A Narrative Review of u-HA/PLLA, a Bioactive Resorbable Reconstruction Material: Applications in Oral and Maxillofacial Surgery
Abstract
:1. Introduction
- -
- First-generation: homogeneous polymers.
- -
- Second-generation: copolymers.
- -
- Third-generation: composites of inorganic/bioceramic fibers or particles, and organic polymers.
- -
- Fourth-generation: composites of inorganic/bioceramic fibers or particles and organic copolymers.
| Generation | Name | Structure | Mechanical Strength | Biocompatibility | Bioactive/Osteoconductivity | Degradation Period | Clinical Applications | |
|---|---|---|---|---|---|---|---|---|
| 1 | PGA |  [39] [39] | High [29] | High [59] | − [59] | 4–12 months [60] | Tissue engineering. Drug-delivery systems [61] | |
| PLA | PLLA |  [62] [62] | High [63] | High [64] | − [51] | > 3.5 years [65] | Tissue engineering. Drug-delivery systems. Fixation devices [66] | |
| PDLA |  [62] [62] | High [63] | High [64] | − [64] | Longer than PLLA [34] | Tissue engineering. Drug-delivery systems, [66] | ||
| PDLLA | 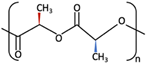 [62] [62] | Lower than PLLA [37] | High [64] | − [64] | 12–30 months [37] | Tissue engineering. Drug-delivery systems [66] | ||
| 2 | PLLA/PGA | 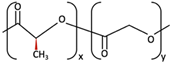 [67] [67] | High [37] | High [68] | − [50] | 12–18 months [44] | Tissue engineering. Drug-delivery systems. Fixation devices [66] | |
| 3 | u-HA/PDLLA | Ca10(PO4)6(OH)2 + 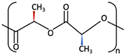 | Low [54] | High [55] | + [56] | 12–18 months [69] | Tissue engineering. Fixation devices [70] | |
| u-HA/PLLA | Ca10(PO4)6(OH)2 +  | Higher than PLLA [19] | High [19] | + [19] | > 5 years [49] | Tissue engineering. Fixation devices [70] | ||
| 4 | u-HA/PLLA/PGA | Ca10(PO4)6(OH)2 + 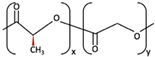 | Similar to u-HA/PLLA [71] | High [72] | + [71] | 2–3 years [73] | Tissue engineering. Fixation devices [73] | |
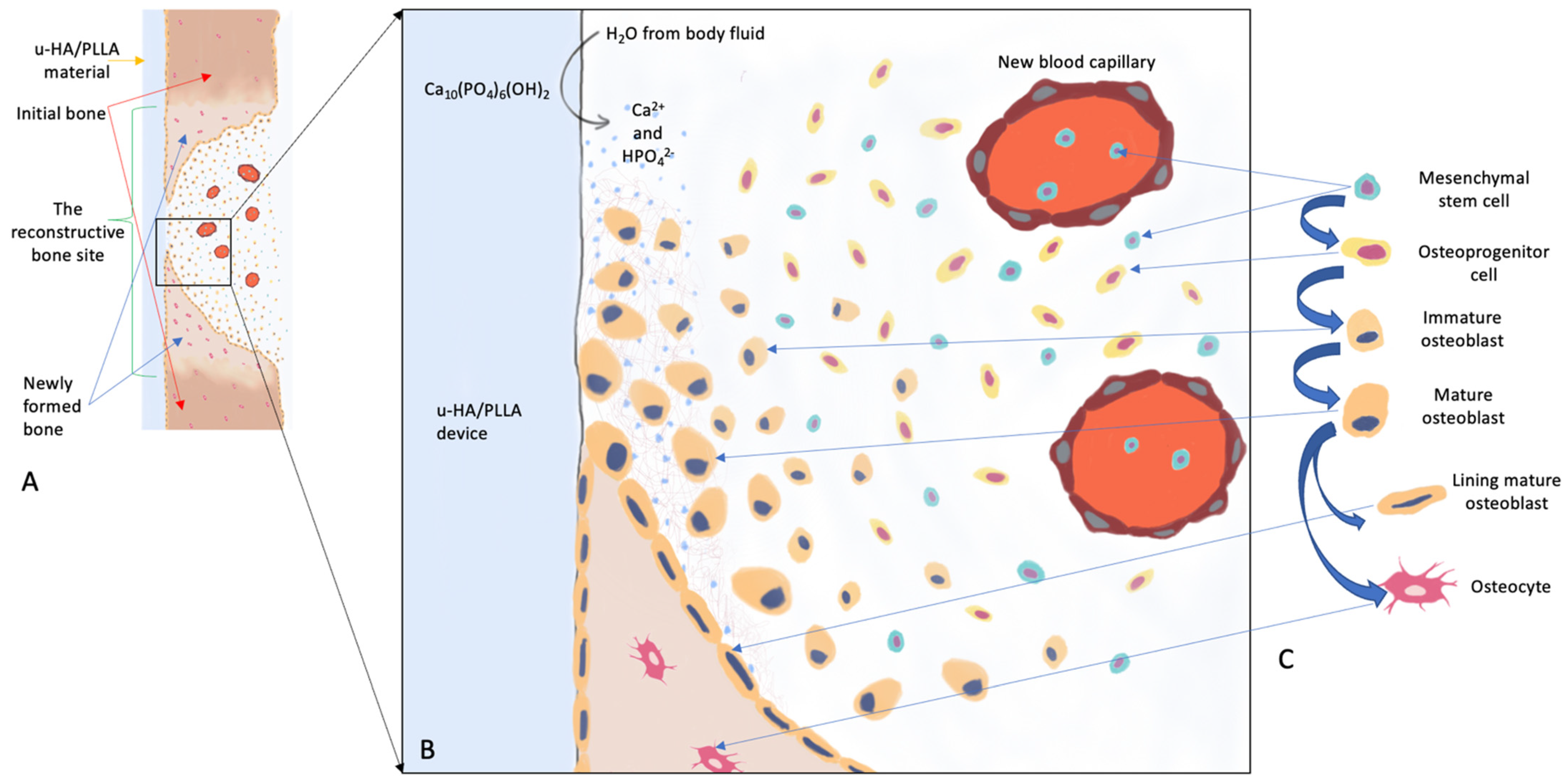
2. u-HA/PLLA, an Outstanding Bioresorbable Composite
2.1. Uncalcined and Unsintered Hydroxyapatite
2.2. PLA (PLLA, PDLA, PDLLA)
2.3. Forged Composite of u-HA Particles and PLLA Polymer
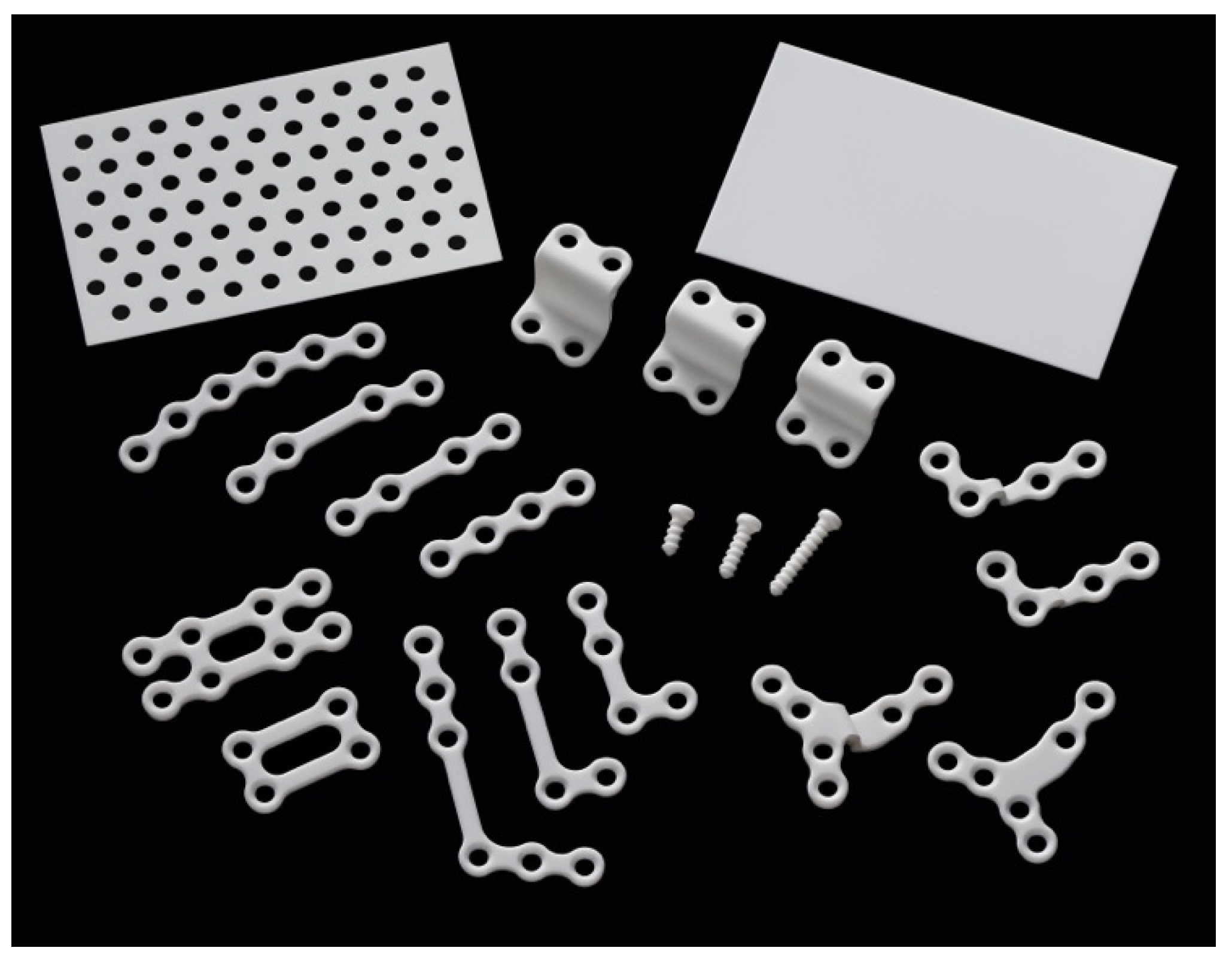
3. Clinical Applications of u-HA/PLLA in Oral and Maxillofacial Surgery
3.1. Maxillofacial Trauma
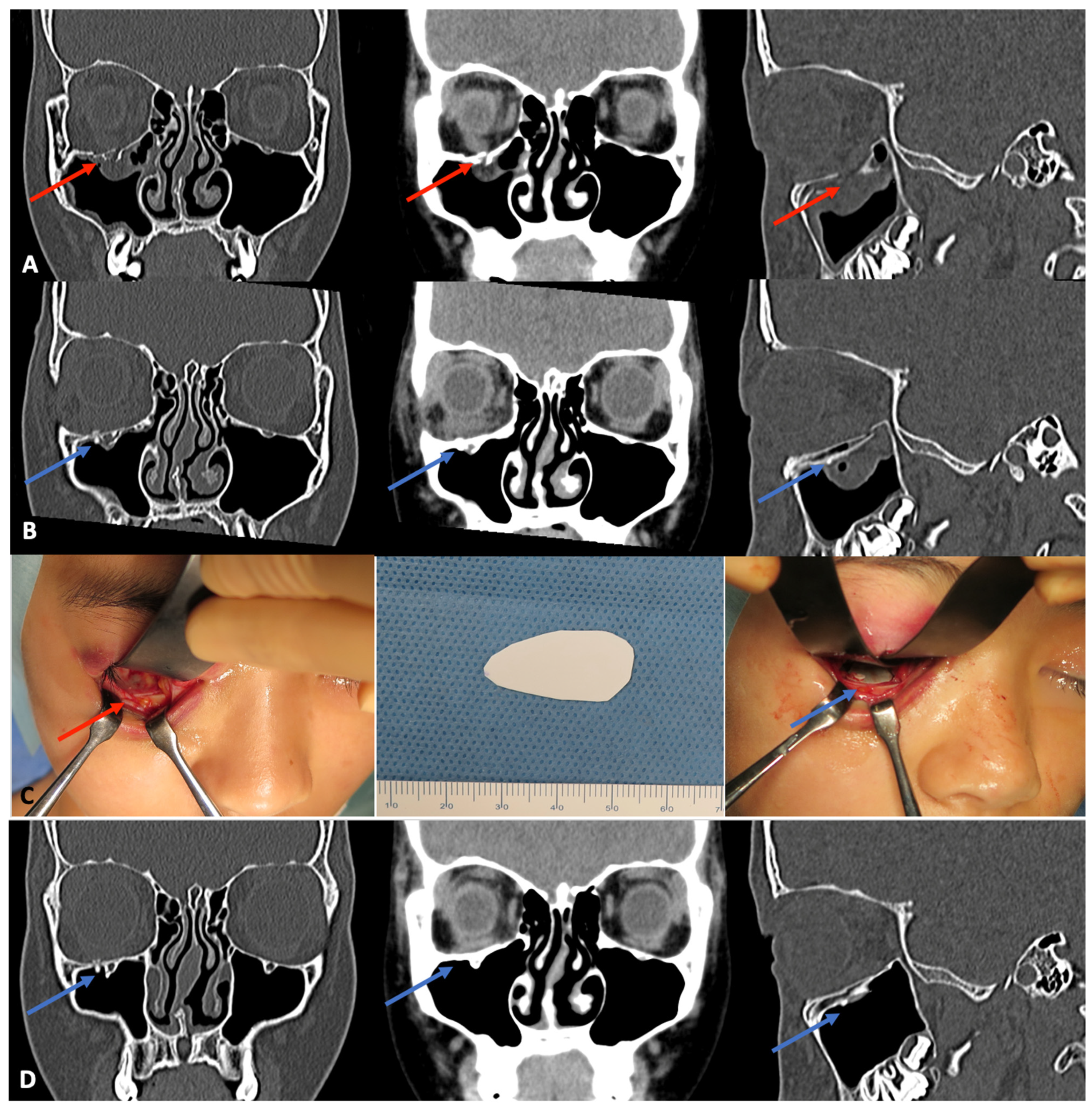
3.1.1. Orbital Wall Fractures
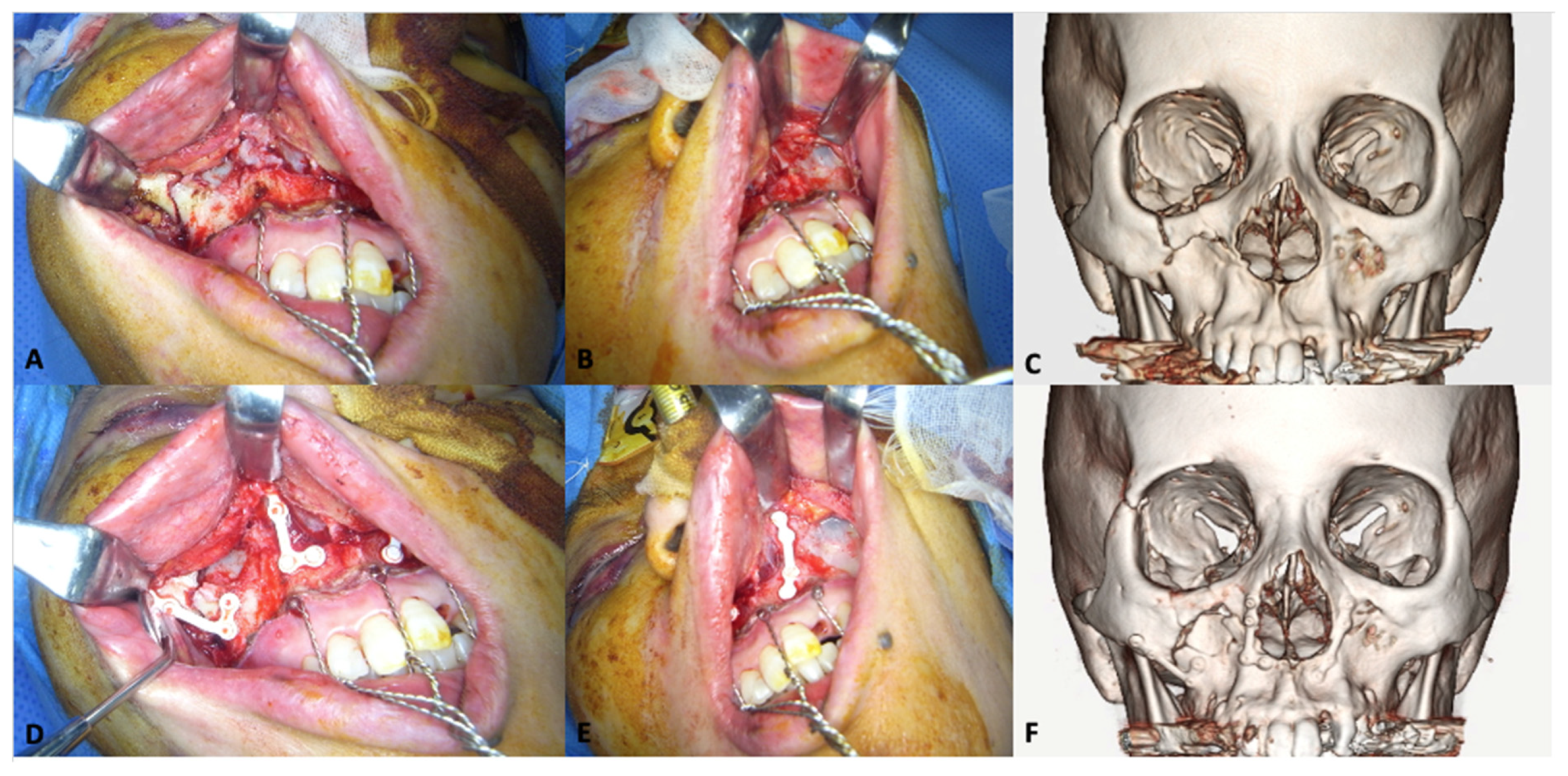
3.1.2. Midfacial Fractures
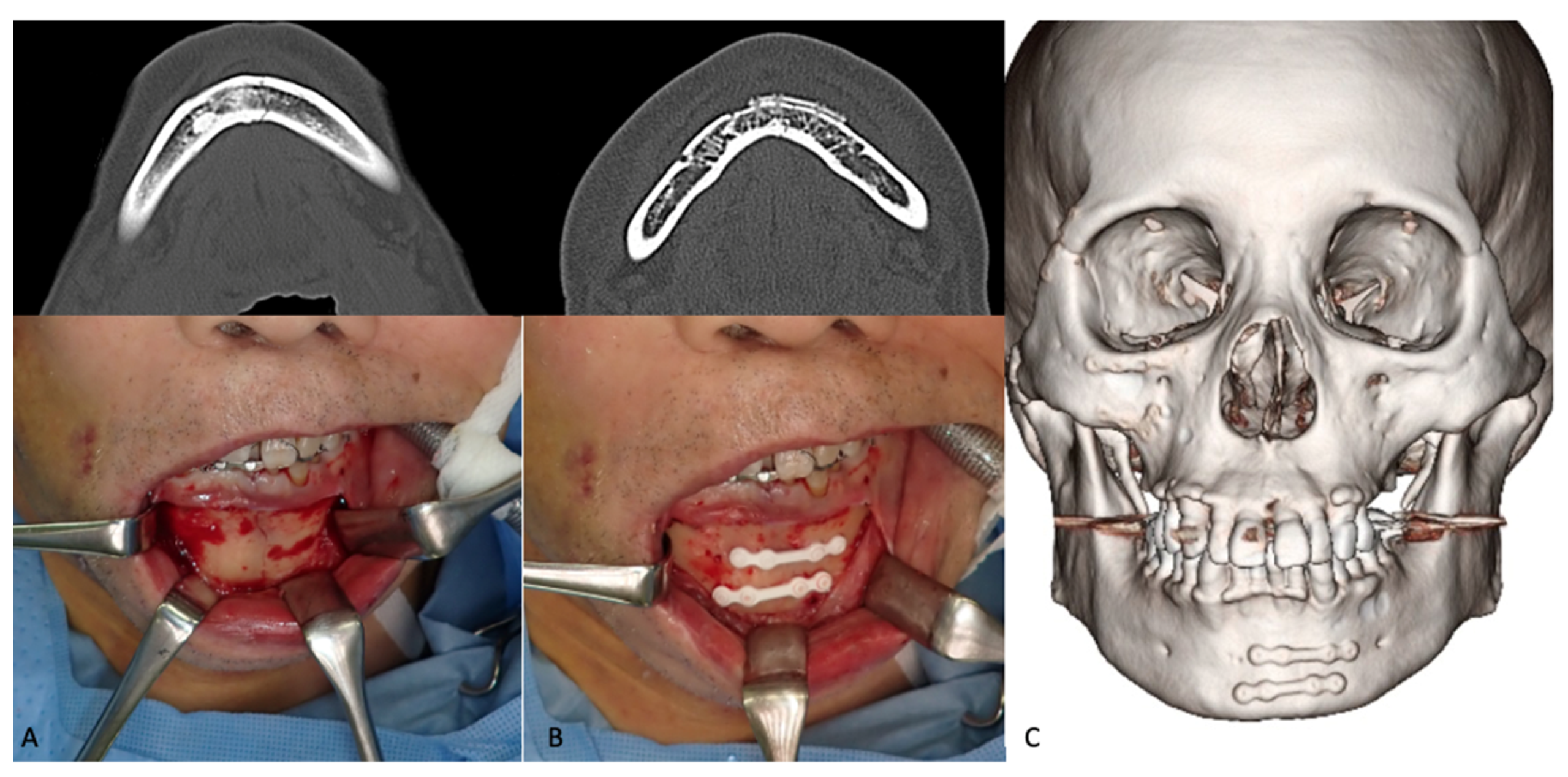
3.1.3. Mandibular Fractures
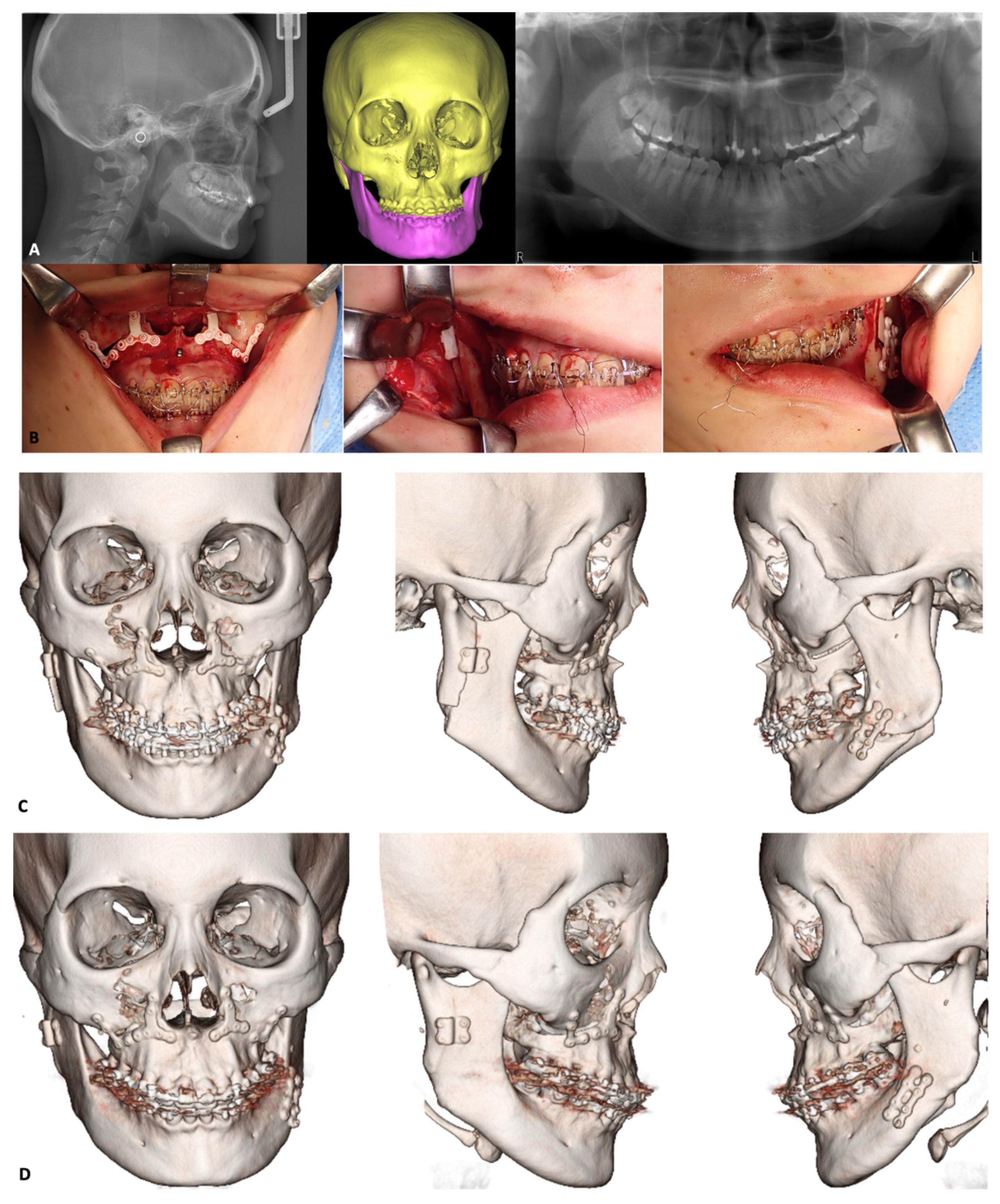
3.2. Orthognathic Surgery
3.2.1. Le Fort I osteotomy
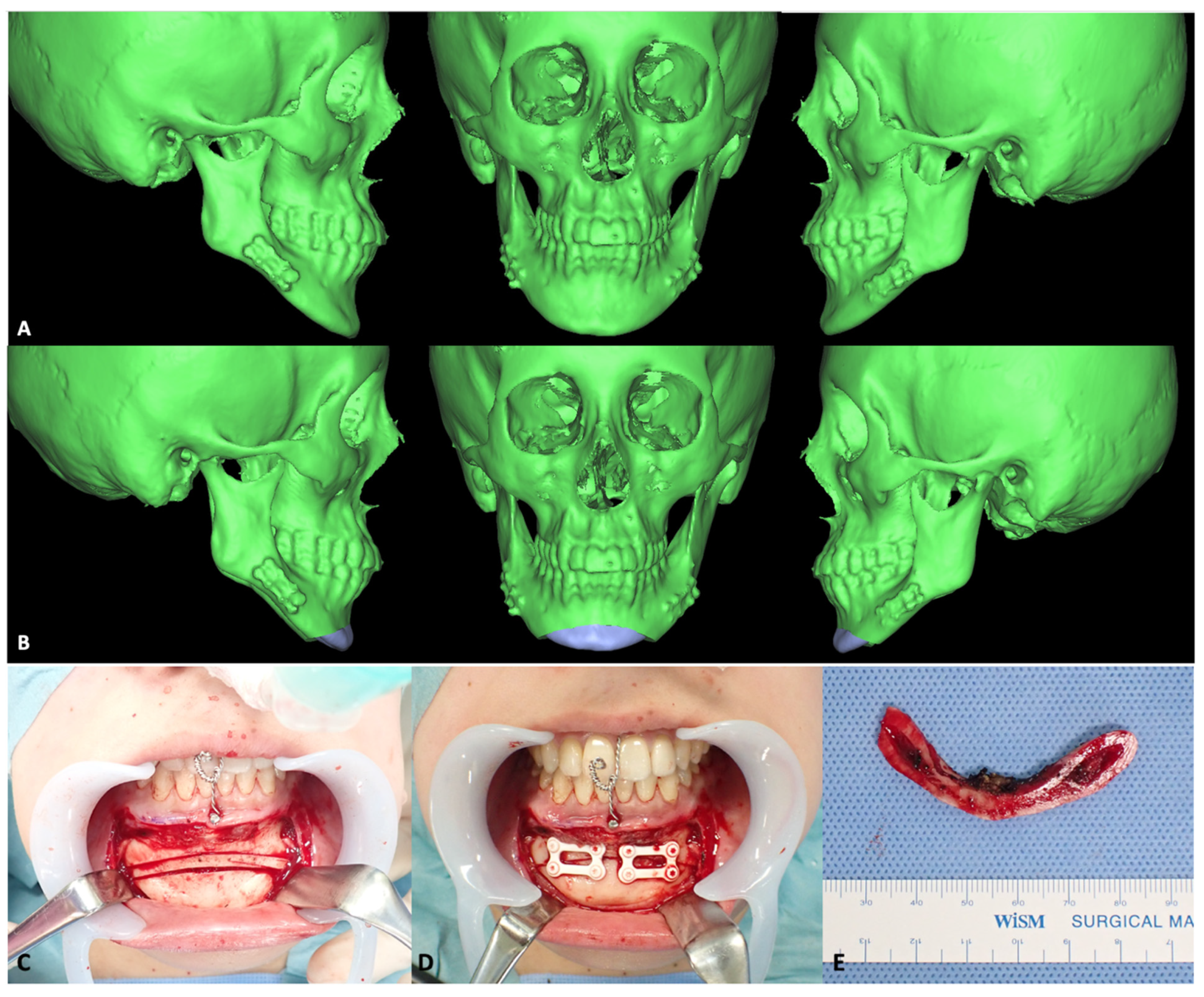
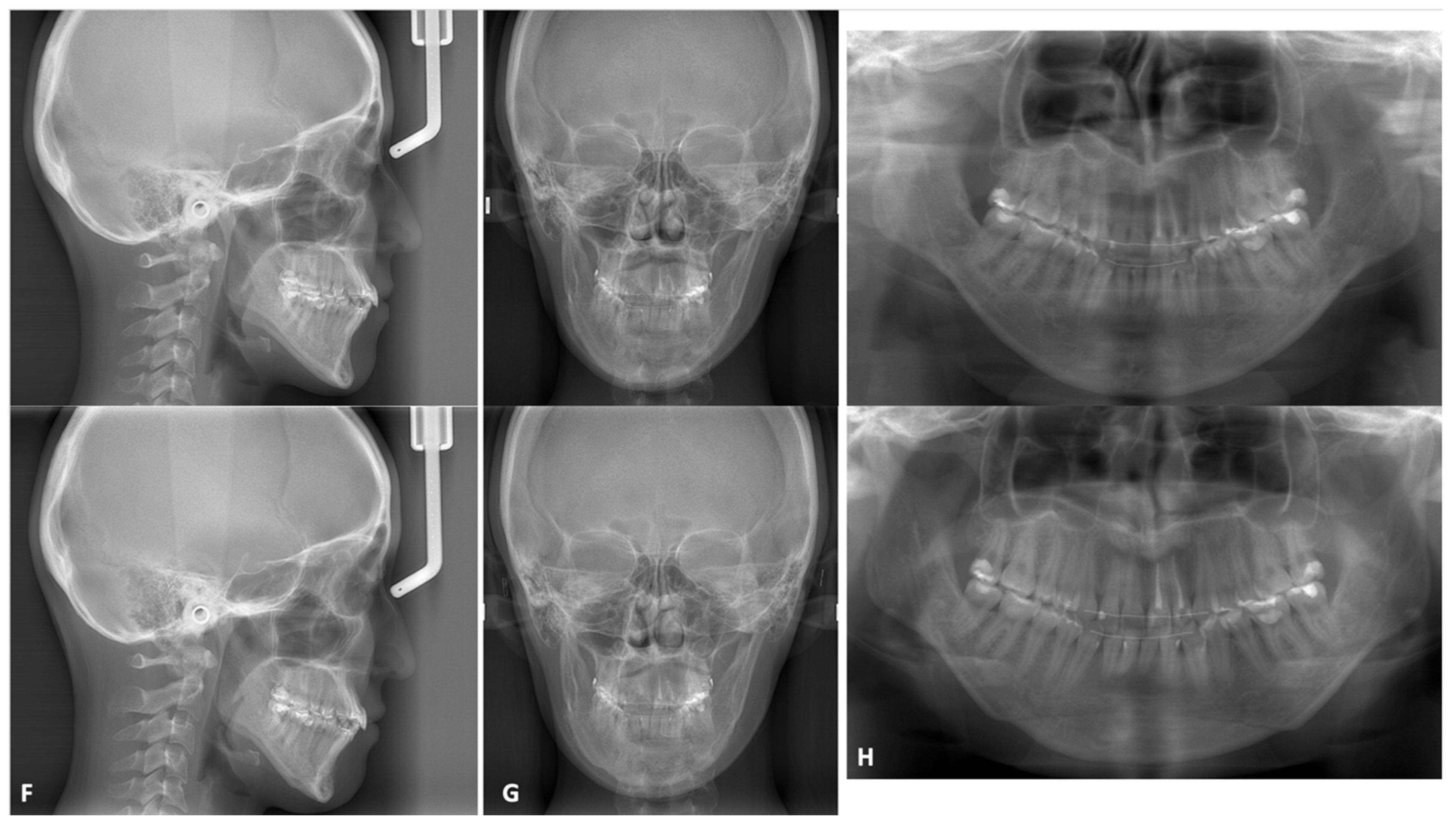
3.2.2. Mandibular Osteotomies
3.3. Other Reconstructive Applications
4. Clinical Complications of u-HA/PLLA
5. Future Perspectives
6. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Montovani, J.C.; de Campos, L.M.P.; Gomes, M.A.; de Moraes, V.R.S.; Ferreira, F.D.; Nogueira, E.A. Etiology and incidence facial fractures in children and adults. Braz. J. Otorhinolaryngol. Engl. Ed. 2006, 72, 235–241. [Google Scholar] [CrossRef] [Green Version]
- Gruss, J.S. Complex Craniomaxillofacial Trauma: Evolving Concepts in Management. A Trauma Unit’s Experience—1989 Fraser B. Gurd Lecture. J. Trauma Acute Care Surg. 1990, 30, 377–383. [Google Scholar] [CrossRef]
- Bell, R.; Kiyak, H.A.; Joondeph, D.R.; McNeill, R.W.; Wallen, T.R. Perceptions of facial profile and their influence on the decision to undergo orthognathic surgery. Am. J. Orthod. 1985, 88, 323–332. [Google Scholar] [CrossRef]
- Guo, S.; Qu, X.; He, X.; Zhou, T.; Duan, B. Powder injection molding of Ti–6Al–4V alloy. J. Mater. Process. Technol. 2006, 173, 310–314. [Google Scholar] [CrossRef]
- Quinn, R.K.; Armstrong, N.R. Electrochemical and Surface Analytical Characterization of Titanium and Titanium Hydride Thin Film Electrode Oxidation. J. Electrochem. Soc. 1978, 125, 1790. [Google Scholar] [CrossRef]
- Leventhal, G.S. Titanium, a metal for surgery. J. Bone Joint Surg. Am. 1951, 33, 473–474. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Francel, T.J.; Birely, B.C.; Ringelman, P.R.; Manson, P.N. The fate of plates and screws after facial fracture reconstruction. Plast. Reconstr. Surg. 1992, 90, 568–573. [Google Scholar] [CrossRef] [PubMed]
- Kahnberg, K.E.; Engström, H. Recovery of maxillary sinus and tooth sensibility after le Fort I osteotomy. Br. J. Oral Maxillofac. Surg. 1987, 25, 68–73. [Google Scholar] [CrossRef]
- Resnick, J.I.; Kinney, B.M.; Kawamoto, H.K. The effect of rigid internal fixation on cranial growth. Ann. Plast. Surg. 1990, 25, 372–374. [Google Scholar] [CrossRef] [PubMed]
- Lin, K.Y.; Bartlett, S.P.; Yaremchuk, M.J.; Grossman, R.F.; Udupa, J.K.; Whitaker, L.A. An experimental study on the effect of rigid fixation on the developing craniofacial skeleton. Plast. Reconstr. Surg. 1991, 87, 229–235. [Google Scholar] [CrossRef]
- Eppley, B.L.; Platis, J.M.; Sadove, A.M. Experimental effects of bone plating in infancy on craniomaxillofacial skeletal growth. Cleft Palate-Craniofacial J. 1993, 30, 164–169. [Google Scholar] [CrossRef]
- Gilardino, M.S.; Chen, E.; Bartlett, S.P. Choice of Internal Rigid Fixation Materials in the Treatment of Facial Fractures. Craniomaxillofacial Trauma Reconstr. 2009, 2, 49–60. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Pan, Z.; Patil, P.M. Titanium osteosynthesis hardware in maxillofacial trauma surgery: To remove or remain? A retrospective study. Eur. J. Trauma Emerg. Surg. Off. Publ. Eur. Trauma Soc. 2014, 40, 587–591. [Google Scholar] [CrossRef]
- Haers, P.E.; Suuronen, R.; Lindqvist, C.; Sailer, H. Biodegradable polylactide plates and screws in orthognathic surgery: Technical note. J. Cranio-Maxillofacial Surg. 1998, 26, 87–91. [Google Scholar] [CrossRef]
- Buijs, G.J.; van Bakelen, N.B.; Jansma, J.; de Visscher, J.G.A.M.; Hoppenreijs, T.J.M.; Bergsma, J.E.; Stegenga, B.; Bos, R.R.M. A randomized clinical trial of biodegradable and titanium fixation systems in maxillofacial surgery. J. Dent. Res. 2012, 91, 299–304. [Google Scholar] [CrossRef]
- van Bakelen, N.B.; Buijs, G.J.; Jansma, J.; de Visscher, J.G.A.M.; Hoppenreijs, T.J.M.; Bergsma, J.E.; Stegenga, B.; Bos, R.R.M. Decision-making considerations in application of biodegradable fixation systems in maxillofacial surgery—A retrospective cohort study. J. Cranio-Maxillofacial Surg. 2014, 42, 417–422. [Google Scholar] [CrossRef] [PubMed]
- Kulkarni, R.K.; Pani, K.C.; Neuman, C.; Leonard, F. Polylactic acid for surgical implants. Arch. Surg. Chic. 1966, 93, 839–843. [Google Scholar] [CrossRef] [PubMed]
- Cutright, D.E.; Hunsuck, E.E.; Beasley, J.D. Fracture reduction using a biodegradable material, polylactic acid. J. Oral Surg. Am. Dent. Assoc. 1971, 29, 393–397. [Google Scholar]
- Shikinami, Y.; Okuno, M. Bioresorbable devices made of forged composites of hydroxyapatite (HA) particles and poly-L-lactide (PLLA): Part I. Basic characteristics. Biomaterials 1999, 20, 859–877. [Google Scholar] [CrossRef]
- Piskin, E. Biodegradable polymers as biomaterials. J. Biomater. Sci. Polym. Ed. 1995, 6, 775–795. [Google Scholar] [CrossRef] [PubMed]
- Yoda, R. Elastomers for biomedical applications. J. Biomater. Sci. Polym. Ed. 1998, 9, 561–626. [Google Scholar] [CrossRef] [PubMed]
- Saad, B.; Neuenschwander, P.; Uhlschmid, G.K.; Suter, U.W. New versatile, elastomeric, degradable polymeric materials for medicine. Int. J. Biol. Macromol. 1999, 25, 293–301. [Google Scholar] [CrossRef]
- Chu, C. Biodegradable polymeric biomaterials: An updated overview. Biomaterials 2003, 95–115. [Google Scholar] [CrossRef]
- Suuronen, R.; Kallela, I.; Lindqvist, C. Bioabsorbable plates and screws: Current state of the art in facial fracture repair. J. Cranio-Maxillofac. Trauma 2000, 6, 19–27; discussion 28–30. [Google Scholar]
- Mohamed-Hashem, I.K.; Mitchell, D.A. Resorbable implants (plates and screws) in orthognathic surgery. J. Orthod. 2000, 27, 198–199. [Google Scholar] [CrossRef]
- Ylikontiola, L.; Sundqvuist, K.; Sàndor, G.K.B.; Törmälä, P.; Ashammakhi, N. Self-reinforced bioresorbable poly-L/DL-lactide [SR-P(L/DL)LA] 70/30 miniplates and miniscrews are reliable for fixation of anterior mandibular fractures: A pilot study. Oral Surg. Oral Med. Oral Pathol. Oral Radiol. Endod. 2004, 97, 312–317. [Google Scholar] [CrossRef]
- Edwards, R.C.; Kiely, K.D.; Eppley, B.L. The fate of resorbable poly-L-lactic/polyglycolic acid (LactoSorb) bone fixation devices in orthognathic surgery. J. Oral Maxillofac. Surg. 2001, 59, 19–25. [Google Scholar] [CrossRef]
- Peltoniemi, H.H.; Tulamo, R.M.; Toivonen, T.; Hallikainen, D.; Törmälä, P.; Waris, T. Biodegradable semirigid plate and miniscrew fixation compared with rigid titanium fixation in experimental calvarial osteotomy. J. Neurosurg. 1999, 90, 910–917. [Google Scholar] [CrossRef] [PubMed]
- Törmälä, P. Biodegradable self-reinforced composite materials; Manufacturing structure and mechanical properties. Clin. Mater. 1992, 10, 29–34. [Google Scholar] [CrossRef]
- Bell, R.B.; Kindsfater, C.S. The Use of Biodegradable Plates and Screws to Stabilize Facial Fractures. J. Oral Maxillofac. Surg. 2006, 64, 31–39. [Google Scholar] [CrossRef] [PubMed]
- Seppänen-Kaijansinkko, R.; Lindqvist, C. Bioresorbable Materials for Bone Fixation: Review of Biological Concepts and Mechanical Aspects; Springer: New York, NY, USA, 2019; pp. 121–128. ISBN 978-1-4939-1528-6. [Google Scholar]
- Gajjar, C.; King, M. Resorbable Fiber-Forming Polymers for Biotextile Applications; Springer: New York, NY, USA, 2014. [Google Scholar] [CrossRef]
- Lopes, M.S.; Jardini, A.L.; Filho, R.M. Poly (Lactic Acid) Production for Tissue Engineering Applications. Procedia Eng. 2012, 42, 1402–1413. [Google Scholar] [CrossRef] [Green Version]
- Pihlajamaki, H. Absorbable pins of self-reinforced poly-L-lactc acid for fixation of fractures and osteotomies. J Bone Jt. Surg. 1992, 74, 853–857. [Google Scholar] [CrossRef] [PubMed]
- Luckachan, G.E.; Pillai, C.K.S. Biodegradable Polymers- A Review on Recent Trends and Emerging Perspectives. J. Polym. Environ. 2011, 19, 637–676. [Google Scholar] [CrossRef]
- Kricheldorf, H.R. Syntheses and application of polylactides. Chemosphere 2001, 43, 49–54. [Google Scholar] [CrossRef]
- Middleton, J.C.; Tipton, A.J. Synthetic biodegradable polymers as orthopedic devices. Biomaterials 2000, 21, 2335–2346. [Google Scholar] [CrossRef]
- Bergsma, J.E.; Rozema, F.R.; Bos, R.R.; Boering, G.; de Bruijn, W.C.; Pennings, A.J. In vivo degradation and biocompatibility study of in vitro pre-degraded as-polymerized polyactide particles. Biomaterials 1995, 16, 267–274. [Google Scholar] [CrossRef] [Green Version]
- Park, Y.-W. Bioabsorbable osteofixation for orthognathic surgery. Maxillofac. Plast. Reconstr. Surg. 2015, 37, 6. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Pina, S.; Ferreira, J. Bioresorbable Plates and Screws for Clinical Applications: A Review. J. Health Eng. 2012, 3, 243–260. [Google Scholar] [CrossRef] [Green Version]
- Mazzonetto, R.; Paza, A.O.; Spagnoli, D.B. A retrospective evaluation of rigid fixation in orthognathic surgery using a biodegradable self-reinforced (70L:30DL) polylactide. Int. J. Oral Maxillofac. Surg. 2004, 33, 664–669. [Google Scholar] [CrossRef]
- Kim, B.C.; Padwa, B.L.; Park, H.-S.; Jung, Y.-S. Stability of Maxillary Position After Le Fort I Osteotomy Using Self-Reinforced Biodegradable Poly-70L/30DL-Lactide Miniplates and Screws. J. Oral Maxillofac. Surg. 2011, 69, 1442–1446. [Google Scholar] [CrossRef]
- Miller, R.A.; Brady, J.M.; Cutright, D.E. Degradation rates of oral resorbable implants (polylactates and polyglycolates): Rate modification with changes in PLA/PGA copolymer ratios. J. Biomed. Mater. Res. 1977, 11, 711–719. [Google Scholar] [CrossRef] [PubMed]
- Wiltfang, J.; Merten, H.A.; Schultze-Mosgau, S.; Schrell, U.; Wénzel, D.; Kessler, P. Biodegradable miniplates (LactoSorb): Long-term results in infant minipigs and clinical results. J. Craniofac. Surg. 2000, 11, 239–243. [Google Scholar] [CrossRef] [PubMed]
- Eppley, B.L.; Prevel, C.D.; Sadove, A.M.; Sarver, D. Resorbable bone fixation: Its potential role in cranio-maxillofacial trauma. J. Cranio-Maxillofac. Trauma 1996, 2, 56–60. [Google Scholar]
- Eppley, B.L.; Reilly, M. Degradation characteristics of PLLA-PGA bone fixation devices. J. Craniofac. Surg. 1997, 8, 116–120. [Google Scholar] [CrossRef]
- Quereshy, F.A.; Goldstein, J.A.; Goldberg, J.S.; Beg, Z. The efficacy of bioresorbable fixation in the repair of mandibular fractures: An animal study. J. Oral Maxillofac. Surg. 2000, 58, 1263–1269. [Google Scholar] [CrossRef] [PubMed]
- Sukegawa, S.; Kanno, T.; Matsumoto, K.; Sukegawa-Takahashi, Y.; Masui, M.; Furuki, Y. Complications of a poly-L-lactic acid and polyglycolic acid osteosynthesis device for internal fixation in maxillofacial surgery. Odontology 2018, 106, 360–368. [Google Scholar] [CrossRef]
- Shikinami, Y.; Matsusue, Y.; Nakamura, T. The complete process of bioresorption and bone replacement using devices made of forged composites of raw hydroxyapatite particles/poly l-lactide (F-u-HA/PLLA). Biomaterials 2005, 26, 5542–5551. [Google Scholar] [CrossRef]
- Barth, J.; Akritopoulos, P.; Graveleau, N.; Barthelemy, R.; Toanen, C.; Saffarini, M. Efficacy of Osteoconductive Ceramics in Bioresorbable Screws for Anterior Cruciate Ligament Reconstruction: A Prospective Intrapatient Comparative Study. Orthop. J. Sports Med. 2016, 4, 2325967116647724. [Google Scholar] [CrossRef] [Green Version]
- Dong, Q.N.; Kanno, T.; Bai, Y.; Sha, J.; Hideshima, K. Bone Regeneration Potential of Uncalcined and Unsintered Hydroxyapatite/Poly l-lactide Bioactive/Osteoconductive Sheet Used for Maxillofacial Reconstructive Surgery: An In Vivo Study. Materials 2019, 12, 2931. [Google Scholar] [CrossRef] [Green Version]
- Matsumoto, M.; Chosa, E.; Nabeshima, K.; Shikinami, Y.; Tajima, N. Influence of bioresorbable, unsintered hydroxyapatite/poly-L-lactide composite films on spinal cord, nerve roots, and epidural space. J. Biomed. Mater. Res. 2002, 60, 101–109. [Google Scholar] [CrossRef]
- Wypych, G. 6—Functional Fillers—Applications. In Functional Fillers; Wypych, G., Ed.; ChemTec Publishing: Scarborough, ON, Canada, 2018; pp. 153–179. ISBN 978-1-927885-37-6. [Google Scholar]
- Hasegawa, S.; Tamura, J.; Neo, M.; Goto, K.; Shikinami, Y.; Saito, M.; Nakamura, T. In Vivo Evaluation of Porous Hydroxyapatite/Poly D/L-Lactide Composite for Bone Substitute and Scaffold. Key Eng. Mater. 2005, 284–286, 769–774. [Google Scholar] [CrossRef]
- Hasegawa, S.; Tamura, J.; Neo, M.; Fujibayashi, S.; Goto, K.; Shikinami, Y.; Okazaki, K.; Nakamura, T. In Vivo Evaluation of Porous Hydroxyapatite/Poly D/L-lactide Composite for Bone Substitutes and Scaffolds. Key Eng. Mater. 2006, 309–311, 1311–1314. [Google Scholar] [CrossRef]
- Bai, Y.; Kanno, T.; Tatsumi, H.; Miyamoto, K.; Sha, J.; Hideshima, K.; Matsuzaki, Y. Feasibility of a Three-Dimensional Porous Uncalcined and Unsintered Hydroxyapatite/poly-d/l-lactide Composite as a Regenerative Biomaterial in Maxillofacial Surgery. Materials 2018, 11, 2047. [Google Scholar] [CrossRef] [Green Version]
- Akino, N.; Tachikawa, N.; Munakata, M.; Kasugai, S. The Use of Porous Composite Uncalcined Hydroxyapatite / poly-DL-lactide for Vertical Ridge Augmentation. J. Oral Tissue Eng. 2013, 10, 123–130. [Google Scholar] [CrossRef]
- Akino, N.; Tachikawa, N.; Miyahara, T.; Ikumi, R.; Kasugai, S. Vertical ridge augmentation using a porous composite of uncalcined hydroxyapatite and poly-DL-lactide enriched with types 1 and 3 collagen. Int. J. Implant Dent. 2019, 5, 16. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Manoukian, O.; Sardashti, N.; Stedman, T.; Gailiunas, K.; Ojha, A.; Penalosa, A.; Mancuso, C.; Hobert, M.; Kumbar, S. Biomaterials for Tissue Engineering and Regenerative Medicine; Elsevier: Amsterdam, The Netherlands, 2018; ISBN 978-0-12-801238-3. [Google Scholar]
- Schumann, P.; Lindhorst, D.; Wagner, M.E.H.; Schramm, A.; Gellrich, N.-C.; Rücker, M. Perspectives on resorbable osteosynthesis materials in craniomaxillofacial surgery. Pathobiol. J. Immunopathol. Mol. Cell. Biol. 2013, 80, 211–217. [Google Scholar] [CrossRef] [PubMed]
- Göktürk, E.; Erdal, H. Biomedical Applications of Polyglycolic Acid (PGA). Sak. Üniversitesi Fen Bilim. Enstitüsü Derg. 2017, 21, 1. [Google Scholar] [CrossRef]
- Chan, C.M.; Vandi, L.-J.; Pratt, S.; Halley, P.; Richardson, D.; Werker, A.; Laycock, B. Composites of Wood and Biodegradable Thermoplastics: A Review. Polym. Rev. 2018, 58, 444–494. [Google Scholar] [CrossRef]
- Farah, S.; Anderson, D.G.; Langer, R. Physical and mechanical properties of PLA, and their functions in widespread applications—A comprehensive review. Adv. Drug Deliv. Rev. 2016, 107, 367–392. [Google Scholar] [CrossRef] [Green Version]
- Ramot, Y.; Haim-Zada, M.; Domb, A.J.; Nyska, A. Biocompatibility and safety of PLA and its copolymers. Adv. Drug Deliv. Rev. 2016, 107, 153–162. [Google Scholar] [CrossRef]
- Bergsma, J.E.; de Bruijn, W.C.; Rozema, F.R.; Bos, R.R.; Boering, G. Late degradation tissue response to poly(L-lactide) bone plates and screws. Biomaterials 1995, 16, 25–31. [Google Scholar] [CrossRef] [Green Version]
- DeStefano, V.; Khan, S.; Tabada, A. Applications of PLA in modern medicine. Eng. Regen. 2020, 1, 76–87. [Google Scholar] [CrossRef]
- Rasool, F.; Ahmad, M.; Khan, H.M.; Khan, S.A.; Murtaza, G. Comparative dissolution study of metoprolol tartrate loaded PLGA (50: 50) and PLGA (75: 25) microparticles. Asian J. Chem. 2011, 23, 3815. [Google Scholar]
- Gentile, P.; Chiono, V.; Carmagnola, I.; Hatton, P.V. An Overview of Poly(lactic-co-glycolic) Acid (PLGA)-Based Biomaterials for Bone Tissue Engineering. Int. J. Mol. Sci. 2014, 15, 3640–3659. [Google Scholar] [CrossRef]
- Tanaka, K.; Takemoto, M.; Fujibayashi, S.; Neo, M.; Shikinami, Y.; Nakamura, T. A bioactive and bioresorbable porous cubic composite scaffold loaded with bone marrow aspirate: A potential alternative to autogenous bone grafting. Spine 2011, 36, 441–447. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Kanno, T.; Sukegawa, S.; Furuki, Y.; Nariai, Y.; Sekine, J. Overview of innovative advances in bioresorbable plate systems for oral and maxillofacial surgery. Jpn. Dent. Sci. Rev. 2018, 54, 127–138. [Google Scholar] [CrossRef]
- Ngo, H.X.; Dong, Q.N.; Bai, Y.; Sha, J.; Ishizuka, S.; Okui, T.; Sukegawa, S.; Kanno, T. Bone Regeneration Capacity of Newly Developed Uncalcined/Unsintered Hydroxyapatite and Poly-l-lactide-co-glycolide Sheet in Maxillofacial Surgery: An In Vivo Study. Nanomaterials 2020, 11, 22. [Google Scholar] [CrossRef]
- Ishizuka, S.; Dong, Q.N.; Ngo, H.X.; Bai, Y.; Sha, J.; Toda, E.; Okui, T.; Kanno, T. Bioactive Regeneration Potential of the Newly Developed Uncalcined/Unsintered Hydroxyapatite and Poly-l-Lactide-Co-Glycolide Biomaterial in Maxillofacial Reconstructive Surgery: An In Vivo Preliminary Study. Materials 2021, 14, 2461. [Google Scholar] [CrossRef]
- Kawai, H.; Sukegawa, S.; Nakano, K.; Takabatake, K.; Ono, S.; Nagatsuka, H.; Furuki, Y. Biological Effects of Bioresorbable Materials in Alveolar Ridge Augmentation: Comparison of Early and Slow Resorbing Osteosynthesis Materials. Materials 2021, 14, 3286. [Google Scholar] [CrossRef]
- Batchelar, D.L.; Davidson, M.T.M.; Dabrowski, W.; Cunningham, I.A. Bone-composition imaging using coherent-scatter computed tomography: Assessing bone health beyond bone mineral density. Med. Phys. 2006, 33, 904–915. [Google Scholar] [CrossRef]
- Malmberg, P.; Nygren, H. Methods for the analysis of the composition of bone tissue, with a focus on imaging mass spectrometry (TOF-SIMS). Proteomics 2008, 8, 3755–3762. [Google Scholar] [CrossRef]
- Hu, Y.-Y.; Rawal, A.; Schmidt-Rohr, K. Strongly bound citrate stabilizes the apatite nanocrystals in bone. Proc. Natl. Acad. Sci.USA 2010, 107, 22425–22429. [Google Scholar] [CrossRef] [Green Version]
- Märten, A.; Fratzl, P.; Paris, O.; Zaslansky, P. On the mineral in collagen of human crown dentine. Biomaterials 2010, 31, 5479–5490. [Google Scholar] [CrossRef] [PubMed]
- Vallet-Regí, M.; González-Calbet, J.M. Calcium phosphates as substitution of bone tissues. Prog. Solid State Chem. 2004, 32, 1–31. [Google Scholar] [CrossRef]
- Hench, L.L. Bioceramics. J. Am. Ceram. Soc. 1998, 81, 1705–1728. [Google Scholar] [CrossRef]
- Xiao, W.; Sonny Bal, B.; Rahaman, M.N. Preparation of resorbable carbonate-substituted hollow hydroxyapatite microspheres and their evaluation in osseous defects in vivo. Mater. Sci. Eng. C Mater. Biol. Appl. 2016, 60, 324–332. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Sadat-Shojai, M.; Khorasani, M.-T.; Dinpanah-Khoshdargi, E.; Jamshidi, A. Synthesis methods for nanosized hydroxyapatite with diverse structures. Acta Biomater. 2013, 9, 7591–7621. [Google Scholar] [CrossRef] [PubMed]
- Gomes, D.S.; Santos, A.M.C.; Neves, G.A.; Menezes, R.R.; Gomes, D.S.; Santos, A.M.C.; Neves, G.A.; Menezes, R.R. A brief review on hydroxyapatite production and use in biomedicine. Cerâmica 2019, 65, 282–302. [Google Scholar] [CrossRef] [Green Version]
- Cai, Y.; Liu, Y.; Yan, W.; Hu, Q.; Tao, J.; Zhang, M.; Shi, Z.; Tang, R. Role of hydroxyapatite nanoparticle size in bone cell proliferation. J. Mater. Chem. 2007, 17, 3780–3787. [Google Scholar] [CrossRef]
- Li, B.; Guo, B.; Fan, H.; Zhang, X. Preparation of nano-hydroxyapatite particles with different morphology and their response to highly malignant melanoma cells in vitro. Appl. Surf. Sci. 2008, 255, 357–360. [Google Scholar] [CrossRef]
- Xu, J.L.; Khor, K.A.; Sui, J.J.; Zhang, J.H.; Chen, W.N. Protein expression profiles in osteoblasts in response to differentially shaped hydroxyapatite nanoparticles. Biomaterials 2009, 30, 5385–5391. [Google Scholar] [CrossRef]
- Wang, A.; Lu, Y.; Zhu, R.-F.; Li, S.; Ma, X. Effect of process parameters on the performance of spray dried hydroxyapatite microspheres. Powder Technol. 2009, 191, 1–6. [Google Scholar] [CrossRef]
- Bai, Y.; Sha, J.; Kanno, T.; Miyamoto, K.; Hideshima, K.; Matsuzaki, Y. Comparison of the Bone Regenerative Capacity of Three-Dimensional Uncalcined and Unsintered Hydroxyapatite/Poly-d/l-Lactide and Beta-Tricalcium Phosphate Used as Bone Graft Substitutes. J. Investig. Surg. Off. J. Acad. Surg. Res. 2021, 34, 243–256. [Google Scholar] [CrossRef] [PubMed]
- LeGeros: Calcium Phosphate Biomaterials: Preparation,...—Google Scholar. Available online: https://scholar.google.com/scholar_lookup?title=Calcium%20phosphate%20biomaterials%3A%20preparation%2C%20properties%20and%20biodegradation&author=R.Z..%20LeGeros&author=J.P..%20LeGeros&author=G..%20Daculsi&author=R..%20Kijkowska&pages=1429&publication_year=1995 (accessed on 3 March 2021).
- Ducheyne, P.; Radin, S.; King, L. The effect of calcium phosphate ceramic composition and structure on in vitro behavior. I. Dissolution. J. Biomed. Mater. Res. 1993, 27, 25–34. [Google Scholar] [CrossRef] [PubMed]
- Ducheyne, P.; Qiu, Q. Bioactive ceramics: The effect of surface reactivity on bone formation and bone cell function. Biomaterials 1999, 20, 2287–2303. [Google Scholar] [CrossRef]
- Porter, A.E.; Hobbs, L.W.; Rosen, V.B.; Spector, M. The ultrastructure of the plasma-sprayed hydroxyapatite–bone interface predisposing to bone bonding. Biomaterials 2002, 23, 725–733. [Google Scholar] [CrossRef]
- Bertazzo, S.; Zambuzzi, W.F.; Campos, D.D.P.; Ogeda, T.L.; Ferreira, C.V.; Bertran, C.A. Hydroxyapatite surface solubility and effect on cell adhesion. Colloids Surf. B Biointerfaces 2010, 78, 177–184. [Google Scholar] [CrossRef] [PubMed]
- Grandfield, K.; Palmquist, A.; Engqvist, H.; Thomsen, P. Resolving the CaP-bone interface. Biomatter 2012, 2, 15–23. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Wang, K.; Zhou, C.; Hong, Y.; Zhang, X. A review of protein adsorption on bioceramics. Interface Focus 2012, 2, 259–277. [Google Scholar] [CrossRef]
- Koike, T.; Sha, J.; Bai, Y.; Matsuda, Y.; Hideshima, K.; Yamada, T.; Kanno, T. Efficacy of Bacterial Cellulose as a Carrier of BMP-2 for Bone Regeneration in a Rabbit Frontal Sinus Model. Materials 2019, 12, 2489. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Webster, T.J.; Siegel, R.W.; Bizios, R. Osteoblast adhesion on nanophase ceramics. Biomaterials 1999, 20, 1221–1227. [Google Scholar] [CrossRef]
- Webster, T.J.; Schadler, L.S.; Siegel, R.W.; Bizios, R. Mechanisms of enhanced osteoblast adhesion on nanophase alumina involve vitronectin. Tissue Eng. 2001, 7, 291–301. [Google Scholar] [CrossRef]
- Webster, T.J.; Ahn, E.S. Nanostructured biomaterials for tissue engineering bone. Adv. Biochem. Eng. Biotechnol. 2007, 103, 275–308. [Google Scholar] [CrossRef]
- Liu, H.; Webster, T.J. Nanomedicine for implants: A review of studies and necessary experimental tools. Biomaterials 2007, 28, 354–369. [Google Scholar] [CrossRef]
- Duan, Y.-R.; Wang, C.; Chen, J.; Zhang, X. A Study of Bone-Like Apatite Formation on Calcium Phosphate Ceramics in Different Simulated Body Fluids (SBF). Key Eng. Mater. 2004, 254–256, 351–354. [Google Scholar] [CrossRef]
- Duan, Y.-R.; Zhang, Z.-R.; Wang, C.; Chen, J.; Zhang, X. Apatite Formation on HA/TCP Ceramics in Dynamic Simulated Body Fluid. Key Eng. Mater. 2004, 254–256, 131–134. [Google Scholar] [CrossRef]
- Li, X.; van Blitterswijk, C.A.; Feng, Q.; Cui, F.; Watari, F. The effect of calcium phosphate microstructure on bone-related cells in vitro. Biomaterials 2008, 29, 3306–3316. [Google Scholar] [CrossRef] [PubMed]
- Sha, J.; Kanno, T.; Miyamoto, K.; Bai, Y.; Hideshima, K.; Matsuzaki, Y. Application of a Bioactive/Bioresorbable Three-Dimensional Porous Uncalcined and Unsintered Hydroxyapatite/Poly-d/l-lactide Composite with Human Mesenchymal Stem Cells for Bone Regeneration in Maxillofacial Surgery: A Pilot Animal Study. Materials 2019, 12, 705. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Shimazaki, K.; Mooney, V. Comparative study of porous hydroxyapatite and tricalcium phosphate as bone substitute. J. Orthop. Res. Off. Public Orthop. Res. Soc. 1985, 3, 301–310. [Google Scholar] [CrossRef]
- van Blitterswijk, C.A.; Grote, J.J.; Kuÿpers, W.; Blok-van Hoek, C.J.; Daems, W.T. Bioreactions at the tissue/hydroxyapatite interface. Biomaterials 1985, 6, 243–251. [Google Scholar] [CrossRef]
- van Blitterswijk, C.A.; Grote, J.J.; Kuijpers, W.; Daems, W.T.; de Groot, K. Macropore tissue ingrowth: A quantitative and qualitative study on hydroxyapatite ceramic. Biomaterials 1986, 7, 137–143. [Google Scholar] [CrossRef]
- Winter, M.; Griss, P.; de Groot, K.; Tagai, H.; Heimke, G.; von Dijk, H.J.; Sawai, K. Comparative histocompatibility testing of seven calcium phosphate ceramics. Biomaterials 1981, 2, 159–160. [Google Scholar] [CrossRef]
- Toda, E.; Bai, Y.; Sha, J.; Dong, Q.N.; Ngo, H.X.; Suyama, T.; Miyamoto, K.; Matsuzaki, Y.; Kanno, T. Feasibility of Application of the Newly Developed Nano-Biomaterial, β-TCP/PDLLA, in Maxillofacial Reconstructive Surgery: A Pilot Rat Study. Nanomaterials 2021, 11, 303. [Google Scholar] [CrossRef]
- Inoue, O.; Ibaraki, K.; Shimabukuro, H.; Shingaki, Y. Packing with high-porosity hydroxyapatite cubes alone for the treatment of simple bone cyst. Clin. Orthop. 1993, 293, 287–292. [Google Scholar] [CrossRef]
- Schepers, E.; de Clercq, M.; Ducheyne, P.; Kempeneers, R. Bioactive glass particulate material as a filler for bone lesions. J. Oral Rehabil. 1991, 18, 439–452. [Google Scholar] [CrossRef] [PubMed]
- Goto, T.; Kojima, T.; Iijima, T.; Yokokura, S.; Kawano, H.; Yamamoto, A.; Matsuda, K. Resorption of synthetic porous hydroxyapatite and replacement by newly formed bone. J. Orthop. Sci. 2001, 6, 444–447. [Google Scholar] [CrossRef] [PubMed]
- Silverstein, S.C.; Steinman, R.M.; Cohn, Z.A. Endocytosis. Annu. Rev. Biochem. 1977, 46, 669–722. [Google Scholar] [CrossRef]
- Oonishi, H.; Hench, L.L.; Wilson, J.; Sugihara, F.; Tsuji, E.; Kushitani, S.; Iwaki, H. Comparative bone growth behavior in granules of bioceramic materials of various sizes. J. Biomed. Mater. Res. 1999, 44, 31–43. [Google Scholar] [CrossRef]
- Masutani, K.; Kimura, Y. Chapter 1 PLA Synthesis. From the Monomer to the Polymer; RSC Publishing: London, UK, 2014; pp. 1–36. [Google Scholar] [CrossRef]
- Esen, A.; Ataoğlu, H.; Gemi, L. Comparison of stability of titanium and absorbable plate and screw fixation for mandibular angle fractures. Oral Surg. Oral Med. Oral Pathol. Oral Radiol. Endod. 2008, 106, 806–811. [Google Scholar] [CrossRef]
- Bayram, B.; Araz, K.; Uckan, S.; Balcik, C. Comparison of fixation stability of resorbable versus titanium plate and screws in mandibular angle fractures. J. Oral Maxillofac. Surg. 2009, 67, 1644–1648. [Google Scholar] [CrossRef]
- Sukegawa, S.; Kanno, T.; Nagano, D.; Shibata, A.; Sukegawa-Takahashi, Y.; Furuki, Y. The Clinical Feasibility of Newly Developed Thin Flat-Type Bioresorbable Osteosynthesis Devices for the Internal Fixation of Zygomatic Fractures: Is There a Difference in Healing Between Bioresorbable Materials and Titanium Osteosynthesis? J. Craniofac. Surg. 2016, 27, 2124–2129. [Google Scholar] [CrossRef] [Green Version]
- Bostman, O. Current concepts review; Absorbable implants for the fixation of fractures. J Bone Jt. Surg. A 1991, 73, 148–153. [Google Scholar] [CrossRef]
- Böstman, O.M. Osteoarthritis of the ankle after foreign-body reaction to absorbable pins and screws: A three- to nine-year follow-up study. J. Bone Joint Surg. Br. 1998, 80, 333–338. [Google Scholar] [CrossRef]
- Tegnander, A.; Engebretsen, L.; Bergh, K.; Eide, E.; Holen, K.; Iversen, O.-J. Activation of the complement system and adverse effects of biodegradable pins of poly-lactic acid (Biofix®) in osteochondritis dissecans. Acta Orthop. 1994, 65, 472–475. [Google Scholar] [CrossRef] [Green Version]
- Bergsma, E.J.; Rozema, F.R.; Bos, R.R.M.; Bruijn, W.C.D. Foreign body reactions to resorbable poly(l-lactide) bone plates and screws used for the fixation of unstable zygomatic fractures. J. Oral Maxillofac. Surg. 1993, 51, 666–670. [Google Scholar] [CrossRef]
- Matsusue, Y.; Nakamura, T.; Iida, H.; Shimizu, K. A long-term clinical study on drawn poly-L-lactide implants in orthopaedic surgery. J. Long. Term Eff. Med. Implant 1997, 7, 119–137. [Google Scholar]
- Matsusue, Y.; Nakamura, T.; Suzuki, S.; Iwasaki, R. Biodegradable pin fixation of osteochondral fragments of the knee. Clin. Orthop. 1996, 322, 166–173. [Google Scholar] [CrossRef]
- Ahl, T.; Dalén, N.; Lundberg, A.; Wykman, A. Biodegradable fixation of ankle fractures. A roentgen stereophotogrammetric study of 32 cases. Acta Orthop. Scand. 1994, 65, 166–170. [Google Scholar] [CrossRef] [Green Version]
- Donigian, A.M.; Plaga, B.R.; Caskey, P.M. Biodegradable fixation of physeal fractures in goat distal femur. J. Pediatr. Orthop. 1993, 13, 349–354. [Google Scholar] [CrossRef]
- Böstman, O.; Hirvensalo, E.; Vainionpää, S.; Mäkelä, A.; Vihtonen, K.; Törmälä, P.; Rokkanen, P. Ankle fractures treated using biodegradable internal fixation. Clin. Orthop. 1989, 238, 195–203. [Google Scholar] [CrossRef]
- Yasunaga, T.; Matsusue, Y.; Furukawa, T.; Shikinami, Y.; Okuno, M.; Nakamura, T. Bonding behavior of ultrahigh strength unsintered hydroxyapatite particles/poly(L-lactide) composites to surface of tibial cortex in rabbits. J. Biomed. Mater. Res. 1999, 47, 412–419. [Google Scholar] [CrossRef]
- Ikumi, R.; Miyahara, T.; Akino, N.; Tachikawa, N.; Kasugai, S. Guided bone regeneration using a hydrophilic membrane made of unsintered hydroxyapatite and poly(L-lactic acid) in a rat bone-defect model. Dent. Mater. J. 2018, 37, 912–918. [Google Scholar] [CrossRef] [Green Version]
- Ikawa, H.; Moroi, A.; Yoshizawa, K.; Saida, Y.; Hotta, A.; Tsutsui, T.; Fukaya, K.; Hiraide, R.; Takayama, A.; Tsunoda, T.; et al. Bone regeneration enhancement by ultra-violet (UV) treatment for uHA/PLLA absorbable mesh. J. Cranio-Maxillofacial Surg. 2017, 45, 634–641. [Google Scholar] [CrossRef]
- Moroi, A.; Okuno, M.; Kobayashi, G.; Gamo, H.; Serizawa, I.; Yoshizawa, K.; Ikawa, H.; Ueki, K. Effect on surface character and mechanical property of unsintered hydroxyapatite/poly-l-lactic acid (uHA/PLLA) material by UV treatment. J. Biomed. Mater. Res. B Appl. Biomater. 2016, 106, 191–200. [Google Scholar] [CrossRef] [PubMed]
- Furukawa, T.; Matsusue, Y.; Yasunaga, T.; Shikinami, Y.; Okuno, M.; Nakamura, T. Biodegradation behavior of ultra-high-strength hydroxyapatite/poly (l-lactide) composite rods for internal fixation of bone fractures. Biomaterials 2000, 21, 889–898. [Google Scholar] [CrossRef]
- Ishii, S.; Tamura, J.; Furukawa, T.; Nakamura, T.; Matsusue, Y.; Shikinami, Y.; Okuno, M. Long-term study of high-strength hydroxyapatite/poly(L-lactide) composite rods for the internal fixation of bone fractures: A 2-4-year follow-up study in rabbits. J. Biomed. Mater. Res. B Appl. Biomater. 2003, 66, 539–547. [Google Scholar] [CrossRef]
- Hasegawa, S.; Ishii, S.; Tamura, J.; Furukawa, T.; Neo, M.; Matsusue, Y.; Shikinami, Y.; Okuno, M.; Nakamura, T. A 5-7 year in vivo study of high-strength hydroxyapatite/poly(L-lactide) composite rods for the internal fixation of bone fractures. Biomaterials 2006, 27, 1327–1332. [Google Scholar] [CrossRef]
- Törmälä, P.; Vasenius, J.; Vainionpää, S.; Laiho, J.; Pohjonen, T.; Rokkanen, P. Ultra-high-strength absorbable self-reinforced polyglycolide (SR-PGA) composite rods for internal fixation of bone fractures: In vitro and in vivo study. J. Biomed. Mater. Res. 1991, 25, 1–22. [Google Scholar] [CrossRef]
- Majola, A.; Vainionpää, S.; Rokkanen, P.; Mikkola, H.-M.; Törmälä, P. Absorbable self-reinforced polylactide (SR-PLA) composite rods for fracture fixation: Strength and strength retention in the bone and subcutaneous tissue of rabbits. J. Mater. Sci. Mater. Med. 1992, 3, 43–47. [Google Scholar] [CrossRef]
- Matsusue, Y.; Yamamuro, T.; Oka, M.; Shikinami, Y.; Hyon, S.H.; Ikada, Y. In vitro and in vivo studies on bioabsorbable ultra-high-strength poly(L-lactide) rods. J. Biomed. Mater. Res. 1992, 26, 1553–1567. [Google Scholar] [CrossRef]
- Hiatt, J.L. Textbook of Head and Neck Anatomy, 4th ed.; Jones & Bartlett Learning: Philadelphia, PA, USA, 2009; ISBN 978-0-7817-8932-5. [Google Scholar]
- Breeland, G.; Aktar, A.; Patel, B.C. Anatomy, Head and Neck, Mandible. In StatPearls; StatPearls Publishing: Treasure Island, FL, USA, 2021. [Google Scholar]
- Park, H.; Kim, H.-S.; Lee, B.-I. Medial Wall Orbital Reconstruction using Unsintered Hydroxyapatite Particles/Poly L-Lactide Composite Implants. Arch. Craniofacial Surg. 2015, 16, 125–130. [Google Scholar] [CrossRef] [Green Version]
- Landes, C.; Ballon, A.; Ghanaati, S.; Tran, A.; Sader, R. Treatment of malar and midfacial fractures with osteoconductive forged unsintered hydroxyapatite and poly-L-lactide composite internal fixation devices. J. Oral Maxillofac. Surg. 2014, 72, 1328–1338. [Google Scholar] [CrossRef] [PubMed]
- Kim, S.Y.; Nam, S.M.; Park, E.S.; Kim, Y.B. Evaluation of one-point fixation for zygomaticomaxillary complex fractures using a three-dimensional photogrammetric analysis. J. Otolaryngol.-Head Neck Surg. 2019, 48, 36. [Google Scholar] [CrossRef] [PubMed]
- Sukegawa, S.; Kanno, T.; Katase, N.; Shibata, A.; Takahashi, Y.; Furuki, Y. Clinical Evaluation of an Unsintered Hydroxyapatite/Poly-L-Lactide Osteoconductive Composite Device for the Internal Fixation of Maxillofacial Fractures. J. Craniofac. Surg. 2016, 27, 1391–1397. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Ueki, K.; Miyazaki, M.; Okabe, K.; Mukozawa, A.; Marukawa, K.; Moroi, A.; Nakagawa, K.; Yamamoto, E. Assessment of bone healing after Le Fort I osteotomy with 3-dimensional computed tomography. J. Cranio-Maxillofacial Surg. 2011, 39, 237–243. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Ueki, K.; Hashiba, Y.; Marukawa, K.; Alam, S.; Nakagawa, K.; Yamamoto, E. Skeletal Stability After Mandibular Setback Surgery: Bicortical Fixation Using a 2.0-mm Locking Plate System Versus Monocortical Fixation Using a Nonlocking Plate System. J. Oral Maxillofac. Surg. 2008, 66, 900–904. [Google Scholar] [CrossRef] [Green Version]
- Ueki, K.; Moroi, A.; Yoshizawa, K. Stability of the chin after advancement genioplasty using absorbable plate and screws with template devices. J. Cranio-Maxillofacial Surg. 2019, 47, 1498–1503. [Google Scholar] [CrossRef]
- Kaneko, T.; Nakamura, S.; Hino, S.; Horie, N.; Shimoyama, T. Continuous intra-sinus bone regeneration after nongrafted sinus lift with a PLLA mesh plate device and dental implant placement in an atrophic posterior maxilla: A case report. Int. J. Implant Dent. 2016, 2, 16. [Google Scholar] [CrossRef] [Green Version]
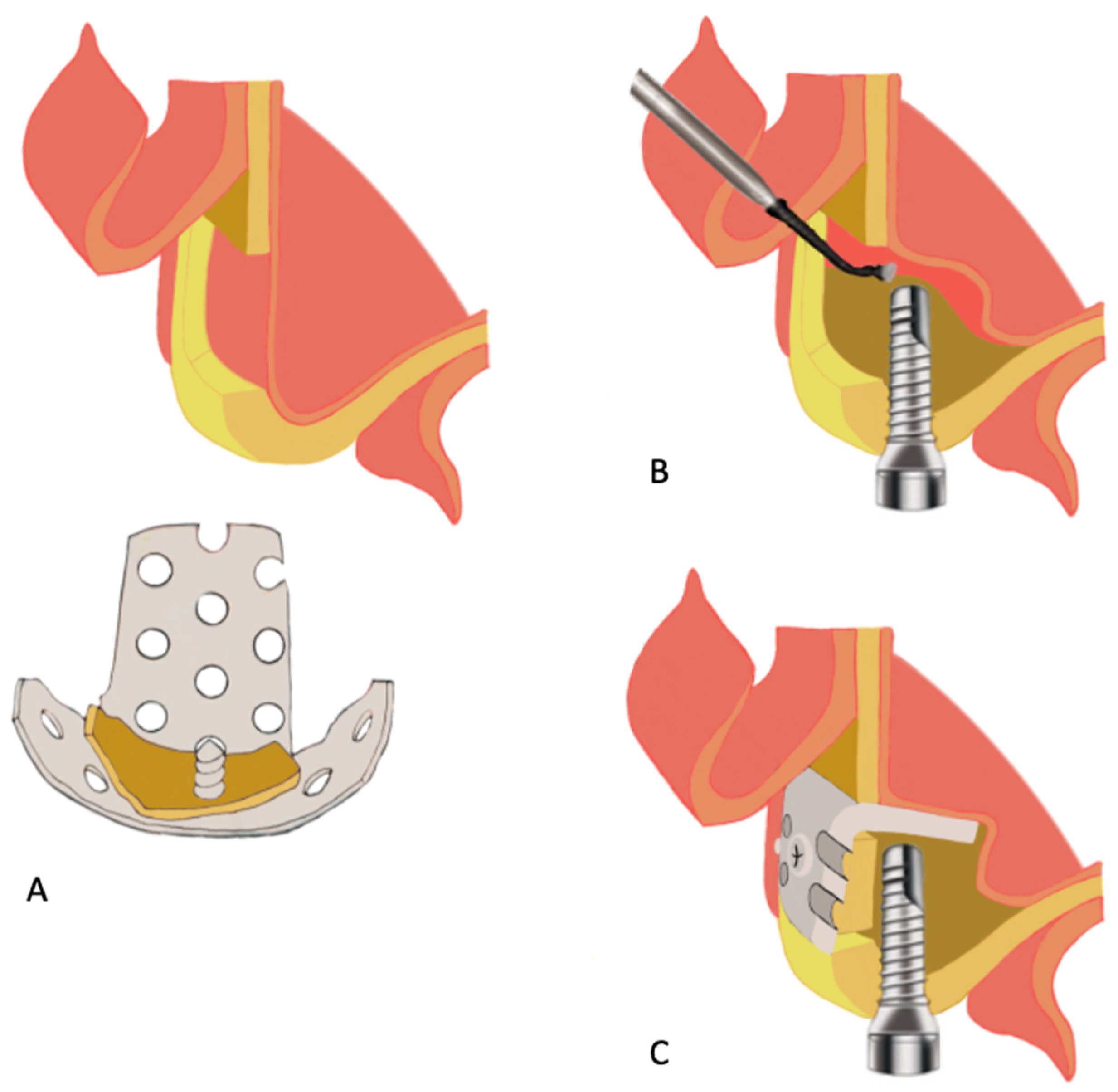
- Sukegawa, S.; Kawai, H.; Nakano, K.; Takabatake, K.; Kanno, T.; Nagatsuka, H.; Furuki, Y. Advantage of Alveolar Ridge Augmentation with Bioactive/Bioresorbable Screws Made of Composites of Unsintered Hydroxyapatite and Poly-L-lactide. Materials 2019, 12, 3681. [Google Scholar] [CrossRef] [Green Version]
- Dubois, L.; Steenen, S.A.; Gooris, P.J.J.; Bos, R.R.M.; Becking, A.G. Controversies in orbital reconstruction-III. Biomaterials for orbital reconstruction: A review with clinical recommendations. Int. J. Oral Maxillofac. Surg. 2016, 45, 41–50. [Google Scholar] [CrossRef]
- Ilankovan, V.; Jackson, I.T. Experience in the use of calvarial bone grafts in orbital reconstruction. Br. J. Oral Maxillofac. Surg. 1992, 30, 92–96. [Google Scholar] [CrossRef]
- Chowdhury, K.; Krause, G.E. Selection of materials for orbital floor reconstruction. Arch. Otolaryngol. Head Neck Surg. 1998, 124, 1398–1401. [Google Scholar] [CrossRef]
- Peng, M.Y.; Merbs, S.L.; Grant, M.P.; Mahoney, N.R. Orbital fracture repair outcomes with preformed titanium mesh implants and comparison to porous polyethylene coated titanium sheets. J. Cranio-Maxillofacial Surg. 2017, 45, 271–274. [Google Scholar] [CrossRef] [PubMed]
- Meyer, D.R. Alloplastic materials for orbital surgery. Curr. Opin. Ophthalmol. 1995, 6, 43–52. [Google Scholar] [CrossRef] [PubMed]
- Ozturk, S.; Sengezer, M.; Isik, S.; Turegun, M.; Deveci, M.; Cil, Y. Long-term outcomes of ultra-thin porous polyethylene implants used for reconstruction of orbital floor defects. J. Craniofac. Surg. 2005, 16, 973–977. [Google Scholar] [CrossRef]
- Tercan, M. Thin Silastic sheet for orbital floor repair. Plast. Reconstr. Surg. 1995, 96, 1238–1239. [Google Scholar]
- Xu, J.; Teng, L.; Jin, X.; Ji, Y.; Lu, J.; Zhang, B. Porous polyethylene implants in orbital blow-out fractures and enophthalmos reconstruction. J. Craniofac. Surg. 2009, 20, 918–920. [Google Scholar] [CrossRef] [PubMed]
- Lemke, B.N.; Kikkawa, D.O. Repair of orbital floor fractures with hydroxyapatite block scaffolding. Ophthal. Plast. Reconstr. Surg. 1999, 15, 161–165. [Google Scholar] [CrossRef]
- Teo, L.; Teoh, S.H.; Liu, Y.; Lim, L.; Tan, B.; Schantz, J.-T.; Seah, L.L. A Novel Bioresorbable Implant for Repair of Orbital Floor Fractures. Orbit Amst. Neth. 2015, 34, 192–200. [Google Scholar] [CrossRef]
- Gierloff, M.; Seeck, N.G.K.; Springer, I.; Becker, S.; Kandzia, C.; Wiltfang, J. Orbital floor reconstruction with resorbable polydioxanone implants. J. Craniofac. Surg. 2012, 23, 161–164. [Google Scholar] [CrossRef]
- Burres, S.A.; Cohn, A.M.; Mathog, R.H. Repair of orbital blowout fractures with marlex mesh and gelfilm. Laryngoscope 1981, 91, 1881–1886. [Google Scholar] [CrossRef] [PubMed]
- Young, S.M.; Sundar, G.; Lim, T.-C.; Lang, S.S.; Thomas, G.; Amrith, S. Use of bioresorbable implants for orbital fracture reconstruction. Br. J. Ophthalmol. 2017, 101, 1080–1085. [Google Scholar] [CrossRef]
- Tsumiyama, S.; Umeda, G.; Ninomiya, K.; Miyawaki, T. Use of Unsintered Hydroxyapatite and Poly-L-lactic Acid Composite Sheets for Management of Orbital Wall Fracture. J. Craniofac. Surg. 2019, 30, 2001–2003. [Google Scholar] [CrossRef] [PubMed]
- Kohyama, K.; Morishima, Y.; Arisawa, K.; Arisawa, Y.; Kato, H. Immediate and long-term results of unsintered hydroxyapatite and poly L-lactide composite sheets for orbital wall fracture reconstruction. J. Plast. Reconstr. Aesthet. Surg. 2018, 71, 1069–1075. [Google Scholar] [CrossRef] [PubMed]
- Watanabe, A.; Yamanaka, Y.; Rajak, S.N.; Nakayama, T.; Ueda, K.; Sotozono, C. Assessment of a Consecutive Series of Orbital Floor Fracture Repairs With the Hess Area Ratio and the Use of Unsintered Hydroxyapatite Particles/Poly l-Lactide Composite Sheets for Orbital Fracture Reconstruction. J. Oral Maxillofac. Surg. 2021, 79, 420–428. [Google Scholar] [CrossRef]
- Jang, H.U.; Kim, S.Y. Biodegradable implants for orbital wall fracture reconstruction. Arch. Craniofacial Surg. 2020, 21, 99–105. [Google Scholar] [CrossRef]
- Kanno, T.; Karino, M.; Yoshino, A.; Koike, T.; Ide, T.; Tatsumi, H.; Tsunematsu, K.; Yoshimatsu, H.; Sekine, J. Feasibility of Single Folded Unsintered Hydroxyapatite Particles/Poly-L-Lactide Composite Sheet in Combined Orbital Floor and Medial Wall Fracture Reconstruction. J. Hard Tissue Biol. 2017, 26, 237–244. [Google Scholar] [CrossRef]
- Kanno, T.; Tatsumi, H.; Karino, M.; Yoshino, A.; Koike, T.; Ide, T.; Sekine, J. Clinical Report: Applicability of an Unsintered Hydroxyapatite Particles/Poly-L-Lactide Composite Sheet with Tack Fixation for Orbital Fracture Reconstruction. J. Hard Tissue Biol. 2016, 3, 329–334. [Google Scholar] [CrossRef] [Green Version]
- Sukegawa, S.; Kanno, T.; Koyama, Y.; Matsumoto, K.; Sukegawa-Takahashi, Y.; Masui, M.; Tanaka, S.; Furuki, Y. Precision of Post-Traumatic Orbital Reconstruction Using Unsintered Hydroxyapatite Particles/Poly-L-Lactide Composite Bioactive/Resorbable Mesh Plate with and without Navigation: A Retrospective Study. J. Hard Tissue Biol. 2017, 26, 274–280. [Google Scholar] [CrossRef] [Green Version]
- Shintaro, S.; Takahiro, K.; Yuta, K.; Akane, S.; Ken-ichi, M.; Yuka, S.; Kyosuke, S.; Shigeto, T.; Yoshihiko, F. Intraoperative Navigation-assisted Surgical Orbital Floor Reconstruction in Orbital Fracture Treatment: A Case Report. Shimane J. Med. Sci. 2017, 33, 87–92. [Google Scholar]
- Dong, Q.N.; Karino, M.; Koike, T.; Ide, T.; Okuma, S.; Kaneko, I.; Osako, R.; Kanno, T. Navigation-Assisted Isolated Medial Orbital Wall Fracture Reconstruction Using an U-HA/PLLA Sheet via a Transcaruncular Approach. J. Investig. Surg. 2020, 33, 644–652. [Google Scholar] [CrossRef] [PubMed]
- Dong, Q.N.; Ide, T.; Karino, M.; Okuma, S.; Koike, T.; Kanno, T. Retrobulbar Orbital Emphysema Associated with Medial Orbital Wall Fracture. J. Craniofac. Surg. 2019, 30, 1549–1551. [Google Scholar] [CrossRef]
- Hwang, K. In Vivo Degradation of Forged-Unsintered Hydroxyapatite and Poly-L-lactide Mesh Used for Orbital Reconstruction. J. Craniofac. Surg. 2019, 30, 1208–1210. [Google Scholar] [CrossRef] [PubMed]
- Hayashi, M.; Muramatsu, H.; Sato, M.; Tomizuka, Y.; Inoue, M.; Yoshimoto, S. Surgical treatment of facial fracture by using unsintered hydroxyapatite particles/poly l-lactide composite device (OSTEOTRANS MX(®)): A clinical study on 17 cases. J. Cranio-Maxillofacial Surg. 2013, 41, 783–788. [Google Scholar] [CrossRef] [PubMed]
- Eppley, B.L.; Sadove, A.M. Effects of resorbable fixation on craniofacial skeletal growth: Modifications in plate size. J. Craniofac. Surg. 1994, 5, 110–114; discussion 115. [Google Scholar] [CrossRef]
- Eppley, B.L.; Sparks, C.; Herman, E.; Edwards, M.; McCarty, M.; Sadove, A.M. Effects of skeletal fixation on craniofacial imaging. J. Craniofac. Surg. 1993, 4, 67–73. [Google Scholar] [CrossRef] [PubMed]
- Yu, J.C.; Bartlett, S.P.; Goldberg, D.S.; Gannon, F.; Hunter, J.; Habecker, P.; Whitaker, L.A. An experimental study of the effects of craniofacial growth on the long-term positional stability of microfixation. J. Craniofac. Surg. 1996, 7, 64–68. [Google Scholar] [CrossRef] [PubMed]
- Alpert, B.; Seligson, D. Removal of asymptomatic bone plates used for orthognathic surgery and facial fractures. J. Oral Maxillofac. Surg. 1996, 54, 618–621. [Google Scholar] [CrossRef]
- Kim, Y.M.; Lee, J.H. Clinical courses and degradation patterns of absorbable plates in facial bone fracture patients. Arch. Craniofacial Surg. 2019, 20, 297–303. [Google Scholar] [CrossRef] [PubMed]
- Lee, S.J.; Park, E.S.; Nam, S.M.; Choi, C.Y.; Shin, H.S.; Kim, Y.B. Surgical Treatment of Mandible Fracture Using Unsintered Hydroxyapatite/Poly L-Lactide Composite Fixation System. J. Craniofac. Surg. 2019, 30, 2573–2575. [Google Scholar] [CrossRef]
- Song, I.-S.; Choi, J.; Kim, S.R.; Lee, J.-H. Stability of bioresorbable plates following reduction of mandibular body fracture: Three-dimensional analysis. J. Cranio-Maxillofacial Surg. 2019, 47, 1752–1757. [Google Scholar] [CrossRef]
- Kellman, R.M.; Cienfuegos, R. Endoscopic approaches to subcondylar fractures of the mandible. Facial Plast. Surg. FPS 2009, 25, 23–28. [Google Scholar] [CrossRef]
- Son, J.-H.; Ha, J.; Cho, Y.-C.; Sung, I.-Y. Are Biodegradable Plates Applicable in Endoscope-Assisted Open Reduction and Internal Fixation of Mandibular Subcondyle Fractures? J. Oral Maxillofac. Surg. 2017, 75, 1706–1715. [Google Scholar] [CrossRef]
- Kim, D.-Y.; Sung, I.-Y.; Cho, Y.-C.; Park, E.-J.; Son, J.-H. Bioabsorbable plates versus metal miniplate systems for use in endoscope-assisted open reduction and internal fixation of mandibular subcondylar fractures. J. Cranio-Maxillofacial Surg. 2018, 46, 413–417. [Google Scholar] [CrossRef]
- Sukegawa, S.; Kanno, T.; Yamamoto, N.; Nakano, K.; Takabatake, K.; Kawai, H.; Nagatsuka, H.; Furuki, Y. Biomechanical Loading Comparison between Titanium and Unsintered Hydroxyapatite/Poly-L-Lactide Plate System for Fixation of Mandibular Subcondylar Fractures. Materials 2019, 12, 1557. [Google Scholar] [CrossRef] [Green Version]
- Sukegawa, S.; Yamamoto, N.; Nakano, K.; Takabatake, K.; Kawai, H.; Kanno, T.; Nagatsuka, H.; Furuki, Y. Biomechanical Loading Comparison between Titanium and Bioactive Resorbable Screw Systems for Fixation of Intracapsular Condylar Head Fractures. Materials 2020, 13, 3153. [Google Scholar] [CrossRef] [PubMed]
- Jorgenson, D.S.; Mayer, M.H.; Ellenbogen, R.G.; Centeno, J.A.; Johnson, F.B.; Mullick, F.G.; Manson, P.N. Detection of titanium in human tissues after craniofacial surgery. Plast. Reconstr. Surg. 1997, 99, 976–979. [Google Scholar] [CrossRef] [PubMed]
- Haers, P.E.; Sailer, H.F. Biodegradable self-reinforced poly-L/DL-lactide plates and screws in bimaxillary orthognathic surgery: Short term skeletal stability and material related failures. J. Cranio-Maxillofacial Surg. 1998, 26, 363–372. [Google Scholar] [CrossRef]
- Cheung, L.K.; Chow, L.K.; Chiu, W.K. A randomized controlled trial of resorbable versus titanium fixation for orthognathic surgery. Oral Surg. Oral Med. Oral Pathol. Oral Radiol. Endod. 2004, 98, 386–397. [Google Scholar] [CrossRef]
- Landes, C.A.; Ballon, A. Skeletal stability in bimaxillary orthognathic surgery: P(L/DL)LA-resorbable versus titanium osteofixation. Plast. Reconstr. Surg. 2006, 118, 703–721; discussion 722. [Google Scholar] [CrossRef] [PubMed]
- Landes, C.A.; Ballon, A.; Sader, R. Segment stability in bimaxillary orthognathic surgery after resorbable Poly(L-lactide-co-glycolide) versus titanium osteosyntheses. J. Craniofac. Surg. 2007, 18, 1216–1229. [Google Scholar] [CrossRef]
- Stockmann, P.; Böhm, H.; Driemel, O.; Mühling, J.; Pistner, H. Resorbable versus titanium osteosynthesis devices in bilateral sagittal split ramus osteotomy of the mandible—The results of a two centre randomised clinical study with an eight-year follow-up. J. Cranio-Maxillofacial Surg. 2010, 38, 522–528. [Google Scholar] [CrossRef]
- Matthews, N.S.; Khambay, B.S.; Ayoub, A.F.; Koppel, D.; Wood, G. Preliminary assessment of skeletal stability after sagittal split mandibular advancement using a bioresorbable fixation system. Br. J. Oral Maxillofac. Surg. 2003, 41, 179–184. [Google Scholar] [CrossRef]
- Ueki, K.; Okabe, K.; Moroi, A.; Marukawa, K.; Sotobori, M.; Ishihara, Y.; Nakagawa, K. Maxillary stability after Le Fort I osteotomy using three different plate systems. Int. J. Oral Maxillofac. Surg. 2012, 41, 942–948. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Okabe, K.; Ueki, K.; Marukawa, K.; Mukozawa, A.; Miyazaki, M.; Nakagawa, K. An experimental study of use of absorbable plate in combination with self-setting α-tricalcium phosphate for orthognathic surgery. Oral Surg. Oral Med. Oral Pathol. Oral Radiol. Endod. 2010, 110, 560–569. [Google Scholar] [CrossRef] [Green Version]
- Ueki, K.; Okabe, K.; Marukawa, K.; Mukozawa, A.; Moroi, A.; Miyazaki, M.; Sotobori, M.; Ishihara, Y.; Yoshizawa, K.; Ooi, K.; et al. Maxillary stability after Le Fort I osteotomy with self-setting α-tricalcium phosphate and an absorbable plate. Int. J. Oral Maxillofac. Surg. 2013, 42, 597–603. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Ueki, K.; Yoshizawa, K.; Moroi, A.; Hotta, A.; Tsutsui, T.; Fukaya, K.; Hiraide, R.; Takayama, A.; Tsunoda, T.; Saito, Y.; et al. Evaluation of maxillary sinus after Le Fort I osteotomy using various fixation materials. J. Cranio-Maxillofacial Surg. 2017, 45, 552–557. [Google Scholar] [CrossRef] [PubMed]
- Meningaud, J.-P.; Poupon, J.; Bertrand, J.-C.; Chenevier, C.; Galliot-Guilley, M.; Guilbert, F. Dynamic study about metal release from titanium miniplates in maxillofacial surgery. Int. J. Oral Maxillofac. Surg. 2001, 30, 185–188. [Google Scholar] [CrossRef]
- Siniscalchi, E.N.; Catalfamo, L.; Allegra, A.; Musolino, C.; De Ponte, F.S. Titanium miniplates: A new risk factor for the development of the bisphosphonate-related osteonecrosis of the jaw. J. Craniofac. Surg. 2013, 24, e1–e2. [Google Scholar] [CrossRef]
- Ueki, K.; Okabe, K.; Miyazaki, M.; Mukozawa, A.; Moroi, A.; Marukawa, K.; Nakagawa, K.; Yamamoto, E. Skeletal stability after mandibular setback surgery: Comparisons among unsintered hydroxyapatite/poly-L-lactic acid plate, poly-L-lactic acid plate, and titanium plate. J. Oral Maxillofac. Surg. 2011, 69, 1464–1468. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Chung, I.-H.; Yoo, C.-K.; Lee, E.-K.; Ihm, J.-A.; Park, C.-J.; Lim, J.-S.; Hwang, K.-G. Postoperative Stability After Sagittal Split Ramus Osteotomies for a Mandibular Setback With Monocortical Plate Fixation or Bicortical Screw Fixation. J. Oral Maxillofac. Surg. 2008, 66, 446–452. [Google Scholar] [CrossRef]
- Van Sickels, J.E. A comparative study of bicortical screws and suspension wires versus bicortical screws in large mandibular advancements. J. Oral Maxillofac. Surg. 1991, 49, 1293–1298. [Google Scholar] [CrossRef]
- Brasileiro, B.F.; Grotta-Grempel, R.; Ambrosano, G.M.B.; Passeri, L.A. An in vitro evaluation of rigid internal fixation techniques for sagittal split ramus osteotomies: Setback surgery. J. Oral Maxillofac. Surg. 2012, 70, 941–951. [Google Scholar] [CrossRef] [PubMed]
- Schwartz, H.C.; Relle, R.J. Bicortical-monocortical fixation of the sagittal mandibular osteotomy. J. Oral Maxillofac. Surg. 1996, 54, 234–235. [Google Scholar] [CrossRef]
- Ueki, K.; Okabe, K.; Marukawa, K.; Mukozawa, A.; Moroi, A.; Miyazaki, M.; Sotobori, M.; Ishihara, Y.; Yoshizawa, K.; Ooi, K. Skeletal stability after mandibular setback surgery: Comparison between the hybrid technique for fixation and the conventional plate fixation using an absorbable plate and screws. J. Cranio-Maxillofacial Surg. 2014, 42, 351–355. [Google Scholar] [CrossRef] [PubMed]
- Ueki, K.; Moroi, A.; Yoshizawa, K.; Hotta, A.; Tsutsui, T.; Fukaya, K.; Hiraide, R.; Takayama, A.; Tsunoda, T.; Saito, Y. Comparison of skeletal stability after sagittal split ramus osteotomy among mono-cortical plate fixation, bi-cortical plate fixation, and hybrid fixation using absorbable plates and screws. J. Cranio-Maxillofacial Surg. 2017, 45, 178–182. [Google Scholar] [CrossRef]
- Ueki, K.; Moroi, A.; Ishihara, Y.; Sotobori, M.; Iguchi, R.; Kosaka, A.; Ikawa, H.; Yoshizawa, K.; Marukawa, K. Comparison of lower lip hypoesthesia between hybrid fixation and conventional fixation following sagittal split ramus osteotomy. J. Cranio-Maxillofacial Surg. 2014, 42, 1808–1812. [Google Scholar] [CrossRef] [PubMed]
- Ueki, K.; Moroi, A.; Iguchi, R.; Kosaka, A.; Ikawa, H.; Yoshizawa, K. Changes in the computed tomography (pixel) value of mandibular ramus bone and fixation screws after sagittal split ramus osteotomy. Int. J. Oral Maxillofac. Surg. 2015, 44, 1337–1345. [Google Scholar] [CrossRef]
- Yamashita, Y.; Mizuashi, K.; Shigematsu, M.; Goto, M. Masticatory function and neurosensory disturbance after mandibular correction by bilateral sagittal split ramus osteotomy: A comparison between miniplate and bicortical screw rigid internal fixation. Int. J. Oral Maxillofac. Surg. 2007, 36, 118–122. [Google Scholar] [CrossRef]
- Sukegawa, S.; Kanno, T.; Manabe, Y.; Matsumoto, K.; Sukegawa-Takahashi, Y.; Masui, M.; Furuki, Y. Biomechanical Loading Evaluation of Unsintered Hydroxyapatite/poly-l-lactide Plate System in Bilateral Sagittal Split Ramus Osteotomy. Materials 2017, 10, 764. [Google Scholar] [CrossRef] [Green Version]
- Park, Y.-W.; Kang, H.-S.; Lee, J.-H. Comparative study on long-term stability in mandibular sagittal split ramus osteotomy: Hydroxyapatite/poly-l-lactide mesh versus titanium miniplate. Maxillofac. Plast. Reconstr. Surg. 2019, 41, 8. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Takayama, A.; Moroi, A.; Saito, Y.; Yoshizawa, K.; Nishida, T.; Ueki, K. Evaluation of Space-Maintaining Sinus Membrane Using the Absorbable Screws in Sinus Lifting Bone Augmentation. Implant Dent. 2019, 28, 28–38. [Google Scholar] [CrossRef] [PubMed]
- Tatsuta, S.; Hayashi, M.; Tokunaka, R.; Muramatsu, H.; Kadomatsu, K. Analysis of the Postoperative Absorption Process of Unsintered Hydroxyapatite Particles/Poly L-Lactide Composite Device (OSTEOTRANS MX®) for Facial Bone Fractures in 13 Cases. Clin. Surg. 2018, 6, 10–11. [Google Scholar]
| Maxillofacial Trauma | Orthognathics Surgery | Other Reconstructive Applications |
|---|---|---|
|
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Ngo, H.X.; Bai, Y.; Sha, J.; Ishizuka, S.; Toda, E.; Osako, R.; Kato, A.; Morioka, R.; Ramanathan, M.; Tatsumi, H.; et al. A Narrative Review of u-HA/PLLA, a Bioactive Resorbable Reconstruction Material: Applications in Oral and Maxillofacial Surgery. Materials 2022, 15, 150. https://doi.org/10.3390/ma15010150
Ngo HX, Bai Y, Sha J, Ishizuka S, Toda E, Osako R, Kato A, Morioka R, Ramanathan M, Tatsumi H, et al. A Narrative Review of u-HA/PLLA, a Bioactive Resorbable Reconstruction Material: Applications in Oral and Maxillofacial Surgery. Materials. 2022; 15(1):150. https://doi.org/10.3390/ma15010150
Chicago/Turabian StyleNgo, Huy Xuan, Yunpeng Bai, Jingjing Sha, Shinji Ishizuka, Erina Toda, Rie Osako, Akira Kato, Reon Morioka, Mrunalini Ramanathan, Hiroto Tatsumi, and et al. 2022. "A Narrative Review of u-HA/PLLA, a Bioactive Resorbable Reconstruction Material: Applications in Oral and Maxillofacial Surgery" Materials 15, no. 1: 150. https://doi.org/10.3390/ma15010150
APA StyleNgo, H. X., Bai, Y., Sha, J., Ishizuka, S., Toda, E., Osako, R., Kato, A., Morioka, R., Ramanathan, M., Tatsumi, H., Okui, T., & Kanno, T. (2022). A Narrative Review of u-HA/PLLA, a Bioactive Resorbable Reconstruction Material: Applications in Oral and Maxillofacial Surgery. Materials, 15(1), 150. https://doi.org/10.3390/ma15010150








