The Use of Laser Energy for Etching Enamel Surfaces in Dentistry—A Scoping Review
Abstract
1. Introduction
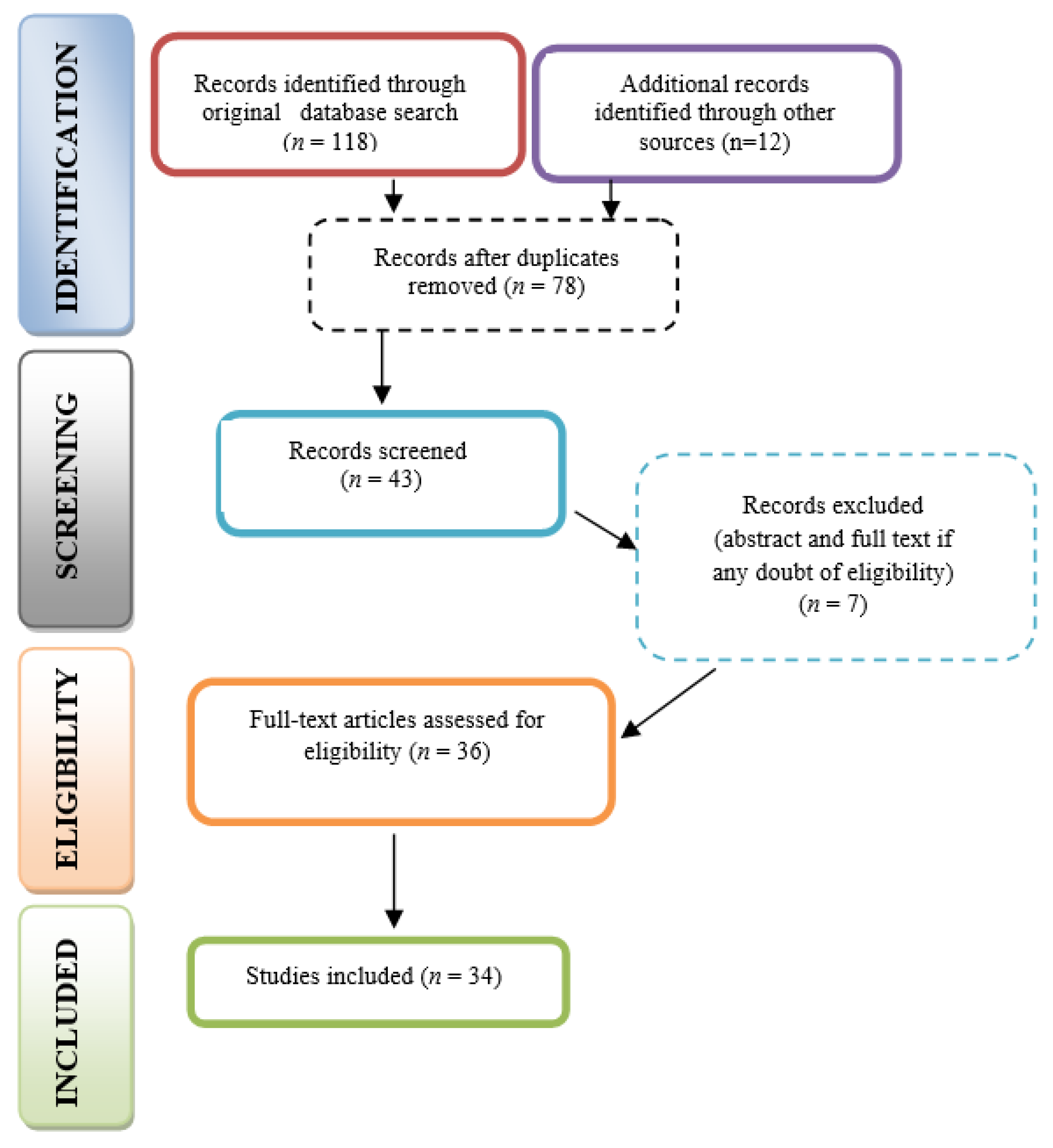
2. Materials and Methods
2.1. Search Strategy
2.2. Selection of Articles
2.3. Data Collection
3. Results
4. Discussion
4.1. Er:YAG Lasers
4.2. Er,Cr:YSGG Laser
4.3. Other Lasers
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Romanos, G.E. Laser Fundamental Principles. In Advanced Laser Surgery in Dentistry; Wiley Blackell: Hoboken, NJ, USA, 2021; pp. 3–11. [Google Scholar]
- Goldman, L.; Goldman, B.; Van Lieu, N. Current laser dentistry. Lasers Surg. Med. 1987, 6, 559–562. [Google Scholar] [CrossRef]
- Miserendino, L.J.; Pick, R.M. Current Applications of Lasers in Dentistry. In Lasers in Dentistry; Quintessence Publishing Co., Inc.: Singapore, 1995; pp. 126–128. [Google Scholar]
- Verma, S.K.; Maheshwari, S.; Singh, R.K.; Chaudhari, P.K. Laser in dentistry: An innovative tool in modern dental practice. Natl. J. Maxillofac. Surg. 2012, 3, 124–132. [Google Scholar] [CrossRef] [PubMed]
- Harashima, T.; Kinoshita, J.; Kimura, Y.; Brugnera, A.; Zanin, F.; Pecora, J.D.; Matsumoto, K. Morphological comparative study on ablation of dental hard tissues at cavity preparation by Er:YAG and Er,Cr:YSGG lasers. Photomed. Laser Surg. 2005, 23, 52–55. [Google Scholar] [CrossRef] [PubMed]
- Ishikawa, I.; Aoki, A.; Takasaki, A.A. Clinical application of erbium: YAG Laser in periodontology. J. Int. Acad. Periodontol. 2008, 10, 22–30. [Google Scholar] [PubMed]
- Hilgers, J.J.; Tracey, S.G. Clinical uses of Diode lasers in orthodontics. J. Clin. Orthod. 2004, 38, 266–273. [Google Scholar] [PubMed]
- Carroll, L.; Humphreys, T.R. LASER-tissue interactions. Clin. Dermatol. 2006, 24, 2–7. [Google Scholar] [CrossRef] [PubMed]
- Sulieman, M. An overview of the use of lasers in general dental practice: 2. Laser wavelengths, soft and hard tissue clinical applications. Dent. Update 2005, 32, 286–288, 291–294, 296. [Google Scholar] [CrossRef] [PubMed]
- Lopes, G.C.; Thys, D.G.; Klaus, P.; Oliveira, G.M.; Widmer, N. Enamel acid etching: A review. Compendium 2007, 28, 662–669. [Google Scholar]
- Kabas, A.S.; Ersoy, T.; Gülsoy, M.; Akturk, S. Femtosecond laser etching of dental enamel for bracket bonding. J. Biomed. Opt. 2013, 18, 098003. [Google Scholar] [CrossRef] [PubMed]
- Myers, T.D. Effects of a pulsed Nd:YAG laser on enamel and dentin. In Proceedings of the SPIE, Los Angeles, CA, USA, 14–19 January 1990; Volume 1200, pp. 425–436. [Google Scholar] [CrossRef]
- Dostálová, T.; Jelínková, H.; Kucerová, H.; Krejsa, O.; Hamal, K.; Kubelka, J.; Procházka, S. Noncontact Er:YAG laser ablation: Clinical evaluation. J. Clin. Laser Med. Surg. 1998, 16, 273–282. [Google Scholar] [CrossRef] [PubMed]
- Obata, A.; Tsumura, T.; Niwa, K.; Ashizawa, Y.; Deguchi, T.; Ito, M. Super pulse CO2 laser for bracket bonding and debonding. Eur. J. Orthod. 1999, 21, 193–198. [Google Scholar] [CrossRef] [PubMed]
- Resaei-Soufi, L.; Ghanadan, K.; Moghimbeigi, A. The effects of Er:YAG, Nd:YAG, and Diode (940 nm) lasers irradiation on microtensile bond strength of two steps self-etch adhesives. Laser Ther. 2019, 28, 131–137. [Google Scholar] [CrossRef] [PubMed]
- Drummond, J.L.; Wigdor, H.A.; Walsh, J.T., Jr.; Fadavi, S.; Punwani, I. Sealant bond strengths of CO2 laser-etched versus acid-etched bovine enamel. Lasers Surg. Med. 2000, 27, 111–118. [Google Scholar] [CrossRef]
- Martínez-Insua, A.; da Silva Dominguez, L.; Rivera, F.G.; Santana-Penín, U.A. Differences in bonding to acid-etched or Er:YAG-laser-treated enamel and dentin surfaces. J. Prosthet. Dent. 2000, 84, 280–288. [Google Scholar] [CrossRef] [PubMed]
- Otsuki, M.; Eguro, T.; Maeda, T.; Tanaka, H. Comparison of the bond strength of composite resin to Er:YAG laser irradiated human enamel pre-treated with various methods in vitro. Lasers Surg. Med. 2002, 30, 351–359. [Google Scholar] [CrossRef] [PubMed]
- Tricco, A.C.; Lillie, E.; Zarin, W.; O’Brien, K.K.; Colquhoun, H.; Levac, D.; Moher, D.; Peters, M.D.; Horsley, T.; Weeks, L.; et al. PRISMA Extension for scoping reviews (PRISMA- ScR): Checklist and explanation. Ann. Intern. Med. 2018, 169, 467–473. [Google Scholar] [CrossRef]
- Arksey, H.; O’Malley, L. Scoping studies: Towards a methodological framework. Int. J. Soc. Res. Methodol. 2005, 8, 19–32. [Google Scholar] [CrossRef]
- The Joanna Briggs Institute. Joanna Briggs Institute Reviewers’ Manual: 2014 Edition; The Joanna Briggs Institute, The University of Adelaide: Adelaide, Australia, 2014. [Google Scholar]
- Groth, E.B.; Mercer, C.E.; Anderson, P. Microtomographic analysis of subsurface enamel and dentine following Er:YAG laser and acid etching. Eur. J. Prosthodont. Restor. Dent. 2001, 9, 73–79. [Google Scholar]
- De Munck, J.; Van Meerbeek, B.; Yudhira, R.; Lambrechts, P.; Vanherle, P. Micro-tensile bond strength of two adhesives to Erbium:YAG-lased vs. bur-cut enamel and dentin. Eur. J. Oral. Sci. 2002, 110, 322–329. [Google Scholar] [CrossRef] [PubMed]
- Dibb, R.G.; Corona, S.A.; Borsatto, M.C.; Ferreira, K.C.; Ramos, R.P.; Pécora, J.D. Assessing microleakage on class V composite resin restorations after Er:YAG laser preparation varying the adhesive systems. J. Clin. Laser Med. Surg. 2002, 20, 129–133. [Google Scholar] [CrossRef] [PubMed]
- Armengol, V.; Laboux, O.; Weiss, P.; Jean, A.; Hamel, H. Effects of Er:YAG and Nd:YAP laser irradiation on the surface roughness and free surface energy of enamel and dentin: An in vitro study. Oper. Dent. 2003, 28, 67–74. [Google Scholar] [PubMed]
- Manhart, J.; Huth, K.C.; Chen, H.Y.; Hickel, R. Influence of the pretreatment of occlusal pits and fissures on the retention of a fissure sealant. Am. J. Dent. 2004, 17, 12–18. [Google Scholar]
- Delme, K.; Deman, P.J.; De Moor, R.J.G. Microleakage of class V resin composite restorations after conventional and Er:YAG laser preparation. J. Oral Rehabil. 2005, 32, 676–685. [Google Scholar] [CrossRef] [PubMed]
- Hosseini, M.H.; Namvar, F.; Chalipa, J.; Saber, K.; Chiniforush, N.; Sarmadi, S.; Mirhashemi, A.H. Comparison of Shear Bond Strength of Orthodontic Brackets Bonded to Enamel Prepared By Er:YAG Laser and Conventional Acid-Etching. J. Dent. 2012, 9, 20–26. [Google Scholar]
- Yung, F.Y.W.; Gutknecht, N.; Franzen, R.; Fischer, H. Shear strength of composite bonded to Er:YAG laser-prepared enamel: An in vitro comparative study. Lasers Med. Sci. 2013, 28, 879–889. [Google Scholar] [CrossRef]
- Zavareh, F.A.; Samimi, P.; Birang, P.; Eskini, M.; Bouraima, S.A. Assessment of Microleakage of Class V Composite Resin Restoration Following Erbium-Doped Yttrium Aluminum Garnet (Er:YAG) Laser Conditioning and Acid Etching with Two Different Bonding Systems. J. Lasers Med. Sci. 2013, 4, 39–47. [Google Scholar]
- Arami, S.; Shahabi, S.; Tabatabaie, M.; Chiniforush, N.; Morshedi, E.; Torabi, S. Assessing microleakage of composite restorations in class V cavities prepared by Er:YAG laser irradiation or diamond bur. J. Conserv. Dent. 2014, 17, 216–219. [Google Scholar]
- Ciucchi, P.; Neuhaus, K.W.; Emerich, M.; Peutzfeldt, A.; Lussi, A. Evaluation of different types of enamel conditioning before application of a fissure sealant. Lasers Med. Sci. 2015, 30, 1–9. [Google Scholar] [CrossRef]
- Çokakoğlu, S.; Nalçacı, R.; Üşümez, S.; Malkoç, S. Effects of different combinations of Er:YAG laser-adhesives on enamel demineralization and bracket bond strength. Photomed. Laser Surg. 2016, 34, 164–170. [Google Scholar] [CrossRef] [PubMed]
- Durmus, B.; Giray, F.; Peker, S.; Kargul, B. Clinical evaluation of a fissure sealant placed by acid etching or Er:YAG laser combined with acid etching. Oral Health Prev. Dent. 2017, 15, 157–162. [Google Scholar]
- Luong, E.; Shayegan, A. Assessment of microleakage of class V restored by resin composite and resin-modified glass ionomer and pit and fissure resin-based sealants following Er:YAG laser conditioning and acid etching: In vitro study. Clin. Cosmet. Investig. Dent. 2018, 30, 83–92. [Google Scholar] [CrossRef]
- Onay, E.O.; Yamanel, K.; Korkmaz-Ceyhan, Y.; Gulsahi, K. Comparison of three adhesive systems in class II composite restorations in endodontically treated teeth: Influence of Er:YAG laser conditioning and gingival margin levels on microleakage. J. Clin. Exp. Dent. 2018, 1, e781–e788. [Google Scholar] [CrossRef]
- Kaviani, A.; Nejad, N.K. Effect of Nd:YAG and Er:YAG laser tooth conditioning on the microleakage of self-adhesive resin cement. Biomater. Investig. Dent. 2021, 20, 152–159. [Google Scholar] [CrossRef] [PubMed]
- Hossain, M.; Nakamura, Y.; Yamada, Y.; Suzuki, N.; Murakami, Y.; Matsumoto, K. Analysis of surface roughness of enamel and dentin after Er,Cr:YSGG laser irradiation. J. Clin. Laser Med. Surg. 2001, 19, 297–303. [Google Scholar] [CrossRef] [PubMed]
- Berk, N.; Başaran, G.; Ozer, T. Comparison of sandblasting, laser irradiation, and conventional acid etching for orthodontic bonding of molar tubes. Eur. J. Orthod. 2008, 30, 183–189. [Google Scholar] [CrossRef]
- Botta, S.B.; da Ana, P.A.; Zezell, D.M.; Powers, J.M.; Matos, A.B. Adhesion after erbium, chromium:yttrium-scandium-gallium-garnet laser application at three different irradiation conditions. Lasers Med. Sci. 2009, 24, 67–73. [Google Scholar] [CrossRef] [PubMed]
- Türkmen, C.; Sazak-Oveçoğlu, H.; Günday, M.; Güngör, G.; Durkan, M.; Oksüz, M. Shear bond strength of composite bonded with three adhesives to Er,Cr:YSGG laser-prepared enamel. Quintessence Int. 2010, 41, e119–e124. [Google Scholar] [PubMed]
- Karaman, E.; Yazici, A.R.; Baseren, M.; Gorucu, J. Comparison of acid versus laser etching on the clinical performance of a fissure sealant: 24-month results. Oper. Dent. 2013, 38, 151–158. [Google Scholar] [CrossRef] [PubMed]
- Ustunkol, I.; Yazici, A.R.; Gorucu, J.; Dayangac, B. Influence of laser etching on enamel and dentin bond strength of Silorane System Adhesive. Lasers Med. Sci. 2015, 30, 695–700. [Google Scholar] [CrossRef]
- Kumar, G.; Dhillon, J.K.; Rehman, F. A comparative evaluation of retention of pit and fissure sealants placed with conventional acid etching and Er,Cr:YSGG laser etching: A randomised controlled trial. Laser Ther. 2016, 30, 291–298. [Google Scholar] [CrossRef] [PubMed]
- Dilip, S.; Srinivas, S.; Noufal, M.N.; Ravi, K.; Krishnaraj, R.; Charles, A. Comparison of surface roughness of enamel and shear bond strength, between conventional acid etching and erbium, chromium-doped: Yttrium scandium-gallium-garnet laser etching—An in vitro study. Dent. Res. J. 2018, 15, 248–255. [Google Scholar]
- Shafiei, F.; Sardarian, A.; Fekrazad, R.; Farjood, A. Comparison of shear bond strength of orthodontic brackets bonded with a universal adhesive using different etching methods. Dent. Press J. Orthod. 2019, 5, 33.e1–33.e8. [Google Scholar] [CrossRef]
- Şimşek, H.; Rüya Yazıcı, A.; Cem Güngör, H. In Vitro Evaluation of Different Protocols for Preventing Microleakage of Fissure Sealants Placed Following Saliva Contamination. J. Clin. Pediatr. Dent. 2020, 1, 240–248. [Google Scholar] [CrossRef] [PubMed]
- Al Habdan, A.H.; Al Rabiah, R.; Al Busayes, R. Shear bond strength of acid and laser conditioned enamel and dentine to composite resin restorations: An in vitro study. Clin. Exp. Dent. Res. 2021, 7, 331–337. [Google Scholar] [CrossRef] [PubMed]
- Fuhrmann, R.; Gutknecht, N.; Magunski, A.; Lampert, F.; Diedrich, P. Conditioning of enamel with Nd:YAG and CO2 dental laser systems and with phosphoric acid. An in-vitro comparison of the tensile bond strength and the morphology of the enamel surface. J. Orofac. Orthop. 2001, 62, 375–386. [Google Scholar] [CrossRef] [PubMed]
- Goswami, M.; Singh, A. Comparative evaluation of shear bond strength of composite resin bonded to acid etched or Nd:Yag lased enamel. J. Indian Soc. Pedod. Prev. Dent. 2011, 29, 140–143. [Google Scholar] [CrossRef]
- Oshagh, M.; Pakshir, H.R.; Najafi, H.Z.; Naseri, M.M.; Nasrabadi, N.I.; Torkan, S. Comparison of the shear bond strength of orthodontic brackets in bonding and rebonding: Preparation with laser versus conventional acid etch technique. Photomed. Laser Surg. 2013, 31, 360–364. [Google Scholar] [CrossRef]
- Suhaimi, F.M.; Alam, N.Z.; Ariffin, S.M.; Razak, N.A.; Razab, M.K. Surface modifications of human tooth using Nd:YAG laser for dental applications. In Proceedings of the 39th Annual International Conference of the IEEE Engineering in Medicine and Biology Society (EMBC), Seogwipo-si, Korea, 11–15 July 2017; Volume 2017, pp. 4537–4540. [Google Scholar]
- Bhandari, D.P.; Anbuselvan, G.J.; Karthi, M. Evaluation of resin penetration depth in enamel surface for orthodontic bonding exposed to five types of enamel conditioning methods: A scanning electron microscopic study. J. Pharm. Bioallied Sci. 2019, 11 (Suppl. S2), S221–S227. [Google Scholar] [CrossRef] [PubMed]
- Nelson, D.G.; Wefel, J.S.; Jongebloed, W.L.; Featherstone, J.D. Morphology, histology and crystallography of human dental enamel treated with pulsed low-energy infrared laser radiation. Caries Res. 1987, 21, 411–426. [Google Scholar] [CrossRef]
- Uysal, T.; Ustdal, A.; Kurt, G. Evaluation of shear bond strength of metallic and ceramic brackets bonded to enamel prepared with self-etching primer. Eur. J. Orthod. 2010, 32, 214–218. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Yassaei, S.; Fekrazad, R.; Shahraki, N.; Goldani Moghadam, M. A Comparison of Shear Bond Strengths of Metal and Ceramic Brackets using Conventional Acid Etching Technique and Er:YAG Laser Etching. J. Dent. Res. Dent. Clin. Dent. Prospects 2014, 8, 27–34. [Google Scholar] [CrossRef]
- Silverstone, L.M.; Saxton, C.A.; Dogon, I.L.; Fejerskov, O. Variation in the pattern of acid etching of human dental enamel examined by scanning electron microscopy. Caries Res. 1975, 9, 373–387. [Google Scholar] [CrossRef] [PubMed]
- Visuri, S.R.; Gilbert, J.L.; Wright, D.D.; Wigdor, H.A.; Walsh, J.T., Jr. Shear strength of composite bonded to Er:YAG laser-prepared dentin. J. Dent. Res. 1996, 75, 599–605. [Google Scholar] [CrossRef] [PubMed]
- Lee, B.S.; Hsieh, T.T.; Lee, Y.L.; Lan, W.H.; Hsu, Y.J.; Wen, P.H.; Lin, C.P. Bond strengths of orthodontic bracket after acid-etched, Er:YAG laser-irradiated and combined treatment on enamel surface. Angle Orthod. 2003, 73, 565–570. [Google Scholar] [PubMed]
| Criterion | Inclusion | Exclusion |
|---|---|---|
| Time period | Publications available between January 2000 and December 2021 | All publications published before January 2000 |
| Language | English | Non-English |
| Type of articles | All research types including primary research (e.g., experimental studies performed on human teeth, clinical trials, pilot studies), secondary research, reviews, related to the use of laser on etching of enamel layer; Publications for which full-text is available | Studies performed on bovine teeth and temporary human teeth; Studies investigating the adhesion specifically on dentin layer; Research only focusing on laser preparation of cavities |
| No. | Year of Publishing | Laser Type | Methods | Results |
|---|---|---|---|---|
| 1 | [22]/2001 | Er:YAG | X-ray microtomography | Laser and acid conditioning increased etching depth; laser-only etched enamel subsurface revealed small reduction in mineral concentration and increase in porosity, allowing greater penetration of acid |
| 2 | [23]/2002 | Er:YAG | Total-etching adhesive OptiBond FL +/− acid etching/self-etching adhesive Clearfil SE Bond +/− laser etching | Laser etching—less effective than acid-etching |
| 3 | [24]/2002 | Er:YAG | Cavities conditioned with short pulsed Er:YAG laser (500 mJ/5 Hz) + for additional 30 s using lower dosimetries (120 mJ/4 Hz): acid etch + Bond-1/acid etching+Prime & Bond NT/self-etching Etch & Prime 3.0 | Prime & Bond NT completely sealed both margins; Etch & Prime 3.0 had the poorest overall results, with a statistically significant difference |
| 4 | [25]/2003 | Er:YAG, Nd:YAP | 37% phosphoric acid/Er:YAG laser/Nd:YAP laser | Morphological changes on hard dental tissues—higher with acid-etch and Er:YAG laser than Nd:YAG laser. Free surface energy—sgn greater with acid-etch or Er:YAG laser |
| 5 | [26]/2004 | Er:YAG | 37% H3PO4, diamond bur/37% H3PO4, Er:YAG laser/Er:YAG laser and 37% H3PO4/air abrasion/air abrasion + acid etching with 37% H3PO4 + compomer fissure sealant | Conventional acid etching—significatly higher sealant retention than Er:YAG laser etching or air abrasion. Mechanical conditioning of the laser or air abrasion + acid-etching results statistically equal to the acid-etch only group |
| 6 | [27]/2005 | Er:YAG | Er:YAG laser and acid etching/Er:YAG laser, laser etching and acid etching/Er:YAG laser and only laser etching/high-speed bur and acid etching | Acid-etch is favored when using resin composite in Er:YAG-lased Class V cavities; the contact seaL at enamel margins in Er:YAG-lased and laser-etched cavities depended on the resin composite composition and on the adhesive |
| 7 | [28]/2012 | Er:YAG | 37% phosphoric acid, Er:YAG laser at 1 W/1.5 W | Mean SBS obtained with Er:YAG laser at 1 W or 1.5 W is similar to conventional etching |
| 8 | [29]/2013 | Er:YAG | Total etching—3 steps and 2 steps, self-etching—2 steps and 1 step | Additional laser etching after phosphoric acid etch–beneficial to generation 5, total etching in 2 steps. No significant change or detrimental effect to the other types in SBS |
| 9 | [30]/2013 | Er:YAG | Er:YAG laser + Optibond FL,/Er:YAG laser + 35% phosphoric acid + Optibond FL/Er:YAG laser + Clearfil SE Bond/a35% phosphoric acid + OptibondFL/Clearfil SE Bond | Er:YAG laser for conditioning followed by different dentin adhesive systems had an influence on the marginal sealing of composite resin restorations |
| 10 | [31]/2014 | Er:YAG | Diamond bur + acid etch/cavity conditioning by Er:YAG laser + acid etch/Er:YAG laser + laser etching/diamond bur + laser etching/Er:YAG laser with no conditioning procedure | No significant difference in evaluating microleakage degree of cavities prepared by Er:YAG laser and diamond bur |
| 11 | [32]/2015 | Er:YAG | Er:YAG/air abrasion/self-etching adhesive with phosphoric acid or laser/acid etching | Conventional acid etching sgn lower microleakage, higher unfilled area proportions than the Er:YAG laser + self-etch adhesive group |
| 12 | [33]/2016 | Er:YAG | Acid + Transbond XT/Er:YAG (100 mJ or 200 mJ 10 Hz) etching + Transbond XT/Transbond Plus self-etching primer/Er:YAG (100 mJ or 200 mJ, 10 Hz) etching + Transbond Plus SEP/Clearfil Protect Bond/Er:YAG (100 mJ or 200 mJ, 10 Hz) etching + Clearfil Protect Bond | Lowest SBS values were in 1 step self etch; the highest were in laser+ self-etch. When two-step self-etch adhesive is used for bonding brackets, laser etching at 1 W (100 mJ, 10 Hz) seems to improve SBS |
| 13 | [34]/2017 | Er:YAG | Phosphoric acid etching/Er:YAG laser + acid etching, fissure sealant | Er:YAG laser + acid etching sgn improves fissure sealant retention over conventional acid etching alone |
| 14 | [35]/2018 | Er:YAG | 37% phosphoric acid, Er:YAG laser and phosphoric acid etching, and combination with Er:YAG laser | Er:YAG laser and the resin composite; the resin-modified glass ionomers and fissure sealant may provide a variant of hard dental tissue etching to acid etching |
| 15 | [36]/2018 | Er:YAG | 37% phosphoric acid/Adper Single Bond 2; Er:YAG laser/37% phosphoric acid/Adper Single Bond 2; Clearfil SE Bond; Er:YAG laser/Clearfil SE Bond; Adper Easy One; Er:YAG laser/Adper Easy One | Er:YAG laser conditioning may show some advantage prior to Adper Single Bond 2 application in enamel |
| 16 | [15]/2019 | Nd:YAG, Er:YAG, Diode | Two-step self-etching adhesives/lasers before or after primer or bonding | Nd:YAG laser after applying the primer, Diode laser after bonding agent, may sgn improve the microtensile bond strength in two-step self-etch adhesive systems |
| 17 | [37]/2021 | Nd:YAG, Er:YAG | No conditioning/Er:YAG laser (2940 nm, 10 Hz, 1.2 W)/Nd:YAG laser (1064 nm, 1.5 W, 10 Hz) + self-etching adhesive | Er:YAG laser (2940 nm, 10 Hz, 1.2 W) on cavity surface shows lower marginal microleakage of self-etch adhesive resin cement restorations compared to Nd:YAG (1064 nm, 1.5 W, 10 Hz) and no conditioning groups |
| Year of Publishing | Laser Type | Methods | Results | |
|---|---|---|---|---|
| 1 | [38]/2001 | Er,Cr:YSGG | Er,Cr:YSGG, 37% phosphoric acid | Surface roughness was sgn higher with the laser system. Scanning electron microscopy showed that the irradiated surface produced a rough surface that was entirely lacking a smear layer, with no cracking of enamel or dentin |
| 2 | [39]/2008 | Er, Cr:YSGG | Er, Cr:YSGG 0.5, 0.75, 1, 1.5, and 2 W, phosphoric acid | A more important layer of adhesive was left on the enamel surface with low-power laser irradiation. Sandblasting and low-power laser irradiation (0.5, 0.75, and 1 W) seem to not etch enamel in a way that is acceptable for orthodontic molar tube bonding, but 1.5- and 2-W laser irradiation was shown to be an alternative to conventional acid etching |
| 3 | [40]/2009 | Er,Cr:YSGG | Er,Cr:YSGG 0.25 W, 20 Hz, 2.8 J/cm2 energy per pulse of 12.5 mJ, water delivery rate 11 mL/min | Laser conditioning significantly lowered the bond strength of several adhesive systems applied on enamel |
| 4 | [41]/2010 | Er,Cr:YSGG | Er,Cr:YSGG laser/37% phosphoric acid + primer adhesive; self-etched primer + adhesive; all-in-one adhesive—single dose | Er,Cr:YSGG laser > 37% phosphoric acid. SBS of laser etched + primer/adhesive group sgn higher than 37% phosphoric acid + primer/adhesive |
| 5 | [42]/2013 | Er,Cr:YSGG | Phosphoric acid etching/laser etching—clinical | The clinical performance of fissure sealants placed after acid or Er,Cr:YSGG laser etching was similar |
| 6 | [43]/2015 | Er, Cr:YSGG | Laser etch/phosphoric acid etched laser + silorane adhesive system | Phosphoric acid best for SBS with Silorane System Adhesive. Non etched = laser etched |
| 7 | [44]/2016 | Er,Cr:YSGG | 37% phosphoric acid/Er,Cr:YSGG laser 2.78 µm, 1.5 W | Overall retention rate in acid etched—slightly higher compared to laser etched; difference statistically non-significant |
| 8 | [45]/2018 | Er,Cr:YSGG | Etching with 37% phosphoric acid for 15 s, irradiation with Er, Cr:YSGG laser at 1 watt for 10 s and 20 s, and irradiation with Er,Cr:YSGG laser at 1.5 watts for 10 s and 20 s. Metal brackets were bonded with Transbond XT | 1.5 W/20 s Er,Cr:YSGG laser produced comparable bond strength to acid etching; no sgn diff between laser and acid etch |
| 9 | [46]/2019 | Er,Cr:YSGG | Er,Cr:YSGG laser, phosphoric acid + Scotchbond Universal/Transond XT | Highest SBS—Scotchbond Universal with laser etching; Transbond XT with acid or laser etching, and Scotchbond in self-etch mode—lowest bond strength |
| 10 | [47]/2020 | Er,Cr:YSGG | Er,Cr:YSSG/phosphoric acid etching/acid etching + etch-and-rinse adhesive/self-etching adhesive—in vitro. contaminating enamel surfaces with artificial saliva + fissure sealant/contamination and repeated conditioning + fissure sealant | Re-application of Er,Cr:YSSG laser and self-etching adhesive did not have an effect on microleakage of fissure sealants. Without re-application, acid-etching + etch-and-rinse adhesive—only superior to acid-etching |
| 11 | [48]/2021 | Er,Cr:YSGG | Er,Cr:YSGG, 37% phosphoric acid | The shear bond strength of composite resin bonded to hard dental tissues etched with phosphoric acid was more important than results obtained when conditioned with Er,Cr:YSGG laser |
| Year of Publishing | Laser Type | Methods | Results | |
|---|---|---|---|---|
| 1 | [49]/2001 | CO2 and Nd:YAG | CO2 laser/Nd:YAG laser/phosphoric acid etching | CO2 laser—demineralization gaps of various dimensions, Nd:YAG laser—honeycomb structures similar to acid-etch technique. CO2 and Nd:YAG lasers—sufficient modification of enamel for bracket bonding |
| 2 | [50]/2011 | Nd:YAG | 35% phosphoric acid/Nd:YAG laser 0.8 W, 10 Hz, for 10 s with 80 mJ/pulse power + bonding + composite | Under SEM, acid showed typical honeycomb appearance, and laser—bubble-like cavities. In enamel, acid etching technique showed higher SBS |
| 3 | [51]/2013 | CO2 | CO2 laser, phosphoric acid | Initial preparation with acid has a higher SBS value than CO2 laser, with higher secondary bonding. Less adhesive residue present on enamel after tooth preparation with laser following debonding |
| 4 | [52]/2017 | Nd:YAG | Nd:YAG laser and 37% phosphoric acid | Comparison of the compositions demonstrated that calcium has higher percentage when exposed to laser-etching compared to acid-etching. Nd:YAG laser can be implemented for etching procedure as a replacement of the conventional technique |
| 5 | [53]/2019 | CO2 | CO2 laser/37% phosphoric acid/polyacrylic acid/self-etching/air abrasion | The teeth etched with 37% phosphoric acid exhibited significantly greater depth of resin penetration (15.1 µm) than self-etching and polyacrylic acid. Laser etching showed similar depth with acid etching. Air abrasion shows lowest depth of all groups |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Labunet, A.; Tonea, A.; Kui, A.; Sava, S. The Use of Laser Energy for Etching Enamel Surfaces in Dentistry—A Scoping Review. Materials 2022, 15, 1988. https://doi.org/10.3390/ma15061988
Labunet A, Tonea A, Kui A, Sava S. The Use of Laser Energy for Etching Enamel Surfaces in Dentistry—A Scoping Review. Materials. 2022; 15(6):1988. https://doi.org/10.3390/ma15061988
Chicago/Turabian StyleLabunet, Anca, Andrada Tonea, Andreea Kui, and Sorina Sava. 2022. "The Use of Laser Energy for Etching Enamel Surfaces in Dentistry—A Scoping Review" Materials 15, no. 6: 1988. https://doi.org/10.3390/ma15061988
APA StyleLabunet, A., Tonea, A., Kui, A., & Sava, S. (2022). The Use of Laser Energy for Etching Enamel Surfaces in Dentistry—A Scoping Review. Materials, 15(6), 1988. https://doi.org/10.3390/ma15061988








