Mechanical Behavior of Different Restorative Materials and Onlay Preparation Designs in Endodontically Treated Molars
Abstract
1. Introduction
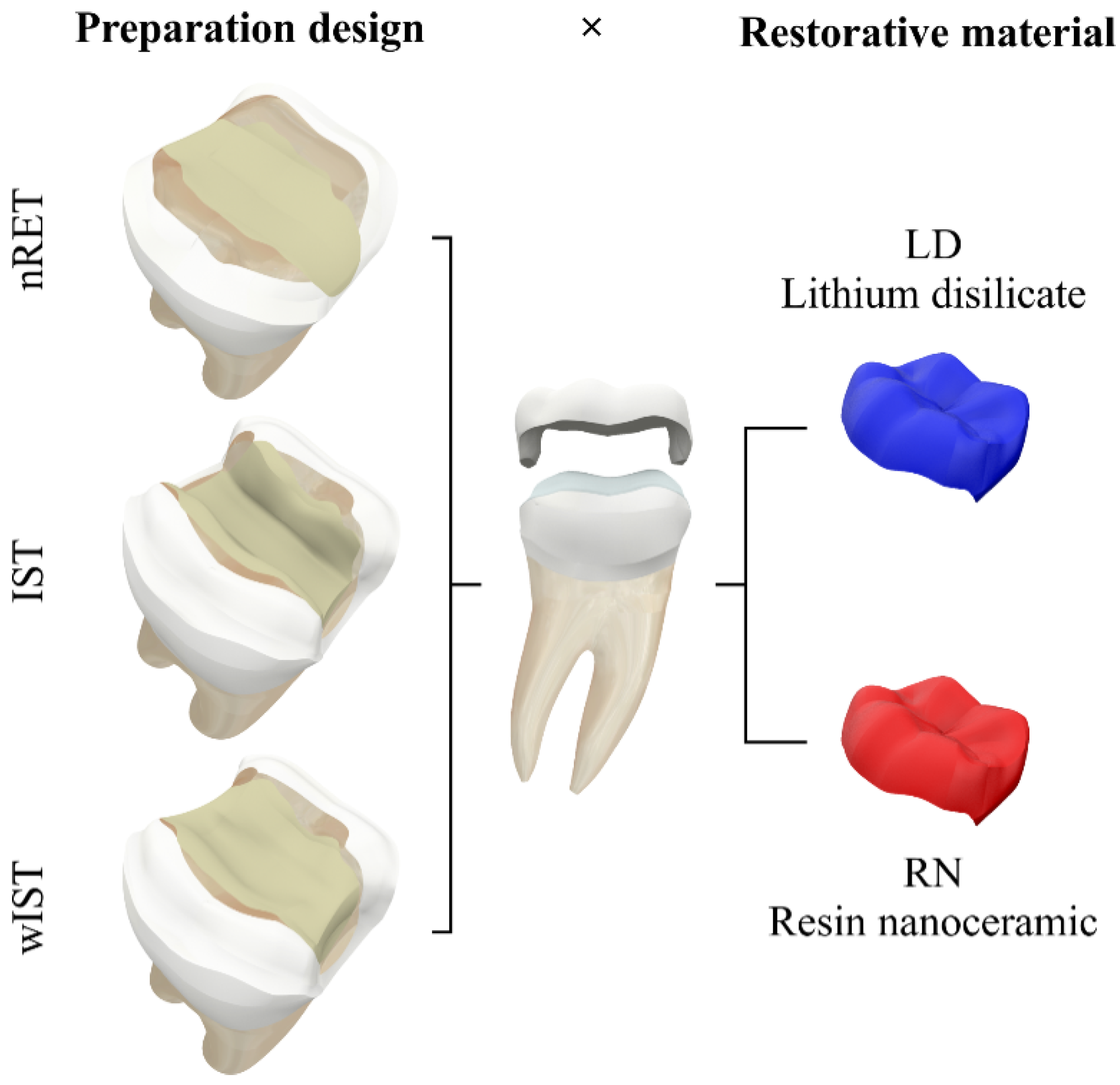
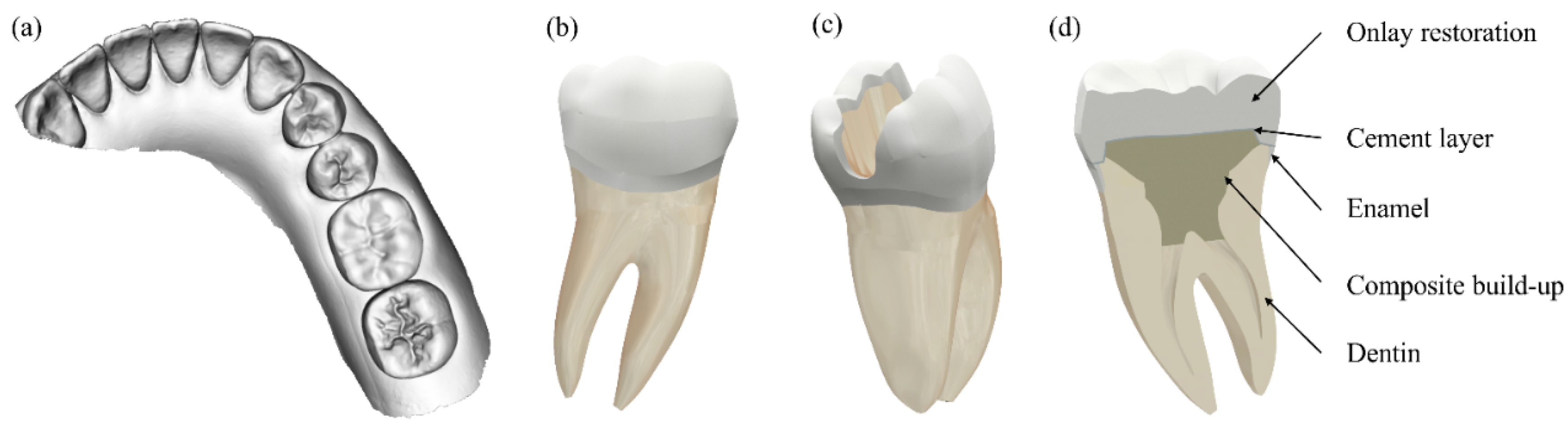
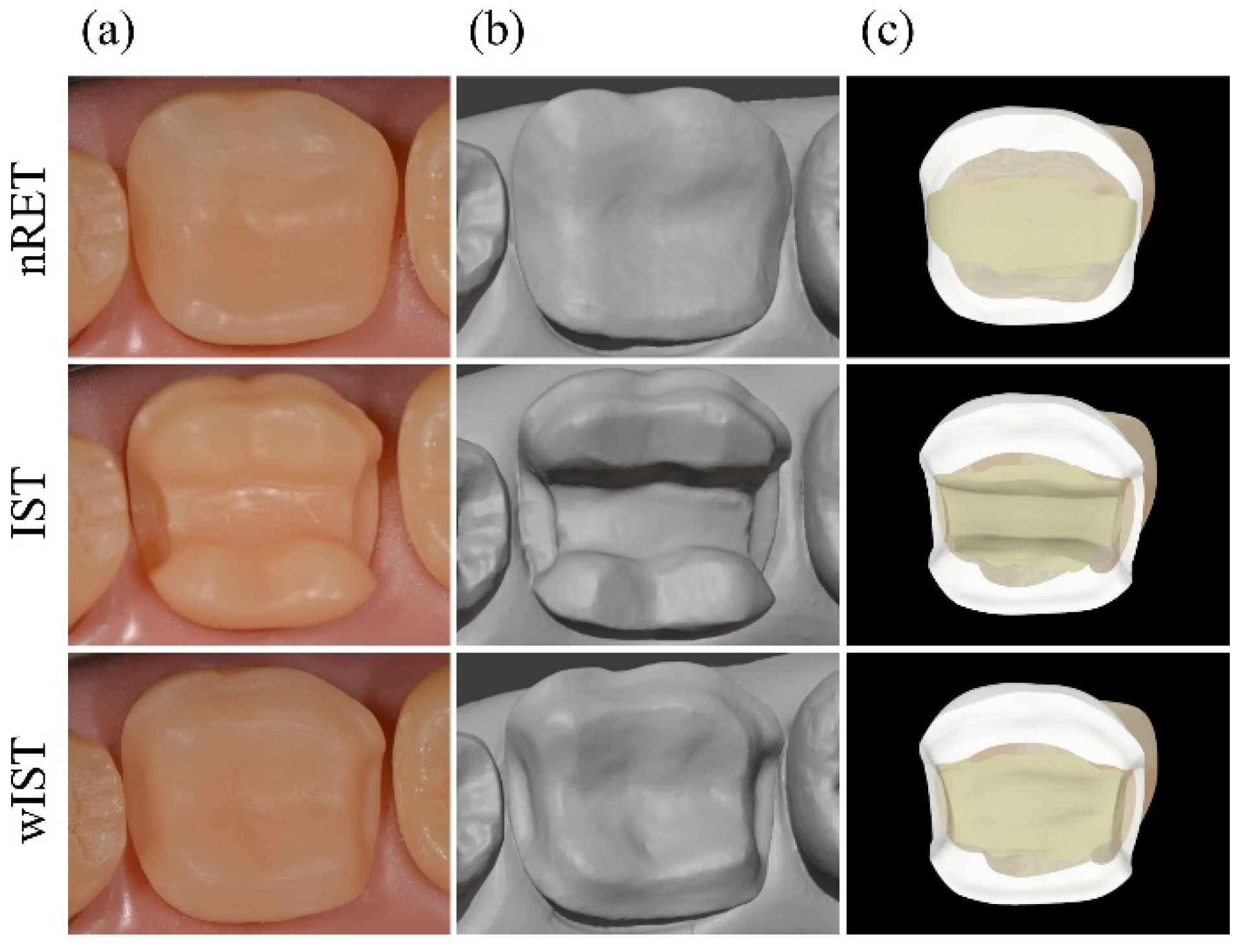
2. Materials and Methods
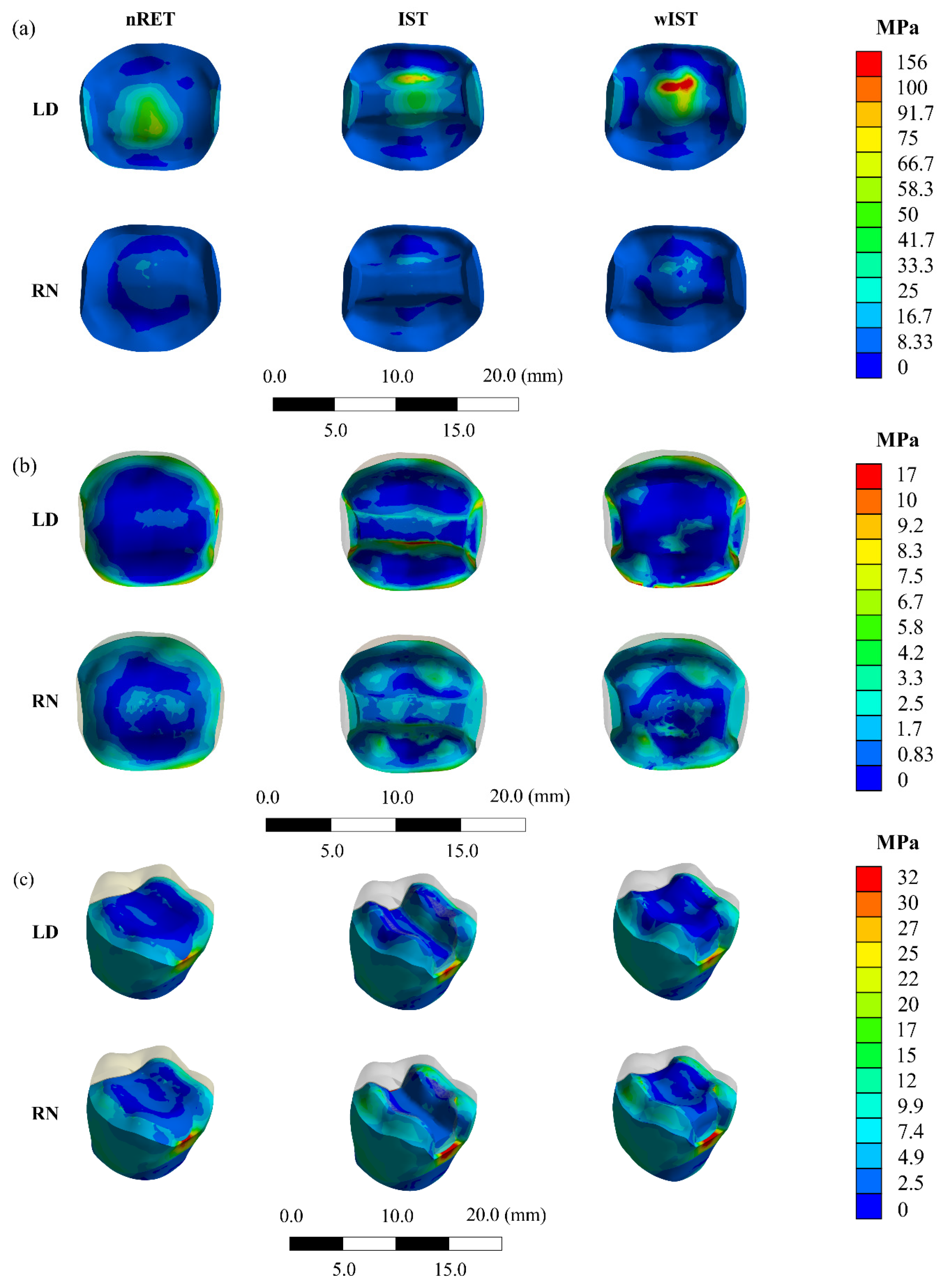
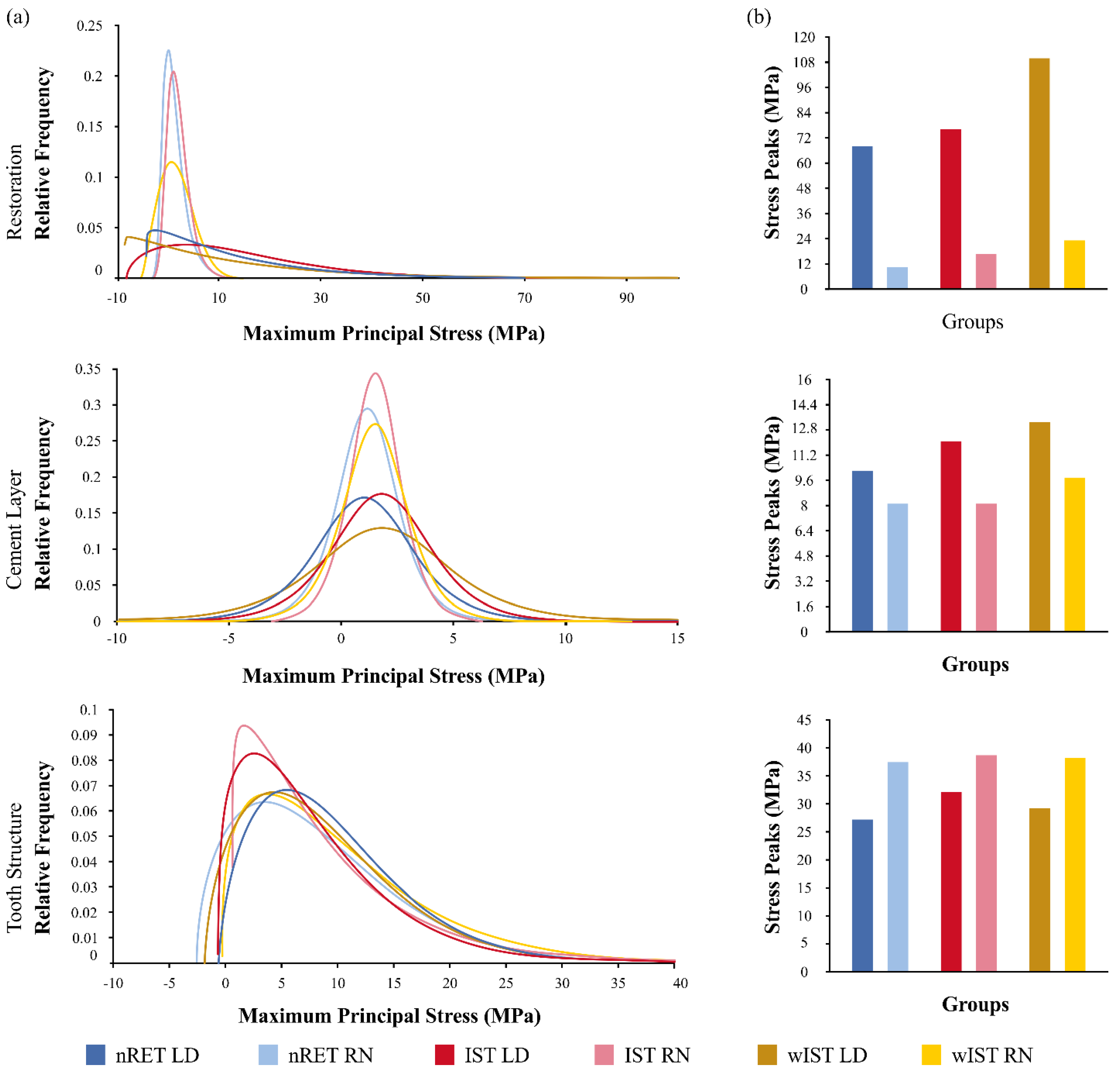
3. Results
4. Discussion
5. Conclusions
- The finite element analysis carried out on non-retentive onlay dental preparation showed the best mechanical behavior compared to other preparation designs;
- The finite element analysis also showed that resin-based materials presented a better mechanical behavior than lithium-disilicate ceramic;
- Lithium-disilicate ceramic materials could represent an interesting alternative of restorative material in specific clinical situations, such as extremely fragile teeth or in the presence of cracks.
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- The Academy of Prosthodontics. The glossary of prosthodontic terms. J. Prosthet. Dent. 2017, 117, e1–e105. [Google Scholar] [CrossRef]
- Bandlish, L.K.; Mariatos, G. Long-term survivals of “direct-wax” cast gold onlays: A retrospective study in a general dental practice. Br. Dent. J. 2009, 207, 111–115. [Google Scholar] [CrossRef]
- Studer, S.P.; Wettstein, F.; Lehner, C.; Zullo, T.G.; Schärer, P. Long-term survival estimates of cast gold inlays and onlays with their analysis of failures. J. Oral Rehabil. 2000, 27, 461–472. [Google Scholar] [CrossRef] [PubMed]
- Buonocore, M.G. A simple method of increasing the adhesion of acrylic filling materials to enamel surfaces. J. Dent. Res. 1955, 34, 849–853. [Google Scholar] [CrossRef] [PubMed]
- Fusayama, T.; Nakamura, M.; Kurosaki, N.; Iwaku, M. Non-pressure adhesion of a new adhesive restorative resin. J. Dent. Res. 1979, 58, 1364–1370. [Google Scholar] [CrossRef] [PubMed]
- Simonsen, R.J.; Calamia, J.R. Tensile bond strength of etched porcelain. J. Dent. Res. 1982, 61, 74–351. [Google Scholar] [CrossRef]
- Felden, A.; Schmalz, G.; Hiller, K.-A. Retrospective clinical study and survival analysis on partial ceramic crowns: Results up to 7 years. Clin. Oral Investig. 2000, 4, 199–205. [Google Scholar] [CrossRef] [PubMed]
- Magne, P.; Belser, U.C. Porcelain versus composite inlays/onlays: Effects of mechanical loads on stress distribution, adhesion, and crown flexure. Int. J. Periodontics Restorative Dent. 2003, 23, 543–555. [Google Scholar]
- Frankenberger, R.; Taschner, M.; Garcia-Godoy, F.; Petschelt, A.; Krämer, N. Leucite-reinforced glass ceramic inlays and onlays after 12 years. J. Adhes. Dent. 2008, 10, 393–398. [Google Scholar]
- Rocca, G.T.; Rizcalla, N.; Krejci, I.; Dietschi, D. Evidence-based concepts and procedures for bonded inlays and onlays. Part II. Guidelines for cavity preparation and restoration fabrication. Int. J. Esthet. Dent. 2015, 10, 392–413. [Google Scholar]
- Dietschi, D.; Spreafico, R. Evidence-based concepts and procedures for bonded inlays and onlays. Part I. Historical perspectives and clinical rationale for a biosubstitutive approach. Int. J. Esthet. Dent. 2015, 10, 210–227. [Google Scholar]
- Christensen, G.J. Considering tooth-colored inlays and onlays versus crowns. J. Am. Dent. Assoc. 2008, 139, 617–620. [Google Scholar] [CrossRef] [PubMed]
- Magne, P.; Schlichting, L.H.; Maia, H.P.; Baratieri, L.N. In vitro fatigue resistance of CAD/CAM composite resin and ceramic posterior occlusal veneers. J Prosthet Dent 2010, 104, 149–157. [Google Scholar] [CrossRef]
- Magne, P. Composite resins and bonded porcelain: The postamalgam era? J. Calif. Dent. Assoc. 2006, 34, 135–147. [Google Scholar] [PubMed]
- Edelhoff, D.; Ahlers, M.O. Occlusal onlays as a modern treatment concept for the reconstruction of severely worn occlusal surfaces. Quintessence Int 2018. [Google Scholar] [CrossRef]
- Gracis, S.; Thompson, V.P.; Ferencz, J.L.; Silva, N.R.F.A.; Bonfante, E.A. A new classification system for all-ceramic and ceramic-like restorative materials. Int. J. Prosthodont. 2015, 28, 227–235. [Google Scholar] [CrossRef]
- Mainjot, A.K.; Dupont, N.M.; Oudkerk, J.C.; Dewael, T.Y.; Sadoun, M.J. From Artisanal to CAD-CAM Blocks. J. Dent. Res. 2016, 95, 487–495. [Google Scholar] [CrossRef]
- Otto, T. Up to 27-years clinical long-term results of chairside Cerec 1 CAD/CAM inlays and onlays. Int. J. Comput. Dent. 2017, 20, 315–329. [Google Scholar]
- Pashley, D.H.; Tay, F.R.; Breschi, L.; Tjäderhane, L.; Carvalho, R.M.; Carrilho, M.; Tezvergil-Mutluay, A. State of the art etch-and-rinse adhesives. Dent. Mater. 2011, 27, 1–16. [Google Scholar] [CrossRef]
- Van Meerbeek, B.; Yoshihara, K.; Yoshida, Y.; Mine, A.; De Munck, J.; Van Landuyt, K.L. State of the art of self-etch adhesives. Dent. Mater. 2011, 27, 17–28. [Google Scholar] [CrossRef]
- Guess, P.C.; Schultheis, S.; Wolkewitz, M.; Zhang, Y.; Strub, J.R. Influence of preparation design and ceramic thicknesses on fracture resistance and failure modes of premolar partial coverage restorations. J. Prosthet. Dent. 2013, 110, 264–273. [Google Scholar] [CrossRef]
- Homaei, E.; Farhangdoost, K.; Tsoi, J.K.H.; Matinlinna, J.P.; Pow, E.H.N. Static and fatigue mechanical behavior of three dental CAD/CAM ceramics. J. Mech. Behav. Biomed. Mater. 2016, 59, 304–313. [Google Scholar] [CrossRef]
- Sasse, M.; Krummel, A.; Klosa, K.; Kern, M. Influence of restoration thickness and dental bonding surface on the fracture resistance of full-coverage occlusal veneers made from lithium disilicate ceramic. Dent. Mater. 2015, 31, 907–915. [Google Scholar] [CrossRef]
- Kaytan, B.; Onal, B.; Pamir, T.; Tezel, H. Clinical evaluation of indirect resin composite and ceramic onlays over a 24-month period. Gen. Dent. 2005, 53, 329–334. [Google Scholar]
- Abduo, J.; Sambrook, R.J. Longevity of ceramic onlays: A systematic review. J. Esthet. Restor. Dent. 2018, 30, 193–215. [Google Scholar] [CrossRef] [PubMed]
- Magne, P. Virtual prototyping of adhesively restored, endodontically treated molars. J. Prosthet. Dent. 2010, 103, 343–351. [Google Scholar] [CrossRef]
- Milicich, G. The compression dome concept: The restorative implications. Gen. Dent. 2017, 65, 55–60. [Google Scholar]
- Veneziani, M. Posterior indirect adhesive restorations: Updated indications and the Morphology Driven Preparation Technique. Int. J. Esthet. Dent. 2017, 12, 204–230. [Google Scholar]
- Politano, G.; Van Meerbeek, B.; Peumans, M. Nonretentive bonded ceramic partial crowns: Concept and simplified protocol for long-lasting dental restorations. J. Adhes. Dent. 2018, 20, 495–510. [Google Scholar] [CrossRef]
- Christensen, G.J. Tooth-colored inlays and onlays. J. Am. Dent. Assoc. 1988, 117, 12E–17E. [Google Scholar] [CrossRef] [PubMed]
- Broderson, S.P. Complete-crown and partial-coverage tooth preparation designs for bonded cast ceramic restorations. Quintessence Int. 1994, 25, 535–539. [Google Scholar]
- Arnetzl, G.V.; Arnetzl, G. Biomechanical examination of inlay geometries--is there a basic biomechanical principle? Int. J. Comput. Dent. 2009, 12, 119–130. [Google Scholar]
- Ahlers, M.O.; Mörig, G.; Blunck, U.; Hajtó, J.; Pröbster, L.; Frankenberger, R. Guidelines for the preparation of CAD/CAM ceramic inlays and partial crowns. Int. J. Comput. Dent. 2009, 12, 309–325. [Google Scholar] [PubMed]
- Banks, R.G. Conservative posterior ceramic restorations: A literature review. J. Prosthet. Dent. 1990, 63, 619–626. [Google Scholar] [CrossRef]
- Anusavice, K.J.; Kakar, K.; Ferree, N. Which mechanical and physical testing methods are relevant for predicting the clinical performance of ceramic-based dental prostheses? Clin. Oral Implants Res. 2007, 18, 218–231. [Google Scholar] [CrossRef] [PubMed]
- Ausiello, P.; Ciaramella, S.; Martorelli, M.; Lanzotti, A.; Gloria, A.; Watts, D.C. CAD-FE modeling and analysis of class II restorations incorporating resin-composite, glass ionomer and glass ceramic materials. Dent. Mater. 2017, 33, 1456–1465. [Google Scholar] [CrossRef]
- Gloria, A.; Maietta, S.; Martorelli, M.; Lanzotti, A.; Watts, D.C.; Ausiello, P. FE analysis of conceptual hybrid composite endodontic post designs in anterior teeth. Dent. Mater. 2018, 34, 1063–1071. [Google Scholar] [CrossRef] [PubMed]
- de Andrade, G.S.; Pinto, A.B.A.; Tribst, J.P.M.; Chun, E.P.; Borges, A.L.S.; de Siqueira Ferreira Anzaloni Saavedra, G. Does overlay preparation design affect polymerization shrinkage stress distribution? A 3D FEA study. Comput. Methods Biomech. Biomed. Engin. 2021, 1–10. [Google Scholar] [CrossRef]
- Falahchai, M.; Babaee Hemmati, Y.; Neshandar Asli, H.; Rezaei, E. Effect of tooth preparation design on fracture resistance of zirconia-reinforced lithium silicate overlays. J. Prosthodont. 2020, 29, 617–622. [Google Scholar] [CrossRef] [PubMed]
- Clausen, J.-O.; Abou Tara, M.; Kern, M. Dynamic fatigue and fracture resistance of non-retentive all-ceramic full-coverage molar restorations. Influence of ceramic material and preparation design. Dent. Mater. 2010, 26, 533–538. [Google Scholar] [CrossRef] [PubMed]
- Falahchai, M.; Hemmati, Y.B.; Asli, H.N.; Asli, M.N. Marginal adaptation of zirconia-reinforced lithium silicate overlays with different preparation designs. J. Esthet. Restor. Dent. 2020, 1–8. [Google Scholar] [CrossRef]
- De Velloso Vianna, A.L.S.; do Prado, C.J.; Bicalho, A.A.; da Silva Pereira, R.A.; das Neves, F.D.; Soares, C.J. Effect of cavity preparation design and ceramic type on the stress distribution, strain and fracture resistance of CAD/CAM onlays in molars. J. Appl. Oral Sci. 2018, 26, 1–10. [Google Scholar] [CrossRef]
- Dietschi, D.; Spreafico, R. Adhesive Metal-free restorations: Current concepts for the esthetic treatment of posterior teeth, 1st ed.; Quintessence Pub. Co: Chicago, IL, USA, 1997; ISBN 0-86715-328-8. [Google Scholar]
- Costa, A.; Xavier, T.; Noritomi, P.; Saavedra, G.; Borges, A. The Influence of Elastic Modulus of Inlay Materials on Stress Distribution and Fracture of Premolars. Oper. Dent. 2014, 39, E160–E170. [Google Scholar] [CrossRef] [PubMed]
- Vieira, G.F.; Agra, C.M.; Arakaki, Y.; Steagall Junior, W.; de Mello Ferreira, A.T. Atlas de anatomia de dentes permanentes-coroa dental, 2nd ed.; Santos: São Paulo, Brazil, 2013. [Google Scholar]
- Martorelli, M.; Ausiello, P. A novel approach for a complete 3D tooth reconstruction using only 3D crown data. Int. J. Interact. Des. Manuf. 2013, 7, 125–133. [Google Scholar] [CrossRef]
- Tribst, J.P.M.; de Oliveira Dal Piva, A.M.; Madruga, C.F.L.; Valera, M.C.; Borges, A.L.S.; Bresciani, E.; de Melo, R.M. Endocrown restorations: Influence of dental remnant and restorative material on stress distribution. Dent. Mater. 2018, 34, 1466–1473. [Google Scholar] [CrossRef] [PubMed]
- Magne, P.; Knezevic, A. Simulated fatigue resistance of composite resin versus porcelain CAD/CAM overlay restorations on endodontically treated molars. Quintessence Int. 2009, 40, 125–133. [Google Scholar]
- Schlichting, L.H.; Maia, H.P.; Baratieri, L.N.; Magne, P. Novel-design ultra-thin CAD/CAM composite resin and ceramic occlusal veneers for the treatment of severe dental erosion. J. Prosthet. Dent. 2011, 105, 217–226. [Google Scholar] [CrossRef]
- Magne, P.; Stanley, K.; Schlichting, L.H. Modeling of ultrathin occlusal veneers. Dent. Mater. 2012. [Google Scholar] [CrossRef]
- Zarone, F.; Sorrentino, R.; Apicella, D.; Valentino, B.; Ferrari, M.; Aversa, R.; Apicella, A. Evaluation of the biomechanical behavior of maxillary central incisors restored by means of endocrowns compared to a natural tooth: A 3D static linear finite elements analysis. Dent. Mater. 2006, 22, 1035–1044. [Google Scholar] [CrossRef]
- de Andrade, G.S.; Tribst, J.P.M.; de Oliveira Dal Piva, A.M.; Bottino, M.A.; Borges, A.L.S.; Valandro, L.F.; Özcan, M. A study on stress distribution to cement layer and root dentin for post and cores made of CAD/CAM materials with different elasticity modulus in the absence of ferrule. J. Clin. Exp. Dent. 2019, 11, e1–e8. [Google Scholar] [CrossRef]
- Pałka, K.; Bieniaś, J.; Dębski, H.; Niewczas, A. Finite element analysis of thermo-mechanical loaded teeth. Comput. Mater. Sci. 2012, 64, 289–294. [Google Scholar] [CrossRef]
- Ausiello, P.; Apicella, A.; Davidson, C.L.; Rengo, S. 3D-finite element analyses of cusp movements in a human upper premolar, restored with adhesive resin-based composites. J. Biomech. 2001, 34, 1269–1277. [Google Scholar] [CrossRef]
- Ausiello, P.; Ciaramella, S.; Garcia-Godoy, F.; Martorelli, M.; Sorrentino, R.; Gloria, A. Stress distribution of bulk-fill resin composite in class II restorations. Am. J. Dent. 2017, 30, 227–232. [Google Scholar]
- Völkel, T. Ivoclar Vivadent Truly Universal Multilink N-Scientific Documentation; Ivoclar Vivadent AG Research and Development: Schaan, Liechtenstein, 2010. [Google Scholar]
- Ausiello, P.; Ciaramella, S.; De Benedictis, A.; Lanzotti, A.; Tribst, J.P.M.; Watts, D.C. The use of different adhesive filling material and mass combinations to restore class II cavities under loading and shrinkage effects: A 3D-FEA. Comput. Methods Biomech. Biomed. Engin. 2020, 1–11. [Google Scholar] [CrossRef]
- Apicella, A.; Di Palma, L.; Aversa, R.; Ausiello, P. DSC kinetic characterization of dental composites using different light sources. J. Adv. Mater. 2002, 34, 22–25. [Google Scholar]
- Podhorsky, A.; Rehmann, P.; Wöstmann, B. Tooth preparation for full-coverage restorations—a literature review. Clin. Oral Investig. 2015, 19, 959–968. [Google Scholar] [CrossRef] [PubMed]
- Strasding, M.; Sebestyén-Hüvös, E.; Studer, S.; Lehner, C.; Jung, R.E.; Sailer, I. Long-term outcomes of all-ceramic inlays and onlays after a mean observation time of 11 years. Quintessence Int. 2020, 51, 566–576. [Google Scholar] [CrossRef] [PubMed]
- Morimoto, S.; Rebello de Sampaio, F.B.W.; Braga, M.M.; Sesma, N.; Özcan, M. Survival Rate of Resin and Ceramic Inlays, Onlays, and Overlays. J. Dent. Res. 2016, 95, 985–994. [Google Scholar] [CrossRef] [PubMed]
- Edelhoff, D.; Sorensen, J.A. Tooth structure removal associated with various preparation designs for anterior teeth. J. Prosthet. Dent. 2002, 87, 503–509. [Google Scholar] [CrossRef]
- Abad-Coronel, C.; Naranjo, B.; Valdiviezo, P. Adhesive systems used in indirect restorations cementation: Review of the literature. Dent. J. 2019, 7, 71. [Google Scholar] [CrossRef]
- Eakle, W.S.; Maxwell, E.H.; Braly, B.V. Fractures of posterior teeth in adults. J. Am. Dent. Assoc. 1986, 112, 215–218. [Google Scholar] [CrossRef]
- Frankenberger, R.; Reinelt, C.; Petschelt, A.; Krämer, N. Operator vs. material influence on clinical outcome of bonded ceramic inlays. Dent. Mater. 2009, 25, 960–968. [Google Scholar] [CrossRef]
- Magne, P.; Kim, T.H.; Cascione, D.; Donovan, T.E. Immediate dentin sealing improves bond strength of indirect restorations. J. Prosthet. Dent. 2005, 94, 511–519. [Google Scholar] [CrossRef]
- Van den Breemer, C.R.; Özcan, M.; Pols, M.R.; Postema, A.R.; Cune, M.S.; Gresnigt, M.M. Adhesion of resin cement to dentin: Effects of adhesive promoters, immediate dentin sealing strategies, and surface conditioning. Int. J. Esthet. Dent. 2019, 14, 52–63. [Google Scholar]
- Giannini, M. Ultimate tensile strength of tooth structures. Dent. Mater. 2004, 20, 322–329. [Google Scholar] [CrossRef]
- Scherrer, S.S.; Cesar, P.F.; Swain, M.V. Direct comparison of the bond strength results of the different test methods: A critical literature review. Dent. Mater. 2010, 26, e78–e93. [Google Scholar] [CrossRef]
- Costa, V.L.S.; Tribst, J.P.M.; Borges, A.L.S. Influence of the occlusal contacts in formation of Abfraction Lesions in the upper premolar. Brazilian Dent. Sci. 2017, 20, 115. [Google Scholar] [CrossRef][Green Version]
- Frankenberger, R.; Hartmann, V.E.; Krech, M.; Krämer, N.; Reich, S.; Braun, A.; Roggendorf, M. Adhesive luting of new CAD/CAM materials. Int. J. Comput. Dent. 2015, 18, 9–20. [Google Scholar] [PubMed]
- Politano, G.; Fabianelli, A.; Papacchini, F.; Cerutti, A. The use of bonded partial ceramic restorations to recover heavily compromised teeth. Int. J. Esthet. Dent. 2016, 11, 314–336. [Google Scholar] [PubMed]
- De Paula Rodrigues, M.; Soares, P.B.F.; Gomes, M.A.B.; Pereira, R.A.; Tantbirojn, D.; Versluis, A.; Soares, C.J. Direct resin composite restoration of endodontically-treated permanent molars in adolescents: Bite force and patient-specific finite element analysis. J. Appl. Oral Sci. 2020, 28, e20190544. [Google Scholar] [CrossRef]
- Magne, P.; Knezevic, A. Influence of overlay restorative materials and load cusps on the fatigue resistance of endodontically treated molars. Quintessence Int. 2009. [Google Scholar] [CrossRef]

| Preparation Design | Nodes | Elements | Volume (mm3) * |
|---|---|---|---|
| nRET | 196,316 | 160,426 | 159 |
| IST | 199,025 | 160,944 | 179 |
| wIST | 200,391 | 161,748 | 159 |
| Structure | Group | Distribution | Correlation Coefficient | Shape/* Local | Scale |
|---|---|---|---|---|---|
| Restoration | nRET LD | Weibull | 0.917 | 1.51 | 16.13 |
| nRET NR | GEV | 0.841 | −2.46 * | 1.63 | |
| IST LD | Weibull | 0.948 | 1.89 | 20.64 | |
| IST NR | GEV | 0.848 | 2.96 * | 1.49 | |
| wIST LD | Weibull | 0.918 | 1.48 | 19.75 | |
| wIST NR | Weibull | 0.962 | 2.80 | 7.40 | |
| Cement Layer | nRET LD | Weibull | 0.968 | 2.01 | 11.06 |
| nRET NR | Weibull | 0.913 | 2.16 | 11.05 | |
| IST LD | Weibull | 0.976 | 1.71 | 9.14 | |
| IST NR | Weibull | 0.973 | 1.49 | 8.36 | |
| wIST LD | Weibull | 0.949 | 2.26 | 11.45 | |
| wIST NR | Weibull | 0.967 | 1.54 | 10.79 | |
| Tooth Structure | nRET LD | Logistic | 0.973 | 1.03 * | 1.36 |
| nRET NR | Logistic | 0.996 | 1.09 * | 0.85 | |
| IST LD | Logistic | 0.969 | 1.79 * | 1.36 | |
| IST NR | Logistic | 0.992 | 1.53 * | 0.72 | |
| wIST LD | Logistic | 0.966 | 1.76 * | 1.84 | |
| wIST NR | Logistic | 0.994 | 1.51 * | 0.91 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Gomes de Carvalho, A.B.; de Andrade, G.S.; Mendes Tribst, J.P.; Grassi, E.D.A.; Ausiello, P.; Saavedra, G.d.S.F.A.; Bressane, A.; Marques de Melo, R.; Borges, A.L.S. Mechanical Behavior of Different Restorative Materials and Onlay Preparation Designs in Endodontically Treated Molars. Materials 2021, 14, 1923. https://doi.org/10.3390/ma14081923
Gomes de Carvalho AB, de Andrade GS, Mendes Tribst JP, Grassi EDA, Ausiello P, Saavedra GdSFA, Bressane A, Marques de Melo R, Borges ALS. Mechanical Behavior of Different Restorative Materials and Onlay Preparation Designs in Endodontically Treated Molars. Materials. 2021; 14(8):1923. https://doi.org/10.3390/ma14081923
Chicago/Turabian StyleGomes de Carvalho, Ana Beatriz, Guilherme Schmitt de Andrade, João Paulo Mendes Tribst, Elisa Donária Aboucauch Grassi, Pietro Ausiello, Guilherme de Siqueira Ferreira Anzaloni Saavedra, Adriano Bressane, Renata Marques de Melo, and Alexandre Luiz Souto Borges. 2021. "Mechanical Behavior of Different Restorative Materials and Onlay Preparation Designs in Endodontically Treated Molars" Materials 14, no. 8: 1923. https://doi.org/10.3390/ma14081923
APA StyleGomes de Carvalho, A. B., de Andrade, G. S., Mendes Tribst, J. P., Grassi, E. D. A., Ausiello, P., Saavedra, G. d. S. F. A., Bressane, A., Marques de Melo, R., & Borges, A. L. S. (2021). Mechanical Behavior of Different Restorative Materials and Onlay Preparation Designs in Endodontically Treated Molars. Materials, 14(8), 1923. https://doi.org/10.3390/ma14081923










