Direct 3D Printing of Clear Orthodontic Aligners: Current State and Future Possibilities
Abstract
1. Background
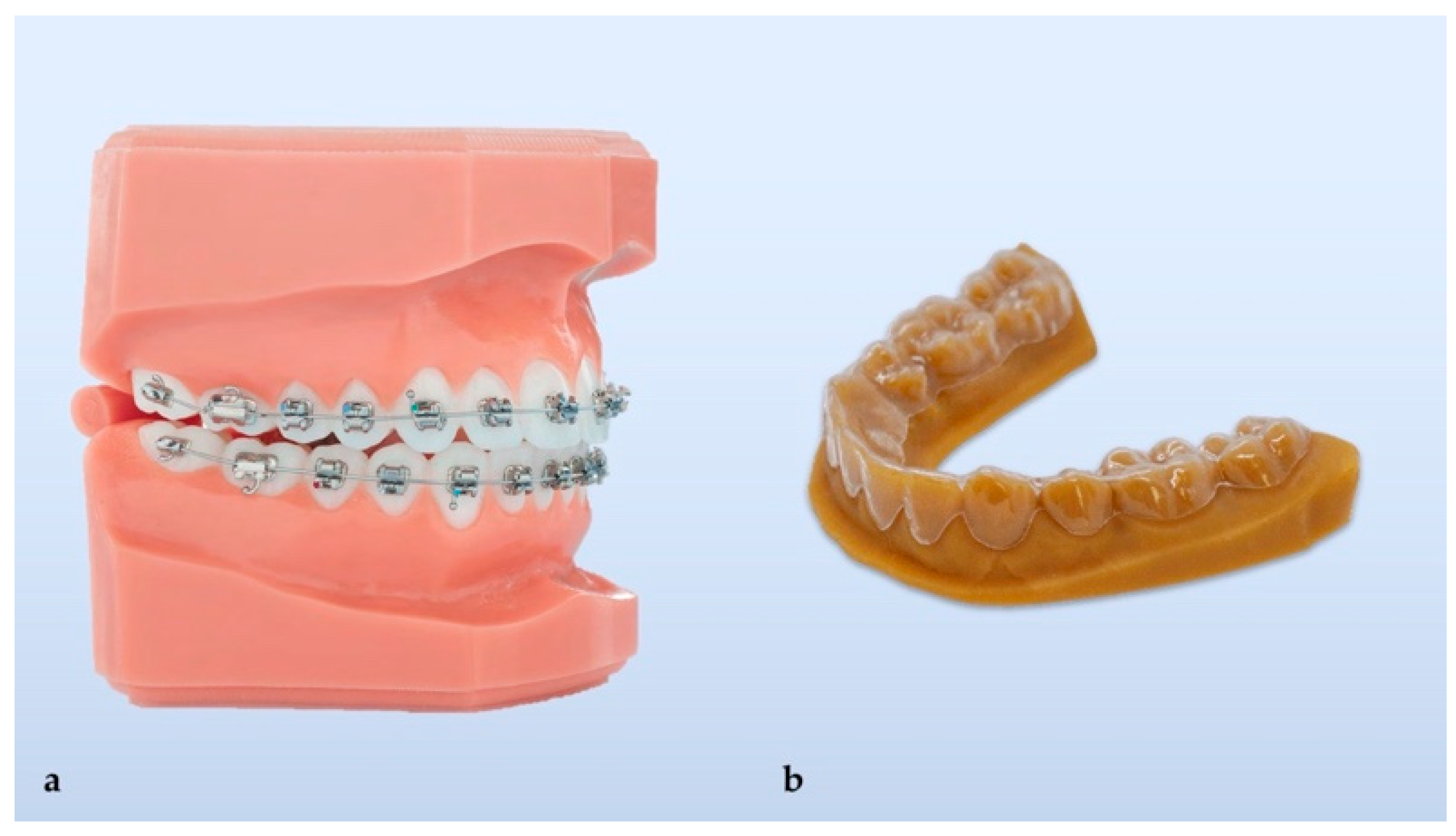
Brief History
2. Main Text
2.1. Development of Clear Aligners- Thermoforming
2.2. Materials for Thermoformed Aligners
2.3. Development of Clear Aligners- 3D Printing
2.4. Materials for 3D Printed Aligners
- borders are digitally designed and identically reproduced for all sets of aligners;
- edges are smooth and do not need trimming or polishing;
- undercuts do not exist because they are digitally defined;
- aligners are fabricated with higher precision as there are no errors introduced during printing of a 3D molding model and thermoforming stage of fabrication;
- higher precision leads to better fitting and higher effectiveness;
- intra-aligner thickness is customizable, and this may reduce the need for attachments, which generally lower the transparency of clear aligners.
3. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Zinelis, S.; Eliades, T.; Eliades, G.; Makou, M.; Silikas, N. Comparative assessment of the roughness, hardness, and wear resistance of aesthetic bracket materials. Dent. Mater. 2005, 21, 890–894. [Google Scholar] [CrossRef]
- Dobrin, R.J.; Kamel, I.L.; Musich, D.R. Load-deformation characteristics of polycarbonate orthodontic brackets. Am. J. Orthod 1975, 67, 24–33. [Google Scholar] [CrossRef]
- Kaur, S.; Singh, R.; Soni, S.; Garg, V.; Kaur, M. Esthetic orthodontic appliances-A review. Ann. Geriatr. Educ. Med. Sci. 2008, 5, 11–14. [Google Scholar]
- Leonardi, R. Cone-beam computed tomography and three-dimensional orthodontics. Where we are and future perspectives. J Orthod. 2019, 46, 45–48. [Google Scholar] [CrossRef]
- Bollen, A.M. Effects of malocclusions and orthodontics on periodontal health: evidence from a systematic review. J. Dent. Educ. 2008, 72, 912–918. [Google Scholar] [CrossRef]
- Chen, S.S.; Greenlee, G.M.; Kim, J.E.; Smith, C.L.; Huang, G.J. Systematic review of self-ligating brackets. Am. J. Orthod. Dentofacial. Orthop. 2010, 137, 726 e1–726 e18; discussion 726–727. [Google Scholar] [CrossRef]
- Rossini, G.; Parrini, S.; Castroflorio, T.; Deregibus, A.; Debernardi, C.L. Efficacy of clear aligners in controlling orthodontic tooth movement: a systematic review. Angle Orthod. 2015, 85, 881–889. [Google Scholar] [CrossRef]
- Shalish, M.; Cooper-Kazaz, R.; Ivgi, I.; Canetti, L.; Tsur, B.; Bachar, E.; Chaushu, S. Adult patients’ adjustability to orthodontic appliances. Part I: a comparison between Labial, Lingual, and Invisalign. Eur. J. Orthod. 2012, 34, 724–730. [Google Scholar] [CrossRef]
- Zheng, M.; Liu, R.; Ni, Z.; Yu, Z. Efficiency, effectiveness and treatment stability of clear aligners: A systematic review and meta-analysis. Orthod. Craniofac. Res. 2017, 20, 127–133. [Google Scholar] [CrossRef]
- Kesling, H.D. Coordinating the predetermined pattern and tooth positioner with conventional treatment. Am. J. Orthod. Oral. Surg. 1946, 32, 285–293. [Google Scholar] [CrossRef]
- Hennessy, J.; Al-Awadhi, E.A. Clear aligners generations and orthodontic tooth movement. J. Orthod. 2016, 43, 68–76. [Google Scholar] [CrossRef]
- Ercoli, F.; Tepedino, M.; Parziale, V.; Luzi, C. A comparative study of two different clear aligner systems. Prog. Orthod. 2014, 15, 31. [Google Scholar] [CrossRef]
- Pithon, M.M. A modified thermoplastic retainer. Prog. Orthod. 2012, 13, 195–199. [Google Scholar] [CrossRef]
- Weir, T. Clear aligners in orthodontic treatment. Aust. Dent. J. 2017, 62 (Suppl. 1), 58–62. [Google Scholar] [CrossRef]
- Martorelli, M.; Gerbino, S.; Giudice, M.; Ausiello, P. A comparison between customized clear and removable orthodontic appliances manufactured using RP and CNC techniques. Dent. Mater. 2013, 29, e1–e10. [Google Scholar] [CrossRef]
- Khosravani, M.R.; Reinicke, T. On the environmental impacts of 3D printing technology. Appl. Mater. Today 2020, 20, 100689. [Google Scholar] [CrossRef]
- Ryu, J.H.; Kwon, J.S.; Jiang, H.B.; Cha, J.Y.; Kim, K.M. Effects of thermoforming on the physical and mechanical properties of thermoplastic materials for transparent orthodontic aligners. Korean J. Orthod. 2018, 48, 316–325. [Google Scholar] [CrossRef] [PubMed]
- Bucci, R.; Rongo, R.; Levate, C.; Michelotti, A.; Barone, S.; Razionale, A.V.; D’Anto, V. Thickness of orthodontic clear aligners after thermoforming and after 10 days of intraoral exposure: a prospective clinical study. Prog. Orthod. 2019, 20, 36. [Google Scholar] [CrossRef] [PubMed]
- Tamburrino, F.; D’Anto, V.; Bucci, R.; Alessandri-Bonetti, G.; Barone, S.; Razionale, A.V. Mechanical Properties of Thermoplastic Polymers for Aligner Manufacturing: In Vitro Study. Dent. J. 2020, 8, 47. [Google Scholar] [CrossRef]
- Skaik, A.; Wei, X.L.; Abusamak, I.; Iddi, I. Effects of time and clear aligner removal frequency on the force delivered by different polyethylene terephthalate glycol-modified materials determined with thin-film pressure sensors. Am. J. Orthod. Dentofac. Orthop. 2019, 155, 98–107. [Google Scholar] [CrossRef]
- Gerard Bradley, T.; Teske, L.; Eliades, G.; Zinelis, S.; Eliades, T. Do the mechanical and chemical properties of Invisalign TM appliances change after use? A retrieval analysis. Eur. J. Orthod. 2015, 38, 27–31. [Google Scholar] [CrossRef]
- Ryokawa, H.; Miyazaki, Y.; Fujishima, A.; Miyazaki, T.; Maki, K. The mechanical properties of dental thermoplastic materials in a simulated intraoral environment. Orthod. Waves. 2006, 65, 64–72. [Google Scholar] [CrossRef]
- Martina, S.; Rongo, R.; Bucci, R.; Razionale, A.V.; Valletta, R.; D’Antò, V. In vitro cytotoxicity of different thermoplastic materials for clear aligners. Angle Orthod. 2019, 89, 942–945. [Google Scholar] [CrossRef]
- Shivapuja, P.; Shah, D.; Shah, N.; Shah, S. Direct 3D-Printed Orthodontic Aligners with Torque, Rotation, and Full Control Anchors. U.S. Patent No. 10,179,035, 15 January 2019. [Google Scholar]
- Prasad, S.; Kader, N.A.; Sujath, G.; Raj, T. 3D printing in dentistry. J. 3D Print. Med. 2018, 2, 89–91. [Google Scholar] [CrossRef]
- Nguyen, T.; Jackson, T. 3D technologies for precision in orthodontics. Semin. Orthod. 2018, 24, 386–392. [Google Scholar] [CrossRef]
- Jindal, P.; Juneja, M.; Siena, F.L.; Bajaj, D.; Breedon, P. Mechanical and geometric properties of thermoformed and 3D printed clear dental aligners. Am. J. Orthod. Dentofacial. Orthop. 2019, 156, 694–701. [Google Scholar] [CrossRef]
- Peeters, B.; Kiratli, N.; Semeijn, J. A barrier analysis for distributed recycling of 3D printing waste: Taking the maker movement perspective. J. Clean. Prod. 2019, 241, 118313. [Google Scholar] [CrossRef]
- Mohnish Kumar, S. Cytotoxicity of 3D Printed Materials: An In Vitro Study; Sri Ramakrishna Dental College and Hospital: Coimbatore, India, 2019. [Google Scholar]
- Jindal, P.; Worcester, F.; Siena, F.L.; Forbes, C.; Juneja, M.; Breedon, P. Mechanical behaviour of 3D printed vs thermoformed clear dental aligner materials under non-linear compressive loading using FEM. J. Mech. Behav. Biomed. Mater. 2020, 112, 104045. [Google Scholar] [CrossRef] [PubMed]
- Maspero, C.; Tartaglia, G.M. 3D Printing of Clear Orthodontic Aligners: Where We Are and Where We Are Going. Materials 2020, 13, 5204. [Google Scholar] [CrossRef] [PubMed]
- Edelmann, A.; English, J.D.; Chen, S.J.; Kasper, F.K. Analysis of the thickness of 3-dimensional-printed orthodontic aligners. Am. J. Orthod. Dentofac. Orthop. 2020, 158, e91–e98. [Google Scholar] [CrossRef]
- McCarty, M.C.; Chen, S.J.; English, J.D.; Kasper, F. Effect of print orientation and duration of ultraviolet curing on the dimensional accuracy of a 3-dimensionally printed orthodontic clear aligner design. Am. J. Orthod. Dentofac. Orthop. 2020, 158, 889–897. [Google Scholar] [CrossRef] [PubMed]
- Jindal, P.; Juneja, M.; Bajaj, D.; Siena, F.L.; Breedon, P. Effects of post-curing conditions on mechanical properties of 3D printed clear dental aligners. Rapid. Prototyp. J. 2020, 26, 1337–1344. [Google Scholar] [CrossRef]
- Aravind Shanmugasundaram, S.; Razmi, J.; Mian, M.J.; Ladani, L. Mechanical Anisotropy and Surface Roughness in Additively Manufactured Parts Fabricated by Stereolithography (SLA) Using Statistical Analysis. Materials 2020, 13, 2496. [Google Scholar] [CrossRef] [PubMed]
- Ahamed, S.F.; Kumar, S.M.; Vijaya kumar, R.K.; Kanna, S.A.; Indrapriya dharshini, K. Cytotoxic evaluation of directly 3D printed aligners and Invisalign. Eur. J. Mol. 2020, 7, 1129–1140. [Google Scholar]
- EnvisionTEC. Available online: https://envisiontec.com/orthodontic-materials-launched-at-lmt-lab-day-chicago (accessed on 11 November 2019).
- Nakano, H.; Kato, R.; Kakami, C.; Okamoto, H.; Mamada, K.; Maki, K. Development of Biocompatible Resins for 3D Printing of Direct Aligners. JPST 2019, 32, 209–216. [Google Scholar] [CrossRef]
- Barone, S.; Paoli, A.; Razionale, A.V.; Savignano, R. Computational design and engineering of polymeric orthodontic aligners. Int. J. Numer. Method Biomed. Eng. 2017, 33, e2839. [Google Scholar] [CrossRef]



| Brand | Material Composition | Density (g/cm3) | Elastic Modulus (MPa) | Tensile Stress (MPa) | Elongation at Break (%) | Cell Viability (%) | Cytotoxicity |
|---|---|---|---|---|---|---|---|
| Duran (Scheu-Dental GmbH) (T) | Polyethylene terephthalate glycol (PET-G) | 1.27 | 2200 | 53 | >40 | 84.6 (Day 14) | Slight |
| Biolon (Dreve Dentamid GmbH) (T) | Polyethylene terephthalate glycol (PET-G) | 1.27 | 2020 | 45 | >35 | 64.6 (Day 14) | Slight |
| Zendura (Bay Material LLC) (T) | Polyurethane resin (PU) | 1.203 | - | - | - | 74.4 (Day 14) | Slight |
| SmartTrack (Align Technology) (T) | Multilayer aromatic thermoplastic polyurethane/copolyester | - | - | - | - | 94.1 (Day 7) 78.8 (Day 14) | Slight |
| Dental LT (Formlabs Inc.) (P) | Photo polymeric clear methacrylate oligomer and glycol methacrylate | 1.1 1.3 | 2300 | 84 | 12 | 60.3 (Day 1) 62.5 (Day 14) | Slight |
| Accura 60 SLA (3D System) (P) | Polycarbonate-based photo-polymeric resin | 1.13 1.21 | 2690–3100 | 58–68 | 5–13 | 13.9 (Day 1) 24.5 (Day 7) | Severe |
| E-Guard (EnvisionTEC) (P) | Photo-polymeric clear resin | 1.06 1.12 | 2050–2130 | 79–85 | 3.81 | 64.1 (Day 1) 75.1 (Day 7) | Slight |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Tartaglia, G.M.; Mapelli, A.; Maspero, C.; Santaniello, T.; Serafin, M.; Farronato, M.; Caprioglio, A. Direct 3D Printing of Clear Orthodontic Aligners: Current State and Future Possibilities. Materials 2021, 14, 1799. https://doi.org/10.3390/ma14071799
Tartaglia GM, Mapelli A, Maspero C, Santaniello T, Serafin M, Farronato M, Caprioglio A. Direct 3D Printing of Clear Orthodontic Aligners: Current State and Future Possibilities. Materials. 2021; 14(7):1799. https://doi.org/10.3390/ma14071799
Chicago/Turabian StyleTartaglia, Gianluca M., Andrea Mapelli, Cinzia Maspero, Tommaso Santaniello, Marco Serafin, Marco Farronato, and Alberto Caprioglio. 2021. "Direct 3D Printing of Clear Orthodontic Aligners: Current State and Future Possibilities" Materials 14, no. 7: 1799. https://doi.org/10.3390/ma14071799
APA StyleTartaglia, G. M., Mapelli, A., Maspero, C., Santaniello, T., Serafin, M., Farronato, M., & Caprioglio, A. (2021). Direct 3D Printing of Clear Orthodontic Aligners: Current State and Future Possibilities. Materials, 14(7), 1799. https://doi.org/10.3390/ma14071799










