Evaluation of the Shear Bond Strength of Four Bioceramic Materials with Different Restorative Materials and Timings
Abstract
1. Introduction
2. Materials and Methods
2.1. Specimen Preparation
2.2. Materials Placement
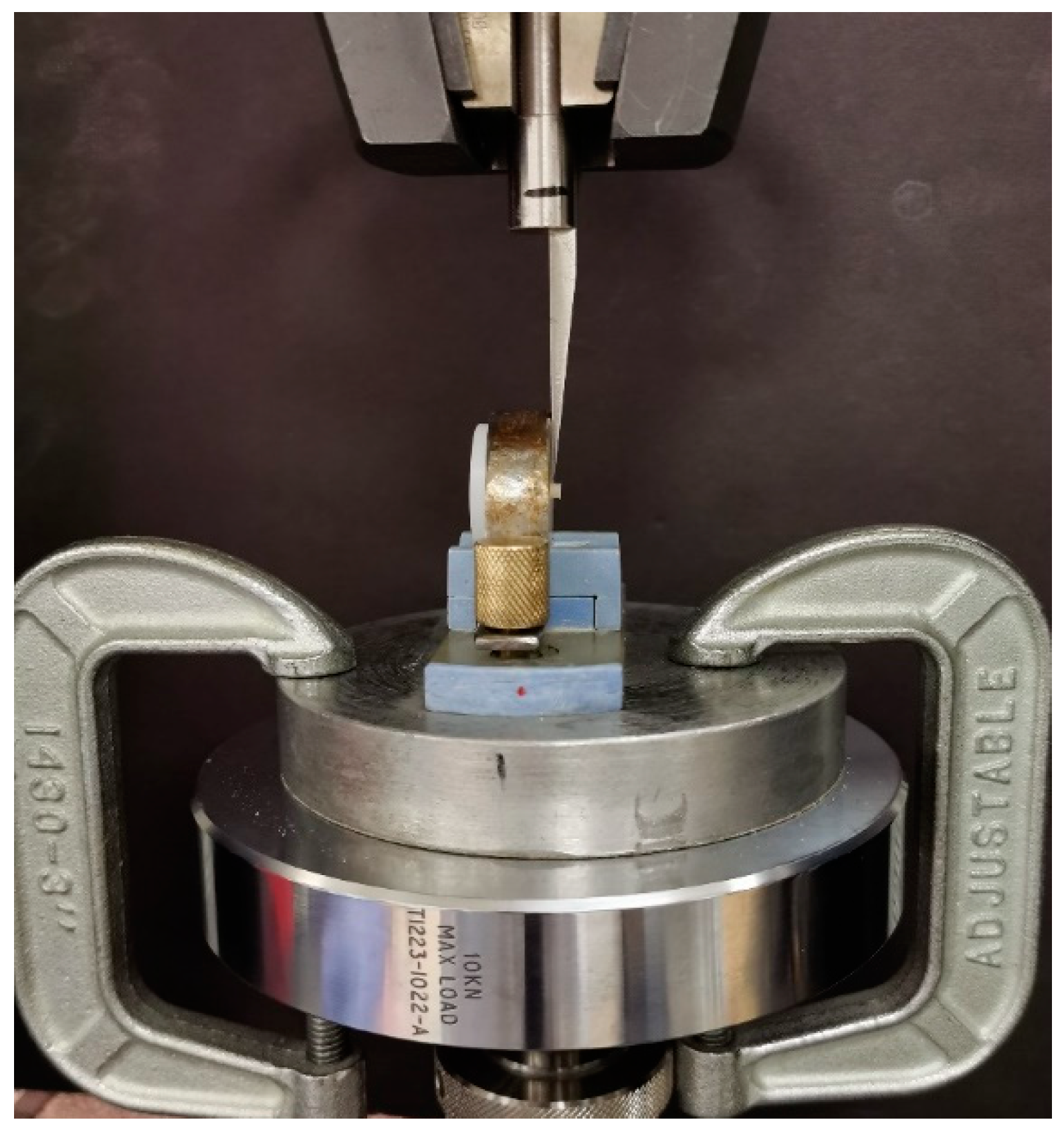
2.3. Shear Bond Strength Test
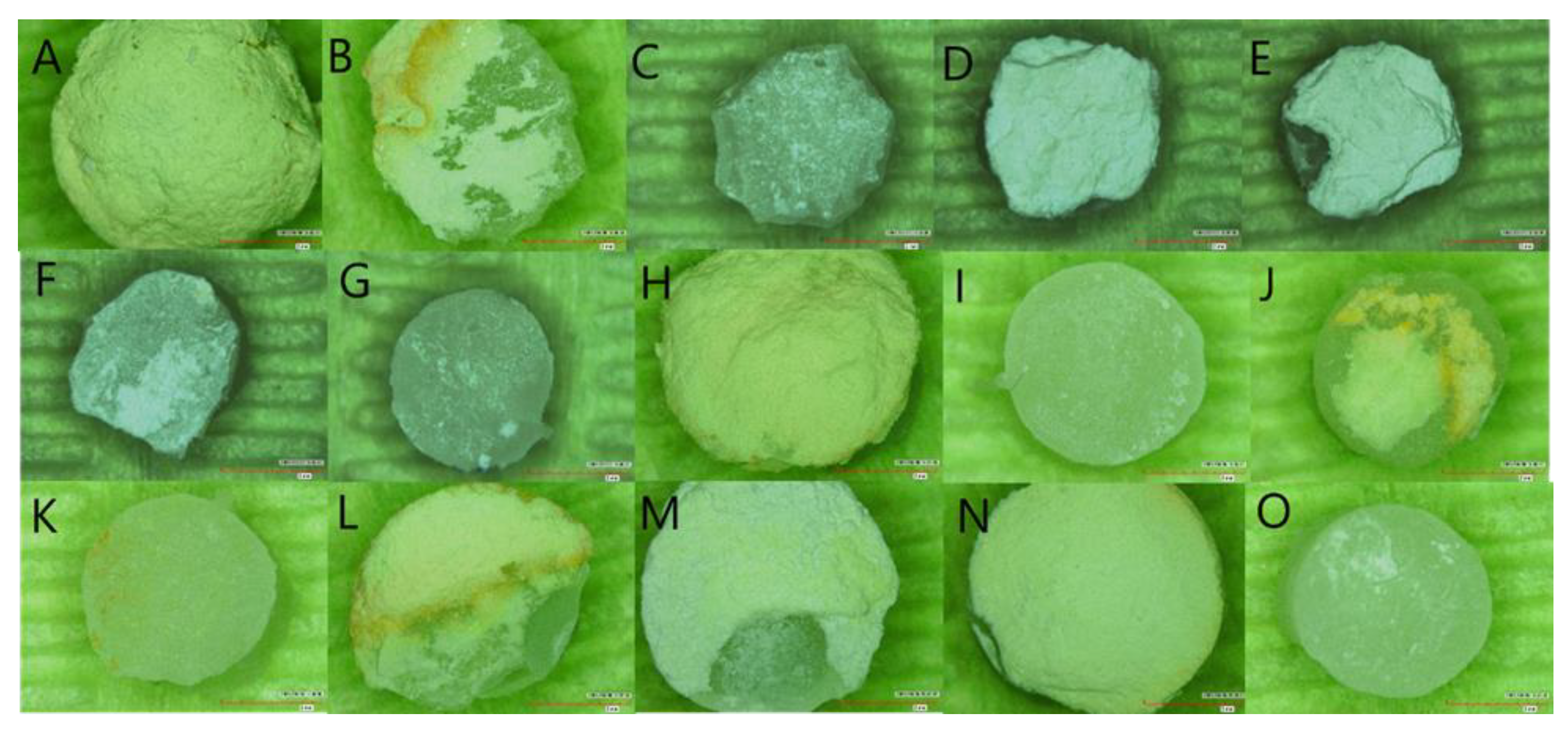
2.4. Fracture Analysis
2.5. Sample Size Calculation and Statistical Analysis
3. Results
4. Discussion
5. Conclusions
- The mean SBS of RC to the bioceramic materials was significantly higher than RMGI except for ProRoot MTA;
- The mean SBS of RC and RMGI to MTA groups was significantly higher than that of premixed bioceramics;
- The SBS of delayed RC was significantly higher than that of immediate timing in all bioceramic materials;
- The SBS of delayed RMGI was significantly higher than immediate timing in the premixed bioceramic groups, whereas the SBS of immediate RMGI placement over MTA was statistically higher than that of delayed timing.
Author Contributions
Funding
Institutional Review Board Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Davaie, S.; Hooshmand, T.; Ansarifard, S. Different Types of Bioceramics as Dental Pulp Capping Materials: A Systematic Review. Ceram. Int. 2021, 47, 20781–20792. [Google Scholar] [CrossRef]
- Parirokh, M.; Torabinejad, M.; Dummer, P.M.H. Mineral Trioxide Aggregate and Other Bioactive Endodontic Cements: An Updated Overview—Part I: Vital Pulp Therapy. Int. Endod. J. 2018, 51, 177–205. [Google Scholar] [CrossRef] [PubMed]
- Torabinejad, M.; Parirokh, M.; Dummer, P.M.H. Mineral Trioxide Aggregate and Other Bioactive Endodontic Cements: An Updated Overview—Part II: Other Clinical Applications and Complications. Int. Endod. J. 2018, 51, 284–317. [Google Scholar] [CrossRef]
- Lin, P.Y.; Chen, H.S.; Wang, Y.H.; Tu, Y.K. Primary Molar Pulpotomy: A Systematic Review and Network Meta-Analysis. J. Dent. 2014, 42, 1060–1077. [Google Scholar] [CrossRef] [PubMed]
- Shirvani, A.; Asgary, S. Mineral Trioxide Aggregate versus Formocresol Pulpotomy: A Systematic Review and Meta-Analysis of Randomized Clinical Trials. Clin. Oral Investig. 2014, 18, 1023–1030. [Google Scholar] [CrossRef] [PubMed]
- Coll, J.A.; Seale, N.S.; Vargas, K.; Marghalani, A.A.; Al Shamali, S.; Graham, L. Primary Tooth Vital Pulp Therapy: A Systematic Review and Meta-Analysis. Pediatr. Dent. 2017, 39, 16–123. [Google Scholar] [PubMed]
- Marghalani, A.A.; Omar, S.; Chen, J.W. Clinical and Radiographic Success of Mineral Trioxide Aggregate Compared with Formocresol as a Pulpotomy Treatment in Primary Molars: A Systematic Review and Meta-Analysis. J. Am. Dent. Assoc. 2014, 145, 714–721. [Google Scholar] [CrossRef]
- Asgary, S.; Shirvani, A.; Fazlyab, M. MTA and Ferric Sulfate in Pulpotomy Outcomes of Primary Molars: A Systematic Review and Meta-Analysis. J. Clin. Pediatr. Dent. 2014, 39, 1–8. [Google Scholar] [CrossRef]
- Camilleri, J. Color Stability of White Mineral Trioxide Aggregate in Contact with Hypochlorite Solution. J. Endod. 2014, 40, 436–440. [Google Scholar] [CrossRef]
- Marciano, M.A.; Duarte, M.A.H.; Camilleri, J. Dental Discoloration Caused by Bismuth Oxide in MTA in the Presence of Sodium Hypochlorite. Clin. Oral Investig. 2015, 19, 2201–2209. [Google Scholar] [CrossRef]
- Parirokh, M.; Torabinejad, M. Mineral Trioxide Aggregate: A Comprehensive Literature Review-Part I: Chemical, Physical, and Antibacterial Properties. J. Endod. 2010, 36, 16–27. [Google Scholar] [CrossRef]
- Watts, J.D.; Holt, D.M.; Beeson, T.J.; Kirkpatrick, T.C.; Rutledge, R.E. Effects of PH and Mixing Agents on the Temporal Setting of Tooth-Colored and Gray Mineral Trioxide Aggregate. J. Endod. 2007, 33, 970–973. [Google Scholar] [CrossRef] [PubMed]
- Boutsioukis, C.; Noula, G.; Lambrianidis, T. Ex Vivo Study of the Efficiency of Two Techniques for the Removal of Mineral Trioxide Aggregate Used as a Root Canal Filling Material. J. Endod. 2008, 34, 1239–1242. [Google Scholar] [CrossRef] [PubMed]
- Eren, S.K.; Örs, S.A.; Aksel, H.; Canay, Ş.; Karasan, D. Effect of Irrigants on the Color Stability, Solubility, and Surface Characteristics of Calcium-Silicate Based Cements. Restor. Dent. Endod. 2022, 47, e10. [Google Scholar] [CrossRef] [PubMed]
- Metlerska, J.; Fagogeni, I.; Metlerski, M.; Nowicka, A. Vital Pulp Therapy in Aesthetic Zone-Identifying the Biomaterial That Reduces the Risk of Tooth Discolouration. Materials 2021, 14, 6026. [Google Scholar] [CrossRef]
- Camilleri, J. Staining Potential of Neo MTA Plus, MTA Plus, and Biodentine Used for Pulpotomy Procedures. J. Endod. 2015, 41, 1139–1145. [Google Scholar] [CrossRef]
- Alsanouni, M.; Bawazir, O.A. A Randomized Clinical Trial of NeoMTA Plus in Primary Molar Pulpotomies. Pediatr. Dent. 2019, 41, 107–111. [Google Scholar]
- Keskin, C.; Sarıyılmaz, E. Color Stability of NeoMTA Plus and MTA Plus When Mixed with Anti-Washout Gel or Distilled Water. Meandros Med. Dent. J. 2018, 19, 296–301. [Google Scholar] [CrossRef]
- Ree, M.; Schwartz, R. Clinical Applications of Bioceramic Materials in Endodontics Endodontic Practice US. Endod. Pract. 2014, 7, 32–40. [Google Scholar]
- Motwani, N.; Ikhar, A.; Nikhade, P.; Chandak, M.; Rathi, S.; Dugar, M.; Rajnekar, R. Premixed Bioceramics: A Novel Pulp Capping Agent. J. Conserv. Dent. 2021, 24, 124–129. [Google Scholar] [CrossRef]
- Debelian, G.; Trope, M. ScienceDirect the Use of Premixed Bioceramic Materials in Endodontics. G. Ital. Endod. 2016, 30, 70–80. [Google Scholar] [CrossRef]
- Malhotra, S. Bioceramic Technology in Endodontics. Br. J. Med. Med. Res. 2014, 4, 2446–2454. [Google Scholar] [CrossRef]
- El-Sherif, S.M.; Sherief, D.I.; El-Refai, D.A. Evaluation of the PH, Calcium Ion Release, and Antibacterial Effect of a Premixed Bioceramic Endodontic Sealer. Gen. Dent. 2022, 70, 40–44. [Google Scholar]
- van Meerbeek, B.; Peumans, M.; Poitevin, A.; Mine, A.; van Ende, A.; Neves, A.; de Munck, J. Relationship between Bond-Strength Tests and Clinical Outcomes. Dent. Mater. 2010, 26, 100–121. [Google Scholar] [CrossRef]
- Keswani, D.; Pandey, R.K.; Ansari, A.; Gupta, S. Comparative Evaluation of Platelet-Rich Fibrin and Mineral Trioxide Aggregate as Pulpotomy Agents in Permanent Teeth with Incomplete Root Development: A Randomized Controlled Trial. J. Endod. 2014, 40, 599–605. [Google Scholar] [CrossRef] [PubMed]
- Eid, A.; Mancino, D.; Rekab, M.S.; Haikel, Y.; Kharouf, N. Effectiveness of Three Agents in Pulpotomy Treatment of Permanent Molars with Incomplete Root Development: A Randomized Controlled Trial. Healthcare 2022, 10, 431. [Google Scholar] [CrossRef] [PubMed]
- Careddu, R.; Duncan, H.F. A Prospective Clinical Study Investigating the Effectiveness of Partial Pulpotomy after Relating Preoperative Symptoms to a New and Established Classification of Pulpitis. Int Endod. J. 2021, 54, 2156–2172. [Google Scholar] [CrossRef]
- Abuelniel, G.M.; Duggal, M.S.; Kabel, N. A Comparison of MTA and Biodentine as Medicaments for Pulpotomy in Traumatized Anterior Immature Permanent Teeth: A Randomized Clinical Trial. Dent. Traumatol. Off. Publ. Int. Assoc. Dent. Traumatol. 2020, 36, 400–410. [Google Scholar] [CrossRef]
- Tunç, E.Ş.; Sönmez, I.S.; Bayrak, Ş.; Eǧilmez, T. The Evaluation of Bond Strength of a Composite and a Compomer to White Mineral Trioxide Aggregate with Two Different Bonding Systems. J. Endod. 2008, 34, 603–605. [Google Scholar] [CrossRef]
- Sindi, A.S. An In Vitro Study to Assess the Effectiveness of the Shear Bond Strength of Mineral Trioxide Aggregate with Different Adhesive Systems. J. Pharm. Bioallied Sci. 2021, 13, S672–S675. [Google Scholar] [CrossRef]
- Tulumbaci, F.; Almaz, M.E.; Arikan, V.; Mutluay, M.S. Shear Bond Strength of Different Restorative Materials to Mineral Trioxide Aggregate and Biodentine. J. Conserv. Dent. 2017, 20, 292–296. [Google Scholar] [CrossRef] [PubMed]
- Doozaneh, M.; Koohpeima, F.; Firouzmandi, M.; Abbassiyan, F. Shear Bond Strength of Self-Adhering Flowable Composite and Resin-Modified Glass Ionomer to Two Pulp Capping Materials. Iran. Endod. J. 2017, 12, 103–107. [Google Scholar] [CrossRef]
- Alhowaish, L.; Salama, F.; Al-Harbi, M.; Abumoatti, M. Shear Bond Strength of a Resin Composite to Six Pulp Capping Materials Used in Primary Teeth. J. Clin. Pediatr. Dent. 2020, 44, 234–239. [Google Scholar] [CrossRef] [PubMed]
- Hursh, K.A.; Kirkpatrick, T.C.; Cardon, J.W.; Brewster, J.A.; Black, S.W.; Himel, V.T.; Sabey, K.A. Shear Bond Comparison between 4 Bioceramic Materials and Dual-Cure Composite Resin. J. Endod. 2019, 45, 1378–1383. [Google Scholar] [CrossRef] [PubMed]
- Ajami, A.A.; Jafari Navimipour, E.; Savadi Oskoee, S.; Abed Kahnamoui, M.; Lotfi, M.; Daneshpooy, M. Comparison of Shear Bond Strength of Resin-Modified Glass Ionomer and Composite Resin to Three Pulp Capping Agents. J. Dent. Res. Dent. Clin. Dent. Prospect. 2013, 7, 164–168. [Google Scholar] [CrossRef]
- Oskoee, S.S.; Kimyai, S.; Bahari, M.; Eghbal, P.M.M.J.; Asgary, S. Comparison of Shear Bond Strength of Calcium-Enriched Mixture Cement and Mineral Trioxide Aggregate to Composite Resin. J. Contemp. Dent. Pract. 2011, 12, 457–462. [Google Scholar] [CrossRef] [PubMed]
- Nagi, S.M.; Omar, N.; Salem, H.N.; Aly, Y. Effect of Different Surface Treatment Protocols on the Shear Bond Strength of Perforation Repair Materials to Resin Composite. J. Adhes. Sci. Technol. 2020, 34, 417–426. [Google Scholar] [CrossRef]
- Samimi, P.; Kazemian, M.; Shirban, F.; Alaei, S.; Khoroushi, M. Bond Strength of Composite Resin to White Mineral Trioxide Aggregate: Effect of Different Surface Treatments. J. Conserv. Dent. 2018, 21, 350–353. [Google Scholar] [CrossRef]
- Palma, P.J.; Marques, J.A.; Antunes, M.; Falacho, R.I.; Sequeira, D.; Roseiro, L.; Santos, J.M.; Ramos, J.C. Effect of Restorative Timing on Shear Bond Strength of Composite Resin/Calcium Silicate–Based Cements Adhesive Interfaces. Clin. Oral Investig. 2020, 25, 3131–3139. [Google Scholar] [CrossRef]
- Tsujimoto, M.; Tsujimoto, Y.; Ookubo, A.; Shiraishi, T.; Watanabe, I.; Yamada, S.; Hayashi, Y. Timing for Composite Resin Placement on Mineral Trioxide Aggregate. J. Endod. 2013, 39, 1167–1170. [Google Scholar] [CrossRef]
- Palma, P.J.; Marques, J.A.; Falacho, R.I.; Vinagre, A.; Santos, J.M.; Ramos, J.C. Does Delayed Restoration Improve Shear Bond Strength of Different Restorative Protocols to Calcium Silicate-Based Cements? Materials 2018, 11, 2216. [Google Scholar] [CrossRef] [PubMed]
- von Fraunhofer, J.A. Adhesion and Cohesion. Int J. Dent. 2012, 2012, 951324. [Google Scholar] [CrossRef] [PubMed]
- Kayahan, M.B.; Nekoofar, M.H.; Kazandağ, M.; Canpolat, C.; Malkondu, O.; Kaptan, F.; Dummer, P.M.H. Effect of Acid-Etching Procedure on Selected Physical Properties of Mineral Trioxide Aggregate. Int. Endod. J. 2009, 42, 1004–1014. [Google Scholar] [CrossRef] [PubMed]
- Al-Homaidhi, M. Shear Bond Strength of an Endodontic Tricalcium Silicate- Based Putty to Different Adhesive Systems at Different Time Intervals. J. Res. Med. Dent. Sci. 2021, 9, 149–153. [Google Scholar]
- Torabinejad, M.; Chivian, N. Clinical Applications of Mineral Trioxide Aggregate. J. Endod. 1999, 25, 197–205. [Google Scholar] [CrossRef]
- Hidari, T.; Takamizawa, T.; Imai, A.; Hirokane, E.; Ishii, R.; Tsujimoto, A.; Suzuki, T.; Miyazaki, M. Role of the Functional Monomer 10-Methacryloyloxydecyl Dihydrogen Phosphate in Dentin Bond Durability of Universal Adhesives in Etch-&-Rinse Mode. Dent. Mater. J. 2020, 39, 616–623. [Google Scholar] [CrossRef]
- Chang, S.-W. Chemical Characteristics of Mineral Trioxide Aggregate and Its Hydration Reaction. Restor. Dent. Endod. 2012, 37, 188–193. [Google Scholar] [CrossRef]
- Eid, A.A.; Komabayashi, T.; Watanabe, E.; Shiraishi, T.; Watanabe, I. Characterization of the Mineral Trioxide Aggregate-Resin Modified Glass Ionomer Cement Interface in Different Setting Conditions. J. Endod. 2012, 38, 1126–1129. [Google Scholar] [CrossRef]
- Kaup, M.; Dammann, C.H.; Schäfer, E.; Dammaschke, T. Shear Bond Strength of Biodentine, ProRoot MTA, Glass Ionomer Cement and Composite Resin on Human Dentine Ex Vivo. Head Face Med. 2015, 11, 14. [Google Scholar] [CrossRef]
- Davidson, C.L.; de Gee, A.J.; Feilzer, A. The Competition between the Composite-Dentin Bond Strength and the Polymerization Contraction Stress. J. Dent. Res. 1984, 63, 1396–1399. [Google Scholar] [CrossRef]
- Teixeira, C.S.; Chain, M.C. Evaluation of Shear Bond Strength between Self-Etching Adhesive Systems and Dentin and Analysis of the Resin-Dentin Interface. Gen. Dent. 2010, 58, e52–e61. [Google Scholar] [PubMed]
- Triolo, P.T.J.; Swift, E.J.J.; Barkmeier, W.W. Shear Bond Strengths of Composite to Dentin Using Six Dental Adhesive Systems. Oper. Dent. 1995, 20, 46–50. [Google Scholar] [PubMed]
- Hardan, L.; Mancino, D.; Bourgi, R.; Alvarado-Orozco, A.; Rodríguez-Vilchis, L.E.; Flores-Ledesma, A.; Cuevas-Suárez, C.E.; Lukomska-Szymanska, M.; Eid, A.; Danhache, M.-L.; et al. Bond Strength of Adhesive Systems to Calcium Silicate-Based Materials: A Systematic Review and Meta-Analysis of In Vitro Studies. Gels 2022, 8, 311. [Google Scholar] [CrossRef] [PubMed]
- Ballini, A.; Mastrangelo, F.; Gastaldi, G.; Tettamanti, L.; Bukvic, N.; Cantore, S.; Cocco, T.; Saini, R.; Desiate, A.; Gherlone, E.; et al. Osteogenic Differentiation and Gene Expression of Dental Pulp Stem Cells under Low-Level Laser Irradiation: A Good Promise for Tissue Engineering. J. Biol. Regul. Homeost. Agents 2015, 29, 813–822. [Google Scholar] [PubMed]
- Tetè, G.; D’Orto, B.; Nagni, M.; Agostinacchio, M.; Polizzi, E.; Agliardi, E. Role of Induced Pluripotent Stem Cells (IPSCS) in Bone Tissue Regeneration in Dentistry: A Narrative Review. J. Biol. Regul. Homeost. Agents 2020, 34 (Suppl. S3), 1–10. [Google Scholar]
| Bioceramic Materials | Restorative Materials | |||
|---|---|---|---|---|
| Filtek™ Z350 XT Flowable | GC Fuji II LC® | |||
| Immediate | Delayed | Immediate | Delayed | |
| ProRoot® MTA (n = 40) | 10 | 10 | 10 | 10 |
| NeoMTA 2® (n = 40) | 10 | 10 | 10 | 10 |
| TotalFill® BC RRM™ Fast Set Putty (n = 40) | 10 | 10 | 10 | 10 |
| NeoPUTTY® (n = 40) | 10 | 10 | 10 | 10 |
| Total = 160 | 40 | 40 | 40 | 40 |
| 80 | 80 | |||
| Bioceramic | Manufacturer | Composition | Application |
|---|---|---|---|
| ProRoot® MTA (Mineral Trioxide Aggregate) | DENTSPLY, Tulsa, OK, USA | Bismuth oxide, tricalcium silicate, dicalcium silicate, calcium dialuminate, and calcium sulfate dehydrated | Mixed powder/liquid ratio: 1/3 |
| NeoMTA 2® (Mineral Trioxide Aggregate) | Nusmile Inc., Houston, TX; USA | Powder and gel system consisting of an extremely fine, inorganic powder of tricalcium and dicalcium silicate, which is mixed with the water-based gel | Mix 1 scoop (0.05 gm or 0.1 gm) of powder with one or two drops of gel. |
| TotalFill® BC RRM™ Fast Set Putty | FKG Dentaire SA, La Chaux-de-Fonds, Switzerland | Calcium silicate, zirconium oxide, tantalum oxide, calcium phosphate monobasic, and fillers | Pre-mixed material and ready to apply |
| NeoPUTTY® | Nusmile Inc., Houston, TX; USA | Bioactive paste consisting of an extremely fine, inorganic powder of tricalcium/dicalcium silicate in an organic medium | Pre-mixed material and ready to apply |
| Restoration | Bioceramics | p-Value * | ||||
|---|---|---|---|---|---|---|
| ProRoot MTA | NeoMTA2 | TotalFill | NeoPUTTY | |||
| Filtek™ Z350 XT | Mean ± SD | 7.64 ± 1.82 a | 8.57 ± 1.84 a | 4.38 ± 0.65 b | 4.04 ± 0.93 b | <0.001 |
| GC Fuji II LC® | Mean ± SD | 7.18 ± 2.60 a | 4.15 ± 0.35 b | 1.54 ± 0.18 c | 1.62 ± 0.12 c | <0.001 |
| p-value ** | 0.655 | 0.001 | <0.001 | 0.002 | ||
| Restoration | Bioceramic | Immediate (Mean ± SD) | Delayed (Mean ± SD) | p-Value |
|---|---|---|---|---|
| Filtek™ Z350 XT | ProRoot MTA | 7.64 ± 1.82 | 14.65 ± 0.95 | <0.001 |
| NeoMTA2 | 8.57 ± 1.84 | 12.01 ± 3.01 | 0.006 | |
| TotalFill | 4.38 ± 0.65 | 13.66 ± 3.81 | 0.002 | |
| NeoPUTTY | 4.04 ± 0.93 | 8.03 ± 1.82 | <0.001 | |
| GC Fuji II LC® | ProRoot MTA | 7.18 ± 2.60 | 3.33 ± 1.12 | 0.001 |
| NeoMTA2 | 4.15 ± 0.35 | 2.31 ± 1.35 | 0.002 | |
| TotalFill | 1.54 ± 0.18 | 2.57 ± 0.23 | <0.001 | |
| NeoPUTTY | 1.62 ± 0.12 | 3.27 ± 0.44 | <0.001 |
| Bioceramic | Restoration | Timing | Failure Type | ||
|---|---|---|---|---|---|
| Cohesive within Bioceramic | Adhesive | Mixed | |||
| ProRoot MTA | Filtek™ Z350 XT | Immediate | 80% (8/10) | 0 | 20% (2/10) |
| Delayed | 50% (5/10) | 0 | 50% (5/10) | ||
| GC Fuji II LC® | Immediate | 20% (2/10) | 20% (2/10) | 60% (6/10) | |
| Delayed | 10% (1/10) | 0 | 60% (6/10) | ||
| NeoMTA2® | Filtek™ Z350 XT | Immediate | 30% (3/10) | 20% (2/10) | 70% (5/10) |
| Delayed | 50% (5/10) | 0 | 50% (5/10) | ||
| GC Fuji II LC® | Immediate | 60% (6/10) | 0 | 40% (4/10) | |
| Delayed | 10% (1/10) | 10% (1/10) | 80% (8/10) | ||
| TotalFill® BC RRM™ Fast Set Putty | Filtek™ Z350 XT | Immediate | 40% (4/10) | 0 | 60% (6/10) |
| Delayed | 100% (10/10) | 0 | 0 | ||
| GC Fuji II LC® | Immediate | 0 | 40% (4/10) | 60% (6/10) | |
| Delayed | 10% (1/10) | 40% (4/10) | 50% (5/10) | ||
| NeoPUTTY® | Filtek™ Z350 XT | Immediate | 80% (8/10) | 0 | 20% (2/10) |
| Delayed | 70% (7/10) | 0 | 30% (3/10) | ||
| GC Fuji II LC® | Immediate | 90% (9/10) | 0 | 10% (1/10) | |
| Delayed | 20% (2/10) | 40% (4/10) | 40% (4/10) | ||
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Alqahtani, A.S.; Sulimany, A.M.; Alayad, A.S.; Alqahtani, A.S.; Bawazir, O.A. Evaluation of the Shear Bond Strength of Four Bioceramic Materials with Different Restorative Materials and Timings. Materials 2022, 15, 4668. https://doi.org/10.3390/ma15134668
Alqahtani AS, Sulimany AM, Alayad AS, Alqahtani AS, Bawazir OA. Evaluation of the Shear Bond Strength of Four Bioceramic Materials with Different Restorative Materials and Timings. Materials. 2022; 15(13):4668. https://doi.org/10.3390/ma15134668
Chicago/Turabian StyleAlqahtani, Abeer S., Ayman M. Sulimany, Abdullah S. Alayad, Abdulaziz S. Alqahtani, and Omar A. Bawazir. 2022. "Evaluation of the Shear Bond Strength of Four Bioceramic Materials with Different Restorative Materials and Timings" Materials 15, no. 13: 4668. https://doi.org/10.3390/ma15134668
APA StyleAlqahtani, A. S., Sulimany, A. M., Alayad, A. S., Alqahtani, A. S., & Bawazir, O. A. (2022). Evaluation of the Shear Bond Strength of Four Bioceramic Materials with Different Restorative Materials and Timings. Materials, 15(13), 4668. https://doi.org/10.3390/ma15134668






