Prosthetic Materials Used for Implant-Supported Restorations and Their Biochemical Oral Interactions: A Narrative Review
Abstract
:1. Introduction
2. Interim Prosthetic Materials Used for Obtaining Implant-Supported Prosthesis
2.1. The Role of Interim Prosthesis in Oral Implant Therapy
2.2. Materials and Techniques Used for Fabrication of Oral Interim Implant-Supported Prosthesis
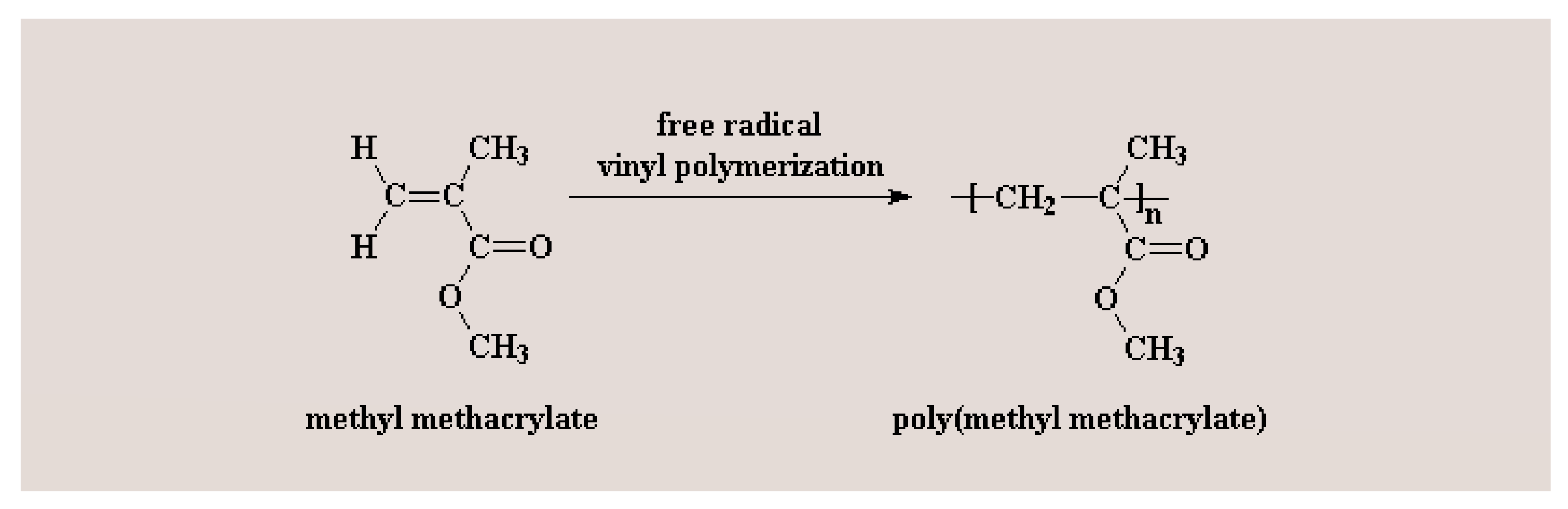
2.3. PMMA (Poly (methyl methacrylate))—An Acknowledged Material Used for Obtaining Oral Interim Implant-Supported Prosthesis with Its Performance Still Being under Evaluation
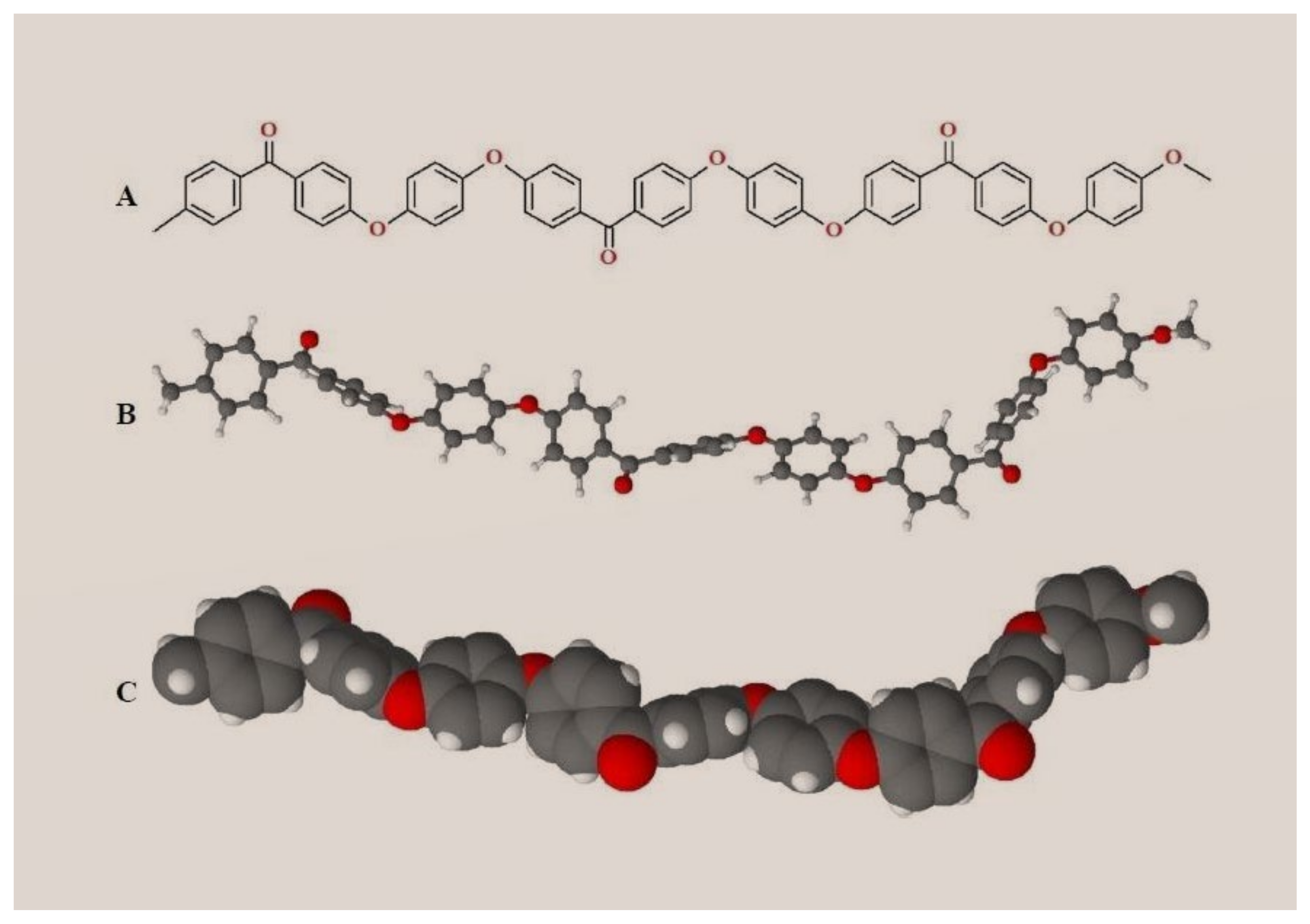
2.4. PEEK (Polyether Ether Ketone)—A High Performance Polymer for Interim & Definitive Use in Prosthodontics
3. Definitive Prosthetic Materials Used for Obtaining Oral Implant-Supported Prostheses
3.1. Materials and Techniques Used for Fabrication of Definitive Implant-Supported Prostheses
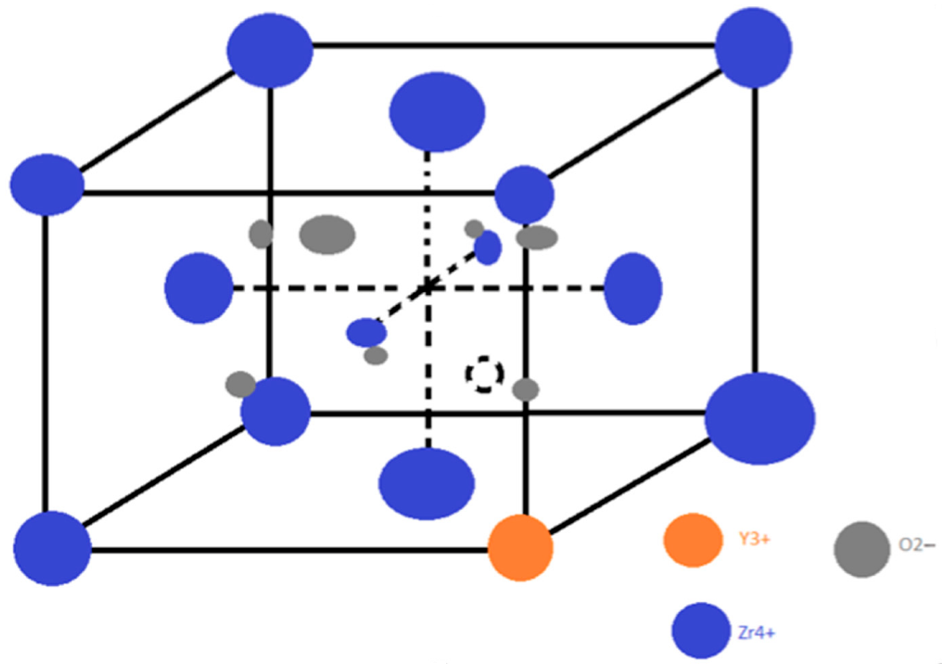
3.2. Zirconia—A Successful Definitive Implant-Supported Prostheses Material
4. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Papaspyridakos, P.; Mokti, M.; Chen, C.J.; Benic, G.I.; Gallucci, G.O.; Chronopoulos, V. Implant and prosthodontic survival rates with implant fixed complete dental prostheses in the edentulous mandible after at least 5 years: A systematic review. Clin. Implant Dent. Relat. Res. 2014, 16, 705–717. [Google Scholar] [CrossRef] [PubMed]
- Moraschini, V.; Poubel, L.A.; Ferreira, V.F.; dos Barboza, E.S.P. Evaluation of survival and success rates of dental implants reported in longitudinal studies with a follow-up period of at least 10 years: A systematic review. Int. J. Oral Maxillofac. Surg. 2015, 44, 377–388. [Google Scholar] [CrossRef] [PubMed]
- Bornstein, M.M.; Halbritter, S.; Harnisch, H.; Weber, H.P.; Buser, D. A retrospective analysis of patients referred for implant placement to a speciality clinic: Indications, surgical procedures and early failures. Int. J. Oral Maxillofac. Implant. 2008, 23, 1109–1116. [Google Scholar]
- Brägger, U.; Aeschlimann, S.; Bürgin, W.; Hämmerle, C.H.; Lang, N.P. Biological and technical complications and failures with fixed partial dentures (FPD) on implants and teeth after four to five years of function. Clin. Oral Implant. Res. 2001, 12, 26–34. [Google Scholar] [CrossRef] [PubMed]
- Pjetursson, B.E.; Brägger, U.; Lang, N.P.; Zwahlen, M. Comparison of survival and complication rates of tooth-supported fixed dental prostheses (FDPs) and implant-supported FDPs and single crowns (SCs). Clin. Oral Implant. Res. 2007, 18 (Suppl. 3), 97–113. [Google Scholar] [CrossRef]
- Wittneben, J.G.; Buser, D.; Salvi, G.E.; Bürgin, W.; Hicklin, S.; Brägger, U. Complication and failure rates with implant-supported fixed dental prostheses and singlecrowns: A 10-year retrospective study. Clin. Implant Dent. Relat. Res. 2014, 16, 356–364. [Google Scholar] [CrossRef]
- Gallucci, G.O.; Avrampou, M.; Taylo, J.C.; Elpers, J.; Thalji, G.; Cooper, L.F. Maxillary Implant-Supported Fixed Prosthesis: A Survey of Reviews and Key Variables for Treatment Planning. Int. J. Oral Maxillofac. Implant. 2016, 31, 192–207. [Google Scholar] [CrossRef]
- Peñarrocha Oltra, D.; Penñarrocha, D.M.; Canullo, L.; Covani, U.; Penñarrocha, M. Patient-reported outcomes of immediate versus conventional loading with fixed full-arch prostheses in the maxilla: A nonrandomized controlled prospective study. Int. J. Oral Maxillofac. Implant. 2014, 29, 690–698. [Google Scholar] [CrossRef] [Green Version]
- Williams, D. Essential Biomaterials Science. In Cambridge Texts in Biomedical Engineering; Cambridge University Press: Cambridge, UK, 2014; pp. 130–132. [Google Scholar]
- Alt, V.; Hannig, M.; Wöstmann, B.; Balkenhol, M. Fracture strength of temporary fixed partial dentures: CAD/CAM versus directly fabricated restorations. Dent. Mater. 2011, 27, 339–347. [Google Scholar] [CrossRef]
- Cheng, C.W.; Chien, C.H.; Chen, C.J.; Papaspyridakos, P. Clinical Results and Technical Complications of Posterior Implant-Supported Modified Monolithic Zirconia Single Crowns and Short-Span Fixed Dental Prostheses: A 2-Year Pilot Study. J. Prosthodont. 2018, 27, 108–114. [Google Scholar] [CrossRef]
- Monje, A.; Amerio, E.; Farina, R.; Nart, J.; Ramanauskaite, A.; Renvert, S.; Wang, H.L. Significance of probing for monitoring peri-implant diseases. Int. J. Oral Implantol. 2021, 14, 385–399. [Google Scholar]
- Santosa, R.E. Provisional restorations options in implant dentistry. Aust. Dent. J. 2007, 52, 234–242. [Google Scholar] [CrossRef] [PubMed]
- Degidi, M.; Nardi, D.; Gianluca, S.; Piattelli, A. The conometric concept: A 5-year follow-up of fixed partial monolithic zirconia restorations supported by cone-in-cone abutments. Int. J. Periodontics Restor. Dent. 2018, 38, 363–371. [Google Scholar] [CrossRef] [PubMed]
- Pituru, S.M.; Greabu, M.; Totan, A.; Imre, M.; Pantea, M.; Spinu, T.; Tancu, A.M.C.; Popoviciu, N.O.; Stanescu, I.-I.; Ionescu, E. A Review on the biocompatibility of PMMA-based dental materials for interim prosthetic restorations with a glimpse into their modern manufacturing techniques. Materials 2020, 13, 2894. [Google Scholar] [CrossRef]
- Abdullah, A.O.; Tsitrou, E.A.; Pollington, S. Comparative in vitro evaluation of CAD/CAM v/s conventional provisional crowns. J. Appl. Oral Sci. 2006, 24, 258–263. [Google Scholar] [CrossRef] [Green Version]
- Skorulska, A.; Piszko, P.; Rybak, Z.; Szymonowicz, M.; Dobrzyński, M. Review on Polymer, Ceramic and Composite Materials for CAD/CAM Indirect Restorations in Dentistry—Application, Mechanical Characteristics and Comparison. Materials 2021, 14, 1592. [Google Scholar] [CrossRef]
- Rayyan, M.M.; Aboushelib, M.; Sayed, N.M.; Ibrahim, A.; Jimbo, R. Comparison of interim restorations fabricated by CAD/CAM with those fabricated manually. J. Prosthet. Dent. 2015, 114, 414–419. [Google Scholar] [CrossRef]
- Lodding, D.W. Long-term esthetic provisional restorations in dentistry. Curr. Opin. Cosmet. Dent. 1997, 4, 16–21. [Google Scholar]
- Trushkowsky, R.D. Fabrication of a fixed provisional restoration utilizing a light-curing acrylic resin. Quintessence Int. 1992, 23, 415–419. [Google Scholar]
- Proussaefs, P. Immediate provisionalization with a CAD/CAM interim abutment and crown: A guided soft tissue healing technique. J. Prosthet. Dent. 2015, 113, 91–95. [Google Scholar] [CrossRef]
- Bakke, M.; Michler, L.; Han, K.; Moller, E. Clinical significance of isometric bite force versus electrical activity in temporal and masseter muscles. Scand. J. Dent. Res. 1989, 97, 539–551. [Google Scholar] [CrossRef] [PubMed]
- Najeeb, S.; Zafar, M.S.; Khurshid, Z.; Siddiqui, F. Application of pol-yetheretherketone (PEEK) in oral implantology and prosthodontic. J. Prosthodont. Res. 2016, 60, 12–19. [Google Scholar] [CrossRef] [PubMed]
- Bathala, L.; Majeti, V.; Rachuri, N.; Singh, N.; Gedela, S. The Role of Polyether Ether Ketone in Dentistry—A Review. J. Med. Life 2016, 12, 5–9. [Google Scholar] [CrossRef] [PubMed]
- Alexakou, E.; Damanaki, M.; Zoidis, P.; Bakiri, E.; Mouzis, N.; Smidt, G.; Kourtis, S. PEEK High Performance Polymers: A Review of Properties and Clinical Applications in Prosthodontics and Restorative Dentistry. Eur. J. Prosthodont. Restor. Dent. 2019, 27, 113–121. [Google Scholar] [PubMed]
- Gad, M.M.; Fouda, S.M.; Al-Harbi, F.A.; Näpänkangas, R.; Raustia, A. PMMA denture base material enhancement: A review of fiber, filler, and nanofiller addition. Int. J. Nanomed. 2017, 12, 3801–3812. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Wegehaupt, F.J.; Lunghi, N.; Belibasakis, G.N.; Attin, T. Influence of light-curing distance on degree of conversion and cytotoxicity of etch-and-rinse and self-etch adhesives. BMC Oral Health 2016, 17, 1–10. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Cebe, M.A.; Cebe, F.; Cengiz, M.; Cetin, A.R.; Arpag, O.F.; Ozturk, B. Elution of monomer from different bulk fill dental composite resins. Dent. Mater. 2015, 31, 141–149. [Google Scholar] [CrossRef]
- Michelsen, V.B.; Kopperud, H.B.M.; Lygre, G.B.; Björkman, L.; Jensen, E.; Kleven, I.S.; Svahn, J.; Lygre, H. Detectional quantification of monomers in unstimulated whole saliva after treatment with resin-based composite fillings in vivo. Eur. J. Oral Sci. 2012, 120, 89–95. [Google Scholar] [CrossRef] [PubMed]
- Jiao, Y.; Ma, S.; Li, J.; Shan, L.; Yang, Y.; Li, M.; Chen, J. The influences of N-acetyl cysteine (NAC) on the cytotoxicity and mechanical properties of poly-methylmethacrylate (PMMA)-baseddental resin. PeerJ 2015, 3, e868. [Google Scholar] [CrossRef]
- Singh, R.D.; Gautam, R.; Siddhartha, R.; Singh, B.P.; Chand, P.; Sharma, V.P.; Jurel, S.K. High-performance liquid chromatographic determination of residual monomer released from heat-cured acrylic resin: An in vivo study. J. Prosthodont. 2013, 22, 358–361. [Google Scholar] [CrossRef]
- Fujisawa, S.; Atsumi, T. Cytotoxicities of a 4-META/MMA-TBBO resin against human pulp fibroblasts. Dent. Mater. J. 2011, 23, 106–108. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Shimada, Y.; Seki, Y.; Uzzaman, M.A.; Sattabanasuk, V.; Sasafuchi, Y.; Foxton, R.M.; Otsuki, M.; Tagami, J. Monkey pulpal response to an MMA-based resin cement as adhesive luting for indirect restorations. J. Adhes. Dent. 2005, 7, 247–251. [Google Scholar] [PubMed]
- Inoue, T.; Miyakoshi, S.; Shimono, M. The in vitro and in vivo influence of 4-META/MMATBB resin components on dental pulp tissues. Adv. Dent. Res. 2001, 15, 101–104. [Google Scholar] [CrossRef] [PubMed]
- Noda, M.; Wataha, J.; Kaga, M.; Lockwood, P.; Volkmann, K.; Sano, H. Components of dentinal adhesives modulate heat shock protein 72 expression in heat-stressed THP-1 human monocytes at sublethal concentrations. J. Dent. Res. 2002, 81, 265–269. [Google Scholar] [CrossRef]
- Galler, K.; Schweikl, H.; Hiller, K.A.; Cavender, A.; Bolay, C.; D’Souza, R.; Schmalz, G. TEGDMA reduces the expression of genes involved in biomineralization. J. Dent. Res. 2011, 90, 257–262. [Google Scholar] [CrossRef] [Green Version]
- About, I. Dentin regeneration in vitro: The pivotal role of supportive cells. Adv. Dent. Res. 2011, 23, 320–324. [Google Scholar] [CrossRef]
- Bakopoulou, A.; Leyhausen, G.; Volk, J.; Tsiftsoglou, A.; Garefis, P.; Koidis, P.; Geurtsen, W. Effects of HEMA and TEDGMA on the in vitro odontogenic differentiation potential of human pulp stem/progenitor cells derived from deciduous teeth. Dent. Mater. 2011, 27, 608–617. [Google Scholar] [CrossRef]
- About, I.; Camps, J.; Mitsiadis, T.A.; Bottero, M.J.; Butler, W.; Franquin, J.C. Influence of resinous monomers on the differentiation in vitro of human pulp cells into odontoblasts. Biomed. Mater. Res. 2002, 63, 418–423. [Google Scholar] [CrossRef]
- Goodman, S.B.; Schatzker, J.; Sumner-Smith, G.; Fornasier, V.L.; Goften, N.; Hunt, C. The effect of polymethylmethacrylate on bone: An experimental study. Arch. Orthop. Trauma Surg. 1985, 104, 150–154. [Google Scholar] [CrossRef]
- Leggat, P.A.; Kedjarune, U. Toxicity of methyl methacrylate in dentistry. Int. Dent. J. 2003, 53, 126–131. [Google Scholar] [CrossRef]
- Gautam, R.; Singh, R.D.; Sharma, V.P.; Siddhartha, R.; Chand, P.; Kumar, R. Biocompatibility of polymethylmethacrylate resins used in dentistry. J. Biomed. Mater. Res. Part B Appl. Biomater. 2012, 100, 1444–1450. [Google Scholar] [CrossRef] [PubMed]
- Mittermüller, P.; Hiller, K.A.; Schmalz, G.; Buchalla, W. Five hundred patients reporting on adverse effects from dental materials: Frequencies, complaints, symptoms, allergies. Dent. Mater. 2018, 34, 1756–1768. [Google Scholar] [CrossRef] [PubMed]
- Granchi, D.; Stea, S.; Ciapetti, G.; Savarino, L.; Cavedagna, D.; Pizzoferrato, A. In vitro effects of bone cements on the cell cycle of osteoblastlike cells. Biomaterials 1995, 16, 1187–1192. [Google Scholar] [CrossRef]
- Ciapetti, G.; Granchi, D.; Savarino, L.; Cenni, E.; Magrini, E.; Baldini, N.; Giunti, A. In vitro testing of the potential for orthopedic bone cements to cause apoptosis of osteoblast-like cells. Biomaterials 2002, 23, 617–627. [Google Scholar] [CrossRef]
- Schweikl, H.; Spagnuolo, G.; Schmalz, G. Genetic and cellular toxicology of dental resin monomers. J. Dent. Res. 2006, 85, 870–877. [Google Scholar] [CrossRef]
- Ratanasathien, S.; Wataha, J.C.; Hanks, C.T.; Dennison, J.B. Cytotoxic interactive effects of dentin bonding components on mouse fibroblasts. J. Dent. Res. 1995, 74, 1602–1606. [Google Scholar] [CrossRef]
- Krifka, S.; Spagnuolo, G.; Schmalz, G.; Schweikl, H. A review of adaptive mechanisms in cell responses towards oxidative stress caused by dental resin monomers. Biomaterials 2013, 34, 4555–4563. [Google Scholar] [CrossRef]
- Jiao, Y.; Wang, Y.; Guo, S.; Wang, G. Glutathione peroxidases as oncotargets. Oncotarget 2017, 8, 80093–80102. [Google Scholar] [CrossRef] [Green Version]
- Ryter, S.W.; Kim, H.P.; Hoetzel, A.; Park, J.W.; Nakahira, K.; Wang, X.; Choi, A.M.K. Mechanisms of cell death in oxidative stress. Antioxid. Redox Signal. 2007, 9, 49–89. [Google Scholar] [CrossRef]
- Jiao, Y.; Ma, S.; Wang, Y.; Li, J.; Shan, L.; Liu, Q.; Liu, Y.; Song, Q.; Yu, F.; Yu, H.; et al. N-Acetyl cysteine depletes reactive oxygen species and prevents dental monomer-induced intrinsic mitochondrial apoptosis in vitro in human dental pulp cells. PLoS ONE 2016, 11, e0147858. [Google Scholar] [CrossRef]
- Jiao, Y.; Niu, L.N.; Ma, S.; Li, J.; Tay, F.R.; Chen, J.H. Quaternary ammonium-based biomedical materials: State-of-theart, toxicological aspects and antimicrobial resistance. Prog. Polym. Sci. 2017, 71, 53–90. [Google Scholar] [CrossRef] [PubMed]
- Gallorini, M.; Petzel, C.; Bolay, C.; Hiller, K.A.; Cataldi, A.; Buchala, W.; Krifka, S.; Schweikl, H. Activation of the Nrf2-regulated antioxidant cell response inhibits HEMA-induced oxidative stress and supports cell viability. Biomaterials 2015, 56, 114–128. [Google Scholar] [CrossRef] [PubMed]
- Jiao, Y.; Niu, T.; Liu, H.; Tay, F.R.; Chen, J. Protection against HEMA-induced mitochondrial injury in vitro by Nrf2 activation. Oxid. Med. Cell. Longev. 2019, 2019, 3501059. [Google Scholar] [CrossRef] [PubMed]
- Zhang, Y.; Xiao, J.; Yang, H.; Jiao, Y.; Cao, W.-W.; Shi, H.-M.; Cun, J.-F.; Tay, F.R.; Ping, J.; Xiao, Y. N-Acetyl Cysteine as a Novel Polymethyl Methacrylate Resin Component: Protection against Cell Apoptosis and Genotoxicity Oxidative. Med. Cell. Longev. 2019, 2019, 1301736. [Google Scholar] [CrossRef] [PubMed]
- Filomeni, G.; De Zio, D.; Cecconi, F. Oxidative stress and autophagy: The clash between damage and metabolic needs. Cell Death Differ. 2015, 22, 377–388. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Marino, G.; Niso-Santano, M.; Baehrecke, E.H.; Kroemer, G. Self-consumption: The interplay of autophagy and apoptosis. Nat. Rev. Mol. Cell Biol. 2014, 15, 81–94. [Google Scholar] [CrossRef] [Green Version]
- Mukhopadhyay, S.; Panda, P.K.; Sinha, N.; Das, D.N.; Bhutia, S.K. Autophagy and apoptosis: Where do they meet? Apoptosis 2014, 19, 555–566. [Google Scholar] [CrossRef]
- Becker, A.L.; Orlotti, N.I.; Folini, M.; Cavalieri, F.; Zelikin, A.N.; Johnston, A.; Zaffaroni, N.; Caruso, F. Redox-active polymer microcapsules for the delivery of a survivin-specific siRNA in prostate cancer cells. ACS Nano 2011, 5, 1335–1344. [Google Scholar] [CrossRef]
- Markovic, Z.M.; Ristic, B.Z.; Arsikin, K.M.; Klisic, D.G.; Harhaji-Trajkovic, L.M.; Todorovic-Markovic, B.M.; Kepic, D.P.; Kravic-Stevovic, T.; Jovanovic, S.P.; Milenkovic, M.M.; et al. Graphene quantum dots as autophagy-inducing photodynamic agents. Biomaterials 2013, 33, 7084–7092. [Google Scholar] [CrossRef]
- Ma, Y.W.; Jin, S.; Tian, Y.; Zhang, X.; Zhao, Y.; Yu, L.; Liang, X.J. Gold nanoparticles induce autophagosome accumulation through size-dependent nanoparticle uptake and lysosome impairment. ACS Nano 2011, 5, 8629–8639. [Google Scholar] [CrossRef]
- Wen, J.W.; Wang, F.; Liu, B.; Huang, C.; Wei, Y. Synthesis and screening of 3-MA derivatives for autophagy inhibitors. Free Radic. Biol. Med. 2013, 65, 402–410. [Google Scholar] [CrossRef] [PubMed]
- Zhang, B.; Wang, D.G.; Guo, F.F.; Xuan, C. Mitochondrial membrane potential and reactive oxygen species in cancer stem cells. Fam. Cancer 2015, 14, 19–23. [Google Scholar] [CrossRef] [PubMed]
- Hale, A.N.; Ledbetter, D.J.; Gawriluk, T.R.; Rucker, E.B. Autophagy: Regulation and role in development. Autophagy 2013, 9, 951–972. [Google Scholar] [CrossRef] [PubMed]
- Boya, P.; Reggiori, F.; Codogno, P. Emerging regulation and functions of autophagy. Nat. Cell Biol. 2013, 15, 713–720. [Google Scholar] [CrossRef] [PubMed]
- Das, B.V.S.; Baehrecke, E.H. Regulation and function of autophagy during cell survival and cell death. Cold Spring Harbor Perspect. Biol. 2012, 4, a008813. [Google Scholar] [CrossRef] [Green Version]
- Wirawan, E.; Vanden, T.; Berghe, S.; Lippens, P.; Agostinis, P.; Vandenabeele, P. Autophagy: For better or for worse. Cell Res. 2012, 22, 43–61. [Google Scholar] [CrossRef]
- Rubinstein, A.D.; Kimchi, A. Life in the balance—A mechanistic view of the crosstalk between autophagy and apoptosis. J. Cell Sci. 2012, 125, 5259–5268. [Google Scholar] [CrossRef] [Green Version]
- Booth, L.; Tavallai, S.; Hamed, H.A.; Cruickshanks, N.; Dent, P. The role of cell signalling in the crosstalk between autophagy and apoptosis. Cell. Signal. 2014, 26, 549–555. [Google Scholar] [CrossRef] [Green Version]
- Pei, Y.; Liu, H.; Yang, Y. Biological activities and potential oral applications of N-acetylcysteine: Progress and prospects. Oxid. Med. Cell. Longev. 2018, 2018, 2835787. [Google Scholar] [CrossRef]
- Yang, Y.; He, X.; Shi, J.; Hickel, R.; Reichl, F.X.; Högg, C. Effects of antioxidants on DNA double-strand breaks in human gingival fibroblasts exposed to dental resin comonomer epoxy metabolites. Dent. Mater. 2017, 33, 418–426. [Google Scholar] [CrossRef]
- Jiao, Y.; Ma, S.; Wang, Y.; Li, J.; Shan, L.; Chen, J. Epigallocatechin-3-gallate reduces cytotoxic effects caused by dental monomers: A hypothesis. Med. Sci. Monit. 2015, 21, 3197–3202. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Rushworth, G.F.; Megson, I.L. Existing and potential therapeutic uses for N-acetylcysteine: The need for conversion to intracellular glutathione for antioxidant benefits. Pharmacol. Ther. 2014, 141, 150–159. [Google Scholar] [CrossRef]
- Yamada, M.; Kojima, N.; Paranjpe, A. N-Acetyl cysteine (NAC)-assisted detoxification of PMMA resin. J. Dent. Res. 2008, 87, 372–377. [Google Scholar] [CrossRef]
- Nishimiya, H.; Yamada, M.; Ueda, T.; Sakurai, K. N-Acetyl cysteine alleviates inflammatory reaction of oral epithelial cells to poly (methyl methacrylate) extract. Acta Odontol. Scand. 2015, 73, 616–625. [Google Scholar] [CrossRef] [PubMed]
- Nocca, G.; D’Antò, V.; Desiderio, C. N-Acetyl cysteine directed detoxification of 2-hydroxyethyl methacrylate by adduct formation. Biomaterials 2010, 31, 2508–2516. [Google Scholar] [CrossRef] [PubMed]
- Spagnuolo, G.; Desiderio, C.; Rivieccio, V. In vitro cellular detoxification of triethylene glycol dimethacrylate by adduct formation with N-acetylcysteine. Dent. Mater. 2013, 29, e153–e160. [Google Scholar] [CrossRef] [PubMed]
- Rosenstiel, S.F.; Land, M.F.; Fujimoto, J. Contemporary Fixed Prosthodontics, 5th ed.; Mosby: St. Louis, MO, USA, 2015; pp. 401–404. [Google Scholar]
- Alqurashi, H.; Khurshid, Z.; Syed, A.U.Y.; Rashid Habib, S.; Rokaya, D.; Zafar, M.S. Polyetherketoneketone (PEKK): An emerging biomaterial for oral implants and dental prostheses. J. Adv. Res. 2021, 28, 87–95. [Google Scholar] [CrossRef]
- Kurtz, S. PEEK Biomaterials Handbook, 2nd ed.; Elsevier Inc.: Amsterdam, The Netherlands, 2019. [Google Scholar]
- De Araújo Nobre, M.; Moura Guedes, C.; Almeida, R.; Silva, A. Poly-ether-ether-ketone and implant dentistry: The future of mimicking natural dentition is now! Polym. Int. 2021, 70, 999–1001. [Google Scholar] [CrossRef]
- Borgonovo, A.E.; Rigaldo, F.; Battaglia, D.; Re, D.; Giannì, A.B. Digital device in postextraction implantology: A clinical case presentation. Case Rep. Dent. 2014, 2014, 327368. [Google Scholar] [CrossRef] [Green Version]
- Aravindakshan, R.; Saju, K.K.; Aruvathottil Rajan, R. Investigation into Effect of Natural Shellac on the Bonding Strength of Magnesium Substituted Hydroxyapatite Coatings Developed on Ti6Al4V Substrates. Coatings 2021, 11, 933. [Google Scholar] [CrossRef]
- Li, S.; Kim, M.-J.; Lee, S.-H.; Jin, L.; Cong, W.; Jeong, H.-G.; Lee, K.-Y. Metallothionein 3 Promotes Osteoblast Differentiation inC2C12 Cells via Reduction of Oxidative Stress. Int. J. Mol. Sci. 2021, 22, 4312. [Google Scholar]
- Yazigi, C.; Kern, M.; Chaar, M.S.; Libecki, W.; Elsayed, A. The influence of the restorative material on the mechanical behavior of screw-retained hybrid-abutment-crowns. J. Mech. Behav. Biomed. Mater. 2020, 111, 103988. [Google Scholar] [CrossRef] [PubMed]
- Skirbutis, G.; Dzingutė, A.; Masiliūnaitė, V.; Šulcaitė, G.; Žilinskas, J. A review of PEEK polymer’s properties and its use in prosthodontics. Stomatologija 2017, 19, 19–23. [Google Scholar]
- Zhou, L.; Qia, Y.; Zhu, Y.; Liu, H.; Gan, K.; Guo, J. The effect of different surface treatments on the bond strength of PEEK composite materials. Dent. Mater. 2014, 30, e209–e215. [Google Scholar] [CrossRef] [PubMed]
- Liebermann, A.; Wimmer, T.; Schmidlin, P.R.; Scherer, H.; Löffler, P.; Roos, M.; Stawarczyk, B. Physicomechanical characterization of polyetheretherketone and current esthetic dental CAD/CAM polymers after aging in different storage media. J. Prosthet. Dent. 2016, 115, 321–328. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Mishra, S.; Chowdhary, R. PEEK materials as an alternative to titanium in dental implants: A systematic review. Clin. Implant Dent. Relat. Res. 2019, 21, 208–222. [Google Scholar] [CrossRef] [Green Version]
- Knaus, J.; Schaffarczyk, D.; Cölfen, H. On the Future Design of Bio-Inspired Polyetheretherketone Dental Implants. Macromol. Biosci. 2020, 20, 1900239. [Google Scholar] [CrossRef] [Green Version]
- Eraslan, R.; Colpak, E.D.; Kilic, K.; Polat, Z.A. Biomechanical Properties and Biocompatibility of Implant-Supported Full Arch Fixed Prosthesis Substructural Materials. Niger. J. Clin. Pract. 2021, 24, 1373–1379. [Google Scholar]
- Peng, T.Y.; Shih, Y.H.; Hsia, S.M.; Wang, T.H.; Li, P.J.; Lin, D.J.; Sun, K.T.; Chiu, K.C.; Shieh, T.M. In vitro assessment of the cell metabolic activity, cytotoxicity, cell attachment, and inflammatory reaction of human oral fibroblasts on polyetheretherketone (PEEK) implant–abutment. Polymers 2021, 13, 2995. [Google Scholar] [CrossRef]
- Sundriyal, P.; Sahu, M.; Prakash, O.; Bhattacharya, S. Long-term surface modification of PEEK polymer using plasma and PEG silane treatment. Surf. Interfaces 2021, 25, 101253. [Google Scholar] [CrossRef]
- Cai, S.; Wu, C.; Yang, W.; Liang, W.; Yu, H.; Liu, L. Recent advance in surface modification for regulating cell adhesion and behaviors. Nanotechnol. Rev. 2020, 9, 971–989. [Google Scholar] [CrossRef]
- Lotfi, M.; Nejib, M.; Naceur, M. Cell adhesion to biomaterials: Concept of biocompatibility. Adv. Biomater. Sci. Biomed. Appl. 2013, 8, 208–240. [Google Scholar]
- Dong, T.; Duan, C.; Wang, S.; Gao, X.; Yang, Q.; Yang, W.; Deng, Y. Multifunctional Surface with Enhanced Angiogenesis for Improving Long-Term Osteogenic Fixation of Poly (ether ether ketone) Implants. ACS Appl. Mater. Interface 2020, 12, 14971–14982. [Google Scholar] [CrossRef] [PubMed]
- Ma, R.; Tang, T. Current strategies to improve the bioactivity of PEEK. Int. J. Mol. Sci. 2014, 15, 5426–5445. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Montaño-Machado, V.; Chevallier, P.; Bonilla-Gameros, L.; Copes, F.; Quarta, C.; Kú-Herrera, J.d.J.; Soriano, F.; Padilla-Gainza, V.; Morales, G.; Mantovani, D. Development of Multifunctional Materials Based on Poly (ether ether ketone) with Improved Biological Performances for Dental Applications. Materials 2021, 14, 1047. [Google Scholar] [CrossRef]
- Pjetursson, B.E.; Tan, K.; Lang, N.P.; Bragger, U.; Egger, M.; Zwahlen., M. A systematic review of the survival and complication rates of fixed partial dentures (FPDs) after an observation period of at least 5 years I. Implant-supported FPDs. Clin. Oral Implant. Res. 2004, 15, 625–642. [Google Scholar] [CrossRef]
- Karasan, D.; Fehmer, V.; Ligoutsikou, M.; Srinivasan, M.; Sailer, I. The Influence of Patient-Related Factors and Material Selection on the Clinical Outcomes of Fixed and Removable Complete Implant Prostheses: An Overview on Systematic Reviews. Int. J. Prosthodont. 2021, 2, 34. [Google Scholar] [CrossRef]
- Raigrodski, A.J.; Hillstead, M.B.; Meng, G.K.; Chung, K.H. Survival and complications of zirconia-based fixed dental prostheses: A systematic review. J. Prosthet. Dent. 2012, 107, 170–177. [Google Scholar] [CrossRef]
- Shen, X.T.; Li, J.Y.; Luo, X.; Feng, Y.; Gai, L.T.; He, F.M. Peri-implant marginal bone changes with implant-supported metal-ceramic or monolithic zirconia single crowns: A retrospective clinical study of 1 to 5 years. J. Prosthet. Dent. 2021, 1–7. [Google Scholar] [CrossRef]
- Nejatidanesh, F.; Abbasi, M.; Savabi, G.; Bonakdarchian, M.; Atash, R.; Savabi, O. Five year clinical outcomes of metal ceramic and zirconia-based implant-supported dental prostheses: A retrospective study. J. Dent. 2020, 100, 103420. [Google Scholar] [CrossRef]
- Wazeh, A.M.; El-Anwar, M.I.; Atia, R.M.G.; Mahjari, R.M.; Linga, S.A.; Al-Pakistani, L.M.A.; Yousief, S.A. 3D FEA study on implant threading role on selection of implant and crown materials. Open Access Maced. J. Med. Sci. 2018, 6, 1702–1706. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Kaleli, N.; Sarac, D.; Külünk, S.; Öztürk, Ö. Effect of different restorative crown and customized abutment materials on stress distribution in single implants and peripheral bone: A three-dimensional finite element analysis study. J. Prosthet. Dent. 2018, 119, 437–445. [Google Scholar] [CrossRef] [PubMed]
- Datte, C.E.; Tribst, J.P.; Dal Piva, A.O.; Nishioka, R.S.; Bottino, M.A.; Evangelhista, A.M.; Monteiro, F.M.D.M. Influence of different restorative materials on the stress distribution in dental implants. J. Clin. Exp. Dent. 2018, 10, e439–e444. [Google Scholar] [CrossRef] [PubMed]
- Bagegni, A.; Abou-Ayash, S.; Rücker, G.; Algarny, A.; Att, W. The influence of prosthetic material on implant and prosthetic survival of implant-supported fixed complete dentures: A systematic review and meta-analysis. J. Prosthodont. Res. 2019, 63, 251–265. [Google Scholar] [CrossRef] [PubMed]
- Flask, J.D.; Thompson, G.A.; Singh, M.; Berzins, D.W. Edge chipping of translucent zirconia. J. Prosthet Dent. 2021, 1–8. [Google Scholar] [CrossRef]
- Arcila, L.V.C.; de Carvalho Ramos, N.; Campos, T.M.B.; Dapieve, K.S.; Valandro, L.F.; de Melo, R.M.; Bottino, M.A. Mechanical behavior and microstructural characterization of different zirconia polycrystals in different thicknesses. J. Adv. Prosthodont. 2021, 13, 385. [Google Scholar] [CrossRef]
- Kwon, S.J.; Lawson, N.C.; McLaren, E.E.; Nejat, A.H.; Burgess, J.O. Comparison of the mechanical properties of translucent zirconia and lithium disilicate. J. Prosthet. Dent. 2018, 120, 132–137. [Google Scholar] [CrossRef]
- Gautam, C.; Joyner, J.; Gautam, A.; Rao, J.; Vajtai, R. Zirconia based dental ceramics: Structure, mechanical properties, biocompatibility and applications. Dalton Trans. 2016, 45, 19194–19215. [Google Scholar] [CrossRef]
- Styles, J.A.; Wilson, J. Comparison between in vitro toxicity of two novel fibrous mineral dusts and their tissue reactions in vivo. Ann. Occup. Hyg. 1976, 19, 63–68. [Google Scholar]
- Covacci, V.; Bruzzese, N.; Maccauro, G.; Andreassi, C.; Ricci, G.A.; Piconi, C.; Marmo, E.; Burger, W.; Cittadini, A. In vitro evaluation of the mutagenic and carcinogenic power of high purity zirconia ceramic. Biomaterials 1999, 20, 371–376. [Google Scholar] [CrossRef]
- Josset, Y.; Oum Hamed, Z.; Zarrinpour, A.; Lorenzato, M.; Adnet, J.J.; Laurent-Maquin, D. In vitro reactions of human osteoblasts in culture with zirconia and alumina ceramics. J. Biomed. Mater. Res. 1999, 47, 481–493. [Google Scholar] [CrossRef]
- Catelas, I.; Petit, A.; Zukor, D.J.; Marchand, R.; Yahia, L.; Huk, O.L. Induction of macrophage apoptosis by ceramic and polyethylene particles in vitro. Biomaterials 1999, 20, 625–630. [Google Scholar] [CrossRef]
- Kim, D.J.; Lee, M.H.; Lee, D.Y.; Han, J.S. Mechanical properties, phase stability, and biocompatibility of (Y, Nb)-TZP/Al(2)O(3) composite abutments for dental implant. J. Biomed. Mater. Res. 2000, 53, 438–443. [Google Scholar] [CrossRef]
- Torricelli, P.; Verné, E.; Brovarone, C.; Appendino, P.; Rustichelli, F.; Krajewski, A.; Ravaglioli, A.; Pierini, G.; Fini, M.; Giavaresi, G.; et al. Biological glass coating on ceramic materials: In vitro evaluation using primary osteoblast cultures from healthy and osteopenic rat bone. Biomaterials 2001, 22, 2535–2543. [Google Scholar] [CrossRef]
- Lohmann, C.H.; Dean, D.D.; Köster, G.; Casasola, D.; Buchhorn, G.H.; Fink, U.; Schwartz, Z.; Boyan, B.D. Ceramic and PMMA particles differentially affect osteoblast phenotype. Biomaterials 2002, 23, 855–1863. [Google Scholar] [CrossRef]
- Manicone, P.F.; Rossi Iommetti, P.; Raffaelli, L. An overview of zirconia ceramics: Basic properties and clinical applications. J. Dent. 2007, 35, 819–826. [Google Scholar] [CrossRef]
- Schwarzl, F.; Langer, M.; Hagena, T.; Hartig, B.; Sader, R.; Becker, J. Cytotoxicity and proinflammatory effects oftitanium and zirconia particles. Int. J. Implant Dent. 2019, 5, 25. [Google Scholar] [CrossRef]
- Wei, C.; Gong, T.; Pow, E.H.N.; Botelho, M.G. Adhesive and oxidative response of stem cell and pre-osteoblasts on titanium and zirconia surfaces in vitro. J. Investig. Clin. Dent. 2019, 10, e12407. [Google Scholar] [CrossRef]
- Giannoni, E.; Buricchi, F.; Raugei, G.; Ramponi, G.; Chiarugi, P. Intracellular reactive oxygen species activate Src tyrosine kinase during cell adhesion and anchorage-dependent cell growth. Mol. Cell Biol. 2005, 25, 6391–6403. [Google Scholar] [CrossRef] [Green Version]
- Vilas-Boas, F.; Bagulho, A.; Tenente, R.; Teixeira, V.H.; Martins, G.; da Costa, G.; Real, C. Hydrogen peroxide regulates cell adhesion through the redox sensor RPSA. Free Radic. Biol. Med. 2016, 90, 145–157. [Google Scholar] [CrossRef]
- Tahayeri, A.; Morgan, M.; Fugolin, A.P.; Bompolaki, D.; Athirasala, A.; Pfeifer, C.S.; Ferracane, J.L.; Bertassoni, L.E. 3D printed versus conventionally cured provisional crown and bridge dental materials. Dent. Mater. 2018, 34, 192–200. [Google Scholar] [CrossRef] [PubMed]
- Wang, Y.; Xu, Z.; Wu, D.; Bai, J. Current Status and Prospects of Polymer Powder 3D Printing Technologies. Materials 2020, 13, 2406. [Google Scholar] [CrossRef]
- Engler, M.L.P.D.; Guth, J.; Keul, C.; Erdelt, K.; Edelhoff, D.; Liebermann, A. Residual monomer elution from different conventional and CAD/CAM dental polymers during artificial aging. Clin. Oral Investig. 2020, 24, 277–284. [Google Scholar] [CrossRef] [PubMed]
- Shim, J.S.; Kim, H.C.; Park, S.I.; Yun, H.J.; Ryu, J.J. Comparison of various implant provisional resin materials for cytotoxicity and attachment to human gingival fibroblasts. Int. J. Oral Maxillofac. Implant. 2019, 34, 390–396. [Google Scholar] [CrossRef] [PubMed]
- Duan, S.; Wu, R.; Xiong, Y.H.; Ren, H.M.; Lei, C.; Zhao, Y.Q.; Zang, X.Y.; Xu, F.J. Multifunctional antimicrobial materials: From rational design to biomedical applications. Prog. Mater. Sci. 2022, 125, 100887. [Google Scholar] [CrossRef]
- Santos, E.O.; Oliveira, P.L.E.; de Mello, T.P.; dos Santos, A.L.S.; Elias, C.N.; Choi, S.-H.; de Castro, A.C.R. Surface Characteristics and Microbiological Analysis of a Vat-Photopolymerization Additive-Manufacturing Dental Resin. Materials 2022, 15, 425. [Google Scholar] [CrossRef]
- González-Henríquez, C.M.; Sarabia-Vallejos, M.A.; Rodríguez Hernandez, J. Antimicrobial Polymers for Additive Manufacturing. Int. J. Mol. Sci. 2019, 20, 1210. [Google Scholar] [CrossRef] [Green Version]
- Lin, C.H.; Lin, Y.M.; Lai, Y.L.; Lee, S.Y. Mechanical properties, accuracy, and cytotoxicity of UV-polymerized 3D printing resins composed of Bis-EMA, UDMA, and TEGDMA. J. Prosthet. Dent. 2020, 123, 349–354. [Google Scholar] [CrossRef]
- Van Hengel, I.A.J.; Tierolf, M.; Valerio, V.P.M.; Minneboo, M.; Fluit, A.C.; Fratila-Apachitei, L.E.; Apachitei, I.; Zadpoor, A.A. Self-defending additively manufactured bone implants bearing silver and copper nanoparticles. J. Mater. Chem. B 2020, 8, 1589–1602. [Google Scholar] [CrossRef] [Green Version]
- Ramburrun, P.; Pringle, N.A.; Dube, A.; Adam, R.Z.; D’Souza, S.; Aucamp, M. Recent Advances in the Development of Antimicrobial and Antifouling Biocompatible Materials for Dental Applications. Materials 2021, 14, 3167. [Google Scholar] [CrossRef]
- Busscher, H.J.; Rinastiti, M.; Siswomihardjo, W.; van der Mei, H.C. Biofilm formation on dental restorative and implant materials. J. Dent. Res. 2010, 89, 657–665. [Google Scholar] [CrossRef] [PubMed]
- Chen, S.; Yang, J.; Jia, Y.G.; Lu, B.; Ren, L. A Study of 3D-Printable Reinforced Composite Resin: PMMA Modified with Silver Nanoparticles Loaded Cellulose Nanocrystal. Materials 2018, 11, 2444. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Barot, T.; Rawtani, D.; Kulkarni, P. Nanotechnology-based materials as emerging trends for dental applications. Rev. Adv. Mater. Sci. 2021, 60, 173–189. [Google Scholar] [CrossRef]
- Ho, D.; Quake, S.R.; McCabe, E.R.; Chng, W.J.; Chow, E.K.; Ding, X.; Gelb, B.D.; Ginsburg, G.S.; Hassenstab, J.; Ho, C.-M.; et al. Enabling Technologies for Personalized and Precision Medicine. Trends Biotechnol. 2020, 38, 497–518. [Google Scholar] [CrossRef]
- Suwardi, A.; Wang, F.; Xue, K.; Han, M.Y.; Teo, P.; Wang, P.; Wang, S.; Liu, Y.; Ye, E.; Li, Z.; et al. Machine Learning-Driven Biomaterials Evolution. Adv. Mater. 2022, 34, 2102703. [Google Scholar] [CrossRef]
| Studied Cell Type and/or Tissue | Study Conclusions | Reference |
|---|---|---|
| Fibroblasts | Yttria-stabilized tetragonal zirconia polycrystals (3Y-TZPs) ceramic did not induce any mutagenic or cellular transforming effects. | [113] |
| Osteoblasts | Zirconia ceramics did not alter cell ploidy or the cell growth rate. | [114] |
| Macrophages | Zirconia ceramics particles induced macrophage apoptotic cell death, in vitro. | [115] |
| Fibroblasts; subcutaneous implant test | ZrO2/Al2O3 composite showed no cytotoxicity and no significant adverse effects in soft tissues. | [116] |
| Osteoblasts | Zirconia samples insured good levels of biocompatibility. | [117] |
| Osteoblasts | ZrO2, Al2O3, and PMMA (poly (methyl methacrylate)) particles triggered direct effects on osteoblasts. Cell responses depended on the particle type. ZrO2 effect on alkaline phosphatase activity was targeted to the matrix vesicles. | [118] |
| Bone and muscle; Fibroblasts | New zirconia implants illustrated good biocompatibility and mechanical properties. | [119] |
|
Osteosarcoma-derived osteoblasts (SaOs-2); human gingival fibroblasts (HGF);monocytes (THP-1) | Zirconia particles affected the viability of SaOs-2 and HGF, but did not induce proinflammatory reactions in THP-1. | [120] |
| Human dental pulp stem cells; murine pre-osteoblasts | Zirconia as a potential dental implant material, illustrated similar or, even, better initial cellular responses versus titanium. | [121] |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Ionescu, R.N.; Totan, A.R.; Imre, M.M.; Țâncu, A.M.C.; Pantea, M.; Butucescu, M.; Farcașiu, A.T. Prosthetic Materials Used for Implant-Supported Restorations and Their Biochemical Oral Interactions: A Narrative Review. Materials 2022, 15, 1016. https://doi.org/10.3390/ma15031016
Ionescu RN, Totan AR, Imre MM, Țâncu AMC, Pantea M, Butucescu M, Farcașiu AT. Prosthetic Materials Used for Implant-Supported Restorations and Their Biochemical Oral Interactions: A Narrative Review. Materials. 2022; 15(3):1016. https://doi.org/10.3390/ma15031016
Chicago/Turabian StyleIonescu, Roxana Nicoleta, Alexandra Ripszky Totan, Marina Meleșcanu Imre, Ana Maria Cristina Țâncu, Mihaela Pantea, Mihai Butucescu, and Alexandru Titus Farcașiu. 2022. "Prosthetic Materials Used for Implant-Supported Restorations and Their Biochemical Oral Interactions: A Narrative Review" Materials 15, no. 3: 1016. https://doi.org/10.3390/ma15031016
APA StyleIonescu, R. N., Totan, A. R., Imre, M. M., Țâncu, A. M. C., Pantea, M., Butucescu, M., & Farcașiu, A. T. (2022). Prosthetic Materials Used for Implant-Supported Restorations and Their Biochemical Oral Interactions: A Narrative Review. Materials, 15(3), 1016. https://doi.org/10.3390/ma15031016








