Fracture Resistance in Non-Vital Teeth: Absence of Interproximal Ferrule and Influence of Preparation Depth in CAD/CAM Endocrown Overlays—An In Vitro Study
Abstract
1. Introduction
2. Materials and Methods
2.1. Groups Distribution and Specimens Preparation
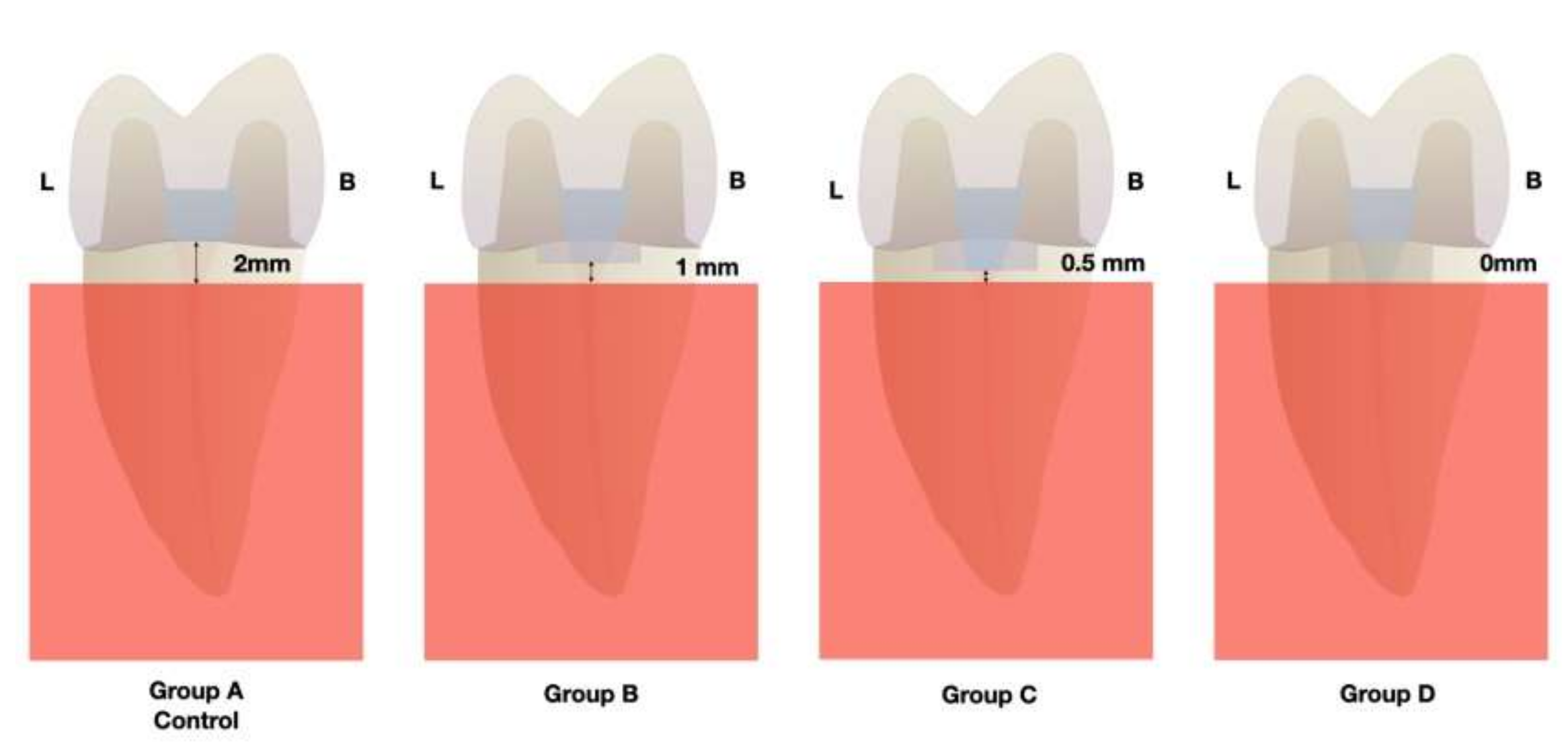
- Group A (control group): the restoration margin was placed at the level of the cement-to-enamel junction (CEJ), 2 mm above the simulated alveolar crest.
- Group B: the restoration margin was placed 1 mm under CEJ in mesial and distal walls, 1 mm above the simulated alveolar crest.
- Group C: the restoration margin was placed at 1.5 mm under CEJ in mesial and distal walls, 0.5 mm from above the simulated alveolar crest.
- Group D: the restoration margin was placed at 2 mm under CEJ in mesial and distal walls, at the level of simulated alveolar crest (Figure 1).
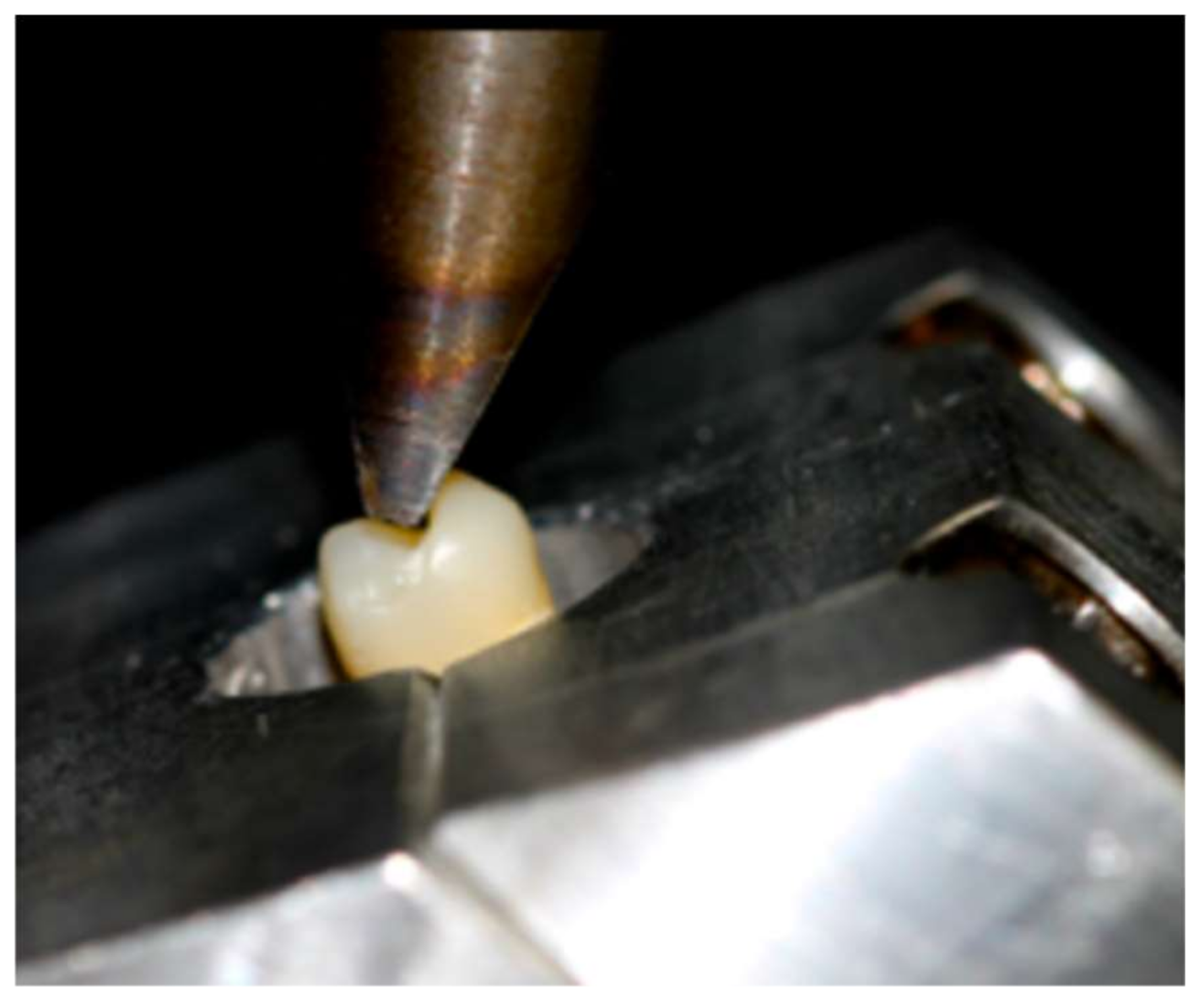
2.2. Loading Test
2.3. Statistical Analysis
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Edelhoff, D.; Liebermann, A.; Beuer, F.; Stimmelmayr, M.; Güth, J.-F. Minimally invasive treatment options in fixed prosthodontics. Quintessence Int. 2016, 47, 207–216. [Google Scholar] [CrossRef] [PubMed]
- Grütter, L.; Vailati, F. Full-mouth adhesive rehabilitation in case of severe dental erosion, a minimally invasive approach following the 3-step technique. Eur. J. Esthet. Dent. Off. J. Eur. Acad. Esthet. Dent. 2013, 8, 358–375. [Google Scholar]
- Assif, D.; Gorfil, C. Biomechanical considerations in restoring endodontically treated teeth. J. Prosthet. Dent. 1994, 71, 565–567. [Google Scholar] [CrossRef]
- Dietschi, D.; Duc, O.; Krejci, I.; Sadan, A. Biomechanical considerations for the restorations of endodontically treated teeth: A systematic review of the literature-part I. Composition and micro and macrostructure alterations. Quintessence Int. 2007, 38, 733–743. [Google Scholar] [PubMed]
- Biacchi, G.R.; Basting, R.T. Comparison of Fracture Strength of Endocrowns and Glass Fiber Post-Retained Conventional Crowns. Oper. Dent. 2012, 37, 130–136. [Google Scholar] [CrossRef] [PubMed]
- Morgano, S.M.; Bracket, S.E. Foundation restorations in fixed prosthodontics: Current knowledge and future needs. J. Prosthet. Dent. 1999, 82, 643–657. [Google Scholar] [CrossRef]
- Sorensen, J.A.; Engelman, M.J. Ferrule design and fracture resistance of endodontically treated teeth. J. Prosthet. Dent. 1990, 63, 529–536. [Google Scholar] [CrossRef]
- Pereira, J.R.; Neto, T.D.M.; Porto, V.D.C.; Pegoraro, L.F.; Valle, A.L.D. Influence of the remaining coronal structure on the resistance of teeth with intraradicular retainer. Braz. Dent. J. 2005, 16, 197–201. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Iqbal, M.; Dua, N.; Kumar, B.; Arunagiri, D.; Pushpa, S.; Hussain, J. Comparative evaluation of the effect of different crown ferrule designs on the fracture resistance of endodontically treated mandibular premolars restored with fiber posts, composite cores, and crowns: An ex-vivo study. J. Conserv. Dent. 2016, 19, 264–269. [Google Scholar] [CrossRef]
- Gegauff, A.G. Effect of crown lengthening and ferrule placement on static load failure of cemented cast post-cores and crowns. J. Prosthet. Dent. 2000, 84, 169–179. [Google Scholar] [CrossRef]
- Garguilo, W.; Wentz, M.F.; Orban, B. Dimensions and relations of the dentogingival junction in humans. J. Periodontol. 1961, 32, 261–267. [Google Scholar] [CrossRef]
- Vacek, J.S.; Gher, M.E.; Assad, D.A.; Richardson, A.C.; Giambarresi, L.I. The dimensions of the human dentogingival junction. Int. J. Periodontics Restor. Dent. 1994, 14, 154–165. [Google Scholar]
- Kosyfaki, P.; del Pilar Pinilla Martín, M.; Strub, J.R. Relationship between crowns and the periodontium: A literature update. Quintessence Int. 2010, 41, 109–126. [Google Scholar]
- De Oliveira, D.W.D.; Maravilha, M.N.P.; Dos Anjos, T.N.; Gonçalves, P.F.; Flecha, O.D.; Tavano, K. Clinical and Radiographic Evaluation of the Periodontium with Biologic Width Invasion by Overextending Restoration Margins—A Pilot Study. J. Int. Acad. Periodontol. 2015, 17, 116–122. [Google Scholar]
- Jepsen, S.; Caton, J.G.; Albandar, J.M.; Bissada, N.F.; Bouchard, P.; Cortellini, P.; Demirel, K.; de Sanctis, M.; Ercoli, C.; Fan, J.; et al. Periodontal manifestations of systemic diseases and developmental and acquired conditions: Consensus report of workgroup 3 of the 2017 World Workshop on the Classification of Periodontal and Peri-Implant Diseases and Conditions. J. Clin. Periodontol. 2018, 45, S219–S229. [Google Scholar] [CrossRef] [PubMed]
- Palomo, F.; Kopczyk, R.A. Rationale and methods for crown lengthening. J. Am. Dent. Assoc. 1978, 96, 257–260. [Google Scholar] [CrossRef] [PubMed]
- Pilalas, I.; Tsalikis, L.; Tatakis, D.N. Pre-restorative crown lengthening surgery outcomes: A systematic review. J. Clin. Periodontol. 2016, 43, 1094–1108. [Google Scholar] [CrossRef]
- Davarpanah, M.; Jansen, C.E.; Vidjak, F.M.; Etienne, D.; Kebir, M.; Martinez, H. Restorative and periodontal considerations of short clinical crowns. Int. J. Periodontics Restor. Dent. 1998, 18, 425–433. [Google Scholar]
- Kireev, V.V.; Chistyakov, E.M.; Filatov, S.N.; Tupikov, A.S.; Panfilova, D.V.; Chetverikova, A.I. Polymeric dental composites modified with carboxyphosphazene methacrylates. Russ. J. Appl. Chem. 2015, 88, 866–870. [Google Scholar] [CrossRef]
- Chistyakov, E.M.; Kolpinskaya, N.; Pspkhova, V.; Chuev, V. Dental composition modified with aryloxyphophazene containing carboxyl groups. Polymers 2020, 12, 1176. [Google Scholar] [CrossRef]
- Khorsandi, D.; Fahimipour, A.; Abasian, P.; Saber, S.S.; Seyedi, M.; Ghanavati, S.; Ahmad, A.; De Stephanis, A.A.; Taghavinezhaddilami, F.; Leonova, A.; et al. 3D and 4D printing in dentistry and maxillofacial surgery: Printing techniques, materials, and applications. Acta Biomater. 2020, 122, 26–49. [Google Scholar] [CrossRef]
- Ghajghouj, O.; Taşar-Faruk, S. Evaluation of Fracture Resistance and Microleakage of Endocrowns with Different Intracoronal Depths and Restorative Materials Luted with Various Resin Cements. Materials 2019, 12, 2528. [Google Scholar] [CrossRef] [PubMed]
- Guo, J.; Wang, Z.; Li, X.; Sun, C.; Gao, E.; Li, H. A comparison of the fracture resistances of endodontically treated mandibular premolars restored with endocrowns and glass fiber post-core retained conventional crowns. J. Adv. Prosthodont. 2016, 8, 489–493. [Google Scholar] [CrossRef] [PubMed]
- Magne, P. Composite resins and bonded porcelain: The postamalgam era? J. Calif. Dent. Assoc. 2006, 34, 135–147. [Google Scholar]
- Morimoto, S.; Rebello de Sampaio, F.B.; Braga, M.M.; Sesma, N.; Özcan, M. Survival rate of resin ceramic inlays, onlays and overlays: A systematic review and meta-analysis. J. Dent. Res. 2016, 95, 985–994. [Google Scholar] [CrossRef] [PubMed]
- Belleflamme, M.M.; Geerts, S.O.; Louwette, M.M.; Grenade, C.F.; Vanheusden, A.J.; Mainjot, A. No post-no core approach to restore severely damaged posterior teeth: An up to 10-year retrospective study of documented endocrown cases. J. Dent. 2017, 63, 1–7. [Google Scholar] [CrossRef] [PubMed]
- Shin, Y.; Park, S.; Park, J.-W.; Kim, K.-M.; Park, Y.-B.; Roh, B.-D. Evaluation of the marginal and internal discrepancies of CAD-CAM endocrowns with different cavity depths: An in vitro study. J. Prosthet. Dent. 2017, 117, 109–115. [Google Scholar] [CrossRef]
- Rocca, G.; Daher, R.; Saratti, C.; Sedláček, R.; Suchy, T.; Feilzer, A.; Krejci, I. Restoration of severely damaged endodontically treated premolars: The influence of the endo-core length on marginal integrity and fatigue resistance of lithium disilicate CAD-CAM ceramic endocrowns. J. Dent. 2018, 68, 41–50. [Google Scholar] [CrossRef] [PubMed]
- Bindl, A.; Mörmann, W.H. Clinical evaluation of adhesively placed Cerec endo-crowns after 2 years--preliminary results. J. Adhes. Dent. 1999, 1, 255–265. [Google Scholar]
- El-Damanhoury, H.; Haj-Ali, R.N.; Platt, J.A. Fracture Resistance and Microleakage of Endocrowns Utilizing Three CAD-CAM Blocks. Oper. Dent. 2015, 40, 201–210. [Google Scholar] [CrossRef] [PubMed]
- Lise, D.P.; Van Ende, A.; De Munck, J.; Suzuki, T.Y.U.; Vieira, L.C.C.; Van Meerbeek, B. Biomechanical behavior of endodontically treated premolars using different preparation designs and CAD/CAM materials. J. Dent. 2017, 59, 54–61. [Google Scholar] [CrossRef]
- Hassouneh, L.; Jum’Ah, A.A.; Ferrari, M.; Wood, D.J. Post-fatigue fracture resistance of premolar teeth restored with endocrowns: An in vitro investigation. J. Dent. 2020, 100, 103426. [Google Scholar] [CrossRef]
- El Ghoul, W.; Özcan, M.; Silwadi, M.; Salameh, Z. Fracture resistance and failure modes of endocrowns manufactured with different CAD/CAM materials under axial and lateral loading. J. Esthet. Restor. Dent. 2019, 31, 378–387. [Google Scholar] [CrossRef]
- Haralur, S.B.; Alamrey, A.A.; AlShehri, S.A.; Alzahrani, D.S.; Alfarsi, M. Effect of different preparation designs and all ceramic materials on fracture strength of molar endocrowns. J. Appl. Biomater. Funct. Mater. 2020, 18, 2280800020947329. [Google Scholar] [CrossRef]
- Schmidlin, P.R.; Stawarczyk, B.; DeAbreu, D.; Bindl, A.; Ender, A.; Ichim, I.P. Fracture resistance of endodontically treated teeth without ferrule using a novel H-shaped short post. Quintessence Int. 2015, 46, 97–109. [Google Scholar]
- Rocca, G.T.; Krejci, I. Bonded indirect restorations for posterior teeth: From cavity preparation to provisionalization. Quintessence Int. 2007, 38, 371–379. [Google Scholar]
- Zicari, F.; Van Meerbeek, B.; Scotti, R.; Naert, I. Effect of ferrule and post placement on fracture resistance of endodontically treated teeth after fatigue loading. J. Dent. 2013, 41, 207–215. [Google Scholar] [CrossRef]
- Rocca, G.T.; Krejci, I. Bonded indirect restorations for posterior teeth: The luting appointment. Quintessence Int. 2007, 38, 543–553. [Google Scholar]
- Attia, A.; Abdelaziz, K.; Freitag, S.; Kern, M. Fracture load of composite resin and feldspathic all-ceramic CAD/CAM crowns. J. Prosthet. Dent. 2006, 95, 117–123. [Google Scholar] [CrossRef]
- Samran, A.; Al-Afandi, M.; Kadour, J.-A.; Kern, M. Effect of ferrule location on the fracture resistance of crowned mandibular premolars: An in vitro study. J. Prosthet. Dent. 2015, 114, 86–91. [Google Scholar] [CrossRef] [PubMed]
- Lin, C.-L.; Chang, Y.-H.; Chang, C.-Y.; Pai, C.-A.; Huang, S.-F. Finite element and Weibull analyses to estimate failure risks in the ceramic endocrown and classical crown for endodontically treated maxillary premolar. Eur. J. Oral Sci. 2010, 118, 87–93. [Google Scholar] [CrossRef] [PubMed]
- Rocca, G.; Sedlakova, P.; Saratti, C.; Sedláček, R.; Gregor, L.; Rizcalla, N.; Feilzer, A.; Krejci, I. Fatigue behavior of resin-modified monolithic CAD–CAM RNC crowns and endocrowns. Dent. Mater. 2016, 32, e338–e350. [Google Scholar] [CrossRef]
- Magne, P.; Knezevic, A. Thickness of CAD–CAM composite resin overlays influences fatigue resistance of endodontically treated premolars. Dent. Mater. 2009, 25, 1264–1268. [Google Scholar] [CrossRef]
- Awada, A.; Nathanson, D. Mechanical properties of resin-ceramic CAD/CAM restorative materials. J. Prosthet. Dent. 2015, 114, 587–593. [Google Scholar] [CrossRef] [PubMed]
- Govare, N.; Contrepois, M. Endocrowns: A systematic review. J. Prosthet. Dent. 2020, 123, 411–418.e9. [Google Scholar] [CrossRef]
- Zahran, M.; El-Mowafy, O.; Tam, L.; Watson, P.A.; Finer, Y. Fracture Strength and Fatigue Resistance of All-Ceramic Molar Crowns Manufactured with CADCAM Technology. J. Prosthodont. 2008, 17, 370–377. [Google Scholar] [CrossRef]
- Chrepa, V.; Konstantinidis, I.; Kotsakis, G.A.; Mitsias, M.E. The survival of indirect composite resin onlays for the restoration of root filled teeth: A retrospective medium-term study. Int. Endod. J. 2014, 47, 967–973. [Google Scholar] [CrossRef]
- Sedrez-Porto, J.A.; Rosa, W.L.D.O.D.; da Silva, A.F.; Munchow, E.; Pereira-Cenci, T. Endocrown restorations: A systematic review and meta-analysis. J. Dent. 2016, 52, 8–14. [Google Scholar] [CrossRef]
- Lang, N.P.; Kiel, R.A.; Anderhalden, K. Clinical and microbiological effects of subgingival restorations with over-hanging or clinically perfect margins. J. Clin. Periodontol. 1983, 10, 563–578. [Google Scholar] [CrossRef]
| Group | Sample | Average (N) | SD | Minimum (N) | Maximum (N) | Range (N) |
|---|---|---|---|---|---|---|
| Group A (Control) | 10 | 859.61 | 267.951 | 515.4 | 1280.0 | 764.6 |
| Group B | 10 | 1053.9 | 333.985 | 628.0 | 1418.0 | 790.0 |
| Group C | 10 | 1124.6 | 291.172 | 525.0 | 1420.0 | 895.0 |
| Group D | 10 | 780.67 | 183.269 | 535.0 | 1077.0 | 542.0 |
| Total | 40 | 954.695 | 299.391 | 515.4 | 1420.0 | 904.6 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Barallat, L.; Arregui, M.; Fernandez-Villar, S.; Paniagua, B.; Pascual-La Rocca, A. Fracture Resistance in Non-Vital Teeth: Absence of Interproximal Ferrule and Influence of Preparation Depth in CAD/CAM Endocrown Overlays—An In Vitro Study. Materials 2022, 15, 436. https://doi.org/10.3390/ma15020436
Barallat L, Arregui M, Fernandez-Villar S, Paniagua B, Pascual-La Rocca A. Fracture Resistance in Non-Vital Teeth: Absence of Interproximal Ferrule and Influence of Preparation Depth in CAD/CAM Endocrown Overlays—An In Vitro Study. Materials. 2022; 15(2):436. https://doi.org/10.3390/ma15020436
Chicago/Turabian StyleBarallat, Lucía, María Arregui, Sandra Fernandez-Villar, Blanca Paniagua, and Andrés Pascual-La Rocca. 2022. "Fracture Resistance in Non-Vital Teeth: Absence of Interproximal Ferrule and Influence of Preparation Depth in CAD/CAM Endocrown Overlays—An In Vitro Study" Materials 15, no. 2: 436. https://doi.org/10.3390/ma15020436
APA StyleBarallat, L., Arregui, M., Fernandez-Villar, S., Paniagua, B., & Pascual-La Rocca, A. (2022). Fracture Resistance in Non-Vital Teeth: Absence of Interproximal Ferrule and Influence of Preparation Depth in CAD/CAM Endocrown Overlays—An In Vitro Study. Materials, 15(2), 436. https://doi.org/10.3390/ma15020436






