The Regenerative Potential of Decellularized Dental Pulp Extracellular Matrix: A Systematic Review
Abstract
:1. Introduction
2. Materials and Methods
2.1. Focused Question
2.2. Eligibility Criteria
2.3. Search of the Literature
2.4. Data Extraction
2.5. Quality Assessment of Studies
3. Results
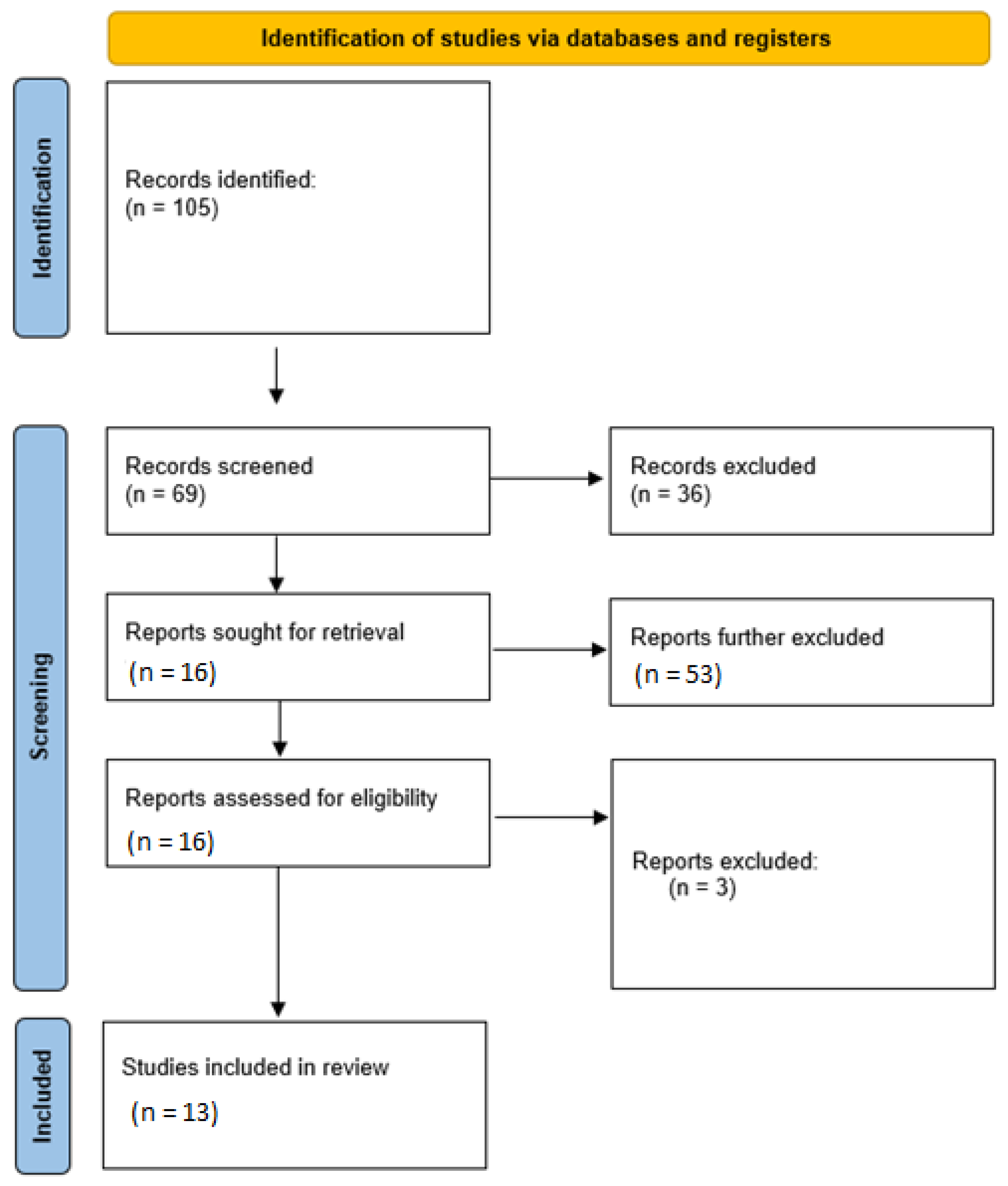
3.1. Literature Search Results
3.2. General Characteristics and Overall Outcomes of In Vitro and Ex Vivo Studies
3.3. General Characteristics and Overall Outcomes of Animal Studies
3.4. Results of Quality Assessment of In Vitro and Ex Vivo Studies
3.5. Results of Quality Assessment of Animal Studies
4. Discussion
5. Conclusions
Author Contributions
Funding
Data Availability Statement
Conflicts of Interest
References
- Carvalho, T.S.; Lussi, A. Age-Related Morphological, Histological and Functional Changes in Teeth. J. Oral Rehabil. 2017, 44, 291–298. [Google Scholar] [CrossRef] [PubMed]
- Coll, J.A.; Seale, N.S.; Vargas, K.; Marghalani, A.A.; Al Shamali, S.; Graham, L. Primary Tooth Vital Pulp Therapy: A Systematic Review and Meta-Analysis. Pediatric Dent. 2017, 39, 16–123. [Google Scholar]
- Asgary, S.; Eghbal, M.J. Treatment Outcomes of Pulpotomy in Permanent Molars with Irreversible Pulpitis Using Biomaterials: A Multi-Center Randomized Controlled Trial. Acta Odontol. Scand. 2013, 71, 130–136. [Google Scholar] [CrossRef]
- Khasnis, S.A.; Kidiyoor, K.H.; Patil, A.B.; Kenganal, S.B. Vertical Root Fractures and Their Management. J. Conserv. Dent. 2014, 17, 103. [Google Scholar] [CrossRef]
- Lee, H.; Han, W.; Kim, H.; Ha, D.-H.; Jang, J.; Kim, B.S.; Cho, D.-W. Development of Liver Decellularized Extracellular Matrix Bioink for Three-Dimensional Cell Printing-Based Liver Tissue Engineering. Biomacromolecules 2017, 18, 1229–1237. [Google Scholar] [CrossRef] [PubMed]
- Robertson, M.J.; Dries-Devlin, J.L.; Kren, S.M.; Burchfield, J.S.; Taylor, D.A. Optimizing Recellularization of Whole Decellularized Heart Extracellular Matrix. PLoS ONE 2014, 9, e90406. [Google Scholar] [CrossRef] [PubMed]
- Tan, Q.; Cao, Y.; Zheng, X.; Peng, M.; Huang, E.; Wang, J. BMP4-Regulated Human Dental Pulp Stromal Cells Promote Pulp-like Tissue Regeneration in a Decellularized Dental Pulp Matrix Scaffold. Odontology 2021, 109, 895–903. [Google Scholar] [CrossRef]
- Miller, E.K.; Lee, J.Y.; Tawil, P.Z.; Teixeira, F.B.; Vann, W.F. Emerging Therapies for the Management of Traumatized Immature Permanent Incisors. Pediatr. Dent. 2012, 34, 66–69. [Google Scholar]
- Wong, M.L.; Griffiths, L.G. Immunogenicity in Xenogeneic Scaffold Generation: Antigen Removal vs. Decellularization. Acta Biomater. 2014, 10, 1806–1816. [Google Scholar] [CrossRef]
- Ravindran, S.; Huang, C.-C.; George, A. Extracellular Matrix of Dental Pulp Stem Cells: Applications in Pulp Tissue Engineering Using Somatic MsCs. Front. Physiol. 2014, 4, 395. [Google Scholar] [CrossRef]
- Bakhtiar, H.; Pezeshki-Modaress, M.; Kiaipour, Z.; Shafiee, M.; Ellini, M.R.; Mazidi, A.; Rajabi, S.; Benisi, S.Z.; Ostad, S.N.; Galler, K.; et al. Pulp ECM-Derived Macroporous Scaffolds for Stimulation of Dental-Pulp Regeneration Process. Dent. Mater. 2019, 36, 76–87. [Google Scholar] [CrossRef]
- Khurshid, Z.; Alnaim, A.J.A.; Alhashim, A.A.A.; Imran, E.; Adanir, N. Future of Decellularized Dental Pulp Matrix in Regenerative Endodontics. Eur. J. Dent. 2022. [Google Scholar] [CrossRef]
- Bakhtiar, H.; Rajabi, S.; Pezeshki-Modaress, M.; Reza, M.; Ellini, M.R.; Panahinia, M.; Alijani, S.; Mazidi, A.; Kamali, A.; Azarpazhooh, A.; et al. Optimizing methods for Bovine Dental Pulp Decellularization. J. Endod. 2021, 47, 62–68. [Google Scholar] [CrossRef] [PubMed]
- Alqahtani, Q.; Zaky, S.; Patil, A.; Beniash, E.; Ray, H.; Sfeir, C. Decellularized Swine Dental Pulp Tissue for Regenerative Root Canal Therapy. J. Dent. Res. 2018, 97, 1460–1467. [Google Scholar] [CrossRef] [PubMed]
- Moher, D.; Altman, D.G.; Liberati, A.; Tetzlaff, J. PRISMA Statement. Epidemiology 2011, 22, 128. [Google Scholar] [CrossRef]
- Khurshid, Z.; Tariq, R.; Asiri, F.Y.; Abid, K.; Zafar, M.S. Literature Search Strategies in Dental Education and Research. J. Taibah Univ. Med. Sci. 2021, 16, 799–806. [Google Scholar] [CrossRef]
- Moher, D.; Schulz, K.F.; Altman, D.G.; Consort, G. The CONSORT Statement: Revised Recommendations for Improving the Quality of Reports of Parallel Group Randomised Trials; Elsevier: Amsterdam, The Netherlands, 2001. [Google Scholar]
- Percie du Sert, N.; Hurst, V.; Ahluwalia, A.; Alam, S.; Avey, M.T.; Baker, M.; Browne, W.J.; Clark, A.; Cuthill, I.C.; Durnagl, U.; et al. The ARRIVE Guidelines 2.0: Updated Guidelines for Reporting Animal Research. J. Cereb. Blood Flow Metab. 2020, 40, 1769–1777. [Google Scholar] [CrossRef]
- Faggion, C.M., Jr. Guidelines for Reporting Pre-Clinical In Vitro Studies on Dental Materials. J. Evid. Based Dent. Pract. 2012, 12, 182–189. [Google Scholar] [CrossRef] [PubMed]
- Matoug-Elwerfelli, M.; Duggal, M.S.; Nazzal, H.; Esteves, F.; Raïf, E. A Biocompatible Decellularized Pulp Scaffold for Regenerative Endodontics. Int. Endod. J. 2017, 51, 663–673. [Google Scholar] [CrossRef]
- Song, J.S.; Takimoto, K.; Jeon, M.; Vadakekalam, J.; Ruparel, N.B.; Diogenes, A. Decellularized Human Dental Pulp as a Scaffold for Regenerative Endodontics. J. Dent. Res. 2017, 96, 640–646. [Google Scholar] [CrossRef]
- Li, J.; Rao, Z.; Zhao, Y.; Xu, Y.; Chen, L.; Shen, Z.; Bai, Y.; Lin, Z.; Huang, Q. A Decellularized Matrix Hydrogel Derived from Hu-Man Dental Pulp Promotes Dental Pulp Stem Cell Proliferation, Migration, and Induced Multidirectional Differentiation In Vitro. J. Endod. 2020, 46, 1438–1447. [Google Scholar] [CrossRef] [PubMed]
- Alghutaimel, H.; Yang, X.; Drummond, B.; Nazzal, H.; Duggal, M.; Raïf, E. Investigating the Vascularization Capacity of a Decellularized Dental Pulp Matrix Seeded with Human Dental Pulp Stem Cells: In Vitro and Preliminary In Vivo Evaluations. Int. Endod. J. 2021, 54, 1300–1316. [Google Scholar] [CrossRef]
- Chen, G.; Chen, J.; Yang, B.; Li, L.; Luo, X.; Zhang, X.; Feng, L.; Jiang, Z.; Yu, M.; Guo, W.; et al. Combination of Aligned PLGA/Gelatin Electrospun Sheets, Native Dental Pulp Extracellular Matrix and Treated Dentin Matrix as Substrates for Tooth Root Regeneration. Biomaterials 2015, 52, 56–70. [Google Scholar] [CrossRef] [PubMed]
- Hu, L.; Gao, Z.; Xu, J.; Zhu, Z.; Fan, Z.; Zhang, C.; Wang, J.; Wang, S. Decellularized Swine Dental Pulp as a Bioscaffold for Pulp Regeneration. BioMed Res. Int. 2017, 2017, 9342714. [Google Scholar] [CrossRef] [PubMed]
- Lee, D.J.; Miguez, P.; Kwon, J.; Daniel, R.; Padilla, R.; Min, S.; Zalal, R.; Ko, C.-C.; Shin, H.W. Decellularized Pulp Matrix as Scaffold for Mesenchymal Stem Cell Mediated Bone Regeneration. J. Tissue Eng. 2020, 11, 2041731420981672. [Google Scholar] [CrossRef]
- Kim, I.-H.; Jeon, M.; Cheon, K.; Kim, S.H.; Jung, H.-S.; Shin, Y.; Kang, C.M.; Kim, S.-O.; Choi, H.-J.; Lee, H.-S.; et al. In Vivo Evaluation of Decellularized Human Tooth Scaffold for Dental Tissue Regeneration. Appl. Sci. 2021, 11, 8472. [Google Scholar] [CrossRef]
- Matoug-Elwerfelli, M.; Nazzal, H.; Raif, E.M.; Wilshaw, S.-P.; Esteves, F.; Duggal, M. Ex-Vivo Recellularisation and Stem Cell Differentiation of a Decellularised Rat Dental Pulp Matrix. Sci. Rep. 2020, 10, 21553. [Google Scholar] [CrossRef]
- Morotomi, T.; Washio, A.; Kitamura, C. Current and Future Options for Dental Pulp Therapy. Jpn. Dent. Sci. Rev. 2018, 55, 5–11. [Google Scholar] [CrossRef]
- Poornejad, N.; Schaumann, L.B.; Buckmiller, E.M.; Momtahan, N.; Gassman, J.R.; Ma, H.H.; Roeder, B.L.; Reynolds, P.R.; Cook, A.D. The Impact of Decellularization Agents on Renal Tissue Extracellular Matrix. J. Biomater. Appl. 2016, 31, 521–533. [Google Scholar] [CrossRef]
- Böer, U.; Lohrenz, A.; Klingenberg, M.; Pich, A.; Haverich, A.; Wilhelmi, M. The Effect of Detergent-Based Decellularization Procedures on Cellular Proteins and Immunogenicity in Equine Carotid Artery Grafts. Biomaterials 2011, 32, 9730–9737. [Google Scholar] [CrossRef]
- Dissanayaka, W.L.; Zhang, C. Scaffold-based and Scaffold-Free Strategies in Dental Pulp Regeneration. J. Endod. 2020, 46, S81–S89. [Google Scholar] [CrossRef] [PubMed]
- Najeeb, S.; Khurshid, Z.; Zafar, M.S.; Zohaib, S.; Siddiqui, F. Efficacy of Enamel Matrix Derivative in Vital Pulp Therapy: A Review of Literature. Iran. Endod. J. 2017, 12, 269–275. [Google Scholar] [CrossRef]
- Zhianmanesh, M.; Varmazyar, M.; Montazerian, H. Fluid Permeability of Graded Porosity Scaffolds Archi-Tectured with Minimal Surfaces. ACS Biomater. Sci. Eng. 2019, 5, 1228–1237. [Google Scholar] [CrossRef] [PubMed]
- Li, Z.; Liu, L.; Wang, L.; Song, D. The Effects and Potential Applications of Concentrated Growth Factor in Dentin–Pulp Complex Regeneration. Stem Cell Res. Ther. 2021, 12, 357. [Google Scholar] [CrossRef] [PubMed]
- Morse, D.R. Age-Related Changes of the Dental Pulp Complex and Their Relationship to Systemic Aging. Oral Surg. Oral Med. Oral Pathol. 1991, 72, 721–745. [Google Scholar] [CrossRef]
- Dereli Can, G.; Akcan, G.; Can, M.E.; Akdere, Ö.E.; Çaylı, S.; Şimşek, G.; Gümüşderelioğlu, M. Surgical and Immunohistochemical Outcomes of Scleral Reconstruction with Autogenic, Allogenic and Xenogenic Grafts: An Experimental Rabbit Model. Curr. Eye Res. 2020, 45, 1572–1582. [Google Scholar] [CrossRef]
| Study (Authors, Year) | Methodology | Sample Size (n) | Study Groups | Duration of Experiment(s) | Investigation(s) | Outcomes |
|---|---|---|---|---|---|---|
| Matoug-Elwerfelli et al., 2017 [20] | HDP-ECM applied on human dental pulp tissue | N = 12 | Cyanoacrylate glue (n = 4); Collagen gel (n = 4); ECM (n = 4) | 14 days | DNA quantification; IHC (nucleic acids, acidic polysaccharides and collagen); cell viability and toxicity assays | No difference between control and test groups. |
| Song et al., 2017 [21] | SCAP seeded in HDP-ECM produced by three different methods | Not stated | Protocol 1 Protocol 2 Protocol 3 Control | 2 weeks | Western blot; SEM; IHC; cell viability; Rt-PCR | HDP ECM increased proliferation of SCAP compared to controls. |
| Li et al., 2020 [22] | HDP cells seeded in HDP-ECM gel | Not stated | HDP cells in HDP-ECM gel HDP cells in collagen gel HDP cells in culture medium only | 7 days | Cell adhesion, migration, and proliferation; Odontoblastic differentiation; IHC; Western blotting; Rt-PCR | HDP-ECM gel promoted odontoblastic differentiation. |
| Bakhtiar et al., 2020 [11] | hBMMSC seeded in crosslinked bovine DP-ECM | Not stated | hBMMSCs in crosslinked and non-crosslinked Bovine DP-ECM hBMMSCs in culture medium only | 21 days | Proliferation and attachment assays; Rt-PCR | No statistical difference between groups. |
| Matoug-Elwerfelli et al., 2020 [28] | Rat DP-ECM recullarized with HDP cells. | n = 8 | Rat DP-HDP seeded with HDP cells (n = 4) Cellular rat dental pulp seeded with HDP (n = 4) | 14 days | Biocompatibility, LIVE/DEAD assay, immunohistology, odontoblast differentiation | Rat DP-ECM was able to support human pulp regeneration |
| Alghutaimel et al., 2021 [23] | HDPSCs cultured in DP-ECM | Not stated | HDPSCs + DP-ECM HDPSCs + Culture medium | 7 days | IHC (collagen type I, dentin matrix protein 1, dentin sialoprotein, and Von Willebrand); ELISA (transforming growth factor β, vascular endothelial growth factor, and basic fibroblast growth factor) | Increased proliferation and angiogenic factor expression when HDPSCs cultured in DP-ECM compared to medium only. |
| No. | Study (Author, Year) | Animal Model (n) | Source of DP-ECM | Methodology | Study Groups (n) | Duration | Investigations | Outcomes |
|---|---|---|---|---|---|---|---|---|
| 1 | Chen et al., 2015 [24] | Pig (n not stated) | Pig | Scaffold/TDM/DP-ECM/Scaffold + TDM + DP-ECM placed in transplanted roots | E-spun scaffolds Treated dentine matrix DP-ECM Scaffold + TDM + DP-ECM | 7 days | SEM; IHC; Histology | Scaffold + TDM + DP-ECM promoted regeneration of root and dental pulp tissues. |
| 2 | Hu et al., 2017 [25] | Pigs (n = 9); Immunodeficient mice (n not stated) | Pig | Seeding human dental pulp stem cells into swine decellularized pulp and transplanted subcutaneously into nude mice | Not stated | 8 weeks | SEM; H&E staining; IHC; | DP-ECM promoted pulpal regeneration in transplanted teeth. |
| 3 | Alqahtani et al., 2018 [14] | Beagle dogs (n = 2) | Pig | Porcine DP-ECM, collagen and blood clot alone compared with each other for pulpal regeneration in the root canal. | DP-ECM (n = 2 teeth) Collagen (n = 3 teeth) Blood clot (n = 3 teeth) | 8 weeks | Micro-CT; IHC (CD31 and DSP) | DP-ECM promoted pulp regeneration and angiogenesis more than collagen and blood clot. |
| 4 | Bakhtiar et al., 2020 [11] | Sprague Dawley rats (n = 24) | Bovine | Crosslinked and non-crosslinked bovine DP-ECM implanted subcutaneously. | Crosslinked Bovine DP-ECM
| 2 weeks | Histology and IHC | Cross-linked scaffolds degraded at a lower rate but produced lesser inflammation compared to non-crosslinked scaffolds. More angiogenesis observed in crosslinked group. |
| 5 | Lee et al., 2020 [26] | Rats (n = 6) | Human | HDP-ECM with and without BMMSCs implant into defects in calvaria | HDP-ECM only HDP-ECM + BMMSC | 12 weeks | Micro-CT and histology | Angiogenesis and bone formation observed in both groups |
| 6 | Alghutaimel et al., 2021 [23] | Immunodeficient mice (n not stated) | Human | HPDP-ECM with and without HDPSCs implanted subcutaneously. | HDP-ECM + HDPSCs HDP-ECM only No treatment n for each group not stated | 30 days | IHC; Histology | HDP-ECM + HDPSCs promoted the highest amount of angiogenesis |
| 7 | Bakhtiar et al., 2021 [13] | Sprague Dawley (n not stated) | Bovine | Bovine DP-ECM implanted subcutaneously. | Bovine DP-ECM | 2 weeks | Immune response | Immune response followed by angiogenesis and fibrous encapsulation. |
| 8 | Kim et al., 2021 [27] | Immunodeficient mice (n = 20) | Human | Human PDLSCs and DPSCs seeded on human DP-ECM transplanted subcutaneously. | HPDL-ECM + PDLSCs HDP-ECM + DPSCs HPDL-ECM HDP-ECM n for each group not stated. | 9 weeks | Histology; IHC | Pro-angiogenic and regenerative biomarkers detected. |
| 9 | Tan et al., 2021 [7] | Mice (n not stated) | Human | Human DPSCs and BMP-4 (via recombinant adenovirus) seeded on human DP-ECM transplanted subcutaneously. | PBS + DPSCs GFP + DPSCs DP-ECM + DPSCs BMP4 + DPSCs BMP4 + DP-ECM + DPSCs | 4 weeks | Gene expression; histology; IHC | BMP-4 promoted upregulation of the expression of osteogenic, odontogenic and angiogenic markers in DPSCs seeded on DP-ECM. |
| Assessment Item | Matoug-Elwerfelli et al., 2017 | Song et al., 2017 | Li et al., 2020 | Bakhtiar et al., 2020 | Matoug-Elwerfelli et al., 2020 | Alghutaimel et al., 2021 |
|---|---|---|---|---|---|---|
| 1. Introduction | ||||||
| Yes | Yes | Yes | Yes | Yes | Yes |
| Yes | Yes | Yes | Yes | Yes | Yes |
| 2. Replicable methods | Yes | Yes | Yes | Yes | Yes | Yes |
| 3. Adequate outcomes | Yes | Yes | Yes | Yes | Yes | Yes |
| 4. Predetermined sample size | No | No | No | No | No | No |
| 5. Allocation of samples | No | No | No | No | No | No |
| 6. Randomization | ||||||
| No | No | No | Yes | No | No |
| No | Yes | No | Yes | No | Yes |
| No | No | No | Yes | No | No |
| 7. Statistics | Yes | Yes | Yes | Yes | Yes | Yes |
| 8. Adequate outcomes & estimation | Yes | Yes | Yes | Yes | Yes | Yes |
| 9. Discussion: Limitations | No | No | No | No | No | No |
| 10. Funding | No | No | Yes | Yes | No | Yes |
| 11. Accessible protocol | No | No | No | No | No | No |
| Overall quality | Low | Medium | Medium | High | Low | Medium |
| Study Characteristics | Chen et al., 2015 | Hu et al., 2017 | Alqahtani et al., 2018 | Bakhtiar et al., 2020 | Lee et al., 2020 | Alghutaimel et al., 2021 | Bakhtiar et al., 2021 | Kim et al., 2021 | Tan et al., 2021 |
|---|---|---|---|---|---|---|---|---|---|
| Animal study identified in title | No | No | No | No | No | Yes | No | Yes | No |
| Abstract | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes |
| Introduction | |||||||||
| Adequate background | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes |
| Objectives/hypotheses described adequately | No | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes |
| Method | |||||||||
| Ethical statement | Yes | Yes | Yes | No | No | Yes | No | Yes | Yes |
| Blinding | No | No | No | Yes | No | No | Yes | No | No |
| Description of animal groups | No | Yes | Yes | Yes | Yes | No | Yes | No | Yes |
| Adequate experimental procedures | Yes | Yes | Yes | Yes | Yes | Yes | Yes | No | Yes |
| Experimental animal groups and controls | Yes | Yes | Yes | No | No | Yes | No | No | Yes |
| Housing details | No | No | No | No | No | No | No | No | No |
| Precalculated sample size | No | No | No | No | No | No | No | No | No |
| Randomization of teeth/animals | No | No | No | Only histological samples | No | Yes | Only histological samples | Only histological samples | No |
| Experimental outcomes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes |
| Statistics | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes |
| Results | |||||||||
| Baseline data | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes |
| Number analyzed/animals lost | No | No | Yes | No | No | No | No | No | No |
| Adequate outcomes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes |
| Reporting of adverse effects | No | No | No | No | No | No | No | No | No |
| Discussion | |||||||||
| Adequate interpretation of results | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes |
| Clinical implications | No | Yes | Yes | Yes | Yes | Yes | Yes | No | No |
| Funding information | Yes | Yes | Yes | Yes | No | Yes | Yes | Yes | Yes |
| Overall quality | Medium | Medium | Medium | Medium | Medium | High | Medium | Medium | Medium |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Adanir, N.; Khurshid, Z.; Ratnayake, J. The Regenerative Potential of Decellularized Dental Pulp Extracellular Matrix: A Systematic Review. Materials 2022, 15, 6386. https://doi.org/10.3390/ma15186386
Adanir N, Khurshid Z, Ratnayake J. The Regenerative Potential of Decellularized Dental Pulp Extracellular Matrix: A Systematic Review. Materials. 2022; 15(18):6386. https://doi.org/10.3390/ma15186386
Chicago/Turabian StyleAdanir, Necdet, Zohaib Khurshid, and Jithendra Ratnayake. 2022. "The Regenerative Potential of Decellularized Dental Pulp Extracellular Matrix: A Systematic Review" Materials 15, no. 18: 6386. https://doi.org/10.3390/ma15186386
APA StyleAdanir, N., Khurshid, Z., & Ratnayake, J. (2022). The Regenerative Potential of Decellularized Dental Pulp Extracellular Matrix: A Systematic Review. Materials, 15(18), 6386. https://doi.org/10.3390/ma15186386








