Foot Orthosis and Sensorized House Slipper by 3D Printing
Abstract
1. Introduction
- For patient-specific data acquisition, 3D scanning of the foot was compared to traditional casting (plaster slipper cast in neutral position).
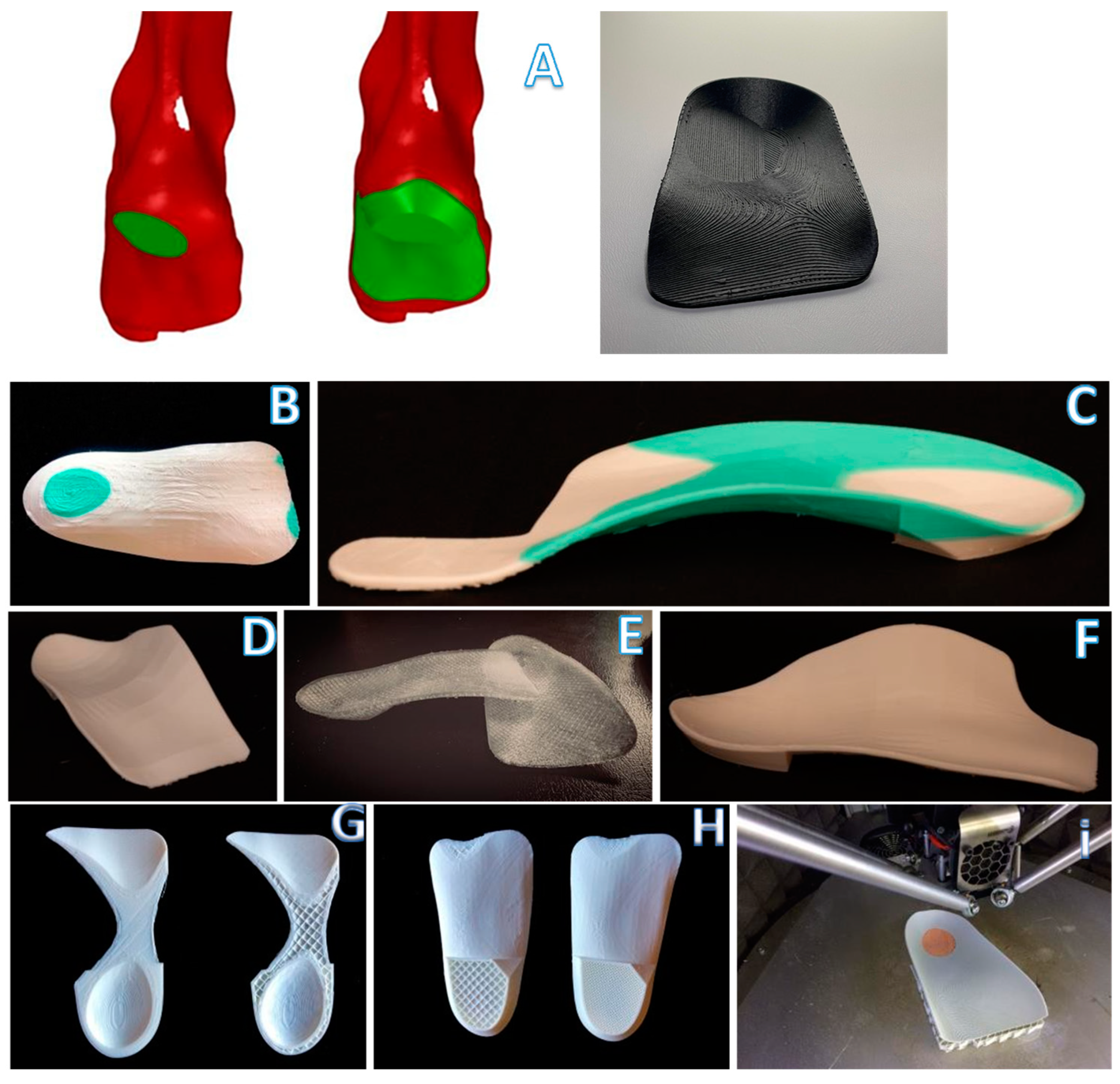
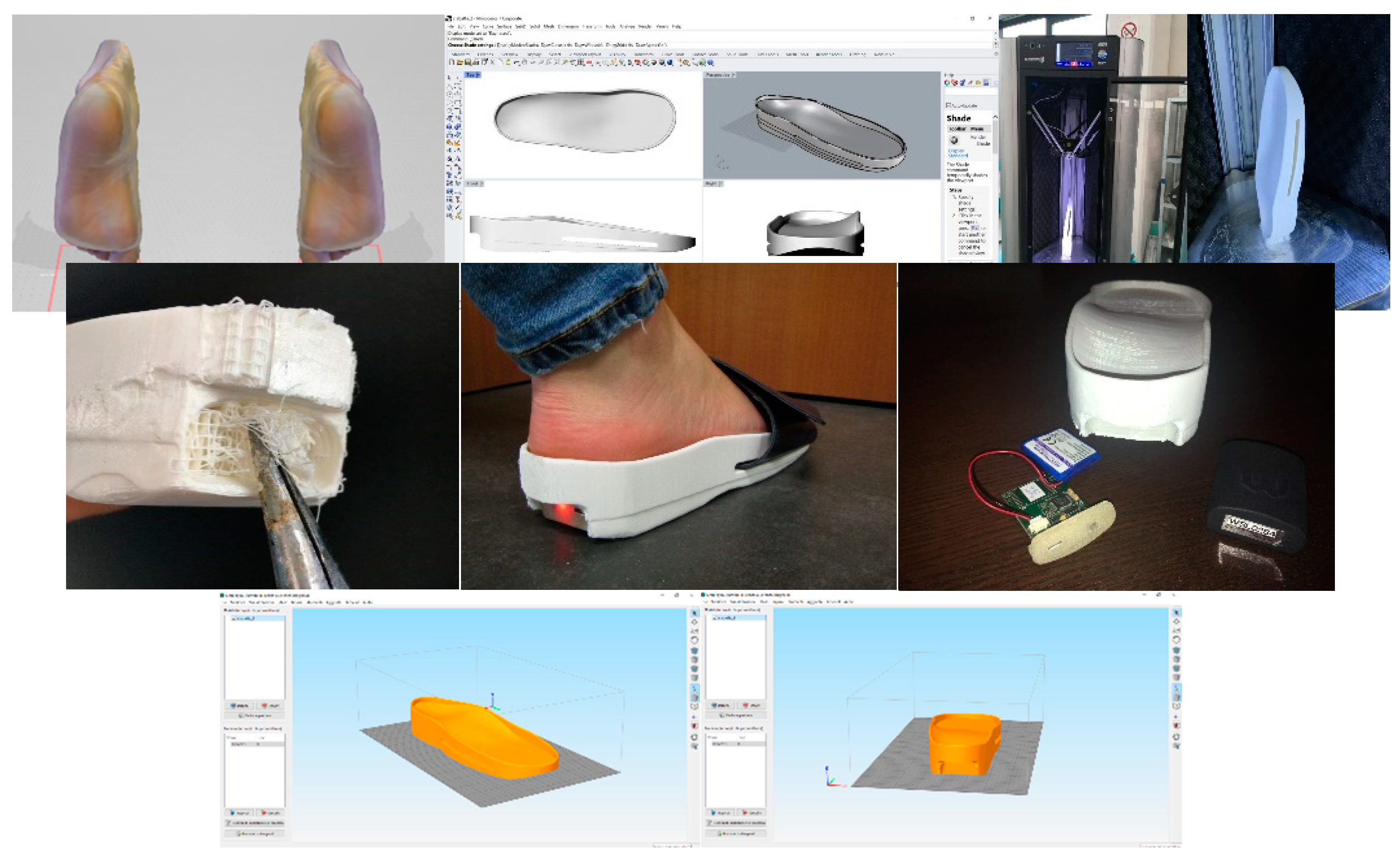
- A Generative Design (GD) workflow was developed to enable podiatrists to easily design and interactively customize foot orthoses and a sensorized house slipper.
- The most 3D printing materials commonly used for manufacturing customized foot orthoses were compared.
2. Materials and Methods
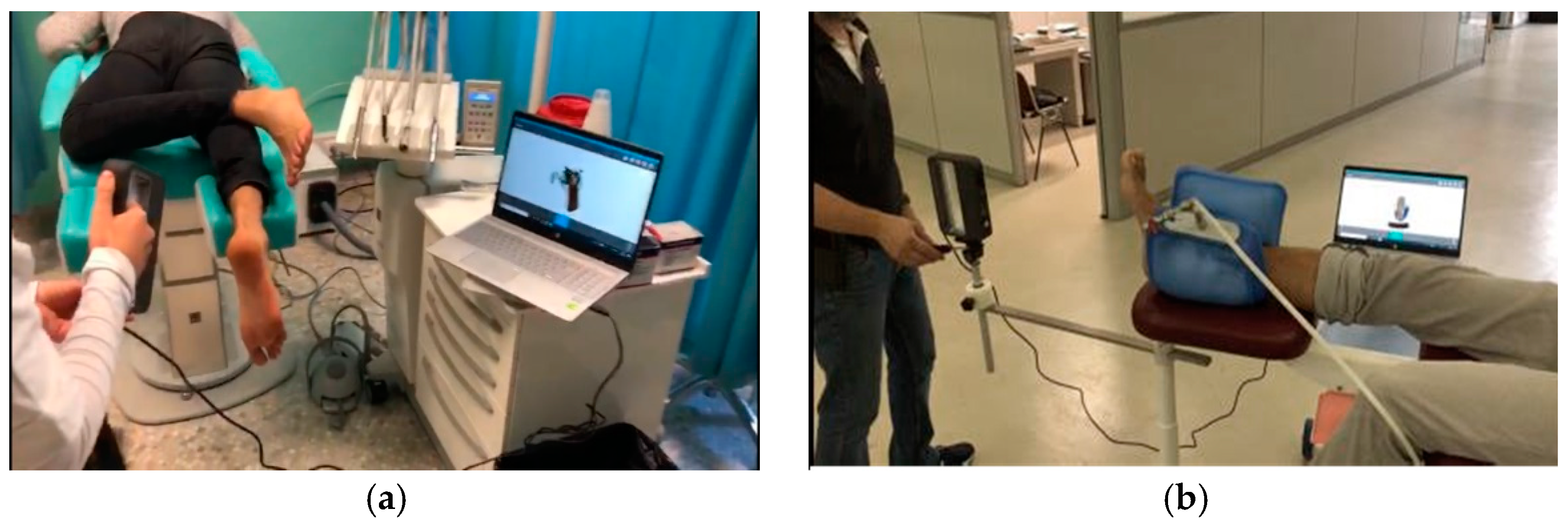
2.1. Foot Scanning
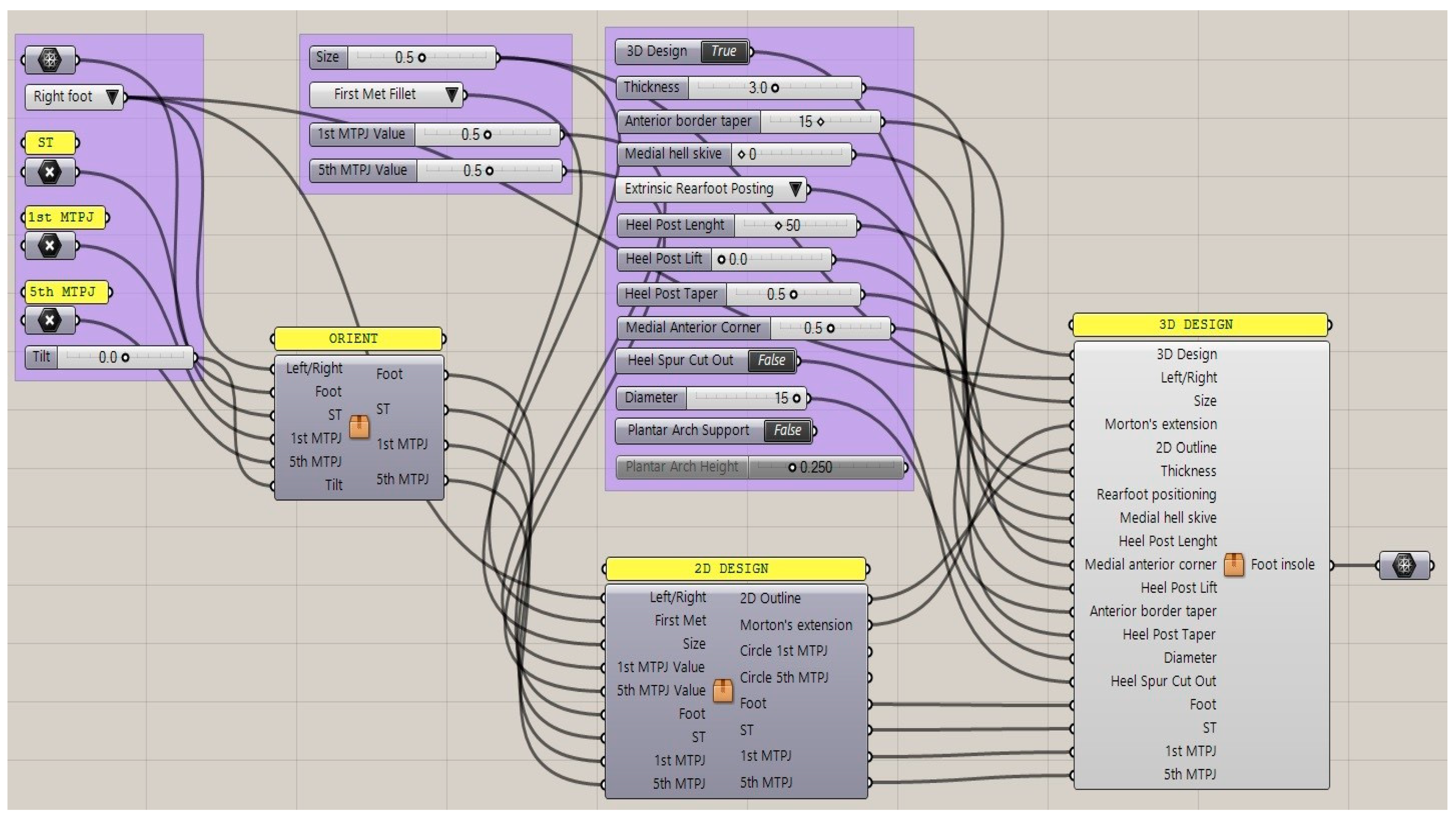
2.2. GD Workflow for Orthosis Customization
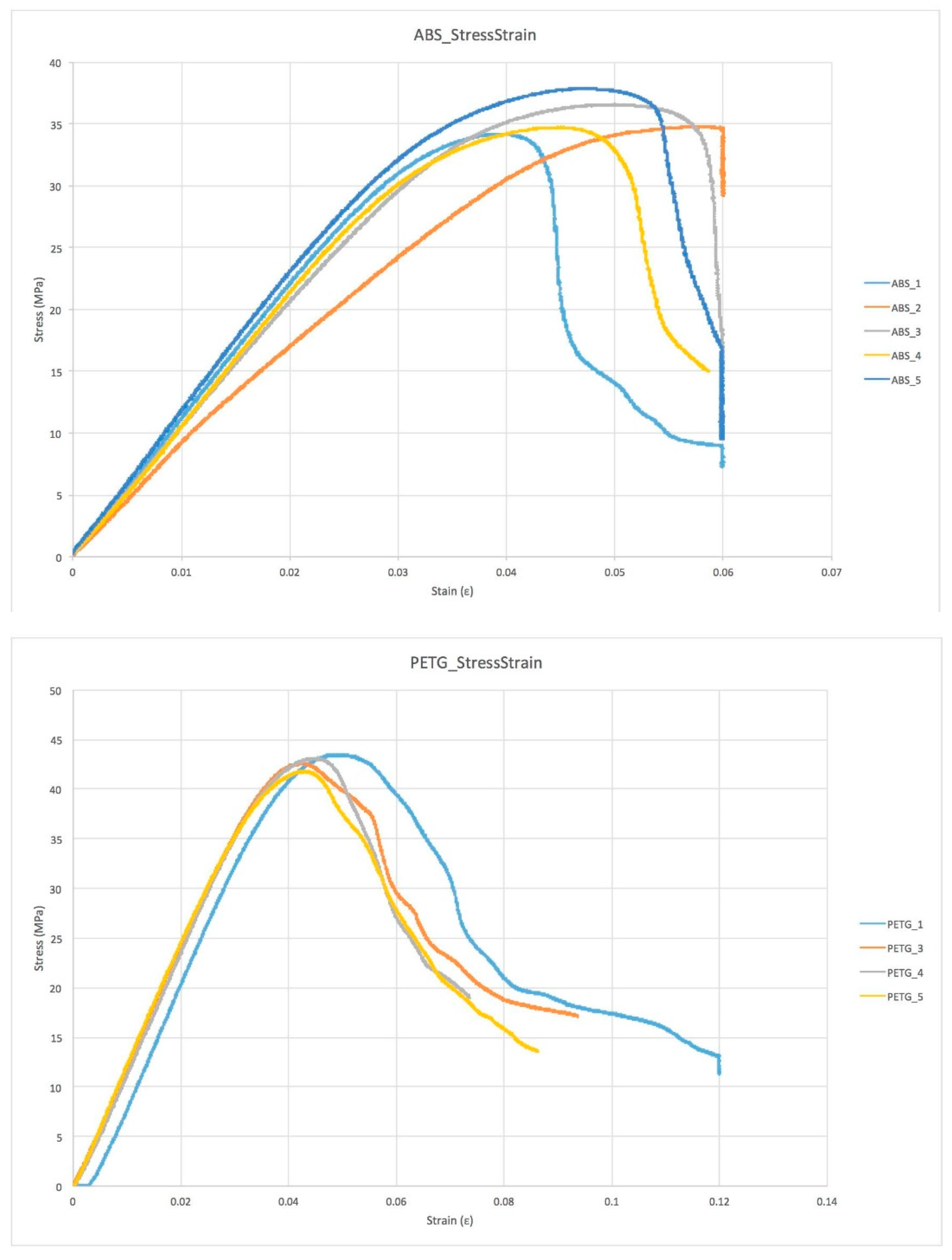
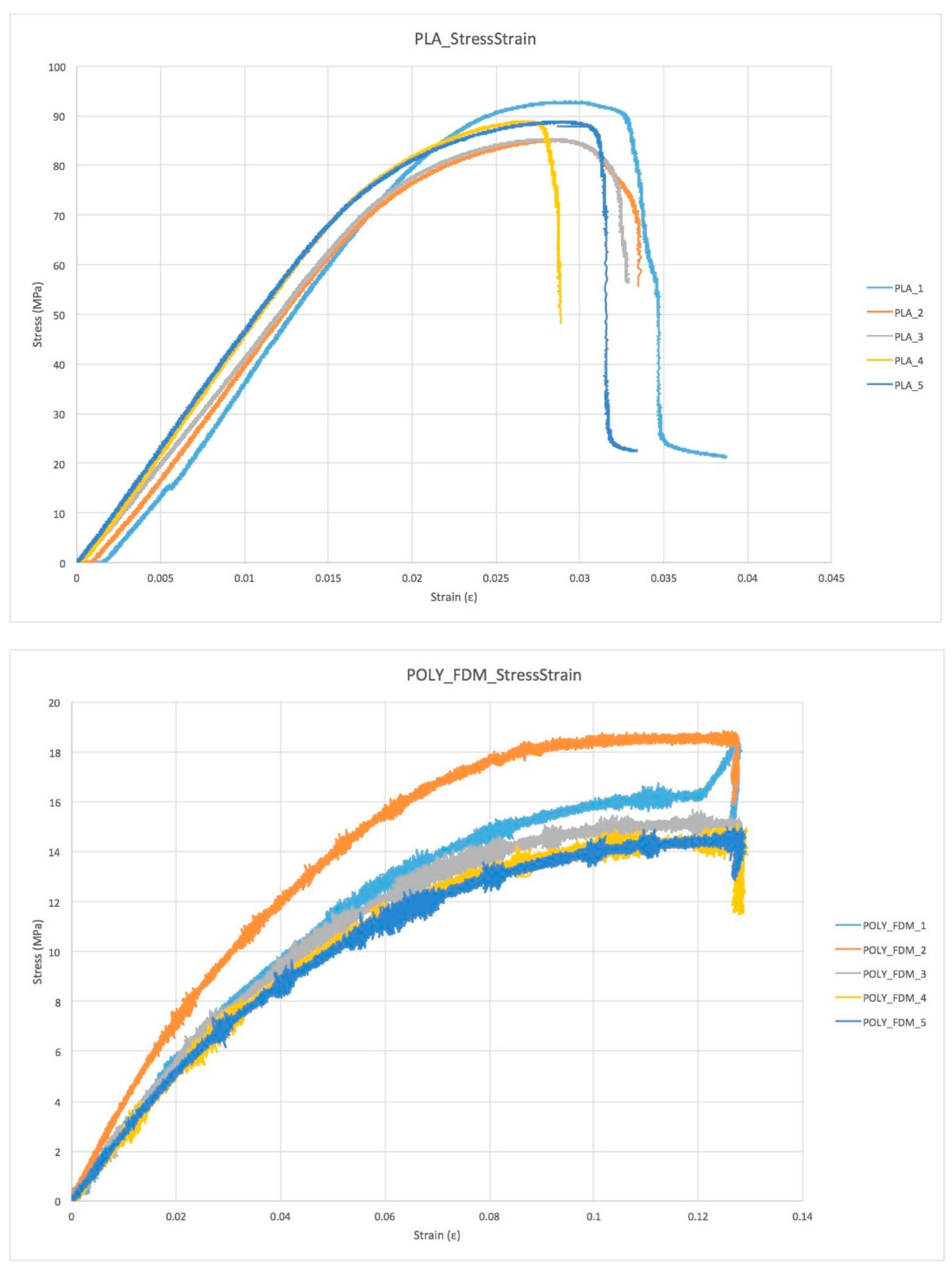
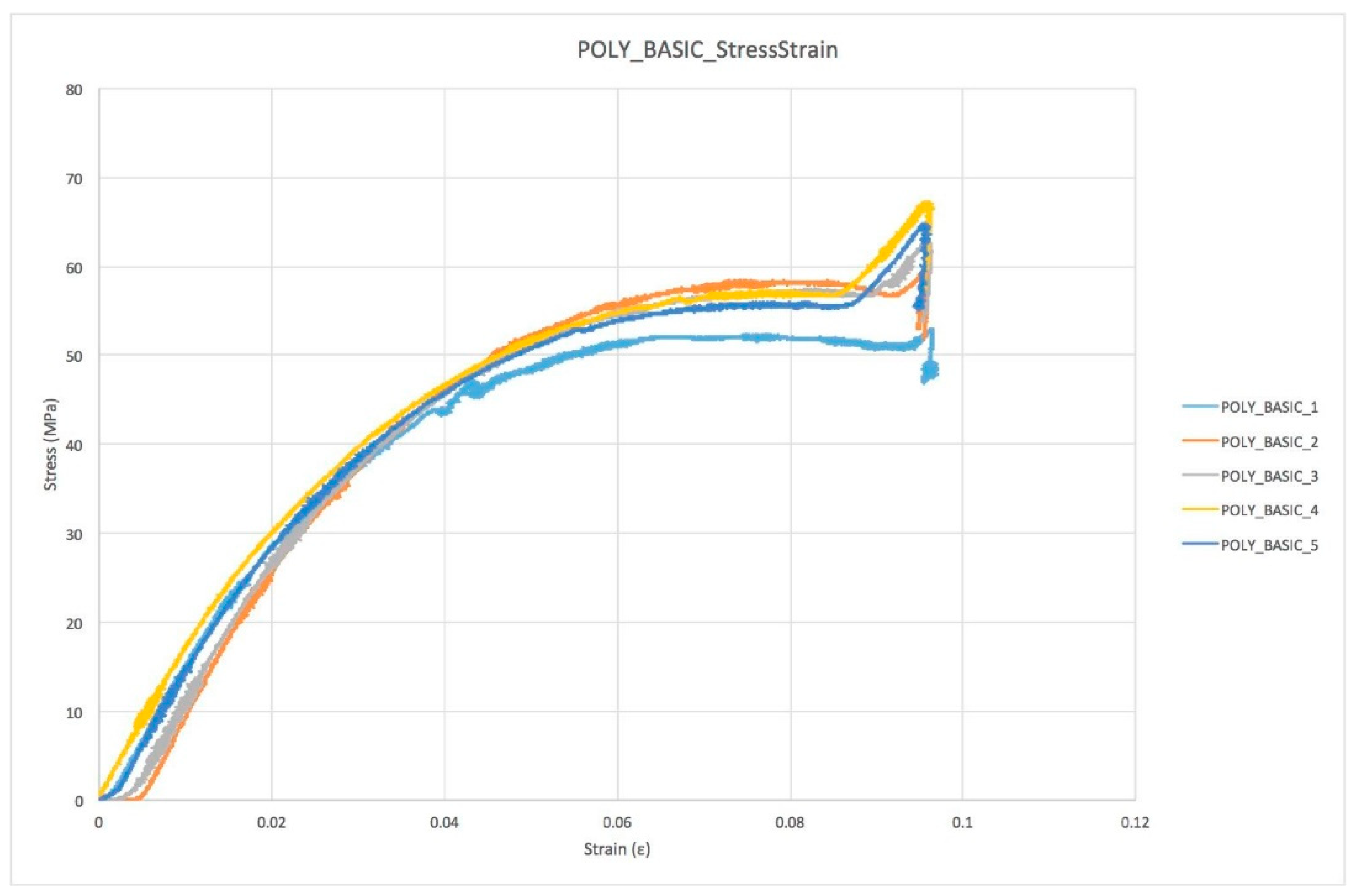
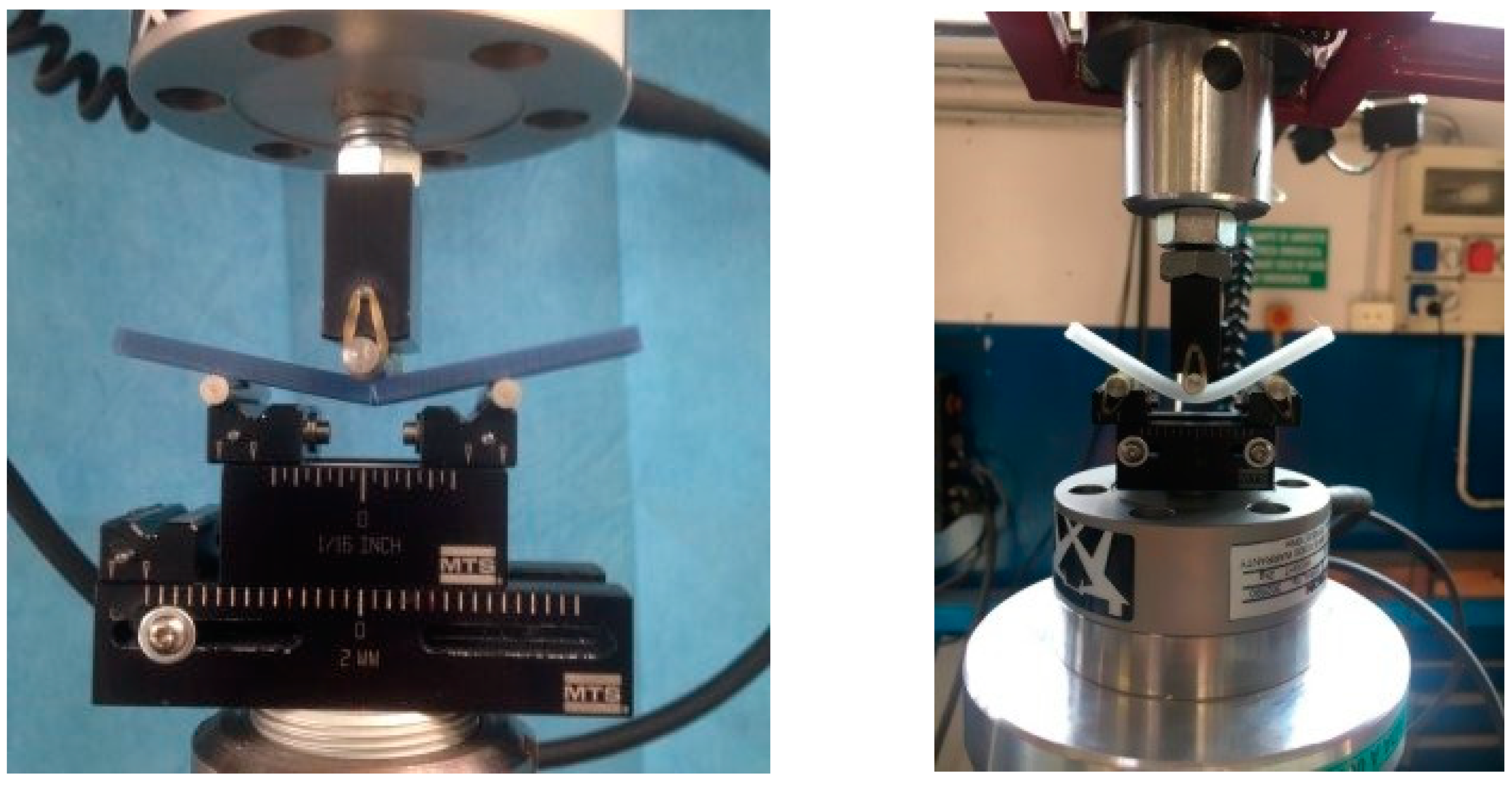
2.3. Three-Point Bending Test
| 5 Polycarbonate Sheet | → | (control specimens) |
| 5 Polycarbonate Extruded | → | (printed specimens) |
| 5 ABS Extruded | → | (printed specimens) |
| 5 PETG Extruded | → | (printed specimens) |
| 5 PLA Extruded | → | (printed specimens) |
- The 1st Failure stress was defined as the first change of slope in stress/strain plot greater than 1% of the previous sample.
- The Max stress was defined as the maximum stress value measured throughout the test.
- The Young Modulus was computed with a linear regression of the stress–strain plot in the range between 20% and 80% of the 1st Failure stress.
- The 1st Failure Work was computed as the integral under the stress–strain curve until the 1st Failure stress occurs.
- The Total Work was computed as the integral under the stress–strain curve until the final failure.
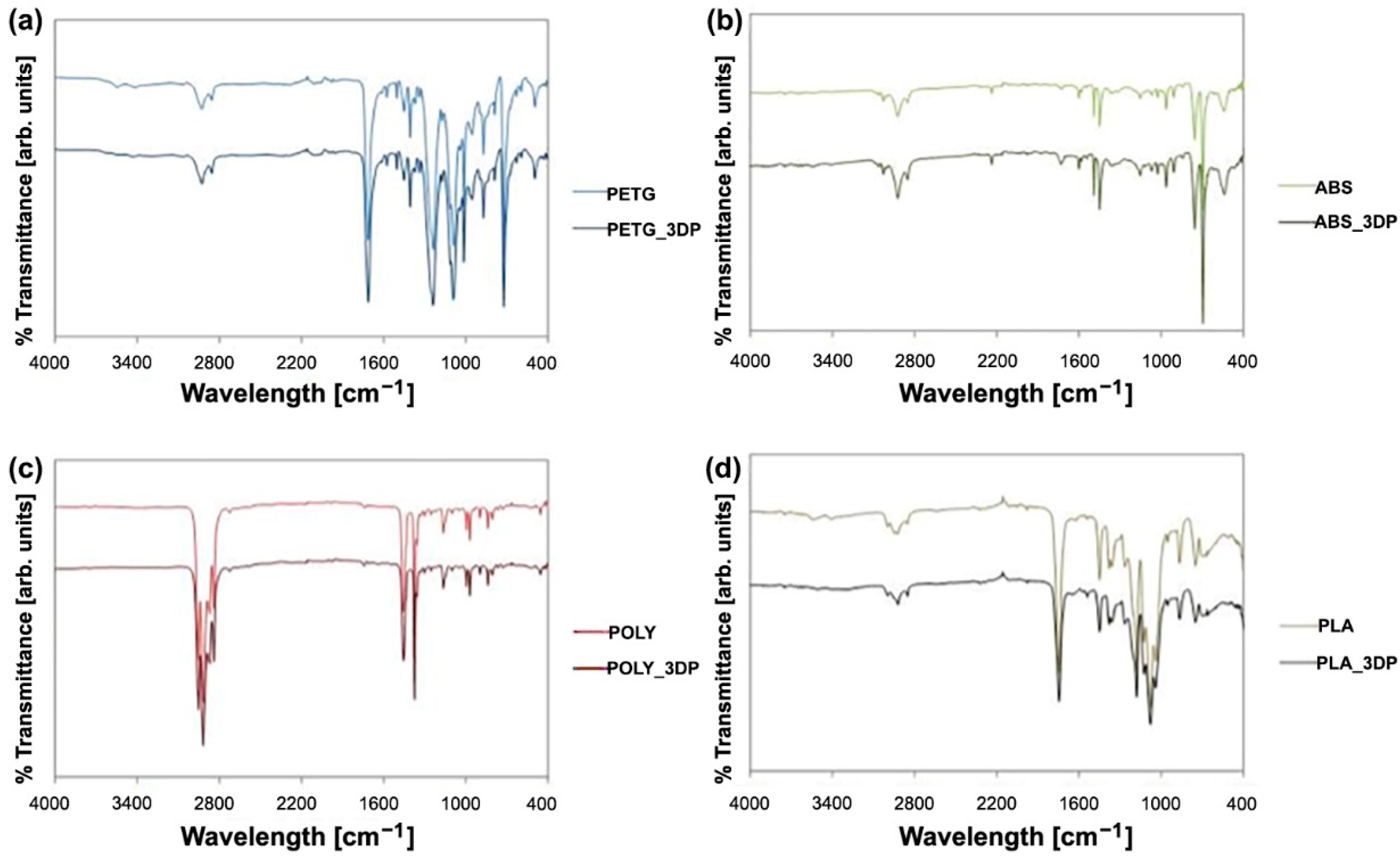
2.4. FT-IR Test
3. Results
3.1. Plot Overview
3.2. Modes of Failure
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Tang, L.; Wang, L.; Bao, W.; Zhu, S.; Li, D.; Liu, C. Functional gradient structural design of customized diabetic insoles. J. Mech. Behav. Biomed. Mater. 2019, 94, 279–287. [Google Scholar] [CrossRef] [PubMed]
- Bandyopadhyay, A.; Bryan, H. Additive manufacturing of multi-material structures. Mater. Sci. Eng. R Rep. 2018, 129, 1–16. [Google Scholar] [CrossRef]
- Ngo, T.D.; Kashani, A.; Imbalzano, G.; Nguyen, K.T.; Hui, D. Additive manufacturing (3D printing): A review of materials, methods, applications and challenges. Compos. Part B Eng. 2018, 143, 172–196. [Google Scholar] [CrossRef]
- Mo, S.; Leung, S.H.; Chan, Z.Y.; Sze, L.K.; Mok, K.M.; Yung, P.S.; Reef, F.; Cheung, R.T.H. The biomechanical difference between running with traditional and 3D printed orthoses. J. Sports Sci. 2019, 37, 2191–2197. [Google Scholar] [CrossRef] [PubMed]
- Xu, R.; Wang, Z.; Ren, Z.; Ma, T.; Jia, Z.; Fang, S.; Jin, H. Comparative Study of the Effects of Customized 3D printed insole and Prefabricated Insole on Plantar Pressure and Comfort in Patients with Symptomatic Flatfoot. Med. Sci. Monit. Int. Med. J. Exp. Clin. Res. 2019, 25, 3510. [Google Scholar] [CrossRef]
- Wang, X.; Jiang, M.; Zhou, Z.; Gou, J.; Hui, D. 3D printing of polymer matrix composites: A review and prospective. Compos. Part B Eng. 2017, 110, 442–458. [Google Scholar] [CrossRef]
- Wohlers, T. Tracking global growth in industrial-scale additive manufacturing. 3D Print. Addit. Manuf. 2014, 1, 2–3. [Google Scholar] [CrossRef]
- Haghighi, A.; Li, L. Study of the relationship between dimensional performance and manufacturing cost in fused deposition modeling. Rapid Prototyp. J. 2018, 24, 395–408. [Google Scholar] [CrossRef]
- Bae, E.J.; Jeong, I.D.; Kim, W.C.; Kim, J.H. A comparative study of additive and subtractive manufacturing for dental restorations. J. Prosthet. Dent. 2017, 118, 187–193. [Google Scholar] [CrossRef]
- Chen, R.K.; Jin, Y.A.; Wensman, J.; Shih, A. Additive manufacturing of custom orthoses and prostheses—A review. Addit. Manuf. 2016, 12, 77–89. [Google Scholar] [CrossRef]
- Yarwindran, M.; Sa’aban, N.A.; Ibrahim, M.; Periyasamy, R. Thermoplastic elastomer infill pattern impact on mechanical properties 3D printed customized orthotic insole. ARPN J. Eng. Appl. Sci. 2016, 11, 6519–6524. [Google Scholar]
- da Silva Barros, K.; Zwolinski, P.; Mansur, A.I. Where do the environmental impacts of Additive Manufacturing come from? Case study of the use of 3D-printing to print orthotic insoles. In Proceedings of the 12ème Congrès International de Génie Industriel, Compiegne, France, 5 May 2017. [Google Scholar]
- Walbran, M.; Turner, K.; McDaid, A.J. Customized 3D printed ankle-foot orthosis with adaptable carbon fibre composite spring joint. Cogent Eng. 2016, 3, 1227022. [Google Scholar] [CrossRef]
- Davia-Aracila, M.; Hinojo-Péreza, J.J.; Jimeno-Morenillab, A.; Morab, H.M. 3D printing of functional anatomical insoles. Comput. Ind. 2018, 94, 38–53. [Google Scholar] [CrossRef]
- Roberts, A.; Wales, J.; Smith, H.; Sampson, C.J.; Jones, P.; James, M. A randomised controlled trial of laser scanning and casting for the construction of ankle–foot orthoses. Prosthet. Orthot. Int. 2016, 40, 253–261. [Google Scholar] [CrossRef] [PubMed]
- Jain, M.L.; Dhande, S.G.; Vyas, N.S. Virtual modeling of an ankle foot orthosis for correc-tion of foot abnormality. Robot. Comput.-Integr. Manuf. 2011, 27, 257–260. [Google Scholar] [CrossRef]
- Mavroidis, C.; Ranky, R.G.; Sivak, M.L.; Patritti, B.L.; DiPisa, J.; Caddle, A.; Gilhooly, K.; Govoni, L.; Sivak, S.; Lancia, M.; et al. Patient specific ankle-foot orthoses using rapid prototyping. J. Neuroeng. Rehabil. 2011, 8, 1. [Google Scholar] [CrossRef]
- Telfer, S.; Pallari, J.; Munguia, J.; Dalgarno, K.; McGeough, M.; Woodburn, J. Embracing additive manufacture: Implications for foot and ankle orthosis design. BMC Musculoskelet. Disord. 2012, 13, 84. [Google Scholar] [CrossRef]
- Alam, M.; Choudhury, I.A.; Azuddin, M. Development of Patient Specific Ankle Foot Orthosis through 3D Reconstruction. In Proceedings of the 3rd International Conference on Environment Energy and Biotechnology, Singapore, 9–10 June 2014; pp. 84–88. [Google Scholar] [CrossRef]
- Palousek, D.; Rosicky, J.; Koutny, D.; Stoklásek, P.; Navrat, T. Pilot study of the wrist orthosis design process. Rapid Prototyp. J. 2014, 20, 27–32. [Google Scholar] [CrossRef]
- Dombroski, C.E.; Balsdon, M.E.; Froats, A. The use of a low cost 3D scanning and printing tool in the manufacture of custom-made foot orthoses: A preliminary study. BMC Res. Notes 2014, 7, 443. [Google Scholar] [CrossRef]
- Song, E.; Yoon, S.W.; Son, H.; Yu, S. Foot Measurement Using 3D Scanning Model. Int. J. Fuzzy Log. Intell. Syst. 2018, 18, 167–174. [Google Scholar] [CrossRef]
- Salles, A.S.; Gy, D.E. An evaluation of personalised insoles developed using additive manufacturing. J. Sports Sci. 2013, 31, 442–450. [Google Scholar] [CrossRef] [PubMed]
- Belvedere, C.; Siegler, S.; Fortunato, A.; Caravaggi, P.; Liverani, E.; Durante, S.; Ensini, A.; Konow, T.; Leardini, A. New comprehensive procedure for custom-made total ankle replacements: Medical imaging, joint modeling, prosthesis design, and 3D printing. J. Orthop. Res. 2019, 37, 760–768. [Google Scholar] [CrossRef] [PubMed]
- Telfer, S.; Woodburn, J. The use of 3D surface scanning for the measurement and assessment of the human foot. J. Foot Ankle Res. 2010, 3, 19–28. [Google Scholar] [CrossRef] [PubMed]
- Menz, H.B.; Auhl, M.; Ristevski, R.; Frescos, N.; Munteanu, S.E. Evaluation of the accuracy of shoe fitting in older people using three-dimensional foot scanning. J. Foot Ankle Res. 2014, 7, 3–13. [Google Scholar] [CrossRef]
- The Pros and Cons of Computerized Foot Orthotic Technology—OPEDGE.COM n.d. Available online: https://opedge.com/Articles/ViewArticle/2004-11_01 (accessed on 27 October 2019).
- Stanković, K.; Booth, B.G.; Danckaers, F.; Burg, F.; Vermaelen, P.; Duerinck, S.; Sijbers, J.; Huysmans, T. Three-dimensional quantitative analysis of healthy foot shape: A proof of concept study. J. Foot Ankle Res. 2018, 11, 8. [Google Scholar] [CrossRef] [PubMed]
- Coudert, T.; Vacher, P.; Smits, C.; Van der Zande, M. A method to obtain 3D foot shape deformation during the gait cycle. In Proceedings of the 9th International Symposium on the 3D Analysis of Human Movement, Valenciennes, France, 28–30 June 2006. [Google Scholar]
- Jezersek, M.; Mozina, J. High-speed measurement of foot shape based on multiple-laserplane triangulation. Opt. Eng. 2009, 48, 113604. [Google Scholar] [CrossRef]
- Kimura, M.; Mochimaru, M.; Kanade, T. 3D measurement of feature cross-sections of foot while walking. Mach. Vis. Appl. 2011, 22, 377–388. [Google Scholar] [CrossRef]
- Barisch-Fritz, B.; Schmeltzpfenning, T.; Plank, C.; Grau, S. Foot deformation during walking: Differences between static and dynamic 3D foot morphology in developing feet. Ergonomics 2014, 57, 921–933. [Google Scholar] [CrossRef]
- Pallari, J.H.; Dalgarno, K.W.; Munguia, J.; Muraru, L.; Peeraer, L.; Telfer, S.; Woodburn, J. Design and additive fabrication of foot and ankle-foot orthoses. In 21st Annual International Solid Freeform Fabrication Symposium–An Additive Manufacturing Conference; University of Texas: Austin, TX, USA, 2010. [Google Scholar]
- Chromy, A.; Zalud, L. Robotic 3D scanner as an alternative to standard modalities of medical imaging. SpringerPlus 2014, 3, 13. [Google Scholar] [CrossRef]
- Payne, C. Cost benefit comparison of plaster casts and optical scans of the foot for the manufacture of foot orthoses. Australas. J. Podiatr. Med. 2007, 41, 29–31. [Google Scholar]
- Drury, J.L.; Mooney, D.J. Hydrogels for tissue engineering: Scaffold design variables and applications. Biomaterials 2003, 24, 4337–4351. [Google Scholar] [CrossRef]
- Tukuru, N.; Gowda, S.K.P.; Ahmed, S.M.; Badami, S. Rapidprototype technique in medical field. Res. J. Pharm. Technol. 2008, 1, 341–344. [Google Scholar]
- Laughton, C.; McClay Davis, I.; Williams, D.S. A comparison of four methods of obtaining a negative impression of the foot. J. Am. Podiatr. Med. Assoc. 2002, 92, 261–268. [Google Scholar] [CrossRef] [PubMed]
- Hin, A.J.S.; Krul, A.J. Performance of Human Solutions Body Dimensions Software; Report 2005-A9; TNO Human Factors: Hague, The Netherlands, 2005. [Google Scholar]
- Zein, N.N.; Hanouneh, I.A.; Bishop, P.D.; Samaan, M.; Eghtesad, B.; Quintini, C.; Miller, C.; Yerian, L.; Klatte, R. Three-dimensional print of a liver for preoperative planning in living donor liver transplantation. Liver Transpl. 2013, 19, 1304–1310. [Google Scholar] [CrossRef] [PubMed]
- Carroll, M.; Annabell, M.E.; Rome, K. Reliability of capturing foot parameters using digital scanning and the neutral suspension casting technique. J. Foot Ankle Res. 2011, 4, 9. [Google Scholar] [CrossRef]
- Cignoni, P.; Callieri, M.; Corsini, M.; Dellepiane, M.; Ganovelli, F.; Ranzuglia, G. MeshLab: An Open-Source Mesh Processing Tool. In Proceedings of the Sixth Eurographics Italian Chapter Conference, Salerno, Italy, 2–4 July 2008; pp. 129–136. [Google Scholar]
- Islam, M.N.; Boswell, B.; Pramanik, A. An investigation of dimensional accuracy of parts produced by three-dimensional printing. In Proceedings of the World Congress on Engineering 2013, IAENG, London, UK, 3–5 July 2013. [Google Scholar]
- Todorov, G.; Sofronov, Y.; Dimova, K. Comparison Analysis Between Different Technologies for Manufacturing Patient-Specific Implants. In Machine and Industrial Design in Mechanical Engineering; Rackov, M., Mitrović, R., Čavić, M., Eds.; KOD, Mechanisms and Machine Science; Springer: Cham, Switzerland, 2021; Volume 109. [Google Scholar] [CrossRef]
- Saqib, S.; Urbanic, J. An experimental study to determine geometric and dimensional accuracy impact factors for fused deposition modelled parts. In Enabling Manufacturing Competitiveness and Economic Sustainability; Springer: Berlin/Heidelberg, Germany, 2012; pp. 293–298. [Google Scholar] [CrossRef]
- Nancharaiah, T.R.; Raju, D.R.; Raju, V.R. An experimental investigation on surface quality and dimensional accuracy of FDM components. Int. J. Emerg. Technol. 2010, 1, 106–111. [Google Scholar]
- Ay, M.; Kubat, T.; Delilbasi, C.; Ekici, B.; Yuzbasioglu, H.E.; Hartomacioglu, S. 3D Bio-Cad modeling of human mandible and fabrication by rapid-prototyping technology. Usak Univ. J. Mater. Sci. 2013, 2, 135–145. [Google Scholar] [CrossRef][Green Version]
- Huang, C.Y.; Luo, L.J.; Lee, P.Y.; Lai, J.Y.; Wang, W.T.; Lin, S.C. Efficient segmentation algorithm for 3D bone models construction on medical images. J. Med. Biol. Eng. 2010, 31, 375–386. [Google Scholar] [CrossRef]
- Karatas, O.H.; Toy, E. Three-dimensional imaging techniques: A literature review. Eur. J. Dent. 2014, 8, 132–140. [Google Scholar] [CrossRef]
- Othman, H.I. Role of computer aided design and computer aided manufacturing technology in prosthetic implant restorations. Int. J. Dent. Clin. 2012, 4, 22–34. [Google Scholar]
- Dizon, J.R.; Espera, A.H., Jr.; Chen, Q.; Advincula, R.C. Mechanical characterization of 3D-printed polymers. Addit. Manuf. 2018, 20, 44–67. [Google Scholar] [CrossRef]
- Yick, K.L.; Lo, W.T.; Ng, S.P.; Yip, J.; Kwan, H.H.; Kwong, Y.Y.; Cheng, F.C. Analysis of Insole Geometry and Deformity by Using a Three-Dimensional Image Processing Technique: A Preliminary Study. J. Am. Podiatr. Med. Assoc. 2019, 109, 98–107. [Google Scholar] [CrossRef] [PubMed]
- Choo, Y.J.; Boudier-Revéret, M.; Chang, M.C. 3D printing technology applied to orthosis manufacturing: Narrative review. Ann. Palliat. Med. 2020, 9, 4262–4270. [Google Scholar] [CrossRef] [PubMed]

| Casts Obtained after Footprint Recording with Pinstripe and Subtalar Joint Bandage in the Neutral Position (Gold Standard) | ||||||
|---|---|---|---|---|---|---|
| Mesh-Mesh Alignment | Global Alignment | Hausdorff Distance (mm) | ||||
| Control Cast | Scanning of the Cast | Avg Err | Error Bound | Max | Mean | RMS |
| 1 | 2 | 0.16 | 0.00 | 11.36 | 0.26 | 0.69 |
| 1 | 3 | 0.27 | 0.00 | 4.87 | 0.32 | 0.48 |
| 1 | 4 | 0.45 | 0.00 | 11.14 | 0.57 | 0.86 |
| 1 | 5 | 0.83 | 0.00 | 16.40 | 1.60 | 2.49 |
| 1 | 6 | 0.21 | 0.00 | 15.66 | 0.57 | 1.35 |
| 1 | 7 | 0.51 | 0.00 | 9.93 | 0.39 | 0.95 |
| 1 | 8 | 0.66 | 0.00 | 10.68 | 1.48 | 2.18 |
| 1 | 9 | 0.19 | 0.00 | 11.12 | 0.54 | 1.27 |
| 1 | 10 | 0.23 | 0.00 | 19.28 | 0.67 | 1.92 |
| 0.74 | ||||||
| Scanning of the Foot without Any Foot Locking System and with a Handheld 3D Scanner | ||||||
|---|---|---|---|---|---|---|
| Mesh-Mesh Alignment | Global Alignment | Hausdorff Distance (mm) | ||||
| Control Scan | Scanning of the Cast | Avg Err | Error Bound | Max | Mean | RMS |
| 1 | 2 | 0.21 | 0.00 | 22.67 | 0.91 | 1.29 |
| 1 | 3 | 0.29 | 0.00 | 50.72 | 1.68 | 4.64 |
| 1 | 4 | 0.29 | 0.00 | 23.95 | 1.20 | 3.06 |
| 1 | 5 | 0.21 | 0.00 | 25.91 | 0.96 | 1.17 |
| 1 | 6 | 0.23 | 0.00 | 19.60 | 1.28 | 1.23 |
| 1 | 7 | 0.21 | 0.00 | 13.35 | 0.93 | 1.51 |
| 1 | 8 | 0.28 | 0.00 | 15.92 | 1.14 | 1.75 |
| 1 | 9 | 0.18 | 0.00 | 12.62 | 0.83 | 1.04 |
| 1 | 10 | 0.29 | 0.00 | 25.46 | 1.31 | 3.46 |
| 1.16 | ||||||
| Scanning of the Foot with a Foot Locking System and with a Tripod for the 3D Scanner | ||||||
|---|---|---|---|---|---|---|
| Mesh-Mesh Alignment | Global Alignment | Hausdorff Distance (mm) | ||||
| Control Scan | Scanning of the Cast | Avg Err | Error Bound | Max | Mean | RMS |
| 1 | 2 | 0.23 | 0.00 | 22.29 | 1.06 | 3.21 |
| 1 | 3 | 0.35 | 0.00 | 15.89 | 0.85 | 2.83 |
| 1 | 4 | 0.22 | 0.00 | 21.61 | 0.69 | 2.05 |
| 1 | 5 | 0.24 | 0.00 | 12.34 | 0.92 | 2.12 |
| 1 | 6 | 0.33 | 0.00 | 18.94 | 0.44 | 3.25 |
| 1 | 7 | 0.24 | 0.00 | 19.04 | 1.30 | 2.66 |
| 1 | 8 | 0.35 | 0.00 | 7.86 | 0.66 | 1.12 |
| 1 | 9 | 0.35 | 0.00 | 18.18 | 1.20 | 3.22 |
| 1 | 10 | 0.28 | 0.00 | 8.98 | 0.74 | 1.13 |
| 0.85 | ||||||
| Specimen Group | Specimen n° | σ 1st Failure (MPa) | ε 1st Failure | Work 1st Failure (MPa) | σmax (GPa) | ε max | Work TOT (MPa) | Young's Modulus (MPa) |
|---|---|---|---|---|---|---|---|---|
| 1 | 32.1 | 0.032 | 0.562 | 34.3 | 0.060 | 0.948 | 1040.00 | |
| 2 | 32.0 | 0.031 | 0.412 | 34.9 | 0.060 | 0.456 | 795.59 | |
| ABS | 3 | 32.1 | 0.034 | 0.575 | 36.6 | 0.060 | 1.044 | 977.04 |
| 4 | 29.2 | 0.028 | 0.418 | 34.8 | 0.059 | 0.891 | 1050.90 | |
| 5 | 34.0 | 0.033 | 0.605 | 38.0 | 0.060 | 1.246 | 1062.10 | |
| Average | 31.9 | 0.032 | 0.515 | 35.7 | 0.060 | 0.917 | 985.13 | |
| Std Dev | 1.5 | 0.002 | 0.082 | 1.4 | 0.001 | 0.260 | 99.25 | |
| 1 | 88.0 | 0.023 | 1.019 | 92.9 | 0.039 | 1.693 | 1040.00 | |
| 2 | 78.2 | 0.028 | 0.847 | 85.2 | 0.033 | 0.943 | 795.59 | |
| PLA | 3 | 80.0 | 0.021 | 0.917 | 85.4 | 0.033 | 0.941 | 977.04 |
| 4 | 75.3 | 0.017 | 0.658 | 89.0 | 0.029 | 0.944 | 1050.90 | |
| 5 | 80.1 | 0.019 | 0.843 | 89.0 | 0.033 | 1.560 | 1062.10 | |
| Average | 80.3 | 0.022 | 0.857 | 88.3 | 0.033 | 1.216 | 985.13 | |
| Std Dev | 4.2 | 0.004 | 0.118 | 2.8 | 0.003 | 0.338 | 99.25 | |
| 1 | 42.1 | 0.042 | 0.900 | 43.6 | 0.120 | 2.248 | 1230.00 | |
| 2 | 42.0 | 0.043 | 1.072 | 42.7 | 0.094 | 1.619 | 1160.00 | |
| PETG | 3 | 42.2 | 0.043 | 1.024 | 43.2 | 0.074 | 1.289 | 1198.00 |
| 4 | 41.0 | 0.043 | 1.055 | 41.9 | 0.086 | 1.594 | 1139.00 | |
| Average | 41.8 | 0.043 | 1.013 | 42.9 | 0.094 | 1.688 | 1181.75 | |
| Std Dev | 0.5 | 0.000 | 0.068 | 0.6 | 0.017 | 0.349 | 34.97 | |
| 1 | 8.5 | 0.034 | 0.153 | 18.5 | 0.127 | 0.488 | 250.77 | |
| 2 | 10.7 | 0.034 | 0.206 | 18.8 | 0.127 | 0.719 | 300.02 | |
| POLY_FFF | 3 | 8.5 | 0.036 | 0.172 | 15.7 | 0.127 | 0.496 | 238.88 |
| 4 | 8.0 | 0.035 | 0.155 | 15.1 | 0.128 | 1.327 | 228.65 | |
| 5 | 8.2 | 0.037 | 0.167 | 15.0 | 0.128 | 0.448 | 218.65 | |
| Average | 8.8 | 0.035 | 0.171 | 16.6 | 0.127 | 0.696 | 247.39 | |
| Std Dev | 1.0 | 0.001 | 0.019 | 1.7 | 0.000 | 0.330 | 28.39 | |
| 1 | 50.4 | 0.027 | 0.513 | 53.0 | 0.097 | 1.584 | 1308.03 | |
| 2 | 55.0 | 0.024 | 0.331 | 59.6 | 0.096 | 1.540 | 1555.05 | |
| POLY_BASIC | 3 | 55.2 | 0.027 | 0.435 | 63.0 | 0.096 | 1.444 | 1454.20 |
| 4 | 55.1 | 0.027 | 0.547 | 67.3 | 0.097 | 1.468 | 1377.40 | |
| 5 | 55.0 | 0.026 | 0.483 | 64.9 | 0.096 | 4.027 | 1415.10 | |
| Average | 54.2 | 0.026 | 0.462 | 61.6 | 0.096 | 2.013 | 1421.96 | |
| Std Dev | 1.9 | 0.001 | 0.075 | 5.0 | 0.000 | 1.008 | 82.18 | |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Brognara, L.; Fantini, M.; Morellato, K.; Graziani, G.; Baldini, N.; Cauli, O. Foot Orthosis and Sensorized House Slipper by 3D Printing. Materials 2022, 15, 4064. https://doi.org/10.3390/ma15124064
Brognara L, Fantini M, Morellato K, Graziani G, Baldini N, Cauli O. Foot Orthosis and Sensorized House Slipper by 3D Printing. Materials. 2022; 15(12):4064. https://doi.org/10.3390/ma15124064
Chicago/Turabian StyleBrognara, Lorenzo, Massimiliano Fantini, Kavin Morellato, Gabriela Graziani, Nicola Baldini, and Omar Cauli. 2022. "Foot Orthosis and Sensorized House Slipper by 3D Printing" Materials 15, no. 12: 4064. https://doi.org/10.3390/ma15124064
APA StyleBrognara, L., Fantini, M., Morellato, K., Graziani, G., Baldini, N., & Cauli, O. (2022). Foot Orthosis and Sensorized House Slipper by 3D Printing. Materials, 15(12), 4064. https://doi.org/10.3390/ma15124064









