Biochemical Interaction between Materials Used for Interim Prosthetic Restorations and Saliva
Abstract
:1. Introduction
2. Materials and Methods
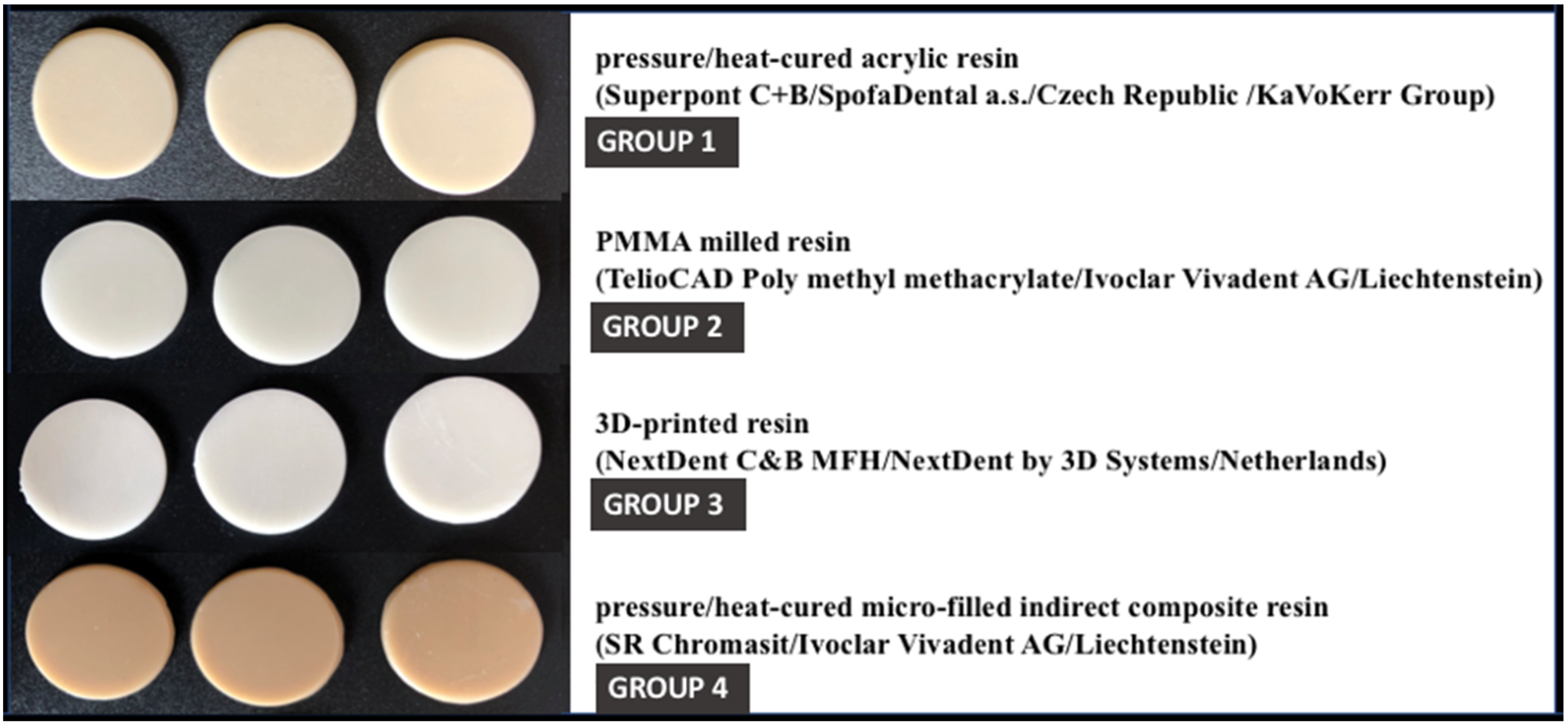
2.1. Fabrication of Resin Specimens
- -
- Group 1—corresponding to pressure/heat-cured acrylic resin;
- -
- Group 2—corresponding to milled PMMA resin;
- -
- Group 3—corresponding to 3D printed resin;
- -
- Group 4—corresponding to indirect composite resin.
2.2. Collection of Saliva Samples
2.3. Preparation of Saliva Samples and Biochemical Testing
2.4. Statistical Analysis
3. Results
4. Discussion
5. Conclusions
- The tested materials do not significantly alter the antioxidant capacity of the incubated saliva;
- The tested materials do not influence the salivary inflammatory status;
- Discreet differences between the distribution of the values of the investigated parameters depending on the material type were noticed without being, however, clinically relevant.
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Revilla-León, M.; Meyers, M.J.; Zandinejad, A.; Ozcan, M. A review on chemical composition, mechanical properties, and manufacturing workflow of additively manufactured current polymers for interim dental restorations. J. Esthet. Restor. Dent. 2019, 31, 51–57. [Google Scholar] [CrossRef] [Green Version]
- Della Bona, A.; Cantelli, V.; Britto, V.T.; Collares, K.F.; Stansbury, J.W. 3D printing restorative materials using a stereolithographic technique: A systematic review. Dent. Mater. 2021, 37, 336–350. [Google Scholar] [CrossRef]
- Jockusch, J.; Ozcan, M. Additive manufacturing of dental polymers: An overview on processes, materials and applications. Dent. Mater. J. 2020, 39, 345–354. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Reeponmaha, T.; Angwaravong, O.; Angwarawong, T. Comparison of fracture strength after thermo-mechanical aging between provisional crowns made with CAD/CAM and conventional method. J. Adv. Prosthodont. 2020, 12, 218–224. [Google Scholar] [CrossRef] [PubMed]
- Simoneti, D.M.; Pereira-Cenci, T.; Dos Santos, M.B.F. Comparison of material properties and biofilm formation in interim single crowns obtained by 3D printing and conventional methods. J. Prosthet. Dent. 2020. [Google Scholar] [CrossRef]
- Schönhoff, L.M.; Mayinger, F.; Eichberger, M.; Reznikova, E.; Stawarczyk, B. 3D printing of dental restorations: Mechanical properties of thermoplastic polymer materials. J. Mech. Behav. Biomed. Mater. 2021, 119, 104544. [Google Scholar] [CrossRef] [PubMed]
- Nold, J.; Wesemann, C.; Rieg, L.; Binder, L.; Witkowski, S.; Spies, B.C.; Kohal, R.J. Does Printing Orientation Matter? In-Vitro Fracture Strength of Temporary Fixed Dental Prostheses after a 1-Year Simulation in the Artificial Mouth. Materials 2021, 14, 259. [Google Scholar] [CrossRef] [PubMed]
- Tribst, J.P.M.; Borges, A.L.S.; Silva-Concílio, L.R.; Bottino, M.A.; Özcan, M. Effect of Restorative Material on Mechanical Response of Provisional Endocrowns: A 3D—FEA Study. Materials 2021, 14, 649. [Google Scholar] [CrossRef]
- Firlej, M.; Pieniak, D.; Niewczas, A.M.; Walczak, A.; Domagała, I.; Borucka, A.; Przystupa, K.; Igielska-Kalwat, J.; Jarosz, W.; Biedziak, B. Effect of Artificial Aging on Mechanical and Tribological Properties of CAD/CAM Composite Materials Used in Dentistry. Materials 2021, 14, 4678. [Google Scholar] [CrossRef]
- Nam, N.-E.; Shin, S.-H.; Lim, J.-H.; Shim, J.-S.; Kim, J.-E. Effects of Artificial Tooth Brushing and Hydrothermal Aging on the Mechanical Properties and Color Stability of Dental 3D-printed and CAD/CAM Materials. Materials 2021, 14, 6207. [Google Scholar] [CrossRef]
- Lim, N.K.; Shin, S.Y. Bonding of conventional interim resin to 3D-printed resin: The role of surface treatments and type of repair resins. J. Adv. Prosthodont. 2020, 12, 322–328. [Google Scholar] [CrossRef] [PubMed]
- Gantz, L.; Fauxpoint, G.; Arntz, Y.; Pelletier, H.; Etienne, O. In vitro comparison of the surface roughness of polymethyl methacrylate and bis-acrylic resins for interim restorations before and after polishing. J. Prosthet. Dent. 2021, 125, 833.e1. [Google Scholar] [CrossRef] [PubMed]
- Skorulska, A.; Piszko, P.; Rybak, Z.; Szymonowicz, M.; Dobrzyński, M. Review on Polymer, Ceramic and Composite Materials for CAD/CAM Indirect Restorations in Dentistry—Application, Mechanical Characteristics and Comparison. Materials 2021, 14, 1592. [Google Scholar] [CrossRef] [PubMed]
- Hussain, B.; Le Thieu, M.K.; Johnsen, G.F.; Reseland, J.E.; Haugen, H.J. Can CAD/CAM resin blocks be considered as substitute for conventional resins? Dent. Mater. 2017, 33, 1362–1370. [Google Scholar] [CrossRef] [PubMed]
- Carve, M.; Wlodkowic, D. 3D-Printed Chips: Compatibility of Additive Manufacturing Photopolymeric Substrata with Biological Applications. Micromachines 2018, 9, 91. [Google Scholar] [CrossRef] [Green Version]
- Garg, P.; Ravi, R.; Ghalaut, P. Outcome of Interim Restorations on Basis of Materials and Techniques of Choice: A Systematic Review. EAS J. Dent. Oral Med. 2021, 3, 6–15. [Google Scholar]
- Sa, L.; Kaiwu, L.; Shenggui, C.; Junzhong, Y.; Yongguang, J.; Lin, W.; Li, R. 3D printing dental composite resins with sustaining antibacterial ability. J. Mater. Sci. 2019, 54, 3309–3318. [Google Scholar] [CrossRef]
- Pantea, M.; Ighigeanu, D.A.; Totan, A.; Greabu, M.; Miricescu, D.; Melescanu-Imre, M.; Totan, C.; Spinu, T.C.; Petre, A.; Bencze, A.; et al. Interactions between dental composite resins and saliva—A comparative biochemical in vitro study. Rev. Mater. Plast. 2019, 56, 529–533. [Google Scholar] [CrossRef]
- Raszewski, Z. Acrylic resins in the CAD/CAM technology: A systematic literature review. Dent. Med. Probl. 2020, 57, 449–454. [Google Scholar] [CrossRef] [PubMed]
- Zafar, M.S. Prosthodontic Applications of Polymethyl Methacrylate (PMMA): An Update. Polymers 2020, 12, 2299. [Google Scholar] [CrossRef] [PubMed]
- Saeed, F.; Muhammad, N.; Khan, A.S.; Sharif, F.; Rahim, A.; Ahmad, P.; Irfan, M. Prosthodontics dental materials: From conventional to unconventional. Mater. Sci. Eng. C 2020, 106, 110167. [Google Scholar] [CrossRef]
- Rutkunas, V.; Borusevicius, R.; Liaudanskaite, D.; Jasinskyte, U.; Drukteinis, S.; Bukelskiene, V.; Mijiritsky, E. The Effect of Different Cleaning Protocols of Polymer-Based Prosthetic Materials on the Behavior of Human Gingival Fibroblasts. Int. J. Environ. Res. Public Health 2020, 17, 7753. [Google Scholar] [CrossRef] [PubMed]
- Reymus, M.; Lümkemann, N.; Stawarczyk, B. 3D-printed material for temporary restorations: Impact of print layer thickness and post-curing method on degree of conversion. Int. J. Comput. Dent. 2019, 22, 231–237. [Google Scholar] [PubMed]
- Tichy, A.; Simkova, M.; Schweiger, J.; Bradna, P.; Güth, J.-F. Release of Bisphenol A from Milled and 3D-Printed Dental Polycarbonate Materials. Materials 2021, 14, 5868. [Google Scholar] [CrossRef]
- Zheng, X.; Zhang, F.; Wang, K.; Zhang, W.; Li, Y.; Sun, Y.; Sun, X.; Li, C.; Dong, B.; Wang, L.; et al. Smart biosensors and intelligent devices for salivary biomarker detection. TrAC Trends Anal. Chem. 2021, 140, 116281. [Google Scholar] [CrossRef]
- Zhang, L.; Henson, B.S.; Camargo, P.M.; Wong, D.T. The clinical value of salivary biomarkers for periodontal disease. Periodontol. 2000 2009, 51, 25–37. [Google Scholar] [CrossRef] [PubMed]
- Kaushik, R.; Yeltiwar, R.K.; Pushpanshu, K. Salivary interleukin-1β levels in patients with chronic periodontitis before and after periodontal phase I therapy and healthy controls: A case-control study. J. Periodontol. 2011, 82, 1353–1359. [Google Scholar] [CrossRef]
- Arias-Bujanda, N.; Regueira-Iglesias, A.; Balsa-Castro, C.; Nibali, L.; Donos, N.; Tomás, I. Accuracy of single molecular biomarkers in saliva for the diagnosis of periodontitis: A systematic review and meta-analysis. J. Clin. Periodontol. 2020, 47, 2–18. [Google Scholar] [CrossRef] [PubMed]
- Roi, A.; Rusu, L.C.; Roi, C.I.; Luca, R.E.; Boia, S.; Munteanu, R.I. A New Approach for the Diagnosis of Systemic and Oral Diseases Based on Salivary Biomolecules. Dis. Markers 2019, 8761860. [Google Scholar] [CrossRef] [Green Version]
- Patel, S.I.; Jadhav, V.; Shetty, P.; Deshpande, P.; Gorwade, N.; Shinde, N. Gamma Glutamyl Transferase—A Link between Oxidative Stress and Periodontitis in Smokeless Tobacco Users and Non Users with Chronic Periodontitis. Int. J. Biochem. Res. Rev. 2017, 20, 1–9. [Google Scholar] [CrossRef]
- Borzangy, S.; Labban, N.; Windsor, L.J. Effects of interim acrylic resins on the expression of cytokines from epithelial cells and on collagen degradation. J. Prosthet. Dent. 2013, 110, 296–302. [Google Scholar] [CrossRef]
- Labban, N.; Song, F.; Al-Shibani, N.; Windsor, L.J. Effects of provisional acrylic resins on gingival fibroblast cytokine/growth factor expression. J. Prosthet. Dent. 2008, 100, 390–397. [Google Scholar] [CrossRef]
- MacEntee, M.I.; Bartlett, S.O.; Loadholt, C.B. A histologic evaluation of tissue response to three currently used temporary acrylic resin crowns. J. Prosthet. Dent. 1978, 39, 42–46. [Google Scholar] [CrossRef]
- Kim, J.-Y.; Kim, K.-R.; Kim, H.-N. The Potential Impact of Salivary IL-1 on the Diagnosis of Periodontal Disease: A Pilot Study. Healthcare 2021, 9, 729. [Google Scholar] [CrossRef]
- Giannobile, W.V.; McDevitt, J.T.; Niedbala, R.S.; Malamud, D. Translational and clinical applications of salivary diagnostics. Adv. Dent. Res. 2011, 23, 375–380. [Google Scholar] [CrossRef]
- Gonçalves, F.P.; Alves, G.; Guimarães, V.O., Jr.; Gallito, M.A.; Oliveira, F.; Scelza, M.Z. Cytotoxicity evaluation of two bis-acryl composite resins using human gingival fibroblasts. Braz. Dent. J. 2016, 27, 492–496. [Google Scholar] [CrossRef] [Green Version]
- Shim, J.S.; Kim, H.C.; Park, S.I.; Yun, H.J.; Ryu, J.J. Comparison of Various Implant Interim Resin Materials for Cytotoxicity and Attachment to Human Gingival Fibroblasts. Int. J. Oral Maxillofac. Implant. 2019, 34, 390–396. [Google Scholar] [CrossRef] [PubMed]
- Souza, I.R.; Pansani, T.N.; Basso, F.G.; Hebling, J.; de Souza Costa, C.A. Cytotoxicity of acrylic resin-based materials used to fabricate interim crowns. J. Prosthet. Dent. 2020, 124, 122.e1. [Google Scholar] [CrossRef] [PubMed]
- Park, J.H.; Lee, H.; Kim, J.W.; Kim, J.H. Cytocompatibility of 3D printed dental materials for temporary restorations on fibroblasts. BMC Oral Health 2020, 20, 157. [Google Scholar] [CrossRef]
- Campaner, M.; Takamiya, A.S.; Bitencourt, S.B.; Mazza, L.C.; de Oliveira, S.H.P.; Shibayama, R.; Barão, V.A.R.; Sukotjo, C.; Pesqueira, A.A. Cytotoxicity and inflammatory response of different types of provisional restorative materials. Arch. Oral Biol. 2020, 111, 104643. [Google Scholar] [CrossRef]
- Rizo-Gorrita, M.; Herráez-Galindo, C.; Torres-Lagares, D.; Serrera-Figallo, M.-Á.; Gutiérre-Pérez, J.-L. Biocompatibility of polymer and ceramic CAD/CAM materials with human gingival fibroblasts (HGFs). Polymers 2019, 11, 1446. [Google Scholar] [CrossRef] [Green Version]
- Herráez-Galindo, C.; Rizo-Gorrita, M.; Luna-Oliva, I.; Serrera-Figallo, M.-Á.; Castillo-Oyagüe, R.; Torres-Lagares, D. In vitro Comparative Study of Fibroblastic Behaviour on Polymethacrylate (PMMA) and Lithium Disilicate Polymer Surfaces. Polymers 2019, 11, 744. [Google Scholar] [CrossRef] [Green Version]
- Lin, C.H.; Lin, Y.M.; Lai, Y.L.; Lee, S.Y. Mechanical properties, accuracy, and cytotoxicity of UV-polymerized 3D printing resins composed of Bis-EMA, UDMA, and TEGDMA. J. Prosthet. Dent. 2020, 123, 349–354. [Google Scholar] [CrossRef]
- Bayarsaikhan, E.; Lim, J.-H.; Shin, S.-H.; Park, K.-H.; Park, Y.-B.; Lee, J.-H.; Kim, J.-E. Effects of Postcuring Temperature on the Mechanical Properties and Biocompatibility of Three-Dimensional Printed Dental Resin Material. Polymers 2021, 13, 1180. [Google Scholar] [CrossRef]
- Jun, S.K.; Mahapatra, C.; Lee, H.H.; Kim, H.W.; Lee, J.H. Biological effects of provisional resin materials on human dental pulp stem cells. Oper. Dent. 2017, 42, E81–E92. [Google Scholar] [CrossRef]
- Lee, J.H.; Jun, S.K.; Moon, H.J.; Lee, H.H. Cytotoxicity and proinflammatory cytokine expression induced by interim resin materials in primary cultured human dental pulp cells. J. Prosthet. Dent. 2017, 118, 524–534. [Google Scholar] [CrossRef]
- Ivkovic, N.; Bozovic, D.; Ristic, S.; Mirjanic, V.; Jankovic, O. The residual monomer in dental acrylic resin and its adverse effects. Contemp. Mater. 2013, 4, 84–91. [Google Scholar] [CrossRef]
- Bandarra, S.; Mascarenhas, P.; Luís, A.R.; Catrau, M.; Bekman, E.; Ribeiro, A.C.; Félix, S.; Caldeira, J.; Barahona, I. In vitro and in silico evaluations of resin-based dental restorative material toxicity. Clin. Oral Investig. 2020, 24, 2691–2700. [Google Scholar] [CrossRef]
- Engler, M.L.P.D.; Güth, J.F.; Keul, C.; Erdelt, K.; Edelhoff, D.; Liebermann, A. Residual monomer elution from different conventional and CAD/CAM dental polymers during artificial aging. Clin. Oral Investig. 2020, 24, 277–284. [Google Scholar] [CrossRef]
- Azizi, A.; Zamparini, F.; Spinelli, A.; Pirani, C.; Gandolfi, M.G.; Prati, C. Maryland-bridge application as a suitable technique to preserve marginal bone level of not-submerged supracrestal implants. Minerva Stomatol. 2020, 69, 335–342. [Google Scholar] [CrossRef]
- Poggio, C.E.; Salvato, A. Bonded provisional restorations for esthetic soft tissue support in single-implant treatment. J. Prosthet. Dent. 2002, 87, 688–691. [Google Scholar] [CrossRef]
- Siadat, H.; Alikhasi, M.; Beyabanaki, E. Interim prosthesis options for dental implants. J. Prosthodont. 2017, 26, 331–338. [Google Scholar] [CrossRef]
- Ulker, M.; Ulker, H.E.; Zortuk, M.; Bulbul, M.; Tuncdemir, A.R.; Bilgin, M.S. Effects of current provisional restoration materials on the viability of fibroblasts. Eur. J. Dent. 2009, 3, 114–119. [Google Scholar] [CrossRef] [Green Version]
- Atay, A.; Gürdal, I.; Bozok Çetıntas, V.; Üşümez, A.; Cal, E. Effects of New Generation All-Ceramic and Provisional Materials on Fibroblast Cells. J. Prosthodont. 2019, 28, e383–e394. [Google Scholar] [CrossRef] [Green Version]
- Giti, R.; Dabiri, S.; Motamedifar, M.; Derafshi, R. Surface roughness, plaque accumulation, and cytotoxicity of provisional restorative materials fabricated by different methods. PLoS ONE 2021, 16, e0249551. [Google Scholar] [CrossRef]
- Pituru, S.M.; Greabu, M.; Totan, A.; Imre, M.; Pantea, M.; Spinu, T.; Tancu, A.M.C.; Popoviciu, N.O.; Stanescu, I.-I.; Ionescu, E. A Review on the Biocompatibility of PMMA-Based Dental Materials for Interim Prosthetic Restorations with a Glimpse into Their Modern Manufacturing Techniques. Materials 2020, 13, 2894. [Google Scholar] [CrossRef]
- Astudillo-Rubio, D.; Delgado-Gaete, A.; Bellot-Arcís, C.; Montiel-Company, J.M.; Pascual-Moscardó, A.; Almerich-Silla, J.M. Mechanical properties of provisional dental materials: A systematic review and meta-analysis. PLoS ONE 2018, 13, e0193162. [Google Scholar] [CrossRef] [Green Version]
- Song, G.; Son, J.W.; Jang, J.H.; Choi, S.H.; Jang, W.H.; Lee, B.N.; Park, C. Comparing volumetric and biological aspects of 3D-printed interim restorations under various post-curing modes. J. Adv. Prosthodont. 2021, 13, 71. [Google Scholar] [CrossRef]
- Piedra-Cascón, W.; Krishnamurthy, V.R.; Att, W.; Revilla-León, M. 3D printing parameters, supporting structures, slicing, and post-processing procedures of vat-polymerization additive manufacturing technologies: A narrative review. J. Dent. 2021, 109, 103630. [Google Scholar] [CrossRef]
- Mostafavi, D.; Methani, M.M.; Piedra-Cascón, W.; Zandinejad, A.; Revilla-León, M. Influence of the Rinsing Postprocessing Procedures on the Manufacturing Accuracy of Vat-Polymerized Dental Model Material. J. Prosthodont. 2021, 30, 610–616. [Google Scholar] [CrossRef]
- Tahayeri, A.; Morgan, M.; Fugolin, A.P.; Bompolaki, D.; Athirasala, A.; Pfeifer, C.S.; Ferracane, J.L.; Bertassoni, L.E. 3D-printed versus conventionally cured provisional crown and bridge dental materials. Dent. Mater. 2018, 34, 192–200. [Google Scholar] [CrossRef] [PubMed]
- Nayar, S.; Bhuminathan, S.; Bhat, W.M. Rapid prototyping and stereolithography in dentistry. J. Pharm. BioAllied Sci. 2015, 7, S216–S219. [Google Scholar] [CrossRef]
- Alharbi, N.; Osman, R.; Wismeijer, D. Effects of build direction on the mechanical properties of 3D-printed complete coverage interim dental restorations. J. Prosthet. Dent. 2016, 115, 760–767. [Google Scholar] [CrossRef] [PubMed]
- Ide, Y.; Nayar, S.; Logan, H.; Gallagher, B.; Wolfaardt, J. The effect of the angle of acuteness of additive manufactured models and the direction of printing on the dimensional fidelity: Clinical implications. Odontology 2017, 105, 108–115. [Google Scholar] [CrossRef] [PubMed]




| Material/ Parameter (Average ± SD) | Pressure/Heat-Cured Acrylic Resin | Milled PMMA | 3D-Printed Resin | Composite Resin | ||||
|---|---|---|---|---|---|---|---|---|
| Before Incubation | After Incubation | Before Incubation | After Incubation | Before Incubation | After Incubation | Before Incubation | After Incubation | |
| Uric acid/albumin | 1.406 ± 0.2 | 1.11 ± 0.175 | 2.1 ± 0.2 | 2.26 ± 0.251 | 1.6 ± 0.36 | 1.5 ± 0.2 | 1.66 ± 0.55 | 1.66 ± 0.461 |
| GGT/albumin | 4.76 ± 1.06 | 4.866 ± 1.3 | 4.16 ± 0.305 | 4.1 ± 0.458 | 4.66 ± 0.75 | 4.5 ± 0.984 | 4.1 ± 0.5 | 4.066 ± 0.763 |
| IL-6/albumin | 91.88 ± 81.95 | 91.36 ± 81.16 | 98.47 ± 9.05 | 95.41 ± 10.53 | 20.33 ± 9.76 | 19.3 ± 8.35 | 46.69 ± 9.302 | 45.64 ± 8.07 |
| OXSR1/albumin | 0.583 ± 0.1 | 0.476 ± 0.151 | 0.433 ± 0.081 | 0.41 ± 0.098 | 0.593 ± 0.258 | 0.556 ± 0.228 | 0.43 ± 0.207 | 0.493 ± 0.283 |
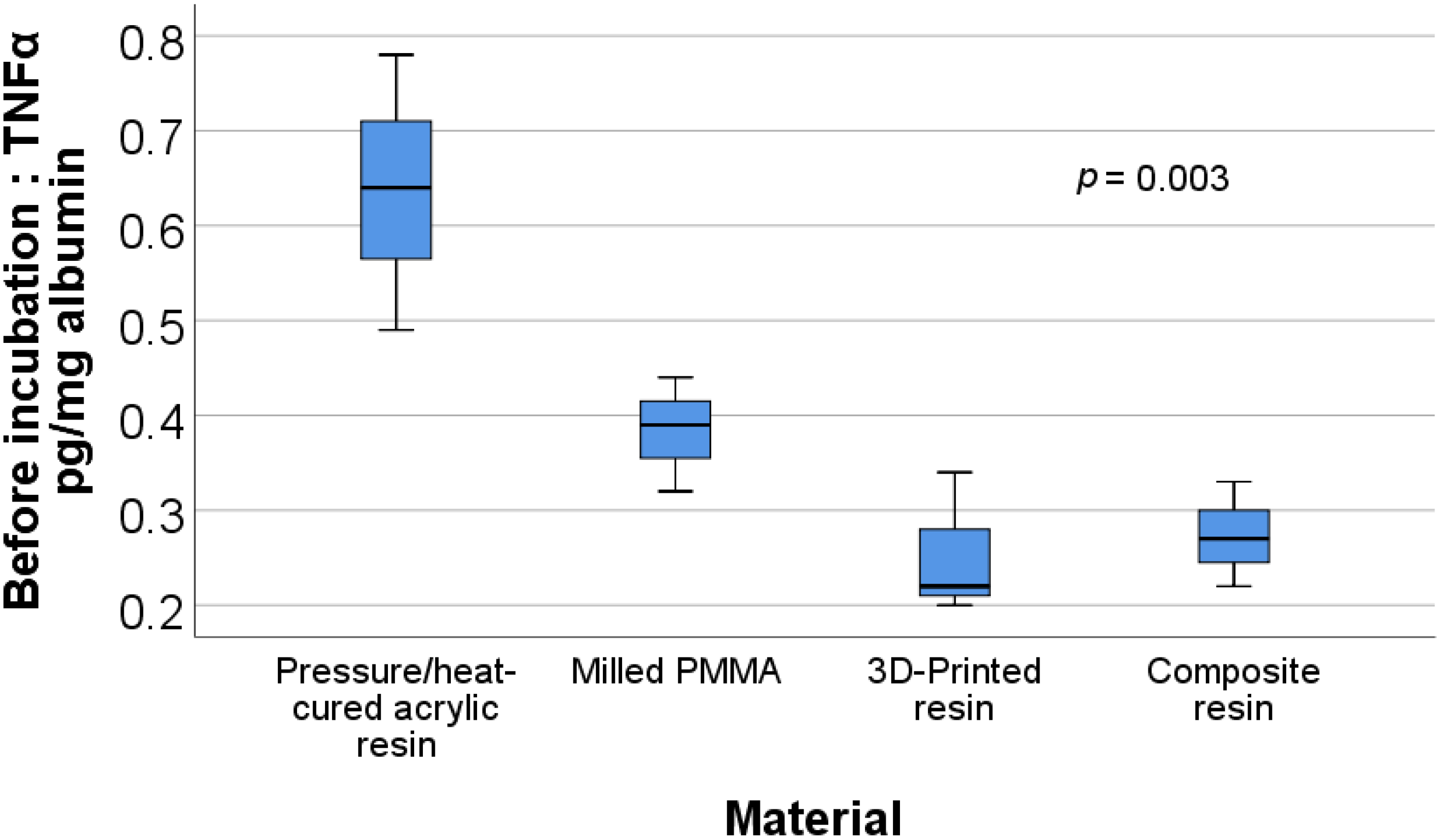
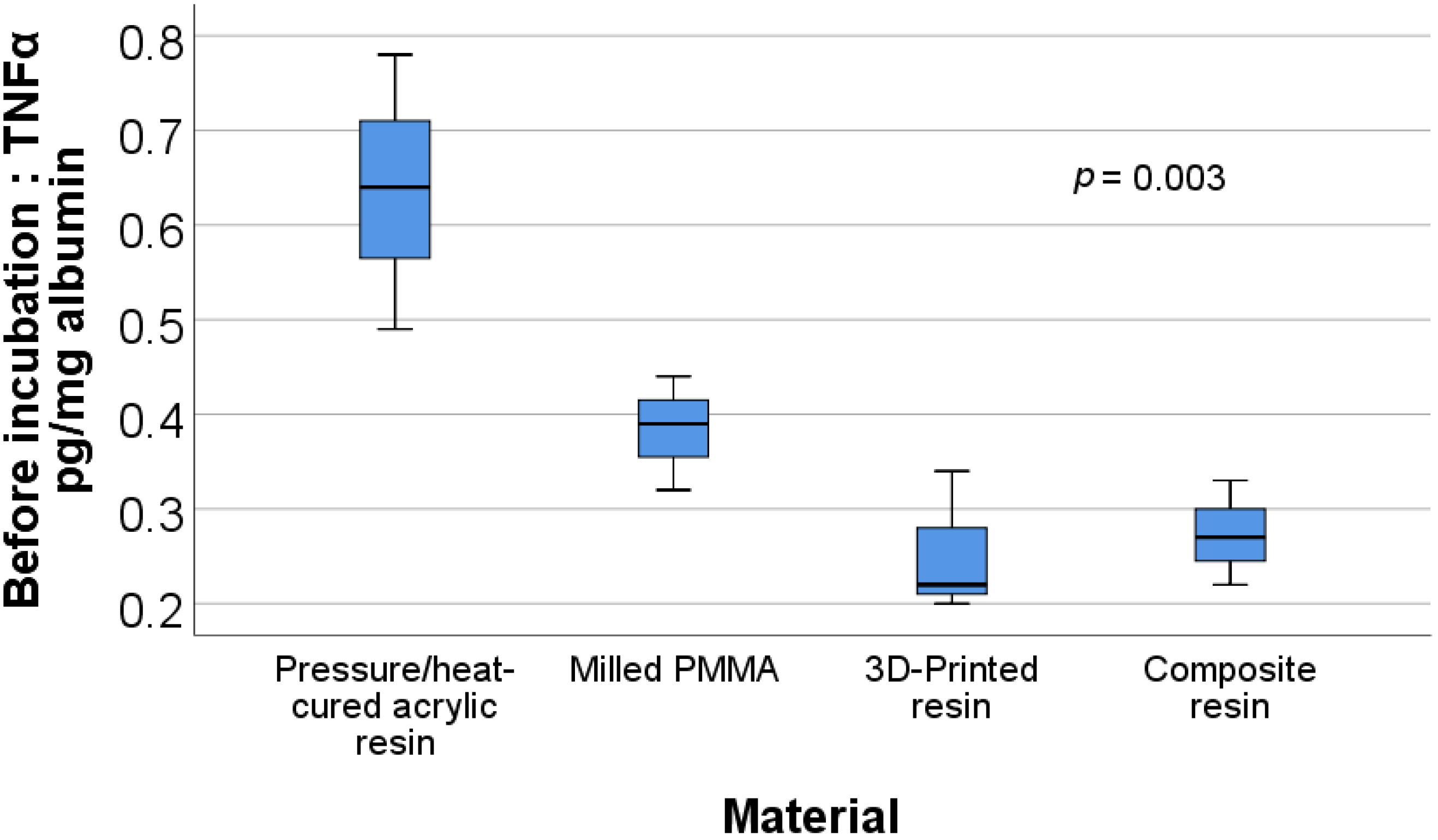
| TNFα/albumin | 0.636 ± 0.145 | 0.616 ± 0.09 | 0.383 ± 0.06 | 0.37 ± 0.06 | 0.253 ± 0.075 | 0.25 ± 0.05 | 0.273 ± 0.055 | 0.286 ± 0.055 |
| TAC/albumin | 1.48 ± 0.137 | 1.173 ± 0.243 | 1.63 ± 0.152 | 1.56 ± 0.23 | 1.933 ± 0.568 | 1.833 ± 0.351 | 2.23 ± 0.75 | 2.166 ± 0.642 |
| Before Incubation | After Incubation | ||
|---|---|---|---|
| Parameter | p | Parameter | p |
| Uric acid/albumin | 0.192 * | Uric acid/albumin | 0.032 ** |
| GGT/albumin | 0.683 ** | GGT/albumin | 0.696 * |
| IL-6/albumin | 0.003 *** | IL-6/albumin | 0.004 *** |
| OXSR1/albumin | 0.592 ** | OXSR1/albumin | 0.850 * |
| TNFα/albumin | 0.003 * | TNFα/albumin | 0.001 * |
| TAC/albumin | 0.267 ** | TAC/albumin | 0.061 ** |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Pantea, M.; Totan, A.R.; Imre, M.; Petre, A.E.; Țâncu, A.M.C.; Tudos, C.; Farcașiu, A.T.; Butucescu, M.; Spînu, T.C. Biochemical Interaction between Materials Used for Interim Prosthetic Restorations and Saliva. Materials 2022, 15, 226. https://doi.org/10.3390/ma15010226
Pantea M, Totan AR, Imre M, Petre AE, Țâncu AMC, Tudos C, Farcașiu AT, Butucescu M, Spînu TC. Biochemical Interaction between Materials Used for Interim Prosthetic Restorations and Saliva. Materials. 2022; 15(1):226. https://doi.org/10.3390/ma15010226
Chicago/Turabian StylePantea, Mihaela, Alexandra Ripszky Totan, Marina Imre, Alexandru Eugen Petre, Ana Maria Cristina Țâncu, Cristian Tudos, Alexandru Titus Farcașiu, Mihai Butucescu, and Tudor Claudiu Spînu. 2022. "Biochemical Interaction between Materials Used for Interim Prosthetic Restorations and Saliva" Materials 15, no. 1: 226. https://doi.org/10.3390/ma15010226
APA StylePantea, M., Totan, A. R., Imre, M., Petre, A. E., Țâncu, A. M. C., Tudos, C., Farcașiu, A. T., Butucescu, M., & Spînu, T. C. (2022). Biochemical Interaction between Materials Used for Interim Prosthetic Restorations and Saliva. Materials, 15(1), 226. https://doi.org/10.3390/ma15010226








