The Toothbrushing Effects on Surface Properties and Color Stability of CAD/CAM and Pressable Ceramic Fixed Restorations—An In Vitro Study
Abstract
1. Introduction
2. Materials and Methods
2.1. Specimens’ Finishing and Polishing
2.2. Toothbrushing Protocol
2.3. Surface Roughness Test (Ra)
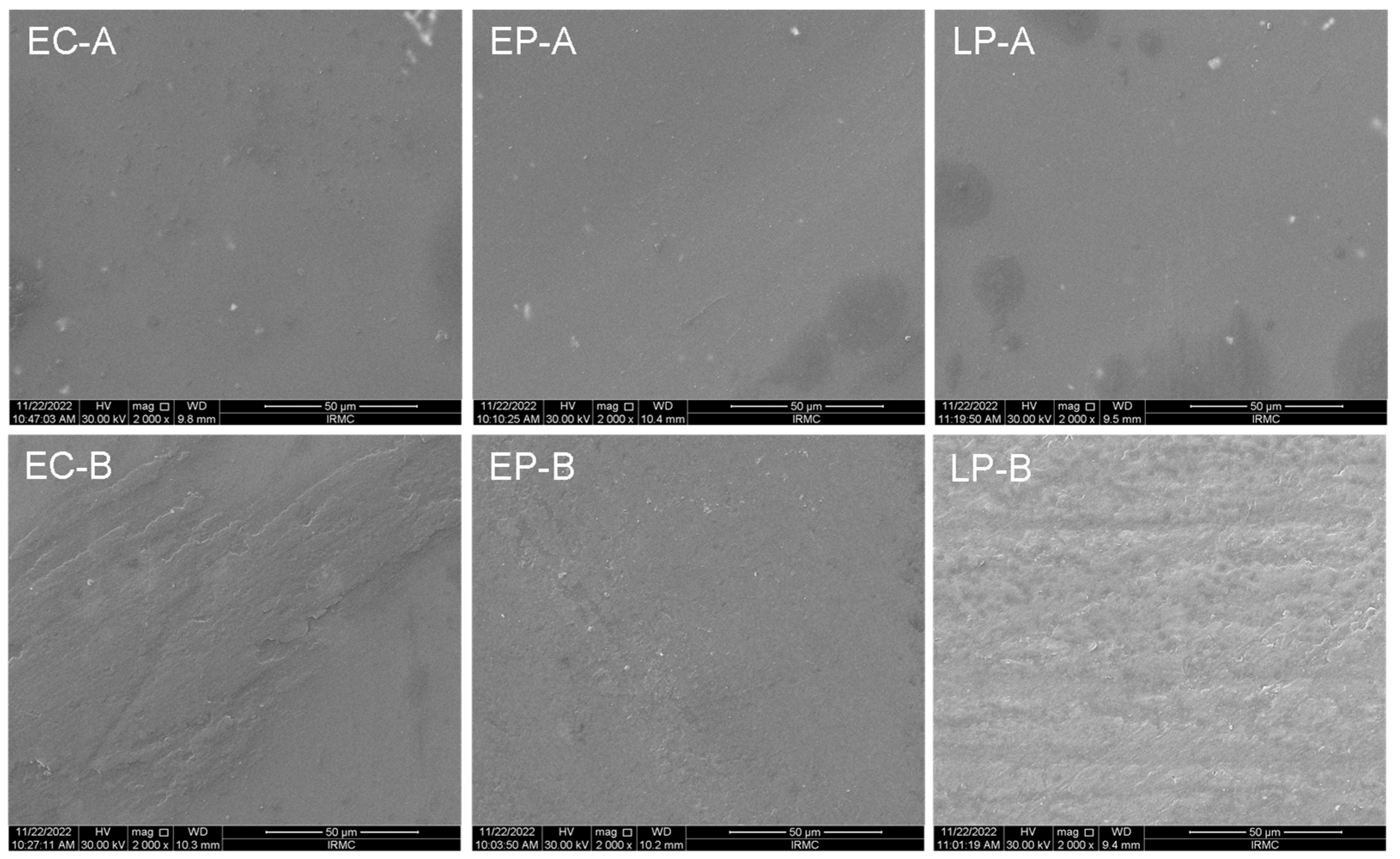
2.4. Scanning Electron Microscopy (SEM) Analysis
2.5. Microhardness Test
2.6. Color Stability (ΔE)
2.7. Statistical Analysis
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Coffman, C.; Visser, C.; Soukup, J.; Peak, M. Crowns and prosthodontics. Wiggs’s Vet. Dent. Princ. Pract. 2019, 2019, 387–410. [Google Scholar]
- McLaren, E.; Giordano, R. Ceramics overview: Classification by microstructure and processing methods. Compend. Contin. Educ. Dent. 2010, 31, 682–684. [Google Scholar]
- Giordano, R. Materials for chairside CAD/CAM–produced restorations. J. Am. Dent. Assoc. 2006, 137, 14S–21S. [Google Scholar] [CrossRef] [PubMed]
- Pituru, S.M.; Greabu, M.; Totan, A.; Imre, M.; Pantea, M.; Spinu, T.; Tancu, A.M.C.; Popoviciu, N.O.; Stanescu, I.-I.; Ionescu, E. A Review on the Biocompatibility of PMMA-Based Dental Materials for Interim Prosthetic Restorations with a Glimpse into Their Modern Manufacturing Techniques. Materials 2020, 13, 2894. [Google Scholar] [CrossRef]
- Joda, T.; Zitzmann, N.U. Personalized workflows in reconstructive dentistry—Current possibilities and future opportunities. Clin. Oral. Investig. 2022, 26, 4283–4290. [Google Scholar] [CrossRef] [PubMed]
- Santos, M.J.M.C.; Costa, M.D.; Rubo, J.H.; Pegoraro, L.F.; Santos, G.C. Current all-ceramic systems in dentistry: A review. Compend. Contin. Educ. Dent. 2015, 36, 31–37. [Google Scholar]
- Shamseddine, L.; Mortada, R.; Rifai, K.; Chidiac, J.J. Marginal and internal fit of pressed ceramic crowns made from conventional and computer-aided design and computer-aided manufacturing wax patterns: An in vitro comparison. J. Prosthet. Dent. 2016, 116, 242–248. [Google Scholar] [CrossRef] [PubMed]
- Dikicier, S.; Ayyildiz, S.; Ozen, J.; Sipahi, C. Influence of core thickness and artificial aging on the biaxial flexural strength of different all-ceramic materials: An in-vitro study. Dent. Mater. J. 2017, 36, 296–302. [Google Scholar] [CrossRef] [PubMed]
- Yılmaz, C.; Korkmaz, T.; Demirköprülü, H.; Ergün, G.; Özkan, Y. Color Stability of Glazed and Polished Dental Porcelains. J. Prosthodont. 2008, 17, 20–24. [Google Scholar] [CrossRef]
- Manjuran, N.G.; Sreelal, T. An In Vitro Study to Identify a Ceramic Polishing Protocol Effecting Smoothness Superior to Glazed Surface. J. Indian Prosthodont. Soc. 2014, 14, 219–227. [Google Scholar] [CrossRef] [PubMed]
- Şen, N.; Tuncelli, B.; Göller, G. Surface deterioration of monolithic CAD/CAM restorative materials after artificial abrasive toothbrushing. J. Adv. Prosthodont. 2018, 10, 271. [Google Scholar] [CrossRef] [PubMed]
- Kotsanos, N.; Sulyanto, R.; Ng, M.W. Dental Caries Prevention in Children and Adolescents. In Pediatric Dentistry; Springer: Berlin/Heidelberg, Germany, 2022; pp. 247–280. [Google Scholar]
- Sehovic, E.; Ioannidis, A.; Hämmerle, C.H.; Özcan, M.; Mühlemann, S. Effect of tooth brush abrasion on the color, gloss and surface roughness of internally and externally stained monolithic ceramic materials. J. Prosthodont. Res. 2022, 66, 303–311. [Google Scholar] [CrossRef] [PubMed]
- Dal Piva, A.M.d.O.; Bottino, M.A.; Anami, L.C.; Werner, A.; Kleverlaan, C.J.; Lo Giudice, R.; Famà, F.; Silva-Concilio, L.R.d.; Tribst, J.P.M. Toothbrushing Wear Resistance of Stained CAD/CAM Ceramics. Coatings 2021, 11, 224. [Google Scholar] [CrossRef]
- Alencar-Silva, F.J.; Barreto, J.O.; Negreiros, W.A.; Silva, P.G.B.; Pinto-Fiamengui, L.M.S.; Regis, R.R. Effect of beverage solutions and toothbrushing on the surface roughness, microhardness, and color stainability of a vitreous CAD-CAM lithium disilicate ceramic. J. Prosthet. Dent. 2019, 121, 711.e711–711.e716. [Google Scholar] [CrossRef]
- Majumder, A.; Giri, T.; Mukherjee, S. An in vitrostudy to compare the influence of different all-ceramic systems on the polymerization of dual-cure resin cement. J. Indian Prosthodont. Soc. 2019, 19, 58–65. [Google Scholar] [CrossRef]
- Taymour, N.; Fahmy, A.E.; Gepreel, M.A.H.; Kandil, S.; El-Fattah, A.A. Improved Mechanical Properties and Bioactivity of Silicate Based Bioceramics Reinforced Poly(ether-ether-ketone) Nanocomposites for Prosthetic Dental Implantology. Polymers 2022, 14, 1632. [Google Scholar] [CrossRef] [PubMed]
- Vichi, A.; Sedda, M.; Fabian Fonzar, R.; Carrabba, M.; Ferrari, M. Comparison of Contrast Ratio, Translucency Parameter, and Flexural Strength of Traditional and “Augmented Translucency” Zirconia for CEREC CAD/CAM System. J. Esthet. Restor. Dent. 2016, 28 (Suppl. 1), S32–S39. [Google Scholar] [CrossRef] [PubMed]
- Dimitrova, M.; Corsalini, M.; Kazakova, R.; Vlahova, A.; Barile, G.; Dell’Olio, F.; Tomova, Z.; Kazakov, S.; Capodiferro, S. Color Stability Determination of CAD/CAM Milled and 3D Printed Acrylic Resins for Denture Bases: A Narrative Review. J. Compos. Sci. 2022, 6, 201. [Google Scholar] [CrossRef]
- Lee, Y.-K. Comparison of CIELAB ΔE* and CIEDE2000 color-differences after polymerization and thermocycling of resin composites. Dent. Mater. 2005, 21, 678–682. [Google Scholar] [CrossRef] [PubMed]
- Tieh, M.T.; Waddell, J.N.; Choi, J.J.E. Optical Properties and Color Stability of Denture Teeth—A Systematic Review. J. Prosthodont. 2022, 31, 385–398. [Google Scholar] [CrossRef]
- de Matos, J.D.M.; Lopes, G.R.S.; Queiroz, D.A.; Nakano, L.J.N.; Ribeiro, N.C.R.; Barbosa, A.B.; Anami, L.C.; Bottino, M.A. Dental Ceramics: Fabrication Methods and Aesthetic Characterization. Coatings 2022, 12, 1228. [Google Scholar] [CrossRef]
- Brandt, S.; Winter, A.; Lauer, H.C.; Kollmar, F.; Portscher-Kim, S.J.; Romanos, G.E. IPS e.max for All-Ceramic Restorations: Clinical Survival and Success Rates of Full-Coverage Crowns and Fixed Partial Dentures. Materials 2019, 12, 462. [Google Scholar] [CrossRef] [PubMed]
- Cagidiaco, E.; Grandini, S.; Goracci, C.; Joda, T. A pilot trial on lithium disilicate partial crowns using a novel prosthodontic functional index for teeth (FIT). BMC Oral Health 2019, 19, 276. [Google Scholar] [CrossRef]
- El-Rashidy, A.A.; Abdelraouf, R.M.; Habib, N.A. Effect of two artificial aging protocols on color and gloss of single-shade versus multi-shade resin composites. BMC Oral Health 2022, 22, 321. [Google Scholar] [CrossRef]
- Heintze, S.; Forjanic, M.; Ohmiti, K.; Rousson, V. Surface deterioration of dental materials after simulated toothbrushing in relation to brushing time and load. Dent. Mater. Off. Publ. Acad. Dent. Mater. 2010, 26, 306–319. [Google Scholar] [CrossRef] [PubMed]
- AlAli, M.; Silikas, N.; Satterthwaite, J. The Effects of Toothbrush Wear on the Surface Roughness and Gloss of Resin Composites with Various Types of Matrices. Dent. J. 2021, 9, 8. [Google Scholar] [CrossRef]
- Köroğlu, A.; Sahin, O.; Küçükekenci, A.; Dede, D.; Yıldırım, H.; Yilmaz, B. Influences of Toothbrushing and Different Toothpastes on the Surface Roughness and Color Stability of Interim Prosthodontic Materials. Materials 2022, 15, 5831. [Google Scholar] [CrossRef] [PubMed]
- Yuan, J.C.-C.; Barão, V.A.R.; Wee, A.G.; Alfaro, M.F.; Afshari, F.S.; Sukotjo, C. Effect of brushing and thermocycling on the shade and surface roughness of CAD-CAM ceramic restorations. J. Prosthet. Dent. 2018, 119, 1000–1006. [Google Scholar] [CrossRef]
- Stawarczyk, B.; Liebermann, A.; Eichberger, M.; Güth, J.-F. Evaluation of mechanical and optical behavior of current esthetic dental restorative CAD/CAM composites. J. Mech. Behav. Biomed. Mater. 2016, 55, 1–11. [Google Scholar] [CrossRef] [PubMed]
- Anil, N.; Bolay, S. Effect of Toothbrushing on the Material Loss, Roughness, and Color of Intrinsically and Extrinsically Stained Porcelain Used in Metal-Ceramic Restorations: An in Vitro Study. Int. J. Prosthodont. 2002, 15, 483–487. [Google Scholar] [PubMed]
- Lee, W.-F.; Iwasaki, N.; Peng, P.-W.; Takahashi, H. Effect of toothbrushing on the optical properties and surface roughness of extrinsically stained high-translucency zirconia. Clin. Oral Investig. 2022, 26, 3041–3048. [Google Scholar] [CrossRef]
- Garza, L.A.; Thompson, G.; Cho, S.H.; Berzins, D.W. Effect of toothbrushing on shade and surface roughness of extrinsically stained pressable ceramics. J. Prosthet. Dent. 2016, 115, 489–494. [Google Scholar] [CrossRef] [PubMed]
- McCracken, G.; Janssen, J.; Swan, M.; Steen, N.; de Jager, M.; Heasman, P. Effect of brushing force and time on plaque removal using a powered toothbrush. J. Clin. Periodontol. 2003, 30, 409–413. [Google Scholar] [CrossRef]
- Kamonkhantikul, K.; Arksornnukit, M.; Lauvahutanon, S.; Takahashi, H. Toothbrushing alters the surface roughness and gloss of composite resin CAD/CAM blocks. Dent. Mater. J. 2016, 35, 225–232. [Google Scholar] [CrossRef] [PubMed]
- Subaşı, M.G.; Çakmak, G.; Sert, M.; Yilmaz, B. Effect of multiple firings on surface roughness and flexural strength of CAD-CAM ceramics. J. Prosthet. Dent. 2022, 128, 216.e211–216.e218. [Google Scholar] [CrossRef] [PubMed]
- Meng, H.; Xie, H.; Yang, L.; Chen, B.; Chen, Y.; Zhang, H.; Chen, C. Effects of multiple firings on mechanical properties and resin bonding of lithium disilicate glass-ceramic. J. Mech. Behav. Biomed. Mater. 2018, 88, 362–369. [Google Scholar] [CrossRef]
- Gonuldas, F.; Yılmaz, K.; Ozturk, C. The effect of repeated firings on the color change and surface roughness of dental ceramics. J. Adv. Prosthodont. 2014, 6, 309–316. [Google Scholar] [CrossRef]
- Tanoue, N.; Matsumura, H.; Atsuta, M. Wear and surface roughness of current prosthetic composites after toothbrush/dentifrice abrasion. J. Prosthet. Dent. 2000, 84, 93–97. [Google Scholar] [CrossRef]
- Vásquez, V.; Ozcan, M.; Nishioka, R.; Souza, R.; Mesquita, A.; Pavanelli, C. Mechanical and thermal cycling effects on the flexural strength of glass ceramics fused to titanium. Dent. Mater. J. 2008, 27, 7–15. [Google Scholar] [CrossRef] [PubMed]
- Egilmez, F.; Ergun, G.; Cekic-Nagas, I.; Vallittu, P.K.; Lassila, L.V.J. Does artificial aging affect mechanical properties of CAD/CAM composite materials. J. Prosthodont. Res. 2018, 62, 65–74. [Google Scholar] [CrossRef]
- Ciobica, A.; Padurariu, M.; Curpan, A.; Antioch, I.; Chirita, R.; Stefanescu, C.; Luca, A.C.; Tomida, M. Minireview on the Connections between the Neuropsychiatric and Dental Disorders: Current Perspectives and the Possible Relevance of Oxidative Stress and Other Factors. Oxid. Med. Cell. Longev. 2020, 2020, 6702314. [Google Scholar] [CrossRef]
- Ludovichetti, F.S.; Trindade, F.Z.; Werner, A.; Kleverlaan, C.J.; Fonseca, R.G. Wear resistance and abrasiveness of CAD-CAM monolithic materials. J. Prosthet. Dent. 2018, 120, 318.e311–318.e318. [Google Scholar] [CrossRef]
- Rodrigues, C.R.T.; Turssi, C.P.; Amaral, F.L.B.; Basting, R.T.; França, F.M.G. Changes to Glazed Dental Ceramic Shade, Roughness, and Microhardness after Bleaching and Simulated Brushing. J. Prosthodont. 2019, 28, e59–e67. [Google Scholar] [CrossRef]
- Nawras, A.; Nafea, I. Effects of Different Core Thickness on The Microhardness of Lithium-Disilicate Glass Ceramic. J. Oral Dent. Res. 2019, 6, 51–58. [Google Scholar]
- Mohammed, B.; Afram, B.; Nazar, Z. An evaluation of the effect of different surface treatment on hardness and smoothness of pressable ceramic (in vitro study). IOSR J. Dent. Med. Sci. 2015, 14, 84–89. [Google Scholar]
- Albakry, M.; Guazzato, M.; Swain, M.V. Fracture toughness and hardness evaluation of three pressable all-ceramic dental materials. J. Dent. 2003, 31, 181–188. [Google Scholar] [CrossRef]
- Della Bona, A.; Pecho, O.E.; Ghinea, R.; Cardona, J.C.; Pérez, M.M. Colour parameters and shade correspondence of CAD-CAM ceramic systems. J. Dent. 2015, 43, 726–734. [Google Scholar] [CrossRef]
- Alessandretti, R.; Borba, M.; Benetti, P.; Corazza, P.H.; Ribeiro, R.; Della Bona, A. Reliability and mode of failure of bonded monolithic and multilayer ceramics. Dent. Mater. 2017, 33, 191–197. [Google Scholar] [CrossRef] [PubMed]
- Sfondrini, M.F.; Gandini, P.; Malfatto, M.; Di Corato, F.; Trovati, F.; Scribante, A. Computerized Casts for Orthodontic Purpose Using Powder-Free Intraoral Scanners: Accuracy, Execution Time, and Patient Feedback. BioMed Res. Int. 2018, 2018, 4103232. [Google Scholar] [CrossRef] [PubMed]
- Abou-Obaid, A.A.; Almawash, A.; Alyabis, N.; Alzaaqi, N. An In Vitro Evaluation of the Effect of Polishing on the Stainability of Different CAD/CAM Ceramic Materials. Saudi Dent. J. 2019, 32, 135–141. [Google Scholar] [CrossRef] [PubMed]
- Maciel, L.; Silva, C.; Jesus, R.; Concílio, L.; Kano, S.; Xible, A. Influence of polishing systems on roughness and color change of two dental ceramics. J. Adv. Prosthodont. 2019, 11, 215. [Google Scholar] [CrossRef]
- Garza, L.A. Effect of Toothbrushing on Surface Roughness and Shade of Extrinsically Stained Pressable Ceramic Restorations. Master’s Thesis, Marquette University, Milwaukee, WI, USA, 2015. [Google Scholar]
- Schelkopf, S.; Dini, C.; Beline, T.; Wee, A.G.; Barão, V.A.; Sukotjo, C.; Yuan, J.C.-C. The Effect of Smoking and Brushing on the Color Stability and Stainability of Different CAD/CAM Restorative Materials. Materials 2022, 15, 6901. [Google Scholar] [CrossRef] [PubMed]
- Palla, E.-S.; Kontonasaki, E.; Kantiranis, N.; Papadopoulou, L.; Zorba, T.; Paraskevopoulos, K.M.; Koidis, P. Color stability of lithium disilicate ceramics after aging and immersion in common beverages. J. Prosthet. Dent. 2018, 119, 632–642. [Google Scholar] [CrossRef]
- Heffernan, M.J.; Aquilino, S.A.; Diaz-Arnold, A.M.; Haselton, D.R.; Stanford, C.M.; Vargas, M.A. Relative translucency of six all-ceramic systems. Part II: Core and veneer materials. J. Prosthet. Dent. 2002, 88, 10–15. [Google Scholar] [CrossRef] [PubMed]
- Comba, A.; Paolone, G.; Baldi, A.; Vichi, A.; Goracci, C.; Bertozzi, G.; Scotti, N. Effects of Substrate and Cement Shade on the Translucency and Color of CAD/CAM Lithium-Disilicate and Zirconia Ceramic Materials. Polymers 2022, 14, 1778. [Google Scholar] [CrossRef]
- Mahrous, A.A.; Ellakany, P.; Abualsaud, R.; Al-Thobity, A.M.; Akhtar, S.; Siddiqui, I.A.; Gad, M.M. Comparative Study of the Effectiveness of Laboratory-Formulated Polishing Pastes for Two CAD/CAM Ceramic Restorative Materials. J. Prosthodont. 2022, 31, 529–536. [Google Scholar] [CrossRef] [PubMed]
| Materials | |||
|---|---|---|---|
| Emax CAD (EC) | Emax Press (EP) | LiSi Press (LP) | |
| Brand name | IPS Emax CAD, Ivoclar Vivadent, Schaan, Liechtenstein. | IPS Emax Press, Ivoclar Vivadent, Schaan, Liechtenstein. | GC Initial LiSi Press, GC Corp, Tokyo, Japan. |
| Composition | SiO2, Li2O, K2O, P2O5, ZrO2, ZnO, Al2O3, MgO. | SiO2, Li2O, K2O, P2O5, ZrO2, ZnO. | SiO2, Al2O3, Li2O, K2O, ZrO2, Na2O, P2O5, ZrO2. |
| Fabrication techniques | Diamond saw on low speed under water cooling (ISOMET 5000 Linear Precision Saw, Buehler Ltd., IL, USA). | ||
| Finishing and polishing | Grit carbide sandpapers (#600, #1200, and #2400) under running water utilizing a polishing machine (MetaServ 250 Grinder-Polisher with Vector Power Head, Buehler, IL, USA). | ||
| Glazing | All the ceramic materials were glazed as per the manufacturer’s instructions (710 °C, Programat CS2; Ivoclar Vivadent AG). Vacuum stages: St 1: 450. St 2: 709. Pre-heat: 6-min, then it will raise the temperature by 60 degrees each min until it reaches 710 degrees. After 1-min, start cooling. | ||
| Properties | Brushing | EC | EP | LP | + P |
|---|---|---|---|---|---|
| Surface roughness (µm) | Before | 0.73 ± 0.06 | 0.73 ± 0.02 | 0.77 ± 016 | 0.993 |
| After | 0.67 ± 0.16 | 0.64 ± 0.13 | 0.64 ± 0.08 | 0.842 | |
| ++ p | 0.327 | 0.069 | 0.161 | ||
| microhardness (VHN) | Before | 1429.92 ± 144.25 | 1381.82 ± 101.31 | 1458.42 ± 179.86 | 0.576 |
| After | 1119.51 ± 164.47 | 862.45 ± 273.83 | 1084.30 ± 159.72 | 0.043 | |
| ++ p | 0.012 | 0.001 | <0.001 |
| Color Parameters | Materials | + P | |||
|---|---|---|---|---|---|
| EC | EP | LP | |||
| L* | Before | 65.18 ± 2.60 | 68.74 ± 1.43 | 65.70 ± 1.35 | 0.002 |
| After | 61.89 ± 5.16 | 60.95 ± 8.04 | 55.94 ± 14.01 | 0.441 | |
| ΔL* | 3.29 ± 5.54 | 7.79 ± 8.02 | 9.76 ± 14.44 | ||
| ++ P | 0.093 | 0.012 | 0.123 | ||
| a* | Before | −1.91 ± 0.72 | −1.72 ± 0.09 | −1.67 ± 0.08 | 0.500 |
| After | −1.72 ± 0.62 | −1.17 ± 0.45 | −1.06 ± 0.58 | 0.060 | |
| Δa* | −0.19 ± 0.36 | −0.56 ± 0.46 | −0.61 ± 0.61 | ||
| ++ P | 0.208 | 0.012 | 0.017 | ||
| b* | Before | −1.13 ± 1.02 | 5.04 ± 0.62 | 4.93 ± 0.59 | <0.001 |
| After | −0.68 ± 0.70 | 4.39 ± 1.11 a | 4.19 ± 2.60 a | <0.001 | |
| Δb* | −0.45 ± 0.90 | 0.64 ± 1.40 | 0.74 ± 2.55 | ||
| ++ P | 0.123 | 0.123 | 0.575 | ||
| Color Change | EC | EP | LP | + p-Value |
|---|---|---|---|---|
| ΔE | 4.23 ± 1.55 | 7.86 ± 4.13 | 11.67 ± 3.02 | 0.251 |
| ++ P | --- | Vs. EC = 0.195 | Vs. EC = 0.161 | |
| --- | -- | Vs. EP = 0.878 |
| Materials | ΔE | NBS | Clinical Considerations |
|---|---|---|---|
| EC | 4.23 ± 1.55 | 3.89 | considerable (NBS = 3.0–6.0) |
| EP | 7.86 ± 4.13 | 7.23 | very (NBS = 6.0–12.0) |
| LP | 11.67 ± 3.02 | 10.73 | very (NBS = 6.0–12.0) |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Mahrous, A.A.; Alhammad, A.; Alqahtani, F.; Aljar, Y.; Alkadi, A.; Taymour, N.; Alotaibi, A.; Akhtar, S.; Gad, M.M. The Toothbrushing Effects on Surface Properties and Color Stability of CAD/CAM and Pressable Ceramic Fixed Restorations—An In Vitro Study. Materials 2023, 16, 2950. https://doi.org/10.3390/ma16082950
Mahrous AA, Alhammad A, Alqahtani F, Aljar Y, Alkadi A, Taymour N, Alotaibi A, Akhtar S, Gad MM. The Toothbrushing Effects on Surface Properties and Color Stability of CAD/CAM and Pressable Ceramic Fixed Restorations—An In Vitro Study. Materials. 2023; 16(8):2950. https://doi.org/10.3390/ma16082950
Chicago/Turabian StyleMahrous, Amr A., Abdullah Alhammad, Faisal Alqahtani, Yousif Aljar, Ahmed Alkadi, Noha Taymour, Abdulkareem Alotaibi, Sultan Akhtar, and Mohammed M. Gad. 2023. "The Toothbrushing Effects on Surface Properties and Color Stability of CAD/CAM and Pressable Ceramic Fixed Restorations—An In Vitro Study" Materials 16, no. 8: 2950. https://doi.org/10.3390/ma16082950
APA StyleMahrous, A. A., Alhammad, A., Alqahtani, F., Aljar, Y., Alkadi, A., Taymour, N., Alotaibi, A., Akhtar, S., & Gad, M. M. (2023). The Toothbrushing Effects on Surface Properties and Color Stability of CAD/CAM and Pressable Ceramic Fixed Restorations—An In Vitro Study. Materials, 16(8), 2950. https://doi.org/10.3390/ma16082950









