Load-to-Failure Resistance and Optical Characteristics of Nano-Lithium Disilicate Ceramic after Different Aging Processes
Abstract
:1. Introduction
2. Materials and Methods
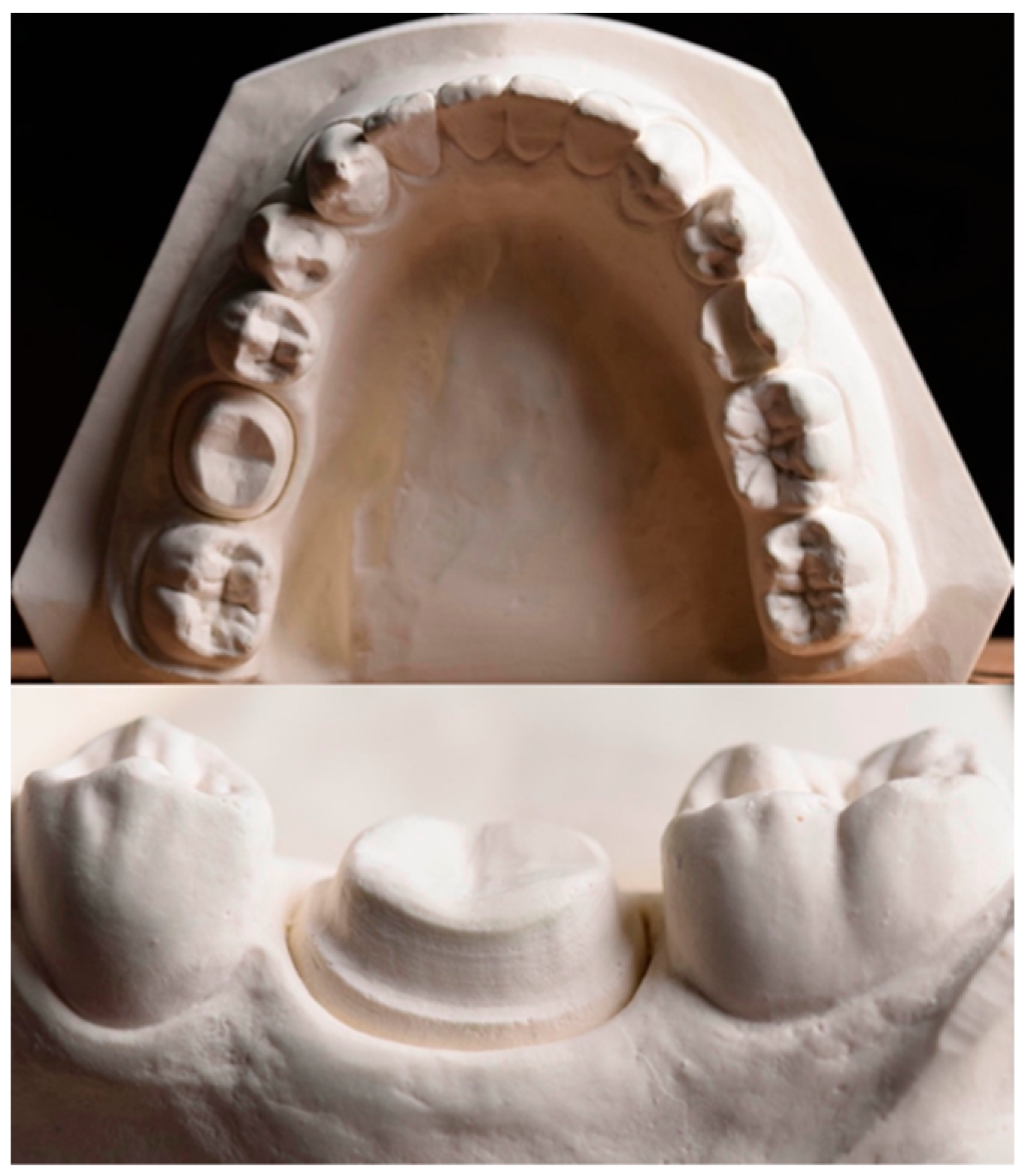
2.1. Crown Fabrication and Load-to-Failure Resistance Test
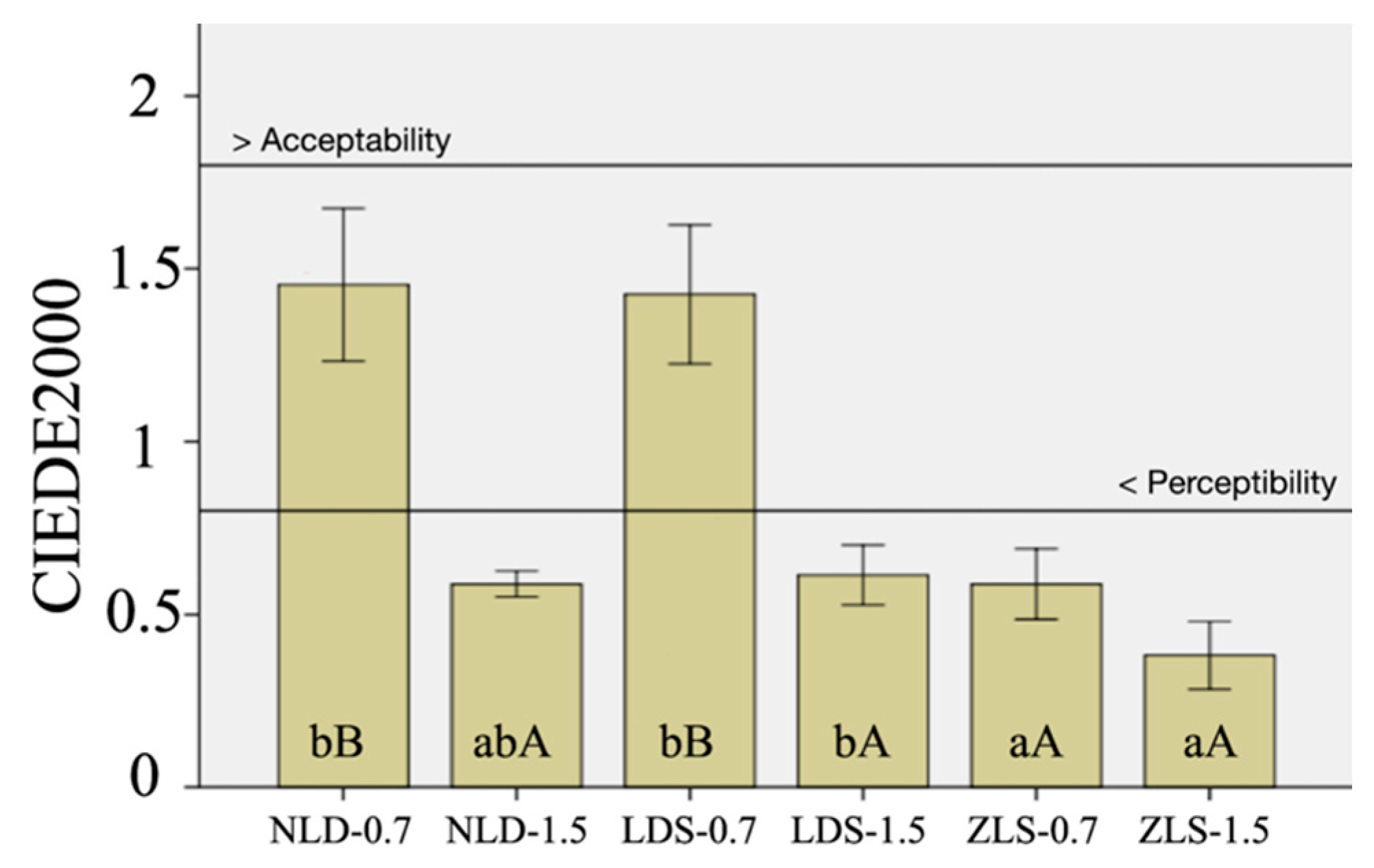
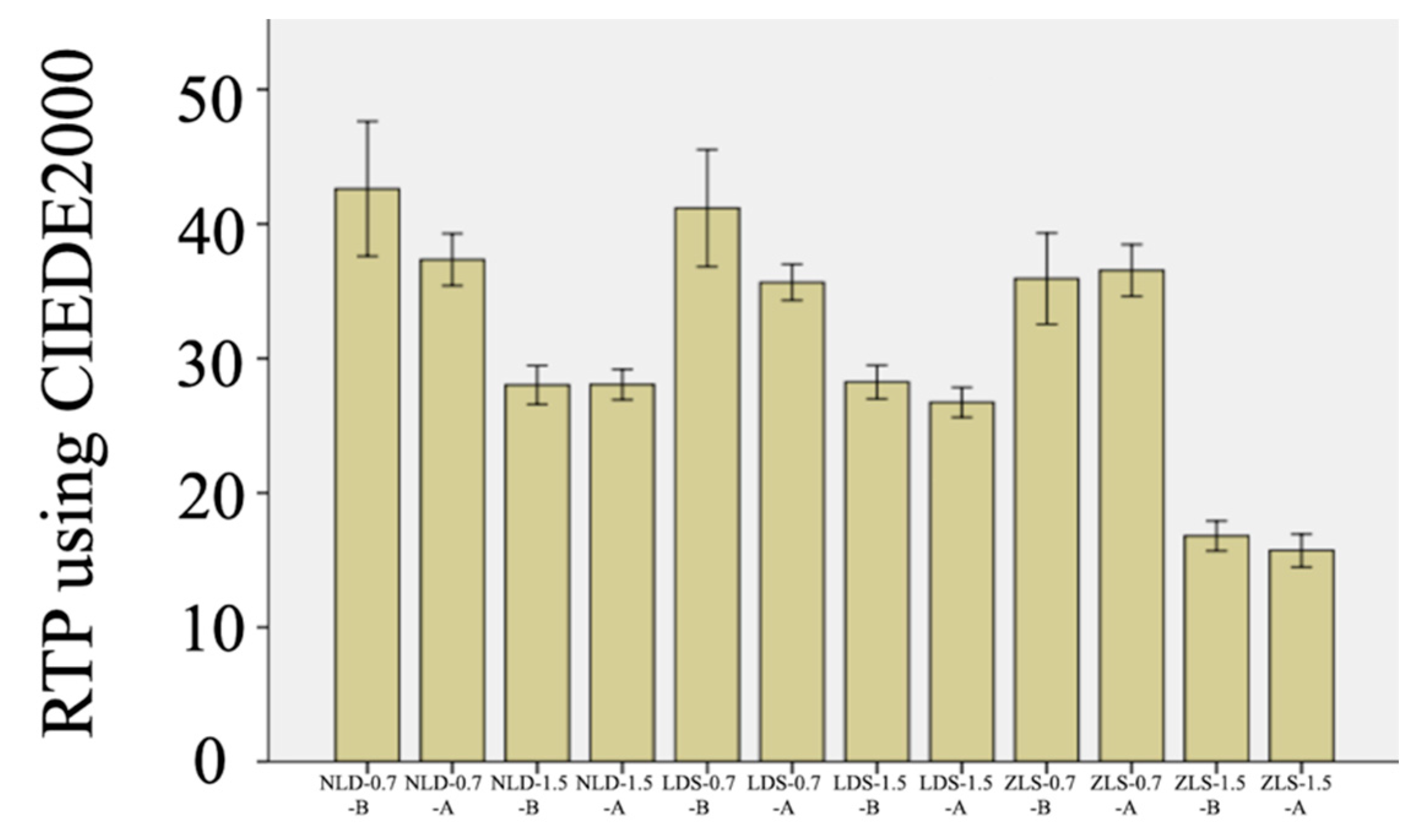
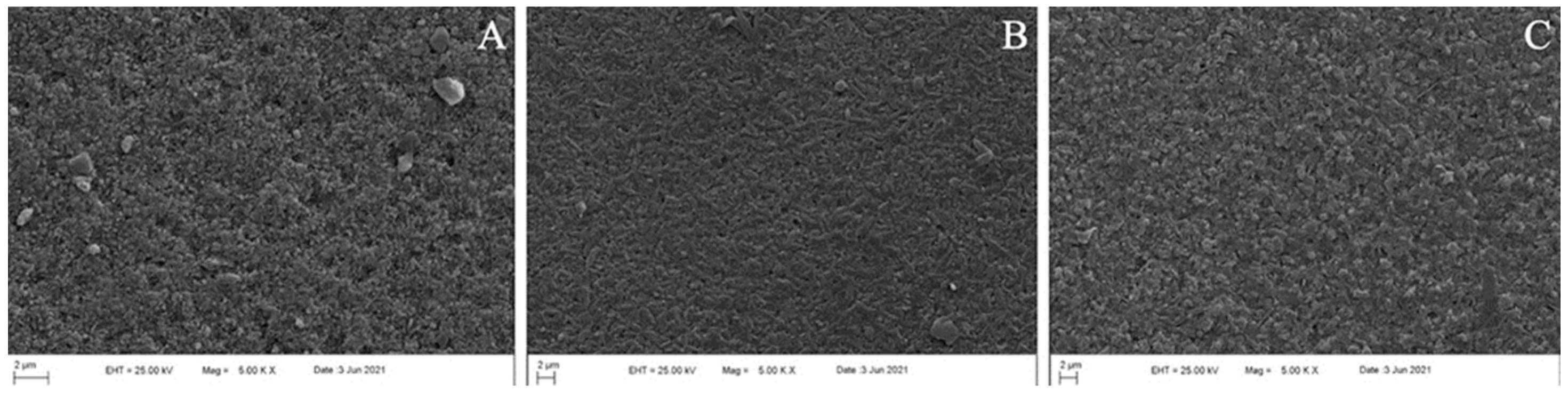
2.2. Color Coordinate Measurements
2.3. Statistical Analysis
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Kashkari, A.; Yilmaz, B.; Brantley, W.A.; Schricker, S.R.; Johnston, W.M. Fracture analysis of monolithic CAD-CAM crowns. J. Esthet. Restor. Dent. 2019, 31, 346–352. [Google Scholar] [CrossRef] [PubMed]
- Khurshid, Z.; Zafar, M.S.; Najeeb, S.; Nejatian, T.; Sefat, F. Introduction to dental biomaterials and their advances. In Advanced dental biomaterials, 1st ed.; Khurshid, Z., Zafar, M.S., Najeeb, S., Nejatian, T., Sefat, F., Eds.; Elsevier: Amsterdam, The Netherlands, 2019; pp. 1–5. [Google Scholar]
- Fasbinder, D.J. Materials for chairside CAD/CAM restorations. Compend. Contin. Educ. Dent. 2010, 31, 702–704, 706, 708–709. [Google Scholar] [PubMed]
- Sen, N.; Us, Y.O. Mechanical and optical properties of monolithic CAD-CAM restorative materials. J. Prosthet. Dent. 2018, 119, 593–599. [Google Scholar] [CrossRef] [PubMed]
- Caprak, Y.O.; Turkoglu, P.; Akgungor, G. does the translucency of novel monolithic cad/cam materials affect resin cement polymerization with different curing modes? J. Prosthodont. 2019, 28, e572–e579. [Google Scholar] [CrossRef]
- Weyhrauch, M.; Igiel, C.; Scheller, H.; Weibrich, G.; Lehmann, K.M. Fracture strength of monolithic all-ceramic crowns on titanium implant abutments. Int. J. Oral. Maxillofac. Implant. 2016, 31, 304–309. [Google Scholar] [CrossRef]
- Lubauer, J.; Belli, R.; Peterlik, H.; Hurle, K.; Lohbauer, U. Grasping the Lithium hype: Insights into modern dental Lithium Silicate glass-ceramics. Dent. Mater. 2022, 38, 318–332. [Google Scholar] [CrossRef]
- Marchesi, G.; Camurri Piloni, A.; Nicolin, V.; Turco, G.; Di Lenarda, R. Chairside CAD/CAM materials: Current trends of clinical uses. Biology 2021, 10, 1170. [Google Scholar] [CrossRef]
- Lim, C.-H.; Jang, Y.-S.; Lee, M.-H.; Bae, T.-S. Evaluation of fracture strength for single crowns made of the different types of lithium disilicate glass–ceramics. Odontology 2020, 108, 231–239. [Google Scholar] [CrossRef]
- Sieper, K.; Wille, S.; Kern, M. Fracture strength of lithium disilicate crowns compared to polymer-infiltrated ceramic-network and zirconia reinforced lithium silicate crowns. J. Mech. Behav. Biomed. Mater. 2017, 74, 342–348. [Google Scholar] [CrossRef]
- Gürdal, I.; Atay, A.; Eichberger, M.; Cal, E.; Üsümez, A.; Stawarczyk, B. Color change of CAD-CAM materials and composite resin cements after thermocycling. J. Prosthet. Dent. 2018, 120, 546–552. [Google Scholar] [CrossRef]
- Phark, J.H.; Duarte, S., Jr. Microstructural considerations for novel lithium disilicate glass ceramics: A review. J. Esthet. Restor. Dent. 2022, 34, 92–103. [Google Scholar] [CrossRef]
- Gunal, B.; Ulusoy, M.M. Optical properties of contemporary monolithic CAD-CAM restorative materials at different thicknesses. J. Esthet. Restor. Dent. 2018, 30, 434–441. [Google Scholar] [CrossRef] [PubMed]
- Kurt, M.; Bankoğlu Güngör, M.; Karakoca Nemli, S.; Turhan Bal, B. Effects of glazing methods on the optical and surface properties of silicate ceramics. J. Prosthodont. Res. 2020, 64, 202–209. [Google Scholar] [CrossRef] [PubMed]
- Çakmak, G.; Donmez, M.B.; Kashkari, A.; Johnston, W.M.; Yilmaz, B. Effect of thickness, cement shade, and coffee thermocycling on the optical properties of zirconia reinforced lithium silicate ceramic. J. Esthet. Restor. Dent. 2021, 33, 1132–1138. [Google Scholar] [CrossRef] [PubMed]
- Jurado, C.A.; El-Gendy, T.; Hyer, J.; Tsujimoto, A. Color stability of fully- and pre-crystalized chair-side CAD-CAM lithium disilicate restorations after required and additional sintering processes. J. Adv. Prosthodont. 2022, 14, 56–62. [Google Scholar] [CrossRef] [PubMed]
- Stawarczyk, B.; Mandl, A.; Liebermann, A. Modern CAD/CAM silicate ceramics, their translucency level and impact of hydrothermal aging on translucency, Martens hardness, biaxial flexural strength and their reliability. J. Mech. Behav. Biomed. Mater. 2021, 118, 104456. [Google Scholar] [CrossRef]
- Kang, S.Y.; Yu, J.M.; Lee, J.S.; Park, K.S.; Lee, S.Y. evaluation of the milling accuracy of zirconia-reinforced lithium silicate crowns fabricated using the dental medical device system: A three-dimensional analysis. Materials 2020, 13, 4680. [Google Scholar] [CrossRef]
- Liebermann, A.; Mandl, A.; Eichberger, M.; Stawarczyk, B. Impact of resin composite cement on color of computer-aided design/computer-aided manufacturing ceramics. J. Esthet. Restor. Dent. 2021, 33, 786–794. [Google Scholar] [CrossRef]
- Yin, R.; Jang, Y.-S.; Lee, M.-H.; Bae, T.-S. Comparative evaluation of mechanical properties and wear ability of five CAD/CAM dental blocks. Materials 2019, 12, 2252. [Google Scholar] [CrossRef] [Green Version]
- Vichi, A.; Carrabba, M.; Paravina, R.; Ferrari, M. Translucency of ceramic materials for CEREC CAD/CAM system. J. Esthet. Restor. Dent. 2014, 26, 224–231. [Google Scholar] [CrossRef]
- Dogan, D.O.; Gorler, O.; Mutaf, B.; Ozcan, M.; Eyuboglu, G.B.; Ulgey, M. Fracture resistance of molar crowns fabricated with monolithic all-ceramic CAD/CAM materials cemented on titanium abutments: An in vitro study. J. Prosthodont. 2017, 26, 309–314. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Della Bona, A.; Nogueira, A.D.; Pecho, O.E. Optical properties of CAD–CAM ceramic systems. J. Dent. 2014, 42, 1202–1209. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Wang, F.; Takahashi, H.; Iwasaki, N. Translucency of dental ceramics with different thicknesses. J. Prosthet. Dent. 2013, 110, 14–20. [Google Scholar] [CrossRef]
- Ilie, N.; Hickel, R. Correlation between ceramics translucency and polymerization efficiency through ceramics. Dent. Mater. 2008, 24, 908–914. [Google Scholar] [CrossRef]
- Alp, G.; Subasi, M.G.; Johnston, W.M.; Yilmaz, B. Effect of surface treatments and coffee thermocycling on the color and translucency of CAD-CAM monolithic glass-ceramic. J. Prosthet. Dent. 2018, 120, 263–268. [Google Scholar] [CrossRef]
- Acar, O.; Yilmaz, B.; Altintas, S.H.; Chandrasekaran, I.; Johnston, W.M. Color stainability of CAD/CAM and nanocomposite resin materials. J. Prosthet. Dent. 2016, 115, 71–75. [Google Scholar] [CrossRef]
- Arif, R.; Yilmaz, B.; Johnston, W.M. In vitro color stainability and relative translucency of CAD-CAM restorative materials used for laminate veneers and complete crowns. J. Prosthet. Dent. 2019, 122, 160–166. [Google Scholar] [CrossRef]
- Subaşı, M.G.; Alp, G.; Johnston, W.M.; Yilmaz, B. Effect of thickness on optical properties of monolithic CAD-CAM ceramics. J. Dent. 2018, 71, 38–42. [Google Scholar] [CrossRef]
- Bankoglu Gungor, M.; Karakoca Nemli, S. Fracture resistance of CAD-CAM monolithic ceramic and veneered zirconia molar crowns after aging in a mastication simulator. J. Prosthet. Dent. 2018, 119, 473–480. [Google Scholar] [CrossRef]
- Furtado de Mendonca, A.; Shahmoradi, M.; Gouvea, C.V.D.; De Souza, G.M.; Ellakwa, A. microstructural and mechanical characterization of CAD/CAM materials for monolithic dental restorations. J. Prosthodont. 2019, 28, e587–e594. [Google Scholar] [CrossRef]
- Choi, S.; Yoon, H.-I.; Park, E.-J. Load-bearing capacity of various CAD/CAM monolithic molar crowns under recommended occlusal thickness and reduced occlusal thickness conditions. J. Adv. Prosthodont. 2017, 9, 423–431. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Chen, S.E.; Park, A.C.; Wang, J.; Knoernschild, K.L.; Campbell, S.; Yang, B. Fracture resistance of various thickness e.max cad lithium disilicate crowns cemented on different supporting substrates: An in vitro study. J. Prosthodont. 2019, 28, 997–1004. [Google Scholar] [CrossRef] [PubMed]
- Alarwali, A.M.; Kutty, M.G.; Al-Haddad, A.Y.; Gonzalez, M.A.G. Fracture resistance of three different all-ceramic crowns: In vitro study. Am. J. Dent. 2018, 31, 39–44. [Google Scholar] [PubMed]
- Barizon, K.T.; Bergeron, C.; Vargas, M.A.; Qian, F.; Cobb, D.S.; Gratton, D.G.; Geraldeli, S. Ceramic materials for porcelain veneers. Part I: Correlation between translucency parameters and contrast ratio. J. Prosthet. Dent. 2013, 110, 397–401. [Google Scholar] [CrossRef] [PubMed]
- Barizon, K.T.L.; Bergeron, C.; Vargas, M.A.; Qian, F.; Cobb, D.S.; Gratton, D.G.; Geraldeli, S. Ceramic materials for porcelain veneers: Part II. Effect of material, shade, and thickness on translucency. J. Prosthet. Dent. 2014, 112, 864–870. [Google Scholar] [CrossRef] [PubMed]
- Kelly, J.R. Clinically relevant approach to failure testing of all-ceramic restorations. J. Prosthet. Dent. 1999, 81, 652–661. [Google Scholar] [CrossRef]
- Elsaka, S.E.; Elnaghy, A.M. Mechanical properties of zirconia reinforced lithium silicate glass-ceramic. Dent. Mater. 2016, 32, 908–914. [Google Scholar] [CrossRef]
- Hamza, T.A.; Sherif, R.M. Fracture resistance of monolithic glass-ceramics versus bilayered zirconia-based restorations. J. Prosthodont. 2019, 28, e259–e264. [Google Scholar] [CrossRef] [Green Version]
- Zimmermann, M.; Ender, A.; Attin, T.; Mehl, A. Fracture load of three-unit full-contour fixed dental prostheses fabricated with subtractive and additive CAD/CAM technology. Clin. Oral. Investig. 2020, 24, 1035–1042. [Google Scholar] [CrossRef]
- Zimmermann, M.; Egli, G.; Zaruba, M.; Mehl, A. Influence of material thickness on fractural strength of CAD/CAM fabricated ceramic crowns. Dent. Mater. J. 2017, 29, 778–783. [Google Scholar] [CrossRef] [Green Version]
- Waltimo, A.; Könönen, M. A novel bite force recorder and maximal isometric bite force values for healthy young adults. Eur. J. Oral Sci. 1993, 101, 171–175. [Google Scholar] [CrossRef] [PubMed]
- Paravina, R.D.; Ghinea, R.; Herrera, L.J.; Bona, A.D.; Igiel, C.; Linninger, M.; Sakai, M.; Takahashi, H.; Tashkandi, E.; Perez Mdel, M. Color difference thresholds in dentistry. J. Esthet. Restor. Dent. 2015, 27 (Suppl. S1), S1–S9. [Google Scholar] [CrossRef] [PubMed]
- Salas, M.; Lucena, C.; Herrera, L.J.; Yebra, A.; Della Bona, A.; Pérez, M.M. Translucency thresholds for dental materials. Dent. Mater. 2018, 34, 1168–1174. [Google Scholar] [CrossRef] [PubMed]

| Material | Classification | Manufacturer |
|---|---|---|
| Amber Mill | Nano-lithium disilicate glass-ceramic, NLD | Hass, Gangneung, Korea |
| IPS e.max CAD | Lithium disilicate glass-ceramic, LDS | Ivoclar Vivadent, Schaan, Liechtenstein |
| Vita Suprinity | Zirconia-reinforced lithium silicate glass-ceramic, ZLS | Vita Zahnfabrick, Bad Säckingen, Germany |
| BRILLIANT Crios | Reinforced composite resin | Coltène AG, Altstätten, Switzerland |
| B (°C) | S (min) | t1/t2 (°C/min) | T1/T2 (°C) | H1/H2 (min) | Vac. 1 (°C)/Vac. 2 (°C) | L (°C) | tL | |
|---|---|---|---|---|---|---|---|---|
| Amber Mill | 400 °C | 3 min | 60 °C/min | 815 °C | 15 min | 550/815 °C | 690 °C | 0 |
| IPS e.max CAD | 403 °C | 6 min | 90/34 °C/min | 830/850 °C | 10 s–7 min | 550–830/830–850 °C | 710 °C | 0 |
| Vita Suprinity | 400 °C | 4 min | 55 °C/min | 840 °C | 8 min | 410/839 °C | 680 °C | 0 |
| Color Change | Sum of Squares | df | Mean Square | F | p |
|---|---|---|---|---|---|
| Material | 1.912 | 2 | 0.956 | 74.726 | <0.001 |
| Thickness | 2.958 | 1 | 2.958 | 231.235 | <0.001 |
| Material × Thickness | 0.671 | 2 | 0.336 | 26.246 | <0.001 |
| RTP | Sum of Squares | df | Mean Square | F | p |
| Material | 710.535 | 2 | 355.268 | 89.110 | <0.001 |
| Thickness | 3061.061 | 1 | 3061.061 | 767.793 | <0.001 |
| Condition | 67.628 | 1 | 67.628 | 16.963 | <0.001 |
| Material × Thickness | 246.614 | 2 | 123.307 | 30.929 | <0.001 |
| Material × Condition | 28.675 | 2 | 14.337 | 3.596 | 0.035 |
| Thickness × Condition | 24.219 | 1 | 24.219 | 6.075 | 0.017 |
| Material × Thickness × Condition | 34.709 | 2 | 17.354 | 4.353 | 0.018 |
| Pairs | Baseline | After Coffee Thermocycling |
|---|---|---|
| 0.7 NLD-0.7 LDS | 0.946 | 0.265 |
| 0.7 NLD-0.7 ZLS | 0.004 | 0.892 |
| 0.7 NLD-1.5 NLD | <0.001 | <0.001 |
| 0.7 LDS-0.7 ZLS | 0.036 | 0.85 |
| 0.7 LDS-1.5 LDS | <0.001 | <0.001 |
| 0.7 ZLS-1.5 ZLS | <0.001 | <0.001 |
| 1.5 NLD-1.5 LDS | >0.05 | 0.517 |
| 1.5 NLD-1.5 ZLS | <0.001 | <0.001 |
| 1.5 LDS-1.5 ZLS | <0.001 | <0.001 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Donmez, M.B.; Olcay, E.O.; Demirel, M. Load-to-Failure Resistance and Optical Characteristics of Nano-Lithium Disilicate Ceramic after Different Aging Processes. Materials 2022, 15, 4011. https://doi.org/10.3390/ma15114011
Donmez MB, Olcay EO, Demirel M. Load-to-Failure Resistance and Optical Characteristics of Nano-Lithium Disilicate Ceramic after Different Aging Processes. Materials. 2022; 15(11):4011. https://doi.org/10.3390/ma15114011
Chicago/Turabian StyleDonmez, Mustafa Borga, Emin Orkun Olcay, and Münir Demirel. 2022. "Load-to-Failure Resistance and Optical Characteristics of Nano-Lithium Disilicate Ceramic after Different Aging Processes" Materials 15, no. 11: 4011. https://doi.org/10.3390/ma15114011
APA StyleDonmez, M. B., Olcay, E. O., & Demirel, M. (2022). Load-to-Failure Resistance and Optical Characteristics of Nano-Lithium Disilicate Ceramic after Different Aging Processes. Materials, 15(11), 4011. https://doi.org/10.3390/ma15114011






