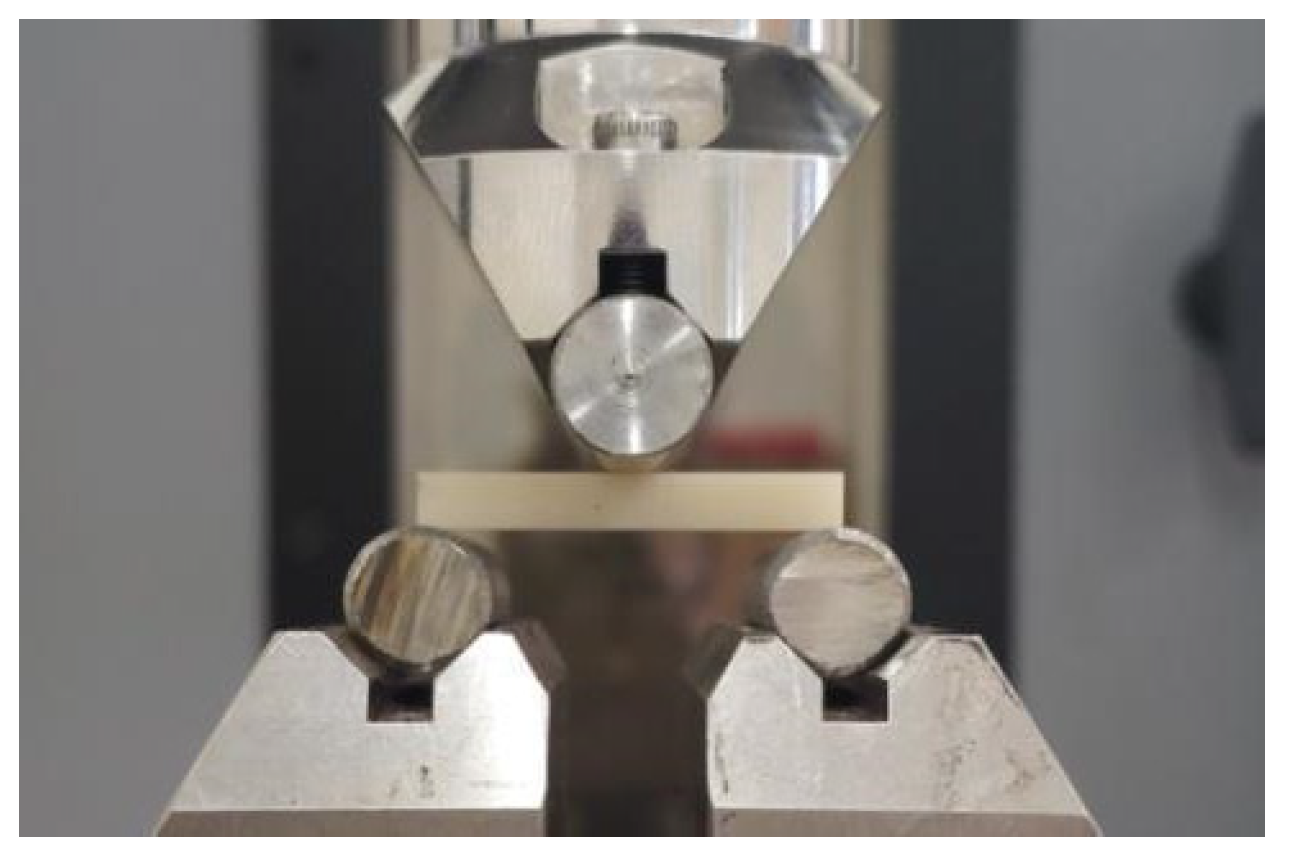
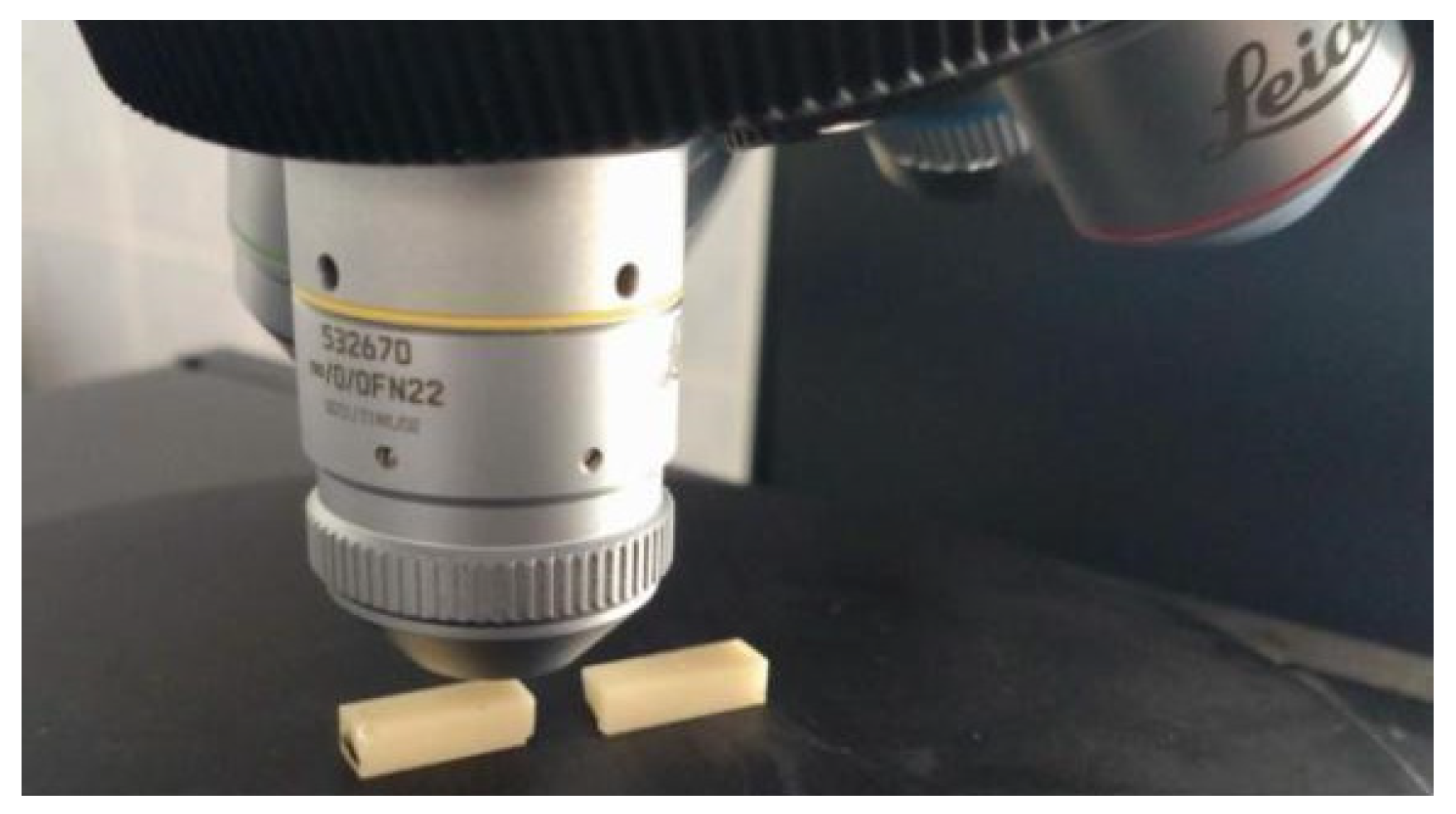
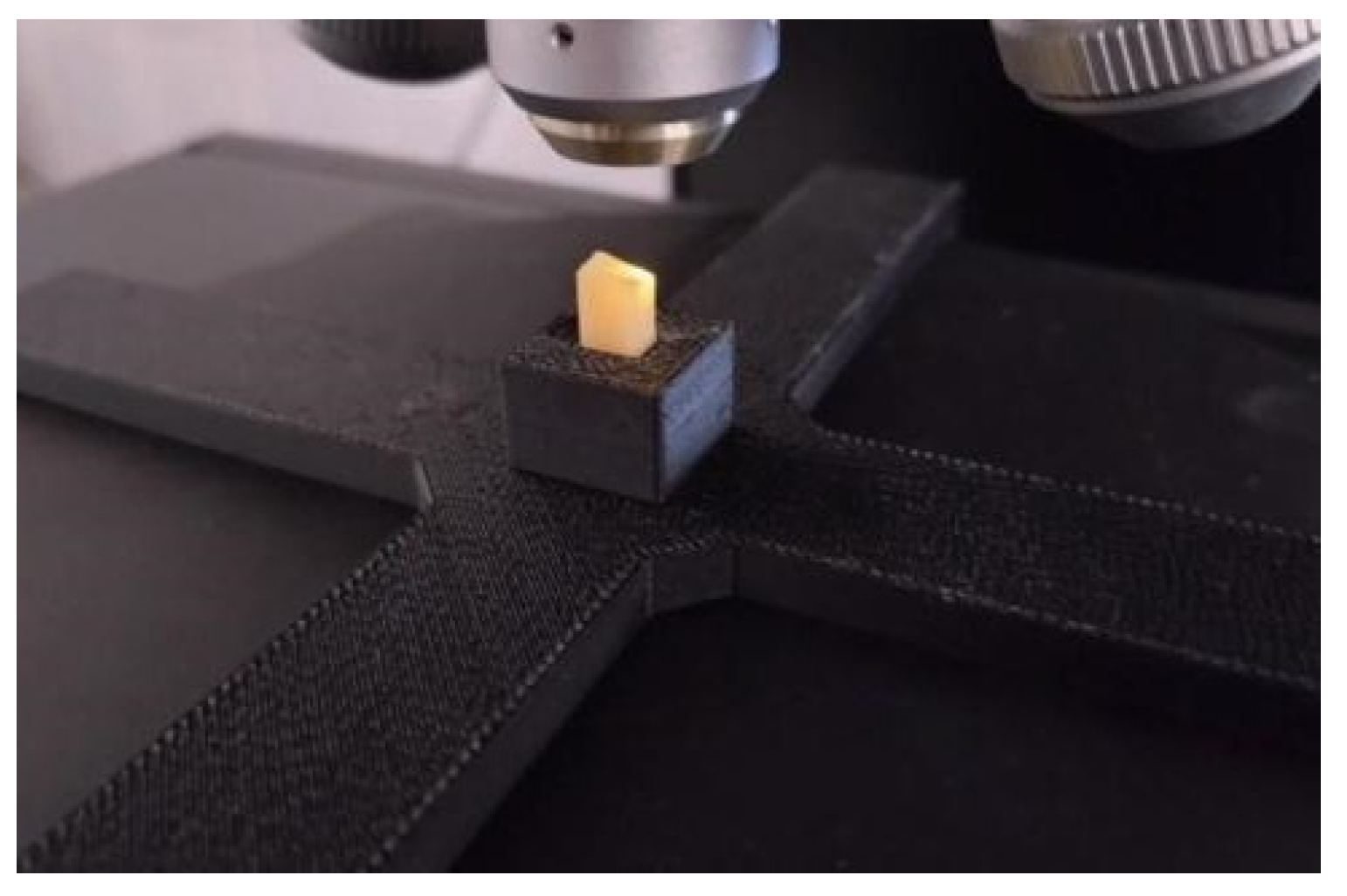
2.1. Assessment of Flexural Strength
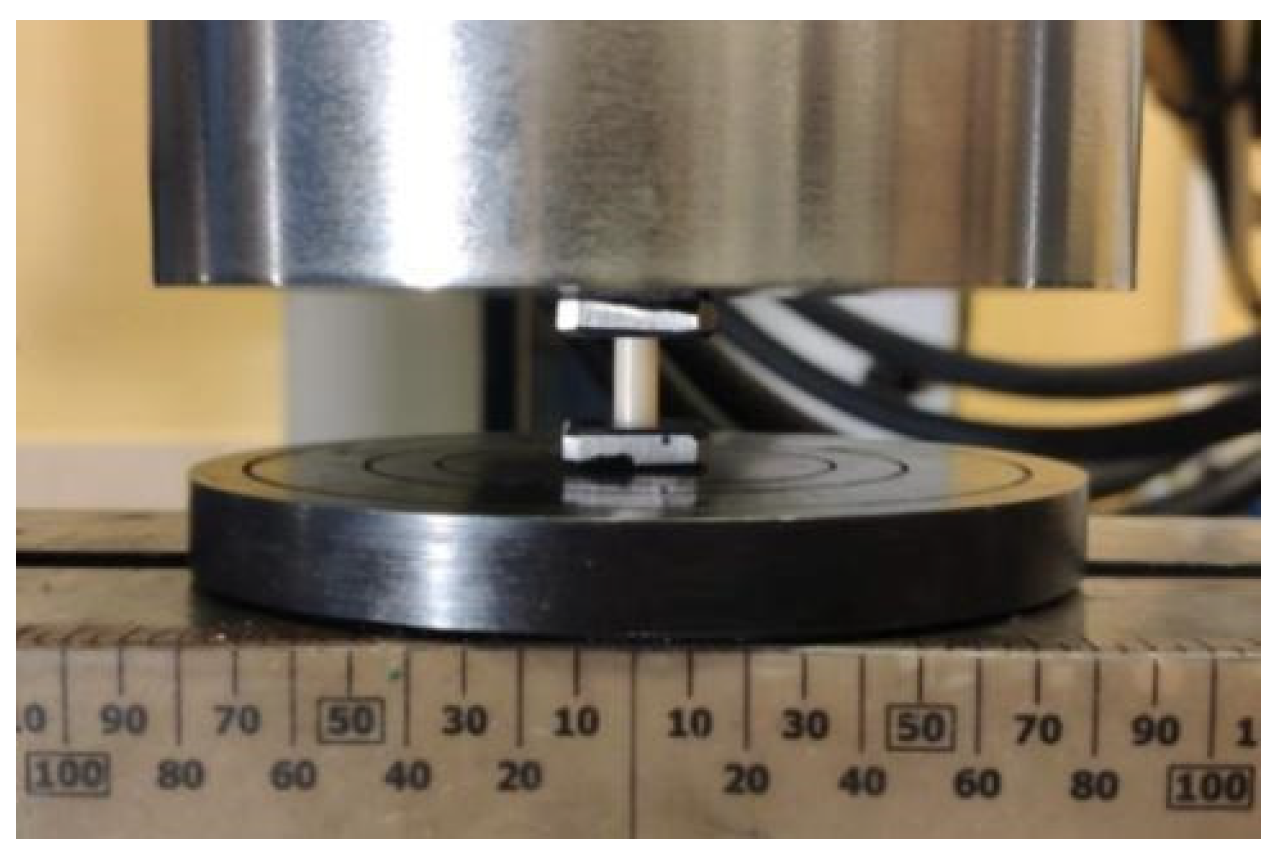
2.2. Assessment of Compressive Strength
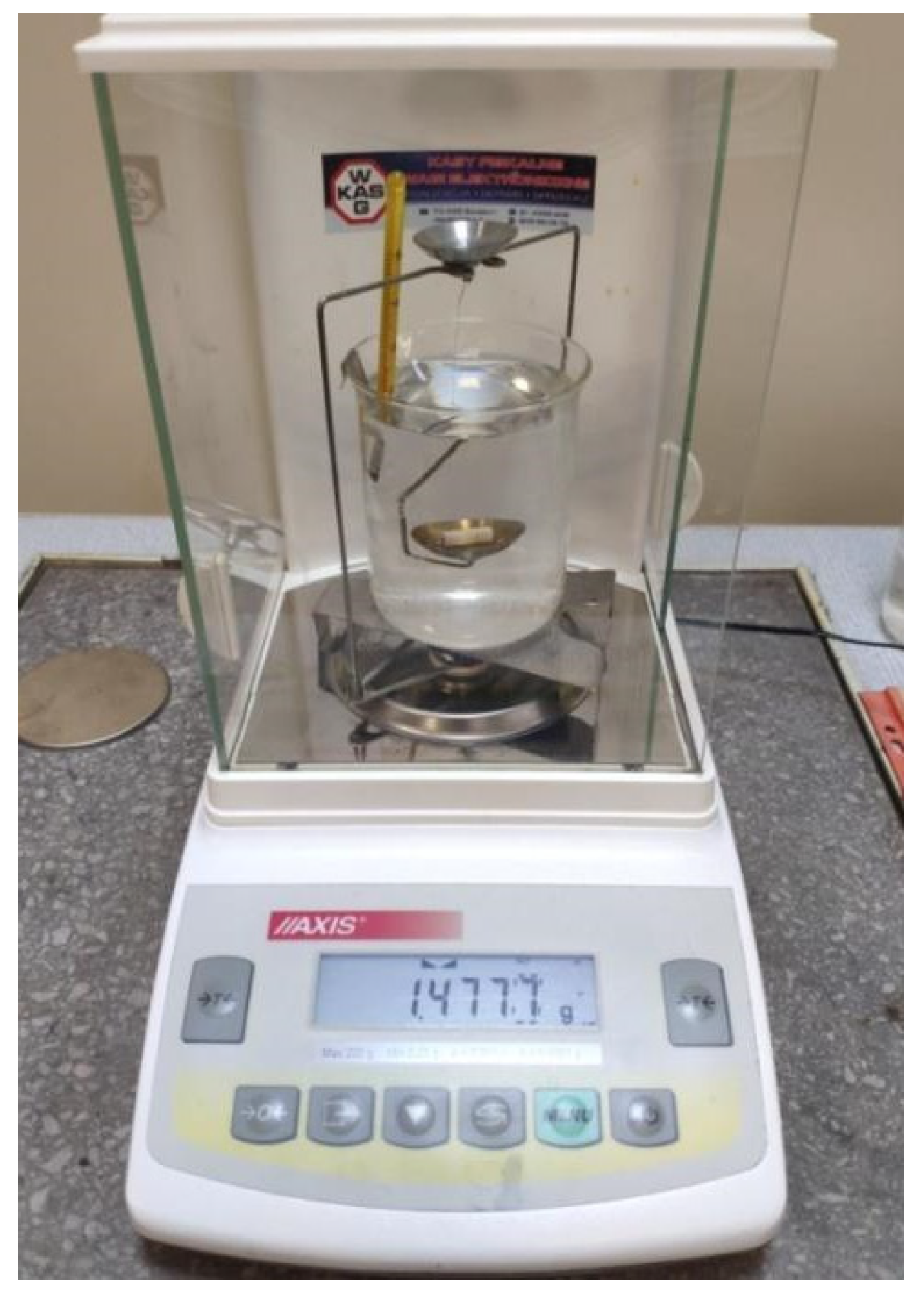
2.3. Density Assessment
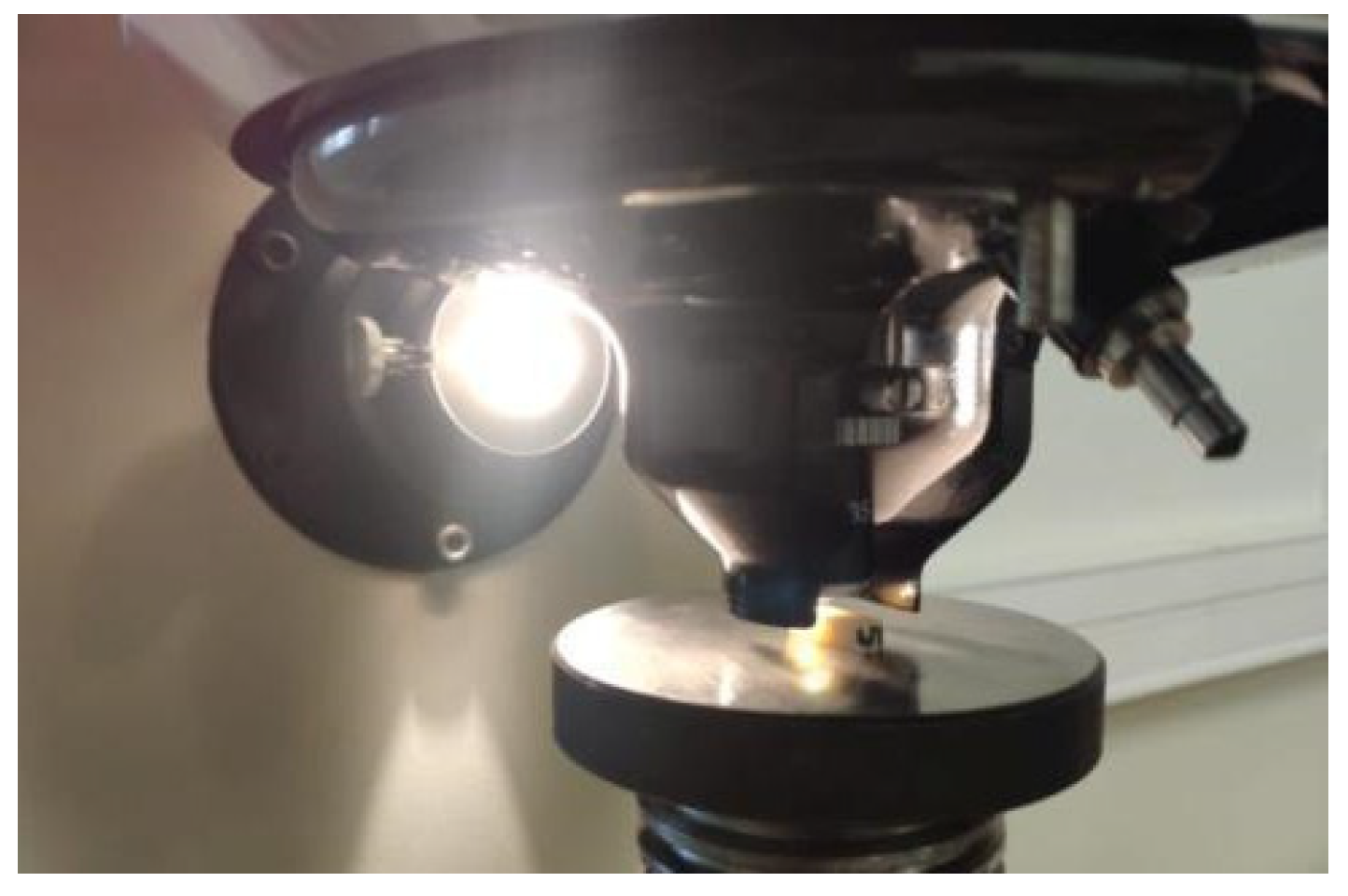
2.4. Hardness Testing
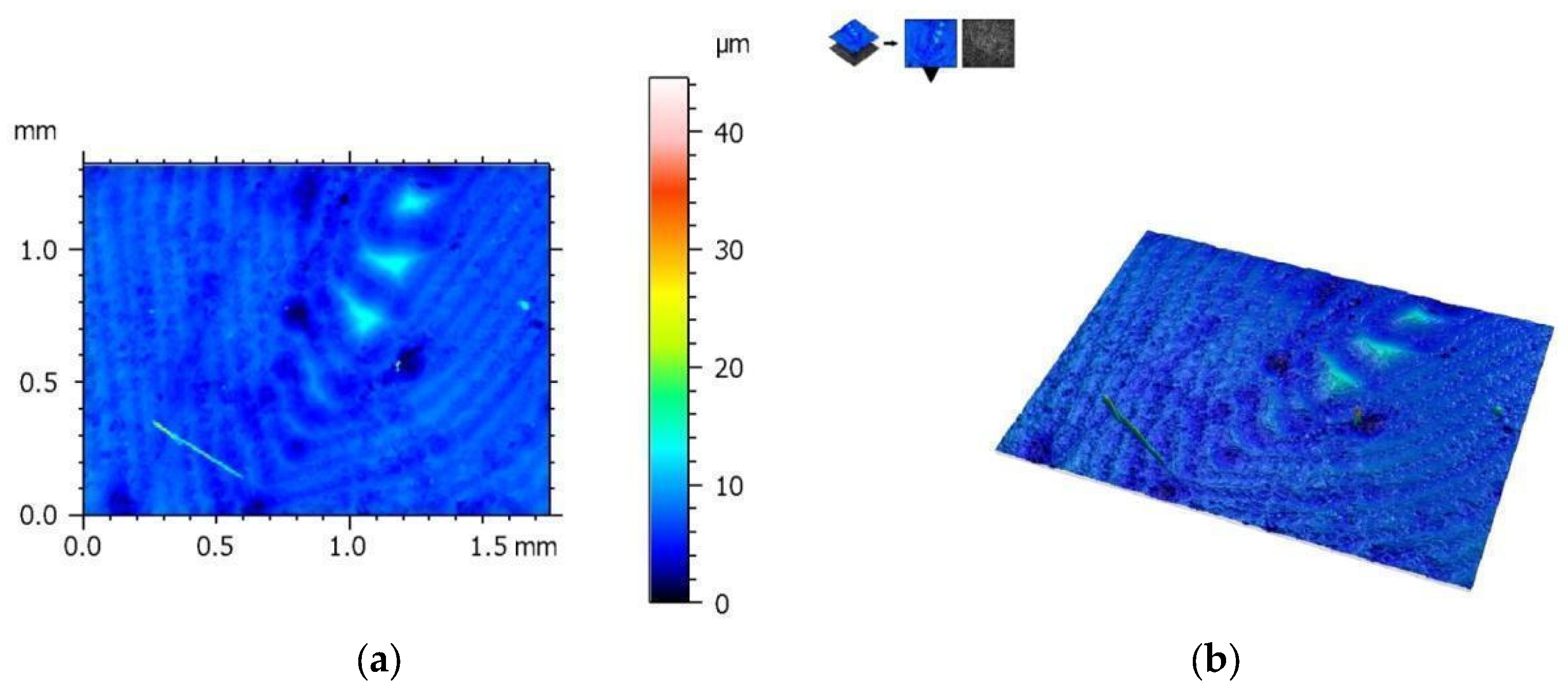
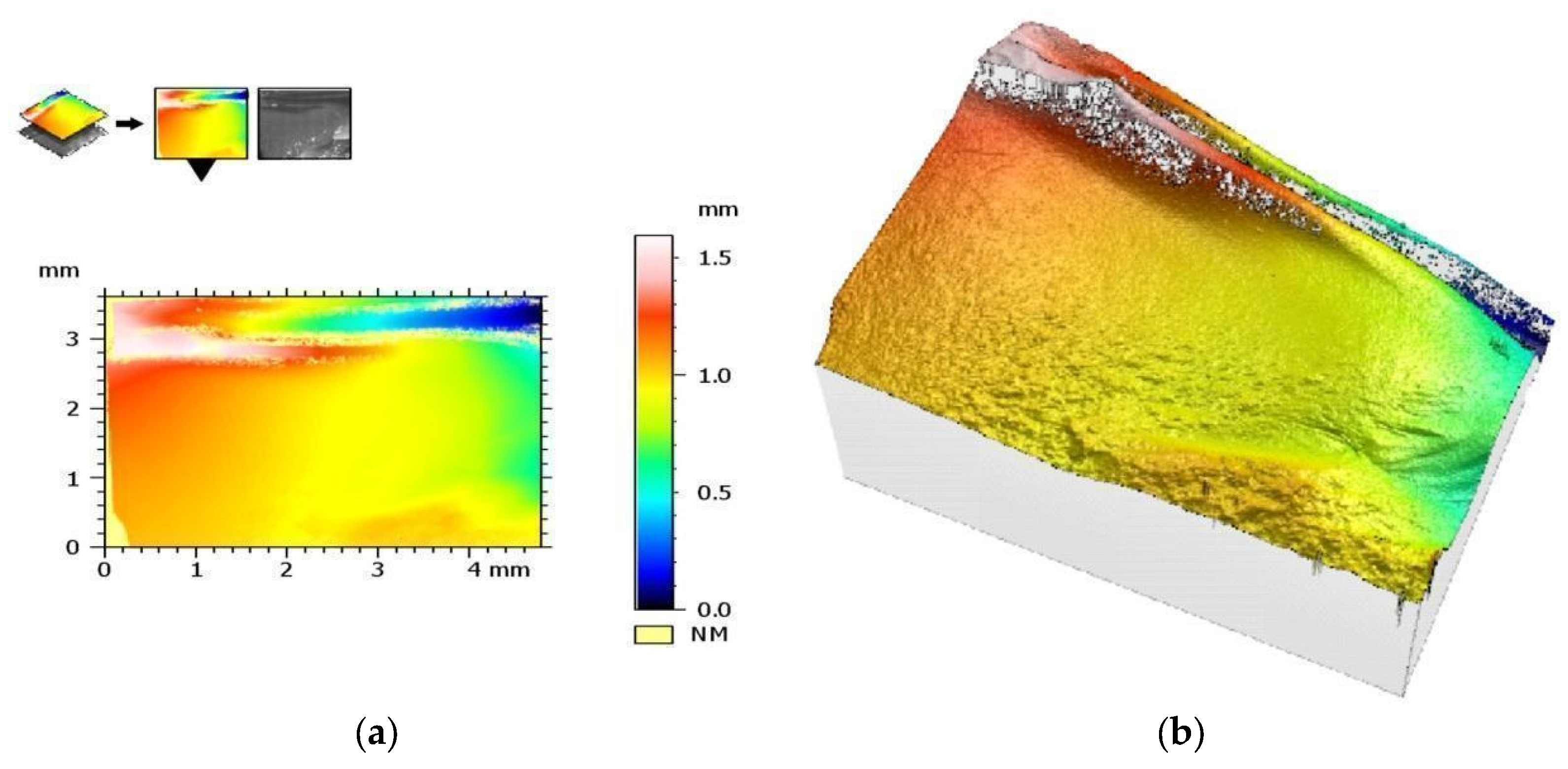
2.5. Analysis of the Geometric Structure of the Surface
2.5.1. Roughness Assessment
2.5.2. Visual Assessment of Crack Propagation
2.6. Statistical Analysis
3. Results
3.1. Assessment of Flexural Strength
3.2. Assessment of Compressive Strength
3.3. Density Assessment
3.4. Hardness Testing
3.5. Analysis of the Geometric Structure of the Surface
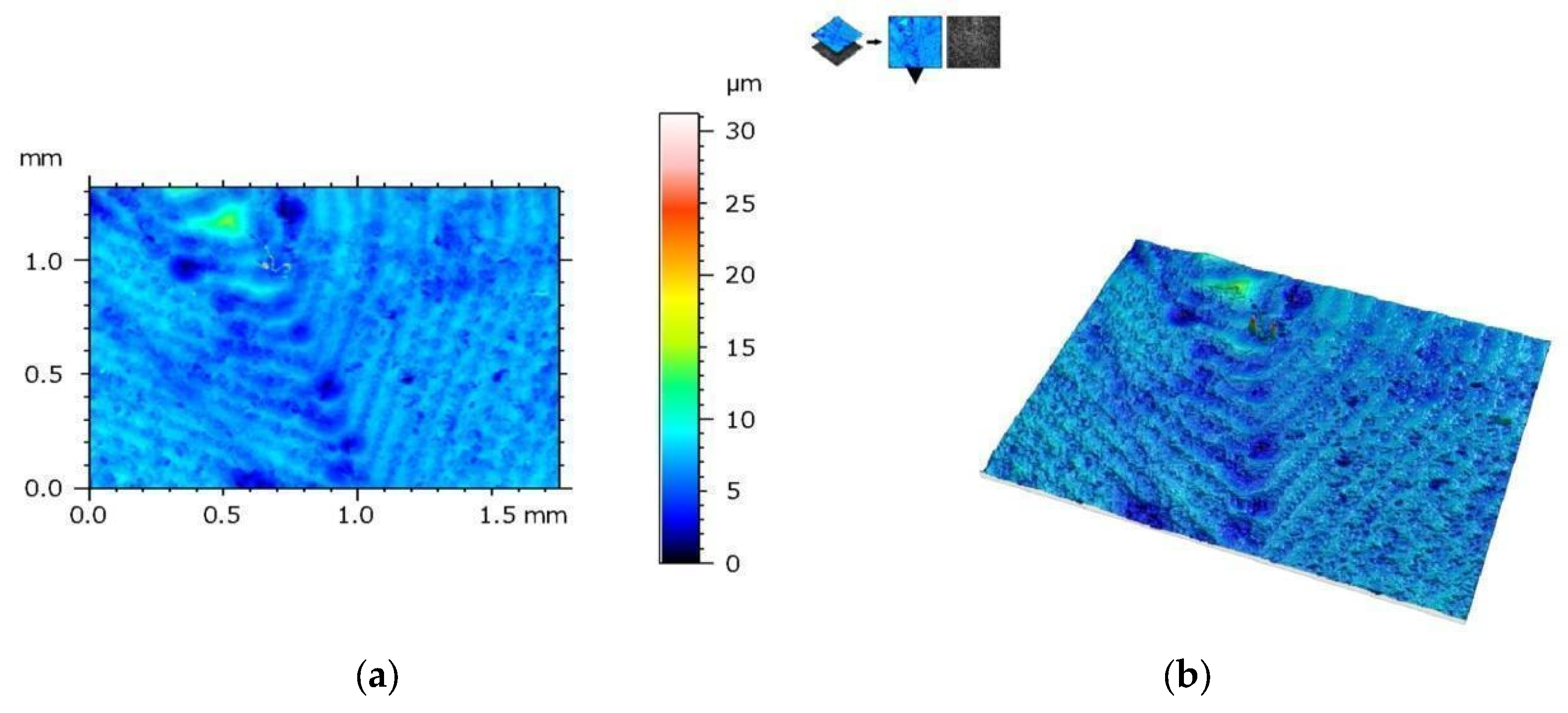
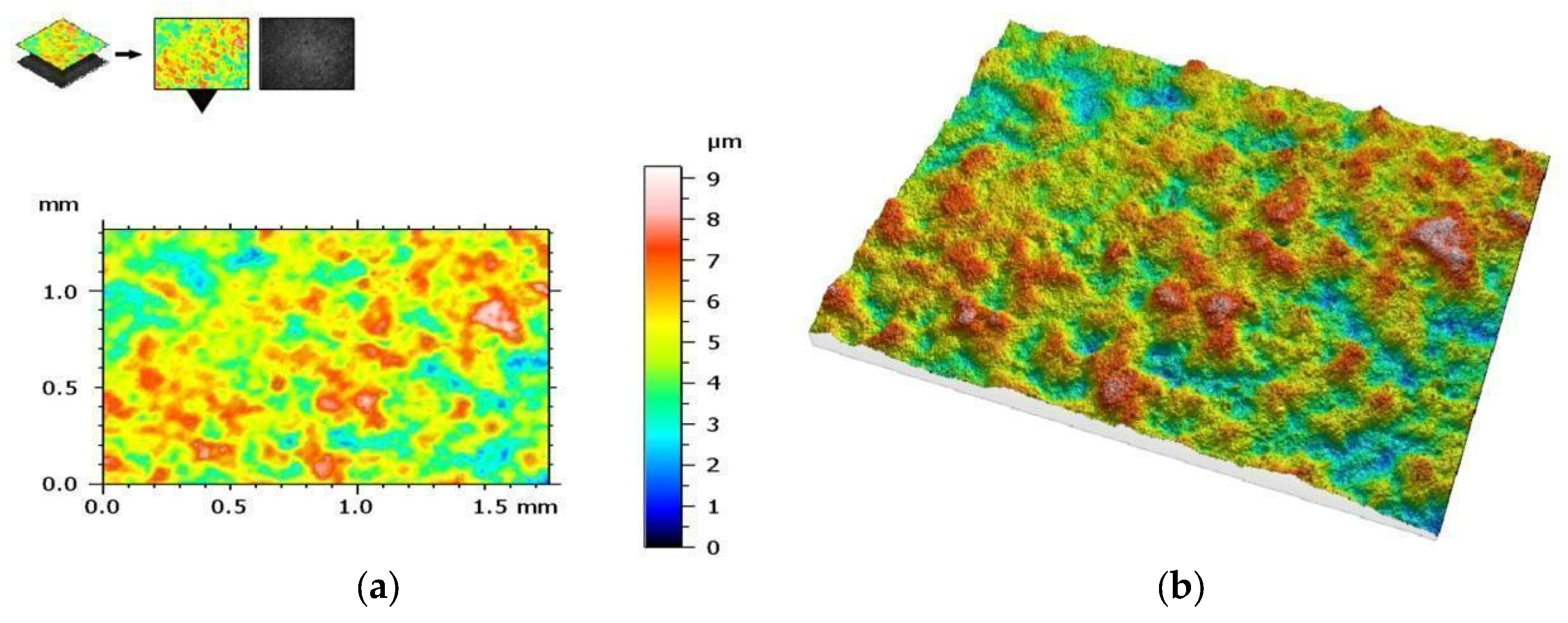
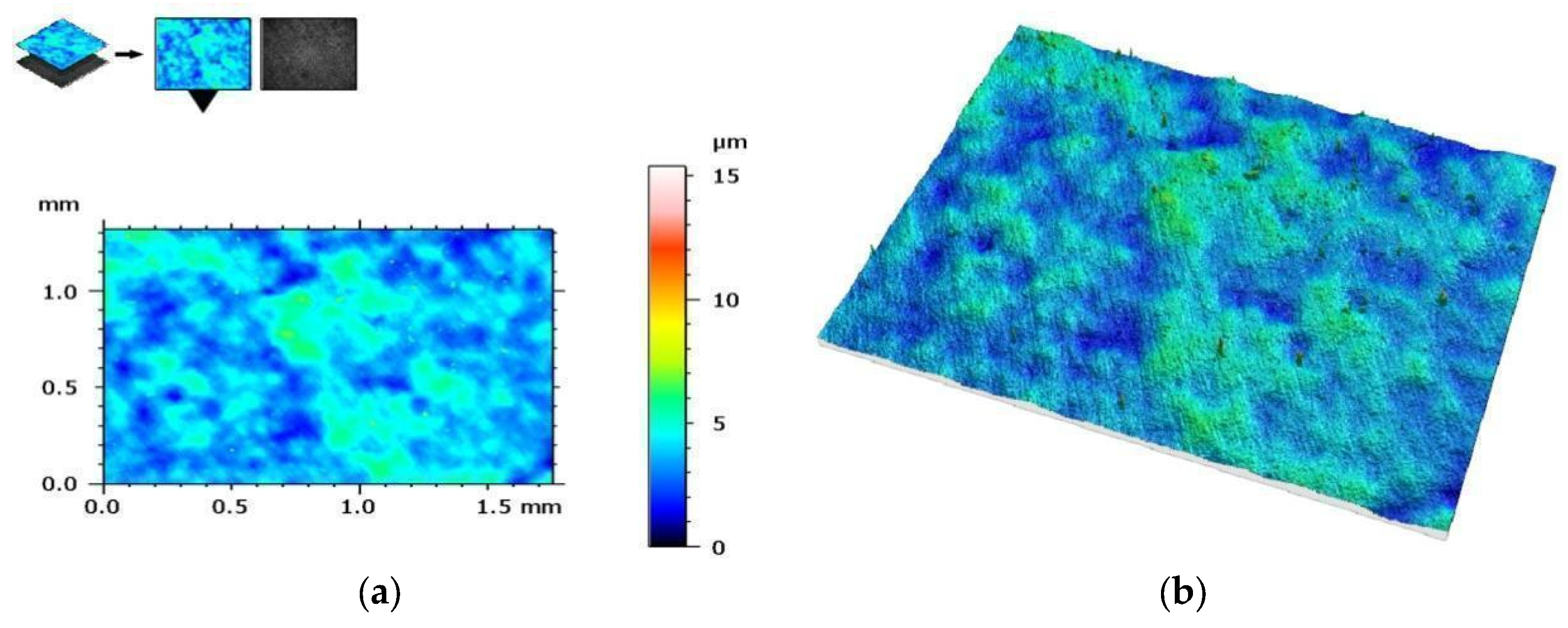
3.5.1. Assessment of the Geometric Structure of Surfaces
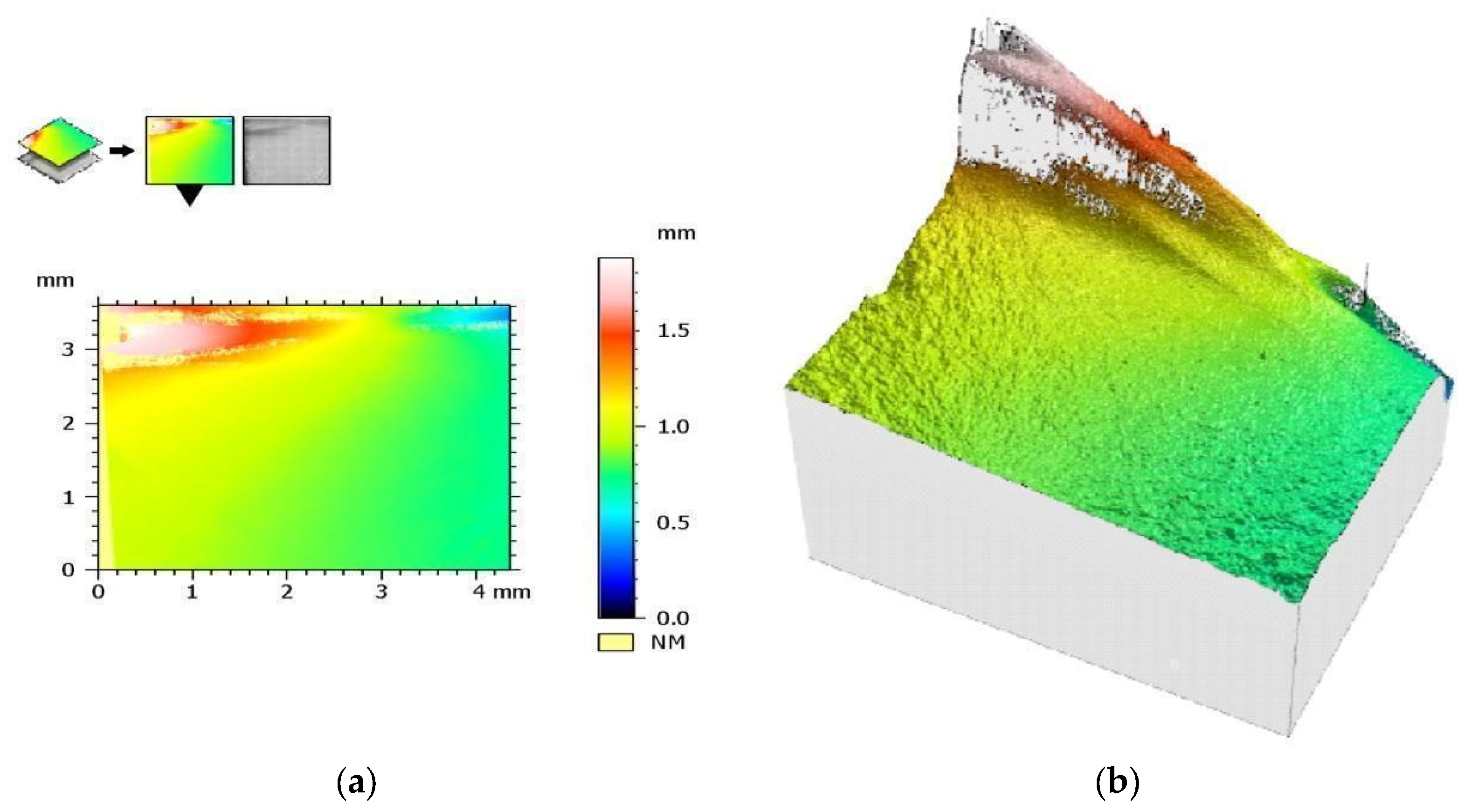
3.5.2. Visual Assessment of Crack Propagation
4. Discussion
The Limitations of This Study
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Macura-Karbownik, A.; Chladek, G.; Żmudzki, J.; Kasperski, J. Chewing efficiency and occlusal forces in PMMA, acetal and polyamide removable partial denture wearers. Acta Bioeng. Biomech. 2016, 18, 137–144. [Google Scholar] [PubMed]
- Wang, B.; Huang, M.; Dang, P.; Xie, J.; Zhang, X.; Yan, X. PEEK in Fixed Dental Prostheses: Application and Adhesion Improvement. Polymers 2022, 14, 2323. [Google Scholar] [CrossRef] [PubMed]
- Donovan, T.E. Factors essential for successful all-ceramic restorations. J. Am. Dent. Assoc. 2008, 139, S14–S18. [Google Scholar] [CrossRef] [PubMed]
- Jacinta, M.; Costa, M.D.; Rubo, J.H.; Pegoraro, L.F.; Santos, G.C., Jr. Current All-Ceramic Systems in Dentistry: A Review. Compend. Contin. Educ. Dent. 2015, 36, 31–38. [Google Scholar]
- Paniz, G.; Kim, Y.; Abualsaud, H.; Hirayama, H. Influence of framework design on the cervical color of metal ceramic crowns. J. Prosthet. Dent. 2011, 106, 310–318. [Google Scholar] [CrossRef] [PubMed]
- Holman, C.D.; Lien, W.; Gallardo, F.F.; Vandewalle, K.S. Assessing Flexural Strength Degradation of New Cubic Containing Zirconia Materials. J. Contemp. Dent. Pract. 2020, 21, 114–118. [Google Scholar] [CrossRef] [PubMed]
- Guess, P.C.; Att, W.; Strub, J.R. Zirconia in fixed implant prosthodontics. Clin. Implant. Dent. Relat. Res. 2010, 14, 633–645. [Google Scholar] [CrossRef] [PubMed]
- Mijiritsky, E.; Elad, A.; Krausz, R.; Ivanova, V.; Zlatev, S. Clinical performance of full-arch implant-supported fixed restorations made of monolithic zirconia luted to a titanium bar: A retrospective study with a mean follow-up of 16 months. J. Dent. 2023, 137, 104675. [Google Scholar] [CrossRef]
- Moreira, A.; Freitas, F.; Marques, D.; Caramês, J. Aesthetic Rehabilitation of a Patient with Bruxism Using Ceramic Veneers and Overlays Combined with Four-Point Monolithic Zirconia Crowns for Occlusal Stabilization: A 4-Year Follow-Up. Case Rep. Dent. 2019, 2019, 1640563. [Google Scholar] [CrossRef]
- Altan, B.; Cınar, S.; Tuncelli, B. Evaluation of shear bond strength of zirconia-based monolithic CAD-CAM materials to resin cement after different surface treatments. Niger. J. Clin. Pract. 2019, 22, 1475–1482. [Google Scholar] [CrossRef]
- Kelly, J.R. Developing meaningful systematic review of CAD/CAM reconstructions and fiber-reinforced composites. Clin. Oral Implant. Res. 2007, 18, 205–217. [Google Scholar] [CrossRef]
- Baba, N.Z.; Goodacre, B.J.; Goodacre, C.J.; Müller, F.; Wagner, S. CAD/CAM Complete Denture Systems and Physical Properties: A Review of the Literature. J. Prosthodont. 2020, 30, 113–124. [Google Scholar] [CrossRef] [PubMed]
- Yeung, M.; Abdulmajeed, A.; Carrico, C.K.; Deeb, G.R.; Bencharit, S. Accuracy and precision of 3D-printed implant surgical guides with different implant systems: An in vitro study. J. Prosthet. Dent. 2019, 123, 821–828. [Google Scholar] [CrossRef] [PubMed]
- Dioguardi, M.; Spirito, F.; Quarta, C.; Sovereto, D.; Basile, E.; Ballini, A.; Caloro, G.A.; Troiano, G.; Muzio, L.L.; Mastrangelo, F. Guided Dental Implant Surgery: Systematic Review. J. Clin. Med. 2023, 12, 1490. [Google Scholar] [CrossRef] [PubMed]
- Haynie, A.S.; English, J.D.; Paravina, R.D.; Moon, A.; Hanigan, J.; Abu Al Tamn, M.A.; Kasper, F.K. Colour stability of 3D-printed resin orthodontic brackets. J. Orthod. 2021, 48, 241–249. [Google Scholar] [CrossRef] [PubMed]
- Tartaglia, G.M.; Mapelli, A.; Maspero, C.; Santaniello, T.; Serafin, M.; Farronato, M.; Caprioglio, A. Direct 3D Printing of Clear Orthodontic Aligners: Current State and Future Possibilities. Materials 2021, 14, 1799. [Google Scholar] [CrossRef] [PubMed]
- Tian, Y.; Chen, C.; Xu, X.; Wang, J.; Hou, X.; Li, K.; Lu, X.; Shi, H.; Lee, E.-S.; Jiang, H.B. A Review of 3D Printing in Dentistry: Technologies, Affecting Factors, and Applications. Scanning 2021, 2021, 9950131. [Google Scholar] [CrossRef] [PubMed]
- Anadioti, E.; Musharbash, L.; Blatz, M.B.; Papavasiliou, G.; Kamposiora, P. 3D printed complete removable dental prostheses: A narrative review. BMC Oral Health 2020, 20, 343. [Google Scholar] [CrossRef] [PubMed]
- Kihara, H.; Sugawara, S.; Yokota, J.; Takafuji, K.; Fukazawa, S.; Tamada, A.; Hatakeyama, W.; Kondo, H. Applications of three-dimensional printers in prosthetic dentistry. J. Oral Sci. 2021, 63, 212–216. [Google Scholar] [CrossRef]
- Mei, Z.; Lu, Y.; Lou, Y.; Yu, P.; Sun, M.; Tan, X.; Zhang, J.; Yue, L.; Yu, H. Determination of Hardness and Fracture Toughness of Y-TZP Manufactured by Digital Light Processing through the Indentation Technique. Biomed. Res. Int. 2021, 2021, 6612840. [Google Scholar]
- Gatto, M.L.; Groppo, R.; Furlani, M.; Giuliani, A.; Mangano, C.; Mangano, F. Lithography-based Ceramic Manufacturing (LCM) versus Milled Zirconia Blocks under uniaxial compressive loading: An in vitro comparative study. J. Dent. 2021, 116, 103886. [Google Scholar] [CrossRef]
- Branco, A.C.; Colaço, R.; Figueiredo-Pina, C.G.; Serro, A.P. Recent Advances on 3D-Printed Zirconia-Based Dental Materials: A Review. Materials 2023, 16, 1860. [Google Scholar] [CrossRef] [PubMed]
- Unkovskiy, A.; Schmidt, F.; Beuer, F.; Li, P.; Spintzyk, S.; Fernandez, P.K. Stereolithography vs. Direct Light Processing for Rapid Manufacturing of Complete Denture Bases: An In Vitro Accuracy Analysis. J. Clin. Med. 2021, 10, 1070. [Google Scholar] [CrossRef] [PubMed]
- Buso, L.; Oliveira-Júnior, O.B.; Hiroshi Fujiy, F.; Leão Lombardo, G.H.; Ramalho Sarmento, H.; Campos, F.; Assunção Souza, R.O. Biaxial flexural strength of CAD/CAM ceramics. Minerva Stomatol. 2011, 60, 311–319. [Google Scholar] [PubMed]
- Zahran, M.; El-Mowafy, O.; Tam, L.; Watson, P.A.; Finer, Y. Fracture strength and fatigue resistance of all-ceramic molar crowns manufactured with CADCAM technology. J. Prosthodont. 2008, 17, 370–377. [Google Scholar] [CrossRef] [PubMed]
- Limpuangthip, N.; Poosanthanasarn, E.; Salimee, P. Surface Roughness and Hardness of CAD/CAM Ceramic Materials after Polishing with a Multipurpose Polishing Kit: An In Vitro Study. Eur. J. Dent. 2022. [Google Scholar] [CrossRef]
- Liebermann, A.; Schultheis, A.; Faber, F.; Rammelsberg, P.; Rues, S.; Schwindling, F. Impact of post printing cleaning methods on geometry, transmission, roughness parameters, and flexural strength of 3D-printed zirconia. Dent. Mater. 2023, 39, 625–633. [Google Scholar] [CrossRef]
- Buj-Corral, I.; Vidal, D.; Tejo-Otero, A.; Padilla, J.A.; Xuriguera, E.; Fenollosa-Artés, F. Characterization of 3D Printed Yttria-Stabilized Zirconia Parts for Use in Prostheses. Nanomaterials 2021, 11, 2942. [Google Scholar] [CrossRef]
- Revilla-León, M.; Husain, N.A.-H.; Ceballos, L.; Özcan, M. Flexural strength and Weibull characteristics of stereolithography additive manufactured versus milled zirconia. J. Prosthet. Dent. 2020, 125, 685–690. [Google Scholar] [CrossRef]
- Machry, R.V.; Dapieve, K.S.; Cadore-Rodrigues, A.C.; Werner, A.; de Jager, N.; Pereira, G.K.R.; Valandro, L.F.; Kleverlaan, C.J. Mechanical characterization of a multi-layered zirconia: Flexural strength, hardness, and fracture toughness of the different layers. J. Mech. Behav. Biomed. Mater. 2022, 135, 105455. [Google Scholar] [CrossRef]
- Vardhaman, S.; Borba, M.R.; Kaizer, M.; Kim, D.; Zhang, Y. Wear behavior and microstructural characterization of translucent multilayer zirconia. Dent. Mater. Off. Publ. Acad. Dent. Mater. 2020, 36, 1407–1417. [Google Scholar] [CrossRef]
- Miura, S.; Shinya, A.; Ishida, Y.; Fujisawa, M. Mechanical and surface properties of additive manufactured zirconia under the different building directions. J. Prosthodont. Res. 2022, 67, 410–417. [Google Scholar] [CrossRef] [PubMed]
- ISO 1183-1; Plastics—Methods for Determining the Density of Non-Porous Plastics—Part 1: Immersion Method, Liquid Pycnometer Method and Titration Method. ISO: Geneva, Switzerland, 2019.
- ISO 25178; Geometrical Product Specifications (GPS). Surface Texture: Areal—Part 2: Terms, Definitions and Surface Texture Parameters. ISO: Geneva, Switzerland, 2021.
- ISO 2854; Statistical Interpretation of Data. Techniques of Estimation and Tests Relating to Means and Variances. ISO: Geneva, Switzerland, 1976.
- Baysal, N.; Tuğba Kalyoncuoğlu, Ü.; Ayyıldız, S. Mechanical Properties and Bond Strength of Additively Manufactured and Milled Dental Zirconia: A Pilot Study. J. Prosthodont. 2022, 31, 629–634. [Google Scholar] [CrossRef] [PubMed]
- Zandinejad, A.; Das, O.; Barmak, A.B.; Kuttolamadom, M.; Revilla-León, M. The Flexural Strength and Flexural Modulus of Stereolithography Additively Manufactured Zirconia with Different Porosities. J. Prosthodont. 2021, 31, 434–440. [Google Scholar] [CrossRef] [PubMed]
- Revilla-León, M.; Husain, N.A.; Barmak, A.B.; Pérez-López, J.; Raigrodski, A.J.; Özcan, M. Chemical Composition and Flexural Strength Discrepancies Between Milled and Lithography-Based Additively Manufactured Zirconia. J. Prosthodont. 2022, 31, 778–783. [Google Scholar] [CrossRef] [PubMed]
- Lu, Y.; Wang, L.; Piva, A.D.; Tribst, J.; Nedeljkovic, I.; Kleverlaan, C.; Feilzer, A. Influence of surface finishing and printing layer orientation on surface roughness and flexural strength of stereolithography-manufactured dental zirconia. J. Mech. Behav. Biomed. Mater. 2023, 143, 105944. [Google Scholar] [CrossRef] [PubMed]
- Opalińska, A.; Malka, I.; Dzwolak, W.; Chudoba, T.; Presz, A.; Lojkowski, W. Size-dependent density of zirconia nanoparticles. Beilstein J. Nanotechnol. 2015, 6, 27–35. [Google Scholar] [CrossRef] [PubMed]
- Li, R.; Wang, Y.; Hu, M.; Wang, Y.; Xv, Y.; Liu, Y.; Sun, Y. Strength and Adaptation of Stereolithography-Fabricated Zirconia Dental Crowns: An In Vitro Study. Int. J. Prosthodont. 2019, 32, 439–443. [Google Scholar] [CrossRef] [PubMed]
- Patil, A.; Bomze, D.; Gopal, V. Wear behaviour of lithography ceramic manufactured dental zirconia. BMC Oral Health 2023, 23, 276. [Google Scholar] [CrossRef]
- ISO 13485; Medical Devices. Quality Management Systems. Requirements for Regulatory Purposes. ISO: Geneva, Switzerland, 2016.
- Colombo, M.; Gallo, S.; Poggio, C.; Ricaldone, V.; Arciola, C.R.; Scribante, A. New Resin-Based Bulk-Fill Composites: In Vitro Evaluation of Micro-Hardness and Depth of Cure as Infection Risk Indexes. Materials 2020, 13, 1308. [Google Scholar] [CrossRef]
- Kamatchi, M.; Ajay, R.; Gawthaman, M.; Maheshmathian, V.; Preethi, K.; Gayatrikumary, T. Tensile Bond Strength and Marginal Integrity of a Self-adhering and a Self-etch Adhesive Flowable Composite after Artificial Thermomechanical Aging. Int. J. Clin. Pediatr. Dent. 2022, 15, 204–209. [Google Scholar] [CrossRef]
| Sq | Root-mean-square height | |
| Ssk | Skewness | Skewness of the height distribution. |
| Sku | Kurtosis | Kurtosis of the height distribution. |
| Sp | Maximum peak height | Height between the highest peak and the mean plane. |
| Sv | Maximum pit depth | Depth between the mean plane and the deepest valley. |
| Sz | Maximum height | Height between the highest peak and the deepest valley. |
| Sa | Arithmetic mean height | Mean surface roughness. |
| Characteristic | SM Group | AM Group | ||
|---|---|---|---|---|
| Mean Value | Confidence Interval 99% | Mean Value | Confidence Interval 99% | |
| Flexural strength (MPa) | 688 | 100 | 813 | 265 |
| Young modulus—for flexural strength (GPa) | 203 | 11 | 206 | 11 |
| Compressive strength (GPa) | 3.99 | 0.65 | 4.16 | 0.53 |
| Young modulus—for compressive strength (GPa) | 230 | 31 | 231 | 37 |
| Density (g/cm3) | 6.056 | 0.031 | 6.003 | 0.035 |
| Hardness (HV) | 1285 | 30 | 1319 | 23 |
| Summary of the Geometric Structure of the Surface Parameters for Samples from the SM Group before Cracking | |||||
| Parameter | Unit | Mean Value | Standard Deviation | Minimum | Maximum |
| Sq | µm | 1.19 | 0.29 | 0.89 | 1.69 |
| Ssk | 2.5 | 3.6 | −1.2 | 8.1 | |
| Sku | 78 | 88 | 6 | 235 | |
| Sp | µm | 26 | 16 | 6 | 44 |
| Sv | µm | 9.7 | 2.5 | 6.7 | 13.1 |
| Sz | µm | 35 | 17 | 14 | 56 |
| Sa | µm | 0.74 | 0.10 | 0.62 | 0.92 |
| Summary of the Geometric Structure of the Surface Parameters for Samples from the SM Group after Cracking | |||||
| Parameter | Unit | Mean Value | Standard Deviation | Minimum | Maximum |
| Sq | µm | 1.17 | 0.29 | 0.83 | 1.52 |
| Ssk | 2.1 | 4.5 | −1.0 | 10.9 | |
| Sku | 89 | 102 | 10 | 288 | |
| Sp | µm | 32 | 14 | 13 | 48 |
| Sv | µm | 9.6 | 2.9 | 6.4 | 14.5 |
| Sz | µm | 42 | 16 | 22 | 63 |
| Sa | µm | 0.76 | 0.13 | 0.59 | 0.92 |
| Summary of the Geometric Structure of the Surface Parameters for Samples from the AM Group before Cracking | |||||
| Parameter | Unit | Mean Value | Standard Deviation | Minimum | Maximum |
| Sq | µm | 0.99 | 0.36 | 0.34 | 1.39 |
| Ssk | −0.08 | 0.16 | −0.36 | 0.10 | |
| Sku | 4.1 | 2.7 | 2.6 | 9.5 | |
| Sp | µm | 5.04 | 0.91 | 3.92 | 6.48 |
| Sv | µm | 4.17 | 0.68 | 3.30 | 5.06 |
| Sz | µm | 9.2 | 1.1 | 7.2 | 10.3 |
| Sa | µm | 0.79 | 0.30 | 0.26 | 1.12 |
| Summary of the Geometric Structure of the Surface Parameters for Samples from the AM Group after Cracking | |||||
| Parameter | Unit | Mean Value | Standard Deviation | Minimum | Maximum |
| Sq | µm | 1.08 | 0.30 | 0.63 | 1.42 |
| Ssk | 1.9 | 2.4 | 0.0 | 5.8 | |
| Sku | 39 | 52 | 3 | 138 | |
| Sp | µm | 19 | 11 | 11 | 40 |
| Sv | µm | 6.0 | 2.4 | 3.5 | 10.6 |
| Sz | µm | 25 | 11 | 15 | 45 |
| Sa | µm | 0.82 | 0.25 | 0.42 | 1.07 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Frąckiewicz, W.; Królikowski, M.; Kwiatkowski, K.; Sobolewska, E.; Szymlet, P.; Tomasik, M. Comparison of Dental Zirconium Oxide Ceramics Produced Using Additive and Removal Technology for Prosthodontics and Restorative Dentistry—Strength and Surface Tests: An In Vitro Study. Materials 2024, 17, 168. https://doi.org/10.3390/ma17010168
Frąckiewicz W, Królikowski M, Kwiatkowski K, Sobolewska E, Szymlet P, Tomasik M. Comparison of Dental Zirconium Oxide Ceramics Produced Using Additive and Removal Technology for Prosthodontics and Restorative Dentistry—Strength and Surface Tests: An In Vitro Study. Materials. 2024; 17(1):168. https://doi.org/10.3390/ma17010168
Chicago/Turabian StyleFrąckiewicz, Wojciech, Marcin Królikowski, Konrad Kwiatkowski, Ewa Sobolewska, Paweł Szymlet, and Małgorzata Tomasik. 2024. "Comparison of Dental Zirconium Oxide Ceramics Produced Using Additive and Removal Technology for Prosthodontics and Restorative Dentistry—Strength and Surface Tests: An In Vitro Study" Materials 17, no. 1: 168. https://doi.org/10.3390/ma17010168
APA StyleFrąckiewicz, W., Królikowski, M., Kwiatkowski, K., Sobolewska, E., Szymlet, P., & Tomasik, M. (2024). Comparison of Dental Zirconium Oxide Ceramics Produced Using Additive and Removal Technology for Prosthodontics and Restorative Dentistry—Strength and Surface Tests: An In Vitro Study. Materials, 17(1), 168. https://doi.org/10.3390/ma17010168






