Comparative Assessment of the Shaping Ability of Reciproc Blue, WaveOne Gold, and ProTaper Gold in Simulated Root Canals
Abstract
:1. Introduction
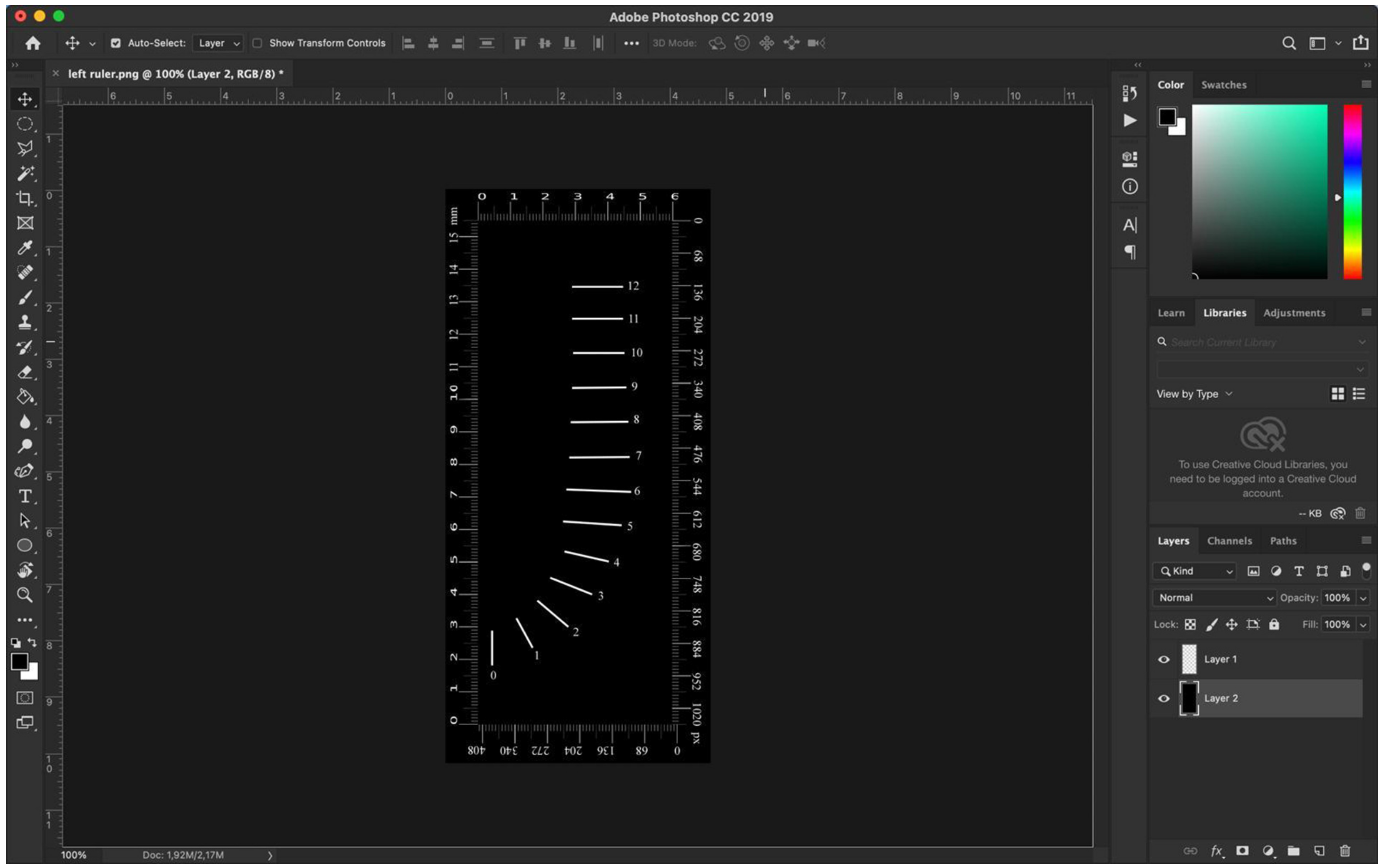
2. Materials and Methods
- the amount of resin removed on the inner part of the curvature, X1
- the amount of resin removed on the outer part of the curvature, X2
- the total amount of resin removed, X1 + X2
- the amount and direction of transportation, X1 − X2
- the centering ratio (X1 − X2)/Y, where Y is the total width of the shaped root canal.
3. Results
3.1. Statistical Analysis of the Apical Third (Levels 0 to 4)
3.2. Statistical Analysis of the Middle Third (Levels 5 to 8)
3.3. Statistical Analysis of the Coronal Third (Levels 9 to 12)
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Hülsmann, M.; Peters, O.A.; Dummer, P.M. Mechanical preparation of root canals: Shaping goals, techniques and means. Endod. Top. 2005, 10, 30–76. [Google Scholar] [CrossRef]
- Goldberg, M. Centering Ability and Influence of Experience When Using Wave One Single-File Technique in Simulated Canals. Int. J. Dent. 2012, 2012, 1–7. [Google Scholar] [CrossRef] [PubMed]
- Yufei, L.; Ning, Q.; Ming, X.; Chuyu, W.; Xiaoqing, Y. Comparison of Shaping Ability of Five Nickel-Titanium Rotary Instruments in Simulated Curved Canals. J. Dent. Oral Health 2017, 3, 1–5. [Google Scholar]
- Jasim, A.A.; Al-Gharrawi, H.A.S. Evaluation of the Canal Transportation and Centering Ratio at Different Levels of Simulated Curved Canals Prepared by OneShape, Protaper Next, Protaper Gold and TwoShape Nickel Titanium Rotary Files. Int. J. Med. Res. Health Sci. 2019, 8, 91–97. [Google Scholar]
- Al-Omari, M.A.; Dummer, P.M.; Newcombe, R.G. Comparison of six files to prepare simulated root canals. Int. Endod. J. 1992, 25, 57–66. [Google Scholar] [CrossRef]
- Lopes, H.P.; Gambarra-Soares, T.; Elias, C.N.; Siqueira, J.F., Jr.; Inojosa, I.F.; Lopes, W.S. Comparison of the mechanical properties of rotary instruments made of conventional nickel-titanium wire, M-wire, or nickel-titanium alloy in R-phase. J. Endod. 2013, 39, 516–520. [Google Scholar] [CrossRef]
- Elnaghy, A.M.; Elsaka, S.E. Evaluation of root canal transportation, centering ratio, and remaining dentin thickness associated with ProTaper Next instruments with and without glide path. J. Endod. 2014, 40, 2053–2056. [Google Scholar] [CrossRef]
- Al-Dhbaan, A.A.; Al-Omari, M.A.; Mathew, S.T.; Baseer, M.A. Shaping ability of ProTaper Gold and WaveOne Gold nickel-titanium rotary file in different canal configurations. Saudi Endod. J. 2018, 8, 202–207. [Google Scholar]
- Elnaghy, A.M.; Elsaka, S.E. Mechanical properties of ProTaper Gold nickel-titanium rotary files. Int. Endod. J. 2016, 49, 1073–1078. [Google Scholar] [CrossRef]
- Özyürek, T. Cyclic fatigue resistance of Reciproc, WaveOne, and WaveOne Gold nickel-titanium instruments. J. Endod. 2016, 42, 1536–1539. [Google Scholar] [CrossRef]
- Elnaghy, A.M.; Elsaka, S.E. Effect of sodium hypochlorite and saline on cyclic fatigue resistance of WaveOne Gold and Reciproc reciprocating instruments. Int. Endod. J. 2017, 50, 991–998. [Google Scholar] [CrossRef] [PubMed]
- Zupanc, J.; Vahdat-Pajouh, N.; Schäfer, E. New thermomechanically treated NiTi alloys—A review. Int. Endod. J. 2018, 51, 1088–1103. [Google Scholar] [CrossRef] [Green Version]
- Gündogar, M.; Özyürek, T. Cyclic fatigue resistance of OneShape, HyFlex EDM, WaveOne gold, and Reciproc blue nickel-titanium instruments. J. Endod. 2017, 43, 1192–1196. [Google Scholar] [CrossRef]
- De-Deus, G.; Silva, E.J.N.L.; Vieira, V.T.L.; Belladonna, F.G.; Elias, C.N.; Plotino, G.; Grande, N.M. Blue thermomechanical treatment optimizes fatigue resistance and flexibility of the Reciproc files. J. Endod. 2017, 43, 462–466. [Google Scholar] [CrossRef] [PubMed]
- Keskin, C.; Inan, U.; Demiral, M.; Keles, A. Cyclic fatigue resistance of Reciproc blue, Reciproc, and WaveOne gold reciprocating instruments. J. Endod. 2017, 43, 1360–1363. [Google Scholar] [CrossRef] [PubMed]
- Oh, S.; Kum, K.Y.; Kim, H.J.; Moon, S.Y.; Kim, H.C.; Chaniotis, A.; Perinpanayagam, H.; Pedullá, E.; Chang, S.W. Bending resistance and cyclic fatigue resistance of WaveOne Gold, Reciproc Blue, and HyFlex EDM instruments. J. Dent. Sci. 2020, 15, 472–478. [Google Scholar] [CrossRef] [PubMed]
- Bürklein, S.; Flüch, S.; Schäfer, E. Shaping ability of reciprocating single-file systems in severly curved canals: WaveOne and Reciproc versus WaveOne Gold and Reciproc Blue. Odontology 2019, 107, 96–102. [Google Scholar] [CrossRef] [PubMed]
- Ausiello, P.; Ciaramella, S.; Garcia-Godoy, F.; Martorelli, M.; Sorrentino, R.; Gloria, A. Stress distribution of bulk-fill resin composite in class II restorations. Am. J. Dent. 2017, 30, 227–232. [Google Scholar]
- Prati, C.; Tribst, J.P.M.; Dal Piva, A.M.d.O.; Borges, A.L.S.; Ventre, M.; Zamparini, F.; Ausiello, P. 3D Finite Element Analysis of Rotary Instruments in Root Canal Dentine with Different Elastic Moduli. Appl. Sci. 2021, 11, 2547. [Google Scholar] [CrossRef]
- Pertot, W.J.; Camps, J.; Damiani, M.G. Transportation of curved canals prepared with canal master U, canal master U NiTi, and stainless steel K-type files. Oral Surg. Oral Med. Oral Pathol. 1995, 79, 504–509. [Google Scholar] [CrossRef]
- Ajuz, N.C.; Armada, L.; Goncalves, L.S.; Debelian, G.; Siqueira, J.F., Jr. Glide path preparation in S-shaped canals with rotary pathfinding nickel-titanium instruments. J. Endod. 2013, 39, 534–537. [Google Scholar] [CrossRef] [PubMed]
- Silva, E.J.; Tameirao, M.D.; Belladonna, F.G.; Neves, A.A.; Souza, E.M.; De-Deus, G. Quantitative transportation assessment in simulated curved canals prepared with an adaptive movement system. J. Endod. 2015, 41, 1125–1129. [Google Scholar] [CrossRef] [PubMed]
- Orel, L.; Velea-Barta, O.-A.; Nica, L.-M.; Boscornea-Pușcu, A.-S.; Horhat, R.M.; Talpos-Niculescu, R.-M.; Sinescu, C.; Duma, V.-F.; Vulcanescu, D.-D.; Topala, F.; et al. Evaluation of the Shaping Ability of Three Thermally Treated Nickel–Titanium Endodontic Instruments on Standardized 3D-printed Dental Replicas Using Cone-Beam Computed Tomography. Medicina 2021, 57, 901. [Google Scholar] [CrossRef] [PubMed]
- Drukteinis, S.; Peciuliene, V.; Bendinskaite, R.; Brukiene, V.; Maneliene, R.; Rutkunas, V. Shaping and Centering Ability, Cyclic Fatigue Resistance and Fractographic Analysis of Three Thermally Treated NiTi Endodontic Instrument Systems. Materials 2020, 13, 5823. [Google Scholar] [CrossRef] [PubMed]
- Shen, Y.; Cheung, G. Methods and models to study nickel–titanium instruments. Endod. Top. 2013, 29, 18–41. [Google Scholar] [CrossRef]
- Tasdemir, T.; Aydemir, H.; Inan, U.; Unal, O. Canal preparation with Hero 642 rotary Ni-Ti instruments compared with stainless steel hand K-file assessed using computed tomography. Int. Endod. J. 2005, 38, 402–408. [Google Scholar] [CrossRef] [PubMed]
- Schäfer, E.; Tepel, J.; Hoppe, W. Properties of endodontic hand instruments used in rotary motion. Part2. Instrumentation of curved canals. J. Endod. 1995, 21, 493–497. [Google Scholar] [CrossRef]
- Ahmad, M. The validity of using simulated root canals as models for ultrasonic instrumentation. J. Endod. 1989, 15, 544–547. [Google Scholar] [CrossRef]
- Uzun, O.; Topuz, O.; Yalpi, F.; Unsal, F.; Aydin, C.; Bodrumlu, E. The evaluation of two rotary instrumentation techniques under “operator-related variables” standardized conditions. Eur. J. Dent. 2013, 7, 395–398. [Google Scholar] [CrossRef] [Green Version]
- Cangül, K.; Murat, D.; Evren, S. Comparison of the shaping ability of novel thermally treated reciprocating instruments. Restor. Dent. Endod. 2018, 43, 1–7. [Google Scholar]
- Hieawy, A.; Haapasalo, M.; Zhou, H.; Wang, Z.J.; Shen, Y. Phase transformation behavior and resistance to bending and cyclic fatigue of ProTaper Gold and ProTaper Universal instruments. J. Endod. 2015, 41, 1134–1138. [Google Scholar] [CrossRef] [PubMed]
- Reciproc® Blue. User Guide. Available online: https://www.vdw-dental.com/fileadmin/Dokumente/Sortiment/Aufbereitung/Reziproke-Aufbereitung/RECIPROC-blue/VDW-Dental-Reciprocblue-brochure-EN.pdf (accessed on 3 March 2018).
- Özyürek, T.; Gündoğar, M.; Uslu, G.; Yılmaz, K.; Staffoli, S.; Nm, G.; Plotino, G.; Polimeni, A. Cyclic fatigue resistances of Hyflex EDM, WaveOne Gold, Reciproc Blue and 2shape NiTi rotary files in different artificial canals. Odontology 2018, 106, 408–413. [Google Scholar] [CrossRef] [PubMed]
- Ebihara, A.; Yahata, Y.; Miyara, K.; Nakano, K.; Hayashi, Y.; Suda, H. Heat treatment of nickel-titanium rotary endodontic instruments: Effects on bending properties and shaping abilities. Int. Endod. J. 2011, 44, 843–849. [Google Scholar] [CrossRef] [PubMed]
- Miyai, K.; Ebihara, A.; Hayashi, Y.; Doi, H.; Suda, H.; Yoneyama, T. Influence of phase transformation on the torsional and bending properties of nickel-titanium rotary endodontic instruments. Int. Endod. J. 2006, 39, 119–126. [Google Scholar] [CrossRef] [PubMed]
- Gao, Y.; Gutmann, J.L.; Wilkinson, K.; Maxwell, R.; Ammon, D. Evaluation of the Impact of Raw Materials on the Fatigue and Mechanical Properties of ProFile Vortex Rotary Instruments. J. Endod. 2012, 38, 398–401. [Google Scholar] [CrossRef] [PubMed]
- de Arruda Santos, L.; López, J.B.; de Las Casas, E.B.; de Azevedo Bahia, M.G.; Buono, V.T.L. Mechanical behavior of three nickel-titanium rotary files: A comparison of numerical simulation with bending and torsion tests. Mater. Sci. Eng. C. 2014, 37, 258–263. [Google Scholar] [CrossRef]
- Tavanafar, S.; Gilani, P.V.; Saleh, A.M.; Schäfer, E. Shaping Ability of ProTaper Universal, ProTaper NEXT and WaveOne Primary in Severely Curved Resin Blocks. J. Contemp. Dent. Pract. 2019, 20, 363–369. [Google Scholar] [CrossRef]
- Schäfer, E.; Vlassis, M. Comparative investigation of two rotary nickel-titanium instruments: ProTaper versus RaCe. Part 2. Cleaning effectiveness and shaping ability in severely curved root canals of extracted teeth. Int. Endod. J. 2004, 37, 239–248. [Google Scholar] [CrossRef]
- Saleh, A.M.; Vakili Gilani, P.; Tavanafar, S.; Schäfer, E. Shaping ability of 4 different single-file systems in simulated S-shaped canals. J. Endod. 2015, 41, 548–552. [Google Scholar] [CrossRef]
- Maia Filho, M.; de Castro Rizzi, C.; Bandeca Coelho, M.; Freitas Santos, S.; Oliviera Costa, L.M.; Carvalho, C.N.; de Jesus Tavarez, R.R.; Alves Soares, J. Shaping ability of Reciproc, UnicOne, and ProTaper Universal in simulated root canals. Sci. World J. 2015, 2015, 690854. [Google Scholar] [CrossRef] [Green Version]
- Tambe, V.H.; Nagmode, P.S.; Abraham, S.; Patait, M.; Lahoti, P.V.; Jaju, N. Comparison of canal transportation and centering ability of rotary Protaper, One Shape system and WaveOne system using cone beam computed tomography: An in vitro study. J. Conserv. Dent. 2014, 17, 561–565. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Dhingra, A.; Ruhal, N.; Miglani, A. Evaluation of single file systems Reciproc, OneShape, and WaveOne using Cone Beam Computed Tomography–an in vitro study. J. Clin. Diagn. Res. 2015, 9, ZC 30-4. [Google Scholar] [CrossRef] [PubMed]
- Saber, S.; Nagy, M.; Schäfer, E. Comparative evaluation of the shaping ability of Wave- One, Reciproc and OneShape single-file systems in severely curved root canals of extracted teeth. Int. Endod. J. 2015, 48, 109–111. [Google Scholar] [CrossRef] [PubMed]
- Wu, H.; Peng, C.; Bai, Y.; Hu, X.; Wang, L.; Li, C. Shaping ability of Protaper Universal, WaveOne and ProTaper Next in simulated L-shaped and S-shaped root canals. BMC Oral Health 2015, 15, 27. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Nabavizadeh, M.; Abbaszadegan, A.; Khojastepour, L.; Amirhosseini, M.; Kiani, E. A comparison of apical transportation in severely curved canals induced by Reciproc and BioRaCe systems. Iran Endod. J. 2014, 9, 117–122. [Google Scholar]
- Gergi, R.; Osta, N.; Bourbouze, G.; Zgheib, C.; Arbab-Chirani, R.; Naaman, A. Effects of three nickel titanium instrument systems on root canal geometry assessed by micro-computed tomography. Int. Endod. J. 2015, 48, 162–170. [Google Scholar] [CrossRef]
- Prabhakar, A.R.; Yavagal, C.; Dixit, K.; Naik, S.V. Reciprocating vs rotary instrumentation in pediatric endodontics: Cone beam computed tomographic analysis of deciduous root canals using two single-file systems. Int. J. Clin. Pediatr. Dent. 2016, 9, 45–49. [Google Scholar] [CrossRef]
- Bane, K.; Faye, B.; Sarr, M.; Niang, S.O.; Ndiaye, D.; Machtou, P. Root canal shaping by single-file systems and rotary instruments: A laboratory study. Iran Endod. J. 2015, 10, 135–139. [Google Scholar]
- Jain, A.; Chauhan, S.; Bahuguna, R.; Sharma, R.; Sharma, M.; Chabra, C. Comparative Evaluation of Root Canal Surface after Mechanical Instrumentation with Protaper Gold and Wave One Gold. Int. J. Oral Health Med. Res. 2019, 6, 25–27. [Google Scholar]
- Boscornea-Pușcu, A.-S.; Orel, L.; Velea-Barta, O.-A.; Horhat, R.M.; Negruțiu, M.-L.; Nica, L.M.; Duma, V.-F.; Stoia, D.I.; Opriș, C.; Sinescu, C. Experimental Study of the Effects of Torsional Loading on Three Types of Nickel-Titanium Endodontic Instruments. Appl. Sci. 2021, 11, 7224. [Google Scholar] [CrossRef]
- Erdelyi, R.-A.; Duma, V.-F.; Sinescu, C.; Dobre, G.M.; Bradu, A.; Podoleanu, A. Dental Diagnosis and Treatment Assessments: Between X-Rays Radiography and Optical Coherence Tomography. Materials 2020, 13, 4825. [Google Scholar] [CrossRef] [PubMed]

| X1 | 0 | 1 | 2 | 3 | 4 | ||
|---|---|---|---|---|---|---|---|
| PTG | Mean ± SD | 0.055 ± 0.024 | 0.060 ± 0.013 | 0.095 ± 0.012 | 0.128 ± 0.034 | 0.196 ± 0.042 | |
| RB | Mean ± SD | 0.080 ± 0.098 | 0.100 ± 0.116 | 0.124 ± 0.139 | 0.188 ± 0.169 | 0.200 ± 0.138 | |
| WOG | Mean ± SD | 0.061 ± 0.044 | 0.067 ± 0.030 | 0.119 ± 0.048 | 0.193 ± 0.075 | 0.264 ± 0.061 | |
| ANOVA | 0.6051 | 0.3337 | 0.6731 | 0.2789 | 0.1310 | ||
| Tukey post hoc | RB vs. WOG | 0.7260 | 0.4797 | 0.9000 | 0.9000 | 0.2051 | |
| RB vs. PTG | 0.5976 | 0.3502 | 0.6708 | 0.3787 | 0.9000 | ||
| WOG vs. PTG | 0.9000 | 0.9000 | 0.7526 | 0.3213 | 0.1679 | ||
| X2 | |||||||
| PTG | Mean ± SD | 0.073 ± 0.030 | 0.101 ± 0.030 | 0.127 ± 0.023 | 0.153 ± 0.028 | 0.140 ± 0.038 | |
| RB | Mean ± SD | 0.0123 ± 0.094 | 0.136 ± 0.112 | 0.167 ± 0.159 | 0.165 ± 0.161 | 0.178 ± 0.138 | |
| WOG | Mean ± SD | 0.108 ± 0.036 | 0.134 ± 0.032 | 0.147 ± 0.041 | 0.111 ± 0.037 | 0.123 ± 0.097 | |
| ANOVA | 0.1217 | 0.3881 | 0.5963 | 0.3686 | 0.4059 | ||
| Tukey post hoc | RB vs. WOG | 0.8009 | 0.9000 | 0.8557 | 0.3680 | 0.3895 | |
| RB vs. PTG | 0.1134 | 0.4420 | 0.5637 | 0.9465 | 0.6316 | ||
| WOG vs. PTG | 0.3262 | 0.4758 | 0.8557 | 0.5490 | 0.9122 | ||
| (X1 − X2)/Y | |||||||
| PTG | Mean ± SD | −0.053 ± 0.062 | −0.111 ± 0.080 | −0.074 ± 0.065 | −0.049 ± 0.107 | 0.096 ± 0.127 | |
| RB | Mean ± SD | −0.109 ± 0.423 | −0.103 ± 0.551 | −0.096 ± 0.635 | 0.039 ± 0.586 | 0.039 ± 0.453 | |
| WOG | Mean ± SD | −0.116 ± 0.182 | −0.167 ± 0.124 | −0.064 ± 0.150 | 0.143 ± 0.189 | 0.249 ± 0.180 | |
| ANOVA | 0.8234 | 0.8745 | 0.9781 | 0.4332 | 0.2332 | ||
| Tukey post hoc | RB vs. WOG | 0.9992 | 0.8792 | 0.9750 | 0.7514 | 0.2259 | |
| RB vs. PTG | 0.8595 | 0.9964 | 0.9866 | 0.8337 | 0.8798 | ||
| WOG vs. PTG | 0.8399 | 0.9142 | 0.9981 | 0.4054 | 0.4604 | ||
| X1 | 5 | 6 | 7 | 8 | ||
|---|---|---|---|---|---|---|
| PTG | Mean ± SD | 0.252 ± 0.038 | 0.258 ± 0.028 | 0.248 ± 0.026 | 0.258 ± 0.037 | |
| RB | Mean ± SD | 0.213 ± 0.107 | 0.208 ± 0.077 | 0.183 ± 0.076 | 0.198 ± 0.065 | |
| WOG | Mean ± SD | 0.285 ± 0.064 | 0.288 ± 0.074 | 0.255 ± 0.055 | 0.266 ± 0.046 | |
| ANOVA | 0.0746 | 0.0136 * | 0.0056 * | 0.0042 * | ||
| Tukey post hoc | RB vs. WOG | 0.0602 | 0.0107 * | 0.0092 * | 0.0064 * | |
| RB vs. PTG | 0.4180 | 0.1412 | 0.0190 * | 0.0178 * | ||
| WOG vs. PTG | 0.5271 | 0.4922 | 0.9000 | 0.9000 | ||
| X2 | ||||||
| PTG | Mean ± SD | 0.123 ± 0.039 | 0.131 ± 0.029 | 0.179 ± 0.040 | 0.203 ± 0.042 | |
| RB | Mean ± SD | 0.183 ± 0.112 | 0.231 ± 0.087 | 0.265 ± 0.093 | 0.287 ± 0.068 | |
| WOG | Mean ± SD | 0.100 ± 0.055 | 0.138 ± 0053 | 0.185 ± 0.050 | 0.230 ± 0.040 | |
| ANOVA | 0.0313 * | 0.0004 * | 0.0066 * | 0.0013 * | ||
| Tukey post hoc | RB vs. WOG | 0.0020 * | 0.0020 * | 0.0137 * | 0.0292 * | |
| RB vs. PTG | 0.0009 * | 0.0009 * | 0.0078 * | 0.0011 * | ||
| WOG vs. PTG | 0.9615 | 0.9615 | 0.9739 | 0.4243 | ||
| (X1 − X2)/Y | ||||||
| PTG | Mean ± SD | 0.215 ± 0.119 | 0.201 ± 0.086 | 0.103 ± 0.094 | 0.075 ± 0.101 | |
| RB | Mean ± SD | 0.050 ± 0.350 | −0.032 ± 0.249 | −0.115 ± 0.235 | −0.117 ± 0.170 | |
| WOG | Mean ± SD | 0.303 ± 0.179 | 0.228 ± 0.175 | 0.100 ± 0.134 | 0.041 ± 0.107 | |
| ANOVA | 0.0409 * | 0.0023 * | 0.0032 * | 0.0021 * | ||
| Tukey post hoc | RB vs. WOG | 0.0331 * | 0.0039 * | 0.0082 * | 0.0134 * | |
| RB vs. PTG | 0.2124 | 0.0097 * | 0.0076 * | 0.0027 * | ||
| WOG vs. PTG | 0.6354 | 0.9358 | 0.9994 | 0.8142 | ||
| X1 | 9 | 10 | 11 | 12 | ||
|---|---|---|---|---|---|---|
| PTG | Mean ± SD | 0.254 ± 0.041 | 0.259 ± 0.036 | 0.248 ± 0.050 | 0.161 ± 0.074 | |
| RB | Mean ± SD | 0.216 ± 0.055 | 0.221 ± 0.067 | 0.220 ± 0.051 | 0.072 ± 0.056 | |
| WOG | Mean ± SD | 0.164 ± 0.043 | 0.291 ± 0.037 | 0.249 ± 0.084 | 0.164 ± 0.060 | |
| ANOVA | 0.0523 | 0.0050 * | 0.4506 | 0.0014 * | ||
| Tukey post hoc | RB vs. WOG | 0.0620 | 0.0035 * | 0.5080 | 0.0034 * | |
| RB vs. PTG | 0.1264 | 0.1454 | 0.5263 | 0.0047 * | ||
| WOG vs. PTG | 0.9000 | 0.2615 | 0.9000 | 0.9000 | ||
| X2 | ||||||
| PTG | Mean ± SD | 0.236 ± 0.024 | 0.252 ± 0.030 | 0.260 ± 0.052 | 0.158 ± 0.061 | |
| RB | Mean ± SD | 0.305 ± 0.072 | 0.296 ± 0.061 | 0.290 ± 0.060 | 0.116 ± 0.064 | |
| WOG | Mean ± SD | 0.261 ± 0.045 | 0.287 ± 0.037 | 0.271 ± 0.044 | 0.151 ± 0.054 | |
| ANOVA | 0.0077 * | 0.0505 | 0.3736 | 0.1991 | ||
| Tukey post hoc | RB vs. WOG | 0.1006 | 0.8703 | 0.6450 | 0.3327 | |
| RB vs. PTG | 0.0060 * | 0.0534 | 0.3493 | 0.2151 | ||
| WOG vs. PTG | 0.4605 | 0.1487 | 0.8680 | 0.9594 | ||
| (X1 − X2)/Y | ||||||
| PTG | Mean ± SD | 0.022 ± 0.064 | 0.009 ± 0.051 | −0.027 ± 0.081 | 0.005 ± 0.080 | |
| RB | Mean ± SD | −0.111 ± 0.152 | −0.089 ± 0.139 | −0.079 ± 0.114 | −0.045 ± 0.097 | |
| WOG | Mean ± SD | −0.009 ± 0.099 | −0.004 ± 0.076 | −0.029 ± 0.077 | 0.008 ± 0.047 | |
| ANOVA | 0.0162 * | 0.0366 * | 0.3131 | 0.1790 | ||
| Tukey post hoc | RB vs. WOG | 0.0752 | 0.0852 | 0.4130 | 0.2269 | |
| RB vs. PTG | 0.0177 * | 0.0459 * | 0.3729 | 0.2573 | ||
| WOG vs. PTG | 0.8031 | 0.9555 | 0.9969 | 0.9968 | ||
| PTG | RB | WOG | ANOVA | Tukey Post-Hoc | ||||
|---|---|---|---|---|---|---|---|---|
| Apical third | RB vs. WOG | RB vs. PTG | WOG vs. PTG | |||||
| X1 | 0.107 | 0.139 | 0.141 | 0.3803 | 0.9959 | 0.4753 | 0.4256 | |
| X2 | 0.119 | 0.154 | 0.125 | 0.3841 | 0.5306 | 0.3974 | 0.9712 | |
| (X1 − X2)/Y | −0.038 | −0.046 | 0.007 | 0.8600 | 0.8664 | 0.9971 | 0.8995 | |
| Middle third | ||||||||
| X1 | 0.254 | 0.200 | 0.274 | 0.0126 | 0.0118 * | 0.0792 | 0.6931 | |
| X2 | 0.159 | 0.241 | 0.163 | 0.0028 | 0.0089 * | 0.0058 * | 0.9844 | |
| (X1 − X2)/Y | 0.148 | −0.054 | 0.168 | 0.0057 | 0.0095 * | 0.0192 * | 0.9566 | |
| Coronal third | ||||||||
| X1 | 0.2306 | 0.1821 | 0.2413 | 0.0034 | 0.0043 * | 0.0206 * | 0.8113 | |
| X2 | 0.2263 | 0.2517 | 0.2423 | 0.2935 | 0.8379 | 0.2726 | 0.5808 | |
| (X1 − X2)/Y | 0.0021 | −0.0809 | −0.0084 | 0.0272 | 0.0730 | 0.0353 * | 0.9420 | |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Orel, L.; Velea-Barta, O.-A.; Sinescu, C.; Duma, V.-F.; Nica, L.-M.; Horhat, R.M.; Chirila, R.D.; Tudor, A.; Vulcănescu, D.-D.; Negrutiu, M.L. Comparative Assessment of the Shaping Ability of Reciproc Blue, WaveOne Gold, and ProTaper Gold in Simulated Root Canals. Materials 2022, 15, 3028. https://doi.org/10.3390/ma15093028
Orel L, Velea-Barta O-A, Sinescu C, Duma V-F, Nica L-M, Horhat RM, Chirila RD, Tudor A, Vulcănescu D-D, Negrutiu ML. Comparative Assessment of the Shaping Ability of Reciproc Blue, WaveOne Gold, and ProTaper Gold in Simulated Root Canals. Materials. 2022; 15(9):3028. https://doi.org/10.3390/ma15093028
Chicago/Turabian StyleOrel, Laura, Oana-Alexandra Velea-Barta, Cosmin Sinescu, Virgil-Florin Duma, Luminița-Maria Nica, Razvan Mihai Horhat, Raul Dorin Chirila, Anca Tudor, Dan-Dumitru Vulcănescu, and Meda Lavinia Negrutiu. 2022. "Comparative Assessment of the Shaping Ability of Reciproc Blue, WaveOne Gold, and ProTaper Gold in Simulated Root Canals" Materials 15, no. 9: 3028. https://doi.org/10.3390/ma15093028
APA StyleOrel, L., Velea-Barta, O.-A., Sinescu, C., Duma, V.-F., Nica, L.-M., Horhat, R. M., Chirila, R. D., Tudor, A., Vulcănescu, D.-D., & Negrutiu, M. L. (2022). Comparative Assessment of the Shaping Ability of Reciproc Blue, WaveOne Gold, and ProTaper Gold in Simulated Root Canals. Materials, 15(9), 3028. https://doi.org/10.3390/ma15093028











