Cauterization of Narrow Root Canals Untouched by Instruments by High-Frequency Current
Abstract
:1. Introduction
2. Materials and Methods
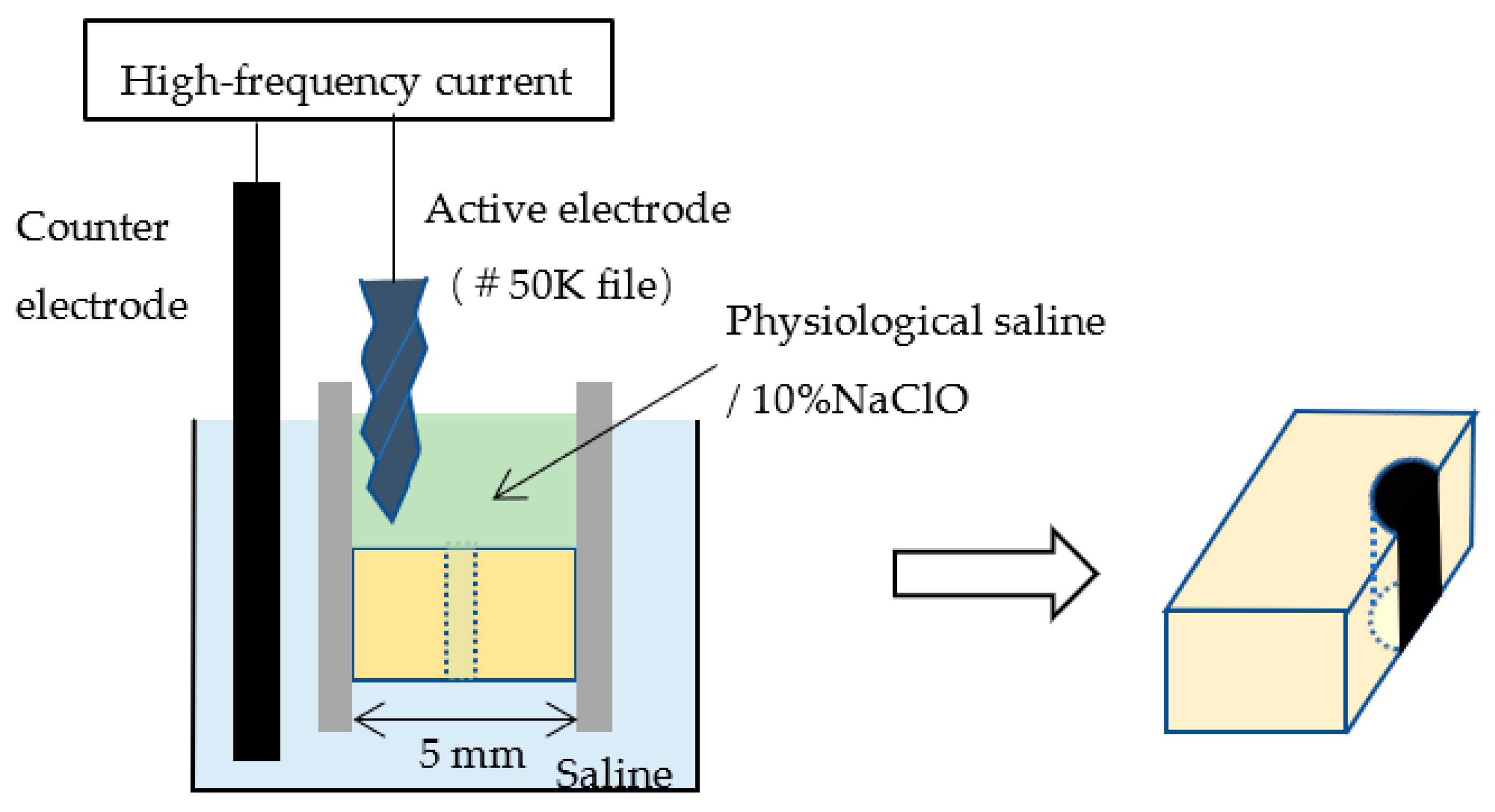
2.1. Root Canal Model Preparation
2.2. Conduction of High-Frequency Electric Current
2.3. Evaluation Method
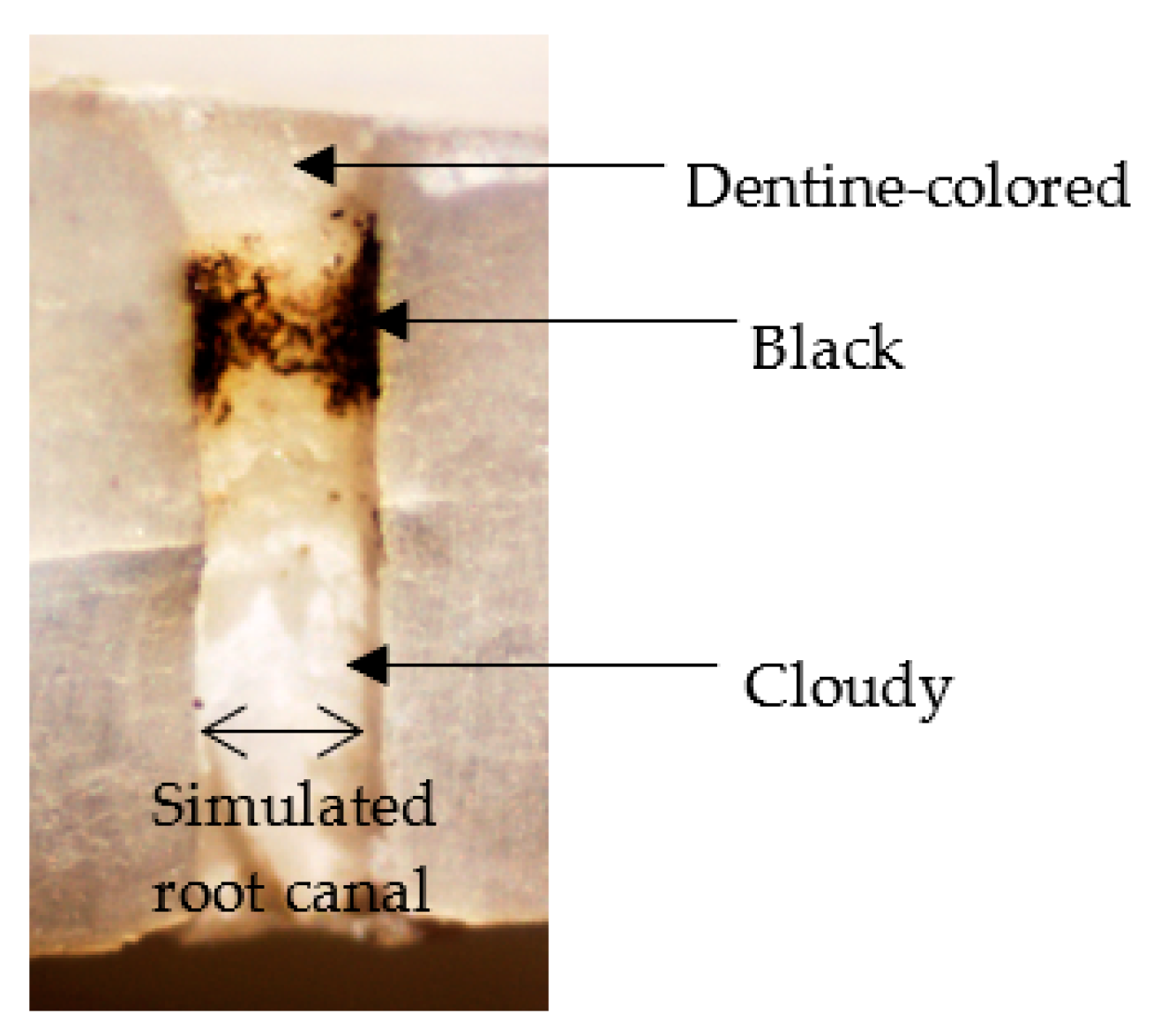
2.3.1. Evaluation by Optical Microscopy
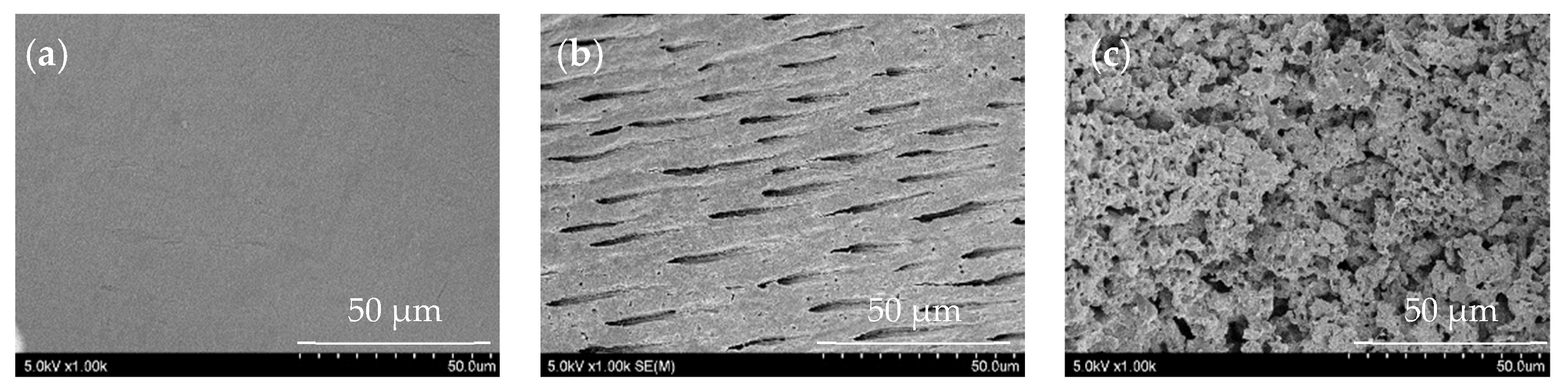
2.3.2. Evaluation by Scanning Electron Microscopy (SEM)
2.3.3. Evaluation by Energy Dispersive X-ray Spectroscopy
2.3.4. Statistical Analysis
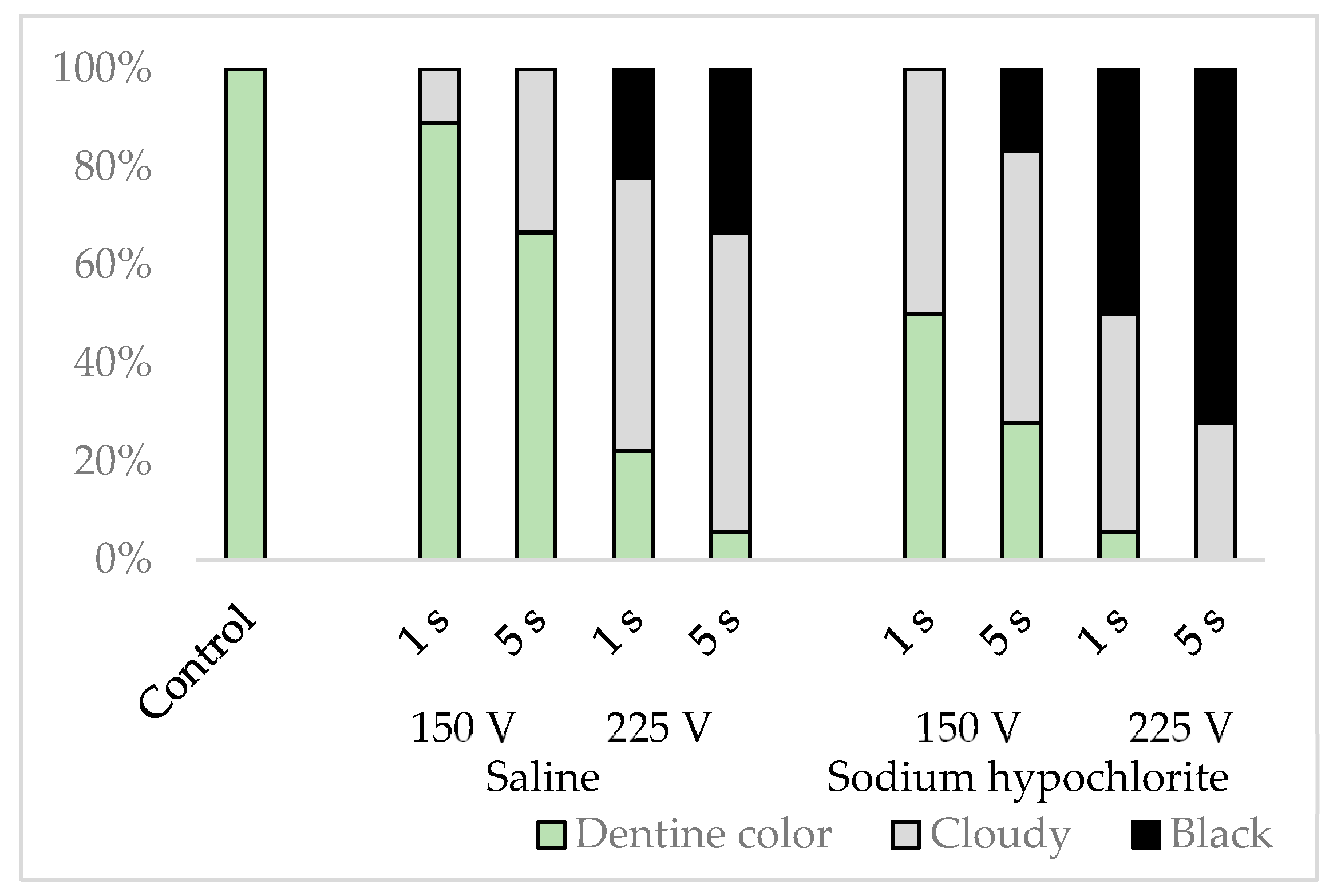
3. Results
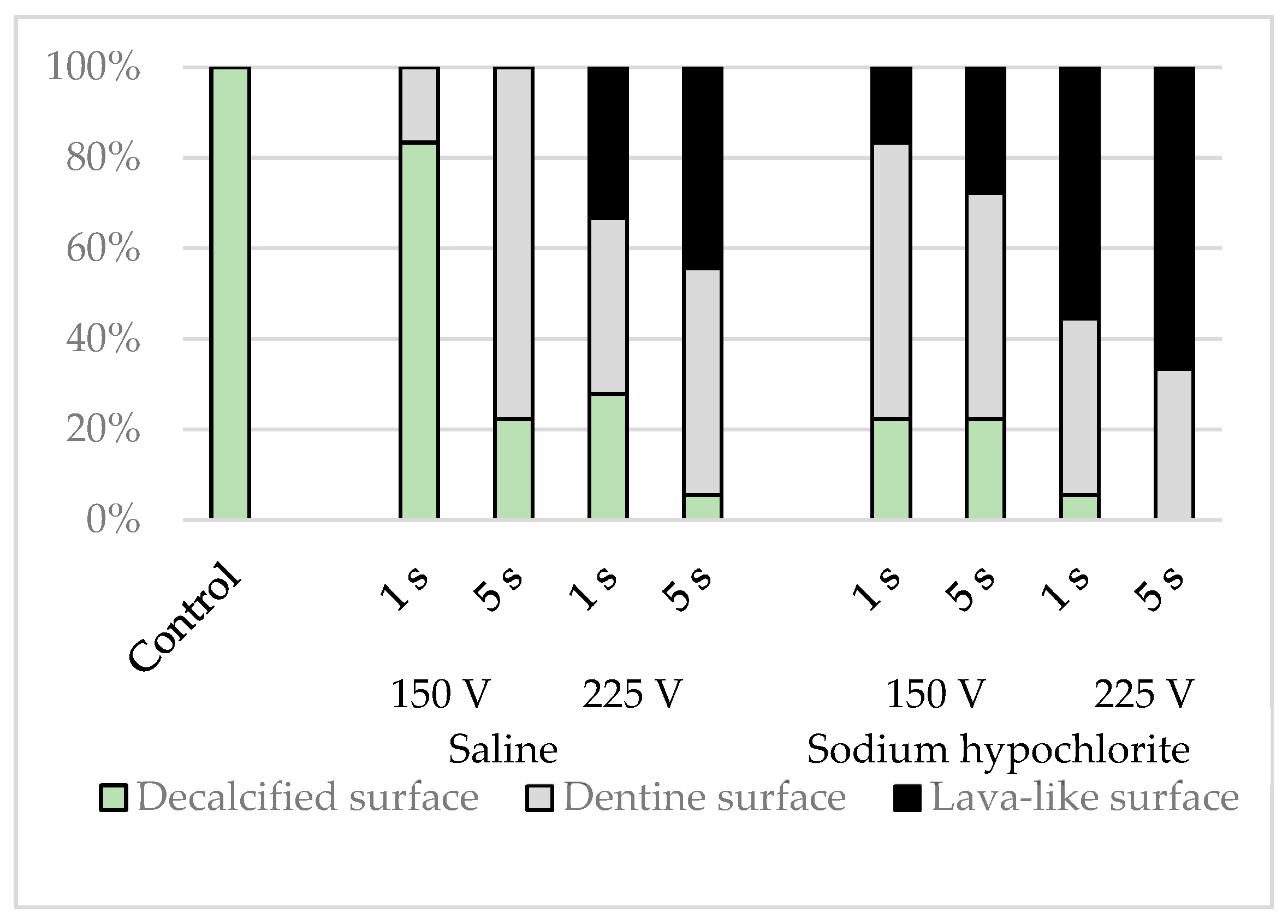
3.1. Evaluation by Optical Microscopy
3.2. Evaluation by SEM
3.3. Evaluation by EDS
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Siqueira, J.F., Jr. Strategies to treat infected root canals. J. Calif. Dent. Assoc. 2001, 29, 825–837. [Google Scholar] [CrossRef] [PubMed]
- Ricucci, D.; Russo, J.; Rutberg, M.; Burleson, J.A. A prospective cohort study of endodontic treatments of 1,369 root canals: Results after 5 years. Oral Surg. Oral Med. Oral Pathol. Oral Radiol. Endod. 2011, 112, 825–842. [Google Scholar] [CrossRef] [PubMed]
- Pettiette, M.T.; Delano, E.O.; Trope, M. Evaluation of success rate of endodontic treatment performed by students with stainless-steel K-files and nickel-titanium hand files. J. Endod. 2001, 27, 124–127. [Google Scholar] [CrossRef] [PubMed]
- Cheung, G.S.; Liu, C.S. A retrospective study of endodontic treatment outcome between nickel-titanium rotary and stainless steel hand filing techniques. J. Endod. 2009, 35, 938–943. [Google Scholar] [CrossRef]
- Kashefinejad, M.; Harandi, A.; Eram, S.; Bijani, A. Comparison of Single Visit Post Endodontic Pain Using Mtwo Rotary and Hand K-File Instruments: A Randomized Clinical Trial. J. Dent. 2016, 13, 10–17. [Google Scholar]
- Nagendrababu, V.; Ahmed, H.M.A. Shaping properties and outcomes of nickel-titanium rotary and reciprocation systems using micro-computed tomography: A systematic review. Quintessence Int. 2019, 50, 186–195. [Google Scholar] [CrossRef]
- Bartols, A.; Bormann, C.; Werner, L.; Schienle, M.; Walther, W.; Dörfer, C.E. A retrospective assessment of different endodontic treatment protocols. PeerJ 2020, 30, e8495. [Google Scholar] [CrossRef]
- Boonchoo, K.; Leelataweewud, P.; Yanpiset, K.; Jirarattanasopha, V. Simplify pulpectomy in primary molars with a single-file reciprocating system: A randomized controlled clinical trial. Clin. Oral Investig. 2020, 24, 2683–2689. [Google Scholar] [CrossRef]
- Liu, Y.; Chen, M.; Tang, W.; Liu, C.; Du, M. Comparison of five single-file systems in the preparation of severely curved root canals: An ex vivo study. BMC Oral Health 2022, 22, 649. [Google Scholar] [CrossRef]
- Sjogren, U.; Hagglund, B.; Sundqvist, G.; Wing, K. Factors affecting the long-term results of endodontic treatment. J. Endod. 1990, 16, 498–504. [Google Scholar] [CrossRef]
- Wu, M.K.; Wesselink, P.R.; Walton, R.E. Apical terminus location of root canal treatment procedures. Oral Surg. Oral Med. Oral Pathol. Oral Radiol. Endod. 2000, 89, 99–103. [Google Scholar] [CrossRef]
- Gorni, F.G.; Gagliani, M.M. The outcome of endodontic retreatment: A 2-yr follow-up. J. Endod. 2004, 30, 1–4. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Arias, A.; Azabal, M.; Hidalgo, J.J.; de la Macorra, J.C. Relationship between postendodontic pain, tooth diagnostic factors, and apical patency. J. Endod. 2009, 35, 189–192. [Google Scholar] [CrossRef]
- Tabassum, S.; Khan, F.R. Failure of endodontic treatment: The usual suspects. Eur. J. Dent. 2016, 10, 144–147. [Google Scholar] [CrossRef] [PubMed]
- Hasselgren, G.; Olsson, B.; Cvek, M. Effects of calcium hydroxide and sodium hypochlorite on the dissolution of necrotic porcine muscle tissue. J. Endod. 1988, 14, 125–127. [Google Scholar] [CrossRef]
- Stevens, R.H.; Grossman, L.I. Evaluation of the antimicrobial potential of calcium hydroxide as an intracanal medicament. J. Endod. 1983, 9, 372–374. [Google Scholar] [CrossRef] [PubMed]
- Wadachi, R.; Araki, K.; Suda, H. Effect of calcium hydroxide on the dissolution of soft tissue on the root canal wall. J. Endod. 1998, 24, 326–330. [Google Scholar] [CrossRef]
- Prada, I.; Micó-Muñoz, P.; Giner-Lluesma, T.; Micó-Martínez, P.; Muwaquet-Rodríguez, S.; Albero-Monteagudo, A. Update of the therapeutic planning of irrigation and intracanal medication in root canal treatment. A literature review. J. Clin. Exp. Dent. 2019, 11, e185–e193. [Google Scholar] [CrossRef]
- Ruksakiet, K.; Hanák, L.; Farkas, N.; Hegyi, P.; Sadaeng, W.; Czumbel, L.M.; Sang-Ngoen, T.; Garami, A.; Mikó, A.; Varga, G.; et al. Antimicrobial efficacy of chlorhexidine and sodium hypochlorite in root canal disinfection: A systematic review and meta-analysis of randomized controlled trials. J. Endod. 2020, 46, 1032–1041.e7. [Google Scholar] [CrossRef]
- Dotto, L.; Sarkis, R.O.; Bacchi, A.; Rocha, P.G.K. Effect of root canal irrigants on the mechanical properties of endodontically treated teeth: A scoping review. J. Endod. 2020, 46, 596–604.e3. [Google Scholar] [CrossRef]
- Bapat, R.A.; Parolia, A.; Chaubal, T.; Yang, H.J.; Kesharwani, P.; Phaik, K.S.; Lin, S.L.; Daood, U. Recent update on applications of quaternary ammonium silane as an antibacterial biomaterial: A novel drug delivery approach in dentistry. Front. Microbiol. 2022, 13, 927282. [Google Scholar] [CrossRef] [PubMed]
- Ali, A.; Bhosale, A.; Pawar, S.; Kakti, A.; Bichpuriya, A.; Agwan, M.A. Current trends in root canal irrigation. Cureus 2022, 14, e24833. [Google Scholar] [CrossRef] [PubMed]
- Tonini, R.; Salvadori, M.; Audino, E.; Sauro, S.; Garo, M.L.; Salgarello, S. Irrigating solutions and activation methods used in clincal endodontics: A systematic review. Front. Oral Health 2022, 3, 838043. [Google Scholar] [CrossRef] [PubMed]
- Shuping, G.B.; Ørstavik, D.; Sigurdsson, A.; Trope, M. Reduction of intracanal bacteria using nickel- titanium rotary instrumentation and various medications. J. Endod. 2000, 26, 751–755. [Google Scholar] [CrossRef]
- Ricucci, D.; Siqueira, J.F. Fate of the tissue in lateral canals and apical ramifications in response to pathologic conditions and treatment procedures. J. Endod. 2010, 36, 1–15. [Google Scholar] [CrossRef]
- Zeng, C.; Willison, J.; Meghil, M.M.; Bergeron, B.E.; Cutler, C.W.; Tay, F.R.; Niu, L.; Ma, J. Antibacterial efficacy of an endodontic sonic-powered irrigation system: An in vitro study. J. Dent. 2018, 75, 105–112. [Google Scholar] [CrossRef] [PubMed]
- Siqueira, J.F., Jr.; Pérez, A.R.; Marceliano-Alves, M.F.; Provenzano, J.C.; Silva, S.G.; Pires, F.R.; Vieira, G.C.S.; Rôças, I.N.; Alves, F.R.F. What happens to unprepared root canal walls: A correlative analysis using micro-computed tomography and histology/scanning electron microscopy. Int. Endod. J. 2018, 5, 501–508. [Google Scholar] [CrossRef]
- Carli, E.; Pasini, M.; Pardossi, F.; Capotosti, I.; Narzisi, A.; Lardani, L. Oral health preventive program in patients with autism spectrum disorder. Children 2022, 9, 535. [Google Scholar] [CrossRef]
- Setzer, F.C.; Kohli, M.R.; Shah, S.B.; Karabucak, B.; Kim, S. Outcome of endodontic surgery: A meta-analysis of the literature—Part 2: Comparison of endodontic microsurgical techniques with and without the use of higher magnification. J. Endod. 2012, 38, 1–10. [Google Scholar] [CrossRef]
- Kohli, M.R.; Berenji, H.; Setzer, F.C.; Lee, S.M.; Karabucak, B. Outcome of endodontic surgery: A meta-analysis of the literature-Part 3: Comparison of endodontic microsurgical techniques with 2 different root-end filling materials. J. Endod. 2018, 44, 923–931. [Google Scholar] [CrossRef]
- De Baets, P. Current indications for electroshock. Scalpel 1957, 110, 925–931. [Google Scholar] [PubMed]
- Marcinko, D.E.; Field, N.; Barnett, L. Use of the Shaw scalpel in podiatric surgery. J. Foot Surg. 1984, 23, 457–460. [Google Scholar] [PubMed]
- Realland, R. Treatment of apical lesions by high frequency currents. Rev. Odontostomatol. 1946, 2, 219–223. [Google Scholar] [PubMed]
- Crone, F.L. Studies in root canal therapy. II. Experimental study on heating of an aqueous 2% solution of chloramine T in the root canal by means of high frequency alternating current generator (joulisator). Tandlaegebladet 1954, 58, 599–621. [Google Scholar]
- Kjaer, E.W. Clinical study on use of high frequency current in root canal therapy. Odontol. Tidskr. 1955, 63, 215–227. [Google Scholar]
- Kownacki, S. High-frequency currents in electrodiagnosis of dental pulp. Protet. Stomatol. 1971, 21, 133–136. [Google Scholar]
- Benz, C.; Schwarz, P.; Sonnabend, E. Effects of the high-frequency current used in electrosurgery on hard tooth substance and pulp. Dtsch. Zahnarztl. Z 1987, 42, 897–899. [Google Scholar]
- Karale, R.; Thakore, A.; Shetty, V.J. An evaluation of antibacterial efficacy of 3% sodium hypochlorite, high-frequency alternating current and 2% chlorhexidine on Enterococcus faecalis: An in vitro study. Conserv. Dent. 2011, 14, 2–5. [Google Scholar] [CrossRef] [Green Version]
- Callen, H.B. Thermodynamics; Wiley International, John Wiley and Sans: New York, NY, USA, 1960; p. 300. [Google Scholar]
- Tarao, H.; Akutagawa, M.; Emoto, T.; Takei, A.; Yumoto, H.; Tominaga, T.; Ikehara, T.; Kinouchi, Y. Evaluation of temperature increase from joule heat in numerical tooth model by applying 500 kHz current for apical periodontitis treatment -effect of applied voltage and tooth conductivity. Bioelectromagnetics 2021, 42, 224–237. [Google Scholar] [CrossRef]
- Armengol, V.; Jean, A.; Rohanizadeh, R.; Hamel, H. Scanning electron microscopic analysis of diseased and healthy dental hard tissues after Er:YAG laser irradiation: In vitro study. J. Endod. 1999, 25, 543–546. [Google Scholar] [CrossRef]
- Takeda, F.H.; Harashima, T.; Eto, J.N.; Kimura, Y.; Matsumoto, K. Effect of Er:YAG laser treatment on the root canal walls of human teeth: An SEM study. Endod. Dent. Traumatol. 1998, 14, 270–273. [Google Scholar] [CrossRef] [PubMed]
- Kim, M.E.; Jeoung, D.J.; Kim, K.S. Effects of water flow on dental hard tissue ablation using Er:YAG laser. J. Clin. Laser Med. Surg. 2003, 21, 139–144. [Google Scholar] [CrossRef] [PubMed]
- Hoke, J.A.; Burkes, E.J., Jr.; Gomes, E.D.; Wolbarsht, M.L. Erbium:YAG (2.94 mum) laser effects on dental tissues. J. Laser Appl. 1990, 2, 61–65. [Google Scholar] [CrossRef] [PubMed]
- Karaki, W.; Rahul, L.C.A.; Borca-Tasciuc, D.A.D.S. A continuum thermomechanical model of in vivo electrosurgical heating of hydrated soft biological tissues. Int. J. Heat Mass Transf. 2018, 127 Pt A, 961–974. [Google Scholar] [CrossRef]
- Sommers, B.S.; Foster, J.E. Plasma formation in underwater gas bubbles. Plasma. Sources Sci. Technol. 2014, 23, 015020. [Google Scholar] [CrossRef]
- Zhou, R.; Zhou, R.; Wang, P.; Luan, B.; Zhang, X.; Fang, Z.; Xian, Y.; Lu, X.; Ostrikov, K.K.; Bazaka, K. Microplasma bubbles: Reactive vehicles for biofilm dispersal. ACS Appl. Mater. Interfaces 2019, 11, 20660–20669. [Google Scholar] [CrossRef]
- Mai-Prochnow, A.; Zhou, R.; Zhang, T.; Ostrikov, K.; Mugunthan, S.; Rice, S.A.; Cullen, P.J. Interactions of plasma-activated water with biofilms: Inactivation, dispersal effects and mechanisms of action. NPJ Biofilms Microbiomes 2021, 7, 11. [Google Scholar] [CrossRef]
- Lin, J.; Zhang, J.; Zhou, R.; Guo, L.; Liu, D.; Rong, M.; Kong, M.G.; Ostrikov, K.K. Plasma-enhanced microbial electrolytic disinfection: Decoupling electro- and plasma-chemistry in plasma-electrolyzed oxidizing water using ion-exchange membranes. Water Res. 2022, 225, 119174. [Google Scholar] [CrossRef]
- Salgado, B.A.B.; Fabbri, S.; Dickenson, A.; Hasan, M.I.; Walsh, J.L. Surface barrier discharges for Escherichia coli biofilm inactivation: Modes of action and the importance of UV radiation. PLoS ONE 2021, 16, e0247589. [Google Scholar] [CrossRef]
- Cassanelli, C.; Marchese, A.; Cagnacci, S.; Debbia, E.A. Alteration of membrane permeability of bacteria and yeast by high frequency alternating current (HFAC). Open Microbiol. J. 2008, 2, 32–37. [Google Scholar] [CrossRef]
- Kvinnsland, S.; Heyeraas, K.; Ofjord, E.S. Effect of experimental tooth movement on periodontal and pulpal blood flow. Eur. J. Orthod. 1989, 11, 200–2005. [Google Scholar] [CrossRef] [PubMed]
- Eriksson, R.; Albrektsson, T. Temperature threshold levels for heat induced bone tissue injury: A vital-microscopic study in the rabbit. J. Prosthet. Dent. 1983, 50, 101–107. [Google Scholar] [CrossRef] [PubMed]
- Holland, G.R. Periapical neural changes after pulpectomy. Oral Surg. Oral Med. Oral Pathol. Oral Radiol. Endod. 1995, 80, 726–734. [Google Scholar] [CrossRef] [PubMed]



| Root Canal Solution | Voltage | Conduction Time | |
|---|---|---|---|
| Conduction group | Physiological saline | 150 | 1 |
| 5 | |||
| 225 | 1 | ||
| 5 | |||
| NaClO | 150 | 1 | |
| 5 | |||
| 225 | 1 | ||
| 5 | |||
| Control group | NaClO | - | - |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Kumagai, H.; Sugaya, T.; Tominaga, T. Cauterization of Narrow Root Canals Untouched by Instruments by High-Frequency Current. Materials 2023, 16, 2542. https://doi.org/10.3390/ma16072542
Kumagai H, Sugaya T, Tominaga T. Cauterization of Narrow Root Canals Untouched by Instruments by High-Frequency Current. Materials. 2023; 16(7):2542. https://doi.org/10.3390/ma16072542
Chicago/Turabian StyleKumagai, Hiromichi, Tsutomu Sugaya, and Toshihiko Tominaga. 2023. "Cauterization of Narrow Root Canals Untouched by Instruments by High-Frequency Current" Materials 16, no. 7: 2542. https://doi.org/10.3390/ma16072542
APA StyleKumagai, H., Sugaya, T., & Tominaga, T. (2023). Cauterization of Narrow Root Canals Untouched by Instruments by High-Frequency Current. Materials, 16(7), 2542. https://doi.org/10.3390/ma16072542






